Abstract
Although health-related policies are abundant, efforts to understand how to ensure that these policies serve as an effective vehicle for translating scientific evidence are relatively sparse. This paper explores how policy-focused implementation science (IS) may contribute to understanding the translation of scientific evidence to health-related policy in governmental and nongovernmental sectors. Expanding the focus of implementation science in cancer control could systematically address policy to both increase the use of scientific evidence in general and to address health equity. In this Commentary, we look to relevant work outside of IS that could be informative, most notably from the field of political science. We propose several ideas for future research that could help move the field of policy implementation science in cancer control in the USA forward. Although most efforts to increase uptake of the scientific evidence base reference translation to “practice and policy,” there has been relatively little emphasis in the USA on implementation at the policy level, especially related to cancer control. If we are to achieve the full benefits of scientific discovery on population and public health, we will need to consider policy as a critical mechanism by which evidence can be translated to practice. We have a robust set of methods within implementation science that are increasing the pace of adoption and maintenance of evidence-based programs in a variety of settings. Building on these efforts, the time is right to expand our focus to include policy implementation.
Keywords: Policy, Cancer control, Implementation science, Evidence translation
Lay Summary
Although health-related policies are abundant, relatively few efforts have been undertaken to ensure that they are used as a way to translate scientific evidence to promote health. This paper explores how policy-focused implementation science (IS) may contribute to understanding the translation of scientific evidence to health-related policy in governmental and nongovernmental sectors. We propose several ideas for future research that could help move the field of policy implementation science in cancer control in the USA forward. We have a robust set of methods within implementation science that are increasing the pace of adoption and maintenance of evidence-based programs in a variety of settings. Building on these efforts, the time is right to expand our methods to include policy implementation.
Implications.
Practice: Although most efforts to increase uptake of the scientific evidence base reference translation to “practice and policy,” there has been relatively little emphasis in the USA on implementation at the policy level, especially related to cancer control.
Policy: Expanding the focus of implementation science in cancer control to systematically address policy could increase use of scientific evidence in general and address health equity.
Research: By systematically applying IS strategies to policy targets and by drawing on political science theories and frameworks, the field of policy implementation science in cancer control in the USA could move forward significantly.
Brief Summary
To achieve the full benefits of scientific discovery on health, policy must be considered as a key mechanism by which evidence can be translated to practice.
Introduction
There is a significant imperative to translate scientific evidence into actions to improve the public’s health. This effort has been embodied in implementation science, which focuses on understanding the context in which evidence-based programs or practices are implemented, and the factors both within and outside the organization that influence adoption [1]. An extensive effort has been undertaken to build the field of implementation science in its application to cancer control, to support more rapid and effective translation of scientific evidence focused on cancer prevention, detection, and treatment. As a result, there has been a strong focus on improving evidence-based practice at the clinical practice, community, organizational, and health system levels. However, there has been relatively little emphasis on integration of evidence at the policy level, especially outside of healthcare. This is a particular concern, as policy sets the context for the delivery of preventive care and for mechanisms outside of the health care system that influence cancer risk and outcomes. Policy can eradicate or reinforce systemic structures that lead to cancer disparities as well as overall health inequalities. For example, federal policy, as written into the Affordable Care Act, mandates coverage of preventive health services without cost-sharing (U.S. Government, 2015). A study using data from community health centers that serve largely low income groups found that all race/ethnicity groups in states that expanded Medicaid as well as non-expansion states improved their odds of cervical cancer screening from before to 2 years following the Affordable Care Act implementation [2]. The largest improvement was among non-Hispanic blacks in expansion states, demonstrating the impact of implementation of policy ensuring access to cancer screening without cost on equity in both income level and race/ethnicity. If over time the gaps close among low-income and racial/ethnic minority women, it will further illustrate the impact of this policy on long-standing inequities in cancer-relevant outcomes.
