Abstract
The aim of the present study was to evaluate the possible utilization of saliva and urine as alternative samples to serum for the diagnosis of human immunodeficiency virus (HIV) infection. A total of 302 individuals participated in the study: 187 HIV-infected individuals (106 had Centers for Disease Control and Prevention [CDC] stage II infection, 19 had CDC stage III infection, and 62 had CDC stage IV infection) and 115 noninfected persons (46 of the noninfected persons were blood donors and 69 belonged to a group at high risk of HIV infection). Paired saliva and urine samples were taken from each of the participants in the study. The presence of HIV-specific antibodies was detected by an enzyme-linked fluorescent assay (ELFA), and the result was confirmed by Western blot analysis (WB). The ELFA with saliva gave maximum sensitivity and specificity values, while ELFA had lower sensitivity (95.2%) and specificity (97.4%) values for detection of HIV antibody in urine samples. WB with all saliva samples fulfilled the World Health Organization criterion for positivity, while only 96.8% of the urine samples were confirmed to be positive by WB. Among the four reactivity patterns found by WB of these alternative samples, the most frequent included bands against three groups of HIV structural proteins (was ENV, POL, and GAG). The reactivity bands most frequently observed were those for the proteins gp160 and gp120. The least common reactivity band was the band for protein p17. The detection of HIV antibodies in saliva samples by means of ELFA with the possibility of later confirmation by WB makes saliva an alternative to serum for possible use in the diagnosis of infection. In contrast, HIV antibody detection in urine samples by the same methodology (ELFA) could be taken into consideration for use in epidemiological studies.
Over the past few years, deep interest has been shown in the possible use of samples other than serum for the diagnosis of infection or screening for various infectious processes (1, 4–8, 33, 37, 45). Among these, infection caused by the human immunodeficiency virus (HIV) has been the most evaluated (38). Traditionally, tests for the detection of HIV infection have been based on the detection of HIV antibodies in serum or plasma derived from whole blood collected by venipuncture and hence require trained health care workers for collection and laboratory facilities for testing. Among these alternative biological fluids, saliva has already been considered an option in numerous studies (11, 17, 24, 25, 27, 34, 40, 41, 44); in fact, the U.S. Food and Drug Administration has authorized the use of an oral device for the collection of saliva for HIV antibody screening (42).
Whole saliva is a mixture consisting of the secretions of the salivary glands together with oral cavity microorganisms, cells, and a gingival-crevicular transudate (GCT). GCT is a fluid into which immunoglobulins and other blood components passing through the mucosae to the oral cavity are passively excreted. Mortimer and Parry (32) have already shown that the GCT of HIV-infected individuals contains high concentrations of HIV-specific immunoglobulin G (IgG) antibodies. This antibody concentration is certainly lower than that found in serum but is quite sufficient to render GCT an adequate sample for anti-HIV antibody detection under certain conditions.
Use of this type of sample affords clear advantages, such as easy, rapid sample collection that does not require specialized personnel, a minimization of contamination risk for health professionals, a lack of trauma for the patient, and applicability to special population groups for whom blood sample collection is difficult (e.g., individuals addicted to parenterally administered drugs).
Meanwhile, other biological fluids with similar advantages, such as urine, are still being evaluated by various groups (10, 15, 16, 36).
The goal of the study described here was to evaluate GCT and urine samples as possible alternatives to serum for the detection of HIV antibodies with an automated system optimized for these sample types and confirmation by Western blot analysis (WB). The use of paired samples from the same individual facilitates better evaluation of the sensitivity and specificity of the technique with these alternative samples.
MATERIALS AND METHODS
A total of 302 individuals participated in the study: 187 infected with HIV type 1 (HIV-1) (106 had Centers for Disease Control and Prevention [CDC] stage II infection, 19 had CDC stage III infection, and 62 had CDC stage IV infection) and 115 noninfected individuals (46 blood donors were from the University Hospital of Valladolid’s Hematology Service and 69 persons belonged to a group at high risk of HIV infection). Paired GCT and urine samples were taken from each participant.
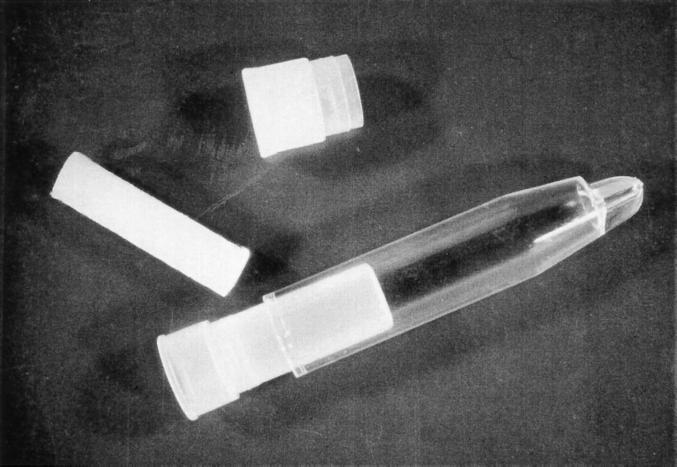
GCT samples were collected with an oral device (Salivette; Sarstedt, Leicester, United Kingdom). The Salivette is a cylinder of cotton wool inside a double polystyrene tube with a snap top (Fig. 1). The cylinder was held in the lateral gingival fold as long as required for the individual to perceive that it had become sufficiently hydrated with GCT to go limp. The participants themselves would then insert the cylinder into the inner tube. The oral devices were centrifuged (4,000 × g for 15 min), and the resulting transparent fluid was aliquoted and kept frozen at −70°C until processing.
