Abstract
Objective:
To test the hypothesis that there were no differences in the skeletal and dental effects of banded vs bonded expanders when evaluated using cone beam computed tomography (CBCT).
Materials and Methods:
The experimental sample consisted of 23 patients: 13 (seven male, six female; mean age = 12.6 ±1.8 years) and 10 (five male, five female; mean age = 13.5 ± 2.1 years) treated with banded and bonded maxillary expanders, respectively. CBCT images were taken at T1 (pretreatment) and T2 (immediately after expansion) to evaluate the changes in the naso-maxillary complex. Relationships between and within groups were assessed using analysis of variance. If the results were significant, post hoc t-tests were used to determine where the significant differences occurred.
Results:
Regardless of the appliance, the maxilla was expanded equally at the level of the canines and first and second premolars. At the level of the first molars, more dental tipping and alveolar bending were evident in the banded expander group. Both appliances equally increased the skeletal and soft tissue dimensions of the nasal cavity and maxillary sinus volume. The posterior airway volume did not significantly change with either method of expansion.
Conclusions:
The hypothesis was rejected. Both appliances expanded the maxilla similarly. However, in the banded group, more dental tipping and alveolar bending occurred at the level of the first molars. Maxillary expansion affected the palatal suture and demonstrated anterior and posterior skeletal widening of the nasal cavity, with corresponding soft tissue changes and increased airway volume.
Keywords: Maxillary expansion, Maxillary sinus, Nasal changes, Cone beam computed tomography, Bonded Hyrax, Banded Hyrax
INTRODUCTION
Rapid maxillary expansion (RME) has been commonly used to increase the transverse width of the maxillary arch, to correct crossbites, to reduce dental crowding, and to create broader smiles.1–7 Appliances used for maxillary expansion have been shown to produce both skeletal and dental effects.2–4,7–11 Skeletal effects include maxillary sutural expansion, widening of the nasal cavity, and reformation of the maxillary sinus.4,7,8
Since the time during which RMEs were popularized by Haas,2–4 variations of the original design have been created to treat transverse discrepancies. Two of the most popular designs to date are the bonded and banded rapid palatal expanders.12 Side effects of maxillary expansion include downward displacement of the maxilla, dental extrusion, lateral rotations of the maxillary segment, opening of the bite, and gingival recession.11,13
Dental tipping also occurs during maxillary expansion, which leads to subsequent alveolar bone changes.11 Nasal width increase has been reported as a side effect of orthopedic expansion.4,10 Bonded expanders have been used to counteract the negative side effects of expansion, such as increased dental tipping and dentoalveolar bending.14–18 Banded expanders are usually preferred because of their more hygienic structure and in relation to patient comfort.19 More recently, it has been suggested11 that expanders anchored in bone with temporary anchorage devices may improve skeletal expansion and reduce dental tipping. However, this was not the case in the study of Lagravere et al.,11 who found little difference in the amount of dental tipping and skeletal expansion between the banded hyrax and bone-anchored expander.
Many studies have shown the effectiveness of maxillary expansion on skeletal and dental structures. Prior research8,20–23 utilized dental casts, two-dimensional lateral and posteroanterior cephalograms, and occlusal radiographs to assess the effect of palatal expanders. Although these studies were able to measure changes in the facial complex, a more accurate evaluation of the dento-skeletal changes is now available. Garrett et al.1 utilized cone beam computed tomography (CBCT) to quantitatively evaluate the effects of two types of Hyrax expanders. In the past, the effects of maxillary expansion on nasal respiration were measured utilizing rhinometry and linear measurements of the maxillary sinus on high-radiation CT scans.20,21
With the utilization of CBCT technology it is possible to measure the maxillary sinus volume and anterior and posterior airway and to quantify craniofacial structural changes in three dimensions with minimal distortion and lower radiation doses than are required for conventional CT scans.18,24–28
The purpose of this study was to assess three dimensionally, with the aid of ICAT technology (Imaging Sciences International, Hatfield, Pa), the skeletal, dental, and volumetric changes of the maxillary sinus that occur with the banded hyrax expander vs the bonded hyrax expander.