Policy provides the context by which structural factors influence health, as has been recognized in Health in All Policies (HiAP), a cross-sector collaborative approach to improving population health and addressing inequities by incorporating health considerations into all levels of policy-making [3]. Most research related to HiAP has been descriptive, and the need for more systematic study of the implementation and outcomes of HiAP approaches has been noted [4,5]. However, it is clear that every aspect of policy development can variably impact different population groups, in terms of who is included and who is not, whose needs are being addressed and whose are not, what evidence is or is not considered in formulating the policy, and who is the target of any evaluation of policy impact. The process of policy implementation can further impact health disparities. For example, in a strategic effort to reduce health care inequality, the Affordable Care Act (ACA) implementation included provisions to ensure access to evidence-based screening interventions at no added cost and provided resources to enable community health centers to meet the demand for increased preventive care among low-income and vulnerable patient populations. If the implementation of the ACA had not included the expanded capacity of the health care system caring for those newly coming into primary care, there would have been limited likelihood of any impact on health equity-related outcomes. Policy clearly has the potential to advance equity by promoting evidence-based structural policy changes that impact social determinants of health.
We have three goals for this Commentary. First, we make the case for expanding the focus of implementation science in cancer control to more systematically address policy aimed to increase use of scientific evidence, to better understand the translation of evidence to health-related policy, and to advance health equity. We refer to this area of inquiry here forward as policy implementation science (IS). Second, we look to the field of political science to inform policy IS through transdisciplinary engagement that could impact both fields. Third, we propose ideas for future research that could help move the field of policy IS in cancer control forward. We use the Centers for Disease Control definition of policy as a law, regulation, procedure, administrative action, incentive, or voluntary practice of governments and other institutions [6].
IMPLEMENTATION SCIENCE SHOULD MORE SYSTEMATICALLY ADDRESS POLICY TO INCREASE USE OF EVIDENCE AND IMPACT ON HEALTH EQUITY” [GOAL #1]
Implementation science (IS) often refers to “practice and policy”; however, little attention has been paid to the development of specific models and methods that would support application to policy. There are some research areas in which policy has been a major focus, such as tobacco control [7]. However, the application of IS principles to the adoption of evidence-based tobacco control policies has been limited [8]. This may at least in part explain why significant variability in tobacco control policies still exists 15 years after the introduction of the WHO Framework Convention on Tobacco Control (FCTC). For example, research has demonstrated that cigarette taxes are the most effective tobacco control measure, but they remain the least utilized approach, with only 14% of countries meeting FCTC tax guidelines [8]. IS could significantly contribute to our understanding of the circumstances under which tobacco control policies are more likely to be implemented. IS could further help ensure full implementation of policies once adopted, which remains a significant problem.
There has been a substantial body of work in IS designed to move evidence-based intervention strategies into practice in settings that may impact on health equity [9–11]. For example, patient navigation is an evidence-based strategy to close gaps and reduce disparities in cancer screening [12], and IS studies have focused on increasing the use of navigation in health systems that provide care for low-income patients [13]. However, patient navigation is generally not a billable service and there are no systemic funding mechanisms for navigators, rendering it difficult to sustain and scale. Policy solutions can increase access to evidence-based approaches, such as patient navigation, by ensuring that funding and access mechanisms are in place in settings that reach underserved populations, which would likely affect health inequality. There has been little if any systematic research on increasing implementation of policies to provide financial sustainability for these programs, which would increase their uptake and use and likely their sustainment [14]. There are many other examples of ways in which IS could address systemic factors that reduce the application of evidence to improve health equity.
A concentrated focus on policy IS should explore how IS may contribute to understanding the translation of scientific evidence to health-related policy in governmental and nongovernmental sectors. Policy IS should consider the entire policy lifecycle, from the factors that influence how scientific evidence is included or excluded in policies when formulated and adopted, to implementation processes designed to ensure that policies are implemented as intended and evaluated for long-term impact on the intended outcomes and on health equity.
CONTRIBUTIONS OF POLITICAL SCIENCE TO ADVANCING POLICY IMPLEMENTATION SCIENCE THROUGH TRANSDISCIPLINARY ENGAGEMENT [GOAL #2]
There are several ways in which research in other fields could inform policy IS. The field of political science in particular has developed a robust body of work that is highly informative, referred to as policy implementation research (PIR). PIR focuses exclusively on the use of policy by governments, is largely descriptive and reliant on case study methodology, and is typically agnostic to health outcomes [15]. In contrast, IS has largely focused on health, developing alongside the evidence-based medicine tradition, drawing on a range of experimental and non-experimental designs, extensive use of quantitative methods, and expansive development of guiding conceptual frameworks. We believe that the field of IS would benefit significantly from considering tools and knowledge generated by the political science field. There are a number of key insights from political science that are particularly relevant.
