Abstract
Aim
Anhedonia in major depressive disorder may be resistant to first-line antidepressants. We examined the effect of vortioxetine, a multimodal antidepressant, on anhedonia-like symptoms in Japanese patients with major depressive disorder.
Methods
This was a post hoc analysis of an 8-week, randomized, double-blind, placebo-controlled, phase 3 study of vortioxetine (10 mg or 20 mg) in Japanese patients aged 20–75 years with recurrent major depressive disorder and a Montgomery–Åsberg Depression Rating Scale (MADRS) total score of at least 26. The primary outcome was the mean change from baseline to week 8 in anhedonia-like symptoms as measured by MADRS anhedonia factor score, composed of: Q1, apparent sadness; Q2, reported sadness; Q6, concentration; Q7, lassitude; and Q8, inability to feel. Mean change in MADRS total score and anhedonia factor score were compared among treatment groups, with data categorized by median baseline anhedonia factor score (0–17 or ≥18).
Results
Data were available for 489 patients. The least-squares mean difference in MADRS anhedonia factor score change from baseline to week 8 versus placebo was −1.34 for vortioxetine 10 mg (P = 0.0300) and −1.77 for vortioxetine 20 mg (P = 0.0044). The least-squares mean difference between vortioxetine and placebo in MADRS total score change from baseline to week 8 was −3.11 (10 mg dose) and −3.37 (20 mg dose) for patients with a higher baseline anhedonia factor score (≥18), and −2.08 (10 mg) and −2.61 (20 mg) for patients with a lower baseline score (0–17).
Conclusion
This post hoc analysis suggests that vortioxetine may have therapeutic potential in patients with anhedonia-like symptoms of major depressive disorder. ClinicalTrials.gov identifier for primary study: NCT02389816.
Keywords: anhedonia, antidepressant, Japanese, major depressive disorder, vortioxetine
Introduction
The symptoms of major depressive disorder (MDD) are heterogeneous; nine symptom categories are defined as criteria for a diagnosis of MDD according to the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5).1 Of these symptoms, the reduced ability to feel pleasure (anhedonia) is a core symptom of depression and a key diagnostic criterion for an MDD episode.2–4 Anhedonia is a particularly difficult symptom to treat; increasing evidence suggests that current first-line treatment options (eg, selective serotonin reuptake inhibitors [SSRIs]) do not adequately address motivational and reward-processing deficits in depression.5 One study found that anhedonia was the only unique negative predictor of time to remission with an SSRI and the number of depression-free days over a 24-week period, which suggests that anhedonia may be a marker of depression severity and could prolong time to remission.6 Consequently, anhedonia may be an important treatment target. Owing to lower expectations of efficacy with current antidepressants, transcranial magnetic stimulation and electroconvulsive therapy have also been investigated for the treatment of anhedonia.7,8 Although statistically or clinically significant improvements in anhedonia have been demonstrated with neuromodulatory interventions,7,8 effective pharmacotherapy is still desired for anhedonia.9
Reward processing comprises three distinct neuropsychological components (essentially “learning”, “liking”, and “wanting”), each of which involve specific neurobiological mechanisms related to various brain regions including the mesolimbic pathway and prefrontal cortex.10 Dopaminergic neurons play a central role in the brain’s reward system by triggering the sensation of pleasure following the achievement of goals.11 Ascending noradrenergic neurons at the locus coeruleus are also thought to be involved in the brain’s reward system.12,13 Neuroimaging and pharmacological studies generally support the hypothesis that anhedonia is the result of dysfunctional reward processing, primarily due to an altered dopaminergic pathway.9,11,14 Noradrenergic pathways, as well as serotonergic, opioid, and glutaminergic pathways, may also play a role in the development of anhedonia in MDD.9,15
Vortioxetine is a multimodal antidepressant that inhibits serotonin reuptake in the synaptic cleft, leading to increased synaptic serotonin (the traditional target of SSRIs).16 Vortioxetine also acts on specific serotonin receptors, modulating the release of serotonin, which, in turn, is involved in the downstream release of neurotransmitters such as glutamate, dopamine, norepinephrine, acetylcholine, and histamine.17–19 Preclinical studies have revealed that norepinephrine and dopamine, in addition to serotonin, are increased in the brain of vortioxetine-treated rats.20 Vortioxetine was approved for the treatment of MDD in Japan following the results of a phase 3 clinical trial of vortioxetine in Japanese patients with MDD that assessed the change from baseline in Montgomery–Åsberg Depression Rating (MADRS) total score after 8 weeks. In the trial, both vortioxetine 10 mg and 20 mg doses significantly reduced MADRS total score compared with placebo at the end of week 8. Both doses were also generally well tolerated.21
The robustness of data collected from the phase 3 trial was the basis for several post hoc analyses, including that discussed here. In other analyses, the authors investigated the therapeutic potential of vortioxetine for anxious depression and early improvement with vortioxetine as a predictor of response and remission in Japanese patients, the results of which have been published in this journal.22,23
Herein, we describe a post hoc analysis investigating the therapeutic potential of vortioxetine for anhedonia-like symptoms of MDD, as assessed by change in MADRS anhedonia factor score from baseline. To our knowledge, this is the first of such studies in an Asian population. An exploratory analysis was also performed to examine the potential of vortioxetine for the treatment of MDD that is largely characterized by anhedonia-like symptoms. Our hypothesis was that both doses of vortioxetine will significantly reduce anhedonia compared with placebo in patients with MDD of an Asian population.
