Abstract
Objective:
To investigate the impact of malocclusion on adolescents' dissatisfaction with dental appearance and oral functions and to identify components of malocclusion that may contribute to these outcomes.
Materials and Methods:
The sample comprised 704 secondary school adolescents aged 12 to 13 years from Balneário Camboriú, Brazil. A trained and calibrated orthodontist examined the severity of malocclusion using the Dental Aesthetic Index (DAI). A pretested questionnaire was used to assess reported dental appearance, self-perception of speech, and self-perception of masticatory function using a 5-point scale of oral health status. The outcomes of the present study were dissatisfaction with dental appearance and dissatisfaction with oral functions. Simple and multivariate logistic regression analysis was performed to explore the association between DAI and outcomes and to quantify the effect of DAI components on dissatisfaction with dental appearance.
Results:
Each DAI unit increase led to a significant increase of 5% in the likelihood of dissatisfaction with dental appearance (OR: 1.05; 95% CI 1.01–1.08). DAI components that exerted influence on dissatisfaction with dental appearance were: missing teeth (P = .010), largest maxillary anterior irregularity ≥3 mm (P = .013), and largest mandibular anterior irregularity ≥2 mm (P = .008). There was no association between severity of malocclusion and dissatisfaction with oral functions.
Conclusions:
Severity of malocclusion interfered with satisfaction of dental appearance in this population. Missing teeth and anterior irregularity were identified as factors influencing this outcome.
Keywords: Epidemiology, Malocclusion, Personal satisfaction, Smiling, Mastication, Speech
INTRODUCTION
The indication for treatment of malocclusion is based traditionally on professional perceptions in relation to normative aspects of orthodontic diagnosis. These aspects take into account primarily anteroposterior, vertical, and transverse disharmonies. Over the last decade, indices of orthodontic treatment need have been used to screen patients for treatment priority, to prevent unnecessary treatment, and to provide a basis for discussion among health professionals, parents, and children.1,2 The most commonly used indices are the Dental Aesthetic Index (DAI), recommended by the World Health Organization3 and the Index of Orthodontic Treatment Need.
The greatest benefit of orthodontic treatment appears to be related to improved physical, psychological, and social well-being,4–6 and possible ways to achieve this goal include improvements of oral function and esthetics (dental appearance). A number of studies have measured the effect of different disharmonies on the perception of adolescents towards esthetics and function.5,7–9 Assuming the premise that the success of care should be defined by criteria that would be meaningful to both professionals and patients,4,10 this knowledge could contribute decisively to the development of protocols on the need and ultimate goals of orthodontic treatment tailored to each patient. Moreover, the definition of individuals who would potentially benefit from treatment by further investigation of possible relationships between malocclusion and perceptions of esthetics and function in different populations is essential to design more cost-effective public policies.
The objectives of this study were (a) to verify the association between malocclusion, as assessed by the DAI, and dissatisfaction with dental appearance and oral functions in a population of adolescents in southern Brazil; and (b) to identify components of the index that might contribute to these outcomes and quantify the strengths of association.
MATERIALS AND METHODS
Subjects and Study Design
This cross-sectional study included students attending all the Municipal Education Centers of Balneário Camboriú, state of Santa Catarina, a city with approximately 100,000 inhabitants located in southern Brazil. Between February and July 2009 students aged 12 to 13 years, whose parents agreed to participate in the study, were examined. Students with current or previous experience of orthodontic or orthopedic treatment were excluded.
Sample size calculation was based on the following parameters: target population of 1200 students, projection of 30% of occlusal problems,11 95% confidence level, statistical power of 80%, and 2.5% margin of error, which determined the minimum sample size of 622 adolescents. Anticipating a nonresponse rate of about 30% and exclusion of 10% of adolescents due to current or previous orthodontic treatment, questionnaires were delivered to all students in all schools.