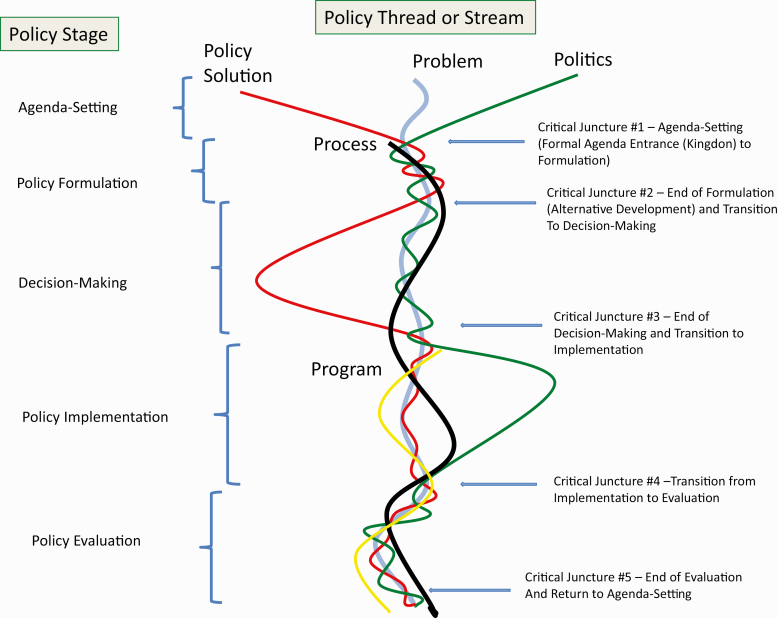
First is the opportunity to understand the policy-making process. The policy-making process is often depicted as a life cycle, that although elegant in its simplicity [16], has been heavily criticized as too neatly depicting what is rarely a linear process [17]. Perl, Howlett, McConnell [18] have recently proposed the Five-Stream Framework that identifies critical juncture points that enable each stage of the policy process (see Fig. 1), reflecting conceptualization of the problem and possible policy solutions, the political context, and the implementation process. Each of the five confluence points brings in new actors, strategies, and resources and yields a different configuration of policy inputs. Analysis of activities and outcomes in the five streams helps understand why particular policy solutions were selected, and what the impact was of different political vs public interests [18]. IS methods could be applied to examine the ways in which the intersection between the policy streams can be facilitated at each stage of the policy process, as well as critical processes within each stream that are associated with various implementation outcomes. IS objectives could help inform several junctures along the policy thread, such as examining how scientific evidence is considered during the formulation phase, to providing an ongoing monitoring toolbox post-implementation. The Five Streams Framework has not to our knowledge been applied to nongovernmental policy development, and this is an area in which IS could make a contribution generally, as well as related to the implementation of effective cancer control policies within organizations that influence people’s daily lives. Nongovernmental policy development is often less structured than public policy making, and implementation may reflect significant variations across levels of an organization. Although legal and regulatory processes may take a different form in nongovernmental policy-making, they are still a factor, as is the political process. With significant opportunities for cancer control policies to be implemented within multiple organizations that influence health, there is a significant benefit in using this Framework and other models from organizational behavior [19].
Fig. 1.
The Five-Stream Framework of the Policy Process. Perl A, Howlett M, McConnell A Moving policy theory forward: Connecting multiple stream and advocacy coalition frameworks to policy cycle models of analysis. Australian Journal of Public Administration 2016. 76(1): p. 65–79.
The second contribution of the political science literature is the emphasis on the outer context. IS recognizes the critical role of context [20], but in application there has been more focus on the inner organizational context such as organizational environment than on outer contextual factors such as the policy and political environment. Rarely are these factors that sit outside of the target system or setting studied in a comprehensive way. Political science frameworks can help us to unpack the components of the outer context, especially as related to policy implementation, and provide an opportunity to explore and expand the role of outer context across content area applications within IS. Chriqui et al. [21] illustrate the importance of studying outer contextual factors for their impact on policy implementation. Researchers examined whether state wellness policy requirement laws and district local wellness policy influence district level policy implementation, as is required of districts that participate in the federal Child Nutrition Program. Even with prevailing federal law, districts that were also subject to state laws requiring wellness policies had more comprehensive policies and higher levels of implementation [22]. This study is notable for examining the association of outer context policy environments on local wellness policy implementation and is a useful case study to better understand the barriers and opportunities for more robust implementation of health-related policies.
