Abstract
The auriculo-condylar syndrome is caused by abnormalities of the first and second pharyngeal arches during embryonic development. Its inheritance follows the autosomal dominant pattern. Both familial and individual cases are reported in the literature. The syndrome is characterized by wide phenotypic variation, with affected individuals expressing clinical signs of variable severity due to variable expressivity of the responsible genes. Clinical signs of the syndrome include auricular malformation, hypoplasia of the mandibular condyles, anomalies of the temporomandibular joints, malocclusion, and, in more severe cases, cleft palate, glossoptosis, facial asymmetry, and respiratory problems. The aim of this article is to report a case of a female patient with signs of the auriculo-condylar syndrome and to present the pedigree of her family. Clinical findings, diagnosis, treatment plan, and final treatment are analyzed.
Keywords: Auriculo-condylar syndrome, Orthodontic treatment, Facial asymmetry, Distraction osteogenesis
INTRODUCTION
Question mark ear is a distinct auricular malformation first described by Cosman et al.1 in 1970. This anomaly is caused by a cleft or constriction of the lower auricle just between the lobule and the helix. This divides the ear in two and gives it the peculiar appearance of a question mark.1,2 Question mark ear can be an isolated finding, or it may appear in association with a series of anomalies called auriculo-condylar syndrome (ACS).
Uuspaa3 first reported a familial case of ACS in a mother and two sons presenting hypoplasia of the mandible and bilateral external ear malformations. In 1978, Jampol et al.4 first described this anomaly as an entity, reporting five-generation occurrence of ACS in a family, with affected subjects presenting prominent, malformed ears with a characteristic constriction at the junction between the lower and middle thirds of the pinna, giving the appearance of question mark ear.
ACS is a syndrome caused by abnormalities that occur during embryonic development of the first and second pharyngeal arches; it follows the autosomal dominant pattern of inheritance. Wide phenotypic variation is seen in both individual and familial cases of ACS; this may be attributed to varying degrees of gene expression, leading to a range in the severity of clinical signs.4–6
The typical clinical appearance of the syndrome includes prominent and constricted ears, stenosis of the ear canals, hypoplastic condyles of the mandible, temporomandibular joint abnormalities, microstomia, malocclusion, puffy cheeks, and a round face.4,6–8 However, because of high clinical variability, other signs can be present, including a simple external auricular malformation,9 cleft palate, hypoplastic tongue, glossoptosis, hypotonia, facial asymmetry, respiratory distress, and apnea.5,10,11 Vincent et al.12 in 1961 and Divizia et al.13 in 2002 reported cases with ear malformations associated with urogenital abnormalities. Additionally, Nezarati and Aftimos14 reported on a patient with microtia, micrognathia, and absence of ossicles in the middle ear.
This case report details a female patient with ACS who presented severe mandibular micrognathia. The family pedigree was compiled and was subsequently compared with similar cases identified from the literature. Patient approval was received for use of the records in this study.
CASE REPORT
A female patient (GK) with facial asymmetry and mandibular micrognathia, aged 11 years 8 months, presented to the graduate orthodontic clinic at the University of Athens. GK was conceived when her mother was 20 years old and her father was 32 years old. No history of trauma or exposure to any known teratogens such as radiation, smoke, or alcohol consumption or intake of any medications by the mother was reported throughout the patient's gestation period. GK had a normal delivery; she weighed 3.920 kg and was 50 cm in length. Her physical and mental development was uneventful, and she had no speech and learning difficulties.
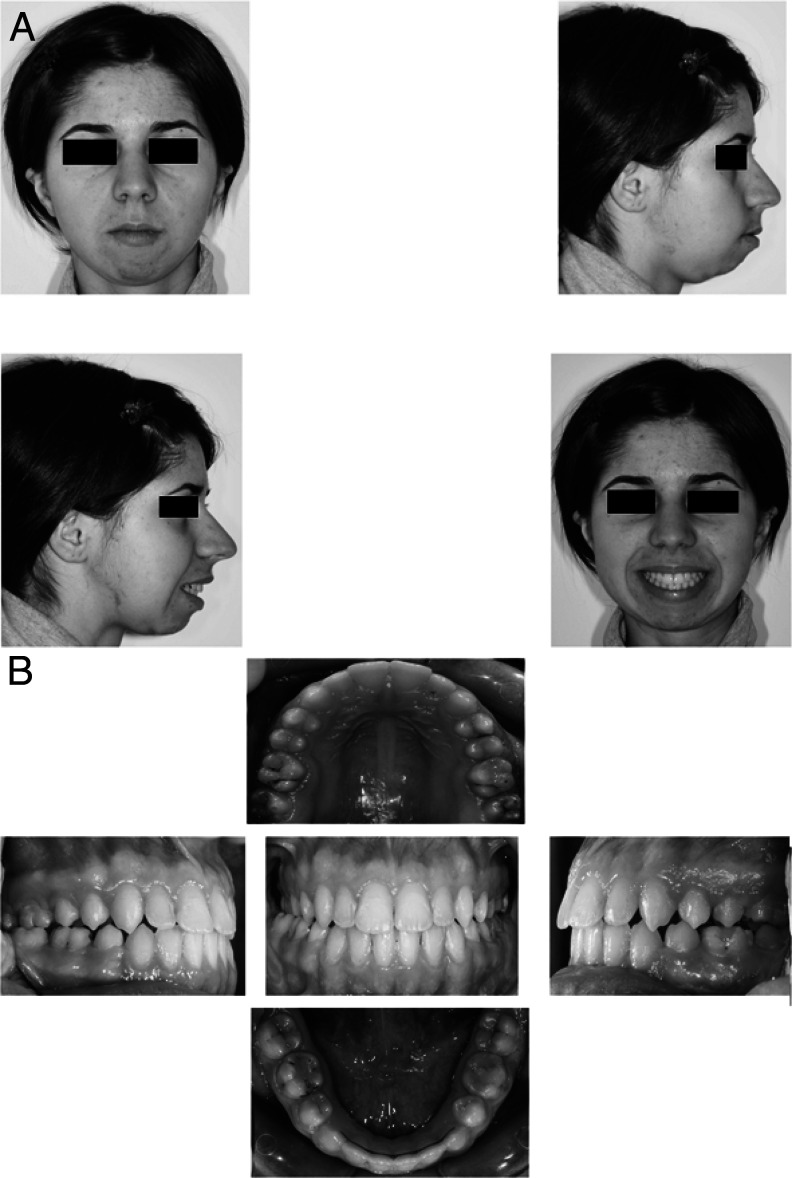
The patient was hospitalized for meningitis at the age of 8. She had a history of orthodontic treatment with fixed appliances from ages 8 to 11. These were removed approximately 6 months before the patient was admitted to our clinic. It was not possible to obtain orthodontic records of this treatment. At the time of examination, her height was 1.52 m and she weighed 41 kg. Her face was round, and severe mandibular hypoplasia was more pronounced on the right side along the lower border of the mandible, thus causing facial asymmetry. The lower facial height was short, with incompetent lips and auricular asymmetry. The pinna of the left auricle was located at a lower position than the pinna of the right auricle (Figure 1).
