Abstract
Objective
Branched-chain amino acids (BCAAs) are essential AAs which are widely used as antioxidants in patients with liver and kidney dysfunction. However, BCAAs are strongly correlated with insulin resistance (IR) and diabetes. This study aimed to evaluate the relationship among BCAAs, oxidative stress, and type 2 diabetes mellitus (T2DM) in a Chinese population.
Methods
Anthropometric and biochemical examinations were performed in 816 individuals who participated in the Huai’an Diabetes Prevention Program. Serum BCAAs concentrations were measured by hydrophilic interaction chromatography-tandem mass spectrometric method. Oxidative stress was evaluated by malondialdehyde (MDA) as an index of lipid peroxidation and the superoxide dismutase (SOD) activity.
Results
A total of 816 participants were divided into three groups: normal glucose metabolism (NGM), prediabetes, and newly-diagnosed diabetes mellitus (NDM). Subjects in NDM group show higher MDA and lower SOD levels than subjects in other groups. L-Val levels positively correlated with MDA levels and negatively with SOD in NDM groups. After adjusting for T2DM risk factors, high L-Val levels were significantly associated with higher BMI, WC, FPG, increased LnTG and decreased HDL-C. L-Val was also independently associated with NDM (OR 1.06, 95% CI 1.02–1.10; P = 0.005). Furthermore, the odds ratios for NDM among participants with high L-Val (≥35.25μg/mL) levels showed a 2.25-fold (95% CI 1.11–4.57; P = 0.024) increase compared to participants with low L-Val (<27.26 μg/mL) levels after adjusting for MDA and confounding factors.
Conclusion
High serum L-Val levels are independently associated with oxidative stress, thus promoting IR and NDM. Further study should be done to clarify the mechanism.
Keywords: branched chain amino acids, oxidative stress, new diagnosed type 2 diabetes mellitus, hydrophilic interaction chromatography-tandem mass spectrometric method
Introduction
Diabetes is a metabolic disorder characterised by chronic hyperglycaemia, affecting carbohydrate, fat, and protein metabolism leading to abnormal insulin secretion, insulin resistance, or both.1–3 While impaired glycemic control and lipotoxicity as well as their underlying mechanisms have been extensively studied in obesity and type 2 diabetes mellitus (T2DM),4 emerging studies suggest a causal role of BCAAs in the pathogenesis of obesity and insulin resistance.3,5,6 In the Framingham Offspring Study,3 the longitudinal analysis was performed to investigate whether metabolite profiles could predict the development of Diabetes Mellitus (DM), which revealed that branched-chain amino acids (BCAAs) and aromatic amino acids (AAAs) levels are significantly related to a future diagnosis of DM. More recently, a prospective cohort study concluded that high consumption of BCAAs is associated with an increased risk of T2DM.6 Therefore, T2DM risks are not only restricted to carbohydrates and fatty acid metabolism disturbance, but also associated with altered protein and amino acid metabolism.
The BCAAs (L-leucine (L-Leu), L-isoleucine (L-Ile) and L-valine (L-Val)) are essential amino acids that cannot be synthesized de novo.7 Excessive amino acids intake or inborn errors in the genes encoding for the catalytic enzymes in the BCAA catabolism pathway causes accumulation of BCAAs and metabolites.8 Increased BCAAs plasma concentration have been found in many pathological conditions such as Maple syrup urine disease (MSUD), obesity, T2DM, dyslipidaemia, cardiovascular complications and some cancer.5,6,9,10 MSUD is a Mendelian disease due to deficiency of the branched-chain ketoacid dehydrogenase (BCKDC) and associated with elevations in the BCAAs and their ketoacids.9 Elevated BCAAs level is associated with insulin resistance and is suggested as new predictors of future diabetes.5,6 Moreover, it can be positively associated with enhanced cardiovascular risk.10
BCAAs and toxic metabolites may induce elevated reactive oxygen species (ROS) levels and mitochondrial dysfunction in brain, liver and heart.11–13 Adding branched-chain α-ketoacid (BCKAs) to glial cells could cause lipid peroxidation and oxidative stress which lead to mitochondrial dysfunction.11 Zhang et al found that BCAA cause significant hepatic damage in high fat diet mice, evidenced by exacerbated hepatic oxidative stress, increased hepatic apoptosis, and elevated circulation hepatic enzymes.12 BCAA could promote endothelial dysfunction through increased ROS generation and inflammation which contribute to the increased cardiovascular risk.13 However, it remains poorly understood that whether such damage is associated with IR and T2DM onset.
Oxidative stress is a major risk factor in the onset and progression of T2DM.14 An oxidative environment may cause the development of impaired glucose tolerance, IR, mitochondrial dysfunction, β-cell dysfunction, all of which contribute ultimately to the diabetic disease state. BCAAs as antioxidants are widely used clinically for chronic liver and renal failure.15,16 Some studies show that BCAAs can also counter the oxidative stress that occurs in the diabetic pancreas and some liver diseases.17,18 But, Deyang Yu and his colleague found that reducing dietary levels of BCAAs promote metabolic health in mice, a low isoleucine diet reprograms liver and adipose metabolism, increasing hepatic insulin sensitivity and ketogenesis.19 Given the health benefits of high dietary BCAAs concentration, it seems paradoxical that increased BCAAs levels were found in obesity and T2DM. Associations between BCAAs dysmetabolism and oxidative stress are consistently observed in animal researches.11–13 It is necessary to clarify the relationship between BCAAs, oxidative stress and T2DM in people.
Therefore, the objective of the present study was to evaluate the association between BCAAs levels, oxidative stress and newly-diagnosed T2DM in a relatively large Chinese population, which might be helpful for improving preventive and therapeutic strategies for T2DM.
Methods
Study Population
In the present study, 1759 participants aged 40 to 79 years were recruited who were retiree and accepted annual routine health examinations between September to October 2014 at the health examination center of The Affiliated Huaian Hospital of Xuzhou Medical College in Huaian (Jiangsu, China). Exclusion criteria was described in earlier published article.20 In addition, missing data for eGFR (n=100) and previously diagnosed diabetes including Type 1 diabetes, T2DM, gestational diabetes (n=247) were excluded. Finally, a total of 816 participants (537 women) were eligible for the analysis.