Demographic and Self-Reported Variables
A structured questionnaire7,12 was used to collect data on the following variables: sex, age, reported dental appearance, self-perception of speech, and self-perception of masticatory function using a 5-point scale (very poor/poor/fair/good/very good) of oral health status. The outcomes of the present study were: dissatisfaction with dental appearance (a poor or very poor reported dental appearance) and dissatisfaction with oral functions, reported as a poor/very poor speech perception, or a poor/very poor masticatory function perception. The questionnaire was previously applied 2 weeks apart to 35 students aged 12 to 13 years, and test-retest reliability was analyzed using kappa statistics.13 An almost perfect reliability (kappa = 0.87; 95% CI 0.77–0.96) was shown for the original 5-point scale instrument and a perfect agreement (kappa = 1.00) for the dichotomous outcome (dissatisfaction: yes/no).
Clinical Variables
Clinical examination was performed by an experienced orthodontist using a mouth mirror, gauze pads, wooden spatula, and Community Periodontal Index periodontal probe,3 in compliance with biosafety standards. Orthodontic treatment need was assessed using the DAI, which involves the assessment of 10 parameters of dentofacial anomalies related to both clinical and esthetic aspects: missing teeth, incisal crowding, incisal spacing, largest anterior maxillary irregularity, largest anterior mandibular irregularity, maxillary overjet, mandibular overjet, anterior open bite, and anteroposterior molar relationship. The results were multiplied by the respective round coefficient (weight) and added up, and a constant value of 13 was then added to the results.14
Intraexaminer reproducibility was previously assessed in two dental examinations conducted 15 days apart in 20 subjects aged 12 to 13 years (kappa = 0.86).
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS Inc, Chicago, Ill), version 16.0, was used for data analysis. Pearson correlation test was used to explore the correlation between DAI and scores of reported dental appearance, self-perception of speech, and self-perception of masticatory function. The chi-square test was then used to verify the association of DAI and sociodemographic variables with the binary outcomes. In this analysis, DAI was categorized into quartiles to reflect the variable distribution in this population.
Simple and multivariate logistic regression analysis was performed to explore the association between DAI (as a quantitative variable) and outcomes, being initially included in the model variables with P < .15. Subsequently, variables with P < .05 were excluded until the final model was obtained; sex was maintained as a variable regardless of its level of significance. Finally, to determine and quantify the association between specific DAI components and outcomes, a new model of simple and multivariate logistic regression analysis was performed. A two-tailed P value of less than .05 was considered statistically significant, and the Hosmer-Lemeshow test was used to assess the goodness of fit of the final model. Comparisons between respondents and nonrespondents regarding baseline variables (gender and level of education) were also performed to investigate the effect of nonresponse (chi-square and t-test for independent samples, respectively).
Ethical Aspects
This study was approved by the Research Ethics Committee of Universidade Luterana do Brasil (ULBRA – Canoas-RS), Brazil. Participation in the study was authorized by parents who signed a written informed consent form.
RESULTS
The final sample included 704 secondary school adolescents from 11 schools. The study subjects showed similar distribution in relation to sex (male: 53.1%; female: 46.9%) and age (12 years: 45.6%; 13 years: 54.4%). As for ethnic group, most individuals were white (75.3%), followed by mestizo (18.7%), and black (6.0%). Maternal education ranged from 0 to 13 years of schooling, with mean (SD) of 7.5 (3.3) years. DAI scores ranged from 13 to 47, with mean (SD) of 25.3 (5.8) and median (P25–P75) of 24 (21–28), showing an approximately normal distribution.
The score of satisfaction with dental appearance significantly decreased with the increase in DAI score (P = .001). The following mean scores were observed in DAI categories: 3.49 (DAI ≤ 20), 3.31 (DAI 21–24), 3.26 (DAI 25–28), and 3.16 (DAI ≥ 29). However, no correlation was found between DAI scores and self-perception of speech or self-perception of masticatory function (P > .05).