Figure 1.

Frontal and profile photographs on presentation.
Profile analysis showed marked convexity of her face with a steep mandibular plane angle and lip incompetence. The upper and lower lips were prominent in relation to the esthetic plane (Figure 1).
Functional analysis revealed asymmetry of the smile with a contraction toward the right side. Upon swallowing, intense contraction of the mentalis muscle was identified. Temporomandibular joint (TMJ) findings included clicking sounds on the left and restricted mandibular range of motion with a maximum interincisal opening of 30 mm (Figure 2).
Figure 2.
Asymmetric smile, mentalis muscle strain, and restricted maximum interincisal opening.
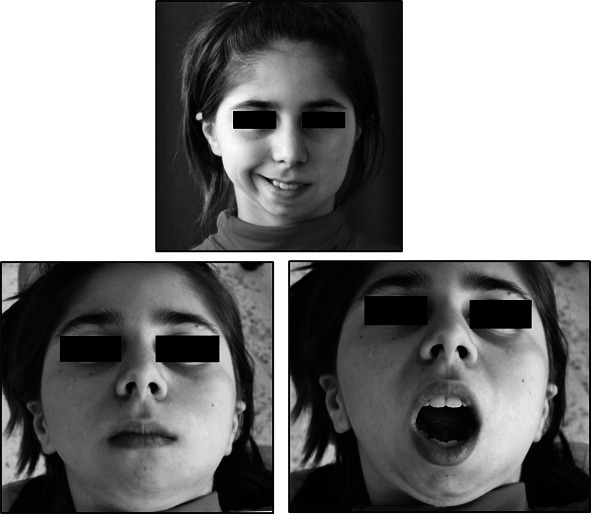
Clinical examination of the auricles revealed pitted and dilated ear lobes, as well as folding and hypertrophy of the upper part of the helices. The left external auditory canal was set in a more anterior position than the right one (Figure 3). The patient was referred to an ear, nose, and throat (ENT) surgeon, and findings regarding morphology and function of the middle and inner ears were normal.
Figure 3.

“Question mark” ears bilaterally.
On clinical examination of the patient's hands, we observed camptodactyly with a medial inclination of the middle and distal phalanges of the fourth and fifth digits (Figure 4). Intraoral examination revealed a mixed dentition, moderate oral hygiene, caries, hypoplastic enamel areas, and previous restorations. The patient presented with a Class III molar relation, crowding of anterior mandibular teeth, anterior open bite, minimal overjet (0.5 mm), a left-side posterior cross-bite, and over-erupted maxillary and mandibular incisors. A 3 mm deviation of the lower dental midline to the left was observed (Figure 5).
Figure 4.
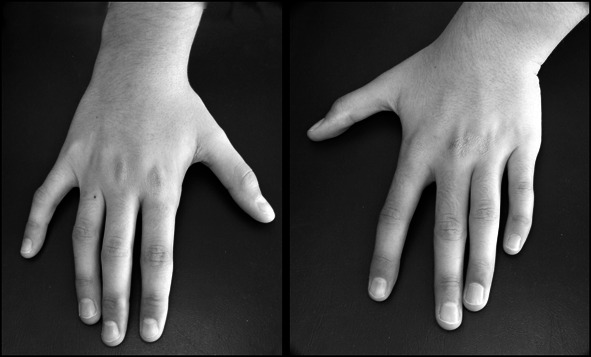
Camptodactyly involving the fourth and fifth digits.
Figure 5.
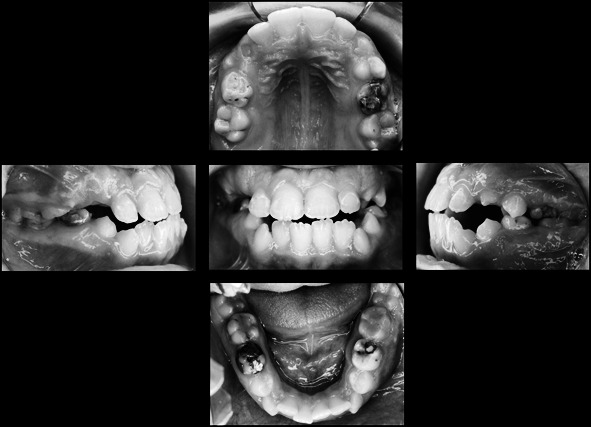
Clinical intraoral photographs on presentation.