Data Collection
The demographic characteristics, lifestyle information and medical history were obtained by trained investigators through a standard questionnaire. Height, weight, blood pressure (BP), Waist circumference (WC) were measured as described before.20 BMI was calculated as weight (kg) divided by height squared (m2). Blood pressure (BP) was consecutively measured 3 times (OMRON Model HEM-752FUZZY, Omron Company, Dalian city, Liaoning Province, China). Blood samples were extracted from the antecubital vein between 8:00 and 10:00 am after overnight fasting at least 10 hours. Total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), fasting glucose (FPG), creatinine (CREA), urea nitrogen (BUN), and uric acid (UA) were measured in a certified laboratory by standardized procedures. We used high performance liquid chromatography (Variant II and D-10 Systems, Bio-Rad Laboratories Inc., Hercules, CA, USA) to measure HbA1c. Diabetes, prediabetes and Normal glucose metabolism (NGM) were defined based on 2012 ADA criteria. The presence of diabetes was defined as follows: FPG≥126mg/dL (7.0mmol/L) or 2-h plasma glucose in the 75-gOGTT≥200mg/dL (11.1mmol/L) or HbA1c≥6.5%. The presence of prediabetes was defined as follows: FPG 100mg/dL (5.6mmol/L) to 125mg/dL (6.9mmol/L) (IFG) or 2-h plasma glucose in the 75-g OGTT 140mg/dL (7.8mmol/L) to 199mg/dL (11.0mmol/L) (IGT) or HbA1C 5.7–6.4%. Based on these criteria, 102 of the 816 subjects included in the analysis were considered to have newly diagnosed diabetes mellitus (NDM), 354 were considered to have prediabetes, and 380 were considered to have NGM.
Laboratory Analysis
Collections of venous blood samples and acquisition of laboratory index referred in this study were reported in before work.20 Malondialdehyde (MDA) as an index of lipid peroxidation was estimated by using the method described by Buege and Aust.21 The Superoxide Dismutase (SOD) activity was evaluated on the basis of its ability to inhibit the oxidation of hydroxylamine.22 Homeostasis Model assessment for Insulin Resistance (HOMA-IR) = fasting insulin (μU/mL) × fasting glucose (mmol/L)/22.5. The estimated glomerular filtration rate (eGFR) 22 was calculated from the creatinine levels using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI).23
Statistical Analysis
The continuous variables in this study exhibited normal or approximately normal distributions, which were presented as means ± standard deviations (SDs); categorical variables were presented as numbers (%). The differences between the groups were analyzed using one-way analysis of variance (ANOVA), with non-parametric tests for non-normally distributed variables and chi-square test for categorical data. After verifying the assumption of a linear relationship between the dependent and independent variables that were introduced into the linear regression model, a multiple linear regression analysis was used to estimate the association of the BCAAs with the SOD (Table 1A) and MDA (Table 1B) in groups with different glucose tolerance (NGM, Prediabetes and NDM). Two models were constructed for each component of glucose metabolism. In Model 1, the variates include age, gender and BMI were adjusted. In model 2, multivariable-adjusted model was used (incorporating age, gender, BMI, SBP, DBP, FBG, TC, LnTG, HDL-c, LDL-c, SUA, smoking status and hypertension) (See Table 1). For analysis, the subjects were divided into four groups based on stratification of L-Val levels using the 25th, 50th and 75th percentiles as cut-off points. Differences in laboratory parameters among the four quartile groups were evaluated using analysis of variance (ANOVA), and laboratory parameters that yielded statistically significant outcomes were further evaluated using analysis of covariance (ANCOVA). Data that were not normally distributed were Napierian logarithmically transformed before analysis.
Table 1.
Multiple Linear Regression Analyses of the Relationship Between BCAAs and SOD(A) or MDA(B) in Different Glucose Metabolism Groups
| A Independent Variable | Total (n=816) | NGM (n = 380) | Prediabetes (n = 334) | NDM (n = 102) | ||||
|---|---|---|---|---|---|---|---|---|
| β ± SE | P value | β ± SE | P value | β ± SE | P value | β ± SE | P value | |
| Model 1 | ||||||||
| BCAAs | −0.028 ± 0.03 | 0.369 | −0.012± 0.05 | 0.841 | 0.051 ± 0.059 | 0.388 | −3.639 ± 1.152 | 0.001 |
| L-Leu | −0.089 ± 0.074 | 0.232 | −0.05 ± 0.123 | 0.684 | −0.111 ± 0.136 | 0.415 | −0.643 ± 0.249 | 0.040 |
| L-Ile | −0.214 ± 0.141 | 0.129 | −0.139 ± 0.216 | 0.520 | −0.214 ± 0.260 | 0.411 | −1.023 ± 0.512 | 0.048 |
| L-Val | −0.009 ± 0.065 | 0.895 | −0.017 ± 0.104 | 0.871 | −0.087 ± 0.126 | 0.491 | −0.437 ± 0.230 | 0.030 |
| Model 2 | ||||||||
| BCAAs | 0.014 ± 0.034 | 0.667 | 0.023 ± 0.052 | 0.213 | 0.101 ± 0.064 | 0.119 | −3.312 ± 1.359 | 0.016 |
| L-Leu | 0.002 ± 0.079 | 0.992 | 0.064 ± 0.134 | 0.926 | 0.074 ± 0.126 | 0.921 | −0.575± 0.270 | 0.076 |
| L-Ile | 0.059 ± 0.151 | 0.694 | −0.038 ± 0.227 | 0.896 | 0.413 ± 0.281 | 0.142 | −0.473 ± 0.292 | 0.102 |
| L-Val | 0.075 ± 0.070 | 0.285 | 0.064 ± 0.134 | 0.457 | 0.181 ± 0.136 | 0.147 | −0.505 ± 0.262 | 0.036 |
| B Independent variable | Total (n=816) | NGM (n = 380) | Prediabetes (n = 334) | NDM (n = 102) | ||||