FIG. 1.
Oral device used for collection of GCT samples.
Urine samples were obtained through simple miction, placed in a sterile container, and preserved at 4°C until analysis (less than 2 months).
All samples were analyzed by means of an automated technique (VIDAS HIV 1+2; bioMérieux, Lyon, France) designed to detect IgG-type immunoglobulins against antigens HIV-1 and HIV type 2 (HIV-2) (synthetic peptides gp41 and gp36) in serum. This enzyme-linked fluorescent assay (ELFA) associates a final automated fluorescence reading with an indirect immunoenzymatic method. The HIV antibody detection equipment features a disposable single-use cone which serves both as an antigen holder and as a pipette system for samples and reagents. The reagents are found in ready-to-use cartridges with various recessed cups where the different reaction phases occur. The sample volume required is 100 μl in all cases. The technique provides concentrations directly related to the fluorescence detected in the reading (the alkaline phosphatase catalyzes the substrate’s conversion into a fluorescent 4-methyl-umbelliferyl product through liberation of the phosphate). The final readings are given as relative fluorescence values (RFVs).
The system was adapted to detect IgG-type immunoglobulins in GCT and urine samples. The RFVs obtained with the GCT and urine samples belonging to the group of noninfected individuals were used to find the cutoff (10 times the average RFV obtained with GCT samples [cutoff, 1 × 10 = 10 RFVs]; 4 times the average RFV obtained with urine samples [cutoff, 2.5 × 4 = 10 RFVs]). Samples with RFVs above 10 were considered to be positive, and those with RFVs equal to or less than 10 RFVs were considered to be negative.
All samples were processed according to the manufacturer’s instructions, with only one HIV antibody test performed with each sample type (GCT and urine).
The positive samples and negative samples belonging to seropositive individuals were confirmed by WB (Bioblot HIV-1 plus; Genelabs Diagnostic, Geneva, Switzerland). The WB combined purified HIV-1 antigens (corresponding to structural genes env, gag, and pol) with an HIV-2 synthetic peptide (gp36) in one strip. Each strip contained a serum control (human anti-immunoglobulin antibody).
The dilutions used were 1/10 (200 μl of GCT plus 1,800 μl of blotting buffer) for the GCT samples and 3/4 (1,500 μl of urine plus 500 μl of blotting buffer) for the urine samples. The GCT and urine samples were incubated for 16 to 20 h.
The 1990 World Health Organization (WHO) criterion was used as positive (reactivity to two bands including bands for gp41, gp120, or gp160) (46). Samples that did not meet this criterion but that displayed reactivities to other bands were classified as indeterminate. Negative samples did not display any reactive bands.
The result of the WB confirmation of HIV antibodies with serum was used as the “gold standard” for sensitivity and specificity calculations. Bonferroni’s test was used to evaluate the significance between the RFVs thus obtained.
In order to find the most appropriate time for the collection of alternative samples, a preliminary trial was run before the material used in the study was obtained to evaluate possible variations in the elimination of HIV antibodies throughout the day in the same individual. To do so, six individuals with CDC stage II infection were asked at random to cooperate. They were tracked over 24 h. Sample collection (urine and GCT simultaneously) began when they woke up in the morning and then continued throughout the 24-h period with no set schedule; every time that they needed to urinate, both GCT and urine samples were collected as described above. All samples were analyzed by ELFA, and the result was confirmed by WB by the procedures described above. In all cases at least four paired saliva and urine samples were collected from the same participant.
RESULTS
All 187 GCT samples from infected individuals were reactive by ELFA (Table 1). Likewise, all GCT samples from noninfected individuals were negative. These results provided sensitivity and specificity values of 100% and positive and negative predictive values of 1 (P < 0.0001).
TABLE 1.
Confirmation of ELFA reactivities by WB of GCT samples
| Group | No. of GCT samples with the indicated results for HIV antibodies by the following assay:
|
No. of WBpb | ||
|---|---|---|---|---|
| Total | ELFA positive | WB positivea | ||
| CDC stage II | 106 | 106 | 106 | 106 |
| CDC stage III | 19 | 19 | 19 | 19 |
| CDC stage IV | 62 | 62 | 62 | 62 |
| Individuals with high risk of HIV infection | 69 | 0 | ||
| Blood donors | 46 | 0 | ||
| Total | 302 | 187 | 187 | 187 |
None of the samples had a negative or indeterminate result.
WBp, serum samples with a positive WB result.
Detection of HIV antibodies in urine samples was positive by ELFA for 181 individuals (Table 2). Of these, 178 were individuals with some stage of HIV infection (102 with CDC stage II infection, 19 with CDC stage III infection, and 57 with CDC stage IV infection), and 3 were noninfected individuals. Nine samples from seropositive individuals were negative by ELFA (four and five samples belonging to individuals with CDC stage II and IV infections, respectively). Of the 115 urine samples from seronegative persons, only 3 urine samples displayed reactivity by the ELFA technique (1 sample belonged to the donor group and the other 2 belonged to the group of individuals with high risk of HIV infection). These results yield a sensitivity of 95.2% and a specificity of 97.4%, with a positive predictive value and a negative predictive value of 0.98 and 0.93, respectively (P < 0.0001).
