Abstract
Background:
Successful rehabilitation is essential to improve the physical and mental outcomes of people with lower limb amputation(s). Individuals have different goals and expectations of successful rehabilitation and experience issues that affect their quality of life.
Objectives:
To determine factors affecting lower limb prosthetic rehabilitation from people with amputation(s), important for studies focusing on prosthetic and socket design and fitting because they provide context of need and user issues.
Study design:
Thematic analysis of semistructured interviews.
Methods:
Ten people with amputation(s) were self-selected from a survey identifying factors affecting lower limb prosthetic rehabilitation. The telephone interviews were semistructured exploring the biggest impactors on and frustrations with rehabilitation and the socket. A thematic analysis was completed by following the undermentioned steps: familiarization, coding, generating themes, reviewing themes, defining and naming themes, and reporting.
Results:
Five distinct but interrelated themes were identified: External to Prosthesis, Body Impactors, Consequences of Ill-Fit, Prosthesis Irritants, and Work and Social Impact. Those living with amputation(s) mentioned prosthetic-related issues affecting their work and social life, including difficulties wearing their prosthesis all day, the socket's rigidity, and the ability to participate in hobbies.
Conclusions:
The study provides new insights into the issues experienced during prosthetic rehabilitation, highlighting impacts beyond just physical health consequences. The study provides an evidence base for areas of the rehabilitation journey which could be improved to improve the quality of life of people with amputation(s).
Keywords: amputation, rehabilitation, prostheses, lower limb amputation
Background
Individuals with amputation(s) are the key stakeholders in lower limb prosthetic rehabilitation. It is not unexpected that people have different definitions of successful rehabilitation: a young military veteran who has lost limbs through trauma may view success as running and playing sport, whereas older individuals may be happy if they can live independently.
Once amputation surgery is completed, in the National Health Service (NHS) setting, the patient is discharged from the surgical team to the rehabilitation team. A multidisciplinary team meeting is sometimes called for different parties to discuss patients' care, but mainly care depends on the local limb fitting service. Prosthesis users are dependent on rehabilitation success to function on their prostheses.
Several studies have assessed satisfaction and issues related to the prostheses and quality of life, including long-term outcomes. One study showed that the number of inpatient rehabilitation nights correlated with functioning in their physical roles, increased vitality, and reduced bodily pain.1 Studies agreed that a focus on socket issues was critical, including sweat, heat, comfort, and fit.1-4
People with lower limb loss reported a lower quality of life and more difficulty integrating into society than the general population.5,6 Those with transfemoral or traumatic causes for amputation typically have lower functional levels and reduced satisfaction in their societal roles.6 Furthermore, poor rehabilitation affects health outcomes, physically and mentally.7 In the elderly persons, higher physical activity is associated with a higher quality of life, although older age and higher amputation levels decreased quality of life.8,9
Aspects of rehabilitation causing problems for individuals with amputations have been explored, noting clear trends. In 2000, four themes were identified in the study conducted by Pezzin et al10: fit of the socket with the residual limb, aspects of the prosthesis' mechanical functioning, other prosthesis qualities, and adaptation and support. The results overlap with those identified in the study conducted by Van der Linde et al,11 which identified service demand, prosthetic prescription, living with a prosthesis, and prosthetic aftercare as themes.
Much of the published literature evaluating the issues experienced by and the long-term outcomes of prosthesis users is based on questionnaire data. Although this method gives an overview of the issues faced, the interpretation of participant answers is limited, and the participant's words and experiences are often lost. No studies to date explicitly asked about rehabilitation experiences. This study intends to address this gap by analyzing these perspectives to determine common themes among different experiences.
Method
A bespoke survey (with an optional follow-up telephone interview), approved by Joint Research and Compliance Office at Imperial College London (ICREC Reference: 18IC4485), was developed, which sought to explore factors affecting rehabilitation, which are not documented by standard outcome tools. Engagement with prosthesis users was sought; however, because none were available at the time of development, the survey was piloted with relevant physiotherapists. The survey aimed to assess the perceived impact socket fit has on rehabilitation, starting with a free text question about rehabilitation frustrations to gather uninfluenced perspectives before asking specifically about sockets.
The following interviews aimed to identify the reasons underpinning the survey answers (Appendix). Semistructured telephone interviews were chosen because individual perspectives were sought to understand individual experiences while minimizing travel, facilitating greater participation.