| β ± SE | P value | β ± SE | P value | β ± SE | P value | β ± SE | P value | |
| Model 1 | ||||||||
| BCAAs | 0.028 ± 0.03 | 0.369 | 0.100 ± 0.033 | 0.001 | 0.045 ± 0.023 | 0.027 | 0.036 ± 0.024 | 0.381 |
| L-Leu | 0.089 ± 0.074 | 0.232 | 0.005 ± 0.007 | 0.440 | 0.005 ± 0.004 | 0.344 | 0.005 ± 0.004 | 0.286 |
| L-Ile | 0.214 ± 0.141 | 0.129 | −0.009 ± 0.016 | 0.998 | 0.003 ± 0.004 | 0.702 | 0.019 ± 0.009 | 0.427 |
| L-Val | 0.020 ± 0.003 | <0.001 | 0.023 ± 0.06 | < 0.001 | 0.017 ± 0.006 | < 0.001 | 0.017 ± 0.04 | 0.040 |
| Model 2 | ||||||||
| BCAAs | 0.004 ± 0.001 | <0.001 | 0.008 ± 0.003 | 0.054 | 0.006 ± 0.002 | 0.010 | −0.006 ± 0.002 | 0.295 |
| L-Leu | 0.014 ± 0.005 | 0.124 | 0.007 ± 0.120 | 0.926 | 0.008 ± 0.112 | 0.234 | 0.003 ± 0.007 | 0.698 |
| L-Ile | 0.007 ± 0.006 | 0.248 | 0.004 ± 0.013 | 0.770 | 0.008 ± 0.010 | 0.436 | 0.019 ± 0.010 | 0.325 |
| L-Val | 0.022 ± 0.004 | <0.001 | 0.024 ± 0.006 | 0.001 | 0.020 ± 0.005 | <0.001 | 0.024 ± 0.009 | 0.022 |
Notes: Model 1: adjusted for age, gender and body mass index; Model 2: adjusted for age, gender, body mass index, systolic blood pressure, diastolic blood pressure, fasting blood glucose, total cholesterol, Ln (triglyceride), high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, serum uric acid, smoking status and hypertension. The bold format serves as an emphasis note. Values were regression coefficient (β) ± standard error (SE). Definitions of NGM (normal glucose metabolism), prediabetes and T2DM (Type 2 diabetes) were in methods.
Abbreviations: BCAAs, branched-chain amino acids; SOD, superoxide dismutase.
To further clarify the relationship between L-Val levels, MDA and NDM, subjects were divided into four sub-groups on the basis of the basis of the level of L-Val quartiles. We constructed unadjusted and multivariable-adjusted models (Model 1 (incorporating age and gender, BMI, MDA) and Model 2 (incorporating age and gender, BMI, MDA, SBP, DBP, TC, TG, HDL-c, LDL-c, SUA, eGFR, and smoking status). P-values for the trends were calculated by Spearman correlation analysis of categorical variables and odds ratios (ORs) for the different groups respectively. P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 16.0 (SPSS Inc., Chicago, IL, USA).
Results
Characteristics of the Study Participants
A total of 816 participants were enrolled (537 females) and divided into three groups (NGM, Prediabetes, and NDM). As shown in Table 2, age, WC, BMI, HbA1c, FPG, TC, TG, LDL-C, SUA and the proportion of subjects with hypertension in the Prediabetes and NDM groups were significantly higher than those in the NGM group (P<0.05), while HDL-c levels were significantly lower (P<0.001). Subjects in NDM group have higher MDA level and lower SOD level than subjects in NGM and prediabetes groups. Moreover, there was higher WC, BMI, BCAAs (L-leu, L-Ile, L-Val) and more unfavorable lipid profile (elevated TC, TG, LDL-C and decreased HDL-C) in NDM group. There were no significant differences between the three groups in gender, smoking status, systolic BP (SBP), diastolic BP (DBP), BUN, Serum creatinine and eGFR.
Table 2.
Characteristics of the Study Participants (n=816)
| NGM (n = 380) | Prediabetes (n = 334) | NDM (n = 102) | P value | |
|---|---|---|---|---|
| Male (%) | 123 (32.4) | 121 (36.2) | 35 (34.7) | 0.096 |
| Age (years) | 57.56 ± 5.79 | 59.38 ± 5.79 | 60.08 ± 6.21 | < 0.001 |
| Smoking (%) | 58 (15.2) | 57 (17.1) | 18 (17.3) | 0.577 |
| Hypertension (%) | 75 (19.6) | 124 (37.1) | 36 (35.6) | 0.033 |
| WC (cm) | 81.26 ± 8.88 | 84.22 ± 9.58 | 87.24 ± 13.97 | < 0.001 |
| BMI (kg/m2) | 23.87 ± 2.90 | 24.70 ± 3.05 | 26.18 ± 4.21 | < 0.001 |
| SBP (mmHg) | 141.46 ± 20.11 | 139.42 ± 19.31 | 139.93 ± 19.64 | 0.597 |
| DBP (mmHg) | 84.75 ± 13.94 | 83.81 ± 13.31 | 84.27 ± 13.19 | 0.073 |
| TC (mmol/L) | 5.11 ± 0.82 | 5.26 ± 0.85 | 5.27 ± 0.99 | 0.008 |
| TG (mmol/L) | 1.55 (0.50, 8.22) | 1.79 (0.58, 7.43) | 1.85 (0.83, 12.5) | < 0.001 |
| HDL-C (mmol/L) | 1.47 ± 0.65 | 1.33 ± 0.38 | 1.29 ± 0.30 | < 0.001 |
| LDL-C (mmol/L) | 2.68 ± 0.68 | 2.87 ± 0.71 | 2.85 ± 0.79 | < 0.001 |
| SUA (mmol/L) | 271.09 ± 76.87 | 293.68 ± 78.21 | 295.94 ± 78.04 | < 0.001 |
| BUN (mmol/L) | 5.11 ± 1.39 | 5.07 ± 1.21 | 4.95 ± 1.33 | 0.282 |
| Serum creatinine (mg/dL) | 0.79 ± 0.17 | 0.78 ± 0.16 | 0.79 ± 0.18 | 0.656 |
| eGFR (mL/min per 1.73 m2) | 90.51 ± 13.76 | 91.03 ± 13.25 | 90.20 ± 14.77 | 0.540 |
| HbA1c (%) | 5.32 (4.3,5.6) | 6.04 (5.0,6.4) | 7.14 (6.0,11.8) | < 0.001 |
| FPG (mmol/L) | 5.06 ± 0.31 | 5.62 ± 0.57 | 7.35 ± 2.42 | < 0.001 |
| BCAAs | ||||
| L-Leu (μg/mL) | 25.57 ± 5.13 | 26.64 ± 5.43 | 27.74 ± 5.11 | < 0.001 |
| L-Ile (μg/mL) | 12.68± 2.97 | 13.22± 2.91 | 13.67± 2.51 | < 0.001 |
| L-Val (μg/mL) | 30.75± 12.12 | 31.48± 5.81 | 32.47± 5.57 | < 0.001 |
| MDA (nmol/L) | 0.86 ± 0.71 | 0.83 ± 0.47 | 0.95 ± 0.43 | 0.023 |
| SOD (u/mL) | 59.53± 12.12 | 56.39 ± 13.46 | 56.98± 12.39 | 0.040 |
Notes: Data were presented as means (±SD) or median with range (minimum, maximum) as appropriate, and categorical variables are expressed as number (%). Comparisons between the three groups were made using ANOVA or Fisher’s exact test, as appropriate. P values testing the overall difference among different glucose metabolism groups. International system of units (SI) conversion: serum creatinine, 1mg/dl=88.41umol/L.
