Abstract
A 65-year-old male post-CABG surgery presented with history of ventricular storm refractory to antiarrhythmics and requiring multiple DC shocks. He got posted for VATs bilateral cardiac denervation for sympathetic remodulation. Patient was induced with high dose opioids and Etomidate and intubated with 37Fr left double lumen tube. A multidisciplinary approach was planned to tackle peri-operative cardiac event along with the placement of invasive monitors. Events that might lead to sympathetic overactivation because of laryngoscopy, pain, capnothorax, and surgical handling were kept in mind and avoided with optimum depth of anesthesia, analgesia, and pharmacological sympatholysis. There was no major cardiac event intraoperatively as well as in postoperative period.
Keywords: Cardiac sympathectomy, VATs, ventricular storm
INTRODUCTION
Electrical storm (ES) is defined as the occurrence of two or more hemodynamically unstable ventricular tachycardia (VT) and/or ventricular fibrillation (VF) in 24 h, requiring electrical cardioversion or defibrillation.[1] Delayed effect onset, no guarantee of prevention with anti-arrhythmics and noncurative nature of AICD with increased morbidity because of repeated shocks led to introduction of cardiac ablation therapy and surgical bilateral cardiac sympathetic denervation (CSD) in case of refractory ES. The technical difficulties and high failure rate of ablation therapy has made surgical cardiac denervation more popular. It leads to cardiac sympathetic modulation and reduces frequency of VT/VF. In this case report, we elaborate the perioperative management of VATs bilateral CSD for ES.
CASE HISTORY
A 65-year-old male weighing 43 kg, post-coronary artery bypass surgery (LIMA to distal LAD) in 2011 presented to another tertiary care centre with a syncopal attack in Nov 2019. Electrocardiography showed monomorphic ventricular tachycardia with rate of 137/min which was reverted with 200J DC shock. However, he developed multiple episodes of VT for which DC shocks were given multiple times and standard protocol for management of refractory ventricular arrhythmias including ruling out electrolyte imbalance, acidosis, and antiarrhythmic drugs including infusion of Inj Amiodarone 150 mg bolus over 10 min followed by 1 mg/min over first 6 h and 0.5 mg/min over next 18 h were started. Finally, patient had to be sedated and temporarily put on mechanical ventilation. History also revealed insertion of thoracic epidural twice in a month. Both the modalities were opted in order to evade sympathetic activation and break the arrhythmogenic circuit. A decision of VATS bilateral CSD was taken to decrease frequency of ventricular tachycardia and amount of shocks for the AICD that was planned in the future to avoid sudden cardiac death.
Patient was shifted to our institute for bilateral sympathectomy with rate and rhythm controlled at 70/min with Tab Amiodarone 200 mg OD and Tab Metoprolol XL 25 mg OD. Transthoracic echocardiography showed EF of 30% with global LV hypokinesia. CART done, 6 months back in view of intermittent chest pain and giddiness showed 40–50% LAD stenosis, 70% LCX stenosis and complete occlusion of RCA, however patient refused to undergo redo CABG due to risk involved because of severely compromised systolic function and failure to perform PTCA because of right subclavian occlusion. The patient was on T Aspirin and T Clopidogrel 75 mg each. All antiarrhythmic agents were continued till the morning of surgery. A multidisciplinary approach was planned including cardiologists and cardiothoracic surgeon to tackle perioperative cardiac events and insertion of intra-aortic balloon pump if required.
Standard perioperative care monitors were attached along with the defibrillator gel pads in antero-posterior position. Patient was induced with Inj Fentanyl 3 mcg/kg plus Inj Etomidate 0.3 mg/kg and intubated with 37Fr left DLT after adequate relaxation with Vecuronium. Carinal response was avoided with 2 min prior injection of 2% Loxicard sprayed beyond vocal cords under vision.[2] Position of DLT and adequacy of one lung ventilation was confirmed by auscultation after occlusion of respective port. Right femoral artery was cannulated and transduced for beat to beat blood pressure monitoring. Left IJV access was secured under USG guidance because of presence of thrombus in the right IJV. Supine position with 30° head up was given with both the arms abducted to 90° [Figure 1]. Vitals were stable throughout the induction. The depth of anesthesia was maintained with intermittent injection of Fentanyl and MAC of 0.9 with sevoflurane.
Figure 1.

