To the Editor:
The outbreak of coronavirus disease (COVID-19) has extensively impacted global health. The spike protein on the surface of the causative pathogen severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) binds to the angiotensin-converting enzyme 2 (ACE2) receptor, a metallocarboxypeptidase, which is expressed in both mACE2 (membrane-anchored ACE2) and sACE2 (soluble ACE2) forms in the lung. Although mACE2 is responsible for viral entry, recent observations also suggest that sACE2 is involved, by its interaction with the spike protein, followed by receptor-mediated endocytosis of the viral particles (1). Tobacco use has been speculated as a risk factor for contracting SARS-CoV-2 infection and subsequent disease severity (2, 3), and electronic cigarettes (e-cigarettes) have been shown to induce harmful proteomic and immune changes in the lungs of vapers (4). In addition, the effect of vaping, and the role of nicotine, in the regulation of ACE2 expression has been demonstrated in animal models and cell culture systems (5–8). We therefore tested the hypothesis that combustible tobacco (e.g., cigarettes) and noncombustible e-cigarettes could affect ACE2 activity and subsequent SARS-CoV-2 infection. Some of our data have been reported previously at an international conference (9) and deposited in a preprint repository (https://doi.org/10.1101/2021.06.04.447156).
We first evaluated sACE2 activity in concentrated bronchoalveolar lavage fluid (BALF) samples from nonsmokers (age, 28.5 ± 9.5 yr; body mass index [BMI], 28.8 ± 7.2 kg/m2; FVC% predicted, 98.0 ± 25.0; FEV1% predicted, 101.6 ± 14.5), smokers (age, 34.4 ± 8.2 yr; BMI, 27.5 ± 7.8 kg/m2; FVC% predicted, 104.2 ± 11.2; FEV1% predicted, 97.9 ± 16.1), and vapers (age, 29.3 ± 9.1 yr; BMI, 29.6 ± 8.0 kg/m2; FVC% predicted, 106.2 ± 11.2; FEV1% predicted, 104.5 ± 7.7). Details of the subject recruitment criteria and the study design have been published (4, 10, 11). We measured cleavage of an ACE2-specific fluorogenic peptide (SFQ-3819-PI; vivitide) by using a microplate reader to evaluate ACE2 activity as described (4). sACE2 activity was significantly increased in BALF from both smokers and vapers compared with age-matched nonsmokers (Figure 1A), indicating heightened vulnerability toward SARS-CoV-2 infection in both groups.