TABLE 2.
Confirmation of ELFA reactivities by WB of urine samples
| Group | No. of urine samples with the indicated results for HIV antibodies by the following assay:
|
No. of WBpa | ||||
|---|---|---|---|---|---|---|
| Total | ELFA positive | WB
|
||||
| Posi-tive | Nega-tive | Indeter-minate | ||||
| CDC stage II | 106 | 102 | 104b | 2b | 106 | |
| CDC stage III | 19 | 19 | 19 | 19 | ||
| CDC stage IV | 62 | 57 | 58c | 2b | 2b | 62 |
| Individuals in a group at high risk | 69 | 2 | 2 | |||
| Blood donors | 46 | 1 | 1 | |||
| Total | 302 | 181 | 181 | 7 | 2 | 187 |
WBp, serum samples with a positive WB result.
Includes two ELFA-negative samples.
Includes one ELFA-negative sample.
The distribution of RFVs with GCT and urine samples can be seen in Tables 3 and 4, respectively. It can be seen from the data in Table 3 that 77% of the samples from seropositive individuals yielded an RFV of over 200, with no samples having values equal to or less than 10 RFVs. In Table 4 it can be seen that only 24.1% of the urine samples from HIV-seropositive individuals had RFVs of >200, while 5.3% of the samples had negative RFVs (four samples from individuals with CDC stage II infection and five samples from individuals with CDC stage IV infection). On the other hand, the seronegative individuals displayed very similar RFVs: an RFV of 0 for 47.8% of GCT samples and 44.3% of urine samples and RFVs of between 1 and 10 for 52.2 and 54.9% for GCT and urine samples, respectively. Among the samples from noninfected persons, three urine samples were positive by ELFA, with RFVs in the range of 11 to 50.
TABLE 3.
Distribution of RFVs for GCT samples from different population groups
| Group | No. of samples with the following RFVs:
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Total | 0 | 1–10 | 11–50 | 51–200 | 201–500 | 501–1,000 | >1,000 | |
| CDC stage II | 106 | 11 | 27 | 17 | 51 | |||
| CDC stage III | 19 | 6 | 4 | 4 | 5 | |||
| CDC stage IV | 62 | 14 | 12 | 12 | 10 | 14 | ||
| Individuals in a group at high risk | 69 | 33 | 36 | |||||
| Blood donors | 46 | 22 | 24 | |||||
| Total | 302 | 55 | 60 | 14 | 29 | 43 | 31 | 70 |
TABLE 4.
Distribution of RFVs for urine samples from different population groups
| Group | RFV
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Total | 0 | 1–10 | 11–50 | 51–200 | 201–500 | 501–1,000 | >1,000 | |
| CDC stage II | 106 | 2 | 2 | 21 | 54 | 15 | 3 | 8 |
| CDC stage III | 19 | 12 | 5 | 2 | ||||
| CDC stage IV | 62 | 3 | 2 | 29 | 11 | 11 | 4 | 2 |
| Individuals with high risk of HIV infection | 69 | 29 | 38 | 2 | ||||
| Blood donors | 46 | 21 | 24 | 1 | ||||
| Total | 302 | 55 | 66 | 65 | 70 | 26 | 9 | 10 |
The average RFVs for GCT and urine samples from seropositive individuals were 1,946 ± 3,153 and 409 ± 980, respectively. Statistical comparison of the RFVs for samples from the HIV-infected groups did not show any significant differences between RFVs belonging to individuals with CDC stage II, III, and IV infections (Bonferroni’s test). This was true for both the GCT and the urine samples. However, significant differences were found between each of these HIV infection stages and the values obtained for noninfected groups.
The ELFA results were confirmed by WB. All GCT samples reactive by ELFA fulfilled the WHO criterion for positivity (Table 1). In contrast, among the WBs performed with 190 urine samples, only 181 met the positivity criterion (96.8%) (Table 2). The samples were distributed by stage as follows: 104 samples belonged to individuals with CDC stage II infection (2 samples were negative by ELFA), 19 samples belonged to individuals with CDC stage III infection, and 58 samples belonged to individuals with CDC stage IV infection (1 sample was negative by ELFA). The seven samples with negative WB results included two urine samples each from individuals with CDC stage II and IV infections (the samples were negative by ELFA), one sample from the blood donor group (the sample was positive by ELFA), and two samples from the group of individuals in a group at high risk of HIV infection (the samples were positive by ELFA). Finally, two samples with indeterminate WB results were found (the samples were from individuals with CDC stage IV infection) and had bands that were reactive to proteins gp160 and gp41, respectively (both samples were negative by ELFA).
The reactivity band most frequently observed by WB was the gp160 protein band (in 100% of GCT samples versus 97.3% of urine samples), and the least common reactivity band was the p17 protein band (in 31.5% of GCT samples versus 21.4% of urine samples) (Tables 5 and 6). The arithmetic mean of the observed number of bands was 6.7 for GCT and 6.5 for urine. Nevertheless, 23.2% of the WBs run with GCT samples showed all nine bands, while 32.2% of the WBs run with urine samples yielded five or fewer reactive bands. In the WBs with GCT proportion dropped to 25.5%.