MATERIALS AND METHODS
Sample Selection
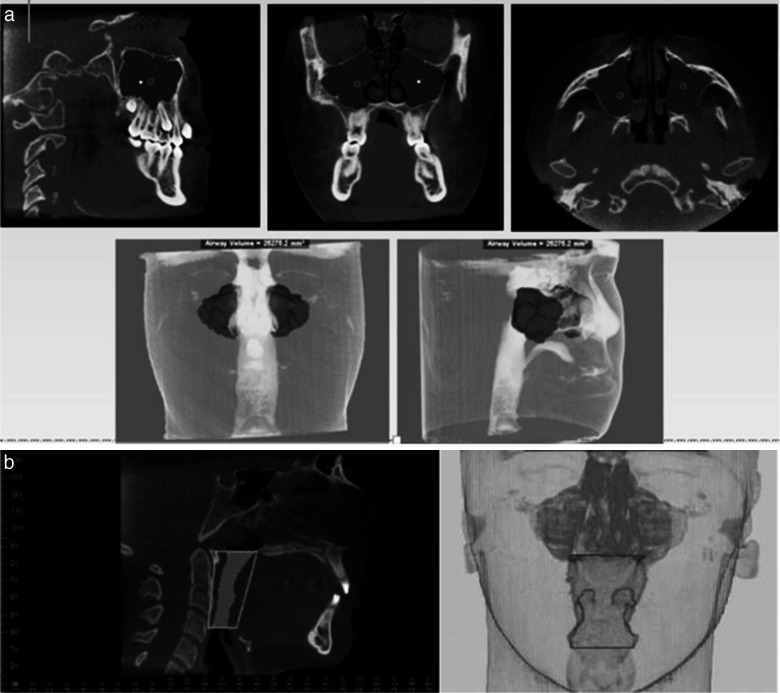
The sample consisted of 23 prospectively treated patients. Thirteen subjects, seven males and six females with a mean age of 12.6 ± 1.8 years, were fitted with banded expanders, and 10 subjects, five males and five females with a mean age of 13.5 ± 2.1 years, were treated with bonded expanders. All subjects had a cervical vertebra maturation at stage 3 or below, indicating good growth potential (Figure 1a,b). Subjects were randomly assigned to either group. Criteria for enrollment in this study were constricted maxillary arches with or without crossbites and full permanent dentitions. Patients with any sign of fluid accumulation in the maxillary sinus CBCT image were excluded from this study. Each group had the same expansion activation protocol and retention time. The expansion time was 4–6 weeks, with 6–10 mm of activation. The retention time was 6 months. To prevent bias, the researcher who evaluated the CBCT had no previous contact with any of the participating subjects. In accordance with federal regulations, this study was reviewed by the University of Detroit Mercy Institutional Review Board, and patient consent was also received.
Figure 1.
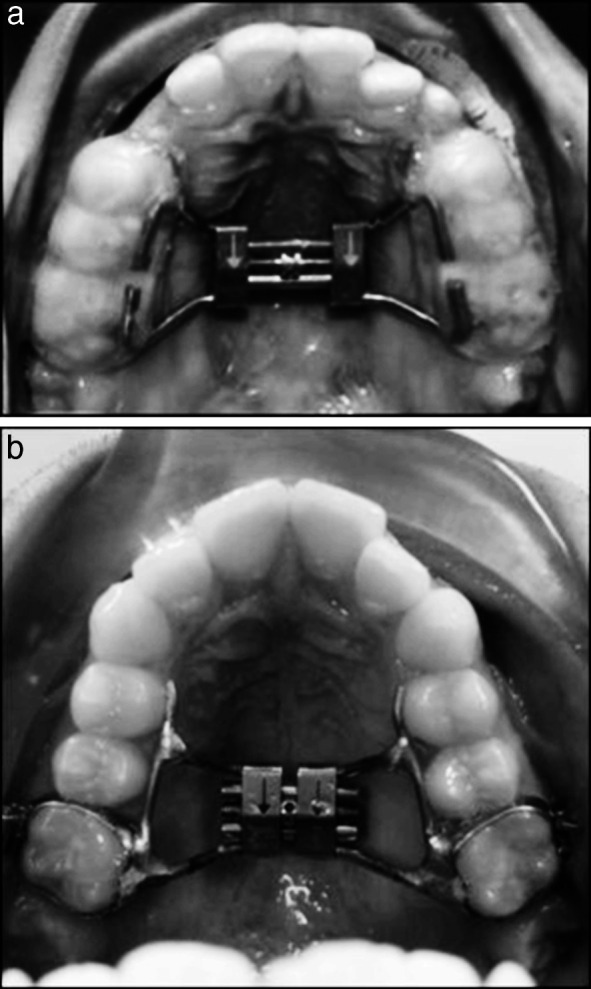
(a) Bonded expander. (b) Banded expander.
CBCT scans were taken at T1 (prior to placement of appliance) and T2 (immediately after appliance removal). DICOM images (Digital Imaging and Communications in Medicine) were assessed utilizing Dolphin Imaging software version 11 (Patterson, Chatsworth, Calif). Linear, angular, and volumetric data were collected using the same software. All CBCT measurements were standardized at the level of the first molar furcation in a sagittal, coronal, and axial dimension (Figure 2). Comparisons of data collected between T1 and T2 were calculated as described in the following sections.
Figure 2.

Sagittal, coronal, and axial slices superimposed on the furcation of the first molar.
Palatal Maxillary Width/Buccal Maxillary Width Changes
Palatal maxillary width (PMW) and buccal maxillary width (BMW) were measured as the distance between the buccal and palatal cortical plates of the maxillary first molars (PMW/BMW, M1), second premolars (PMW/BMW, P2), first premolars (PMW/BMW, P1), and canines (PMW/BMW, C) (Figure 3).
Figure 3.