Figure 1.
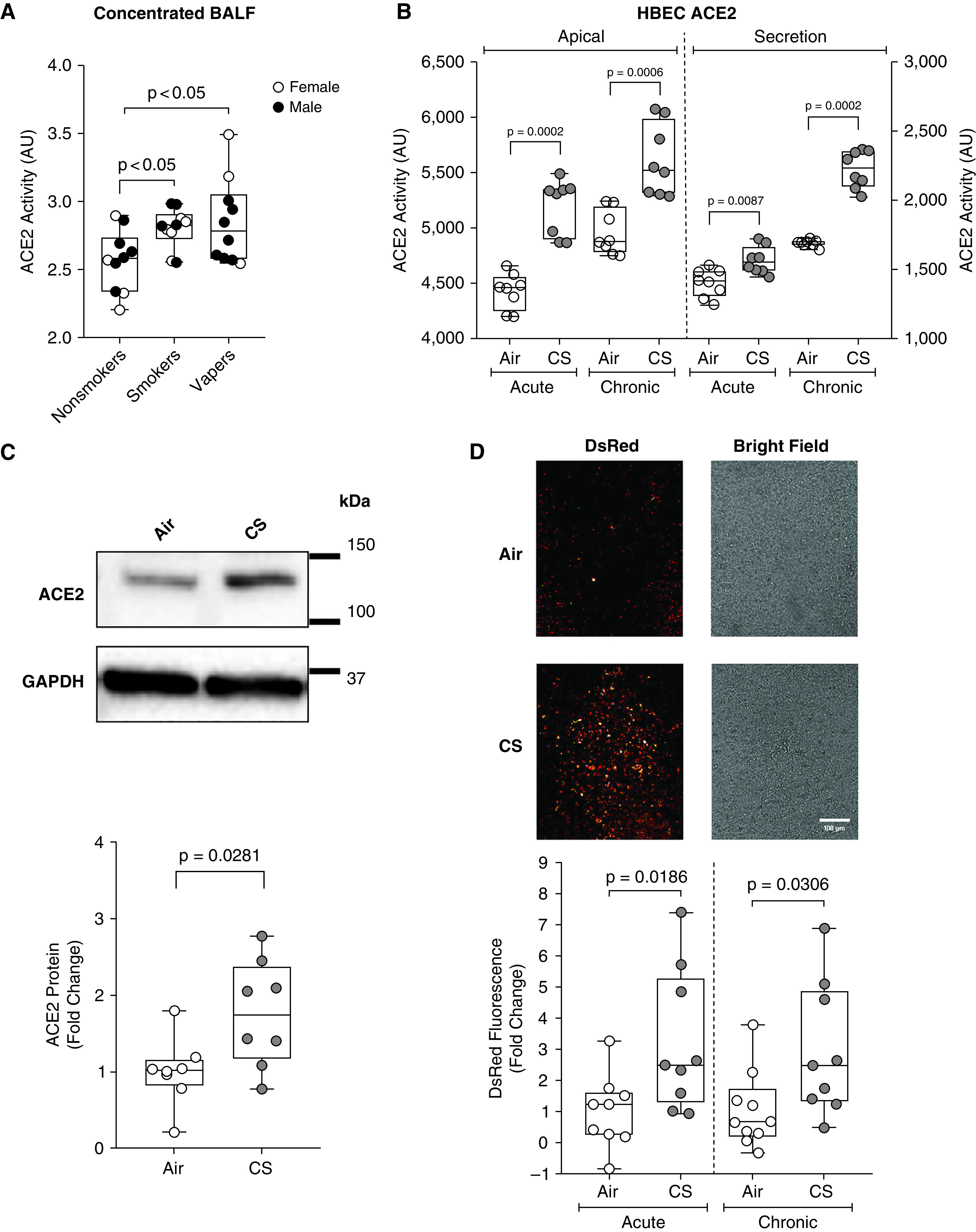
Cigarette smoke (CS) increases ACE2 (angiotensin-converting enzyme 2) activity and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. BAL fluids from nonsmokers, smokers, and vapers (n = 10 each) were concentrated, and ACE2 activity was measured by using 50-μM specific fluorogenic substrates. (A) Cleaved substrate–derived fluorescence shown as arbitrary units following 1 hour of reaction. HBECs were cultured at the air–liquid interface and exposed to smoke from one Kentucky research cigarette (1R6F) per day for 1 day (acute) or 4 days (chronic). The apical surface was washed with PBS to collect the mucosal secretion and 50-μM fluorogenic substrate was added on the apical surface to evaluate apical ACE2 activity. (B) ACE2 activity on the apical side of acutely and chronically smoke-exposed cultures and the corresponding apical washes. Activities are presented as accumulated fluorescence in arbitrary units of the cleaved products following 10 minutes of reaction. Whole-cell lysates were collected from chronically CS-exposed cultures, and ACE2 and GAPDH protein expression were evaluated by using immunoblotting. (C) Representative and GAPDH-normalized ACE2 expression in air- and smoke-exposed cultures shown as the fold change. (D) Acutely or chronically smoke-exposed cultures were apically exposed to a Spike pseudovirus suspension, and the resulting DsRed marker fluorescence was recorded after 3 days. Representative confocal microscopic images (SP8; Leica Microsystems) with the corresponding bright fields are shown above the DsRed fluorescence fold changes. Scale bar, 100 μm. Data are presented as the median and lower and upper quartiles; n = 8–9 per group from 3–4 different donors. P values are provided on the graph. AU = arbitrary unit; BALF = BAL fluid; CS = cigarette smoke; HBEC = human bronchial epithelial cell.