TABLE 5.
Reactivity patterns of GCT samples from HIV-infected individuals by WB for HIV
| Reactivity pattern | No. (%) of samples with the following bands by WB:
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | ENV
|
POL
|
GAG
|
|||||||
| gp160 | gp120 | gp41 | p66 | p51 | p31 | p55 | p24 | p17 | ||
| ENV | 9 | 9 | 9 | 6 | 0 | 0 | 0 | 0 | 0 | 0 |
| ENV + GAG | 9 | 9 | 9 | 7 | 0 | 0 | 0 | 2 | 9 | 0 |
| ENV + POL | 21 | 21 | 21 | 16 | 7 | 6 | 21 | 0 | 0 | 0 |
| ENV + POL + GAG | 148 | 148 | 148 | 145 | 113 | 126 | 130 | 105 | 138 | 59 |
| Total | 187 | 187 (100) | 187 (100) | 174 (93) | 120 (64.2) | 132 (70.6) | 151 (80.8) | 107 (57.2) | 147 (78.6) | 59 (31.5) |
TABLE 6.
Reactivity patterns of urine samples from HIV-infected individuals by WB for HIV
| Reactivity pattern | No. (%) of samples with the following bands by WB:
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | ENV
|
POL
|
GAG
|
|||||||
| gp160 | gp120 | gp41 | p66 | p51 | p31 | p55 | p24 | p17 | ||
| ENV | 9 | 8 | 7 | 7 | 0 | 0 | 0 | 0 | 0 | 0 |
| ENV + GAG | 8 | 8 | 8 | 4 | 0 | 0 | 0 | 1 | 7 | 1 |
| ENV + POL | 31 | 31 | 31 | 22 | 11 | 6 | 26 | 0 | 0 | 0 |
| ENV + POL + GAG | 135 | 135 | 135 | 131 | 105 | 120 | 122 | 108 | 129 | 39 |
| None | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 187 | 182 (97.3) | 181 (96.8) | 164 (87.7) | 116 (62.0) | 126 (67.4) | 148 (79.1) | 109 (58.3) | 136 (72.7) | 40 (21.4) |
Only 1.6 and 0.5% of the WBs with GCT and urine, respectively, had the minimum WHO criterion for positivity, since the Western blots displayed only two bands, those for the envelope proteins (gp160 and gp120). In the Western blots with three bands (5.3% of GCT samples versus 6.4% of urine samples), in addition to the bands of reactivity to proteins gp160 and gp120, reactivity was observed to other proteins: gp41 (60% of GCT samples versus 50% of urine samples), p24 (20% of GCT samples versus 25% of urine samples), and p31 (20% of GCT samples versus 25% of urine samples).
Only WBs with urine samples displayed one reactive band (indeterminate WB results belonging to samples from individuals with CDC stage IV infection had two reactive bands to proteins gp160 and gp41, respectively).
Four reactivity patterns were observed for both types of samples: ENV (4.8% of GCT samples versus 4.8% of urine samples), ENV plus POL (11.2% of GCT samples versus 16.6% of urine samples), ENV plus GAG (4.8% of GCT samples versus 4.3% of urine samples), and ENV, POL, and GAG (79.2% of GCT samples versus 72.2% of urine samples).
Finally, Table 7 gives the results from the ELFA analysis of the GCT and urine samples taken over a 24-h period from a group of six volunteers infected with HIV (CDC stage II infection). These results draw attention to the disproportionate RFVs between the RFVs found for GCT samples and their paired urine samples. In general, the RFVs for the GCT samples were always higher. The RFVs for samples subsequently obtained from each individual were similar. The same was true for urine samples. There seems to exist a certain parallel between the RFVs for GCT and urine samples from the same individual.
TABLE 7.
Evolution of RFVs in GCT and urine samples over a 24-h period
| Individuala | RFV in GCT (urine) samples for the following sample no.:
|
||||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | S-5 | S-6 | S-7 | |
| A | 438 (53) | 282 (83) | 228 (56) | 431 (17) | 1,035 (43) | ||
| B | 477 (90) | 370 (20) | 177 (18) | 210 (21) | |||
| C | 3,404 (200) | 5,141 (341) | 4,066 (435) | 5,709 (372) | 7,374 (418) | 6,934 (74) | |
| D | 2,314 (102) | 539 (40) | 380 (64) | 1,280 (59) | 2,289 (36) | ||
| E | 2,180 (115) | 1,294 (216) | 346 (100) | 717 (53) | 1,357 (164) | 1,075 (181) | 1,819 (102) |
| F | 7,920 (4,288) | 9,858 (5,064) | 1,516 (3,696) | 3,826 (2,752) | |||
All individuals had CDC stage II HIV infection.