The third contribution of political science is its definition of different policy instruments that can be used to translate evidence into policy. Just as there are a range of implementation strategies that we use to translate evidence into practice, there are a range of policy approaches that can be used, including (a) education/knowledge (e.g., training, certification, and reporting); (b) authority (e.g., regulation, licenses, treaties, and reporting); (c) treasury (e.g., financial incentives/disincentives, taxes, and grants); and (d) organizational structure (e.g., governance, record-keeping, tools, and information technology infrastructure) [23–25]. The political science field largely examines how governments put policies into effect. There are key opportunities for implementation scientists to expand their range of translation strategies to include a range of policy instruments, and to add understanding to how these policy vehicles may apply to nongovernmental policies.
Fourth, the political science literature recognizes the long and complex time trajectory of policy-making, sometimes spanning many years, as well as the interdependency between the many factors that influence the policy process [15]. IS studies targeting uptake of evidence-based practices typically focus on short time perspectives for adopting processes into a healthcare delivery system or community organization. As the IS field expands to include a focus on policy, it will be critical to consider a longer time horizon and how to integrate a more fluid process than is typically found in implementation of evidence-based practices. The impact of time on the policy context is also important to consider. For example, in the early days of tobacco control, the tobacco industry formed strong alliances with retailers to combat tobacco taxes and other policy restrictions. A recent study of the implementation context for a $2 tobacco tax increase in San Francisco revealed retailers’ concerns about selling tobacco in relation to the health of their customers [26]. These findings suggest that retailers may now be allies in tobacco control efforts, reflecting a significant change in the policy implementation climate over time.
Finally, we argue that implementation science frameworks, methods, and outcomes could add value to the political science field. There can be significant value in shared training experiences across these fields, and in developing transdisciplinary teams that could traverse between the methods and measures of both fields.
DEVELOPING A RESEARCH AGENDA TO ADVANCE POLICY IMPLEMENTATION SCIENCE [GOAL #3]
Building on contributions from the political science field, there are key gap areas that could be addressed by IS related to cancer control policy implementation, as noted in Table 1 and in the text that follows.
Table 1.
Recommendations for expanding research inquiry in Policy Implementation Science
| Examine whether existing IS conceptual frameworks can more explicitly focus on policy |
| Develop and use policy-relevant measures |
| Study the intersection between policy instruments and the policy context |
| Develop collaboration structures that support policy implementation science |
| Be explicit about the factors that influence the knowledge to policy interface |
| Comprehensively explore the impact of all aspects of policy implementation on health equity |
We should examine whether existing IS conceptual frameworks can accommodate a more explicit focus on policy. There is much to be said about adopting frameworks that are fully focused on policy. However, there could also be significant gains made by integrating policy-relevant factors into more traditional IS frameworks that include other implementation targets. Bullock et al. [27] conducted a critical interpretive synthesis to develop an integrated conceptual framework of the determinants of implementation from a policy perspective. Further consideration of the intersection between policy-oriented and IS frameworks would likely move the field forward in more fully integrating policy as a translational lever and may simultaneously inform our conceptualization of implementation overall. For example, in describing the policy context, Bullock notes the importance of the context of policy actors that are central to the formulation, adoption, and implementation of policy. Although inner context is a key part of most IS frameworks, less common is a clear focus on the context of the specific people involved, and the critical impact that may have on implementation outcomes.
We need to develop and use policy-relevant measures. A key gap has been the availability of valid measures that can enable us to disentangle the differential impacts of policy implementation determinants and outcomes. A recent systematic review by Allen et al. [28] identified quantitative measures to assess both determinants and outcomes for policy IS. They identified 15 “mostly transferable” measures from studies of health policy implementation, including measures of fidelity and adaptation, organizational culture and climate, implementation costs, acceptability, and readiness for implementation. However, it was rare for these constructs to be defined, and little data on measuring validity and reliability were available. There is a clear need for precision, clarity, and rigor in the development and use of policy-relevant measures.