To evaluate the impact of tobacco smoke on ACE2 activity, we cultured primary human bronchial epithelial cells (HBECs) at the air–liquid interface until they were well differentiated into ciliated and goblet cells (12) and then exposed them to 14 puffs of smoke per day from Kentucky research cigarettes (1R6F) for 1 day (acute) and 4 days (chronic) as previously reported (13). Acute smoke exposure significantly increased both mACE2 and sACE2 activity (Figure 1B). After chronic smoke exposure, both mACE2 and sACE2 activity remained significantly elevated in smoke-exposed cultures compared with air-exposed controls (Figure 1B). Consistent with these observations, ACE2 protein was significantly increased in chronically smoke-exposed cultures compared with air-exposed controls (Figure 1C), indicating that more receptors were potentially available for SARS-CoV-2 binding. As an orthogonal approach, we developed a pseudovirus by using recombinant vesicular stomatitis virus ΔG (a gift from Pengfei Wang, Columbia University) that contains the SARS-CoV-2 spike protein (145032; Addgene) in its membrane and expressed DsRed for the identification of infected cells. We exposed HBECs to acute and chronic tobacco smoke, which was followed by infection with 3 × 104 U/ml pseudovirus, and measured DsRed expression by using a microplate reader. Cigarette smoke exposure significantly increased DsRed fluorescence (increased viral infection; Figure 1D). We then incubated chronically air- and smoke-exposed HBECs with fluorescently labeled recombinant SARS-CoV-2 S1 protein. Consistent with the observed increase in ACE2 activity, smoke exposure caused a significant (20%, n = 9, P = 0.024) increase in S1 binding. Taken together, these data indicate that cigarette smoke exposure upregulates ACE2 activity and increases SARS-CoV-2 binding.
Next, to compare the potential impact of smoking and vaping on SARS-CoV-2 pseudovirus infection in cells from both the lower and upper airways, we explored the impact of cigarette smoke condensate (CSC) and e-liquid exposure on pseudovirus infection on ACE2 gene–expressing primary tracheobronchial cells (PCS-300-010; American