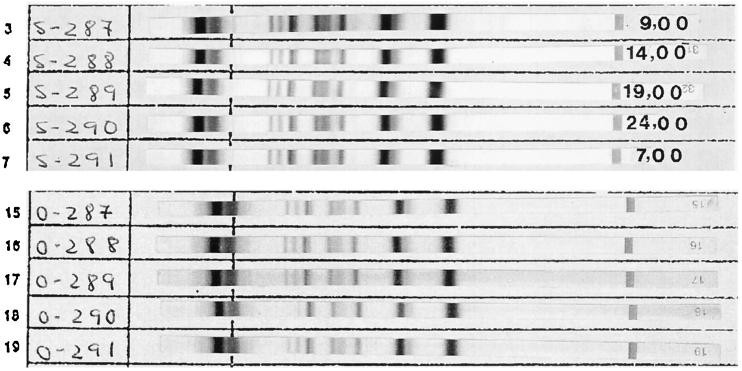
The confirmation of the results by WB with GCT samples demonstrated that serial WBs displayed approximately the same intense bands. However, for urine samples, not only were the bands’ intensities less, but in some cases, some bands could be seen to be missing, even though they were present in the WBs performed with the respective GCT samples (Fig. 2).
FIG. 2.
Reactivities observed by WB of GCT and urine samples from the same individual obtained over 24 h.
DISCUSSION
When gathering GCT samples for testing, the device that is used and the mouth site chosen for sample collection seem to be crucial to the results of the trial (29). However, the time of sample collection does not appear to be decisive if the results obtained in the follow-up performed with the six individuals infected with HIV (CDC stage II infection) over 24 h are taken into account. Several devices specifically designed for the collection of GCT samples exist (31, 32). For this project we selected a device which we feel affords a greater content of GCT in the final sample volume that is collected because the device remains in the lateral gingival fold long enough and has a large absorbent surface. Another advantage of this device is that it does not seem to alter the original concentration of IgG-type immunoglobulins present in the GCT sample. This is not true of the devices used in other studies (20, 43), which incorporate solutions that dilute the sample and that thus may cause a decrease in antibody levels and therefore the sensitivity of the detection technique. Nevertheless, use of such devices may be best when no freezing facility that can preserve the sample once it has been taken is available.
Screening for HIV antibodies in biological samples from populations for whom the final objective is not diagnosis involves the use of techniques in which the most important criterion for selection must be sensitivity (3, 9, 14, 18, 21, 35). The sensitivity shown in the ELFA study with GCT samples for the detection of HIV antibodies could make it acceptable for epidemiological studies.
Another important aspect is the possibility of using WB to confirm the reactivity of the alternative samples that are positive by the preliminary screening.
Most positive samples displayed reactivities to more than six bands. This feature seems to be favored by an increased sample volume and overnight incubation, which cause an increase in band intensity, which in turn facilitates band observation and therefore enhances test sensitivity. Sometimes a short incubation period combined with very stringent criteria for positivity by WB can reduce the sensitivity of WB with alternative biological fluids (19).
As far as the intensities of the bands observed in the WBs with GCT samples is concerned, our results coincide with those of other researchers (31, 33, 39), who have observed that reactivity to HIV envelope antigens is usually strong, while reactivity to GAG antigens is weak.
The reactivity pattern most frequently observed by WB included bands to ENV, POL, and GAG, which makes for easier interpretation of the results of confirmation tests. The presence of a predominant reactivity to the envelope proteins (gp120 and gp160) in all of the WBs performed with GCT samples coincides with the results obtained by other groups (2, 19, 22, 29). This fact seems to indicate that the WHO criteria for serum samples could be used with GCT samples with no decrease in the operational characteristics in terms of the sensitivity and specificity of WB (28). In some studies, use of other criteria causes a drop in the sensitivity of WB with an increase in the number of samples with indeterminate results by WB (19, 22).
Our findings seem to indicate that HIV antibodies can be detected in GCT as well as in serum. Some studies have compared serum and GCT in a longitudinal manner during the period of immunoconversion and hypothesize that immunoconversion can likely be detected GCT and serum at about the same time (3, 12, 18).
The use of urine as an alternative to serum offers worse results than the use of GCT; the antibody concentration present in urine samples is much lower than that present in serum; some investigators state that it is even 104 times less (13). On the other hand, other factors may influence the antibody concentration found in urine samples and may cause a sample to be nonreactive by the screening and confirmation techniques used in the study, even though the sample belonged to an HIV-infected individual. Among such factors which would explain the presence of false-negative results are certain medications (i.e., diuretics), consumption of large quantities of liquids, urine collection without a long enough waiting period after the last urination to allow the antibody concentration to return to normal, and deterioration in the individual’s immunological state (30). Other factors to be borne in mind when analyzing results for the three urine samples that had false-negative results by the screening test but that were reactive by WB are sample preservation time and lower ELFA sensitivity with respect to the results of WB. Therefore, for studies that rely on the analysis of urine samples, it seems recommendable that samples be analyzed as quickly as possible, even when they are preserved at 4°C. Another aspect which should be considered is sample freezing, because it seems that the processes of freezing and defrosting can cause a drop in the specificity of the technique (26). In our study none of the urine samples were frozen.
The intensities of the bands observed by the WB of urine samples were generally weaker than the intensities observed by WB of GCT samples. As with GCT samples, a predominant reactivity to envelope proteins (gp41, gp120, and gp160) was observed among the samples with reactive bands by WB. This particular reactivity and the possibility of detecting antibodies against all the structural antigens of the virus have already been described by Cao et al. (10).
As has been shown here, the results obtained with urine samples permit the use of this easily obtained and easily preserved sample in epidemiological studies that deal with large populations similar to those handled in this study. In contrast, use of urine samples for diagnosis does not seem to be advisable when one takes into consideration the sensitivities that were found.
