Background:
There are different approaches for reconstruction of little finger and dorsal hand defects. The ulnar parametacarpal flap, first introduced by Backhach et al in 1995, is considered a good option for reconstructing such defects. In this study, we elevated this flap on one perforator and applied it as a propeller flap. We then discussed the reliability of this flap and which perforator (the proximal or the distal one) is more reliable.
Methods:
This study was carried out on 20 patients with different little finger and dorsal hand defects between June 2017 and March 2019. All defects were covered by perforator-based ulnar parametacarpal flaps. Ten flaps were based on the proximal perforator, whereas the other 10 were based on the distal perforator.
Results:
With a period of follow-up ranging from 6 months to 1 year, all flaps that were raised on the proximal perforator survived completely, whereas two of 10 flaps raised on the distal perforator showed venous congestion and also one flap showed partial necrosis of the distal one-third due to ischemia.
Conclusions:
The perforator based ulnar parametacarpal flap is a reliable option for reconstruction of little finger and dorsal hand defects. It is more reliable when it is raised on the proximal perforator rather than on the distal one.
Takeaways
Question: Coverage of little finger and dorsal hand defects with UPM flap.
Findings: All flaps that were raised on the proximal perforator survived completely, whereas two of 10 flaps raised on the distal perforator showed venous congestion. Also, one of 10 flaps that was raised on distal perforator showed partial necrosis of the distal one-third due to ischemia.
Meaning: The perforator-based ulnar parametacarpal flap is a reliable option for reconstruction of little finger and dorsal hand defects.
INTRODUCTION
Hand trauma with defects ranging from small and superficial to extensive soft tissue injuries with exposure of vital structures is very common worldwide.1 This kind of trauma represents 10% of patients who came to the emergency departments.2 Early reconstruction of such defects is required for optimal function and rehabilitation, and it remains a challenge for the plastic and reconstructive surgeon.3 As the little finger is a border digit, it is commonly involved in hand trauma. Different causes contribute to defects on the little fingers, including industrial injuries, burns, and results of tumor excision. Coverage by stable and durable tissue with preservation of its function is required. There are different modalities for reconstruction of defects in its palmar and dorsal aspects. Local and regional flaps as cross finger flaps are also considered good options, but they have donor site morbidity.4 The reverse radial forearm flap is also an option, but it compromises a main vascular axis.5 The posterior interosseous artery flap is rather difficult, and its main complication is venous congestion.6 The advances in microsurgery allow transfer of small free flaps for this purpose7; however, this is not available in all centers.
The ulnar parametacarpal flap described by Bakhach et al was raised from the dorsoulnar aspect of the hand.8 It is supplied by a constant connection between distal division of dorsal branch of the ulnar artery and ulnar palmar digital artery of the fifth finger. It can cover defects of the little finger up to the distal interphalangeal joints; also, it can cover defects around the fourth and fifth metacarpophalangeal joints, and the fourth web space as well. Bakhach et al transferred this flap without identification of communicating branch with the palmar system. According to personal communication with Joseph Bakhach, they did not visualize the artery nor the communications with the palmar artery during dissection of the flap.9
In this study, we identified the proximal and distal perforators for this flap with their exposure during dissection; then we rotated the flap 180 degrees as a propeller flap on one of these perforators and traced the reliability of this flap and which perforator is more reliable to supply this flap.