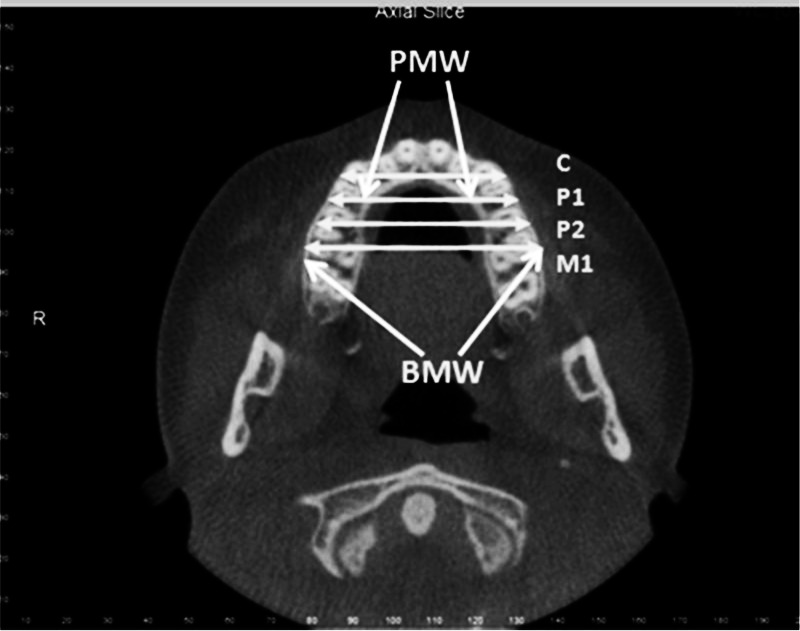
Linear measurements of the palatal maxillary width (PMW) and the buccal maxillary width (BMW) at C, P1, P2, and M1.
Dental/Alveolar Tipping
The alveolar tipping was measured by the angles formed by lines traced from the buccal and lingual cemento-enamel junctions of the maxillary first molars to the crista galli vertex (X) (Figure 4).
Figure 4.
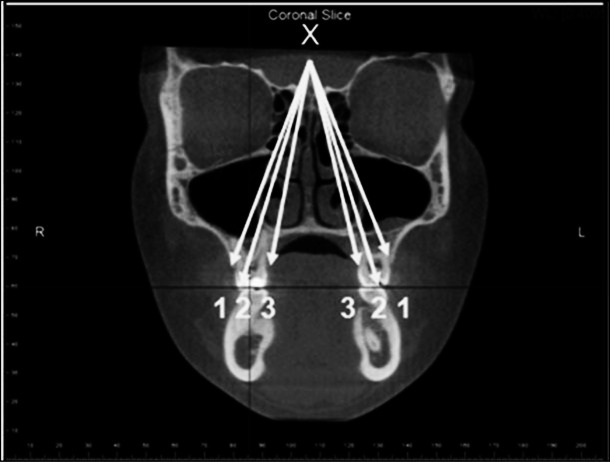
Angular measurements of dental tipping. Angle 1: Buccal CEJ of M1R-X-buccal CEJ of M1L (BCEJ-X). Angle 2: Buccal cusp tip of M1R-X-palatal CEJ of M1L (Bcusp-X). Angle 3: Palatal CEJ of M1R-X-palatal CEJ of M1L (PCEJ-X).
Posterior Nasal Width Changes
Posterior nasal width (PNW) was assessed from a coronal cut of the CBCT image; the widest superior transverse portion of the nasal aperture was established as the PNW and the lowest as the posterior nasal floor (PNF) (Figure 5a).
Figure 5.
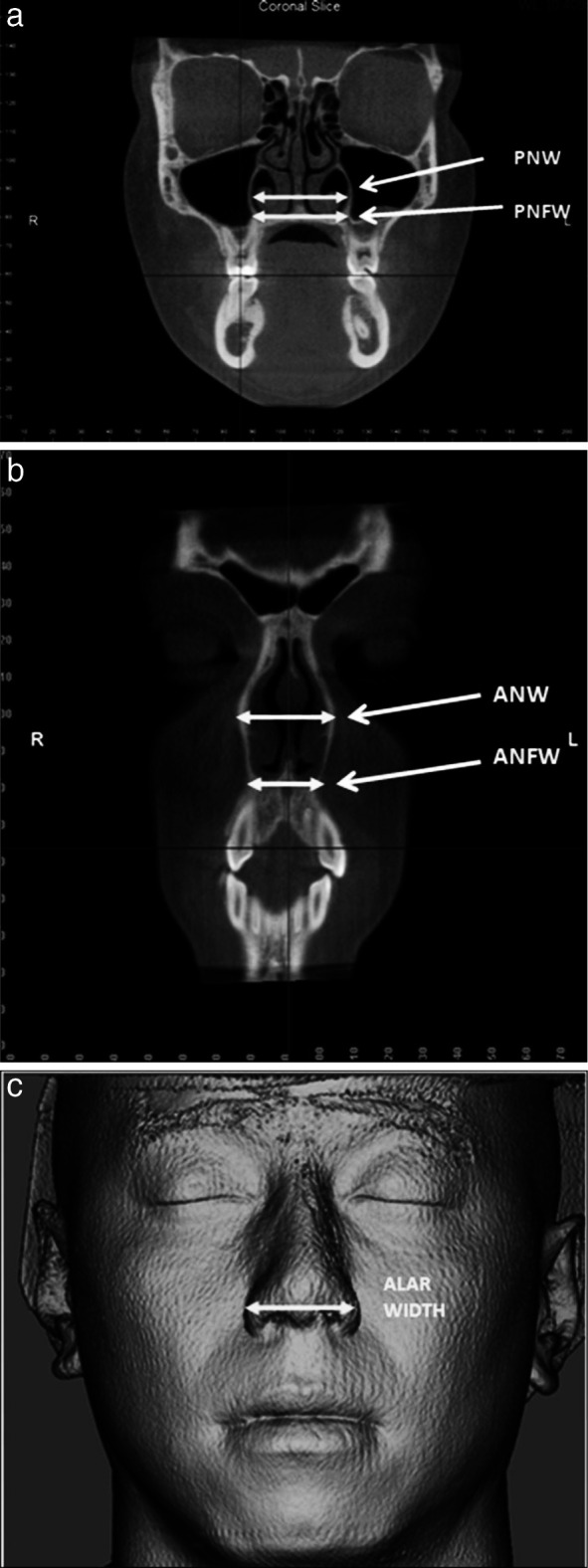
(a) Linear measurements of the posterior nasal width (PNW) and nasal floor width (PNFW). (b) Linear measurements of the anterior nasal width (ANW) and anterior nasal floor width (ANFW). (c) Linear measurement of the soft tissue alar width.
