Abstract
Objective:
To investigate the incidence and severity of root resorption during orthodontic treatment by means of cone beam computed tomography (CBCT) and to explore factors affecting orthodontically induced inflammatory root resorption (OIIRR).
Materials and Methods:
CBCT examinations were performed on 152 patients with Class I malocclusion. All roots from incisors to first molars were assessed on two or three occasions.
Results:
At treatment end, 94% of patients had ≥1 root with shortening >1 mm, and 6.6% had ≥1 tooth where it exceeded 4 mm. Among teeth, 56.3% of upper lateral incisors had root shortening >1 mm. Of upper incisors and the palatal root of upper premolars, 2.6% showed root shortenings >4 mm. Slanted surface resorptions of buccal and palatal surfaces were found in 15.1% of upper central and 11.5% of lateral incisors. Monthly root shortening was greater after 6-month control than before. Upper jaw teeth and anterior teeth were significantly associated with the degree of root shortening. Gender, root length at baseline, and treatment duration were not.
Conclusion:
Practically all patients and up to 91% of all teeth showed some degree of root shortening, but few patients and teeth had root shortenings >4 mm. Slanted root resorption was found on root surfaces that could be evaluated only by a tomographic technique. A CBCT technique can provide more valid and accurate information about root resorption.
Keywords: CBCT, Root resorption, Adolescents, Orthodontics
INTRODUCTION
Inflammatory root resorption is a side effect related to the biological tissue response1,2 that enables teeth to be moved during orthodontic treatment and with which it was first associated already in 1914.3 In histologically examined teeth, it has been found in up to 100% of orthodontically treated teeth but less often in teeth examined by panoramic or intraoral radiography.1,4
In most studies of orthodontically induced inflammatory root resorption (OIIRR), intraoral radiography has been used.5 Even with efforts to obtain periodically identical radiographs,6,7 this technique has shortcomings.8–11 An in vitro study12 showed that, to become visualized on intraoral radiographs, buccal or palatal surface resorption had to result in root shortening. On panoramic radiographs, root apices, especially in anterior regions, may become placed outside the narrow focal trough. The usefulness of lateral cephalometric radiography in detecting root resorption is limited by super-impositioning of teeth.13
For demanding diagnostic tasks in the maxillofacial region, computed tomography (CT) can be used, but high radiation doses and costs have prevented it from becoming a standard tool in dental imaging. Despite inherent capabilities in diagnosing OIIRR, it has not been considered for this purpose. Cone beam CT (CBCT) was introduced in dentistry in the late 1990s,14,15 and its high spatial resolution, affordability, and relatively low radiation doses quickly led to its acceptance,16 also in orthodontics.17 Radiation doses, however, vary between CBCT machines for various reasons (eg, exposed volume size, exposure parameters used).18–20 The ability of CBCT to obtain distortion-free and reproducible images of single roots provides excellent possibilities to study root resorption,21 not least because it, more closely than its alternatives, approaches a histologic method.
This study aimed, by means of CBCT, to investigate the incidence and severity of root resorption during orthodontic treatment and to explore factors that have a possible influence on the degree of root shortening.
MATERIALS AND METHODS
Subjects
From March 2005 to June 2008, 183 patients from the Department of Orthodontics, Public Dental Health, Gothenburg, Sweden, were consecutively invited to participate in the study. Inclusion criteria included the following: age 9–18 years, Class I malocclusion (super Class I: cusp-to-cusp distal molar relationship) with crowding, and an overjet ≤5mm. Crowding had to be of an extent motivating extraction of one premolar in each jaw quadrant. Informed consent from the patients' parents and ethical approval from the Regional Ethical Review Board were obtained.
Twelve patients did not wish to participate, leaving 171 patients undergoing the first of two or three radiographic examinations. Mean age of patients at the start of the study was 15.2 years (SD 1.6; range 10.1–18.6). At the end of the study, 152 patients (65 boys, 87 girls), or 83% of all invited, remained.
The treatment protocol was standardized using an MBT preadjusted appliance (3M Unitek Orthodontic Products, Monrovia, Calif) with 0.022 inch slots. Initial leveling and alignment were done using round, heat-activated, nickel-titanium wires. Space closure was performed using rectangular .019 × .025 stainless steel wires. Mean treatment duration was 20.7 months (median 20; SD 5.7; range 11–43). In accordance with the treatment plan, 582 premolars (48%) were extracted. In five patients, no extractions were performed, and in four patients, two or three premolars were removed.