ANATOMICAL BACKGROUND
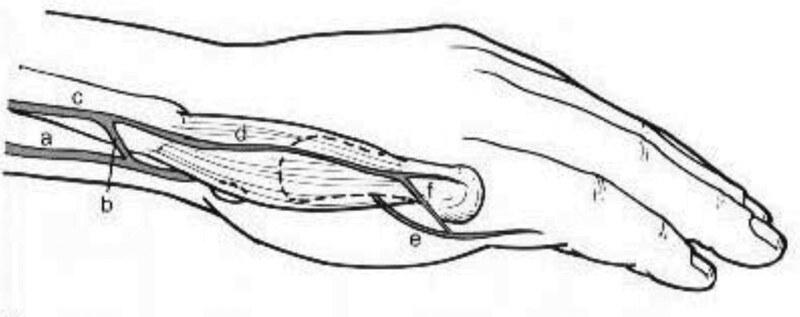
The ulnar parametacarpal flap is a fasciocutaneous flap raised from the dorsoulnar aspect of the hand. The ulnar artery, as shown in Figure 1, gives a dorsal perforating branch 3 cm above the pisiform. This perforating branch passes dorsally and divides into an ascending branch (which nourishes Backer’s flap) and descending branch (which supplies the ulnar parametacarpal flap). The descending branch is considered the fifth dorsal metacarpal artery and runs under the fascia of the hypothenar muscles. It fades at the proximal phalanx of the little digit. Proximal and distal to the fifth metacarpophalangeal joint, it communicates with the ulnar digital artery of the fifth finger. The ulnar parametacarpal flaps depend on either communication for the reversal of blood flow.10, 11
Fig. 1.
a: ulnar artery, b: dorsal perforating branch, c: ascending branch, d: descending branch (fifth dorsal metacarpal artery), e: ulnar digital artery of the fifth finger, f: communicating branch at the neck of the fifth metacarpal bone.
PATIENT AND METHODS
This study was done between June 2017 and March 2019 at Ain Shams University Hospitals. We enrolled into this study 20 patients (13 men and seven women) with different defects on little fingers and dorsum of hands. Their ages ranged from 23 to 50 years. All defects were covered by perforator-based ulnar parametacarpal flaps. Ten flaps were based on the proximal perforator. The most distal extent of the defects to be reconstructed was the proximal interphalangeal joints and the proximal one third of the middle phalanges. However, the other 10 flaps were based on the distal perforator, with the most distal location of the defects to be reconstructed near the distal interphalangeal joint of the little fingers. All operations were done by the same surgical team with a period of follow-up ranging from 6 months to 1 year.
OPERATIVE TECHNIQUE
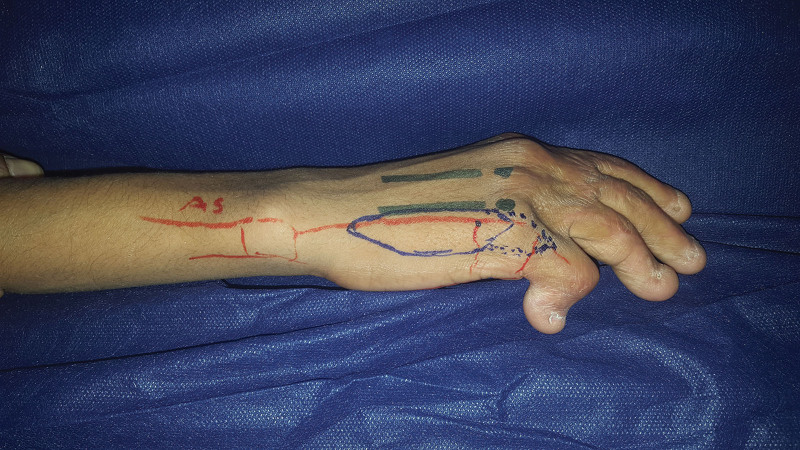
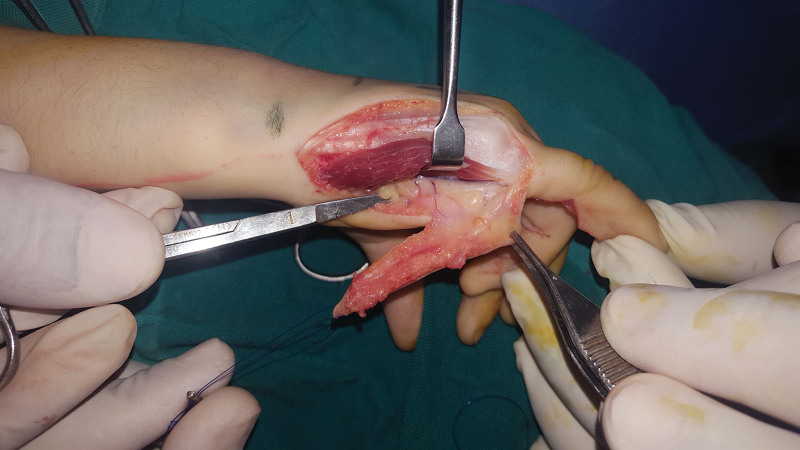
According to the defect site and size, marking of the flap, as shown in Figure 2, was done with the help of a handheld Doppler for identification of the proximal and dorsal perforators that were proximal and distal to the interphalangeal joint correspondingly. Then, after debridement of all necrotic tissues until a healthy bed was reached, arm tourniquet was elevated to 250 mm Hg for 90 minutes without complete exsanguination of the hand, incision, and dissection in a subfacial plane (fascia of abductor digitiminimi) started from proximal to distal with the aid of loupe magnification and bipolar cautery for the dorsal veins and the descending branch. Careful dissection was done when approximating the neck of the fifth metacarpal where the perforators are found one proximal to it and the other distal to it as shown in Figure 3. Then‚ judicious dissection of the communicating perforator was done without excessive skeletonization‚ leaving a cuff of soft tissues around it without including sensory nerve branch. Then, according to location of the defect and reach of the flap, we ligated and cauterized one of the perforators, with the aim to preserve the distal one if more distal defect to be covered. After that‚ the flaps were rotated to cover the defect as a propeller flap. Finally, the donor site was closed primarily with no need for skin graft, except in one case that needed a full thickness skin graft taken from the medial arm to cover the proximal part of the donor site of the flap.