Anterior Nasal Width Changes
Anterior nasal width (ANW) was measured by locating an axial slice that bisected the maxillary canines. Horizontal measurement was taken from both the deepest concavity of the lateral walls of the nasal cavity and at the transitional concavity from the lateral wall to the floor of nose. The anterior nasal floor width is designated “ANF.” The soft tissue nasal expansion was measured from the most lateral borders of the ala (Figure 5b,c).
Maxillary Width Changes
The deepest point in the concavity of the posterior maxilla was identified on the right and left sides. A line connecting these two points measured maxillary width (MaxW) (Figure 6).
Figure 6.
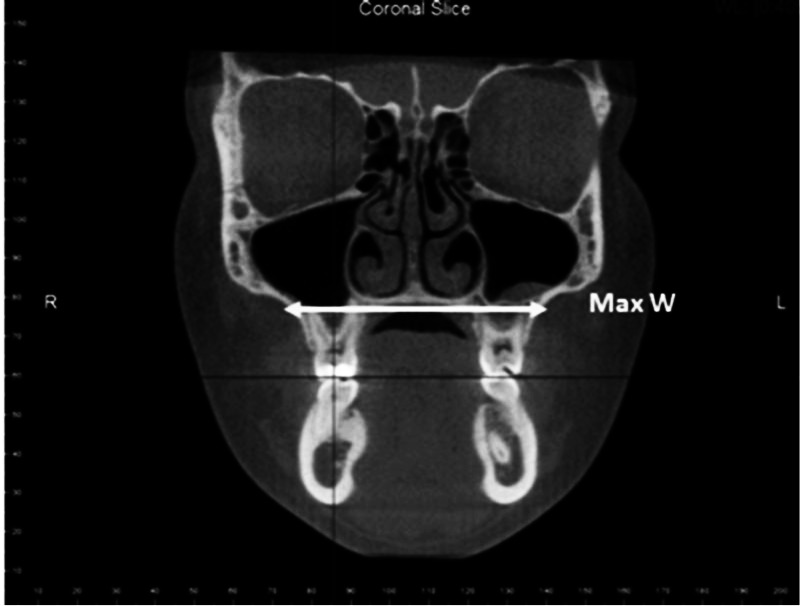
Linear measurement of the maxillary width (MaxW).
Maxillary Sinus Volume
The maxillary sinus was divided in an axial, coronal, and sagittal slice at the furcation of the first molar. The maxillary sinus volume (MSV) was measured at its greatest width in the coronal and sagittal slices. The widest area of the sinus in the axial slice was consistent with the first view of the body of the mandible in multiple axial slices (Figure 7a).
Figure 7.
(a) Volumetric measurement of the maxillary sinus (MSV). (b) Limits of the posterior airway.
Posterior Airway Analysis
The posterior airway was measured from the most superior portion of the posterior nasal spine to the epiglottis (Figure 7b). Posterior airway analysis is designated “PAWA.”
Statistical Analysis
Analysis of variance (ANOVA) was used to evaluate the effects of the expansion devices. Fifteen different variables were tested, setting the significance level for each statistic at α = .05/18, or .003. When ANOVA results were significant (P ≤ .003), post hoc t-tests were used to determine the individual differences. To test for landmark accuracy location and measurements, ICAT images were evaluated by one operator at two different time intervals within 1 month on 10 randomly selected images. The Pearson's R-test demonstrated nearly 100% reliability (range 0.993–1.000) for the individual measurements recorded with a minimal margin of error.