Participant recruitment
A subset of participants of an online survey was recruited to participate in telephone interviews. Participants of the survey were able to provide their contact details to participate in the interviews and were subsequently contacted by the research team. The survey link was distributed through social media and emailed to personal contacts in relevant clinical teams, charities, and professional organizations to recruit relevant physiotherapists, prosthetists, and prosthesis users, although this study reports only prosthesis user responses.
Inclusion criteria for prosthesis user participants were that they must be 18 years or older, be currently not taking medication that affected their cognitive function, have a good understanding of written and spoken English, and currently use a prosthesis. Relationships between participants were not monitored. All survey participants who provided contact details and arranged an interview were included in the study; recruitment was limited by the number of interested participants. Identifying details were removed before analysis to maintain anonymity.
Consent and data collection
The survey was deployed online using Qualtrics (Utah), a web-based survey tool, and paper. Consent was collected after presentation of the Participant Information Sheet with a checkbox before commencing the survey. The interviews were recorded using a smartphone application. Data were collected between May 2018 and January 2019.
The interviews were semistructured, an approach used within multidisciplinary clinical environments for studies to explore individual perspectives involving different participant groups.12 This approach gives participants the freedom to talk with minimal interference while allowing relevant information to be collected. An open question to understand the reasoning behind each of the main three survey questions was asked: although being the same general question, each referred to participant’s specific responses. Closed follow-up questions were asked for clarification or to direct participants toward the details sought. Interviews were recorded before being transcribed and anonymized for analysis.
Data analysis
Survey responses were analyzed using descriptive statistics in Python to determine the perceived impact of socket fit for different demographics, outlined in Turner and McGregor.13 A thematic analysis was conducted on interview responses to capture the breadth of information. In this study, only prosthesis user participant responses have been included. The following steps were taken: familiarization, coding, generating themes, reviewing themes, defining and naming themes, and reporting.14 Professional transcription of the interview recordings was completed, followed by coding by hand on printed transcripts and tabulation of key information. All transcriptions were anonymized before analysis.
Results
The responses from 10 participants with lower limb amputations were analyzed to identify themes. Participant demographics were varied regarding etiology, age, and time since amputation, with most of them being female participants (Table 1).
Table 1.
Participant demographics, n = 10.
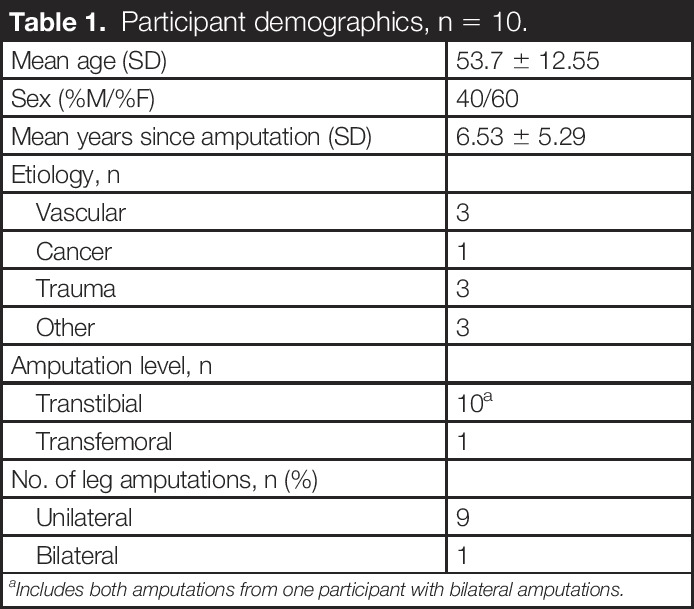
| Mean age (SD) | 53.7 ± 12.55 |
| Sex (%M/%F) | 40/60 |
| Mean years since amputation (SD) | 6.53 ± 5.29 |
| Etiology, n | |
| Vascular | 3 |
| Cancer | 1 |
| Trauma | 3 |
| Other | 3 |
| Amputation level, n | |
| Transtibial | 10a |
| Transfemoral | 1 |
| No. of leg amputations, n (%) | |
| Unilateral | 9 |
| Bilateral | 1 |
Includes both amputations from one participant with bilateral amputations.
Five interrelated themes were identified (Figure 1): External to Prosthesis, Body Impactors, Consequences of Ill-Fit, Prosthesis Irritants, and Work and Social Impact. The Work and Social Impact theme is believed to be a consequence of the other four themes. Quotations are accompanied by participant number and sex, so each is identifiable to a different participant. It was deemed appropriate for data to be sex disaggregated to demonstrate the range of participants, particularly because female individuals tend to be underrepresented in studies.