Fig. 2.
Marking of the flap along the dorsoulnar aspect of the hand.
Fig. 3.
Dissection of the flap from proximal to distal with identification of the communicating perforators with the palmar arterial system.
RESULTS
With a period of follow-up ranging from 6 months to 1 year, all flaps (10 flaps) that were raised on the proximal perforator survived completely, whereas two of 10 flaps (20%) raised on the distal perforator showed venous congestion that was managed by release of sutures and frequent dressings with healing by secondary intention. Also, one of 10 flaps (10 %) that was raised on the distal perforator showed partial necrosis of the distal one-third due to ischemia and was managed by debridement with frequent dressings and local flap coverage. Donor site scar was accepted by all patients. Regarding the functional outcomes as the range of motion of the MCP, PIP, and DIP joints of the fingers, the flap itself did not affect the range of motion of the fingers with no contractures. However, some patients (especially posttraumatic patients) had some degree of limited range of motion and joint contracture due to associated fractures and joint injuries; these were managed by physiotherapy within a period of 2 months (Table 1).
Table 1.
Patient Demographics, Perforator Used, and the Surgical Outcome
| No. | Age | Gender | BMI | Smoking History | Etiology | Defect Size (Flap Size) | Perforator Used | Venous Congestion | Partial or Total Flap Necrosis |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 27 y | Woman | 25 | No | Trauma | 1.5 × 2 cm | Proximal | No | No |
| 2 | 28 y | Man | 27 | Yes | Trauma | 1.8 × 1.9 cm | Distal | No | No |
| 3 | 44 y | Man | 20 | Yes | Trauma | 2 × 2 cm | Proximal | No | No |
| 4 | 30 y | Woman | 19 | No | Contracture release | 2 × 2.3 cm | Proximal | No | No |
| 5 | 33 y | Man | 22 | No | Trauma | 1.8 × 2.4 cm | Proximal | No | No |
| 6 | 23 y | Man | 30 | No | Trauma | 1.9 × 2 cm | Distal | No | No |
| 7 | 32 y | Woman | 32 | No | Trauma | 2.3 × 2.5 cm | Distal | Yes | No |
| 8 | 30 y | Man | 27 | Yes | Trauma | 2 × 2.2 cm | Proximal | No | No |
| 9 | 35 y | Man | 19 | Yes | Contracture release | 1.9 × 1.8 cm | Distal | No | No |
| 10 | 29 y | Man | 20 | No | Trauma | 1.7 × 2.2 cm | Distal | No | No |
| 11 | 29 y | Woman | 22 | No | Trauma | 1.7 × 1.9 cm | Distal | No | No |
| 12 | 40 y | Man | 24 | Yes | Trauma | 2 × 2.3 cm | Proximal | No | No |
| 13 | 25 y | Woman | 21 | No | Tumor excision | 2 × 2.2 cm | Distal | No | Partial |
| 14 | 33 y | Man | 28 | No | Trauma | 1.5 × 1.9 cm | Proximal | No | No |
| 15 | 32 y | Man | 26 | No | Trauma | 1.3 × 2.4 cm | Distal | No | No |
| 16 | 28 y | Woman | 24 | No | Trauma | 2 × 1.8 cm | Proximal | No | No |
| 17 | 25 y | Man | 27 | No | Contracture release | 1.7 × 2 cm | Distal | No | No |
| 18 | 50 y | Man | 28 | Yes | Trauma | 1.8 × 1.7 cm | Proximal | No | No |
| 19 | 36 y | Woman | 30 | No | Trauma | 2 × 2.3 cm | Proximal | No | No |
| 20 | 48 y | Man | 29 | No | Tumor excision | 2.4 × 2.3 cm | Distal | Yes | No |