Patients and Methods
Study Design
This was a post hoc analysis of CCT-004, a multicenter, randomized, double-blind, placebo-controlled, parallel-group, phase 3 trial investigating the safety and efficacy of vortioxetine in Japanese patients with MDD (ClinicalTrials.gov identifier: NCT02389816).21 The trial was conducted from April 10, 2015 to March 16, 2018. Eligible patients completed a 1–3-week screening period and a single-blind 1-week placebo run-in period to minimize the placebo response. Patients were then randomly assigned (1:1:1) to receive vortioxetine 10 mg, vortioxetine 20 mg, or placebo once daily for 8 weeks during a double-blind treatment period. Two vortioxetine doses were investigated because both 10 mg and 20 mg demonstrated nominally significant improvements in MADRS total score and response rate, and acceptable tolerability, in the secondary analysis of a randomized, placebo-controlled, multinational, 8-week, phase 2/3 trial of vortioxetine that included Japanese participants with MDD.24
After the treatment period, study drugs were subsequently withdrawn, at which point patients entered a 4-week safety follow-up period for the analysis of outcomes of adverse events. All patients provided written informed consent before study entry. Investigations were conducted in accordance with the Declaration of Helsinki and the International Council on Harmonisation tripartite guideline on Good Clinical Practice.25 The clinical study protocol, the investigator’s brochure, a sample informed consent form, and other study-related documents were reviewed and approved by the local or central Institutional Review Boards of all study sites (Supplemental Information S1).
Patients
Data for patients who comprised the full analysis set in the primary study were included in this post hoc analysis; these were patients who received at least one dose of study treatment during the 8-week, double-blind, randomized treatment period. Full inclusion, exclusion, and study entry criteria have been described previously.21 Briefly, patients were adults aged 20–75 years and had a primary diagnosis of recurrent MDD according to the DSM, fourth edition (DSM-IV) text revision (TR) criteria for 296.3x, corresponding to F33 in ICD-10,26 with the current major depressive episode having lasted 3–12 months (inclusive) at the time of enrollment for clear diagnostic certainty and exclusion of possible concurrent mental disorders. Patients were required to have a MADRS total score ≥26 from screening to study drug initiation, to include patients with moderate or severe MDD. Patients were excluded if they had previously not responded to two or more antidepressants prescribed for at least 6 weeks, or if they tested positive in a urine drug-screening test. Patients who were diagnosed with any psychiatric disorder as defined by the DSM-IV-TR and patients who had any substance-induced mood disorder (excluding nicotine- and caffeine-related disorders) were also excluded.
Efficacy Outcomes
The primary outcome of this analysis was change in anhedonia-like symptoms, as measured by the baseline to week 8 change in MADRS anhedonia factor score, composed of the following items, measured at each visit: Q1, apparent sadness; Q2, reported sadness; Q6, concentration; Q7, lassitude; and Q8, inability to feel.27–29 Mean changes from baseline to week 8 in MADRS anhedonia factor score and total score were compared among treatment groups, with patient data categorized by median baseline anhedonia factor score (0–17 or ≥18). Other key outcomes from the primary study (week 8 MADRS response and remission) were analyzed by anhedonia subgroup. MADRS response was defined as patients having experienced at least a 50% decrease in the MADRS total score from baseline. Remission was defined as patients having experienced a decrease in MADRS total score to 10 or lower from baseline.
Statistical Analyses
Baseline demographics are summarized descriptively. Changes from baseline in the MADRS anhedonia factor score after 8 weeks (last observation carried forward [LOCF]) were analyzed using an analysis of covariance (ANCOVA) model, with treatment as a fixed effect and the baseline MADRS anhedonia factor score as a covariate. Least-squares (LS) means and two-sided 95% confidence intervals (CIs) were provided for each treatment group. Differences in the LS means between each vortioxetine group and the placebo group (each vortioxetine group − placebo group) with two-sided 95% CIs were calculated.
Changes from baseline in the MADRS anhedonia factor score after 8 weeks (LOCF) were further analyzed using a model including the median MADRS anhedonia factor score at baseline (dichotomous categorization by median score at baseline; 0–17 or ≥18) and its interaction with treatment. A similar analysis was performed for the change from baseline in the MADRS total score after 8 weeks (LOCF). MADRS response and remission rates at week 8 (LOCF) and the two-sided 95% CIs were calculated by treatment group in patients with a median MADRS anhedonia factor score of 0–17 or ≥18 at baseline.
Results
Patients
Patient demographics and baseline characteristics, including disease severity (MADRS score), were well balanced among treatment groups in the primary study and have been described previously.21
Of the 493 patients randomly assigned to treatment, four patients were excluded from the analysis because they received no study drug after randomization, or owing to duplicate enrollment, as described previously.21 There were 489 patients included in this post hoc analysis: 161 of these patients received placebo, 165 received vortioxetine 10 mg, and 163 received vortioxetine 20 mg. Mean MADRS total score and anhedonia factor score at baseline were similar among treatment groups (Table 1).
Table 1.