Position of the Patient for surgery
Left one lung ventilation was achieved with TV = 4-6 ml/kg, PEEP = 7, FiO2 = 70%. Saturation was maintained up to 92–93%. Respiratory rate was adjusted based on End tidal CO2, so that EtCO2 was maintained between 50 and 55 cm H2O with PaCO2 of 55–60 mm hg on ABG. Similar adjustments were repeated on right side. However, saturation levels were better with right lung ventilation. Sympathetic denervation from T2–T4 along with excision of half of the stellate ganglion was done first on the right side followed by the left [Figures 2 and 3]. Intra-ganglionic 2% Loxicard was given prior to clamping. A cautery firing was done along the lower border of second and third rib for ablation of Nerve of Kuntz. Dual lung ventilation was done till the preparation of the either side and insertion of the first port. Despite lower CO2 flow rates, intermittent bilateral lung ventilation and low insufflation pressures, higher PCO2 values were observed in the serial ABGs done intraoperatively. Thus, patient was electively ventilated with 8 mm single lumen tube post procedure and extubated once alert and responsive. There was no major cardiac event intraoperatively as well as in postoperative period and patient was shifted back to the institute from which he was referred on day three.
Figure 2.
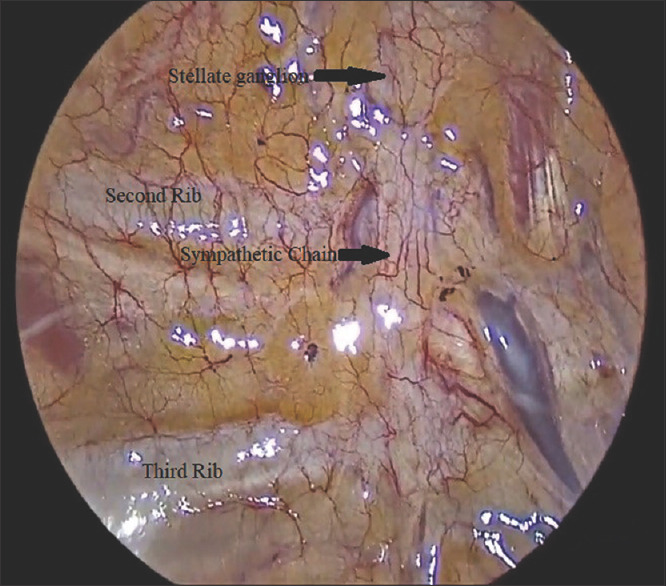
Sympathetic chain with stellate ganglion
Figure 3.
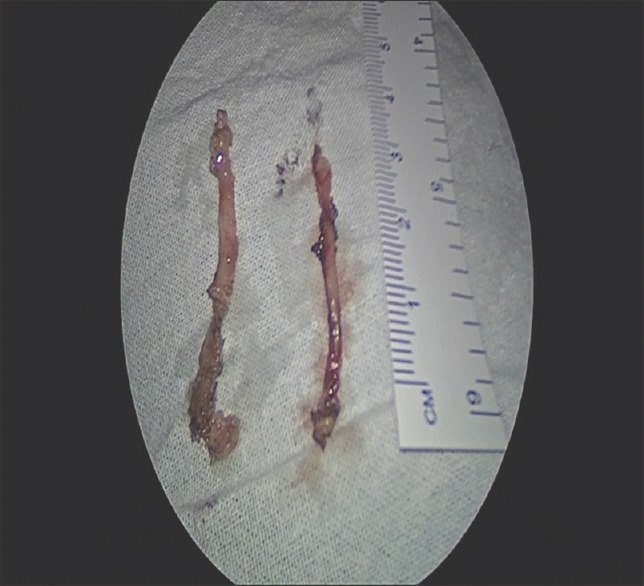
Removed Left and Right Sympathetic chains (Half T2-T4)
DISCUSSION
The management of ventricular storm poses a unique challenge to anesthesiologists because of high immediate cardiac mortality risk. Therefore, a vigilant plan of anesthesia was formulated for our patient to tackle intraoperative hemodynamic instability, arrhythmias, and cardiac arrest. Another major challenge was management of complicated respiratory changes and sympathetic activation secondary to capnothorax with single lung ventilation.