Abbreviations: NGM, normal glucose metabolism; NDM, newly diagnosed diabetes; WC, waist circumference; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c; TG, triglycerides; TC, total cholesterol; SUA, serum uric acid; BUN, urea nitrogen; e-GFR, estimated glomerular filtration rate; L-Leu, L-leucine; L-Ile, L-isoleucine; L-Val, L-valine; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; BCAAs, branched-chain amino acids; SOD, superoxide dismutase; MDA, malondialdehyde.
Multiple Linear Regression Analysis for Association Between BCAAs and Oxidative Stress
As presented in Table 1, two models were constructed to analyze the association of individual BCAA with SOD and MDA in different glucose metabolism groups (total BCAAs, L-leu, L-Ile and L-Val were analyzed separately due to co-linearity). In model 1, the L-Leu, L-Ile and L-Val levels were independently negatively related to the SOD levels in NDM group. After adjusting for age, gender, smoking status, BMI, SBP, DBP, FBG, TC, LnTG(triglyceride), LDL-c and HDL-c, only L-Val levels were also found to be negatively related to the SOD levels in NDM group in model 2 (Table 1A). Similarly, L-Val levels were independently positively associated with MDA in different glucose metabolism groups (NGM, prediabetes, and NDM) in model 2 (Table 1B).
Comparison of Clinical Parameters According to the Level of L-Val Quartiles
Participants were divided into four groups according to the level of L-Val quartiles. As shown in Table 3, most of the parameters did not differ among the four groups except for gender, WC, BMI, FPG, LnHbA1c, LnTG, SUA and MDA. As L-Val quartiles increased, subjects were more likely to have higher WC, BMI, FPG and more unfavorable lipid profile (increased LnTG and decreased HDL-C). Moreover, after adjusting for several traditional risk factors, there was a significant trend toward higher MDA levels and the ratio of NGM.
Table 3.
Comparison of Clinical Parameters According to the Level of L-Val Quartiles (n=816)
| Characteristics | L-Val (μg/mL) | |||||||
|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | P-value | ||||
| (<27.26, n=203) | (27.26–31.12, n=205) | (31.12–35.25, n=204) | (≥35.25 n=204) | Unadjusted | Model 1 | Model 2 | Model 3 | |
| L-Val (μg/mL) | 24.04± 2.52 | 29.21 ±1.19 | 32.83± 1.09 | 38.91 ± 3.63 | <0.001 | <0.001 | <0.001 | <0.001 |
| Male, n (%) | 51 (25.1) | 72 (35.1) | 78 (38.2) | 73 (35.2) | 0.027 | – | ||
| Age (years) | 58.15 ± 6.49 | 58.86 ± 5.82 | 59.43 ± 5.67 | 58.84 ± 6.25 | 0.111 | – | ||
| Current smoking, n (%) | 23 (11.3) | 31 (15.1) | 43 (38.2) | 37 (18.1) | 0.0407 | – | ||
| Hypertension, n (%) | 52 (25.6) | 54 (26.1) | 70 (34.3) | 64 (31.4) | 0.166 | – | ||
| WC (cm) | 81.43 ± 9.88 | 83.77 ± 9.97 | 85.39 ± 9.66 | 84.32 ± 10.00 | <0.001 | <0.001 | ||
| BMI (kg/m2) | 23.95 ± 3.18 | 24.27 ± 3.24 | 24.98 ± 3.43 | 24.91 ± 3.73 | <0.001 | <0.001 | ||
| SBP (mmHg) | 140.05 ± 19.16 | 141.44±20.37 | 137.98± 19.91 | 142.73 ± 21.87 | 0.987 | – | ||
| DBP (mmHg) | 85.25 ± 13.23 | 84.93 ± 14.17 | 82.68 ± 16.07 | 83.69 ± 14.01 | 0.482 | – | ||
| FPG (mmol/L) | 5.34 ± 0.73 | 5.50 ± 0.96 | 5.55 ± 1.01 | 5.82 ± 1.67 | <0.001 | <0.001 | ||
| HbA1c (%) | 5.50 (5.1, 7.4) | 5.50 (5.1, 8.6) | 5.86 (5.1, 11.2) | 5.90 (5.1, 11.8) | 0.002 | <0.001 | ||