Radiographic Examination
Radiographic examinations were performed on two or three occasions: before the start of treatment (baseline, n = 171), after 6 months (n = 97), and when treatment was completed (endpoint, n = 152). The 6-month control, to which patients were randomly selected, was conducted to determine whether root resorption had occurred to an extent (score 3 according to Malmgren et al.22) motivating temporary treatment discontinuation. Three patients showed root shortening to an extent motivating 3-month treatment discontinuation.23
Examinations were performed with a 3DX Accuitomo FPD CBCT unit (J Morita Mfg Corp, Kyoto, Japan) equipped with a flat panel detector. Exposed volume was 60 mm × 60 mm (voxel size 0.125 mm), encompassing all teeth from incisors to first molars in both jaws. Exposure parameters were 75 kV and 4–5.5 mA (based on subject size) with a single 360-degree rotation (17.5 s) seen in approximately 556 projections.
Workstation
Primary data reconstructions were made with the use of acquisition software (i-Dixel-3DX, 3D, version 1.691) at the Accuitomo workstation, resulting in perpendicular axial, coronal, and sagittal slices. A second reconstruction was made to obtain contiguous 0.5-mm-thick slices. Using DICOM-export, the axial slices were sent to PACS for later reformatting using a workstation with Sectra IDS5 (Sectra Imtec AB, Linköping, Sweden) PACS MPR (multiplanar reconstruction). The workstation consisted of a computer (Optiplex 755, Dell AB, Stockholm, Sweden) with a graphic card (NVIDIA GeForce 6800 Series GPU 32-bit, Matrox MED2mp-DVI). Measurements were made on a monochromatic 20-inch flat panel monitor (resolution 1600 × 1200 pixels, OLÓRIN Medic Line ML187D TFT-LCD, Olorin AB, Kungsbacka, Sweden).
Assessment of Root Length and Apical Surface Resorption
Reconstructions were made so that the axial slices became perpendicular to the long axis of the tooth/root. This provided optimal visualization of the tooth/root in axial, coronal, and sagittal planes. A reference line was placed connecting the buccal and palatal/lingual cementoenamel junctions. Parallel to this, a second reference line was placed at the root apex. Without access to previous radiographs or protocols, the perpendicular distance between these reference lines was measured (Figure 1) at incisors to first molars by one of the authors. It was measured to the nearest 0.01 mm at fully erupted teeth at which the cementoenamel junction (CEJ) and the apex could be clearly identified. At teeth with multiple roots, each root was separately assessed. The precision of the method has been found to be within the range 0.19–0.32 mm.21 As can be derived from Table 1b, few roots were unreadable at one or more examinations. An exception was the distal root of the lower first molar, which was unreadable in 32% because it was not always contained in the imaged volume. Surface resorptions not resulting in root shortening (Figure 2) were noted, as were roots with incomplete root development.
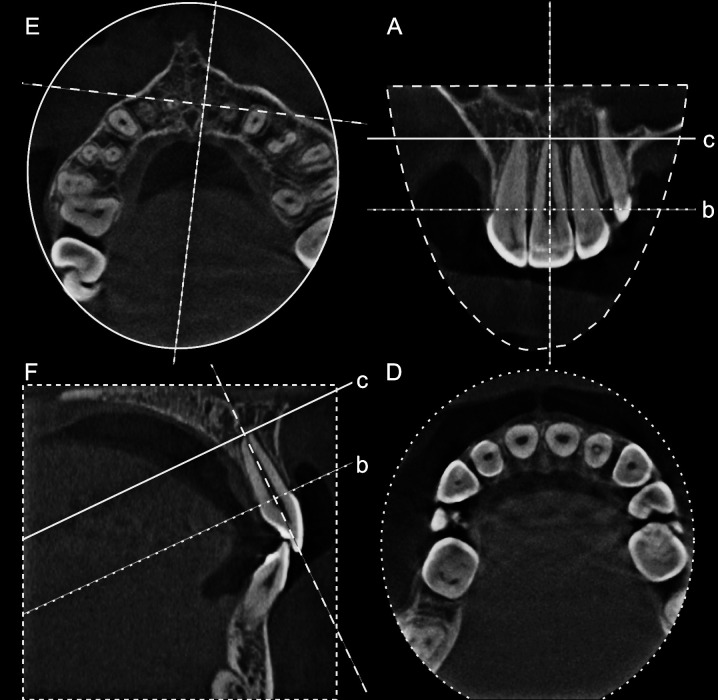
Figure 1.