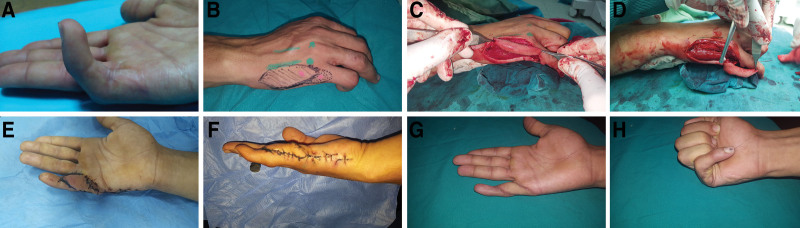
Clinical Case
A 22-year-old male patient presented with a posttraumatic contracted right little finger. An ulnar parametacarpal flap was elevated to resurface the defect based on the proximal communication with the palmar arterial system. Stable coverage was achieved with accepted door site scar after 4 months, as shown in Figure 4.
Fig. 4.
Reconstruction of post-traumatic contracted right little finger with ulnar parametacarpal flap, with pre-, intra- and postoperative photographs. A, Post-traumatic contracted right little finger. B, Design and marking of the ulnar parametacarpal flap. C, Flap elevated from proximal to distal. D, Judicious dissection of the perforator and 180-degree rotation. E, Flap after few days with intact vascularity. F: Donor site closed primarily. G, Stable coverage for the defect after 4 months. H, Good function of the PIP joint, although the patient still has rehabilitation sessions.
DISCUSSION
Reconstruction of soft tissue defects of the hand and little digit represents a challenge to plastic surgeons,12 especially for the reconstructive demands of texture, thickness, pliability, color matching, sensation, and durability. The main goal for reconstruction of such defects is to provide stable, reliable, and durable coverage with minimal donor site morbidity, early rehabilitation, and good functional results.13 In 1995, Joseph Backhach et al described the anatomical basis of an ulnar parametacarpal flap based on cadaveric dissection.14 This study was followed by a clinical series of 10 clinical cases. They used this flap for resurfacing, mainly the dorsal aspect of the little finger, and they stopped dissection at the neck of the fifth metacarpal bone and rotated the flap without visualization of the descending division of the dorsal ulnar perforating branch and the communicating branches with the palmar arterial system as well. A similar flap was described by Omokawa et al15; they named it the reverse ulnar hypothenar flap. It appears at the beginning as an ulnar parametacarpal flap with the same vascular basis. This flap is different because it is a completely reversed flow flap, where they compromise the ulnar digital artery of the little finger, and so it augments its blood supply.16 Usami et al17 reported the application of perforator-based free or reverse pedicled ulnar parametacarpal artery flaps on a series of 25 patients with 17 free transfers to the thumb, index, middle and ring fingers, and eight reverse pedicled transfers to the little fingers. They used these flaps based on the palmar digital system.
In this study, we used the ulnar parametacarpal flap based on perforators of the descending branch of the dorsal ulnar artery to cover various defects on the little finger and dorsum of the hand. Based on one perforator, these flaps were rotated as propeller flaps. Proximal perforator-based flaps were used to reconstruct the defects safely up to the proximal interphalangeal joints and the proximal one-third of the middle phalanges of the little fingers, whereas the distal perforator-based flaps can safely reconstruct defects up to the distal interphalangeal joints of the little fingers. These flaps can reconstruct defects up to 2.5 × 2.5 cm on the little finger and dorsoulnar region of the hand.