The concentration in serum of an antibody against a specific infectious disease agent can undergo oscillations over time. Such variations tend to be slow and are rarely established in a matter of days except in patients in the acute stage of the infection. When samples other than serum are used for diagnosis of a chronic infection such as HIV infection, one problem that may arise is the presence of different HIV antibody concentrations in the fluids used as alternatives to serum (16, 23, 31). The concentration may be influenced by the antibody levels that previously existed in the serum, by the quantity of serum filtrate that passes to the fluids, or by its final dilution, depending on the secretion volume of the alternative fluid. With this in mind it seems reasonable to venture that the antibody concentration in urine may suffer more circadian alterations than that in GCT. According to Mortimer and Parry (31), the immunoglobulin concentration in GCT is between four and five times lower than that in plasma. Slight fluctuations in RFVs for both GCT and urine throughout the day were observed in our study. At any rate, it should be indicated that just as when GCT and urine reactivities were observed, very significant quantitative reactivity differences were found between GCT and urine samples from the same individuals. The fact that the values for GCT samples were always higher than those for urine samples confirms what various investigators have indicated, that more immunoglobulins are present in GCT than in urine (31). Nonetheless, we could observe how the titer of HIV antibodies found in urine paralleled the titer of HIV antibodies in the same individual’s GCT. It is therefore possible for the corresponding serum sample to be included in this correlation. Some studies that have observed the existence of a correlation between the antibody levels found in urine and the levels found in respective serum samples confirm this possibility (10).
In conclusion, both types of samples seem to be useful for epidemiological studies, while the use of WB with an appropriate sample volume and incubation time, plus positivity criteria that prefer observed reactivities to envelope proteins, could allow GCT to be used for the diagnosis of HIV infection.
ACKNOWLEDGMENTS
We gratefully acknowledge J. M. Pérez, E. Medrano, M. Flores, M. Morillo, and E. Perlado for the collection of samples and C. Martín and H. Torres for bibliographic support.
REFERENCES
- 1.Adams L E, Donovan B R, Friedman K A, El Ramahi K, Hess E V. Sperm and seminal plasma antibodies in acquired immune deficiency (AIDS) and other associated syndromes. Clin Immunol Immunopathol. 1988;46:442–449. doi: 10.1016/0090-1229(88)90063-3. [DOI] [PubMed] [Google Scholar]
- 2.Akker R, Hoek J A, Akker W M, Kooy H, Vijge E, Roosendaal G, Coutinho R A, Loon A M. Detection of HIV antibodies in saliva as a tool for epidemiological studies. AIDS. 1992;6:953–957. doi: 10.1097/00002030-199209000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Behets F M, Edidi B, Quinn T C, Atikala L, Bishagara K, Nzila N, Laga M, Piot P, Ryder R W, Brown C C. Detection of salivary HIV-1 specific IgG antibodies in high-risk populations in Zaire. J Acquired Immune Defic Syndr. 1991;4:183–187. [PubMed] [Google Scholar]
- 4.Belec L, Georges A J, Steenman G, Martin P M. Antibodies to human immunodeficiency virus in vaginal secretions of heterosexual women. J Infect Dis. 1989;160:385–391. doi: 10.1093/infdis/160.3.385. [DOI] [PubMed] [Google Scholar]
- 5.Belec L, Georges A J, Steenman G, Martin P M. Antibodies to human immunodeficiency virus in the semen of heterosexual men. J Infect Dis. 1989;159:324–327. doi: 10.1093/infdis/159.2.324. [DOI] [PubMed] [Google Scholar]
- 6.Belec L, Tevi-Benissan C, Lu X S, Prazuck T, Pillot J. Local synthesis of IgG antibodies to HIV within the female and male genital tracts during asymptomatic and pre-AIDS stages of HIV infection. AIDS Res Hum Retroviruses. 1995;11:719–729. doi: 10.1089/aid.1995.11.719. [DOI] [PubMed] [Google Scholar]
- 7.Belec L, Gresenguet G, Dragon M A, Meillet D, Pillot J. Detection of antibodies to human immunodeficiency virus in vaginal secretions by immunoglobulin G antibody capture enzyme-linked immunosorbent assay: application to detection of seminal antibodies after sexual intercourse. J Clin Microbiol. 1994;32:1249–1255. doi: 10.1128/jcm.32.5.1249-1255.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Belec L, Peghini M, Georges A J, Barabe P, Martin P M. Antibodies to HIV-2 in genital secretions. Res Virol. 1989;140:15–21. doi: 10.1016/s0923-2516(89)80079-2. [DOI] [PubMed] [Google Scholar]
