Abstract
Objective:
To evaluate the root resorption after rapid maxillary expansion (RME) via cone-beam computed tomography (CBCT).
Materials and Methods:
Records of 25 patients who had undergone RME with tooth-borne banded expander were obtained from the archive of the orthodontic department. CBCT data were reconstructed with surface and volume rendering, and the volumetric images were manipulated to display the root surfaces from various orientations. On these three-dimensional images, permanent first molars and first and second premolars were segmented, and their roots were isolated. Volumes of roots were calculated. The difference between pre-expansion and postexpansion root volumes was statistically evaluated with a paired-samples t-test. Also, the percentage of root volume loss was calculated for each root and statistically compared with each other with one-way analysis of variance at the P < .05 level.
Results:
The difference between the pre-expansion and postexpansion root volumes was statistically significant for all roots investigated. Maximum volume decrease was observed for the mesiobuccal root of first molar teeth (18.60 mm3). It was determined that the distobuccal root of first molar teeth was less affected from the expansion procedure (9.47 mm3). No statistically significant difference was found for the percentage of root volume loss.
Conclusion:
Following RME treatment, significant root volume loss was observed for all investigated posterior teeth. However, the percentage of volume loss was not statistically different among roots.
Keywords: Root resorption, Rapid maxillary expansion, Cone-beam computed tomography
INTRODUCTION
Rapid maxillary expansion (RME) is a commonly used procedure to solve maxillary constriction. This was first defined by Angell in 1860,1 and it gained popularity in the 1900s with the belief that it could improve nasal breathing and the patient's overall well-being.2 During the RME procedure, Isaacson and Ingram3 reported that one-turn activation of the screw generated as high as 10-kg forces. These heavy forces are transmitted to the maxilla by the anchor teeth, and root resorption was shown in histological sections of anchor premolar teeth, which were extracted after RME.4–9
Langford6 reported that the root resorption was basically on the buccal surface and was expansive rather than axially invasive. Langford and Sims7 showed resorption on the buccal part of the root. Barber and Sims10 reported severe buccal root resorption and also found that the mesial, distal, and apical parts of the roots were affected. Odenrick et al.8 concluded that the most common resorption site was the buccal side, and minor resorption was found apically. Likewise, Erverdi et al.9 reported that most of the resorption takes place on the buccal part of the root, whereas in a few specimens, resorption was also seen on the apical and coronal parts.
Root resorption after orthodontic therapy has been assessed through conventional radiographs,11 light microscope,12 and scanning electron microscope.10 Histologic techniques are reported to be more sensitive and show the actual extent of root resorption.13 Histological evaluation of these teeth included embedding and serial sectioning. With light microscopy, resorption craters were quantified, but this technique was found to be destructive and caused material loss during preparation.14 According to Chan and Darendeliler,15 the quantitative value of histological root resorption evaluation is questionable. Irregular C-shaped craters and/or smaller craters could be partially or totally missed or miscalculated. Another point that should be taken into account is the high variability of root morphology and anatomy of permanent first premolars. This is an important aspect because an absolute cut through the long axis of the tooth is extremely difficult. This also leads to missing apical or midroot craters.15 Scanning electron microscope (SEM) evaluation was suggested to provide resolution and detail that was not achievable via histological models reconstructed from serial sections. However, the curved anatomy of the premolars complicate obtaining a straight-on view, and the actual size of resorption craters may not be accurate.15 SEM evaluation of a resorption crater is performed with piecing two-dimensional (2D) micrographs, and the quantitative value of this technique is supposed to be inadequate.15
Severe root resorption can be detected using conventional radiographs,16–19 but resorption at the mesial and distal portion of the root or mild apical resorption is hardly visible.20 Two-dimensional conventional radiography has severe limitations to visualize root resorption.21,22 In a review by Chan and Darendeliler,15 it was concluded that 2D radiography might be a good diagnostic tool, but quantitative evaluation of root resorption should be avoided.