| TC (mmol/L) | 5.23 ± 0.97 | 5.13 ± 0.83 | 5.25 ± 0.88 | 5.11 ± 0.74 | 0.334 | – | ||
| TG (mmol/L) | 1.48 (0.60,7.40) | 1.60 (0.50, 6.40) | 1.80 (0.62,12.50) | 1.89 (0.58,8.22) | <0.001 | 0.008 | ||
| LDL-C (mmol/L) | 2.83 ± 0.78 | 2.73 ± 0.66 | 2.81 ± 0.69 | 2.74 ± 0.69 | 0.438 | – | ||
| HDL-C (mmol/L) | 1.45 ± 0.44 | 1.38 ± 0.41 | 1.29 ± 0.48 | 1.34 ± 0.65 | 0.020 | 0.167 | ||
| SUA (mmol/L) | 270.12 ± 74.17 | 282.46 ± 81.99 | 291.58 ± 81.93 | 299.06 ± 86.56 | <0.001 | <0.001 | 0.052 | 0.096 |
| BUN (mmol/L) | 5.11 ± 1.32 | 5.02 ± 1.31 | 5.26 ± 1.21 | 5.23 ± 1.39 | 0.106 | |||
| Serum creatinine (μmol/L) | 69.01 ± 13.93 | 70.52 ± 15.59 | 69.82 ± 13.19 | 71.16 ± 16.72 | 0.278 | – | ||
| eGFR (ml/min/1.73 m2) | 90.88 ± 21.32 | 91.95 ± 13.14 | 90.09 ± 14.56 | 90.79 ± 13.72 | 0.634 | – | ||
| SOD (u/mL) | 58.26 ± 12.6 | 60.12 ± 11.87 | 57.64± 12.76 | 57.19 ± 13.0 | 0.553 | – | ||
| MDA (nmol/L) | 0.72± 0.52 | 0.85 ± 0.47 | 0.88 ± 0.49 | 1.01 ± 0.83 | <0.001 | <0.001 | <0.001 | <0.001 |
| NDM | 14 (6.9) | 22 (10.7) | 26 (12.7) | 40 (19.6) | <0.001 | |||
Notes: Data were presented as means (±SD) and categorical variables are expressed as number (%). Means and proportions were compared by ANCOVA, and categorical variables were compared by the chi-square test respectively. P values testing the overall difference among L-Val quartiles. Model 1: adjusting for age, gender, SBP, DBP, LnTG, HDL-C, FPG and smoking status. Model 2: adjusting for age, gender, BMI, SBP, DBP, LnTG, HDL-C and smoking status. Model 3: adjusting for age, gender, SBP, DBP, HOMA-IR and smoking status. TG which is not normal distribution were analyzed by logarithmic transformation. Definitions of T2DM, NDM and L-Val quartiles were in methods.
Abbreviations: L-Val, L-valine; T2DM, type 2 diabetes mellitus; NDM, newly diagnosed diabetes mellitus; WC, waist circumference; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c; TG, triglycerides; TC, total cholesterol; SUA, serum uric acid; eGFR, estimated glomerular filtration rate; SOD, superoxide dismutase; MDA, malondialdehyde; HOMA-IR, homeostasis model assessment of insulin resistance.
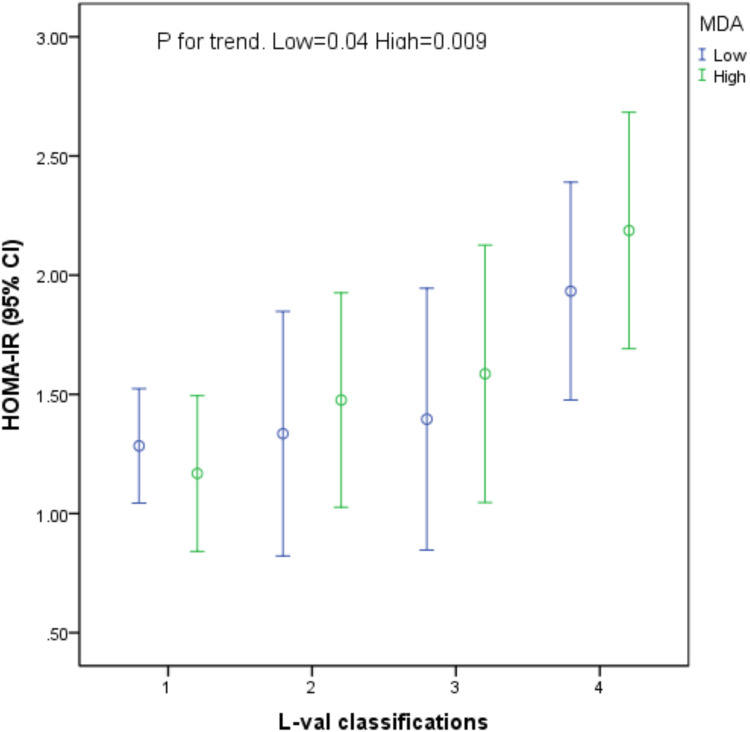
Association Between L-Val Quartiles, MDA and HOMA-IR
The synergistic effect of L-Val and MDA in HOMA-IR were described in Figure 1. The stepwise increased L-Val levels showed a significant, additive role to IR levels in both high and low MDA level. It seems that L-Val and MDA synergistic increased IR.
Figure 1.
Association between L-Val, MDA and HOMA-IR.
Multiple Logistic Regression Analysis for the Incidence of NDM
After adjusting for age, gender, smoking, BMI, MDA, SBP, DBP, TC, TG, HDL-C LDL-C, SUA, eGFR and smoking status., L-Val were independently associated with NDM risk (OR= 1.06 95% CI 1.02–1.10; P=0.005) (Table 4). To further investigate the relationship between L-Val levels, MDA and risk of NDM, subjects were divided into four sub-groups based on the levels of L-Val quartiles (Table 4). After adjusting for age, gender, smoking, BMI, MDA, SBP, DBP, TC, TG, HDL-C, LDL-C, SUA, eGFR and smoking status, compared with the reference (L-Val I (<27.26 μg/mL)), participants in L-Val IV (≥ 35.25 μg/mL) group had a significantly increased risk of NDM (OR= 2.25 95% CI 1.11–4.57; P=0.024). However, there were no significant associations for those in L-Val II and L-Val III groups.