Figure 1.
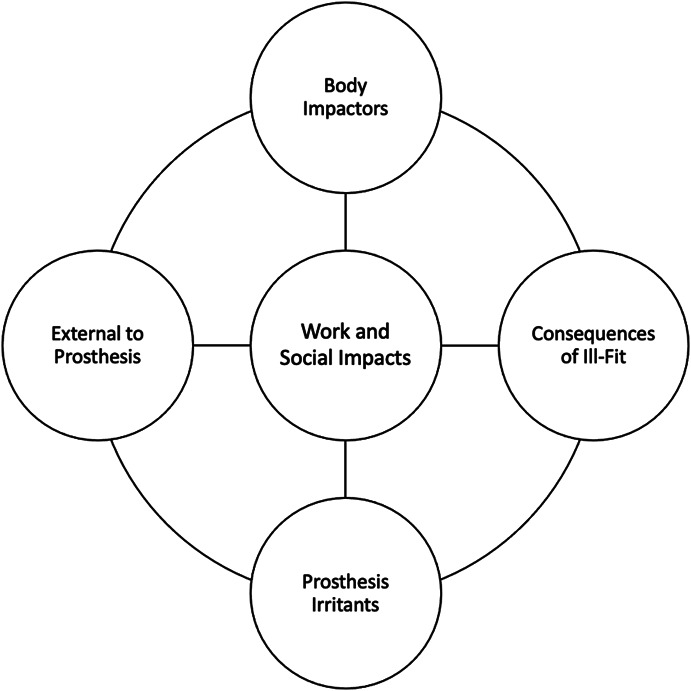
Themes identified in interviews.
External to prosthesis
Interviewees noted that the disparity in service provisions across centers affected their rehabilitation. The differences include sockets and other prosthetic componentry, time shared by clinicians and patients, functional outcomes, and waiting times.
“It's nice to actually have a timeframe which is reasonable and not too long…I had to wait probably longer than I expected. I wanted it quicker.” (Prosthesis User 3, Male individual)
Regarding the function of those going through rehabilitation, it was believed that those who received inpatient care for their rehabilitation achieved higher functionality in less time.
“I went straight from the ward after 2 weeks there, and I had three weeks of intensive therapy. I could have had up to eight weeks, but actually I was walking unaided.” (Prosthesis User 1, Female individual)
The difference was noted between components; the time to fit and manufacture and the quality. Those treated on the NHS explained that it seemed one had to be a military veteran, an athlete, or seen privately to get higher quality limbs and to receive activity or more advanced limbs, they had to be “demanded.” The burden of buying these was left to the individual for those not sponsored or provided by the NHS.
“Your average [people] do not count like military heroes or Paralympians. We do not get the same treatment at all, and the actual range of quality of the prosthetic legs is not as good.” (Prosthesis User 4, Female individual)
However, provision of activity limbs did not seem consistent across the NHS. Some participants noted they were not prescribed activity limbs. Furthermore, they also noted the service was inadequate when transferred to new centers.
“I don't think that the protocol…was particularly good for a transition. They didn't have a written down process to go through.” (Prosthesis User 3, Male individual)
Body impactors
Changes to residual limb volume and shape are common and particularly large in the year after amputation. Changes are noticeable with weather and activity, even during one physiotherapy session. A once well-fitting socket may become loose, allowing for limb movement in the socket causing residual limb damage. The socket may become so tight; the prosthesis cannot be worn because of pain or skin conditions.
“If it is going to swell, you can feel like a burning sensation on your stump, and it just gets worse, and worse, and worse, until…they tell us to take it off.” (Prosthesis User 2, Male individual)
These changes mean a test socket may fit, but due to turnaround times of socket manufacture, it may not fit once produced. Individuals may use an ill-fitting socket for some time if their residual limb is regularly changing while its characteristics stabilize.
“After they take a cast and you've got to wait a wee bit before they can actually take you in for a fitting by the time that comes the leg is either far too big or far too small. They’ve got to start doing adjustments straight away.” (Prosthesis User 9, Female individual)
Sockets are typically made of nonbreathable materials, with individuals wearing socks or liners to aid comfort and fit. Socket fit issues due to residual limb changes are compounded by sweat. Temperature issues are exacerbated by activity and weather, affecting the amount of residual limb movement inside the socket, causing skin breakdown, infection, or the prosthesis to slip off. It can be challenging to deal with sweat rising over the socket's top staining clothes or forming puddles in the socket.