Type Culture Collection) and small airway epithelial cells (PCS-301-010; American Type Culture Collection). We have previously demonstrated that these cell types express ACE2 (14). To ensure that these different cell types were studied at the same time, they were cultured to confluence on plastic instead of on semipermeable membranes; treated with a range of different doses of CSC (Murty Pharmaceuticals) or JUUL Virginia tobacco–flavored e-liquid (59 mg/ml nicotine) for 24 hours, which corresponded to a final nicotine concentration of 21.6–176 μM for CSC and 364–3,641 μM for JUUL e-liquid; and infected them with pseudovirus (2.5–5 × 105 U/ml). After all exposures, cellular viability was confirmed by positive culture characteristics under light microscopy. We then used fluorescent microscopy and flow cytometry to visualize and quantify this infection, respectively. Acute exposure to both CSC and JUUL e-liquid significantly increased DsRed fluorescence, indicating increased pseudovirus infection compared with control cells (Figures 2A–2D). These data correlate with our BALF data (Figure 1A) and indicate that both cigarettes and e-cigarettes increase the potential for SARS-CoV-2 infection.
Figure 2.
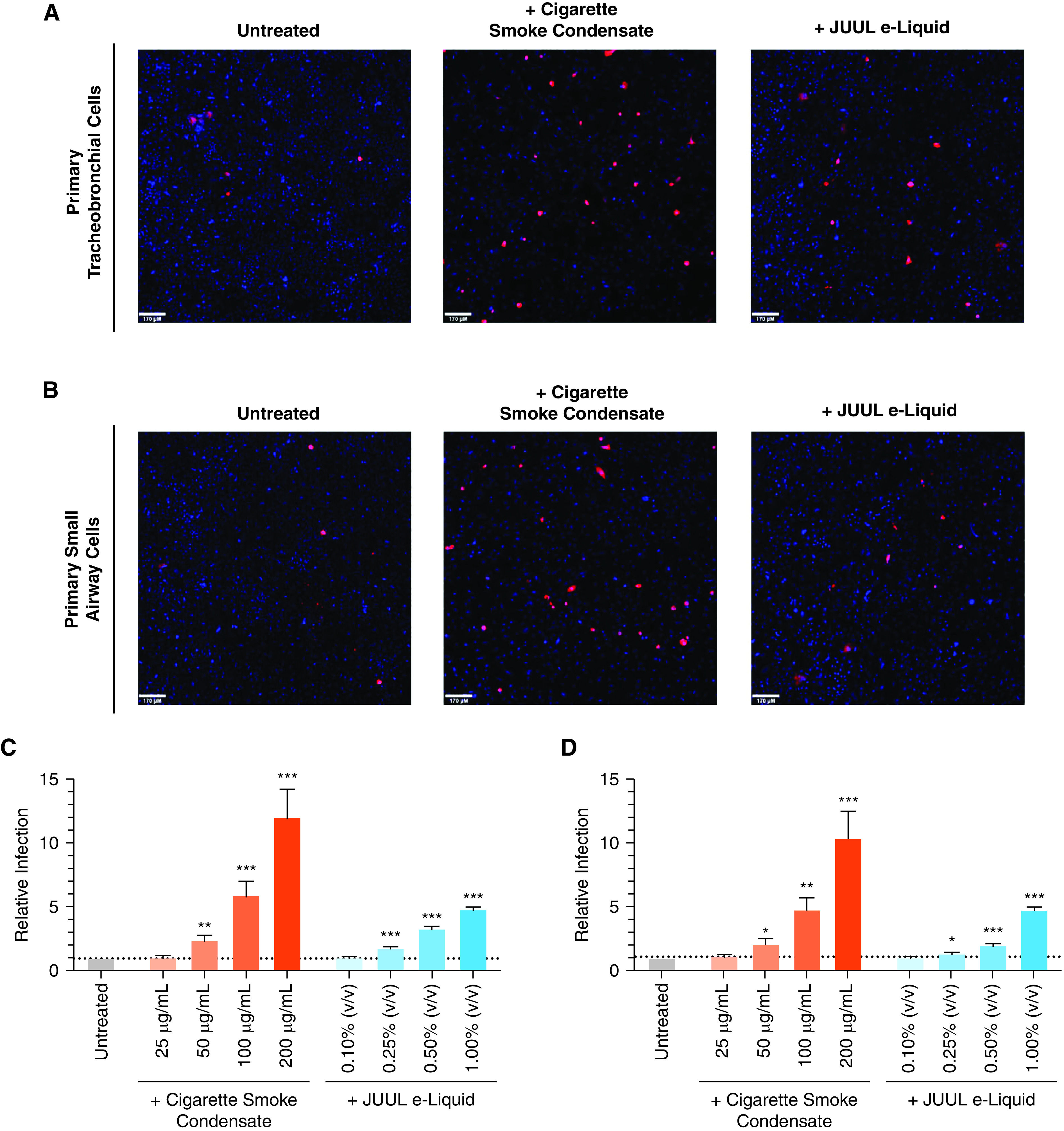
Cigarette smoke condensate (CSC) exposure increases severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pseudovirus infection. (A) Primary tracheobronchial cells and (B) small airway cells were pretreated with 200 μg/ml CSC (middle) and 1.00% JUUL e-liquid (right) for 24 hours and challenged with SARS-CoV-2 pseudovirus. After incubation for 48 hours, live cells were imaged on a spinning-disc confocal microscopy system (UltraVIEW Vox; PerkinElmer). Cell nuclei were stained with Hoechst dye, and infected cells are shown in red. Flow cytometry quantification of relative SARS-CoV-2 pseudovirus infection reported as the fold change in (C) primary tracheobronchial cells and (D) small airway cells pretreated with different doses of CSC and JUUL e-liquid; n = 11–12 separate experiments. Bars represent the mean ± SEM. *P < 0.05, **P < 0.005, and ***P < 0.0005, unpaired t test. Scale bars, 170 μm.