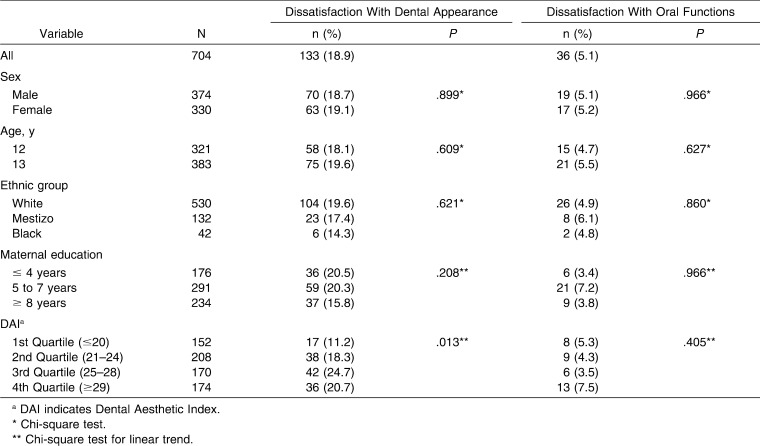
The prevalence of poor self-rated dental appearance was 18.9% (95% CI 16.0–21.7), significantly higher than the prevalence of poor self-rated speech and masticatory function (1.6% and 4.0%, respectively). Overall, the prevalence of dissatisfaction with oral functions was 5.1% (95% CI 3.5–6.7). The increase in DAI categories was associated with an increase in the occurrence of dissatisfaction with dental appearance (P = .013). However, no association was found between DAI categories and dissatisfaction with oral functions (Table 1).
Table 1.
Distribution of Students in Relation to Dissatisfaction With Dental Appearance and Oral Functions (Speech and Masticatory Function)
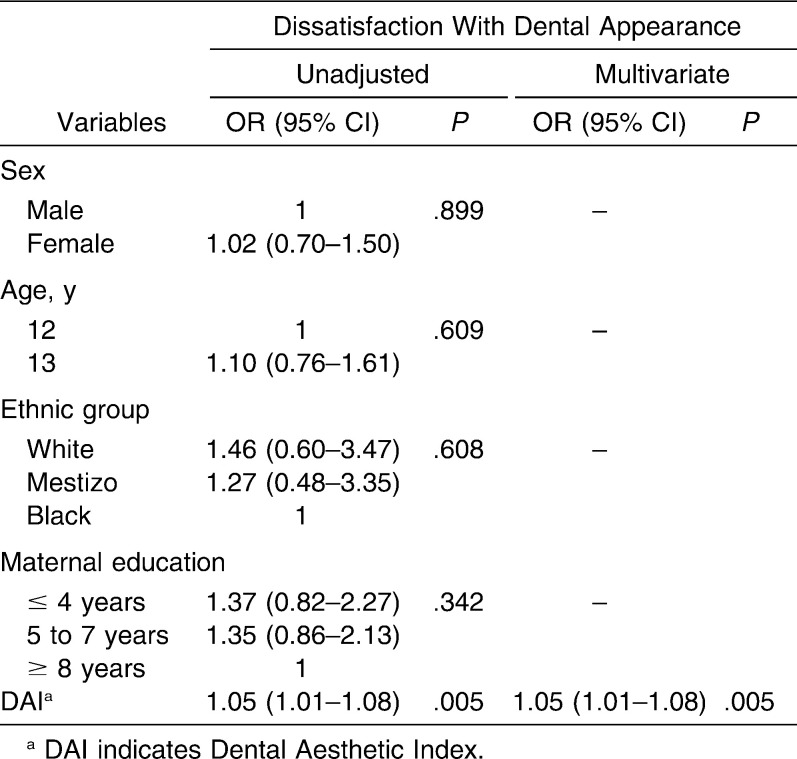
According to the unadjusted logistic regression model, DAI was significantly associated with dissatisfaction with dental appearance (P = .005), whereas sex, age, ethnic group, and maternal education were not associated. In the final model, after adjustment for sex, there were no changes in DAI estimates, noting that each DAI unit increase led to an increase of 5% in the likelihood of dissatisfaction with dental appearance (OR: 1.05; 95% CI 1.01–1.08) (Table 2). The Hosmer-Lemeshow test indicated a good model fit (P = .192).
Table 2.