RESULTS
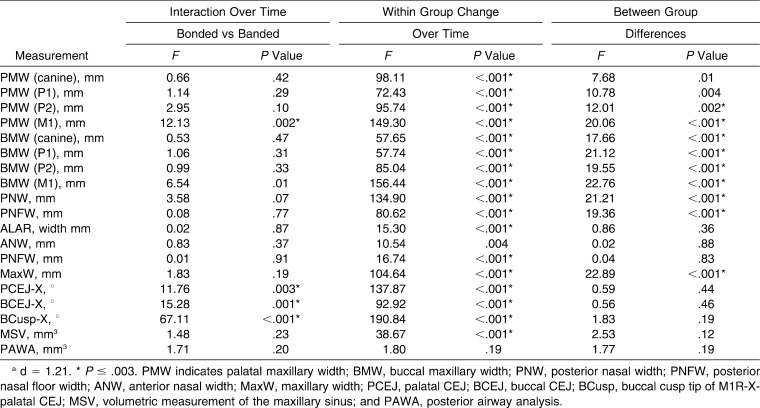
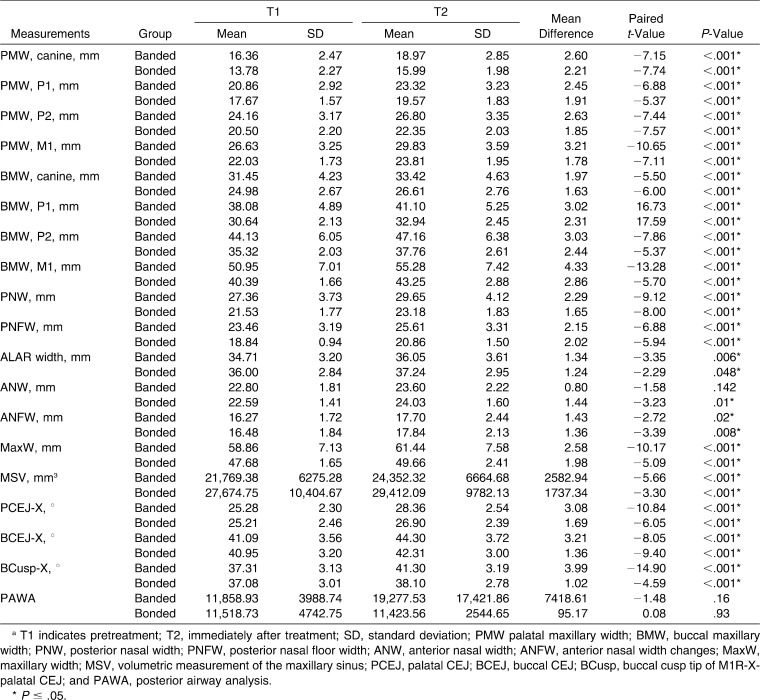
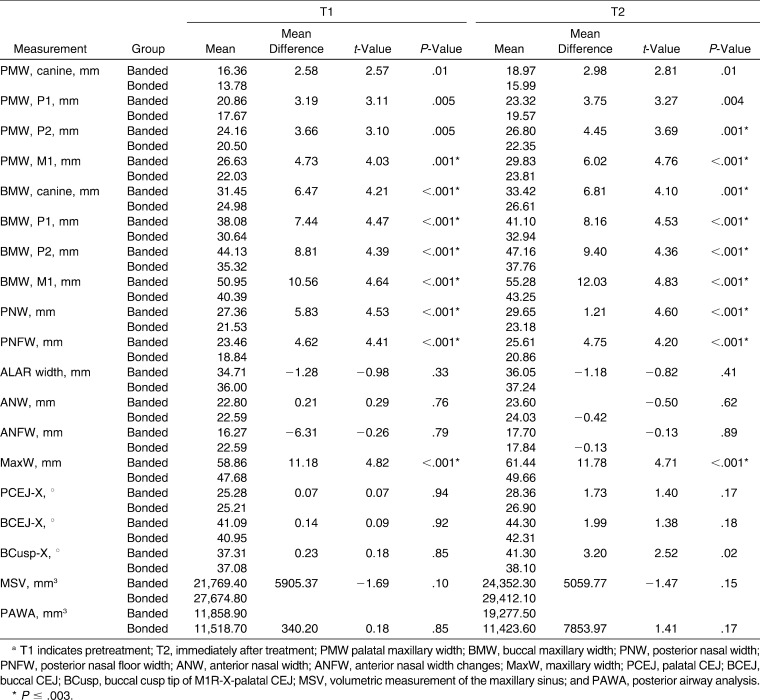
Changes within and between the groups are listed in Tables 1 through 3. At the level of the canine and first and second premolars, the two groups showed a significant increase in PMW, and there were no statistically significant differences between the groups (Figure 8). However, at the level of the first molars (PMW, M1), there was a significant difference between the two groups. The banded group had a mean PMW increase of 3.2 mm (P < .001), while the bonded group increased only 1.78 mm (P < .001). BMW at the level of the canine, first and second premolars, and first molars increased similarly in both groups over time (Figure 9). Significant tipping was observed with both types of expanders. However, the tipping was more pronounced in the banded expander group (P < .001). The two groups showed significant and similar increases in nasal (PNW, PNFW, ANW, ANFW) alar width (P < .001). The MSV of the two groups changed similarly over time. The banded group had a mean volume increase of 2582.94 mm3 (P < .001), or 11%. The bonded group increased by 1737.34 mm3 (P < .001), or 6%. The posterior airway showed no statistical difference in volume within or between the two groups.
Table 1.
Analysis of Variance (ANOVA) Comparing the Differences Between and Within Bonded and Banded Groupsa
Table 2.
Linear, Angular, and Volumetric Measurements Within Groups Over Timea
Table 3.
Linear, Angular, and Volumetric Changes Between Groups Over Timea
Figure 8.