“[Sweat] actually comes over the top of the liner…it's obviously quite uncomfortable and it can wet shorts and wet trousers because the sweat is actually coming over the top of the liner.” (Prosthesis User 6, Male)
Once the residual limb's shape and size have stabilized, it may not be ideal for wearing a prosthesis. There can be excess skin, soft tissue, or bony prominences at the residual limb's distal end, making prosthesis use painful.
“It feels like where they've gone so tight around my knee, and so close to the bottom of the stump it feels there's no comfort there, so I've got constant pain because I'm on my bone all the time.” (Prosthesis User 5, Female individual)
“Where the surgery actually took place, there's actually a skin fold and that sometimes gives me issues with pain, being sore and things.” (Prosthesis User 6, Male individual)
Adherent scars and skin grafts are common for some etiology, with internal tissue fused to skeletal structures, which become stiff and immobile. These can lead to significant pain in the residual limb and contribute to skin breakdown, resulting in not using a prosthesis.
“I would say the skin graft was a bigger [issue]…when the leg has shrunk…that actually broke down quite badly and blistered up, which caused me some issues to wearing the leg.” (Prosthesis User 6, Male individual)
Little can be done to control the length of the body’s healing process, which varies for injury type and individual. Although clinicians can facilitate healing, unhealed wounds significantly disrupt rehabilitation. With open wounds, wearing the prosthesis is discouraged, and although some exercises are possible, using the prosthesis is most beneficial physically and mentally for these individuals.
Mentality is critical, with some becoming demotivated when they feel they are not progressing as hoped. Individuals must adjust to a significant change in their lives and manage their expectations of what is achievable.
“It was depressing because I thought it was going to be a major change to my life, and it took some time to accept that…the mental aspect of an amputation is perhaps a bit understated.” (Prosthesis User 10, Male individual)
Consequences of ill-fit
Owing to socket rigidity, achieving an ideal shape can be challenging. The socket does not mold with the person and can cause pain and discomfort in everyday activities, preventing prosthesis use.
“It’s because of the top of the leg, the prosthetic is such hard, unforgiving plastic that when you sit on it, it digs into the back of my leg.” (Prosthesis User 7, Female individual)
Ill-fitting sockets compound issues of residual limb health, facilitating skin breakdown and pressure sore development. An ill-fitting socket can put excess pressure on load-intolerant anatomy, which can cause enough pain and discomfort to stop prosthesis use.
“[An] Ill-fitting socket causes you to not walk correctly in your prosthesis. It causes you to have skin problems, breakdowns, friction burns, pain, which also affects your confidence in using this piece of kit.” (Prosthesis User 8, Female individual)
“If it doesn't fit properly then…your leg hurts…it aches…It presses on the muscles or the bones of the residual limb. Possibly the skin gets inflamed and sore. You get blisters. It just hurts.” (Prosthesis User 10, Male individual)
Continued prosthesis use, despite pain or skin conditions, can have adverse effects across the body. Individuals tend to compensate for pain and discomfort by changing their weight distribution or movement. The change affects the body’s biomechanics, leading to musculoskeletal overuse injuries, affecting rehabilitation, function, and long-term health.
“You either can't fit into it, or you're squeezing yourself into it, and then that causes problems with the condition of your skin which is in contact with the socket. That then causes you to walk in a way which is not correct, which again causes you to fall.” (Prosthesis User 8, Female individual)
Prosthesis irritants
The socket's rigidity does not adapt to the body’s short-term or long-term changes, leading to pain and ill-fit due to residual limb volume and shape fluctuation.
“They'd give me an absolutely perfect test socket…but when I got the socket for the pin-lock, it was much bigger than the test socket.” (Prosthesis User 4, Female individual)
“Most sockets are designed to be one size, and they don't take into account the fact that that the human body is constantly adapting and changing and responding to its environment.” (Prosthesis User 8, Female individual)
Not only was the socket’s fixed shape an issue but also its weight. It was believed that the prosthetic leg was already heavy because of its metal componentry and batteries. On the NHS, typically, sockets are plastic or other heavier materials; given the availability of lighter material, for example, carbon fiber, excess socket weight was seen as resolvable. The limb's weight affects gait and can influence whether individuals use their prostheses, particularly when they are adjusting to long periods of prostheses use.