Measurement procedure for assessment of root length by means of axial, coronal, and sagittal slices. Measurements were made (A) in the coronal view between two reference lines, (b) one at the cementoenamel junction, (c) and one at the root apex. D and E, Corresponding axial views and (F) sagittal view were used to ensure proper positioning of reference lines.
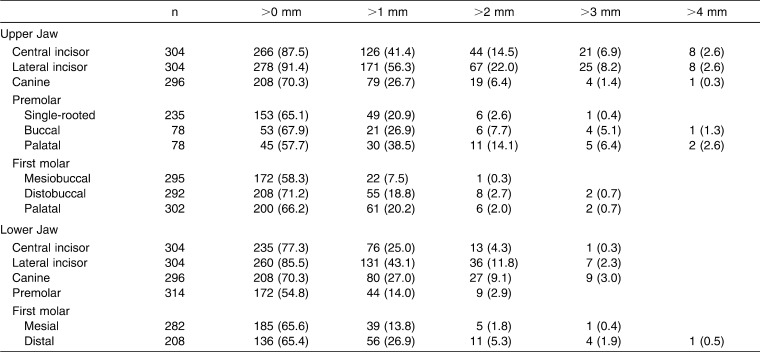
Table 1b.
Numbers and Percentages of Roots With Different Extent of Root Shortening From Baseline to Endpoint
Figure 2.
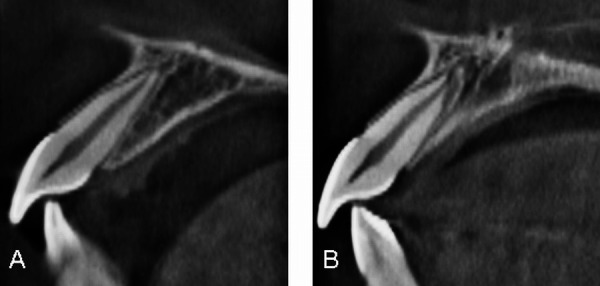
A, Example of an upper central incisor at baseline, with (B) palatal surface resorption at endpoint.
Statistical Analyses
Changes in root length between baseline and subsequent examinations are presented by means of descriptive statistics. The premolars in each jaw quadrant were merged into a single group. Teeth with multiple roots were analyzed separately. Analyses of changes in root length per month during the two observation periods (baseline to 6-month and 6-month to endpoint) were completed using Wilcoxon's signed rank test. Root shortening was evaluated with a mixed covariance pattern model including a compound symmetry covariance model to estimate dependence within patients. A significance level of P < .05 was used in all statistical analyses. Descriptive analyses were made with Microsoft Office Excel 2003 (Microsoft Professional Edition 2003, Microsoft Corporation, Redmond, Wash) and statistical analyses by means of SAS 9.2 (SAS Institute Inc, Cary, NC).
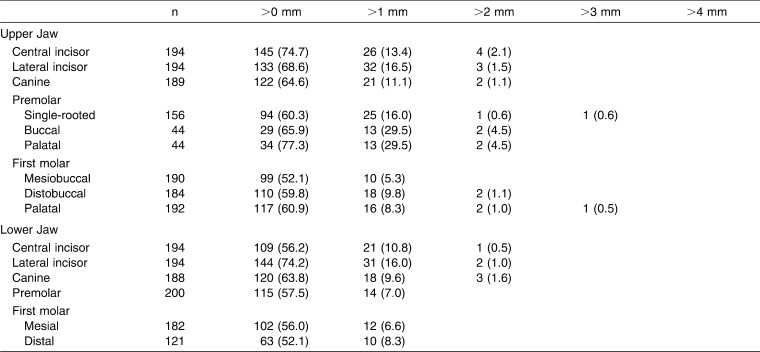
RESULTS
Sixty-one roots (1.6%) had incomplete root development at baseline. Percentages of roots with different extent of root shortenings from baseline to 6-month and from baseline to endpoint are found in Tables 1 and 1b. At the 6-month control, the highest frequencies of root shortening >1 mm were found at both roots of upper two-rooted premolars (29.5%), lateral incisors (upper 16.5%, lower 16%), and upper, single-rooted premolars (16%). Few roots had shortenings >2 mm, and none had shortening >4 mm. At endpoint, the highest frequencies of root shortenings exceeding 1 mm were found at lateral incisors (upper 56.3%, lower 43.1%), followed by upper central incisors (41.4%). Root shortenings >4 mm were found in 2.6% of upper incisors and in the palatal root of two-rooted upper premolars. Of all patients, 94% had at least one tooth with root shortening >1 mm, and 6.6% had one or more teeth with root shortening >4 mm. Approximately 1% of patients had ≥14 teeth with root shortening ≥1 mm; none had ≥4 teeth with root shortening >4 mm.