Table 4.
Multiple Logistic Regression Analyses of the Relationship Between L-Val, MDA and NDM
| Independent Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | P-value | OR (95% CI) | P-value | OR (95% CI) | P-value | |
| L-Val (μg/mL) | 1.08 (1.04–1.11) | <0.001 | 1.08 (1.03–1.12) | 0.001 | 1.06 (1.02–1.10) | 0.005 |
| L-Val | ||||||
| I | 1 | 1 | 1 | |||
| II | 1.62 (0.81–3.27) | 0.175 | 1.47 (0.79–3.26) | 0.297 | 1.62 (0.77–3.44) | 0.205 |
| III | 1.97 (0.998–3.89) | 0.051 | 1.35 (0.71–3.05) | 0.415 | 1.25 (0.59–2.64) | 0.562 |
| IV | 2.61 (1.47–4.61) | 0.001 | 2.37 (1.20–4.69) | 0.013 | 2.25 (1.11–4.57) | 0.024 |
Notes: Model 1: un-adjusting. Model 2: adjusting for age, gender BMI and MDA. Model 2: adjusting for age, gender, BMI, MDA, SBP, DBP, TC, TG, HDL-C, LDL-C, eGFR and smoking status. Definitions of T2DM were in statistical analysis. Classifying patients into four sub-groups on the basis of the level of L-Val quartiles.
Abbreviations: CI, confidence interval; L-Val, L-valine; MDA, malondialdehyde; T2DM, type 2 diabetes.
Discussion
Our data showed that 1) L-Val was positively correlated with MDA levels in different glucose metabolism groups and negatively correlated with SOD in NDM group, showing a linkage between L-Val and oxidative stress. 2) High L-Val levels (≥ 35.25μg/mL) were significantly associated with higher BMI, WC, FPG, HOMA-IR, MDA, more unfavorable lipid profile (increased LnTG and decreased HDL-C) and NDM. 3) the OR for the risk of NDM were 2.25-fold (95% CI 1.11–4.57; P=0.024) among participants in high L-Val group compared with the participants in low L-Val group after adjusting for MDA and other risk factors. These findings suggest that high L-Val (≥ 35.25μg/mL) could elevate MDA, thus promoting NDM. 3) In our study, it is more sense for prevention of T2DM because subjects were middle-aged and elderly and relatively healthy due to many chronic diseases excluded including the history of DM.
Recent years, more evidence has showed that elevated levels of BCAAs predict future IR or T2DM and is suggested causative factor in IR and T2DM. In a study, more than 100 analytes were measured in plasma samples from obese, insulin-resistant versus lean, insulin-sensitive subjects.24 Newgard et al surprisingly found the components most strongly associated with insulin resistance were not lipid-related, but BCAAs (Val, Leu, Ile) and AAAs (phenylalanine (Phe), tyrosine (Tyr)). The preferential association of this BCAA-related metabolite cluster as a new risk factor with IR, T2DM and CVD was discussed in many cross-sectional studies.25–27
As we know, when excessive ROS overwhelm the defense system or exceed its scavenging capability, oxidative stress may be ineluctable. A study revealed that BCAA dysmetabolism leads to the accumulation of toxic metabolites that maybe cause mitochondrial elevated ROS levels.28 In our study we observed a significant positive correlation between serum L-Val levels and MDA (an index of lipid peroxidation) in different glucose metabolism groups. L-Val levels were also found to be negatively related to the SOD levels in NDM group. However, the mechanism is unclear. BCAAs may significantly down-regulated the expression of some antioxidant genes and up-regulating the expression of some oxygen transporters in the brain of C57Bl/6J mice.29 Addition of BCKAs as metabolites of BCAAs to glial cells or to the cerebral cortex increases lipid peroxidation and oxidative stress leading to mitochondrial bioenergetic dysfunction.11 BCAA could promote endothelial dysfunction through increased ROS generation and inflammation which contribute to the increased cardiovascular risk.13,30 However, there are some inconsistent studies.16–18 Recent study concluded BCAAs counter oxidative stress in the kidneys of diabetic rats via decreasing ROS levels, proteinuria and alleviate diabetic kidney injury via the JNK/TGF-b/MMP-9 pathway.31 And administration of BCAAs and microelements is likely to suppress the progression of non-alcoholic steatohepatitis (NASH) by reducing oxidative stress, primarily via the downregulation of the endoplasmic reticulum (ER) stress pathway.18 However, human research is differed from animal in BCAAs tolerance dose, BCAAs metabolism and status of the oxidative stress. Accordingly, a large multi-center study is necessary to evaluate the relationship between the serum amino acids and oxidative stress in population.
Interestingly, there is no association among L-Leu, L-Ile, MDA and SOD in our study. A large scale, cross-sectional and prospective analyses of ethnicity, amino acids and diabetes in a South Asian and European cohort reported that the increased levels of Ile, Tyr, alanine and glutamine were seen in more centrally obese South Asian men.27 They explained that altered amino acids metabolism in the liver, kidneys, muscle or adipose tissue is due to different races. According to our data, it is inferred that whether the valine metabolic abnormalities is popular in Asian populations. However, it is necessary to verify by a large multi-centers research in different races.