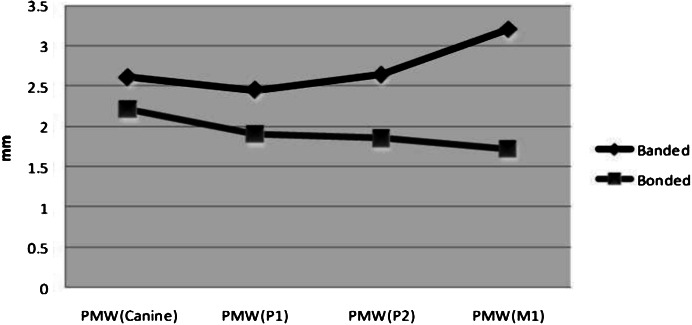
Comparison of linear changes of the palatal maxillary width (PMW) between banded and bonded expanders.
Figure 9.
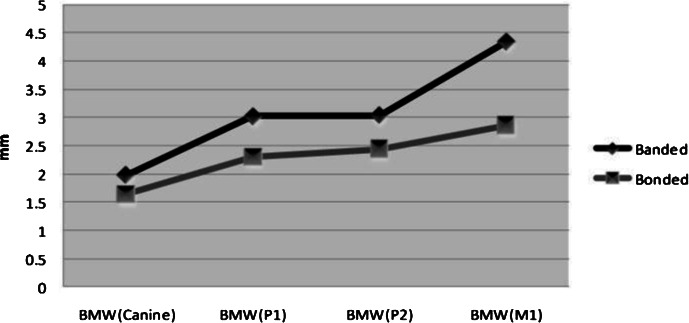
Comparison of linear changes of the buccal maxillary width (BMW) between banded and bonded expanders.
DISCUSSION
The results obtained from this three-dimensional study were similar to those of previous research2,29–32 demonstrating sutural opening in a triangular pattern, with the wide base at the anterior portion of the maxilla. The decrease in opening of the posterior part of the maxillary suture was attributed to the interlocking of the pyramidal processes of the palatine bone along with immobilization of the medial and lateral pterygoid plates of the sphenoid bone.1,30 As a result of a decrease in posterior sutural opening, dental tipping and alveolar bending occurred.14 Garrett et al.1 showed that alveolar bending accounted for 13% of total maxillary expansion, compared to 6% at the first premolar area.
Current literature indicates that expansion produces an average of 50% skeletal and 50% dental movements.1 In the present study, the banded expander demonstrated an increase in alveolar bending and dental tipping at the level of the first molar, more than in the bonded expander (Figure 10). This effect, combined with the lack of increase in maxillary width, attests to the failure of posterior sutural opening. These results are contrary to the findings of Asanza et al.,16 who showed no difference in the two appliances except for better vertical dimensional control with the bonded expander. The disparity in findings may be related to the differences in age and sample size of the two studies as well as to the methods of landmark locations and measurements in the two-dimensional study of Asanza et al.16 vs this CBCT research.
Figure 10.
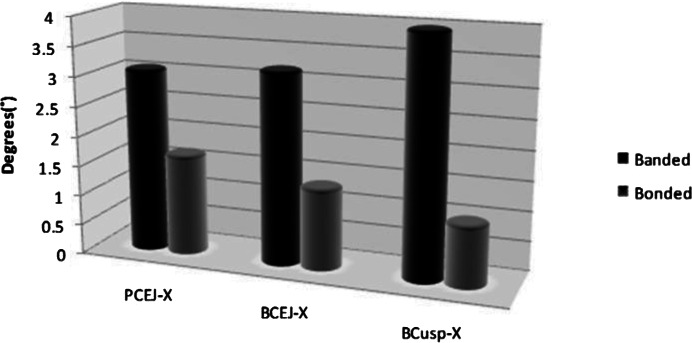
Comparison of maxillary first molar tipping between the banded and bonded expanders.
Skeletal expansion is not just limited to the maxilla during RME. Surrounding skeletal structures such as the nasal aperture and maxillary sinus are modified during maxillary expansion treatment. In this study, the average nasal width change was slightly smaller than the 3.15 mm change reported by Haas4 in a radiographic study. Coincidentally, he also showed that in chronic mouth breathers, increased nasal respiration occurred concomitantly with widening of the maxilla and the nose. In this study, the nasal width increases were determined to be significant for the nasal floor, anterior/posterior nasal aperture, and the soft tissue. The bony nasal width increase was similar to the findings of Garrett et al.,1 who determined expansion of the nasal floor (NWL) to be 1.59 mm and that of the lateral wall (NWH) 1.89 mm. No previous studies have related anterior to posterior nasal bony changes, which is now possible as a result of CBCT imaging.
Palatal expansion results in not only a posterior, but also an anterior, widening of the nasal cavity. This skeletal nasal widening could have a significant effect on nasal respiration, nasal resistance, and soft tissue nasal changes.10,33,34 In a systematic review of the literature, Baratieri et al.35 reported moderate evidence that changes in the airway after RME are moderately stable in the long term. The changes in nasal floor and maxillary width observed in this study are similar to those of Berger et al.,10 who saw similar increases in nasal floor width and maxillary width using exclusively bonded expanders. The increase in soft tissue nasal width is a significant finding in the present study. The skeletal nasal width increases at a 1∶1 ratio with the soft tissue response. The increase in MSV found in this investigation has not been previously reported. Garrett et al.1 showed a decrease in linear dimension of the maxillary sinus due to an increased width of the nasal cavity. The increase in MSV may be due to skeletal reorganization postexpansion or to generalized growth. This finding is significant since an increase in MSV may lead to increased nasal respiration and decreased nasal resistance. Further studies of the maxillary sinus complex will be needed to confirm this finding. No statistical difference was found within or between the two groups when the posterior airway volume was observed. Although statistically the banded group showed a larger increase in volume, the standard deviation is very large, resulting in no statistical difference between the groups. Unfortunately, there are no data evaluating the relationship between expansion and airway volume with which to compare the results. There is also a lack of agreement in the landmark limits for the posterior airway.33,34 Further studies are needed in this field.