Table 1a.
Numbers and Percentages of Roots With Different Extent of Root Shortening From Baseline to 6-Month Control
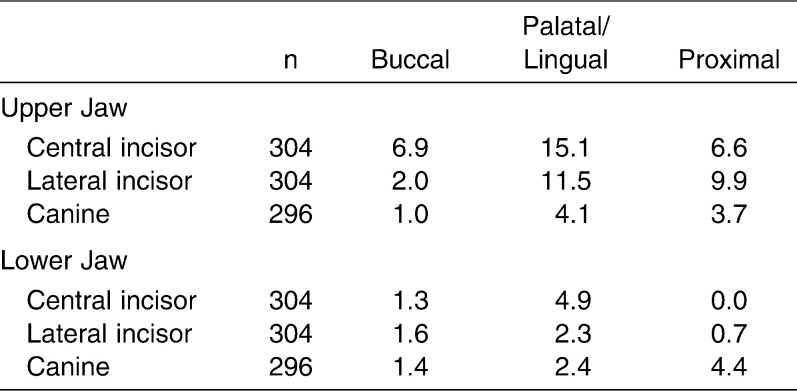
Surface resorption (slanted resorption) was most often found at palatal surfaces of upper central (15.1%) and lateral incisors (11.5%) (Table 3). Among patients, 57% had this type of resorption at ≥1 teeth and 11% at ≥4 teeth, regardless of the surface affected.
Table 2.
Percentage of Slanted Surface Resorption per Surface
Changes in root length per month during the two observation periods are shown in Table 4. Except for the lower lateral incisors, all teeth showed a greater extent of root shortening per month after the first 6 months. The difference was statistically significant only for the upper lateral incisor. Radiographs from a patient with severe root shortening of the incisors are shown in Figure 3.
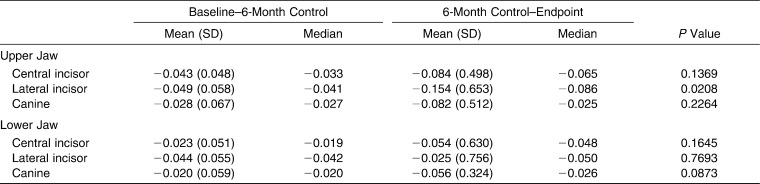
Table 3.
Root Shortening per Month (mm) During Two Observation Periods
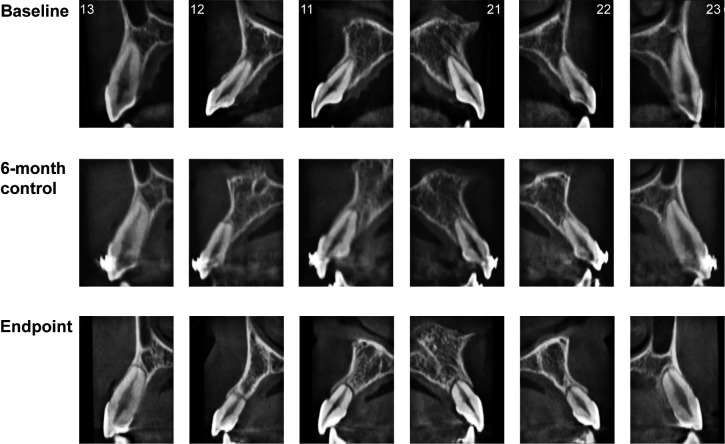
Figure 3.
A case with severe root shortening during the course of treatment. Teeth are numbered according to FDI.