An alternative method to 2D radiography is the use of cone-beam computed tomography (CBCT). CBCT has particular application in the assessment of postorthodontic root resorption,23 and the images free from distortion and superimposition allow classifying root resorption type. Moreover, CBCT provides high-definition images at a radiation dose similar to that of standard dental films.24
In light of the literature, it may be concluded that RME causes resorption at the buccal aspects of the roots. However, approximal and palatal aspects of the roots as well as buccal surfaces may undergo resorption. Resorption can be assessed for an individual root if a tooth has multiple roots.25 To the best of our knowledge, no study was performed to evaluate root volume changes after RME. Thus, the aim of this study was to quantitatively evaluate the root resorption changes associated with RME therapy by tooth-borne banded expander using CBCT.
MATERIALS AND METHODS
Totally, CBCT records of 25 patients (14 girls and 11 boys; mean age, 12.7 years) who had undergone RME therapy by tooth-borne banded expander as a part of their orthodontic treatment were selected from the archive of the Orthodontic Department of Dicle University. Of these patients, two were in the mixed dentition period.
An ethical approval had already been obtained from the Ethical Committee of the Dicle University (DUDFEK 2009/21) for the aims of another study; the patients were not exposed to extra radiation particularly for this retrospective study. Therefore, another ethical approval was not gained.
The initial CBCT records had been taken immediately before expansion. The expansion appliance was a Hyrax expander, which consisted of an expansion screw, welded on the bands on the first premolar and molar teeth. As a routine clinical procedure, the expansion screw is activated two turns per day, and active expansion is continued until the palatal cusps of the maxillary molars were in contact with the buccal cusps of the first mandibular molars. After active expansion therapy, postexpansion CBCT records were taken.
All tomography had been obtained by using the same device (i-CAT, model 17–19, Imaging Sciences International, Hatfield, PA) at the following settings: exposures were made with 5.0 mA, 120 kV, and exposure time was 9.6 seconds and with a voxel size of 0.3 mm.
DICOM data sets of the patients were imported into Mimics software (Materialise NV, Leuven, Belgium). This program manually segments the tissues according to density values, which are so-called Hounsfield units (HU).
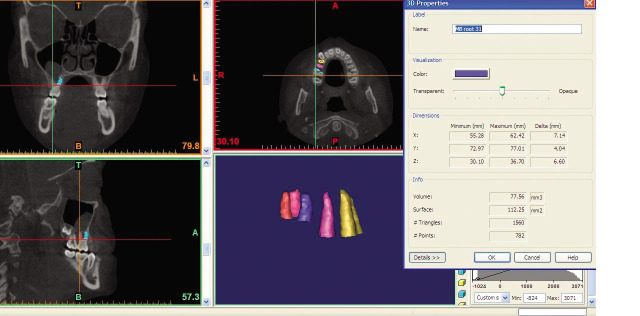
CBCT data were reconstructed with surface and volume rendering, and the volumetric image was manipulated to display the root surfaces from various orientations. Threshold values were set individually with regard to each patient. The same HU were used for the segmentation of each patient's before and after records. On these 3D images, permanent first molars and first and second premolars were segmented cautiously (Figure 1). After segmentation, permanent first molar teeth were separated from other teeth and adjusted for 3D orientations (Figure 2). The mesial and distal cusp tips were oriented parallel to the floor. The mesiobuccal and distobuccal roots were separated according to a plane parallel to the cement-enamel junction and passing through the deepest point of the furcation between these roots (Figures 3 and 4). Each root was isolated and color coded. The volume of each root was calculated by the program (Figure 5). The same measurement protocol was applied to the roots of the first and second premolars without the separation of the roots. Two measurements were calculated: root volume loss and percentage of root volume loss. Root volume loss was the difference between pre-expansion (T0) and postexpansion (T1) root volumes. The percentage of root volume loss was calculated as:
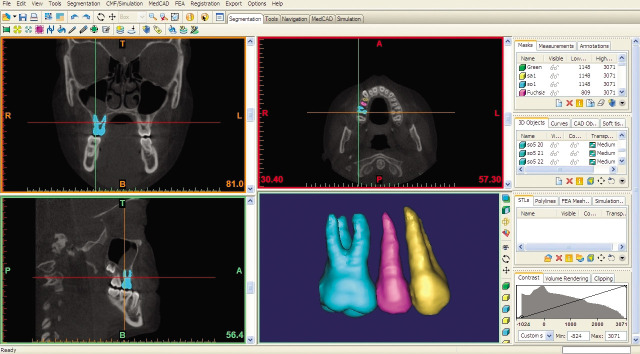
Figure 1.