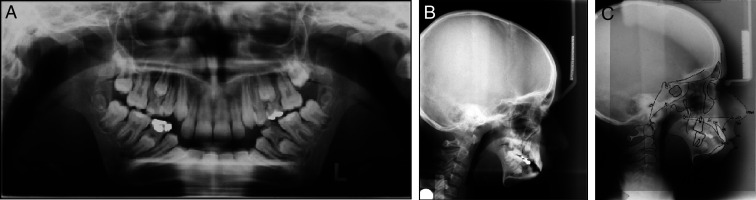
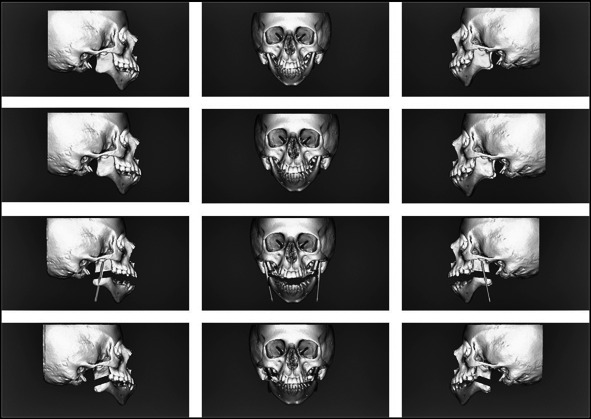
Lateral cephalometric analysis presented severe mandibular retrognathia, mandibular micrognathia, hyperdivergence of the facial skeletal planes, short lower facial height, labial tipping of maxillary and mandibular incisors, and protrusion of the upper and lower lips. Other significant findings included bilateral excessive antegonial notching, bilaterally reduced ramus vertical height, and bilateral hypoplastic condyles. The condyles were displaced anteriorly and appeared to articulate outside the glenoid fossae, classifying the patient as a bilateral Kaban type IIb skeletal deformity15 (Figures 6A,B,C and 18D).
Figure 6.
(A) Panoramic radiograph on presentation. (B) Lateral cephalometric radiograph on presentation. (C) Tracing of the lateral cephalometric radiograph on presentation.
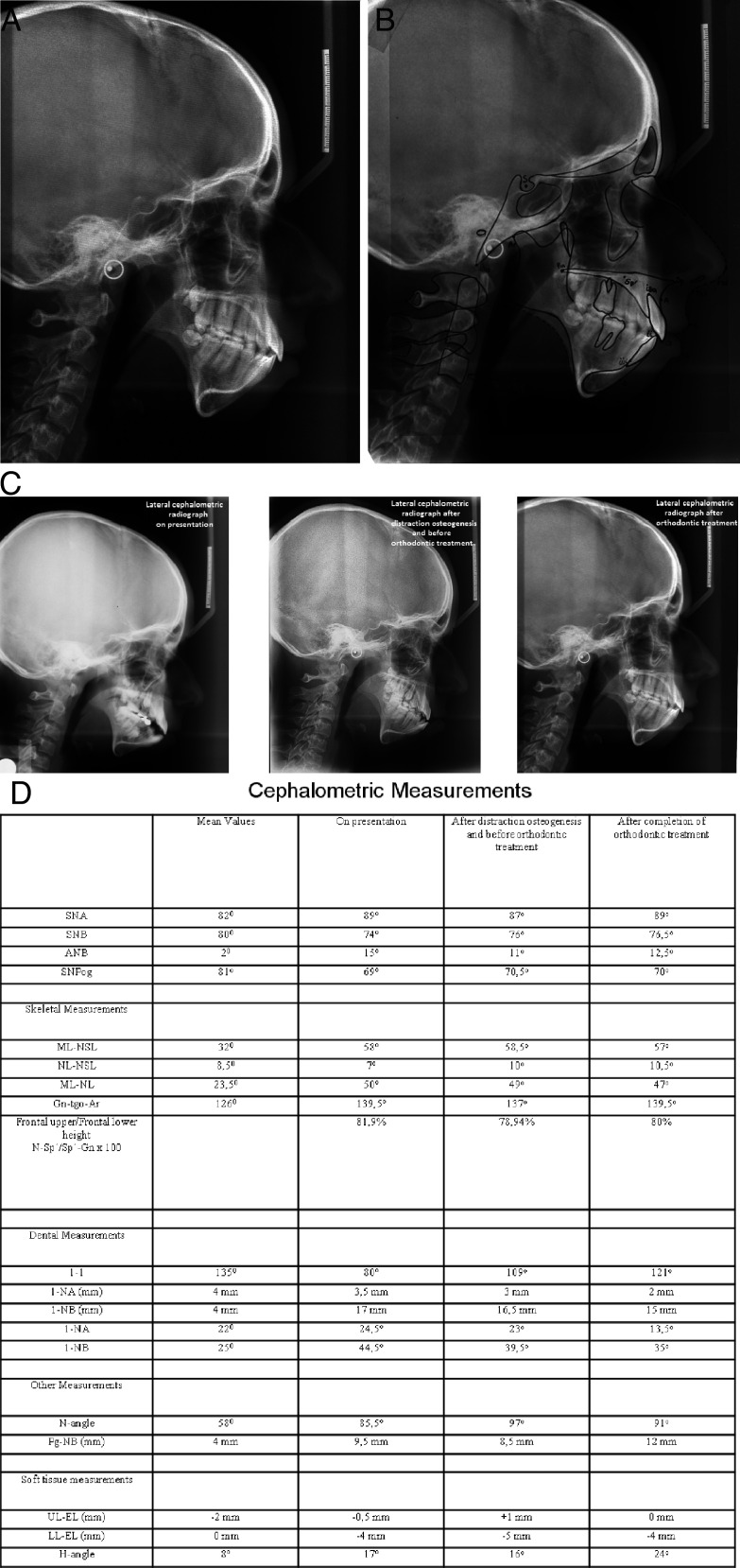
Figure 18.