L-Val were independently associated NDM in our study in accordance with previous cross-sectional studies.32,33 As L-Val levels increased, there was a significant trend toward higher ratio of NDM. However, the mechanism of this association is not clear. One hypothesis is that an excess of dietary BCAAs activates mTORC1 signaling, which leads to IR and T2DM.5,24,34 However, it is contradictory that supplementing or increasing circulating levels of BCAAs is associated with metabolic improvements despite increased mTORC1 signaling.35 Moreover, individuals with morbid obesity have raised levels of BCAAs that normalize after gastric bypass surgery, however, mTORC1 activation in muscle did not change after gastric bypass surgery in a longitudinal study.35,36
The second hypothesis originates from studies of MSUD.9 BCAA dysmetabolism leads to the accumulation of toxic metabolites that maybe cause mitochondrial dysfunction in pancreatic islet β cells (or elsewhere) and could be associated with insulin resistance and T2DM.11,37 In our study, after adjusting for T2DM risk factors, high L-Val levels were significantly associated with higher BMI, WC, FPG, more unfavorable lipid profile (increased LnTG and decreased HDL-C). A longitudinal study from Japan showed that plasma free amino acids profile can predict the four-year risk for developing lifestyle-related diseases, including diabetes, dyslipidemia, hypertension and metabolic syndrome in a general Japanese population which based on oxidative stress and IR.33 Similarly we concluded that BCAAs are associated with metabolic dyslipidemia and metabolic syndrome in previous study.10,20 Moreover, the odds ratios (OR) for NDM were 2.25-fold among participants in high L-Val group compared with the participants in low L-Val group in our study after adjusting for MDA and other risk factors. These findings suggest that elevated L-Val concentrations may elevate MDA, thus contributing to NDM. But mechanism remains unclear. Therefore, further investigation on L-Val, oxidative stress and mitochondrial function in pancreatic islet β cells in animal model is necessary.
There are some limitations in our study. First, the index of oxidative stress detection was too single, the evaluation of oxidative stress was not comprehensive. Second, a cross-sectional study cannot infer the causality between BCAAs, MDA and NDM. Third, this study was a single-center study, and our population consisted primarily of urban workers who underwent an annual health checkup and had a low prevalence of NDM.
Conclusion
In conclusion, our results suggest that L-Val is an independent risk factor of oxidative stress in different glucose metabolism groups. Moreover, high L-Val levels with oxidative stress could be a significant risk factor for increased T2DM incidence risk; and that elevated MDA may contribute to IR and an increased NDM in subjects with high L-Val levels. Intervention studies are needed to investigate whether a strategy to reduce L-Val levels can improve oxidative stress and reduce the risk of T2DM incident.
Funding Statement
The work was supported by the National Natural Sciences Foundation of China to Wen Hu (No.81700776), the Health Department Fund Projects of Jiangsu Province to WenHu (No.H2018054) and Major Research plan of the National Natural Science Foundation of China to Hongwen Zhou [grant number 91854122].
Data Sharing Statement
All data presented in the manuscript are available upon request.
Ethical Approval
Written informed consent was obtained from all participants who were informed in detail about the objectives and procedures of the study before. This cross-sectional study was rooted in Huaian Diabetes Prevention Program (HADPP) (ChiCTR-TRC-14005029) which was approved by the medical ethics committees of The Affiliated Huaian Hospital of Xuzhou Medical College. This study was conducted in accordance with the Declaration of Helsinki.
Consent
No consent was required for this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest.
References
- 1.Silva JAD, Souza ECF, Echazu Boschemeier AG, Costa C, Bezerra HS, Feitosa E. Diagnosis of diabetes mellitus and living with a chronic condition: participatory study. BMC Public Health. 2018;18(1):699. doi: 10.1186/s12889-018-5637-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yang J, Kang J, Guan Y. The mechanisms linking adiposopathy to type 2 diabetes. Front Med. 2013;7(4):433–444. doi: 10.1007/s11684-013-0288-9 [DOI] [PubMed] [Google Scholar]
- 3.Wang TJ, Larson MG, Vasan RS, et al. Metabolite profiles and the risk of developing diabetes. Nat Med. 2011;17(4):448–453. doi: 10.1038/nm.2307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruud J, Steculorum SM, Bruning JC. Neuronal control of peripheral insulin sensitivity and glucose metabolism. Nat Commun. 2017;8(1):15259. doi: 10.1038/ncomms15259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newgard CB. Interplay between lipids and branched-chain amino acids in development of insulin resistance. Cell Metab. 2012;15(5):606–614. doi: 10.1016/j.cmet.2012.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng Y, Li Y, Qi Q, et al. Cumulative consumption of branched-chain amino acids and incidence of type 2 diabetes. Int J Epidemiol. 2016;45(5):1482–1492. doi: 10.1093/ije/dyw143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Harris RA, Joshi M, Jeoung NH. Mechanisms responsible for regulation of branched-chain amino acid catabolism. Biochem Biophys Res Commun. 2004;313(2):391–396. doi: 10.1016/j.bbrc.2003.11.007 [DOI] [PubMed] [Google Scholar]
- 8.Ogier de Baulny H, Saudubray JM. Branched-chain organic acidurias. Semin Neonatol. 2002;7(1):65–74. doi: 10.1053/siny.2001.0087 [DOI] [PubMed] [Google Scholar]
- 9.Burrage LC, Nagamani SC, Campeau PM, Lee BH. Branched-chain amino acid metabolism: from rare Mendelian diseases to more common disorders. Hum Mol Genet. 2014;23(R1):R1–8. doi: 10.1093/hmg/ddu123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang P, Hu W, Fu Z, et al. The positive association of branched-chain amino acids and metabolic dyslipidemia in Chinese Han population. Lipids Health Dis. 2016;15(1):120. doi: 10.1186/s12944-016-0291-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amaral AU, Leipnitz G, Fernandes CG, Seminotti B, Schuck PF, Wajner M. Alpha-ketoisocaproic acid and leucine provoke mitochondrial bioenergetic dysfunction in rat brain. Brain Res. 2010;1324:75–84. doi: 10.1016/j.brainres.2010.02.018 [DOI] [PubMed] [Google Scholar]