Unadjusted and Adjusted Odds Ratio (OR) and 95% Confidence Interval (CI) of Dissatisfaction with Dental Appearance, According to Categories of Independent Variables
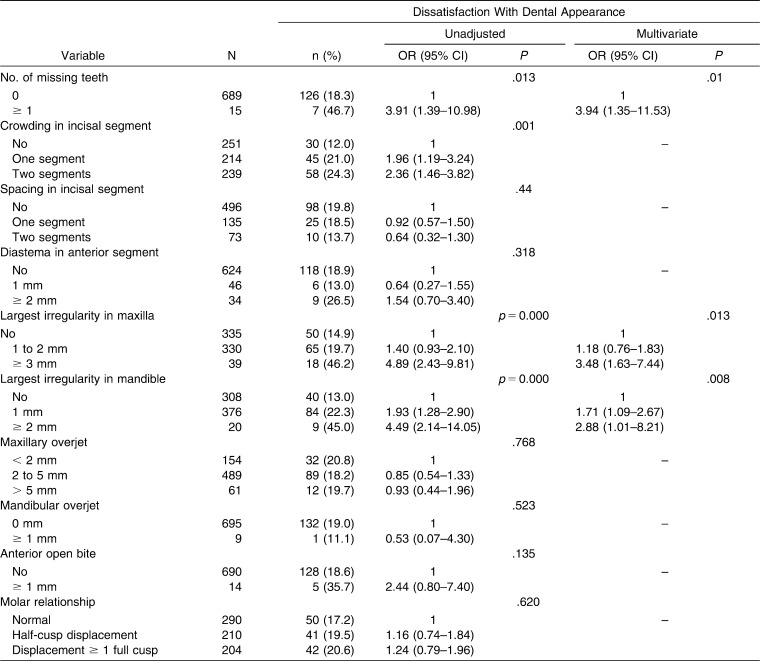
The following DAI components were associated with dissatisfaction with dental appearance in the unadjusted model: missing teeth (P = .013), crowding in incisal segment (P = .001), largest anterior irregularity in the maxilla ≥3 mm (P < .001), and largest irregularity in mandible ≥2 mm (P < .001). In the multivariate model, however, crowding in the incisal segment lost association. The final model showed a 4-fold increase in the likelihood of dissatisfaction with dental appearance when patients had at least one tooth missing and a 3.5-fold increase when patients had a largest anterior irregularity in the maxilla of at least 3 mm. In addition, this outcome was 70% more likely to occur with a 1-mm largest anterior irregularity in the mandible and almost three times more likely to occur with a largest anterior irregularity in the mandible of at least 2 mm (Table 3). The Hosmer-Lemeshow test indicated a good model fit (P = .939).
Table 3.
Unadjusted and Adjusted Odds Ratio (OR) and 95% Confidence Interval (CI) of Dissatisfaction With Dental Appearance, According to DAI Components
According to the unadjusted logistic regression analysis, there was no association between DAI and dissatisfaction with oral functions (OR: 1.04; 95% CI 0.98–1.09). The inclusion of possible confounding variables did not change estimates, and DAI remained not associated. Likewise, none of DAI components was associated with dissatisfaction with oral functions.
No difference was found between respondents and non-respondents with respect to gender (male respondents: 53.1% vs male non-respondents 51.8%; P = 0.665) and level of education [mean (SD): respondents: 6.6 (1.0) years vs non-respondents: 6.5 (0.9) years; P = 0.083].