(A) Lateral cephalometric radiograph after removal of fixed orthodontic appliances. (B) Tracing of the lateral cephalometric radiograph after removal of fixed orthodontic appliances. (C) Lateral cephalometric radiographs on presentation, after distraction osteogenesis and before orthodontic treatment and after completion of orthodontic treatment. (D) Cephalometric measurements on presentation, after distraction osteogenesis and before orthodontic treatment and after completion of orthodontic treatment.
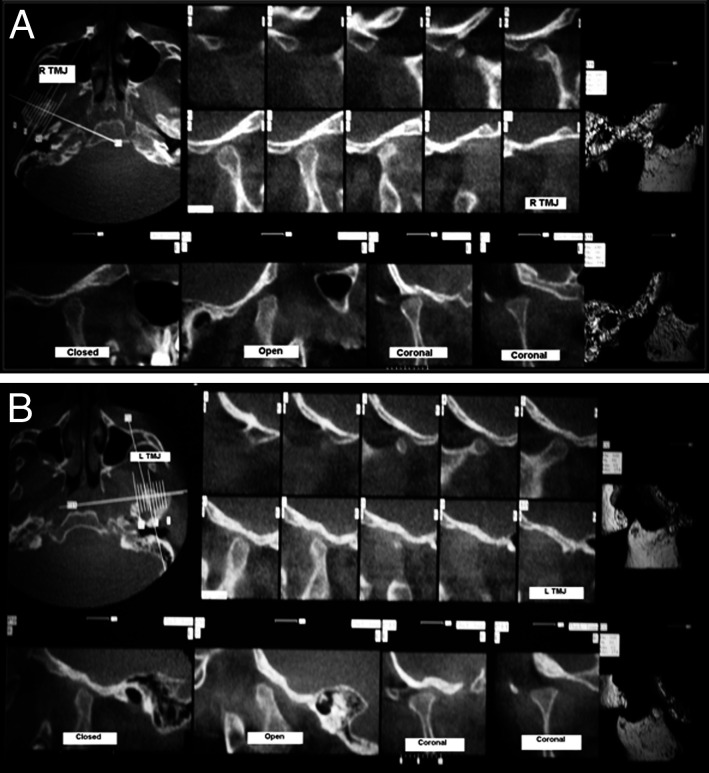
The patient's features were further studied by three-dimensional computed tomography (CT) scan of the temporomandibular joints, which confirmed anterior and medial displacement of the hypoplastic condylar heads (Figures 7A,B).
Figure 7.
(A) Computed tomography (CT) imaging of the right (R) temporomandibular joint (TMJ) on presentation. On the three-dimensional (3D) reconstructed image, note that the hypoplastic condyle is articulating anterior to the articular eminence. (B) CT imaging of the left (L) TMJ on presentation.
The patient's principal problem to be addressed in treatment planning was the abnormal pattern of her facial growth and development. The convexity of her face evidenced the deficiency and retrognathism of the mandible intensified by the hyperdivergent skeletal planes. Hypoplasia of the condyles and the short rami of the mandible were the main causes of retrognathism because they caused clockwise development and rotation of the mandible.
Family History
The reviewed family history led to construction of the pedigree shown in Figure 8. All affected subjects were blood-related, descending from the paternal family, and the same syndromic phenotype was inherited for at least three generations. Signs of the syndrome reportedly affected the patient's father, sister, and paternal grandfather, as well as a paternal uncle, a paternal aunt, and her son.
Figure 8.
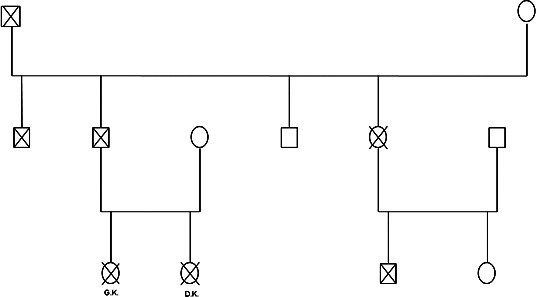
The pedigree of the patient's family.
The patient's sister, DK, aged 9 years was also examined. She presented similarities in the pattern of craniofacial development with her sister. Clinical examination revealed convex facial type, lip separation at rest, steep mandibular plane angle, protrusion of the lips, and clicking sounds originating from both temporomandibular joints during mastication. She also had camptodactyly, but no abnormalities were found on examination of the ears. The patient had a Class III molar relationship and minimal overjet, along with tooth rotations and tipping.
Panoramic radiography revealed short rami of the mandible and flattening of the articular eminences. Analysis of the lateral cephalometric radiograph revealed that the patient also had mandibular retrognathia (Figure 9). Three-dimensional TMJ CT scan revealed flattening of the condylar heads and flattening of the glenoid fossae.
Figure 9.