CONCLUSIONS
The perforator-based ulnar parametacarpal flap is a reliable option for reconstruction of little finger and dorsal hand defects. It is more reliable when it is raised on the proximal perforator rather than on the distal one. It is easy to perform and provides stable and durable coverage for little finger and dorsal hand defects‚ and it should be considered while reconstructing such defects.
Footnotes
Published online 22 February 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Unal C, Ozdemir J, Hasdemir M. Clinical application of distal ulnar artery perforator flap in hand trauma. J Reconstr Microsurg. 2011;27:559–565. [DOI] [PubMed] [Google Scholar]
- 2.Khan AZ, Khan IZ, Khan A, et al. Audit of occupational hand trauma presenting in the accident and emergency departments of two major hospitals. Ann King Edward Med Coll. 1998;4:14–16. [Google Scholar]
- 3.Becker C, Gilbert A. [The cubital flap]. Ann Chir Main. 1988;7:136–142. [DOI] [PubMed] [Google Scholar]
- 4.Paterson P, Titley OG, Nancarrow JD. Donor finger morbidity in cross-finger flaps. Injury. 2000;31:215–218. [DOI] [PubMed] [Google Scholar]
- 5.Ali H, Zulfiqar B. Reverse radial forearm flap; management of soft tissue defects of dorsum of hand and wrist using reverse radial forearm flap. Professional Med J. 2018;25:1791–1795. [Google Scholar]
- 6.Shahzad MN, Ahmed N, Qureshi KH. Reverse flow posterior interosseous flap: experience with 53 flaps at Nishtar Hospital, Multan. J Pak Med Assoc. 2012;62:950–954. [PubMed] [Google Scholar]
- 7.May JW, Jr, Chait LA, Cohen BE, et al. Free neurovascular flap from the first web of the foot in hand reconstruction. J Hand Surg Am. 1977;2:387–393. [DOI] [PubMed] [Google Scholar]
- 8.Bakhach J, Martin D, Baudet J. The para metacarpal ulnar flap, experience on ten clinical cases. Ann Plast Aesthet Surg. 1996;41:269–275. [PubMed] [Google Scholar]
- 9.Bakhach J. Personal Communication. 2016.
- 10.Becker C, Gilbert A. The ulnar flap. Handchir Mikrochir PlastChir . 1988. 20:180–183. [Google Scholar]
- 11.Strauch B, de Moura, W. Arterial system of the fingers. J. Hand Surg Am. 1990;15:148. [DOI] [PubMed] [Google Scholar]
- 12.Ahmad M. Management of hand trauma. J Surg Pak. 2008;13:128–131. [Google Scholar]
- 13.Shahzad MN, Ahmed N, Qureshi KH. Reverse flow posterior interosseous flap: experience with 53 flaps at Nishtar Hospital, Multan. J Pak Med Assoc. 2012;62:950–954. [PubMed] [Google Scholar]
- 14.Bakhach J, Saint Cast Y, Gazarian A, et al. The para metacarpal ulnar flap, anatomical study and clinical application. Ann Plast Aesthet Surg. 1995;40:136–147. [PubMed] [Google Scholar]
- 15.Omokawa S, Yajima H, Inada Y, et al. A reverse ulnar hypothenar flap for finger reconstruction. Plast Reconstr Surg. 2000;106:828–833. [DOI] [PubMed] [Google Scholar]
- 16.Omokawa S, Tanaka Y, Ryu J, et al. The anatomical basis for reverse first to fifth dorsal metacarpal arterial flaps. J Hand Surg Br. 2005;30:40–44. [DOI] [PubMed] [Google Scholar]
- 17.Satoshi U, Kohei I, Yuichi H, et al. An ulnar parametacarpal perforator flap for volar digital soft tissue reconstruction. J Hand Surg Br. 2020;45:1–7. [DOI] [PubMed] [Google Scholar]