Baseline Disease Characteristics
| Characteristics | Placebo (n=161) | Vortioxetine 10 mg (n=165) | Vortioxetine 20 mg (n=163) |
|---|---|---|---|
| Mean (SD) MADRS anhedonia factor score | 17.9 (2.4) | 18.0 (2.5) | 17.9 (2.3) |
| ≥18 at baseline, n (%) | 87 (54.0) | 102 (61.8) | 94 (57.7) |
| ≥18 at baseline, mean factor score (SD) | 19.7 (1.6) | 19.5 (1.7) | 19.4 (1.5) |
| 0–17 at baseline, n (%) | 74 (46.0) | 63 (38.2) | 69 (42.3) |
| 0–17 at baseline, mean factor score (SD) | 15.9 (1.2) | 15.6 (1.2) | 15.8 (1.3) |
| Mean (SD) MADRS total score | 30.5 (3.9) | 30.8 (3.7) | 30.6 (3.6) |
| Anhedonia factor score ≥18 at baseline, mean total score (SD) | 32.8 (3.8) | 32.3 (3.7) | 32.4 (3.6) |
| Anhedonia factor score 0–17 at baseline, mean total score (SD) | 27.9 (1.7) | 28.3 (2.0) | 28.2 (2.0) |
Abbreviations: MADRS, Montgomery–Åsberg Depression Rating Scale; SD, standard deviation.
Study Assessments
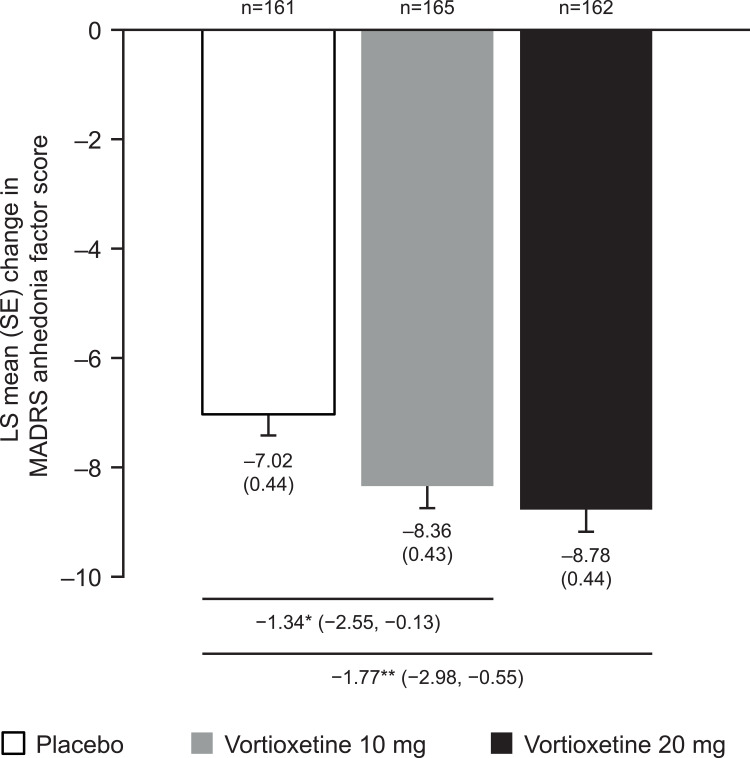
Compared with placebo, the LS mean change in MADRS anhedonia factor score from baseline to the end of week 8 was significantly larger with vortioxetine 10 mg (LS mean difference −1.34; P=0.0300) and vortioxetine 20 mg (LS mean difference −1.77; P=0.0044; Figure 1). An approximately 30% larger effect size was observed for patients receiving vortioxetine 20 mg than for those receiving the 10 mg dose (−0.318 vs −0.241), which indicates a dose–response relationship.
Figure 1.
Change from baseline to week 8 (LOCF) in MADRS anhedonia factor score. *P<0.05, **P<0.01. Data are LS mean (SE) change in MADRS anhedonia factor score and LS mean difference versus placebo (95% CI). MADRS anhedonia factor is derived from the sum of the following items: Q1, apparent sadness; Q2, reported sadness; Q6, concentration; Q7, lassitude; and Q8, inability to feel.
Abbreviations: CI, confidence interval; LOCF, last observation carried forward; LS, least-squares; MADRS, Montgomery–Åsberg Depression Rating Scale; SE, standard error.