“It is harder to walk with it than, obviously, it is your own leg because it's heavier…I see people with carbon fibre tops and all that…you can see why because the weight would be half.” (Prosthesis User 7, Female individual)
The issues with the socket were critical and, in most instances, fixable. However, there was a view that the socket was not as exciting to develop and so did not receive development focus.
“I think a lot of effort is put into the ankles and the legs…but I think actually the socket fit is something that’s really important but of course not as glamorous and therefore gets forgotten.” (Prosthesis User 1, Female individual)
Prosthetic liners also caused issues; users found they increased the temperature of the residual limb, making them hot and sweaty. Temperature issues are exacerbated when liners are paired with socks, frequently used when the residual limb shrinks, to facilitate continued prosthesis use without extensive residual limb movement.
Silicon liners, used to aid suction suspension, have caused allergic reactions. Sometimes, this reaction settles after a couple of weeks, but it can take longer, preventing prosthesis use.
“I’ve got quite a good liner now, but unfortunately it's much thicker, but it's an anti-allergenic one, and I still react to it when I get a new one.” (Prosthesis User 1, Female individual)
Users had issues with prescribed components that were too basic for daily living and hobbies. Basic components predicted to last a year broke in several months, and more advanced prescriptions were also limited, stopping individuals from completing desired activities.
“My first leg…that they said should do me for the first year, and I kept breaking it within 3 months.” (Prosthesis User 1, Female individual)
Work and social impact
The impacts of issues vary and affect different aspects of prosthesis users' lives, both mental and physical. It can be challenging for prosthesis users to work when unable to wear their prosthesis. The need to remove their limb because of fatigue or pain or to make regular adjustments can affect employment. When residual limb health is compromised, and the prosthesis cannot be worn, many must take time off work. Time for appointments and associated travel also take individuals away from work.
Prosthesis use, particularly early in rehabilitation, can affect individuals' social lives. Fatigue is common, which is exacerbated by ill-fitting sockets causing pain or discomfort. It becomes necessary for individuals to rest or sit down, where they may have previously been able to stand.
“After church, when we're hanging around chatting, I will hang around, but I will sit down, and people have to come to me to chat because if I stay stood for too long, I get very bad backache.” (Prosthesis User 4, Female individual)
The basic componentry prescribed during rehabilitation affects hobby participation. The prescriptions did not allow for those with higher goals to achieve them. Hobbies have been excluded from individuals' lives because of prosthetic limitations, whether component prescriptions or socket fit.
“I used to walk quite a bit, so I can't do that no more. I find I can't go to the gym because I can’t do what I should be doing in the gym because it’s like my leg hurts more.” (Prosthesis User 5, Female individual)
Independence can be compromised during rehabilitation because of the need to adapt to using prostheses in different environments and managing associated issues. Traveling can be challenging, given uneven surfaces and differences in disability provision.
“Access to public transport has been pretty much denied to me…as a result of the amputation.” (Prosthesis User 4, Female individual)
“If you have a serious fall somewhere really far away from home and it's just you by yourself, and there's no way for you to almost easily recover from that, that fall could make you stay as close to home as possible, at least close to support or as close to support as possible.” (Prosthesis User 8, Female individual)
Managing associated problems of prosthesis use can be challenging and inhibit participation in family life. Removing the prosthesis in public can be difficult because of the associated stigma of disability. Some do not feel comfortable traveling or going out for prolonged periods because of difficulties managing residual limb heat and pain, leading to unpleasant odor or sweat stains.
“You can't be sat in the middle of somewhere taking your leg off and wiping it all and everything. It's bad enough people looking at you because you've got the leg let alone taking it off.” (Prosthesis User 5, Female individual)
“Doing a job, if it hurts, you don't want to do the job, or you don't want to go out, or you don’t want to go on holiday because of all the hassle that might entail.” (Prosthesis User 10, Male individual)
Discussion
This analysis aimed to portray firsthand experiences of individuals with amputation(s) through lower limb prosthetic rehabilitation, documenting major frustrations and impacts. Unlike previous studies, this study has not explicitly focused on long-term outcomes or specific experiences with prostheses but has included affecting factors of processes and life during rehabilitation. The main advantage of analyzing the interview transcripts is that respondents have explained their reasoning in their own words, talking about their experiences and impactful issues.