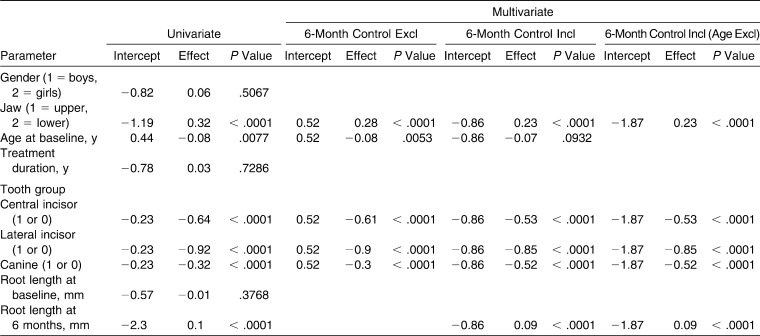
Univariate analysis (Table 5) revealed that age at baseline, jaw, tooth group, and root length at the 6-month control all had statistically significant effects on the extent of root shortening at endpoint. Upper jaw teeth had larger extents of root shortening than did lower jaw teeth, and anterior teeth were more affected than posterior ones. In older patients, the extent of root shortening was significantly greater than in younger ones. Neither gender nor root length at baseline or treatment time had any statistically significant effect on the extent of root shortening. When age at baseline, jaw, tooth group, and root length at the 6-month control were included in a multivariate analysis, age at baseline had no statistically significant effect on root shortening, but the other variables did.
Table 4.
Results of Univariate and Multivariate Analyses
DISCUSSION
Over many years, there has been an interest in evaluating the side effects of orthodontic treatment, particularly apical root resorption. Most studies have been conducted with the aid of intraoral radiography, which means that only root shortening and resorption on the mesial and distal aspects of the roots could be evaluated. Cone beam CT (CBCT) offers the possibility of assessing root surfaces not displayed on conventional radiographs and creating scenes similar to previous ones despite changes in tooth/root position. Therefore, it may be safe to assume that measurements of root length changes can be made reliably with CBCT. However, large differences are noted between CBCT units. For visualization of subtle anatomic structures, factors such as voxel size, scatter radiation, gray scale bit depth, and artifacts caused by metallic objects are important.24 More specifically, small voxel size and field of view (volume size) are needed. The smaller the voxel size, the higher the spatial resolution, and the smaller the field of view, the less noise from scatter radiation. Therefore, we used a CBCT unit with voxel size of 0.125 mm and a field of view of 6 × 6 cm.
Durack et al.25 investigated the accuracy of CBCT and intraoral radiography for the detection of simulated root resorption cavities. Their findings verified the shortcomings of intraoral radiography and showed that these were overcome by CBCT. When investigating the accuracy and reliability of root length measurements, Sherrard et al.26 found root lengths to be underestimated by an average of 2.6 mm in intraoral radiographs but by less than 0.3 mm on CBCT images. The error between replicate measurements was higher for intraoral radiography (0.57 mm) than for CBCT (0.30–0.36 mm), where the lowest error was found when the smallest available voxel size (0.2 mm) was used. With the CBCT unit used to measure root lengths, errors between repeated measurements ranged from 0.19–0.32 mm.21
Compared with most other studies on OIIRR, the present trial is based on a more homogeneous patient sample in terms of age and the reason for orthodontic treatment. Because of this and methodologic differences, it is difficult to make direct comparisons with previous studies on root resorption and percentage of affected teeth. Difficulties in making comparisons between studies of OIIRR were pointed out by Brezniak and coworkers.4 Our results related to teeth with severe root shortenings (>4 mm) are found within the range reported by Weltman et al.27 and confirm that upper incisors are more prone to root shortening than other teeth.28,29 In contrast to Janson et al.,30 we found the lateral incisor to be the most frequently affected tooth.
Almost 7% of patients had ≥1 tooth with root shortening ≥4 mm—a slightly higher percentage than that reported by Årtun et al.31 (5.3%). One reason for this difference may be that their study was limited to the front teeth, but one cannot rule out that it can depend on methodologic differences, namely, those between intraoral radiography and CBCT. Univariate analysis revealed that age at baseline, jaw, tooth group, and root length at 6 months had statistically significant effects on the extent of root shortening at endpoint. When age at baseline was included in the multivariate analysis, it had no significant effect on the extent of root shortening, in accordance with the findings of Årtun and coworkers.32 In contrast to the results of a meta-analysis of treatment-related factors in apical root resorption,33 we found no statistically significant effect of treatment duration on the extent of root shortening. Consistent with an overview by Harris,34 no differences in the incidence of root resorption between genders could be found, nor any effect of root length at baseline.