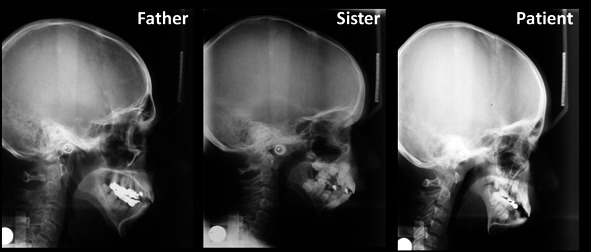
Lateral cephalometric radiographs of the patient, her father, and her sister.
Treatment
Surgery
Before orthodontic treatment was initiated, the patient underwent bilateral vertical mandibular ramus lengthening using distraction osteogenesis. An intraoral approach was utilized for the bilateral placement of buried distractors (Zürich pediatric ramus distractors, KLS Martin, Umkirch, Germany) (Figure 10). The activation rods of the distractors exited through small stab incisions in the submandibular areas.
Figure 10.
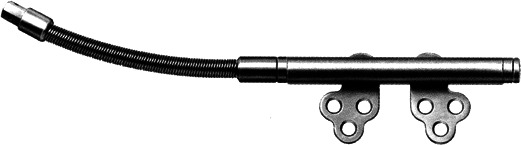
The ramus distractor (KLS Martin, Umkirch, Germany).
Before the distraction osteogenesis appliance was placed, a maxillofacial computed tomography (CT) scan was obtained. CT data were processed in a computer utilizing appropriate maxillofacial surgical planning software (Materialise, Leuven, Belgium), and a stereolithographic model of the patient's skull and mandible was fabricated (Figure 11). On three-dimensional (3D) reconstructed images, the horizontal ramus osteotomies at the level of the mandibular foramina were drawn. Additionally, the distraction vectors were selected in a way that the mandibular rami would lengthen purely vertically, thereby minimizing as much as possible any tendency for horizontal mandibular distraction that would accentuate the Class III anterior and posterior dental relationships and ideally minimizing the anterior open bite (Figure 12). Additional stereolithographic models for each of the patient's rami were fabricated, along with surgical guides for accurate angulation of the osteotomy, as well as for accurate placement of the osteosynthesis screw holes (Figure 13).
Figure 11.
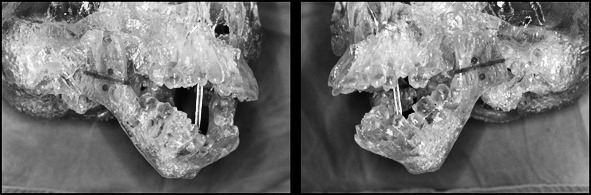
Stereolithographic models of the case. Note the planned ramus osteotomy (red line) and the proposed distraction vector (red dots) for vertical distraction.
Figure 12.
Images depicting digital simulation of the distraction utilizing special software (Materialise, Leuven, Belgium).
Figure 13.
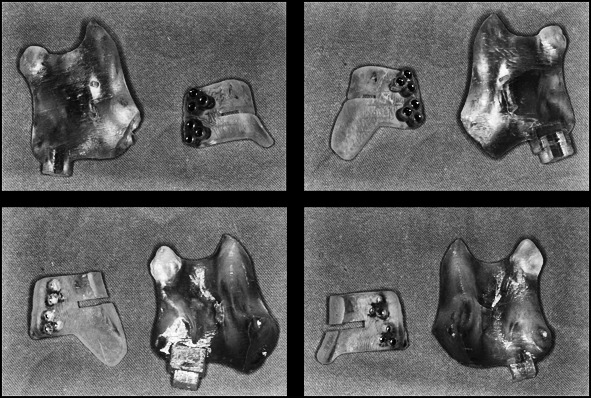
Surgical guides for accurate angulation of the osteotomy and precise placement of the distraction hardware.
Under general anesthesia via nasotracheal intubation, the patient underwent bilateral horizontal osteotomies of the mandibular rami, as described by Rachmiel et al.,16 and fixation of ramus distractors, as prescribed by the previously mentioned surgical guides. After a latency period of 1 week, bilateral vertical ramus distraction was initiated at a rate of 0.5 mm (one full turn of the distractor activation rod) twice daily. After the endpoint of the active distraction phase was reached (15 mm of vertical ramus lengthening bilaterally) (Figure 14), a 2.5-month consolidation period was allowed before removal of the distractor appliances and scar revision of the activation rod exit wounds, again under general anesthesia. A manageable with fixed orthodontics anterior dental relationship was maintained, without lateral mandibular midline shifting or significant anterior open bite.
Figure 14.

Postdistraction panoramic radiograph of the case.
Orthodontics
Problem list, diagnosis, and treatment plan
Following completion of the mandibular ramus distraction osteogenesis, the patient presented a bilateral Class III canine and molar relation, 1 mm negative overjet, 0 mm overbite, and bilateral crossbite of several posterior teeth, while the maxillary and mandibular midlines coincided at the midsagittal plane. The lower dental arch had 9 mm of crowding (Figures 15A,B).
Figure 15.
(A) Frontal and profile photographs after distraction osteogenesis and before orthodontic treatment. (B) Clinical intraoral photographs after distraction osteogenesis and before orthodontic treatment.
Although on clinical and cephalometric examination a Class III dental and skeletal relationship was readily identified, the ANB measurement was 11 degrees, which indicated a Class II relationship with regard to the anterior cranial base. The clinically apparent Class III pattern was attributed to forward growth and repositioning of the mandible as a result of the applied distraction osteogenesis, and the cephalometrically identified Class II pattern was attributed to the still present hyperdivergent underlying skeletal facial type and the vertically growing facial pattern of the patient (Figure 16A,B,D).
Figure 16.