Upper thoracic epidural infusion with local anesthetic has been recommended by many authors with advantages of pharmacological sympathetic denervation as well as intraoperative analgesia.[2,3] However, both, epidural/paravertebral block[4,5] were not given to our patient as he was on clopidogrel because of presence of right Subclavian artery thrombosis. Induction with high dose opioids and local anesthetic spray over carina aided smooth intubation.[2] Despite, Wong RY[6] and A. Martin[7] suggestion of VATS with single lumen tube to avoid misplacement and maintenance of better oxygenation, we opted for DLT with intrathoracic CO2 insufflation for better surgical access.[7] However, fibreoptic confirmation of DLT was not done because of unavailability of pediatric scope in our OT. Right sympathectomy was done first in our patient because of technical difficulties on left side but that gave us the advantage of better hemodynamic stability.[8,9] M. Vaseghi et al.[10] however recommends operating left side first in cases of ventricular storm as patient may not be able to tolerate single lung ventilation. Prior intra-ganglionic instillation of Loxicard avoided sympathetic activation during manipulation of the sympathetic chain. Two theoretical complications were Horner's syndrome and reduced myocardial contractility secondary to sympatholysis. The incidence of Horner's syndrome is close to nil when only half of the stellate ganglion is removed.
Methangkool et al[11] in their case series were required to give ionotropic support in 50% of the patients and observed perioperative mortality in 2 out of 26 patients. Though a transient drop in heart rate and blood pressure was observed on either sympathectomy in our patient, no active intervention was needed intraoperatively as well as in first 24 h period.
One lung ventilation with DLT has potential for intraoperative hypoxia in previously healthy lungs, more so on the second operating side because of residual atelectasis and impaired hypoxic pulmonary vasoconstriction.[7] This though expected was not observed in our patient. A slight fall in saturation with right lung down was managed by increasing FiO2, MAC < 1, intermittent recruitment.
CONCLUSION
The key to management for ventricular storm is to keep the sympathetic activation or the arrhythmogenic trigger at bay. Optimum analgesia, co-ordinated titration of depth of anaesthesia and intra-ganglionic injection of Loxicard prior to handling of sympathetic chain helped us avoid sympathetic stimulation even though epidural sympathetic denervation could not be achieved.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Eifling M, Razavi M, Massumi A. The evaluation and management of electrical storm. Texas Hear Inst J. 2011;38:111–21. [PMC free article] [PubMed] [Google Scholar]
- 2.Pirlich N, Lohse JA, Noppens RR. Topical airway anesthesia for awake-endoscopic intubation using the spray-as-you-go technique with high oxygen flow? J Vis Exp. 2017;2017:1–5. doi: 10.3791/55116. doi: 10.3791/55116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Do DH, Bradfield J, Ajijola OA, Vaseghi M, Le J, Rahman S, et al. Thoracic epidural anesthesia can be effective for the short-term management of ventricular tachycardia storm. J Am Heart Assoc. 2017;6:e007080. doi: 10.1161/JAHA.117.007080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahajan A, Moore J, Cesario DA, Shivkumar K. Use of thoracic epidural anesthesia for management of electrical storm: A case report. Hear Rhythm. 2005;2:1359–62. doi: 10.1016/j.hrthm.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 5.D’Ercole F, Arora H, Kumar PA. Paravertebral block for thoracic surgery. J Cardiothorac Vasc Anesth. 2018;32:915–27. doi: 10.1053/j.jvca.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 6.Wong RY, Fung ST, Jawan B, Chen HJ, Lee JH. Use of a single lumen endotracheal tube and continuous CO2 insufflation in transthoracic endoscopic sympathectomy. Acta Anaesthesiol Sin. 1995;33:21–6. [PubMed] [Google Scholar]
- 7.Martin A, Telford R. Anaesthesia for endoscopic thoracic sympathectomy. Contin Educ Anaesthesia, Crit Care Pain. 2009;9:52–5. [Google Scholar]
- 8.Upadya M, Misquith JCR, Rao R. Anaesthesia for left thoracoscopic sympathectomy for refractory long QT syndrome: Three case reports. South African J Anaesth Analg. 2016;22:156–9. [Google Scholar]
- 9.Kharbanda M, Prasad A, Malik A. Right or left first during bilateral thoracoscopy? Surg Endosc. 2013;27:2868–76. doi: 10.1007/s00464-013-2843-5. [DOI] [PubMed] [Google Scholar]
- 10.Vaseghi M, Gima J, Kanaan C, Ajijola OA, Marmureanu A, Mahajan A, et al. Cardiac sympathetic denervation in patients with refractory ventricular arrhythmias or electrical storm: Intermediate and long-term follow-up. Hear Rhythm. 2014;11:360–6. doi: 10.1016/j.hrthm.2013.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Methangkool E, Chua JH, Gopinath A, Shivkumar K, Mahajan A. Anesthetic considerations for thoracoscopic sympathetic ganglionectomy to treat ventricular tachycardia storm: A single-center experience. J Cardiothorac Vasc Anesth. 2014;28:69–75. doi: 10.1053/j.jvca.2013.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]