Segmentation of premolars and first molar teeth.
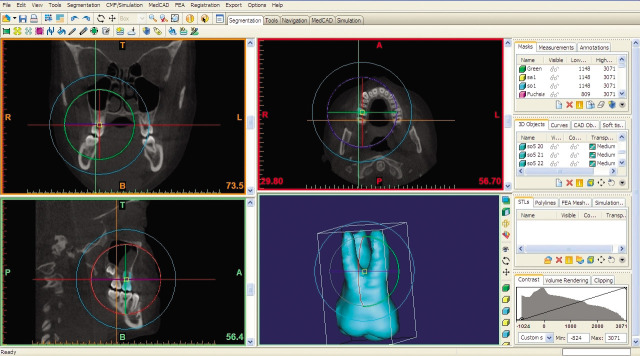
Figure 2.
Adjustment of first molar for 3D orientation.
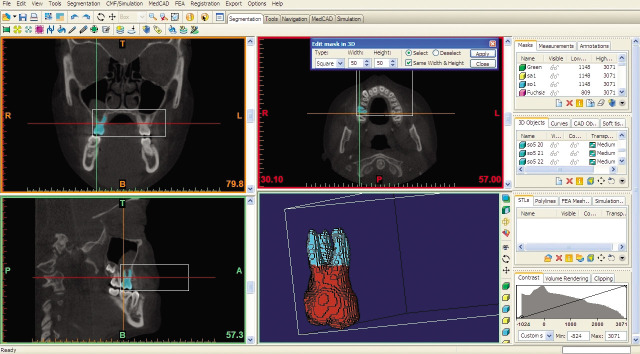
Figure 3.
Construction of the reference plane.
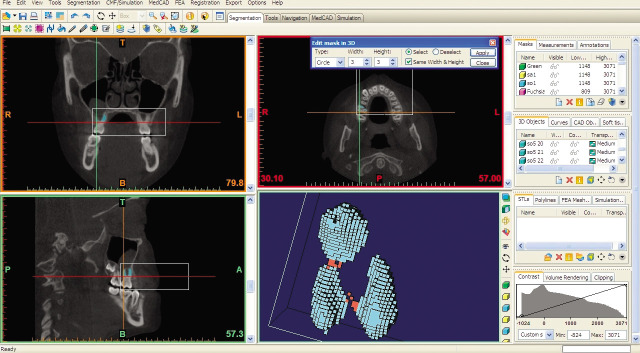
Figure 4.
Isolation of the roots of first molar tooth.
Figure 5.
Automatic calculation of root volume.
Premolar teeth were not evaluated in mixed dentition patients, as the apex is not completed. In addition, one first permanent molar, six first premolars, and two second premolars had been extracted before second CBCT records were taken. In one patient, bilateral fusion of the distobuccal and palatal root of the first permanent molar was observed, and these teeth were also excluded. Volumetric measurements were not performed for these teeth.
Statistical Analysis
All statistical analyses were performed with the Statistical Package for the Social Sciences software (SPSS 15.0, Chicago, IL). The normality test of Shapiro-Wilks and the Levene's variance homogeneity test were applied to the data. The data were found normally distributed, and there was homogeneity of variance among the groups. Thus, the statistical evaluation of pre-expansion and postexpansion root volumes was performed using parametric tests. To test the difference between the left and right sides, an independent samples t-test was performed. No significant difference was found between the left and right sides and the data pooled. The means, standard deviations, and minimum and maximum values were calculated for all roots. The root volume values were tested with a paired-samples t-test.
The percentage of root volume loss was calculated by subtracting the postexpansion root volume from the pre-expansion root volume. Then, the difference was divided by the pre-expansion volume and then multiplied by 100. To test the percentages, one-way analysis of variance was used. The statistical significance level was set at P < .05.