DISCUSSION
The main result of this study was the observation that an increase in the severity of malocclusion, as measured by DAI, increases the likelihood of dissatisfaction with dental appearance, and anterior irregularity and missing teeth were identified as key factors in this association. These easily visible undesirable traits coupled with low social acceptance of such changes by others provide a possible explanation for this association. The main clinical significance of these findings is the need for the orthodontist to prioritize the correction of anterior irregularity in order to improve the patient's self-perception of dental appearance.5,6 Furthermore, this professional may contribute to replace missing teeth through a model of integrated care with a multidisciplinary team approach. Providing better dental appearance appears to have a direct impact on psychosocial issues, such as shyness, embarrassment, being upset, and avoidance of smiling, especially on more relevant issues.4,15
The influence of malocclusion on appearance dissatisfaction has been previously reported in other adolescent populations.15,16 However, it is noteworthy that in this study maxillary overjet and anterior diastema did not influence this outcome. This is different from an Asian population, in which increased overjet was perceived by laypersons as the major occlusal trait affecting dental esthetics.17 One must consider that the development of physical self-concept is thought to be based on the perceived reactions of others and the comparisons a child makes of his/her physical attributes relative to those of others, which might be strongly influenced by the culture of each population. In this context, self-concept issues are more likely related to an adolescent's own self-adjustment and overall self-perception of the dentofacial region, rather than strictly to malocclusion.18
In the present study, the fact that the adolescents' perception of oral functions did not vary according to the level of malocclusion, in relation to DAI and its components, is surprising. On the other hand, malocclusions were associated with significantly lower skillfulness of masticatory jaw motion in Japanese patients.19 It has been reported previously in patients from the Finnish publicly funded orthodontic care that priority given to functional rather than esthetic aspects determined a lower level of satisfaction with orthodontic treatment.20
It is worth mentioning that molar relationship, a condition representing an important aspect of normative orthodontic diagnosis, was not associated with dissatisfaction with appearance or oral functions in the present study. However, its correction is crucial to occlusal balance and indirectly contributes to outcomes considered relevant to patients, such as anterior irregularity in the maxilla and mandible, and should therefore remain as a goal to be achieved in orthodontic treatment. Likewise, increased overjet predisposes patients to other clinically relevant outcomes such as dentoalveolar trauma21,22 and its correction should remain as a goal of orthodontic treatment. On the other hand, our results reinforce the concept that the goals of orthodontic intervention should be even more comprehensive, going beyond the simple solution of normative aspects and assigning the relative weights of the conditions identified as a cause of dissatisfaction in each population.23
Although worse clinical orthodontic status was associated with a more negative perception of dental appearance in the present study, a high proportion of adolescents in the highest tertile of DAI did not report dissatisfaction with their dental appearance or oral functions. Similar results have been reported in relation to the impact of malocclusion on quality of life,9,24–26 and this knowledge may have important implications, considering the limited resources available in public health. The exclusive use of clinical criteria as a determinant of access to treatment can result in setting goals that are impossible to achieve, contributing to inequalities in access to orthodontic treatment already reported in different populations.11,16 It is possible that the adoption of approaches based on clinical criteria, followed by the assessment of the perceived oral health impacts and needs, can yield a better cost-effectiveness ratio.4,15 This strategy is of particular importance in countries that have not yet included orthodontic treatment in public attention to oral health, such as Brazil,16 and therefore need to redesign public policies based on scientific evidence.
One limitation of the present study is the fact that DAI may underestimate the occurrence of malocclusion for failing to address conditions such as posterior crossbite, deep bite, or midline displacement.1,27 Nevertheless, DAI was integrated into the International Collaboration Study of Oral Health Outcomes by the World Health Organization28 and has been used worldwide in epidemiologic studies of orthodontic treatment need.5,6,15,26 Another aspect to note is that studies have increasingly used validated instruments to assess the impact of malocclusion on quality of life. One must consider that the scope of this study was exactly to detect the subject's self-perception of the two major reasons, from a theoretical point of view, for orthodontic correction: dissatisfaction with appearance and oral functions. Furthermore, the use of only three simple questions, which demonstrated excellent reproducibility, enabled us to evaluate a large sample size, providing the clinician with more accurate estimates of the relationship between malocclusion and its components, with relevant outcomes to patients. Selection bias is unlikely to be a problem in this study. Although it is impossible to determine the level of dissatisfaction with dental appearance of nonrespondents, a significant difference is not expected in relation to those who actually participated in the study, considering the similarity in baseline characteristics between both groups.
Our findings can be generalized to populations with cultural and demographic characteristics similar to those of the population living in southern Brazil: mostly white individuals, with heterogeneous socioeconomic status, living in a developing country. It is possible that in populations with greater severity of malocclusion the strengths of association become even greater, and some level of influence might also be detected in oral functions.
CONCLUSIONS
Increased malocclusion severity levels lead to a worsening of the subject's own perception of dental appearance.
Special attention should be directed to factors that appear to individually influence this outcome; anterior irregularity in maxilla and in the mandible and missing teeth.