CONCLUSIONS
Both expanders increased the transverse dimension of the skeletal and soft tissue nasomaxillary complex equally. However, more dental tipping was observed with the banded expander.
Maxillary sinus volume increased between 6% and 11% after expansion. No statistical difference was found in the posterior airway volume.
CBCT can be used reliably to assess skeletal and dental changes associated with RME.
REFERENCES
- 1.Garrett B. J, Caruso J. M, Rungcharassaeng K, Farrage J. R, Kim J. S, Taylor G. D. Skeletal effects to the maxilla after rapid maxillary expansion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2008;134:8.e1–8.e11. doi: 10.1016/j.ajodo.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Haas A. J. The treatment of maxillary deficiency by opening of the mid-palatal suture. Angle Orthod. 1965;65:200–217. doi: 10.1043/0003-3219(1965)035<0200:TTOMDB>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Haas A. J. Long term posttreatment evaluation of rapid palatal expansion. Angle Orthod. 1980;50:189–217. doi: 10.1043/0003-3219(1980)050<0189:LPEORP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.Haas A. J. Rapid expansion of the maxillary dental arch and nasal cavity by opening the mid palatal suture. Angle Orthod. 1961;31:73–89. [Google Scholar]
- 5.Isaacson R. J, Wood J. L, Ingram A. H. Forces produced by rapid maxillary expansion. Part I. Design of the force measuring system. Angle Orthod. 1964;34:256–260. [Google Scholar]
- 6.Isaacson R. J, Ingram A. H. Forces produced by rapid maxillary expansion. Part II. Forces present during treatment. Angle Orthod. 1964;34:261–269. doi: 10.1043/0003-3219(1965)035<0178:FPBRME>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Starnbach H, Bayne D, Cleall J, Subtelny J. D. Facioskeletal and dental changes resulting from rapid maxillary expansion. Angle Orthod. 1966;36:152–164. doi: 10.1043/0003-3219(1966)036<0152:FADCRF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Chung C. H, Font B. Skeletal and dental changes in the sagittal, vertical, and transverse dimensions after rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2004;126:569–575. doi: 10.1016/j.ajodo.2003.10.035. [DOI] [PubMed] [Google Scholar]
- 9.Phatouros A, Goonewardene M. S. Morphologic changes of the palate after rapid maxillary expansion: a 3-dimensional computed tomography evaluation. Am J Orthod Dentofacial Orthop. 2008;1:117–124. doi: 10.1016/j.ajodo.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Berger J. L, Pangrazio-Kulbersh V, Thomas B. W, Kaczynski R. Photographic analysis of facial changes associated with maxillary expansion. Am J Orthod Dentofacial Orthop. 1999;116:563–571. doi: 10.1016/s0889-5406(99)70190-3. [DOI] [PubMed] [Google Scholar]
- 11.Lagravere M, Carey J, Heo G, et al. Transverse, vertical and anteroposterior changes from bone-anchored maxillary expansion vs. traditional rapid maxillary expansion: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2010;137:e304–e312. doi: 10.1016/j.ajodo.2009.09.016. [DOI] [PubMed] [Google Scholar]
- 12.McNamara J. A, Jr, Brudon W. L. Orthodontic and Orthopedic Treatment in the Mixed Dentition. Ann Arbor, Mich: Needham Press; 1993. [Google Scholar]
- 13.Ballanti F, Lione R, Fanucci E, Franchi L, Baccetti T, Cozza P. Immediate and post-retention effects of rapid maxillary expansion investigated by computed tomography in growing patients. Angle Orthod. 2009;79:24–29. doi: 10.2319/012008-35.1. [DOI] [PubMed] [Google Scholar]
- 14.Rungcharassaeng K, Caruso J. M, Kan J. Y. K, Kim J, Taylor G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am J Orthod Dentofacial Orthop. 2007;132:428.e1–428.e8. doi: 10.1016/j.ajodo.2007.02.052. [DOI] [PubMed] [Google Scholar]
- 15.Geran R. G, McNamara J. A, Baccetti T, Franchi L, Shapiro L. M. A prospective long-term study on the effects of rapid maxillary expansion in the early mixed dentition. Am J Orthod Dentofacial Orthop. 2006;129:631–640. doi: 10.1016/j.ajodo.2005.01.020. [DOI] [PubMed] [Google Scholar]
- 16.Asanza S, Cisneros G. J, Nieberg L. G. Comparison of hyrax and bonded expansion appliances. Angle Orthod. 1997;67:15–22. doi: 10.1043/0003-3219(1997)067<0015:COHABE>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Berger J. L, Pangrazio-Kulbersh V, Borgula T, Kaczynski R. Stability of orthopedic and surgically assisted rapid palatal expansion over time. Am J Orthod Dentofacial Orthop. 1998;114:638–645. doi: 10.1016/s0889-5406(98)70195-7. [DOI] [PubMed] [Google Scholar]