RESULTS
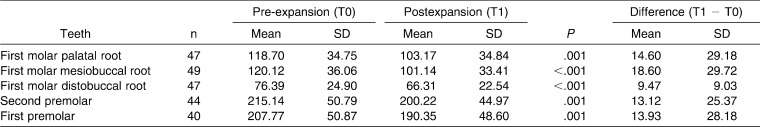
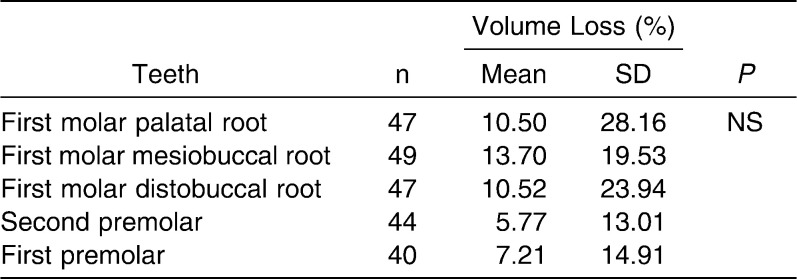
Descriptive statistics and comparison of root volumes before and after RME therapy are given in Table 1. The mean root volumes were decreased after RME. According to the results of the paired-samples t-test, statistically significant differences were found between pre-expansion and postexpansion root volumes. The difference was statistically significant at P < .001 for the buccal roots of the first molar teeth and P = .001 for the second and first premolars and palatal root of the first molar teeth. The highest mean volume loss (MVL) was recorded for the mesiobuccal root of first molar teeth (18.60 mm3), whereas the distobuccal root showed the least MVL (9.47 mm3). First premolar teeth (MVL: 13.12 mm3) were affected nearly to the same extent as second premolars (13.93 mm3). When the percentage of root volume loss was considered, no significant difference was found among the roots (Table 2).
Table 1.
Descriptive Statistics and Statistical Comparison of Pre-expansion and Postexpansion Root Volumes (mm3)
Table 2.
Descriptive Statistics and Statistical Comparison of Root Volume Loss (%)
DISCUSSION
To date, root resorption was studied on anchor premolar teeth, which were subsequently extracted after RME according to the patients' individual treatment plan. Generally, control teeth were obtained from the same patients but from the lower jaw, which was not subjected to orthodontic force. In this study, premolar and molar root volumes were measured in patients who had undergone RME therapy with a tooth-borne banded expander. This was the first study in the literature in which 3D measurements were performed to assess the root volume loss after RME. It was found that root volumes decreased in all investigated roots. The difference between the pre-expansion and postexpansion measurements was statistically significant.
Root volume loss percentages were calculated to determine the most severely affected roots following RME. There were no statistically significant differences, and according to the results of this study, it is not possible to say that the anchor teeth were more severely affected from RME. On the other hand, the age of the patients ranged between 11.2 and 14.1 years. At these ages, root development is expected to continue, especially for the second premolars. In this study, mean root volume was found to decrease in all investigated roots. This finding may be evidence of the disruption of root development. Further studies should be performed whether RME results in shorter roots or not.
In this study, both attached (anchor teeth, first premolars) and unattached (second premolars) premolars were evaluated. Root resorption was also observed in second premolars. Odenrick et al.8 showed root resorption of all maxillary premolars. On the other hand, Barber and Sims10 showed no resorption or repair on unattached premolars. They suggested that these teeth moved laterally with the alveolar process and during the retention phase they relocate palatally. Similarly, no resorption was detected on mandibular first premolars.9,10
Radiographs, histological sections, and SEM evaluations provide 2D evaluations. Except radiographs, evaluation with these methods necessitates and tooth extractions and they are not applicable to vital tooth. In the current study, total root volumes were calculated on CBCT images. Three-dimensional reconstruction of the roots allows us study volume loss during RME. In this way, all posterior teeth were evaluated despite anchor premolars extracted following RME. Thus, to our knowledge, this is the first study that evaluated root resorption of the first permanent molars and second premolars after RME. In this study, root resorption of the first permanent molars and second premolars were evaluated after RME.
Langford and Sims7 found no direct relationship between total area of resorption and length of retention period, but they claim that repair advanced with longer retention periods. Odenrick et al.8 stated that the resorption lacunae decreased with increasing retention period due to repair. Langford6 reported that strong relapse forces might cause significant root resorption until 3 months after RME, whereas Zimring and Isaacson26 found that the residual forces dissipated within 5 to 7 weeks during retention. In this study, the second CBCT records were taken after active expansion was completed. It may be thought that the resorption process was not completed when the second records were taken.