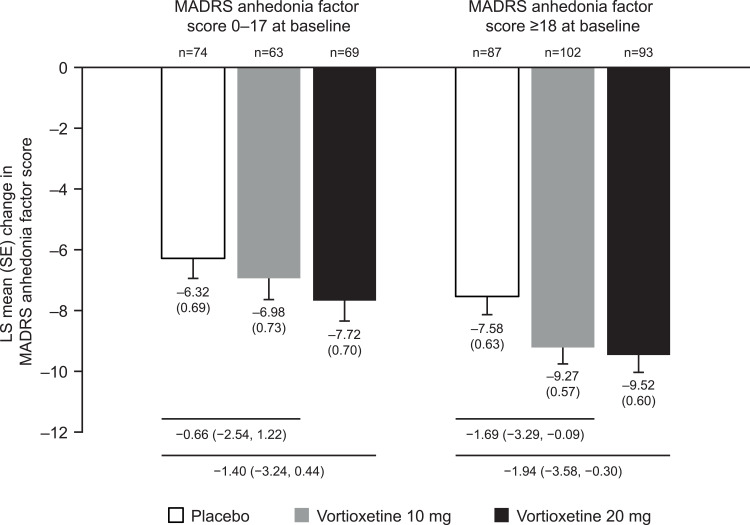
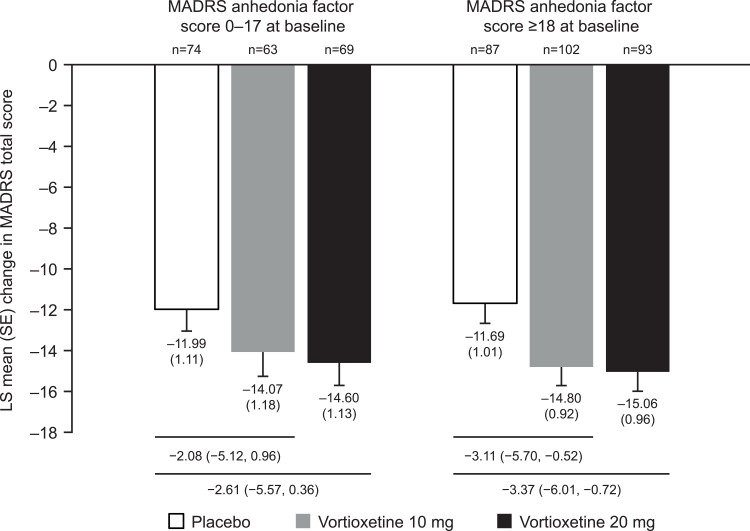
With respect to MADRS anhedonia factor score change from baseline to week 8, the LS mean difference (95% CI) versus placebo was −1.69 (−3.29, −0.09) with vortioxetine 10 mg and −1.94 (−3.58, −0.30) with vortioxetine 20 mg for patients with an anhedonia factor score of at least 18 at baseline; the LS mean difference (95% CI) versus placebo was −0.66 (−2.54, 1.22) with vortioxetine 10 mg and −1.40 (−3.24, 0.44) with vortioxetine 20 mg for patients with a lower baseline anhedonia factor score (0–17; Figure 2). A similar trend was observed for the change in MADRS total score from baseline to week 8 (Figure 3). The LS mean difference (95% CI) versus placebo in MADRS total score change was −3.11 (−5.70, −0.52) with vortioxetine 10 mg and −3.37 (−6.01, −0.72) with vortioxetine 20 mg for patients with a higher anhedonia factor score at baseline; for patients with a lower baseline score, the LS mean difference (95% CI) versus placebo was −2.08 (−5.12, 0.96) with vortioxetine 10 mg and −2.61 (−5.57, 0.36) with vortioxetine 20 mg.
Figure 2.
Change from baseline to week 8 (LOCF) in MADRS anhedonia factor score categorized by median baseline anhedonia factor score (0–17 or ≥18). Data are LS mean (SE) change in MADRS anhedonia factor score and LS mean difference versus placebo (95% CI). MADRS anhedonia factor is derived from the sum of the following items: Q1, apparent sadness; Q2, reported sadness; Q6, concentration; Q7, lassitude; and Q8, inability to feel.
Abbreviations: CI, confidence interval; LOCF, last observation carried forward; LS, least-squares; MADRS, Montgomery–Åsberg Depression Rating Scale; SE, standard error.
Figure 3.
Change from baseline to week 8 (LOCF) in MADRS total score categorized by median baseline anhedonia factor score (0–17 or ≥18). Data are LS mean (SE) change in MADRS total score and LS mean difference versus placebo (95% CI). MADRS anhedonia factor is derived from the sum of the following items: Q1, apparent sadness; Q2, reported sadness; Q6, concentration; Q7, lassitude; and Q8, inability to feel.
Abbreviations: CI, confidence interval; LOCF, last observation carried forward; LS, least-squares; MADRS, Montgomery–Åsberg Depression Rating Scale; SE, standard error.
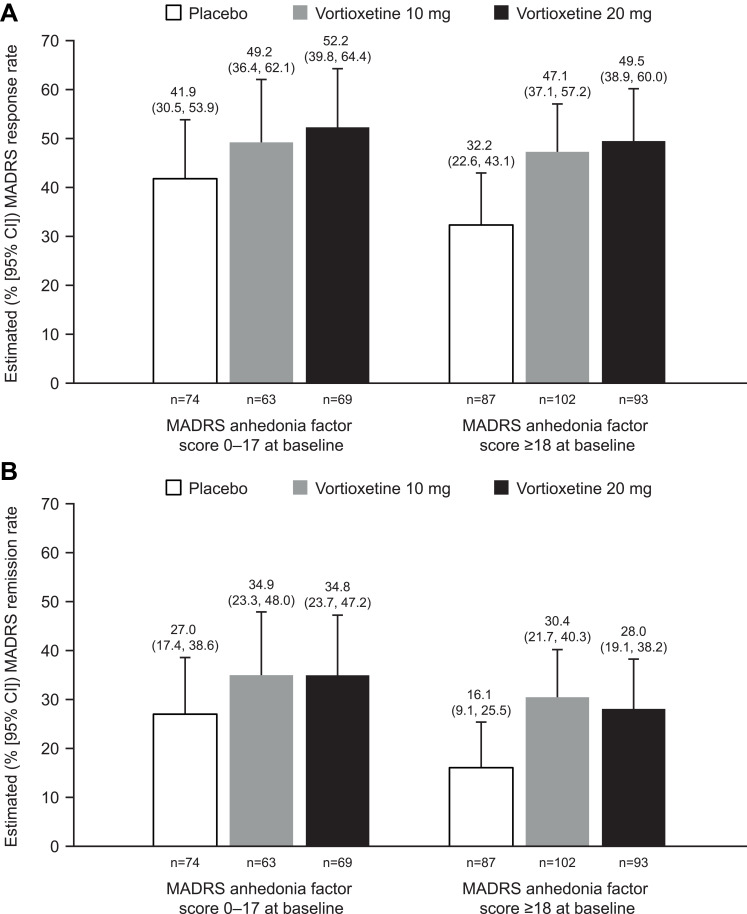
For patients with a MADRS anhedonia factor score of at least 18 at baseline, MADRS response rates (95% CI) were 32.2% (22.6%, 43.1%), 47.1% (37.1%, 57.2%), and 49.5% (38.9%, 60.0%) and MADRS remission rates (95% CI) were 16.1% (9.1%, 25.5%), 30.4% (21.7%, 40.3%), and 28.0% (19.1%, 38.2%) for placebo, vortioxetine 10 mg, and vortioxetine 20 mg, respectively, at week 8 (Figure 4). For patients with a lower baseline anhedonia factor score (0–17), week 8 response rates (95% CI) were 41.9% (30.5%, 53.9%), 49.2% (36.4%, 62.1%), and 52.2% (39.8%, 64.4%) and remission rates (95% CI) were 27.0% (17.4%, 38.6%), 34.9% (23.3%, 48.0%), and 34.8% (23.7%, 47.2%) for placebo, vortioxetine 10 mg, and vortioxetine 20 mg, respectively (Figure 4).