We need to study the intersection between policy instruments and the policy context. The field will benefit from understanding the impact of different policy instruments on different policy issues, and the ways in which policy instruments may shape and define context. For example, policies governing the sale of tobacco establish a context in which those thinking about implementation of tobacco use prevention or treatment programs operate, shifting the locus and nature of those programs. Policies that change the rules for the sale of e-cigarettes, the legal age of tobacco use, and the availability of flavored products ideally reduce the sale of products that increase cancer risk and provide a context in which evidence-based prevention and treatment programs can be offered. However, policies may also cause unintended consequences that adversely change the context, such as when policies in adjacent localities do not change, or when loopholes allow barriers to tobacco use to be easily overcome. It is unclear what the impact on tobacco use will be of a ban in one state when population centers are in close proximity to other states that do not have such bans. This is especially a concern when a policy is designed to address health equity, such as the recently enacted menthol flavor ban in Massachusetts. This is an excellent example of the intersection between the use of a strong policy instrument, such as a product ban, and policy context in which the ban may be easily by-passed.
Similarly, we need to understand how the policy context shapes the development and implementation of the policy instrument itself. Even if a policy as designed was evidence-based, lobbying interests and political processes that are part of the policy context can lead to changes that diminish reliance on evidence. We also need to understand the way in which context shapes policy throughout adoption and implementation processes. As policy instruments themselves are interventions that need to fit the context in which they are being placed, it would be extremely helpful to identify contextual factors that increase their adoption, and whether those vary by policy topic. For example, some policy innovations are designed to directly engage patients and flexibly provide care, such as policies that support use of telehealth. However, the local context in settings with limited broadband access does not allow for the intended benefits to be derived. Without careful consideration of the ways in which different policy options could influence outcomes in different contexts, policy development and implementation could reduce or exacerbate health inequality. We need research that helps us understand the ways in which the specific policy target and the context are optimally considered in the policy process. For example, Falbe et al. [29] utilized an implementation process approach to examine the impact of the first U.S. sugar-sweetened beverage tax in Berkeley, CA. They determined that the simplicity of the policy package, the inner and outer context, and the process utilized to implement the tax facilitated its success. In particular, key contextual factors included local leadership that was supported by a history of policies focused on health equity, supportive institutions, and positive public opinion [30]. Makse and Volden [31] also note the importance of simplicity in increasing uptake, irrespective of the policy instruments used.
We need collaboration structures that support policy implementation science. In the USA, knowledge translation to policy has largely been a decentralized process, with little governmental intervention to facilitate evidence-based policy-making. Several other countries have been more systematic, building translational networks specifically designed to improve evidence translation to policy. For example, the Canadian Health Services Research Foundation was established specifically to facilitate the translation of research evidence into policy [32]. By embedding strategies to link researchers and policy-makers and provide opportunities for knowledge exchange, they created an infrastructure in which both cultural and structural barriers were naturally addressed. Ontario’s AIDS Bureau explicitly uses “receptors,” or roles that have explicit responsibility for establishing and maintaining linkages with researchers [32]. The Centre for Informing Policy in Health with Evidence from Research (CIPHER) was an explicit collaboration between research and national policy agencies in Australia to create a network designed to support the use of research in policies [33]. England conducts pilots in most areas of health policy development, which serves as both an important function within evidence translation and as a political process extends beyond evidence generation [34].
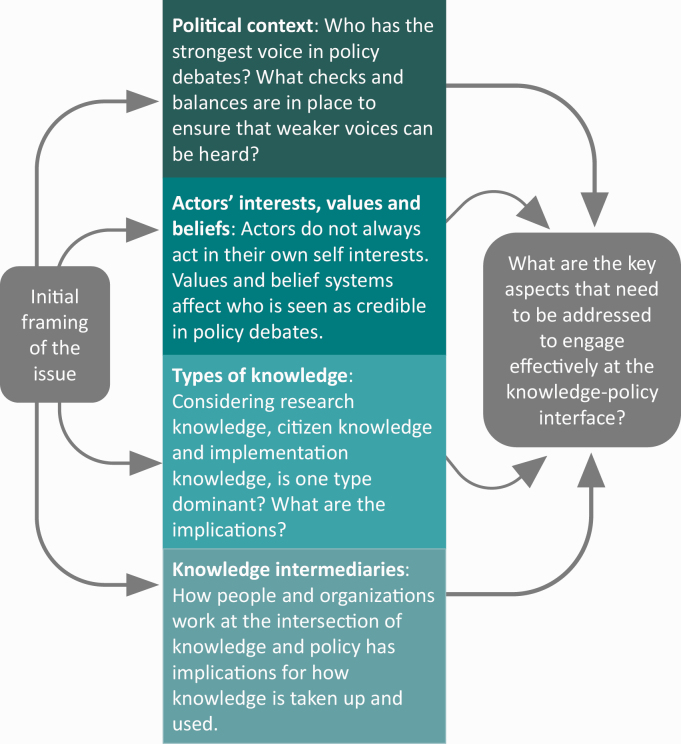