Malocclusion as a whole, or through its components, had no influence upon the individual's perception of oral functions.
REFERENCES
- 1.Abdullah M. S, Rock W. P. Assessment of orthodontic treatment need in 5,112 Malaysian children using the IOTN and DAI indices. Community Dent Health. 2001;18:242–248. [PubMed] [Google Scholar]
- 2.Spalj S, Slaj M, Varga S, Strujic M, Slaj M. Perception of orthodontic treatment need in children and adolescents. Eur J Orthod. 2010;32:387–394. doi: 10.1093/ejo/cjp101. Epub 2009 Oct 27. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Oral Health Surveys Basic Methods 4th ed. Geneva: World Health Organization; 1997. [Google Scholar]
- 4.Tsakos G. Combining normative and psychosocial perceptions for assessing orthodontic treatment needs. J Dent Educ. 2008;72:876–885. [PubMed] [Google Scholar]
- 5.Nagarajan S, Pushpanjali K. The relationship of malocclusion as assessed by the Dental Aesthetic Index (DAI) with perceptions of aesthetics, function, speech and treatment needs among 14- to 15-year-old schoolchildren of Bangalore, India. Oral Health Prev Dent. 2010;8:221–228. [PubMed] [Google Scholar]
- 6.Paula D. F, Jr, Silva E. T, Campos A. C, Nuñez M. O, Leles C. R. Effect of anterior teeth display during smiling on the self-perceived impacts of malocclusion in adolescents. Angle Orthod. 2011;81:540–545. doi: 10.2319/051710-263.1. Epub 2011 Jan 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shue-Te Yeh M, Koochek A. R, Vlaskalic V, Boyd R, Richmond S. The relationship of 2 professional occlusal indexes with patients' perceptions of aesthetics, function, speech, and orthodontic treatment need. Am J Orthod Dentofacial Orthop. 2000;118:421–428. doi: 10.1067/mod.2000.107008. [DOI] [PubMed] [Google Scholar]
- 8.Agou S, Locker D, Streiner D. L, Tompson B. Impact of self-esteem on the oral-health-related quality of life of children with malocclusion. Am J Orthod Dentofacial Orthop. 2008;134:484–489. doi: 10.1016/j.ajodo.2006.11.021. [DOI] [PubMed] [Google Scholar]
- 9.Bos A, Hoogstraten J, Zentner A. Perceptions of Dutch orthodontic patients and their parents on oral health-related quality of life. Angle Orthod. 2010;80:367–372. doi: 10.2319/031109-141.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Svedstrom-Oristo A. L, Pietilä I, Vahlberg T, Alanen P, Vaela J. Acceptability of dental appearance in a group of Finnish 16- to 25-year-olds. Angle Orthod. 2009;79:479–483. doi: 10.2319/040108-184.1. [DOI] [PubMed] [Google Scholar]
- 11.Nelson S, Armogan V, Abel Y, Broadbent B. H, Hans M. Disparity in orthodontic utilization and treatment need among high school students. J Public Health Dent. 2004;64:26–30. doi: 10.1111/j.1752-7325.2004.tb02722.x. [DOI] [PubMed] [Google Scholar]
- 12.Onyeaso C. O. An assessment of relationship between self-esteem, orthodontic concern, and Dental Aesthetic Index (DAI) scores among secondary school students in Ibadan, Nigeria. Int Dent J. 2003;53:79–84. doi: 10.1111/j.1875-595x.2003.tb00663.x. [DOI] [PubMed] [Google Scholar]
- 13.Landis J. R, Koch G. G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 14.Jenny J, Cons N. C. Establishing malocclusion severity levels on the Dental Aesthetic Index (DAI) scale. Aust Dent J. 1996;41:43–46. doi: 10.1111/j.1834-7819.1996.tb05654.x. [DOI] [PubMed] [Google Scholar]
- 15.de Paula Júnior D. F, Santos N. C, da Silva E. T, Nunes M. F, Leles C. R. Psychosocial impact of dental esthetics on quality of life in adolescents. Angle Orthod. 2009;79:1188–1193. doi: 10.2319/082608-452R.1. [DOI] [PubMed] [Google Scholar]