Figure 4.
MADRS (A) response and (B) remission rates at week 8 (LOCF) categorized by median baseline anhedonia factor score (0–17 or ≥18). Data are rate estimates (95% CI). MADRS anhedonia factor is derived from the sum of the following items: Q1, apparent sadness; Q2, reported sadness; Q6, concentration; Q7, lassitude; and Q8, inability to feel. Response for anhedonia was defined as having a ≥50% decrease in the MADRS total score from baseline. Remission of anhedonia was defined as a decrease in total MADRS score to ≤10 from baseline.
Abbreviations: CI, confidence interval; LOCF, last observation carried forward; LS, least-squares; MADRS, Montgomery–Åsberg Depression Rating Scale.
Discussion
Anhedonia, a core symptom of depression, is hypothesized to result from dysfunctional reward processing, involving the dopaminergic system as well as several other neurotransmitter systems and various regions of the brain.9,10 Anhedonia is generally resistant to common first-line antidepressant options (such as SSRIs and serotonin–norepinephrine reuptake inhibitors), owing to their inadequate effect on dopamine transmission.30 Anhedonia can therefore persist in individuals with MDD who have experienced improvement in other symptoms and may continue to affect quality of life.31,32
Multiple pharmacological treatment approaches for anhedonia have been investigated over the years; certain monoaminergic antidepressants, glutamatergic agents, psychedelics, and stimulants have all shown some degree of efficacy in improving anhedonia, although these results are preliminary.27,33–40 It has also been suggested that the involvement of indirect modulation of the dopaminergic circuit by antidepressants without dopaminergic affinity could improve anhedonia in patients with MDD.41,42 It is hypothesized that vortioxetine may have a distinct effect on anhedonia owing to the direct and indirect influence of the agent on relevant neurotransmitter systems;15,16,20,43,44 in particular, by stimulating an increase in extracellular dopamine levels, as demonstrated in various regions of the rodent brain.20
In this post hoc analysis of a phase 3 study investigating Japanese patients with MDD, treatment with vortioxetine 10 mg or 20 mg once daily resulted in significant reductions from baseline in MADRS anhedonia factor scores compared with placebo at the end of the 8-week treatment period. These findings are consistent with those from a previous study that showed a significant decrease from baseline in Snaith–Hamilton Pleasure Scale (SHAPS) and MADRS anhedonia factor scores after 8 weeks of vortioxetine treatment,27 and thus provide further evidence to support vortioxetine as a potential therapeutic option for anhedonia as a core symptom of MDD. A recent pooled analysis of global data has also shown that vortioxetine 10 mg and 20 mg resulted in greater reductions in MADRS anhedonia factor score than placebo.15
Given that the risks of anhedonia and other depressive symptoms may differ by race and ethnicity,45 this post hoc analysis provided further evidence to support the therapeutic potential of vortioxetine for Japanese patients with MDD.21 To our knowledge, this is the first exploratory study of the therapeutic potential of vortioxetine for anhedonia-like symptoms to be conducted in an Asian population. Antidepressive efficacy was observed with vortioxetine for all tested parameters, even in patients with more severe anhedonia at baseline (MADRS anhedonia factor score ≥18). These findings are consistent with the primary study, in which vortioxetine demonstrated improvements versus placebo regardless of depression severity, as assessed by MADRS total score at baseline.21 Furthermore, this study provides evidence to suggest that patients with a higher baseline MADRS anhedonia factor score may experience greater improvements with vortioxetine compared with all enrolled patients, although the threshold for clinically significant improvement in MADRS anhedonia factor score has not yet been established. The effect size of vortioxetine on MADRS anhedonia factor score was modest, but similar to the size of effect of vortioxetine on overall MADRS score.46 It may follow that the improvement of MADRS anhedonia factor score seen with vortioxetine is of clinical significance, because the improvement in overall MADRS score was deemed clinically significant and led to regulatory approval of vortioxetine in Japan.