We need to be explicit about the factors that influence the knowledge to policy interface. Jones et al. [35] developed the Knowledge, Policy, and Power (KPP) Framework to illustrate the knowledge translation process in the context of international development (see Fig. 2). Four dimensions influence the use of knowledge in policy, including: (a) features of the political context that shape knowledge-policy interactions, such as spaces for participation, informal politics, and the ability to absorb change; (b) the relative strengths of participants involved in both knowledge production and policy-making; (c) the salience of different types of knowledge generated and sought; and (d) the availability and role of knowledge intermediaries that sit between the systems of knowledge production and policy development. This framework highlights the fact that different factors may be important at different points of knowledge-policy interface and for different types of knowledge. The authors note the importance of triangulating research-based knowledge, practice-informed knowledge, and citizen or participatory knowledge, and the importance of broadening the range of channels available for knowledge interaction. The KPP Framework could contribute to understanding impact on policy translation of different collaborations.
Fig. 2.
The Knowledge, Policy, and Power Framework. Shaxson L, Jones H, Jones N, Walker D. Knoweldge, policy and power in international development: A practical framework for improving policy., in Background Note. 2013, Overseas Development Institute. https://cdn.odi.org/media/documents/8201.pdf
In the USA, elected legislators are central to the policymaking process and make decisions that affect health without specialized knowledge of health issues. Consideration of strategies to translate and disseminate evidence to legislators that are clear and resonate is vital and IS can offer strategies to more effectively expand on such opportunities. Research by Dodson et al. [36] to increase the dissemination of evidence-based interventions among state-level policymakers found that a majority of legislators working on health-related issues sought evidence in the form of data and statistics—specifically data on demographics of populations affected by disease, prevalence, causes of health issues, and disparity information. Other legislators indicated a preference for information in the form of stories because of their power to convince. Others still indicated that they find information helpful when it includes both stories and data. This heterogeneity dovetails with findings by Purtle et al. [37] who used audience segmentation research to better understand and inform dissemination strategies tailored for legislators with different characteristics. They categorized state legislators based on characteristics that may have implications for knowledge transfer to lawmakers. For example, legislators who were most influenced by budget impact were also most skeptical of behavioral health treatment effectiveness. This suggests that to increase research use, evidence clearinghouses could include economic evaluation data in their analysis, while also fostering positive relationships with behavioral health researchers.
We need to comprehensively explore the impact of policies on health equity. Although health equity is implicit in the Health in All Policies Framework, IS could greatly contribute to our understanding of the ways in which cross-sector policy adoption can mitigate health inequities, especially those maintained by structural forces [28]. The COVID-19 pandemic has revealed in stark terms the deep-seated and systemic inequalities in health for communities of color and renewed focus on the social and economic factors that contribute to poor health outcomes. State and local policies related to where and when COVID testing and subsequently vaccine was available in some cases targeted those inequities explicitly, ensuring that those who had the most risk and disease burden had easy and convenient access. In other jurisdictions, policies were set based on aggregated state-level data, obscuring inequities and the social factors that must be considered in addressing them, such as access to transportation to testing and vaccination sites and ability to seek care during working hours. The influence of policies derived by different systems can also reinforce health inequities, as we have seen by the impact of work at home and sick leave policies which significantly reduced COVID risk among more affluent workers, and increased risk and burden among lower income and vulnerable groups who did not have the ability to work from home or access to sick leave.
IS offers a lens through which we can recognize health inequities as a special case of implementation failure. Woodward et al. [38] combined two conceptual frameworks—one from implementation science and one from healthcare disparities research to develop the Health Equity Implementation Framework. This framework has helped to identify barriers and facilitators across levels, highlighting that some barriers are due to general implementation issues (e.g., poor care coordination after positive test results), while other barriers are related to structural forces. We should not miss the opportunity to consider and rigorously evaluate policies for their impact on health inequity, and the structural forces that hold them in place. In fact, we argue that equity considerations should be an integral component of policy IS efforts, because of the significant risk of doing harm without such a focus.