Slanted surface resorption was found to be relatively common at buccal and palatal root surfaces—an interesting finding because these surfaces are not displayed on intraoral radiographs, and because such resorption eventually may result in root shortening. In attempts to identify patients at risk for severe root shortening, slanted surface resorption could be a relevant research topic in future studies of OIIRR with CBCT.
CONCLUSIONS
Almost all patients and between 55% and 91% of teeth showed some degree of root shortening.
Nearly 7% of patients had one tooth or more with root shortening exceeding 4 mm, but none had more than three teeth affected to this degree. Few factors other than those already known had a statistically significant effect on the degree of root shortening.
Slanted root resorption was found in up to 15% of palatal root surfaces and could be evaluated only on tomographic images. A CBCT technique thus can provide more valid and accurate information about root resorption and may be of value in research.
REFERENCES
- 1.Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part I. The basic science aspects. Angle Orthod. 2002;72:175–179. doi: 10.1043/0003-3219(2002)072<0175:OIIRRP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Melsen B. Tissue reaction to orthodontic tooth movement—a new paradigm. Eur J Orthod. 2001;23:671–681. doi: 10.1093/ejo/23.6.671. [DOI] [PubMed] [Google Scholar]
- 3.Ottolengui R. The physiological and pathological resorption of tooth roots. Dental Items of Interest. 1914;36:322–362. [Google Scholar]
- 4.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment. Part 1. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:62–66. doi: 10.1016/0889-5406(93)70106-X. [DOI] [PubMed] [Google Scholar]
- 5.Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part II. The clinical aspects. Angle Orthod. 2002;72:180–184. doi: 10.1043/0003-3219(2002)072<0180:OIIRRP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Brezniak N, Goren S, Zoizner R, et al. The use of an individual jig in measuring tooth length changes. Angle Orthod. 2004;74:780–785. doi: 10.1043/0003-3219(2004)074<0780:TUOAIJ>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Gegler A, Fontanella V. In vitro evaluation of a method for obtaining periapical radiographs for diagnosis of external apical root resorption. Eur J Orthod. 2008;30:315–319. doi: 10.1093/ejo/cjm125. [DOI] [PubMed] [Google Scholar]
- 8.Brezniak N, Goren S, Zoizner R, et al. A comparison of three methods to accurately measure root length. Angle Orthod. 2004;74:786–791. doi: 10.1043/0003-3219(2004)074<0786:ACOTMT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 9.Brezniak N, Goren S, Zoizner R, et al. The accuracy of the cementoenamel junction identification on periapical films. Angle Orthod. 2004;74:496–500. doi: 10.1043/0003-3219(2004)074<0496:TAOTCJ>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Katona T. R. Flaws in root resorption assessment algorithms: role of tooth shape. Am J Orthod Dentofacial Orthop. 2006;130:698e619–e627. doi: 10.1016/j.ajodo.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 11.Katona T. R. The flaws in tooth root resorption assessment algorithms: the role of source position. Dentomaxillofac Radiol. 2007;36:311–316. doi: 10.1259/dmfr/52061649. [DOI] [PubMed] [Google Scholar]
- 12.Follin M. E, Lindvall A. M. Detection of lingual root resorptions in the intraoral radiographs: an experimental study. Swed Dent J. 2005;29:35–42. [PubMed] [Google Scholar]
- 13.Leach H. A, Ireland A. J, Whaites E. J. Radiographic diagnosis of root resorption in relation to orthodontics. Br Dent J. 2001;190:16–22. doi: 10.1038/sj.bdj.4800870. [DOI] [PubMed] [Google Scholar]
- 14.Mozzo P, Procacci C, Tacconi A, Martini P. T, Andreis I. A. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8:1558–1564. doi: 10.1007/s003300050586. [DOI] [PubMed] [Google Scholar]
- 15.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol. 1999;28:245–248. doi: 10.1038/sj/dmfr/4600448. [DOI] [PubMed] [Google Scholar]
- 16.Suomalainen A, Salo A, Robinson S, Peltola J. The 3DX multi image micro-CT device in clinical dental practice. Dentomaxillofac Radiol. 2007;36:80–85. doi: 10.1259/dmfr/30358216. [DOI] [PubMed] [Google Scholar]