Hammond and Parker et al used factor analysis and principal component analysis by drawing on data gathered from geriatric patients with MDD to determine the core symptoms of MDD from the MADRS items; subsequently, MADRS anhedonia factor was identified.28,29 Because this scale was not determined through factor analysis or principal component analysis of data from non-geriatric adult patients with MDD, neurochemical alterations in geriatric depressive abnormalities, such as vascular depression, may have contributed to the identification of the scale; however, geriatric patients with severe physical disability or neurologic illness were excluded from the analysis used for subscale identification.28,29 Since then, studies have evaluated anhedonia symptoms with MADRS anhedonia factor in non-geriatric adult patients with MDD.27,37 MADRS anhedonia factor is not designed to evaluate anhedonia specifically; however, anhedonia-specific assessment scales such as SHAPS have not yet been adequately validated for use in clinical trials, unlike the MADRS.47 Although MADRS anhedonia factor was not formulated to reflect anhedonia severity by definition, there does appear to be high correlation between MADRS anhedonia factor scores and SHAPS scores, which suggests that MADRS anhedonia factor score indicates an aspect of symptom severity of anhedonia.27
Some limitations of this study should be acknowledged. First, this is a post hoc analysis of a study that investigated the efficacy of vortioxetine in relation to MDD;21 specific evaluation of anhedonia was not an aim of the trial, and an investigation of the effect of baseline MADRS anhedonia factor score and its interaction with treatment was not designated in the trial, and thus statistical significance was not examined. Second, conclusions regarding the efficacy of vortioxetine in relation to anhedonia cannot be made based on this analysis alone because the anhedonia MADRS subscale was not designed for the stand-alone assessment of anhedonia. Third, it is not yet clear whether improvements in anhedonia observed with vortioxetine treatment are clinically meaningful. Fourth, although our data suggest that the efficacy of vortioxetine is not affected by baseline anhedonia score, it remains to be clarified whether these findings can be generalized to other antidepressants. Anhedonia appears to be largely resistant to treatment with SSRIs48 and has been shown to be a predictor of poorer outcomes.6 It should be also noted that treatment response to an SSRI has previously been negatively correlated with the severity of anhedonia at baseline.49 Finally, bias in the interpretation of results cannot be ruled out, because this analysis was funded by a pharmaceutical company that markets vortioxetine and employs several of the authors of this paper.
Conclusions
In summary, this post hoc analysis, the first of its kind involving patients of an Asian population, provides evidence to suggest that vortioxetine may have therapeutic potential in patients with anhedonia-like symptoms of MDD, regardless of the severity of the anhedonia at treatment initiation. Based on these results, further study of the therapeutic potential of vortioxetine in anhedonia is warranted.
Acknowledgments
We would like to pay our respects to Dr Yoshinori Watanabe (Himorogi Psychiatric Institute, Tokyo, Japan), who passed away in August of 2021 shortly before submission of this manuscript. We are grateful for his contributions as an investigator in the primary study and the development of this manuscript. Y.W. received speaker’s honoraria from Janssen Pharmaceutical K.K., Meiji Seika Pharma Co., Ltd, Mitsubishi Tanabe Pharma Corp., Mochida Pharmaceutical Co., Ltd, Otsuka Pharmaceutical Co., Ltd, Pfizer Japan Inc., Sumitomo Dainippon Pharma Co., and Takeda Pharmaceutical Co., Ltd. We are grateful to current and former employees of Takeda Pharmaceutical Co. and Lundbeck Japan for their contributions to the study: Akira Nishimura and Kiyofumi Sasai (executed the primary clinical trial); Takafumi Akimoto and Aya Makita (supported the design of the analysis); and Isao Inada, Akihiro Takano, and Manami Imazaki (supported the interpretation of the results). Medical writing support was provided by Svetha Sankar, BSc, BVMS, of Oxford PharmaGenesis, Melbourne, Australia, and was funded by Takeda Pharmaceutical Co., Ltd.
Funding Statement
This study was funded by Takeda Pharmaceutical Co., Ltd.
Abbreviations
CI, confidence interval; DSM, Diagnostic and Statistical Manual of Mental Disorders; LOCF, last observation carried forward; LS, least-squares; MADRS, Montgomery–Åsberg Depression Rating Scale; MDD, major depressive disorder; SHAPS, Snaith–Hamilton Pleasure Scale; SSRI, selective serotonin reuptake inhibitor.