- 9.Bird A, Gore S, Jollife D, Burns S. Anonymous HIV surveillance in Saughton Prison, Edinburgh. AIDS. 1992;6:725–733. doi: 10.1097/00002030-199207000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Cao Y Z, Hosein B, Borkowsky W, Mirabile M, Baker L, Baldwin D, Poiesz B J, Friedman-Kien A E. Antibodies to human immunodeficiency virus type 1 in the urine specimens of HIV-1-seropositive individuals. AIDS Res Hum Retroviruses. 1989;5:311–319. doi: 10.1089/aid.1989.5.311. [DOI] [PubMed] [Google Scholar]
- 11.Chamnanput J, Phanuphak P. Comparison of eight commercial test kits for detecting anti-HIV antibodies in saliva specimens. AIDS. 1993;7:1026. doi: 10.1097/00002030-199307000-00026. . (Letter.) [DOI] [PubMed] [Google Scholar]
- 12.Connell J A, Parry J V. Detection of anti-HIV in saliva and urine at the time of seroconversion. Clin Diagnost Virol. 1994;1:299–311. doi: 10.1016/0928-0197(94)90060-4. [DOI] [PubMed] [Google Scholar]
- 13.Connell J A, Parry J V, Mortimer P P, Duncan R J, McLean K A, Johnson A M, Hambling M H, Barbara J, Farrington C P. Preliminary report: accurate assays for anti-HIV in urine. Lancet. 1990;335:1366–1369. doi: 10.1016/0140-6736(90)91245-6. [DOI] [PubMed] [Google Scholar]
- 14.Connell J A, Parry J V, Mortimer P P, Duncan R J. Novel assay for the detection of immunoglobulin G antihuman immunodeficiency virus in untreated saliva and urine. J Med Virol. 1993;41:159–164. doi: 10.1002/jmv.1890410212. [DOI] [PubMed] [Google Scholar]
- 15.Constantine N, Zhang X, Li L, Bansal J, Hyams K, Smialek J. Application of a rapid assay for detection of antibodies to human immunodeficiency virus in urine. Am J Clin Pathol. 1994;101:157–161. doi: 10.1093/ajcp/101.2.157. [DOI] [PubMed] [Google Scholar]
- 16.Desai S, Bates H, Michalski F J. Detection of antibody to HIV-1 in urine. Lancet. 1991;337:183–184. doi: 10.1016/0140-6736(91)90855-j. . (Letter.) [DOI] [PubMed] [Google Scholar]
- 17.Frerichs R, Htoon M, Eskes N, Soe L. Comparison of saliva and serum for HIV surveillance in developing countries. Lancet. 1992;340:1496–1499. doi: 10.1016/0140-6736(92)92755-5. [DOI] [PubMed] [Google Scholar]
- 18.Frerichs R R, Silarug N, Eskes N, Pagcharoenpol P, Rodklai A, Thangsupachai S, Wongba C. Saliva-based HIV-antibody testing in Thailand. AIDS. 1994;8:885–894. doi: 10.1097/00002030-199407000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Gallo D, George J R, Fitchen J H, Goldstein A S, Hindahl M S. Evaluation of a system using oral mucosal transudate for HIV-1 antibody screening and confirmatory testing. JAMA. 1997;227:254–258. [PubMed] [Google Scholar]
- 20.Gómez C, Gutiérrez M, Martínez-Acacio P, Soriano V. Evaluation of a new saliva collection device for HIV antibody screening purposes. Vox Sang. 1994;66:244. doi: 10.1111/j.1423-0410.1994.tb00319.x. . (Letter.) [DOI] [PubMed] [Google Scholar]
- 21.Hart G J, Dawson J, Fitzpatrick R M, Boulton M, McLean J, Brookes M, Parry J. Risk behaviour, anti-HIV and anti-hepatitis B core prevalence in clinic and non-clinic samples of gay men in England, 1991–1992. AIDS. 1993;7:863–869. doi: 10.1097/00002030-199306000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Holmström P, Syrjänem S, Laine P, Valle S L, Suni J. HIV antibodies in whole saliva detected by ELISA and Western blot assays. J Med Virol. 1990;30:245–248. doi: 10.1002/jmv.1890300403. [DOI] [PubMed] [Google Scholar]
- 23.Ishikawa S, Hashida S, Haskinaka K, Hirota K, Saitoh A, Takamizawa A, Shinagawa H, Oka S, Shimada K, Ishikawa E. Diagnosis of HIV-1 infection with whole saliva by detection of antibody IgG to HIV-1 with ultrasensitive enzyme immunoassay using recombinant reverse transcriptase as antigen. J Acquired Immune Defic Syndr Hum Retrovirol. 1995;10:41–47. [PubMed] [Google Scholar]
- 24.Jayashree S, Bhan M K, Kumar R, Raj P, Glass R, Bhandari N. Serum and salivary antibodies as indicators of rotavirus infection in neonates. J Infect Dis. 1989;158:1117–1120. doi: 10.1093/infdis/158.5.1117. [DOI] [PubMed] [Google Scholar]
- 25.Johnson A M, Parry J V, Best S J, Smith A M, De Silva M, Mortimer P P. HIV surveillance by testing saliva. AIDS. 1988;2:369–371. doi: 10.1097/00002030-198810000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Kostolansky F, Li J, Friedman-Kien A. Detection of false antibodies to HIV-1 in urine. AIDS. 1993;7:531–532. [PubMed] [Google Scholar]
- 27.Lucht E, Albert J, Linde A, Xu W, Brytting M, Lundeberg J, Uhlen M, Bratt G, Sandstrom E, Heimdahl A. Human immunodeficiency virus type 1 and cytomegalovirus in saliva. J Med Virol. 1993;39:156–162. doi: 10.1002/jmv.1890390213. [DOI] [PubMed] [Google Scholar]