The relationship between the longevity of the teeth and root resorption is generally associated with the root shortening. Zachrisson27 reported that 2-mm apical root shortening is not detrimental to the function of the dentition. Phillips28 claimed that 2-mm root shortening reduced the total attachment area of 5–10%. Barber and Sims10 attracted attention to the periodontal fiber reattachment to the repaired root surface after resorption. They found very few periodontal fiber reattachments up to 8 months of fixed retention. Langford and Sims7 investigated anchor teeth under retention periods of 14 to 53 weeks. They showed sparse and inconsistent Sharpey's fibers depressions into the cellular cementum, which was different from that of normal cellular cementum. Odenrick et al.8 in their polarized light evaluation failed to show periodontal fiber attachment between the reparative cementum and periodontal ligament. In this point of view, it may be said that RME may lead to detrimental effects to the teeth when the life span and the function of the teeth are taken into account.
During 3D reconstruction of first permanent molar roots, roots were separated and evaluated individually. Separation was performed over the cement-enamel junction. Thus, the absolute root volume was not recorded. This was because of the bands on molar teeth, which cause artifacts at the cement-enamel level. Artifacts were clipped manually with great caution, and standardization was achieved with 3D orientation and reference planes.
According to the results of this study, it may be said that RME causes the loss of root structure of posterior teeth. In high-risk patients, RME should be avoided if possible. Young adults may suffer seriously from RME as the skeletal effect is low and greater forces were applied to the anchor teeth. Surgically assisted expansion procedures or orthognathic surgery should be taken into account for the treatment plans of these patients.
CONCLUSIONS
In the current study, the effect of RME on the roots of posterior teeth (premolars and first molar) was assessed with CBCT, and it was concluded that all investigated roots showed statistically significant volume loss.
When the volume loss percentages are considered, no statistically difference was found among roots.
REFERENCES
- 1.Angell E. H. Treatment of irregularity of the permanent or adult teeth. Dent Cosmos. 1860;1:540–544. [Google Scholar]
- 2.Pollock H. C. St. Louis and early orthodontics. Am J Orthod. 1955;41:809–818. [Google Scholar]
- 3.Isaacson R. J, Ingram A. H. Forces produced by rapid maxillary expansion. II. Forces present during treatment. Angle Orthod. 1964;34:261–270. doi: 10.1043/0003-3219(1965)035<0178:FPBRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Isaacson R. J, Wood J. L, Ingrain A. H. Forces produced by rapid maxillary expansion. I. Design of the force measuring system. Angle Orthod. 1964;34:256–260. [Google Scholar]
- 5.Odenrick L, Lilja E, Lindback K. Root surface resorption in two cases of rapid maxillary expansion. Br J Orthod. 1982;9:37–40. doi: 10.1179/bjo.9.1.37. [DOI] [PubMed] [Google Scholar]
- 6.Langford S. R. Root resorption extremes resulting from clinical RME. Am J Orthod. 1982;81:371–377. doi: 10.1016/0002-9416(82)90074-4. [DOI] [PubMed] [Google Scholar]
- 7.Langford S. R, Sims M. R. Root surface resorption, repair and periodontal attachment following rapid maxillary expansion in man. Am J Orthod. 1982;81:108–115. doi: 10.1016/0002-9416(82)90034-3. [DOI] [PubMed] [Google Scholar]
- 8.Odenrick L, Karlander E. L, Pierce A, Kretschmar U. Surface resorption following two forms of rapid maxillary expansion. Eur J Orthod. 1991;13:264–270. doi: 10.1093/ejo/13.4.264. [DOI] [PubMed] [Google Scholar]
- 9.Erverdi N, Okar I, Kucukkeles N, Arbak S. A comparison of two different rapid palatal expansion techniques from the point of root resorption. Am J Orthod Dentofac Orthop. 1994;106:47–51. doi: 10.1016/S0889-5406(94)70020-6. [DOI] [PubMed] [Google Scholar]