Data Sharing Statement
The data sets, including the redacted study protocol, redacted statistical analysis plan, and individual participant data supporting the results reported in this article, will be made available by the corresponding author within 3 months from initial request to researchers who provide a methodologically sound proposal. The data will be provided after their de-identification, in compliance with applicable privacy laws, data protection, and requirements for consent and anonymization.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in study conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Disclosure
K.W. has received manuscript fees or speaker’s honoraria from Astellas, Daiichi Sankyo, GlaxoSmithKline, Janssen Pharmaceuticals, Kyowa Pharmaceutical Industry, Lilly, Meiji Seika Pharma Co., Ltd, Mitsubishi Tanabe Pharma Corp., MSD, Otsuka Pharmaceutical Co., Pfizer, Shionogi Inc., Sumitomo Dainippon Pharma Co., Ltd, Takeda Pharmaceutical Co., Ltd, and Yoshitomi; has received research and grant support from Astellas, Daiichi Sankyo, Eisai, Meiji Seika Pharma Co., Ltd, Mitsubishi Tanabe Pharma Corp., MSD, Otsuka Pharmaceutical Co., Ltd, Pfizer, and Shionogi Inc.; is a consultant for Eisai, Janssen Pharmaceutical, Kyowa Pharmaceutical, Lilly, Mitsubishi Tanabe Pharma Corp., Otsuka Pharmaceutical Co., Ltd, Pfizer, Sumitomo Dainippon Pharma Co., Ltd, Taisho Toyama Pharmaceutical, Lundbeck, Viatris, and Takeda Pharmaceutical Co., Ltd outside the submitted work. S.F., T.M., T.K., K.I., T.N., and K.F. are employees of Takeda Pharmaceutical Co., Ltd. Y.M. is an employee of Lundbeck Japan K.K. T.I. served as medical Officer of the primary study; has received personal fees from Daiichi Sankyo, Janssen Pharmaceuticals, Lilly, Mochida Pharmaceutical Co., Ltd, MSD, Taisho Toyama Pharmaceutical, Takeda Pharmaceutical Co., Ltd, and Yoshitomiyakuhin; has received grants from Astellas, Eisai, Shionogi Inc., and Tsumura; has received grants and personal fees from Sumitomo Dainippon Pharma, Kyowa Pharmaceutical Industry, Meiji Seika Pharma Co., Ltd, Mitsubishi Tanabe Pharma Corp., Novartis Pharma, Otsuka Pharmaceutical Co., Ltd, and Pfizer; and is a member of the advisory boards of Mitsubishi Tanabe Pharma Corp., Novartis Pharma, and Pfizer. The authors report no other conflicts of interest in this work.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington (VA): American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Dichter G. Anhedonia in unipolar major depressive disorder: a review. Open Psychiatr J. 2010;4:1–9. doi: 10.2174/1874354401004010001 [DOI] [Google Scholar]
- 3.Uher R, Perlis RH, Henigsberg N, et al. Depression symptom dimensions as predictors of antidepressant treatment outcome: replicable evidence for interest-activity symptoms. Psychol Med. 2012;42:967–980. doi: 10.1017/S0033291711001905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vrieze E, Demyttenaere K, Bruffaerts R, et al. Dimensions in major depressive disorder and their relevance for treatment outcome. J Affect Disord. 2014;155:35–41. doi: 10.1016/j.jad.2013.10.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Treadway MT, Zald DH. Reconsidering anhedonia in depression: lessons from translational neuroscience. Neurosci Biobehav Rev. 2011;35:537–555. doi: 10.1016/j.neubiorev.2010.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McMakin DL, Olino TM, Porta G, et al. Anhedonia predicts poorer recovery among youth with selective serotonin reuptake inhibitor treatment-resistant depression. J Am Acad Child Adolesc Psychiatry. 2012;51:404–411. doi: 10.1016/j.jaac.2012.01.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fukuda AM, Kang JWD, Gobin AP, et al. Effects of transcranial magnetic stimulation on anhedonia in treatment resistant major depressive disorder. Brain Behav. 2021;11:e2329. doi: 10.1002/brb3.2329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang T, He K, Bai T, et al. Altered neural activity in the reward-related circuit and executive control network associated with amelioration of anhedonia in major depressive disorder by electroconvulsive therapy. Prog Neuropsychopharmacol Biol Psychiatry. 2021;109:110193. doi: 10.1016/j.pnpbp.2020.110193 [DOI] [PubMed] [Google Scholar]
- 9.Höflich A, Michenthaler P, Kasper S, et al. Circuit mechanisms of reward, anhedonia, and depression. Int J Neuropsychopharmacol. 2019;22:105–118. doi: 10.1093/ijnp/pyy081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cléry-Melin ML, Jollant F, Gorwood P. Reward systems and cognitions in major depressive disorder. CNS Spectr. 2019;24:64–77. doi: 10.1017/S1092852918001335 [DOI] [PubMed] [Google Scholar]