- 28.Martínez P, Ortiz de Lejarazu R, Eiros J M, Rodríguez-Torres A. Usefulness of oral mucosal transudate for HIV antibody testing. JAMA. 1997;277:1592. . (Letter.) [PubMed] [Google Scholar]
- 29.Martínez P, Ortiz de Lejarazu R, Eiros J M, Perlado E, Flores M, del Pozo M A, Rodríguez-Torres A. Comparison of two assays for detection of HIV antibodies in saliva. Eur J Clin Microbiol Infect Dis. 1995;14:330–336. doi: 10.1007/BF02116526. [DOI] [PubMed] [Google Scholar]
- 30.Martínez P, Ortiz de Lejarazu R, Eiros J M, De Benito J, Rodríguez-Torres A. Urine samples as a possible alternative to serum for human immunodeficiency virus antibody screening. Eur J Clin Microbiol Infect Dis. 1996;15:810–813. doi: 10.1007/BF01701524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mortimer P P, Parry J V. Non-invasive virological diagnosis: are saliva and urine specimens adequate substitutes for blood? J Med Virol. 1991;1:73–78. [Google Scholar]
- 32.Mortimer P P, Parry J V. Detection of antibody to HIV in saliva: a brief review. Clin Diagn Virol. 1994;2:231–243. doi: 10.1016/0928-0197(94)90048-5. [DOI] [PubMed] [Google Scholar]
- 33.O’Shea S, Cordery M, Barrett W Y, Richman D D, Bradbeer C, Banatvala J E. HIV excretion patterns and specific antibody response in body fluids. J Med Virol. 1993;31:291–296. doi: 10.1002/jmv.1890310409. [DOI] [PubMed] [Google Scholar]
- 34.Parry J V, Perry K R, Panday S, Mortimer P P. Diagnosis of hepatitis A and B by testing saliva. J Med Virol. 1989;28:255–260. doi: 10.1002/jmv.1890280410. [DOI] [PubMed] [Google Scholar]
- 35.Raab G M, Burns S M, Scott G, Cudmore S, Ross A, Gore S M, O’Brien F, Shaw T. HIV prevalence and risk factors in university students. AIDS. 1995;9:191–197. [PubMed] [Google Scholar]
- 36.Reagan K J, Lile C C, Book G W, Devash Y, Winslow D L, Bincsik A. Use of urine for HIV-1 antibody screening. Lancet. 1990;335:358–359. doi: 10.1016/0140-6736(90)90649-p. . (Letter.) [DOI] [PubMed] [Google Scholar]
- 37.Renom G, Bouquety J C, Lanckriet C, Georges A J, Siopathis M R, Martin P M. Detection of anti-HIV IgA in tears of children born to seropositive mother is highly specific. Res Virol. 1990;141:557–562. doi: 10.1016/0923-2516(90)90086-x. [DOI] [PubMed] [Google Scholar]
- 38.Schopper D, Vercauteren G. Testing for HIV at home: what are the issues? AIDS. 1996;10:1455–1465. doi: 10.1097/00002030-199611000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Soto-Ramirez L E, Hernandez-Gomez L, Sifuentes-Osornio J, Barriga-Angulo G, Duarte-De Lima D, Lopez-Portillo M, Ruiz-Palacios G M. Detection of specific antibodies in gingival crevicular transudate by enzyme-linked immunosorbent assay for diagnosis of human immunodeficiency virus type 1 infection. J Clin Microbiol. 1992;30:2780–2783. doi: 10.1128/jcm.30.11.2780-2783.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Thieme T, Yoshihara P, Piacentini S, Beller M. Clinical evaluation of oral fluid samples for diagnosis of viral hepatitis. J Clin Microbiol. 1992;30:1076–1079. doi: 10.1128/jcm.30.5.1076-1079.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thongcharoen P, Wasi C, Louisirirotchanakul S, Parry J, Connell J, Mortimer P. Immunoglobulin G antibody capture enzyme-linked immunosorbent assay: a versatile assay for detection of anti-human immunodeficiency virus type 1 and 2 antibodies in body fluids. J Clin Microbiol. 1992;30:3288–3289. doi: 10.1128/jcm.30.12.3288-3289.1992. . (Letter.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.U.S. Department of Health and Human Services. HHS news. U.S. Washington, D.C: Department of Health and Human Services; 1996. FDA approves first HIV home test system; pp. 96–100. [Google Scholar]
- 43.Vall Mayans M, Casabona J, Rabella N, De Miniac D. Testing of saliva and serum for HIV in high-risk populations. Eur J Clin Microbiol Infect Dis. 1995;14:710–713. doi: 10.1007/BF01690881. [DOI] [PubMed] [Google Scholar]
- 44.Ward R, Pax K A, Sherwood J R, Young E C, Schiff G M, Bernstein D I. Salivary antibody titers in adults challenged with a human rotavirus. J Med Virol. 1992;36:222–225. doi: 10.1002/jmv.1890360313. [DOI] [PubMed] [Google Scholar]
- 45.Wolff H, Mayer K, Seage G, Politch J, Horsburgh C R, Anderson D. A comparison of HIV-1 antibody classes, titers, and specificities in paire semen and blood samples from HIV-1 seropositive men. J Acquired Immune Defic Syndr. 1992;5:65–69. [PubMed] [Google Scholar]
- 46.World Health Organization. AIDS. Proposed WHO criteria for interpreting results from Western blot assays for HIV-1, HIV-2 and HTLV-I/HTLV-II. Weekly Epidemiol Rec. 1990;65:281–283. [PubMed] [Google Scholar]