Several meta-analyses have been performed to look at tobacco use and COVID-19 disease severity, which have reported contradictory findings. A “nicotinic hypothesis” was proposed, which suggested that nicotine exerted a protective role against SARS-CoV-2 infection (15). Conversely, other reports confirmed a strong association between smoking and COVID-19 symptoms (2, 3). Increased ACE2 expression in smokers has been proposed as a risk factor for COVID-19 (16). Moreover, tobacco smoking is a risk factor for several other respiratory viruses, including influenza (17). Our current study provides further in vivo evidence that sACE2 is upregulated in smokers’ and vapers’ BALF. However, our study has some limitations. First, our study was cross-sectional and of a relatively low sample size, and we were unable to probe our data sets to understand the impact of sex, race, and other factors. A second limitation of our study is that we only measured sACE2, and not mACE2, in vivo. However, sACE2 facilitates SARS-CoV-2 infection through interactions with the renin–angiotensin system, and elevated sACE2 in smokers and vapers is expected to contribute toward SARS-CoV-2 infection (1). The increase in sACE2 most likely reflects an overall increase in cellular ACE2 expression. Indeed, ACE2 mRNA expression is elevated in smokers’ pulmonary cells relative to those derived from nonsmokers, suggesting that both mACE2 and sACE2 may be increased (14). Moreover, elevated sACE2 was positively associated with COVID-19 severity (18), demonstrating the utility of sACE2 as a marker of COVID-19 risk. Our in vitro CSC exposure represented the nicotine concentrations typically reached in smokers’ lungs (19). JUUL e-liquids contain 5% nicotine (∼300 mM). However, nicotine concentrations in the human lung after JUUL e-liquid inhalation are not known. Therefore, we added ∼0.1–1% of the JUUL e-liquid to cells on the basis of the assumption that 0.1–1% of e-liquid is deposited in the lung after vaping, owing to nicotine dilution kinetics. However, additional studies will be required to define JUUL nicotine concentrations in the lung and to understand whether different e-liquids affect ACE2 expression and SARS-CoV-2 infection in a similar fashion.
Nicotine, which is present in both combustible cigarettes and e-cigarettes, increases cellular Ca2+ concentrations (4). Elevated Ca2+ signaling is well recognized to play a vital role in facilitating viral entry, gene and protein processing, and subsequent viral release (20). Our studies demonstrate that tobacco and e-liquid exposures increase both ACE2 and SARS-CoV-2 spike protein binding. Thus, we hypothesize that nicotine may be responsible for the increased spike protein binding and subsequent pseudovirus infection. However, the underlying mechanisms, and the purported link to nicotine, will require additional study. We further speculate that acute but persistent increases in ACE2 and spike protein binding place tobacco users at risk of SARS-CoV-2 infection. Overall, these observations indicate that tobacco product use elevates ACE2 activity and increases the potential for SARS-CoV-2 infection through enhanced spike protein binding. Importantly, our results strongly urge consideration of vaping as a risk factor for COVID-19.
Footnotes
Supported by NIH/Food and Drug Administration grants HL120100 and HL153698, NIH/NHLBI grant HL135642, NIH grants R01CA237652 and 1DP5OD021385, an American Cancer Society Research Scholar Grant (J.M.S.), and a New York Community Trust grant (J.M.S.). Research reported in this publication was supported in part by the NIH and the Family Smoking Prevention and Tobacco Control Act. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Originally Published in Press as DOI: 10.1164/rccm.202106-1377LE on November 8, 2021
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1. Yeung ML, Teng JLL, Jia L, Zhang C, Huang C, Cai JP, et al. Soluble ACE2-mediated cell entry of SARS-CoV-2 via interaction with proteins related to the renin-angiotensin system. Cell . 2021;184:2212–2228, e12. doi: 10.1016/j.cell.2021.02.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Farsalinos K, Barbouni A, Poulas K, Polosa R, Caponnetto P, Niaura R. Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis. Ther Adv Chronic Dis . 2020;11 doi: 10.1177/2040622320935765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Karanasos A, Aznaouridis K, Latsios G, Synetos A, Plitaria S, Tousoulis D, et al. Impact of smoking status on disease severity and mortality of hospitalized patients with COVID-19 infection: a systematic review and meta-analysis. Nicotine Tob Res . 