Conclusions
Our goal for this Commentary was to stimulate the field of implementation science to more systematically consider policy implementation. Although most efforts to increase uptake of the scientific evidence base reference translation to “practice and policy,” there has been relatively little emphasis in the USA on implementation at the policy level, especially related to cancer control. If we are to achieve the full benefits of scientific discovery on population and public health, we will need to consider both governmental and nongovernmental policy as a critical mechanism by which evidence can translated to practice. The more that policies consider health impacts and that implementation efforts are evaluated for their impact on health and health equity, the more positive benefits we will likely see. We have a robust set of methods within implementation science that are increasing the pace of adoption and maintenance of evidence-based programs in a variety of settings. Building on these efforts, the time is right to expand our methods and focus on policy implementation.
Acknowledgments
The first author’s work on this paper was funded through an IPA with the Division of Cancer Prevention and Control Sciences at NCI.
Authors’ Contributions: All authors participated in the conceptualization, writing, and editing of the manuscript.
COMPLIANCE WITH ETHICAL STANDARDS
Conflicts of Interest: Karen M. Emmons, David Chambers, and Ali Abazeed have no conflict of interest to report.
Ethical Approval: This article does not contain any studies with human participants performed by any of the authors. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: This study does not involve human participants and informed consent was therefore not required.
References
- 1. Brownson RC, Proctor E, Colditz GA.. Dissemination and Implementation Research in Health: Translating Science to Practice 2 nd Edition. New York: Oxford University Press; 2018. [Google Scholar]
- 2. Huguet N, Angier H, Rdesinski R, Hoopes M, Marino M, Holderness H, DeVoe JE. Cervical and colorectal cancer screening prevalence before and after Affordable Care Act Medicaid expansion. Prev Med. 2019;124:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rudolph L, Caplan J, Ben-Moshe K, Dillon L.. Health in All Policies: A Guide for State and Local Governments. Washington, DC: American Public Health Association and Public Health Institute, 2013. [Google Scholar]
- 4. Hahn RA. Two paths to health in all policies: the traditional public health path and the path of social determinants. Am J Public Health. 2019;109(2):253–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hoagwood KE, Purtle J, Spandorfer J, Peth-Pierce R, Horwitz SM. Aligning dissemination and implementation science with health policies to improve children’s mental health. Am Psychol. 2020;75(8):1130–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Centers for Disease Control and Prevention. Overview of CDC’s Policy Process. Atlanta, GA: Centers for Disease Control; 2012. [Google Scholar]
- 7. Peruga A, Lopez MJ, Martinez C, Fernandez E. Tobacco control policies in the 21(st) century: achievements and open challenges. Mol Oncol 2021;15(3):744–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Salloum RG, Parascandola M, LeLaurin JH, Shelley D. The Role of Dissemination and Implementation Research in Global Tobacco Control: a Report from the American Society of Preventive Oncology. Cancer Epidemiol Biomarkers Prev. 2020;29(12):2740–2743. [DOI] [PubMed] [Google Scholar]
- 9. Baumann AA, Cabassa LJ. Reframing implementation science to address inequities in healthcare delivery. BMC Health Serv Res. 2020;20(1):190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mensah GA, Riley WT. Social determinants of health and implementation research: three decades of progress and a need for convergence. Ethn Dis. 2021;31(1):1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chinman M, Woodward EN, Curran GM, Hausmann LRM. Harnessing implementation science to increase the impact of health equity research. Med Care. 2017;55Suppl 9 Suppl 2:S16–S23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. The Community Guide to Preventive Services. Atlanta, GA: Centers for Disease Control and Prevention; 2020. [Google Scholar]
- 13. Highfield L, Valerio MA, Fernandez ME, Eldridge-Bartholomew LK. Development of an implementation intervention using intervention mapping to increase mammography among low income women. Front Public Health. 2018;6:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shelton RC, Cooper BR, Stirman SW. The sustainability of evidence-based interventions and practices in public health and health care. Annu Rev Public Health. 2018;39:55–76. [DOI] [PubMed] [Google Scholar]