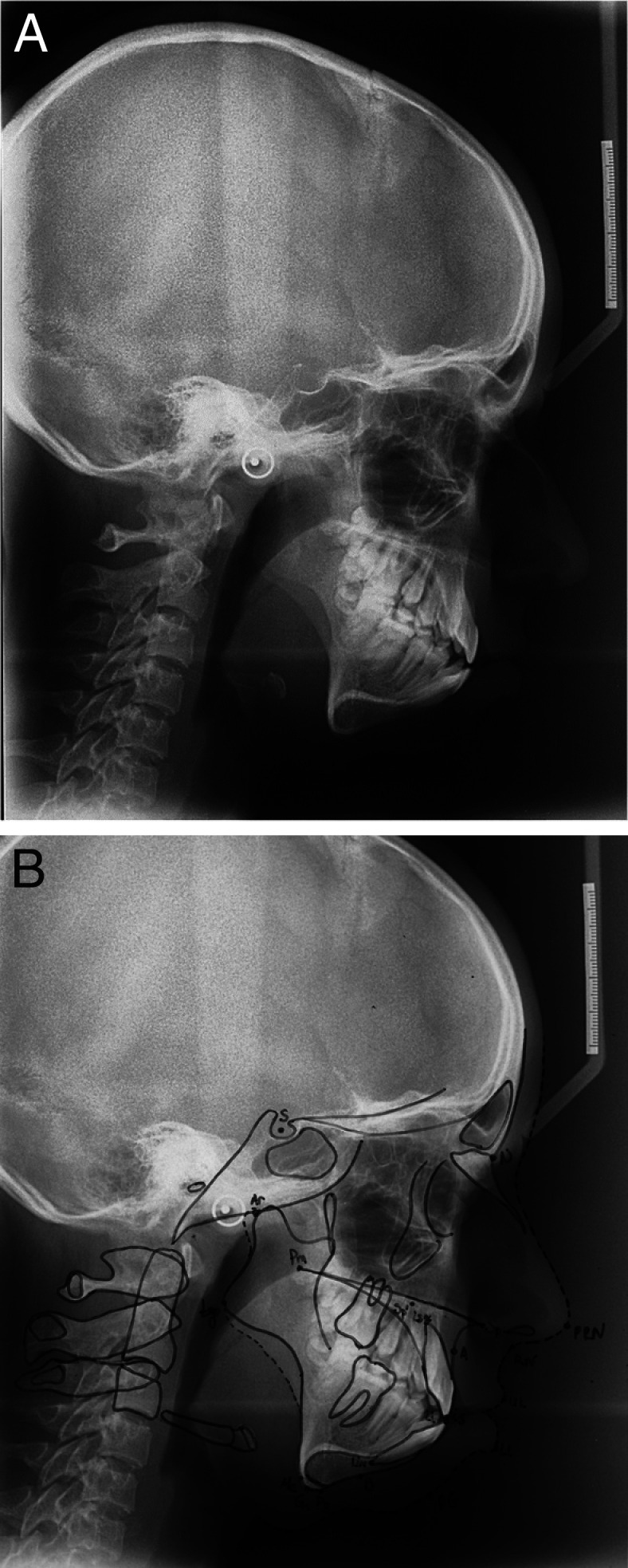
(A) Lateral cephalometric radiograph after distraction osteogenesis and before orthodontic treatment. (B) Tracing of the lateral cephalometric radiograph after distraction osteogenesis and before orthodontic treatment.
The orthodontic treatment plan for the patient included maxillary expansion to correct the posterior dental crossbite and extraction of the mandibular first premolars to provide the necessary space for retraction of the anterior mandibular teeth, thus facilitating correction of the negative dental overjet and overbite and relief of the crowding of the lower dental arch. The patient was informed about all aspects of the described treatment, thereby accepting that this option would adequately address the dental malocclusion but would not significantly improve her facial appearance. Upon completion of facial growth at the age of approximately 16 to 17 years, an advancement genioplasty would still be required to improve the esthetic appearance of the lower facial third, possibly augmented with bilateral gonial implant placement. The patient and her parents agreed to the presented plan.
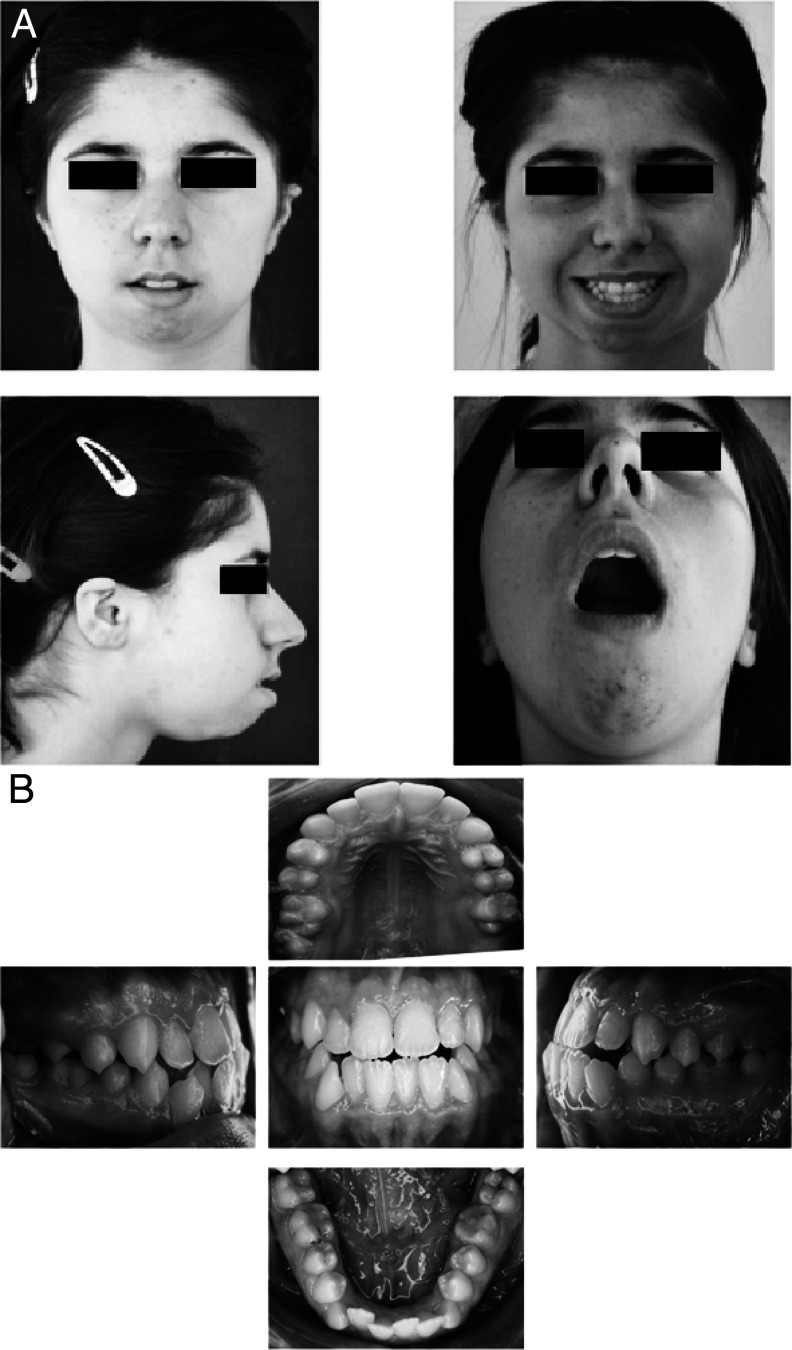
Orthodontic treatment
Orthodontic treatment was initiated by placing a bonded rapid maxillary expander (RME). The patient was instructed to activate the screw once a day for 35 days. Six months later, after expansion of the upper arch had been completed, the RME was removed and fixed appliances were bonded on all maxillary teeth. Following this, both mandibular first premolars were extracted, thus allowing for retraction of the lower canines to the extraction spaces. After a Class I canine relationship was established, fixed appliances were bonded to the lower incisors to relieve anterior crowding. Overbite correction was primarily achieved by surgically induced autorotation of the mandible, in addition to orthodontic uprighting and lingual inclination of the mandibular incisors. The relative contribution of the palatal inclination of the maxillary incisors was very limited. Once coordination of the dental arches was established, the right posterior segment displayed a degree of relapse to a crossbite relationship. The final molar relationship was a full unit Class III. Nevertheless, the overall orthodontic result was acceptable with Class I canine relationship, good intercuspation of the dental arches, and establishment of a normal overjet and overbite (Figures 17A,B). Treatment with fixed orthodontic appliances lasted a total of 2 years.
Figure 17.