- 12.Zhang F, Zhao S, Yan W, et al. Branched chain amino acids cause liver injury in obese/diabetic mice by promoting adipocyte lipolysis and inhibiting hepatic autophagy. EBioMedicine. 2016;13:157–167. doi: 10.1016/j.ebiom.2016.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhenyukh O, Gonzalez-Amor M, Rodrigues-Diez RR, et al. Branched-chain amino acids promote endothelial dysfunction through increased reactive oxygen species generation and inflammation. J Cell Mol Med. 2018;22(10):4948–4962. doi: 10.1111/jcmm.13759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ceriello A, Testa R. Antioxidant anti-inflammatory treatment in type 2 diabetes. Diabetes Care. 2009;32(Suppl 2):S232–6. doi: 10.2337/dc09-S316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cano NJ, Fouque D, Leverve XM. Application of branched-chain amino acids in human pathological states: renal failure. J Nutr. 2006;136(1):299S–307S. doi: 10.1093/jn/136.1.299S [DOI] [PubMed] [Google Scholar]
- 16.Kawaguchi T, Izumi N, Charlton MR, Sata M. Branched-chain amino acids as pharmacological nutrients in chronic liver disease. Hepatology. 2011;54(3):1063–1070. doi: 10.1002/hep.24412 [DOI] [PubMed] [Google Scholar]
- 17.Lu M, Zhang X, Zheng D, Jiang X, Chen Q. Branched-chain amino acids supplementation protects streptozotocin-induced insulin secretion and the correlated mechanism. Biofactors. 2015;41(2):127–133. doi: 10.1002/biof.1188 [DOI] [PubMed] [Google Scholar]
- 18.Tanaka H, Fukahori S, Baba S, et al. Branched-chain amino acid-rich supplements containing microelements have antioxidant effects on nonalcoholic steatohepatitis in mice. J Parenter Enteral Nutr. 2016;40(4):519–528. doi: 10.1177/0148607114555160 [DOI] [PubMed] [Google Scholar]
- 19.Yu D, Richardson NE, Green CL, et al. The adverse metabolic effects of branched-chain amino acids are mediated by isoleucine and valine. Cell Metab. 2021;33:905–22 e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hu W, Sun L, Gong Y, et al. Relationship between branched-chain amino acids, metabolic syndrome, and cardiovascular risk profile in a Chinese population: a cross-sectional study. Int J Endocrinol. 2016;2016:8173905. doi: 10.1155/2016/8173905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978;52:302–310. [DOI] [PubMed] [Google Scholar]
- 22.Beutler E, Duron O, Kelly BM. Improved method for the determination of blood glutathione. J Lab Clin Med. 1963;61:882–888. [PubMed] [Google Scholar]
- 23.Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Newgard CB, An J, Bain JR, et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. 2009;9(4):311–326. doi: 10.1016/j.cmet.2009.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah SH, Crosslin DR, Haynes CS, et al. Branched-chain amino acid levels are associated with improvement in insulin resistance with weight loss. Diabetologia. 2012;55(2):321–330. doi: 10.1007/s00125-011-2356-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah SH, Bain JR, Muehlbauer MJ, et al. Association of a peripheral blood metabolic profile with coronary artery disease and risk of subsequent cardiovascular events. Circ Cardiovasc Genet. 2010;3(2):207–214. doi: 10.1161/CIRCGENETICS.109.852814 [DOI] [PubMed] [Google Scholar]
- 27.Tillin T, Hughes AD, Wang Q, et al. Diabetes risk and amino acid profiles: cross-sectional and prospective analyses of ethnicity, amino acids and diabetes in a South Asian and European cohort from the SABRE (Southall And Brent REvisited) study. Diabetologia. 2015;58(5):968–979. doi: 10.1007/s00125-015-3517-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun H, Lu G, Ren S, Chen J, Wang Y. Catabolism of branched-chain amino acids in heart failure: insights from genetic models. Pediatr Cardiol. 2011;32(3):305–310. doi: 10.1007/s00246-010-9856-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Piscopo P, Crestini A, Adduci A, et al. Altered oxidative stress profile in the cortex of mice fed an enriched branched-chain amino acids diet: possible link with amyotrophic lateral sclerosis? J Neurosci Res. 2011;89(8):1276–1283. doi: 10.1002/jnr.22655 [DOI] [PubMed] [Google Scholar]
- 30.Zhenyukh O, Civantos E, Ruiz-Ortega M, et al. High concentration of branched-chain amino acids promotes oxidative stress, inflammation and migration of human peripheral blood mononuclear cells via mTORC1 activation. Free Radic Biol Med. 2017;104:165–177. doi: 10.1016/j.freeradbiomed.2017.01.009 [DOI] [PubMed] [Google Scholar]
- 31.Mi N, Zhang XJ, Ding Y, et al. Branched-chain amino acids attenuate early kidney injury in diabetic rats. Biochem Biophys Res Commun. 2015;466(2):240–246. doi: 10.1016/j.bbrc.2015.09.017 [DOI] [PubMed] [Google Scholar]
- 32.Tai ES, Tan ML, Stevens RD, et al. Insulin resistance is associated with a metabolic profile of altered protein metabolism in Chinese and Asian-Indian men. Diabetologia. 2010;53(4):757–767. doi: 10.1007/s00125-009-1637-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yamakado M, Nagao K, Imaizumi A, et al. Plasma free amino acid profiles predict four-year risk of developing diabetes, metabolic syndrome, dyslipidemia, and hypertension in Japanese population. Sci Rep. 2015;5(1):11918. doi: 10.1038/srep11918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Um SH, D’Alessio D, Thomas G. Nutrient overload, insulin resistance, and ribosomal protein S6 kinase 1, S6K1. Cell Metab. 2006;3(6):393–402. doi: 10.1016/j.cmet.2006.05.003 [DOI] [PubMed] [Google Scholar]
- 35.Macotela Y, Emanuelli B, Bang AM, et al. Dietary leucine–an environmental modifier of insulin resistance acting on multiple levels of metabolism. PLoS One. 2011;6(6):e21187. doi: 10.1371/journal.pone.0021187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Magkos F, Bradley D, Schweitzer GG, et al. Effect of Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding on branched-chain amino acid metabolism. Diabetes. 2013;62(8):2757–2761. doi: 10.2337/db13-0185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Walajtys-Rode E, Williamson JR. Effects of branched chain alpha-ketoacids on the metabolism of isolated rat liver cells. III. Interactions with pyruvate dehydrogenase. J Biol Chem. 1980;255(2):2757–2761. doi: 10.1016/S0021-9258(19)86189-6 [DOI] [PubMed] [Google Scholar]