Five themes were identified in this study: External to Prosthesis, Body Impactors, Consequences of Ill-Fit, Prosthesis Irritants, and Work and Social Impact. Although distinct, the themes are interrelated, focusing on the frustration causes and the impacts. Analyzing the personal experiences of people with amputations(s) highlights the far-reaching consequences of individual issues on quality of life, affecting not only physical health but also mental health and lifestyle (including relationships and socializing, work and holiday, and hobbies). This finding is not unique to this study and is not restricted to only rehabilitation. It has been previously noted that there are varying psychological consequences related to amputation.15
The themes identified in this study align with previous research that noted fit of the socket, aspects of the prosthesis' mechanical functioning, other qualities of the prosthesis, adaptation and support, and prosthetic aftercare to be important.2,11 These themes are also identified in the 2018 NHS study of prosthesis users and their carers, which highlighted many of the specific concerns mentioned by interview participants.16 One of the most common complaints in the NHS report was relating to “socket fit,” with specific mention of the lengthy process of socket fitting, with long wait times and multiple trips to hospital required. Interviewee responses in this study highlight this issue in different ways: one participant acknowledges that limb is constantly changing and the wait times for fitting mean that adjustments must be made immediately to the socket. Another noted that there was a size change of the socket between testing and fitting but did not acknowledge the body’s influence on this. This discrepancy highlights the lack of consistent knowledge transfer and understanding of prosthesis users, another point highlighted in the NHS report.
This analysis, however, takes a broader look at issues throughout rehabilitation, including issues related to care provision and early adoption of the prosthesis, which are not present after rehabilitation. The External to Prosthesis theme seems to be unique in this study, perhaps due to the openness of the questions asked.
Prosthesis users were clear about the impacts on rehabilitation due to disparity in services. Although there are little published data on this, the “postcode lottery” of services is outlined on a leading charity website.17 Noted issues from our study include the disparity across NHS centers and the difference in NHS, private, and military settings—all issues found in the NHS report.16 There is a perception among NHS patients that a “better” service is available for private patients and veterans. However, some participants were happy with their prescriptions and provision of care received. Without considering all the influencing variables on rehabilitation, including expectations, socioeconomic impacts and levels of injuries and medical conditions, it is difficult to conclude whether the service is “better” in the private and military settings. When comparing care provision, it may be more pertinent to assess factors such as the number of nights in inpatient rehabilitation, particularly because a previous study for those with trauma-related amputations found a correlation with high functional outcomes, irrespective of the funding body.10 This was hinted at in this study, with one participant stating how successful their inpatient rehabilitation was for them. However, given this was mentioned only once, it is difficult to evaluate other factors that may have influenced their fast rehabilitation.
Prosthesis issues are not all solved by changes to service provision. For instance, liners are required to suspend the prostheses and maintain control during activity. There are known hygiene issues (e.g. heat, sweat) associated with the nature of the materials used.18 The clinical setting also does not change that most clinicians must react to the different issues as they arise. Because individuals' bodies are unique, it is difficult to prevent all issues proactively. Clinicians must balance patient comfort, requirements for adequate limb control, and potential benefit of referring a patient for prosthetic changes. The latter consideration is more efficient in some settings, particularly when prosthetist and physiotherapist work together, as implied by the call for joint working between involved clinicians for continuity of care and prompt problem-solving.16
Given the NHS is publicly funded, the prostheses available are limited compared with privately funded settings. The discrepancies in availability are likely due to the expense of components and materials; for instance, carbon fiber used for sockets costs more. The NHS ensures patients can recover and function in everyday life. Therefore, the cost burden lies with the service user for advanced equipment, such as running blades, or is “reserved” for those who can make a case for it, as found in this study and supported by the NHS report.16
Consequences of Ill-Fit and Body Impactors are themes identified in this study with extensive literature backing. The themes are heavily related because body changes can influence socket fit, causing further injury, taking time to heal. Multiple studies have shown that residual limb breakdown and pain are commonly reported in prosthesis users,1,3,5,10 another aspect shown to affect rehabilitation in this study.
Another aspect of this study shown in others is the impact of prosthetic rehabilitation on individuals' work and social lives. Although specific examples may differ, individuals believe their daily lives have been impaired; critically, the ability to function and get satisfaction from what they do. Studies have shown that individuals with amputation(s) experience a lower quality of life than their fully limbed counterparts, relating to their ability to conduct tasks, social interaction, and psychological well-being,5,6,19 on top of the psychological impact of the amputation itself as highlighted in this study and past literature.7,19 Although, the evaluation that function is most important is not supported in all studies,9 the issue remains pertinent.