- 18.Sun Z, Smith T, Kortam S, Kim D. G, Tee B. C, Fields H. Effect of bone thickness on alveolar bone height measurements from cone-beam computed tomography images. Am J Orthod Dentofacial Orthop. 2011;139:e117–e127. doi: 10.1016/j.ajodo.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 19.Garib D. G, Henriques J. F. C, Janson G, Freitas M. R, Coelho R. A. Rapid maxillary expansion-tooth tissue-borne versus tooth-borne expanders: a computed tomography evaluation of dentoskeletal effects. Angle Orthod. 2005;75:548–557. doi: 10.1043/0003-3219(2005)75[548:RMETVT]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Ladner P. T, Muhl Z. F. Changes with orthodontic treatment when maxillary expansion is a primary goal. Am J Orthod Dentofacial Orthop. 1995;108:184–193. doi: 10.1016/s0889-5406(95)70082-x. [DOI] [PubMed] [Google Scholar]
- 21.Da Silva Filho O. G, Montes L. A, Torelly L. F. Rapid maxillary expansion in the deciduous and mixed dentition evaluated through postero-anterior cephalometric analysis. Am J Orthod Dentofacial Orthop. 1995;107:268–275. doi: 10.1016/s0889-5406(95)70142-7. [DOI] [PubMed] [Google Scholar]
- 22.Spillane L. M, McNamara J. A. Maxillary adaptation to expansion in the mixed dentition. Semin Orthod. 1995;1:176–187. doi: 10.1016/s1073-8746(95)80021-2. [DOI] [PubMed] [Google Scholar]
- 23.Brieden C. M, Pangrazio-Kulbersh V, Kulbersh R. Maxillary skeletal and dental changes with Frankel appliance therapy. Angle Orthod. 1984;54:226–232. doi: 10.1043/0003-3219(1984)054<0226:MSADCW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Jun B. C, Song S. W, Park C. S, Lee D. H, Cho K. J, Cho J. H. The analysis of maxillary sinus aeration according to aging process; volume assessment by 3-dimensional reconstruction by high resolutional CT scanning. Otolaryngol Head Neck Surg. 2005;132:429–434. doi: 10.1016/j.otohns.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 25.Kim H. Y, Kim M. B, Dhong H. J, et al. Changes of maxillary sinus volume and bony thickness of the paranasal sinuses in longstanding pediatric chronic rhinosinusitis. Int J Pediatr Otorhinolaryngol. 2008;72:103–108. doi: 10.1016/j.ijporl.2007.09.018. [DOI] [PubMed] [Google Scholar]
- 26.Scarfe W. C, Farman A. G, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006;72:75–80. [PubMed] [Google Scholar]
- 27.Oliveria N. L, Da Silveira A. C, Kusnoto B, Viana G. Three-dimensional assessment of morphologic changes in the maxilla: a comparison of 2 kinds of palatal expanders. Am J Orthod Dentofacial Orthop. 2004;126:354–362. doi: 10.1016/j.ajodo.2003.07.008. [DOI] [PubMed] [Google Scholar]
- 28.Kau C. H, Richmond S, Palomo J. M, Hans M. G. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 29.Krebs A. Mid-palatal expansion studied by the implant method over a seven-year period. Trans Eur Orthod Soc. 1964;40:131–142. [PubMed] [Google Scholar]
- 30.Wertz R. A. Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod. 1970;58:41–66. doi: 10.1016/0002-9416(70)90127-2. [DOI] [PubMed] [Google Scholar]
- 31.Habersack K, Karoglan A, Sommer B, Benner K. U. High-resolution multislice computerized tomography with multiplanar and 3-dimensional reformation imaging in rapid palatal expansion. Am J Orthod Dentofacial Orthop. 2007;131:776–781. doi: 10.1016/j.ajodo.2005.09.030. [DOI] [PubMed] [Google Scholar]
- 32.Abramson Z, Susarla S, Tagoni J, Kaban L. Three-dimensional computed tomographic analysis of airway anatomy. J Oral Maxillofac Surg. 2010;68:363–371. doi: 10.1016/j.joms.2009.09.086. [DOI] [PubMed] [Google Scholar]
- 33.De Felippe N. L. O, Da Silveira A. C, Viana G, Kusnoto B, Smith B, Evans C. A. Relationship between rapid maxillary expansion and nasal cavity size and airway resistance: short and long term effects. Am J Orthod Dentofacial Orthop. 2008;134:370–382. doi: 10.1016/j.ajodo.2006.10.034. [DOI] [PubMed] [Google Scholar]
- 34.Zhao Y, Nguyen M, Gohl E, Mah J. K, Sameshima G, Enciso R. Oropharyngeal airway changes after rapid palatal expansion evaluated with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;137:S71–S78. doi: 10.1016/j.ajodo.2008.08.026. [DOI] [PubMed] [Google Scholar]
- 35.Baratieri C, Alves M, Souza M, Araujo M, Maia L. Does rapid maxillary expansion have long-term effects on airway dimensions and breathing? Am J Orthod Dentofacial Orthop. 2011;140:146–156. doi: 10.1016/j.ajodo.2011.02.019. [DOI] [PubMed] [Google Scholar]