- 15. Nilsen P, Ståhl C, Roback K, Cairney P. Never the twain shall meet?–a comparison of implementation science and policy implementation research. Implement Sci. 2013;8(1):63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nakamura R. The textbook policy process and implementation research. Policy Stud Rev. 1987;7(1):142–154. [Google Scholar]
- 17. Cairney P, Kwiatkowski R. How to communicate effectively with policymakers: combine insights from psychology and policy studies. Palgrave Commun. 2017;3(1):37. [Google Scholar]
- 18. Perl A, Howlett M, McConnell A. Moving policy theory forward: connecting multiple stream and advocacy coalition frameworks to policy cycle models of analysis. Aust J Public Adm. 2016;76(1):65–79. [Google Scholar]
- 19. Borkowski N, Meese K.. Organizational Behavior, Theory, and Design in Health Care. 3rd ed. Burligton MA: Jones & Bartlett Learning; 2022. [Google Scholar]
- 20. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Chriqui JF, Leider J, Turner L, Piekarz-Porter E, Schwartz MB. State Wellness Policy Requirement Laws matter for District Wellness Policy Comprehensiveness and Wellness Policy Implementation in the United States. Nutrients 2021;13(1):88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Centers for Disease Control and Prevention. Putting Local School Wellness Policies into Action. Atlanta, GA: US Dept of Health and Human Services; 2014. [Google Scholar]
- 23. Howlett M, Ramesh M.. Studying Public Policy: Policy Cycles and Policy Subsystems. 2nd ed. New York, NY: Oxford University Press; 2003. [Google Scholar]
- 24. Shroff MR, Jones SJ, Frongillo EA, Howlett M. Policy instruments used by States seeking to improve school food environments. Am J Public Health. 2012;102(2):222–229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ejler N, J Ostersen, Graff D, Dyrby T.. New Approaches to Policy Implementation. Copenhagen, Denmark: Ramboll; 2016. [Google Scholar]
- 26. Chavez G, Minkler M, McDaniel PA, Estrada J, Thayer R, Falbe J. Retailers’ perspectives on selling tobacco in a low-income San Francisco neighbourhood after California’s $2 tobacco tax increase. Tob Control. 2019;28(6):657–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bullock HL, Lavis JN, Wilson MG, Mulvale G, Miatello A. Understanding the implementation of evidence-informed policies and practices from a policy perspective: a critical interpretive synthesis. Implement Sci. 2021;16(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Allen P, Pilar M, Walsh-Bailey C, et al. Quantitative measures of health policy implementation determinants and outcomes: a systematic review. Implement Sci. 2020;15(1):47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Falbe J, Grummon AH, Rojas N, Ryan-Ibarra S, Silver LD, Madsen KA. Implementation of the First US Sugar-Sweetened Beverage Tax in Berkeley, CA, 2015-2019. Am J Public Health. 2020;110(9):1429–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bleich SN, Chriqui J, Ng SW. Implementation science is important for understanding and advancing Beverage Taxes. Am J Public Health. 2020;110(9):1266–1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Makse T, Volden C. The role of policy attributes in the diffusion of innovations. J. Politics 2011;73(1):108–124. [Google Scholar]
- 32. Williamson A, Barker D, Green S, et al. Using ‘linkage and exchange’ to move research into policy at a Canadian foundation. Health Aff (Millwood). 2000;19(3):236–240. [DOI] [PubMed] [Google Scholar]
- 33. Williamson A, Barker D, Green S, et al. Increasing the capacity of policy agencies to use research findings: a stepped-wedge trial. Health Res Policy Syst. 2019;17(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ettelt S, Mays N, Allen P. The multiple purposes of policy piloting and their consequences: three examples from National Health and Social Care Policy in England. J. Soc. Policy 2014;44(2):319–337. [Google Scholar]
- 35. Jones H, Jones N, Shaxson L, Walker D.. Knoweldge, policy and power in international development: A practical framework for improving policy., in Background Note. London: Overseas Development Institute; 2013. [Google Scholar]
- 36. Dodson EA, Geary NA, Brownson RC. State legislators’ sources and use of information: bridging the gap between research and policy. Health Educ Res. 2015;30(6):840–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Purtle J, Lê-Scherban F, Wang X, Shattuck PT, Proctor EK, Brownson RC. Audience segmentation to disseminate behavioral health evidence to legislators: an empirical clustering analysis. Implement Sci. 2018;13(1):121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Woodward EN, Matthieu MM, Uchendu US, Rogal S, Kirchner JE. The health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement Sci. 2019;14(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]