Unsurprisingly, issues in the Consequences of Ill-Fit, Body Impactors, and Work and Social Impact themes have been reported over the years because the physiological reaction to amputation has not changed over time. Volume fluctuation of the limb and sensitivity to loading the soft tissue continue, leading to the same issues being reported repeatedly for a significant period with no solutions forthcoming.20-22 Although there have been changes to prosthetic sockets' material and suspension mechanisms, they are primarily the same in the sense of a rigid, unbreathable case around the residual limb. Contributing to difficulties solving issues is the nonstandard approach to amputation surgery. Surgical technique varies, with different methods preferred across geography and teaching methods, and with less experienced surgeons, there is a higher complication risk.23 Techniques influence how and where bone is cut and shaped, and how the wound is closed, affecting socket fit. This nonstandard approach makes it difficult to have a standard response to socket issues. Issues relating to other body parts too (e.g. musculoskeletal overuse injuries), as a consequence of prosthesis use, particularly when ill-fitting have been reported, again supporting the reports of pain and the need for solution in this study.24,25
Work and Social Impact is the theme that relates to all others, emphasizing the wide-reaching consequences of the other issues reported. Not only is the limited progress to improve accessibility to transport and flexible work options an area of development but also the other issues throughout the themes reported by prosthesis users in this study. The implications of allowing issues to go unsolved, whether with the prosthetic socket, physical health, or mental health are not limited to rehabilitation. The consequent impacts on other issues, for example, work and Hobbies, have a long-term impact on the quality of life of prosthesis users.19
Limitations
Participant recruitment for the telephone interviews was from a survey conducted asking about rehabilitation issues, but with a focus on socket fit. Participants may have been predisposed to talking about this topic because of the influence of the survey. However, all interviews were analyzed entirely separately of the survey results, and all themes were based solely on the responses.
The small sample size (n = 10) and only two reviewers evaluating the themes may mean the results are not representative of the overall population. Although a small number, the study is a preliminary insight into the issues faced during prosthetic rehabilitation and serves as a basis for further research.
Conclusion
The thematic analysis gives an insight into the firsthand perspectives of individuals with amputation(s) and relevant clinicians involved in lower limb prosthetic rehabilitation. Six distinct but interrelated themes have been identified about frustrations that affect rehabilitation: External to Prosthesis, Body Impactors, Consequences of Ill-Fit, Prosthesis Irritants, Limitations of Practice, and Work and Social Impact. This study provides a basis for further research to address frustrations, limit their impact, and improve quality of life.
Funding
The authors disclosed that they received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interest
The authors disclosed no potential conflicts of interest with respect to the research, authorship, and or publication of this article.
Supplemental material
No supplemental digital content is available in this article.
Acknowledgments
This work was conducted under the auspices of the Royal British Legion Centre for Blast Injury Studies at Imperial College London. The authors acknowledge the financial support of the Royal British Legion. No grant number is given.
Appendix. Interview Questions for Participants With Amputations
-
In your questionnaire you mentioned that you believed ________ had the biggest impact on your function. Please could you describe what you mean in more detail?
Could you explain why this is a problem for you?
How do you think it limits what you want to do?
In your survey you said ______ was your biggest frustration with your rehabilitation. Please could you explain what you mean in more detail?
-
In your survey you said that ______ was your biggest frustration with your socket. If a new technology was developed to be able to solve this problem would you be willing to try it?
If no, please could you explain why?
If yes, what would stop you wanting to adopt the new technology into your everyday routine?
Footnotes
Associate Editor: Daniel Norvell
Contributor Information
Athina Belsi, Email: a.belsi@imperial.ac.uk.
Alison H. McGregor, Email: a.mcgregor@imperial.ac.uk.