- 10.Barber A. E, Sims M. R. Rapid maxillary expansion and external root resorption in man: a scanning electron microscopic study. Am J Orthod. 1981;79:630–652. doi: 10.1016/0002-9416(81)90356-0. [DOI] [PubMed] [Google Scholar]
- 11.Ketcham A. H. A preliminary report of an investigation of apical root resorption of permanent teeth. Int J Orthod. 1929;15:310–328. [Google Scholar]
- 12.Reitan K. Initial tissue behavior during apical root resorption. Angle Orthod. 1974;44:68–82. doi: 10.1043/0003-3219(1974)044<0068:ITBDAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Owman-Moll P, Kurol J, Lundgren D. Effects of a doubled orthodontic force magnitude on tooth movement and root resorption. Eur J Orthod. 1996;18:141–150. doi: 10.1093/ejo/18.2.141. [DOI] [PubMed] [Google Scholar]
- 14.Amano M, Agematsu H, Abe S, Usami A, Matsunaga S, Suto K, Ide Y. Three-dimensional analysis of pulp chambers in maxillary second deciduous molars. J Dent. 2006;34:503–508. doi: 10.1016/j.jdent.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Chan E. K. M, Darendeliler M. A. Exploring the third dimension in root resorption. Orthod Craniofac Res. 2004;7:64–70. doi: 10.1111/j.1601-6343.2004.00280.x. [DOI] [PubMed] [Google Scholar]
- 16.Dermaut L. R, De Munck A. Apical root resorption of upper incisors caused by intrusive tooth movement: a radiographic study. Am J Orthod Dentofac Orthop. 1986;90:321–326. doi: 10.1016/0889-5406(86)90088-0. [DOI] [PubMed] [Google Scholar]
- 17.Levander E, Malmgren O. Evaluation of the risk of root resorption during orthodontic treatment: a study of upper incisors. Eur J Orthod. 1988;10:30–38. doi: 10.1093/ejo/10.1.30. [DOI] [PubMed] [Google Scholar]
- 18.Linge L, Linge B. O. Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. Am J Orthod Dentofac Orthop. 1991;99:35–43. doi: 10.1016/S0889-5406(05)81678-6. [DOI] [PubMed] [Google Scholar]
- 19.Beck B. W, Harris E. F. Apical root resorption in orthodontically treated subjects: analysis of edgewise and light wire mechanics. Am J Orthod Dentofac Orthop. 1994;105:350–361. doi: 10.1016/S0889-5406(94)70129-6. [DOI] [PubMed] [Google Scholar]
- 20.Maltha J. C, van Leeuwen E. J, Dijkman G. E. H. M, Kuijpers-Jagtman A. M. Incidence and severity of root resorption in orthodontically moved premolars in dogs. Orthod Craniofac Res. 2004;7:115–121. doi: 10.1111/j.1601-6343.2004.00283.x. [DOI] [PubMed] [Google Scholar]
- 21.Ericson S, Kurol J. Incisor root resorptions due to ectopic maxillary canines imaged by computerized tomography: a comparative study in extracted teeth. Angle Orthod. 2000;70:276–283. doi: 10.1043/0003-3219(2000)070<0276:IRRDTE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Heimisdottir K, Bosshardt D, Ruf S. Can the severity of root resorption be accurately judged by means of radiographs? A case report with histology. Am J Orthod Dentofacial Orthop. 2005;128:106–109. doi: 10.1016/j.ajodo.2004.11.028. [DOI] [PubMed] [Google Scholar]
- 23.Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135:434–437. doi: 10.1016/j.ajodo.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 24.Huang J, Bumann A, Mah J. Three-dimensional radiographic analysis in orthodontics. J Clin Orthod. 2005;39:421–428. [PubMed] [Google Scholar]
- 25.Mah J. K, Liu Yi, Huang R. C, Choo H. R. Advanced applications of cone beam computed tomography in orthodontics. Semin Orthod. 2011;17:57–71. [Google Scholar]
- 26.Zimring J. F, Isaacson R. J. Forces produced by rapid maxillary expansion. III. Forces present during retention. Angle Orthod. 1965;35:178–186. doi: 10.1043/0003-3219(1965)035<0178:FPBRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Zachrisson B. U. Iatrogenic tissue damage following orthodontic treatment. Trans Eur Orthod Soc. 1975:488–501. [Google Scholar]
- 28.Phillips J. R. Apical root resorption under orthodontic therapy. Angle Orthod. 1955;25:1–22. [Google Scholar]