- 17.Kau C. H, Richmond S, Palomo J. M, Hans M. G. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 18.Lofthag-Hansen S, Thilander-Klang A, Ekestubbe A, Helmrot E, Gröndahl K. Calculating effective dose on a cone beam computed tomography device: 3D Accuitomo and 3D Accuitomo FPD. Dentomaxillofac Radiol. 2008;37:72–79. doi: 10.1259/dmfr/60375385. [DOI] [PubMed] [Google Scholar]
- 19.Ludlow J. B, Davies-Ludlow L. E, Brooks S. L, Howerton W. B. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–226. doi: 10.1259/dmfr/14340323. [DOI] [PubMed] [Google Scholar]
- 20.Pauwels R, Beinsberger J, Collaert B, et al. Effective dose range for dental cone beam computed tomography scanners. E J Radiology. 2010;31 doi: 10.1016/j.ejrad.2010.11.028. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.Lund H, Gröndahl K, Gröndahl H. G. Cone beam computed tomography for assessment of root length and marginal bone level during orthodontic treatment. Angle Orthod. 2010;80:466–473. doi: 10.2319/072909-427.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod. 1982;82:487–491. doi: 10.1016/0002-9416(82)90317-7. [DOI] [PubMed] [Google Scholar]
- 23.Levander E, Malmgren O, Eliasson S. R. Evaluation of root resorption in relation to two orthodontic treatment regimes: a clinical experimental study. E J Orthod. 1994;16:223–228. doi: 10.1093/ejo/16.3.223. [DOI] [PubMed] [Google Scholar]
- 24.Molen A. D. Considerations in the use of cone-beam computed tomography for buccal bone measurements. Am J Orthod Dentofacial Orthop. 2010;137:130–135. doi: 10.1016/j.ajodo.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 25.Durack C, Patel S, Davies J, Wilson R, Mannocci F. Diagnostic accuracy of small volume cone beam computed tomography and intraoral periapical radiography for the detection of simulated external inflammatory root resorption. International Endodontic Journal. 2011;44:136–147. doi: 10.1111/j.1365-2591.2010.01819.x. [DOI] [PubMed] [Google Scholar]
- 26.Sherrard J. F, Rossouw P. E, Benson B. W, Carrillo R, Buschang P. H. Accuracy and reliability of tooth and root lengths measured on cone-beam computed tomographs. Am J Orthod Dentofacial Orthop. 2010;137(4 Suppl):S100–S108. doi: 10.1016/j.ajodo.2009.03.040. [DOI] [PubMed] [Google Scholar]
- 27.Weltman B, Vig K. W. L, Fields H. W, Shanker S, Kaizar E. E. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 28.Blake M, Woodside D. G, Pharoah M. J. A radiographic comparison of apical root resorption after orthodontic treatment with the edgewise and Speed appliances. Am J Orthod Dentofacial Orthop. 1995;108:76–84. doi: 10.1016/s0889-5406(95)70069-2. [DOI] [PubMed] [Google Scholar]
- 29.Sameshima G. T, Sinclair P. M. Predicting and preventing root resorption. Part I. Diagnostic factors. Am J Orthod Dentofacial Orthop. 2001;119:505–510. doi: 10.1067/mod.2001.113409. [DOI] [PubMed] [Google Scholar]
- 30.Janson G. R. P, de Luca Canto G, Martins D. R, Henriques J. F. C, de Freitas M. R. A radiographic comparison of apical root resorption after orthodontic treatment with 3 different fixed appliance techniques. Am J Orthod Dentofacial Orthop. 2000;118:262–273. doi: 10.1067/mod.2000.99136. [DOI] [PubMed] [Google Scholar]
- 31.Årtun J, Smale I, Behbehani F, Doppel D, Van't Hof M, Kuijpers-Jagtman A. M. Apical root resorption six and 12 months after initiation of fixed orthodontic appliance therapy. Angle Orthod. 2005;75:919–926. doi: 10.1043/0003-3219(2005)75[919:ARRSAM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Årtun J, Van't Hullenaar R, Doppel D, Kuijpers-Jagtman A. M. Identification of orthodontic patients at risk of severe apical root resorption. Am J Orthod Dentofacial Orthop. 2009;135:448–455. doi: 10.1016/j.ajodo.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 33.Segal G. R, Schiffman P. H, Tuncay O. C. Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 2004;7:71–78. doi: 10.1111/j.1601-6343.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- 34.Harris E. F. Root resorption during orthodontic therapy. Semin Orthod. 2000;6:183–194. [Google Scholar]