References
- 1.Pezzin LE, Dillingham TR, MacKenzie EJ, et al. Use and satisfaction with prosthetic limb devices and related services. Arch Phys Med Rehabil 2004; 85: 723–729. [DOI] [PubMed] [Google Scholar]
- 2.Legro MW, Reiber GD, Smith DG, et al. Issues of importance reported by persons with lower limb amputations and prostheses. J Rehabil Res Dev 1999; 36: 155–163. [PubMed] [Google Scholar]
- 3.Hagberg K and Branemark R. Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems. Prosthet Orthot Int 2001; 25: 186–194. [DOI] [PubMed] [Google Scholar]
- 4.Mohd Hawari N, Jawaid M, Md Tahir P, et al. Case study: survey of patient satisfaction with prosthesis quality and design among below-knee prosthetic leg socket users. Disabil Rehabil Assist Technol 2017; 12: 868–874. [DOI] [PubMed] [Google Scholar]
- 5.Demet K, Martinet N, Guillemin F, et al. Health related quality of life and related factors in 539 persons with amputation of upper and lower limb. Disabil Rehabil 2003; 25: 480–486. [DOI] [PubMed] [Google Scholar]
- 6.Amtmann D, Morgan SJ, Kim J, et al. Health-related profiles of people with lower limb loss. Arch Phys Med Rehabil 2015; 96: 1474–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horgan O and MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disabil Rehabil 2004; 26: 837–850. [DOI] [PubMed] [Google Scholar]
- 8.Deans SA McFadyen AK and Rowe PJ. Physical activity and quality of life: a study of a lower-limb amputee population. Prosthet Orthot Int 2008; 32: 186–200. [DOI] [PubMed] [Google Scholar]
- 9.Fortington LV, Dijkstra PU, Bosmans JC, et al. Change in health-related quality of life in the first 18 months after lower limb amputation: a prospective, longitudinal study. J Rehabil Med 2013; 45: 587–594. [DOI] [PubMed] [Google Scholar]
- 10.Pezzin LE Dillingham TR and MacKenzie EJ. Rehabilitation and the long-term outcomes of persons with trauma-related amputations. Arch Phys Med Rehabil 2000; 81: 292–300. [DOI] [PubMed] [Google Scholar]
- 11.Van der Linde H, Hofstad CJ, Geertzen JH, et al. From satisfaction to expectation: the patient’s perspective in lower limb prosthetic care. Disabil Rehabil 2007; 29: 1049–1055. [DOI] [PubMed] [Google Scholar]
- 12.Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol 2013; 13: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turner S and McGregor AH. Perceived impact of socket fit on major lower limb prosthetic rehabilitation: a clinician and amputee perspective. Arch Rehabil Res Clin Transl 2020; 2: 100059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Braun V and Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 15.Roșca AC, Baciu CC, Burtăverde V, et al. Psychological consequences in patients with amputation of a limb. An interpretative-phenomenological analysis. Front Psychol 2021; 12: 537493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.NHS England. Specialised Commissioning: Prosthetics Patient Survey Report. National Health Service; 2018. [Google Scholar]
- 17.Diabetes UK. Amputation Postcode Lottery Getting Worse. Diabetes UK; 2018. https://www.diabetes.org.uk/About_us/News/Amputation-postcode-lottery-getting-worse. [Google Scholar]
- 18.Hachisuka K, Nakamura T, Ohmine S, et al. Hygiene problems of residual limb and silicone liners in transtibial amputees wearing the total surface bearing socket. Arch Phys Med Rehabil 2001; 82: 1286–1290. [DOI] [PubMed] [Google Scholar]
- 19.MacKay C, Cimino SR, Guilcher SJT, et al. A qualitative study exploring individuals' experiences living with dysvascular lower limb amputation. Disabil Rehabil 2020. doi: 10.1080/09638288.2020.1803999. [DOI] [PubMed] [Google Scholar]
- 20.Naylor PFD. Experimental friction blisters. Br J Dermatol 1955; 67: 327–342. [DOI] [PubMed] [Google Scholar]
- 21.Levy SW. Skin problems of the leg amputee. Prosthet Orthot Int 1980; 4: 37–44. [DOI] [PubMed] [Google Scholar]
- 22.Meulenbelt HEJ, Dijkstra PU, Jonkman MF, et al. Skin problems in lower limb amputees: a systematic review. Disabil Rehabil 2006; 28: 603–608. [DOI] [PubMed] [Google Scholar]
- 23.De Souza BA Brown I and Shibu MM. Surgical experience and supervision may influence the quality of lower limb amputation. Ann R Coll Surg Engl 2004; 86: 237–238. [PMC free article] [PubMed] [Google Scholar]
- 24.Gailey R, Allen K, Castles J, et al. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev 2008; 45: 15–29. [DOI] [PubMed] [Google Scholar]
- 25.Farrokhi S, Mazzone B, Eskridge S, et al. Incidence of overuse musculoskeletal injuries in military service members with traumatic lower limb amputation. Arch Phys Med Rehabil 2018; 99: 348-354 e1. [DOI] [PubMed] [Google Scholar]