(A) Frontal and profile photographs after completion of orthodontic treatment. (B) Clinical intraoral photographs after completion of orthodontic treatment.
On clinical examination, although clicking sounds on elevation and depression of the mandible remained, marked improvement of the mandibular range of movement was observed with a maximal opening capacity of 40 mm. This was attributed to improved functional balancing between mandibular sides and favorable repositioning of the mandibular condyles in their respective glenoid fossae following the surgical intervention.
Orthodontic retention included application of a 3 to 3 SS twist flex fixed retention for the mandibular teeth and a Hawley-type removable appliance for the maxillary dental arch.
The lateral cephalometric radiograph of the patient taken just after removal of the fixed orthodontic appliances, its tracing together with the corresponding cephalometric analysis, and the comparison of it versus cephalographs taken before surgery and pictures of the initial phase of orthodontic treatment are shown in Figures 18A, 18B, 18C, and 18D.
One year after completion of treatment, no clinical signs of skeletal or dental relapse were evident.
DISCUSSION
Auriculo-condylar syndrome (ACS) is a rare syndrome with an autosomal dominant pattern of inheritance. Very few reports describe this syndrome in the literature, and all focus on diagnosis.3,4,7,8,10–14 Only one paper refers to the cause of the syndrome based on genetic diagnostic procedures. According to this paper, a disease locus for a family with ACS has been mapped to 1p21.1–23.3.
Our patient presented all features of the syndrome, except hearing loss. Plain radiographs and CT scans revealed bilateral abnormalities of the ramus–condyle complex. Distraction osteogenesis was chosen as the surgical procedure of choice to increase the vertical height of the mandibular rami and to establish a more acceptable condyle-to-fossa articulation. An alternative surgical option to ramus distraction osteogenesis would consist of reconstruction of the ramus–condyle complexes with bilateral costochondral grafts. This option would be chosen if the ramus–condyle deformity was even greater, as would be the case in a Kaban type III deformity. Furthermore, TMJ reconstruction with costochondral grafts carries with it far greater postoperative morbidity than intraoral distraction osteogenesis and does not stretch the soft tissue envelope (distraction histogenesis). For this reason, costochondral grafting is regarded as a potentially less stable procedure than distraction osteogenesis.
A similar treatment is usually selected for patients presenting with hemifacial microsomia.