2020;22:1657–1659. doi: 10.1093/ntr/ntaa107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ghosh A, Coakley RD, Ghio AJ, Muhlebach MS, Esther CR, Jr, Alexis NE, et al. Chronic e-cigarette use increases neutrophil elastase and matrix metalloprotease levels in the lung. Am J Respir Crit Care Med . 2019;200:1392–1401. doi: 10.1164/rccm.201903-0615OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang Q, Sundar IK, Li D, Lucas JH, Muthumalage T, McDonough SR, et al. E-cigarette-induced pulmonary inflammation and dysregulated repair are mediated by nAChR α7 receptor: role of nAChR α7 in SARS-CoV-2 COVID-19 ACE2 receptor regulation. Respir Res . 2020;21:154. doi: 10.1186/s12931-020-01396-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Naidu V, Zeki AA, Sharma P. Sex differences in the induction of angiotensin converting enzyme 2 (ACE-2) in mouse lungs after e-cigarette vapor exposure and its relevance to COVID-19. J Investig Med . 2021;69:954–961. doi: 10.1136/jim-2020-001768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Masso-Silva JA, Moshensky A, Shin J, Olay J, Nilaad S, Advani I, et al. Chronic E-cigarette aerosol inhalation alters the immune state of the lungs and increases ACE2 expression, raising concern for altered response and susceptibility to SARS-CoV-2. Front Physiol . 2021;12:649604. doi: 10.3389/fphys.2021.649604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. McAlinden KD, Lu W, Ferdowsi PV, Myers S, Markos J, Larby J, et al. Electronic cigarette aerosol is cytotoxic and increases ACE2 expression on human airway epithelial cells: implications for SARS-CoV-2 (COVID-19) J Clin Med . 2021;10:1028. doi: 10.3390/jcm10051028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghosh A, Coakley RD, Wrennall JA, Sheltzer JM, Alexis NE, Tarran R.2021.
- 10.Ghosh A, Ahmad S, Coakley RD, Sassano MF, Alexis NE, Tarran R.Lipid-laden macrophages are not unique to patients with e-cigarette or vaping product use-associated lung injury Am J Respir Crit Care Med 20212031030–1033.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ghosh A, Coakley RC, Mascenik T, Rowell TR, Davis ES, Rogers K, et al. Chronic e-cigarette exposure alters the human bronchial epithelial proteome. Am J Respir Crit Care Med . 2018;198:67–76. doi: 10.1164/rccm.201710-2033OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fulcher ML, Gabriel S, Burns KA, Yankaskas JR, Randell SH. Well-differentiated human airway epithelial cell cultures. Methods Mol Med . 2005;107:183–206. doi: 10.1385/1-59259-861-7:183. [DOI] [PubMed] [Google Scholar]
- 13. Ghosh A, Abdelwahab SH, Reeber SL, Reidel B, Marklew AJ, Garrison AJ, et al. Little cigars are more toxic than cigarettes and uniquely change the airway gene and protein expression. Sci Rep . 2017;7:46239. doi: 10.1038/srep46239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Smith JC, Sausville EL, Girish V, Yuan ML, Vasudevan A, John KM, et al. Cigarette smoke exposure and inflammatory signaling increase the expression of the SARS-CoV-2 receptor ACE2 in the respiratory tract. Dev Cell . 2020;53:514–529, e3. doi: 10.1016/j.devcel.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Changeux JP, Amoura Z, Rey FA, Miyara M. A nicotinic hypothesis for COVID-19 with preventive and therapeutic implications. C R Biol . 2020;343:33–39. doi: 10.5802/crbiol.8. [DOI] [PubMed] [Google Scholar]
- 16. Li G, He X, Zhang L, Ran Q, Wang J, Xiong A, et al. Assessing ACE2 expression patterns in lung tissues in the pathogenesis of COVID-19. J Autoimmun . 2020;112:102463. doi: 10.1016/j.jaut.2020.102463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jiang C, Chen Q, Xie M. Smoking increases the risk of infectious diseases: a narrative review. Tob Induc Dis . 2020;18:60. doi: 10.18332/tid/123845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Swärd P, Edsfeldt A, Reepalu A, Jehpsson L, Rosengren BE, Karlsson MK. Age and sex differences in soluble ACE2 may give insights for COVID-19. Crit Care . 2020;24:221. doi: 10.1186/s13054-020-02942-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Clunes LA, Bridges A, Alexis N, Tarran R. In vivo versus in vitro airway surface liquid nicotine levels following cigarette smoke exposure. J Anal Toxicol . 2008;32:201–207. doi: 10.1093/jat/32.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zhou Y, Frey TK, Yang JJ. Viral calciomics: interplays between Ca2+ and virus. Cell Calcium . 2009;46:1–17. doi: 10.1016/j.ceca.2009.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