- 16.Marques L. S, Filogônio C. A, Filogônio C. B, Pereira L. J, Pordeus I. A, Paiva S. M, Ramos-Jorge M. L. Aesthetic impact of malocclusion in the daily living of Brazilian adolescents. J Orthod. 2009;36:152–159. doi: 10.1179/14653120723139. [DOI] [PubMed] [Google Scholar]
- 17.Soh J, Chew M. T, Chan Y. H. Perceptions of dental esthetics of Asian orthodontists and laypersons. Am J Orthod Dentofacial Orthop. 2006;130:170–176. doi: 10.1016/j.ajodo.2005.05.048. [DOI] [PubMed] [Google Scholar]
- 18.Phillips C, Beal K. N. Self-concept and the perception of facial appearance in children and adolescents seeking orthodontic treatment. Angle Orthod. 2009;79:12–16. doi: 10.2319/071307-328.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tome W, Yashiro K, Takada K. Orthodontic treatment of malocclusion improves impaired skillfulness of masticatory jaw movements. Angle Orthod. 2009;79:1078–1083. doi: 10.2319/052708-282R.1. [DOI] [PubMed] [Google Scholar]
- 20.Svedström-Oristo A. L, Pietilä T, Pietilä I, Alanen P, Varrela J. Morphological, functional and aesthetic criteria of acceptable mature occlusion. Eur J Orthod. 2001;23:373–381. doi: 10.1093/ejo/23.4.373. [DOI] [PubMed] [Google Scholar]
- 21.Viegas C. M, Scarpelli A. C, Carvalho A. C, Ferreira F. M, Pordeus I. A, Paiva S. M. Predisposing factors for traumatic dental injuries in Brazilian preschool children. Eur J Paediatr Dent. 2010;11:59–65. [PubMed] [Google Scholar]
- 22.Feldens C. A, Kramer P. F, Ferreira S. H, Spiguel M. H, Marquezan M. Exploring factors associated with traumatic dental injuries in preschool children: a Poisson regression analysis. Dent Traumatol. 2010;26:143–148. doi: 10.1111/j.1600-9657.2009.00858.x. [DOI] [PubMed] [Google Scholar]
- 23.Taylor K. R, Kiyak A, Huang G. J, Greenlee G. M, Jolley C. J, King G. J. Effects of malocclusion and its treatment on the quality of life of adolescents. Am J Orthod Dentofacial Orthop. 2009;136:382–392. doi: 10.1016/j.ajodo.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 24.de Oliveira C. M, Sheiham A, Tsakos G, O'Brien K. D. Oral health-related quality of life and the IOTN index as predictors of children's perceived needs and acceptance for orthodontic treatment. Br Dent J. 2008;12;204(7):1–5. doi: 10.1038/bdj.2008.239. discussion 384–385. [DOI] [PubMed] [Google Scholar]
- 25.Feu D, de Oliveira B. H, de Oliveira Almeida M. A, Kiyak H. A, Miguel J. A. Oral health-related quality of life and orthodontic treatment seeking. Am J Orthod Dentofacial Orthop. 2010;138:152–159. doi: 10.1016/j.ajodo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 26.Agou S, Locker D, Muirhead V, Tompson B, Streiner D. L. Does psychological well-being influence oral-health-related quality of life reports in children receiving orthodontic treatment? Am J Orthod Dentofacial Orthop. 2011;139:369–377. doi: 10.1016/j.ajodo.2009.05.034. [DOI] [PubMed] [Google Scholar]
- 27.Baca-Garcia A, Bravo M, Baca P, Baca A, Junco P. Malocclusions and orthodontic treatment needs in a group of Spanish adolescents using the Dental Aesthetic Index. Int Dent J. 2004;54:138–142. doi: 10.1111/j.1875-595x.2004.tb00269.x. [DOI] [PubMed] [Google Scholar]
- 28.Chen M, Andersen R. M, Barmes D. E, Leclerq M. H, Lyttle S. C. Comparing Oral Health Systems A Second International Collaborative Study. Geneva: World Health Organization; 1997. [Google Scholar]