In an atypical fashion, this patient had a severely retrusive mandible with bilateral poorly developed ramus–condyle complexes and Class III dental relationships in both anterior and posterior parts of her occlusion. For this reason, the choice and implementation of appropriate distraction vectors were considered quite demanding, thus necessitating digital planning, stereolithography, and fabrication of precise surgical guides for execution of the ramus osteotomies and accurate fixation of the distraction hardware. Nevertheless, and because of her dentoskeletal anatomy, the underlying Class III dental relationship deteriorated even further after completion of the mandibular distraction phase. Although the treatment of choice for the underlying skeletal discrepancy would be the application of combined orthodontic treatment and orthognathic surgery, such an option was turned down by the patient and her parents. As a result, we selected the option of camouflaging the skeletal discrepancy through properly planned and carefully applied orthodontic tooth movements.
Extraction of the mandibular first premolars was deemed necessary to provide space for retraction of the anterior mandibular teeth. Following completion of the orthodontic camouflage treatment, the patient still needed an advancement genioplasty and possibly bilateral gonial implant placement to achieve an improved cosmetic result. Interventions of this type can raise stability issues, which would be difficult for us to address because of the distant location of the patient's residence. Besides, the patient and her parents were satisfied by the esthetic result and did not think that further surgery was necessary at this stage. It did remain though as an option to be discussed in the future, if deemed necessary.
REFERENCES
- 1.Cosman B, Bellin H, Crikelair G. F. The question mark ear. Plast Reconstr Surg. 1970;46:454–457. doi: 10.1097/00006534-197011000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Takato T, Takeda H, Kamei M, Uchiyama K. The question mark ear (congenital auricular cleft): a familial case. Ann Plast Surg. 1989;22:69–73. doi: 10.1097/00000637-198901000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Uuspaa V. Combined bilateral external ear deformity and hypoplastic mandible: case report. Scand J Plast Reconstr Surg. 1978;12:165–167. doi: 10.3109/02844317809012989. [DOI] [PubMed] [Google Scholar]
- 4.Jampol M, Repetto G, Keith D. A, Curtin H, Remensynder J, Holmes L. B. New syndrome? Prominent, constricted ears with malformed condyle of the mandible. Am J Med Genet. 1998;75:449–452. doi: 10.1002/(sici)1096-8628(19980217)75:5<449::aid-ajmg1>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 5.Masotti C, Oliveira K. G, Poerner F, et al. Auriculo-condylar syndrome: mapping of a first locus and evidence for genetic heterogeneity. Eur J Hum Genet. 2008;16:145–152. doi: 10.1038/sj.ejhg.5201955. [DOI] [PubMed] [Google Scholar]
- 6.Passos-Bueno M. R, Ornelas C. C, Fanganiello R. D. Syndromes of the first and second pharyngeal arches: a review. Am J Med Genet A. 2009;149A:1853–1859. doi: 10.1002/ajmg.a.32950. [DOI] [PubMed] [Google Scholar]
- 7.Guion-Almeida M. L, Kokitsu-Nakata N. M, Zechi-Ceide R. M, Vendramini S. Auriculo-condylar syndrome: further evidence for a new disorder. Am J Med Genet. 1999;86:130–133. doi: 10.1002/(sici)1096-8628(19990910)86:2<130::aid-ajmg8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 8.Guion-Almeida M. L, Zechi-Ceide R. M, Vendramini S, Kokitsu-Nakata N. M. Auriculo-condylar syndrome: additional patients. Am J Med Genet. 2002;112:209–214. doi: 10.1002/ajmg.10631. [DOI] [PubMed] [Google Scholar]
- 9.Shkalim V, Eliaz N, Linder N, Merlob P, Basel-Vanagaite L. Autosomal dominant isolated question mark ear. Am J Med Genet A. 2008;146A:2280–2283. doi: 10.1002/ajmg.a.32452. [DOI] [PubMed] [Google Scholar]
- 10.Priolo M, Lerone M, Rosaia L, Calcagno E. P, Sadeghi A. K, Ghezzi F, Ravazzolo R, Silengo M. Question mark ears, temporo-mandibular joint malformation and hypotonia: auriculo-condylar syndrome or a distinct entity? Clin Dysmorphol. 2000;9:277–280. doi: 10.1097/00019605-200009040-00009. [DOI] [PubMed] [Google Scholar]
- 11.Storm A. L, Johnson J. M, Lammer E, Green G. E, Cunniff C. Auriculo-condylar syndrome is associated with highly variable ear and mandibular defects in multiple kindreds. Am J Med Genet A. 2005;138A:141–145. doi: 10.1002/ajmg.a.30883. [DOI] [PubMed] [Google Scholar]
- 12.Vincent R. W, Ryan R. F, Longenecker C. G. Malformation of ear associated with urogenital anomalies. Plast Reconstr Surg Transplant Bull. 1961;28:214–220. doi: 10.1097/00006534-196108000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Divizia M. T, Cordone A, Bado M, Rosaia L, Cirillo Silengo M, Ravazzolo R, Lerone M. Auriculo-condylar syndrome or new syndrome? Clin Dysmorphol. 2002;11:143–144. doi: 10.1097/00019605-200204000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Nezarati M. M, Aftimos S. Microtia, severe micrognathia and absent ossicles: auriculo-condylar syndrome or new entity? Clin Dysmorphol. 2007;16:9–13. doi: 10.1097/MCD.0b013e3280110b57. [DOI] [PubMed] [Google Scholar]
- 15.Kaban L. B, Mulliken J. B, Murray J. E. Three-dimensional approach to analysis and treatment of hemifacial microsomia. Cleft Palate J. 1981;18:90–99. [PubMed] [Google Scholar]
- 16.Rachmiel A, Manor R, Peled M, Laufer D. Intraoral distraction osteogenesis of the mandible in hemifacial microsomia. J Oral Maxillofac Surg. 2001;59:728–733. doi: 10.1053/joms.2001.24280. [DOI] [PubMed] [Google Scholar]