- 11.Juárez Olguín H, Calderón Guzmán D, Hernández García E, et al. The role of dopamine and its dysfunction as a consequence of oxidative stress. Oxid Med Cell Longev. 2016;9730467. doi: 10.1155/2016/9730467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Varazzani C, San-Galli A, Gilardeau S, et al. Noradrenaline and dopamine neurons in the reward/effort trade-off: a direct electrophysiological comparison in behaving monkeys. J Neurosci. 2015;35:7866–7877. doi: 10.1523/JNEUROSCI.0454-15.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bouret S, Richmond BJ. Sensitivity of locus coeruleus neurons to reward value for goal-directed actions. J Neurosci. 2015;35:4005–4014. doi: 10.1523/JNEUROSCI.4553-14.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cooper JA, Arulpragasam AR, Treadway MT. Anhedonia in depression: biological mechanisms and computational models. Curr Opin Behav Sci. 2018;22:128–135. doi: 10.1016/j.cobeha.2018.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McIntyre RS, Loft H, Christensen MC. Efficacy of vortioxetine on anhedonia: results from a pooled analysis of short-term studies in patients with major depressive disorder. Neuropsychiatr Dis Treat. 2021;17:575–585. doi: 10.2147/NDT.S296451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanchez C, Asin KE, Artigas F. Vortioxetine, a novel antidepressant with multimodal activity: review of preclinical and clinical data. Pharmacol Ther. 2015;145:43–57. doi: 10.1016/j.pharmthera.2014.07.001 [DOI] [PubMed] [Google Scholar]
- 17.Bang-Andersen B, Ruhland T, Jørgensen M, et al. Discovery of 1-[2-(2,4-dimethylphenylsulfanyl)phenyl]piperazine (Lu AA21004): a novel multimodal compound for the treatment of major depressive disorder. J Med Chem. 2011;54:3206–3221. doi: 10.1021/jm101459g [DOI] [PubMed] [Google Scholar]
- 18.D’Agostino A, English CD, Rey JA. Vortioxetine (brintellix): a new serotonergic antidepressant. P T. 2015;40:36–40. [PMC free article] [PubMed] [Google Scholar]
- 19.Dale E, Grunnet M, Pehrson AL, et al. The multimodal antidepressant vortioxetine may facilitate pyramidal cell firing by inhibition of 5-HT(3) receptor expressing interneurons: an in vitro study in rat hippocampus slices. Brain Res. 2018;1689:1–11. doi: 10.1016/j.brainres.2017.12.025 [DOI] [PubMed] [Google Scholar]
- 20.Pehrson AL, Cremers T, Bétry C, et al. Lu AA21004, a novel multimodal antidepressant, produces regionally selective increases of multiple neurotransmitters – a rat microdialysis and electrophysiology study. Eur Neuropsychopharmacol. 2013;23:133–145. doi: 10.1016/j.euroneuro.2012.04.006 [DOI] [PubMed] [Google Scholar]
- 21.Inoue T, Sasai K, Kitagawa T, et al. Randomized, double-blind, placebo-controlled study to assess the efficacy and safety of vortioxetine in Japanese patients with major depressive disorder. Psychiatry Clin Neurosci. 2020;74:140–148. doi: 10.1111/pcn.12956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inoue T, Fujimoto S, Marumoto T, et al. Therapeutic potential of vortioxetine for anxious depression: a post hoc analysis of data from a clinical trial conducted in Japan. Neuropsychiatr Dis Treat. 2021;17:3781–3790. doi: 10.2147/NDT.S335028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Inoue T, Fujimoto S, Marumoto T, et al. Early improvement with vortioxetine predicts response and remission: a post hoc analysis of data from a clinical trial conducted in Japan. Neuropsychiatr Dis Treat. 2021;17:3735–3741. doi: 10.2147/NDT.S340309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nishimura A, Aritomi Y, Sasai K, et al. Randomized, double-blind, placebo-controlled 8-week trial of the efficacy, safety, and tolerability of 5, 10, and 20 mg/day vortioxetine in adults with major depressive disorder. Psychiatry Clin Neurosci. 2018;72:64–72. doi: 10.1111/pcn.12565 [DOI] [PubMed] [Google Scholar]
- 25.International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH harmonized tripartite guideline: guideline for good clinical practice. J Postgrad Med. 2001;47:45–50. [PubMed] [Google Scholar]
- 26.World Health Organization. Recurrent Depressive Disorder - International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10). World Health Organization; 2019. [Google Scholar]
- 27.Cao B, Park C, Subramaniapillai M, et al. The efficacy of vortioxetine on anhedonia in patients with major depressive disorder. Front Psychiatry. 2019;10:17. doi: 10.3389/fpsyt.2019.00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hammond MF. Rating depression severity in the elderly physically ill patient: reliability and factor structure of the Hamilton and the Montgomery-Asberg Depression Rating Scales. Int J Geriatr Psychiatry. 1998;13:257–261. doi: [DOI] [PubMed] [Google Scholar]
- 29.Parker RD, Flint EP, Bosworth HB, et al. A three-factor analytic model of the MADRS in geriatric depression. Int J Geriatr Psychiatry. 2003;18:73–77. doi: 10.1002/gps.776 [DOI] [PubMed] [Google Scholar]
- 30.Dunlop BW, Nemeroff CB. The role of dopamine in the pathophysiology of depression. Arch Gen Psychiatry. 2007;64:327–337. doi: 10.1001/archpsyc.64.3.327 [DOI] [PubMed] [Google Scholar]
- 31.Cao B, Zhu J, Zuckerman H, et al. Pharmacological interventions targeting anhedonia in patients with major depressive disorder: a systematic review. Prog Neuropsychopharmacol Biol Psychiatry. 2019;92:109–117. doi: 10.1016/j.pnpbp.2019.01.002 [DOI] [PubMed] [Google Scholar]
- 32.Vinckier F, Gourion D, Mouchabac S. Anhedonia predicts poor psychosocial functioning: results from a large cohort of patients treated for major depressive disorder by general practitioners. Eur Psychiatry. 2017;44:1–8. doi: 10.1016/j.eurpsy.2017.02.485 [DOI] [PubMed] [Google Scholar]
- 33.Mazza M, Squillacioti MR, Pecora RD, et al. Effect of aripiprazole on self-reported anhedonia in bipolar depressed patients. Psychiatry Res. 2009;165:193–196. doi: 10.1016/j.psychres.2008.05.003 [DOI] [PubMed] [Google Scholar]
- 34.Gargoloff PD, Corral R, Herbst L, et al. Effectiveness of agomelatine on anhedonia in depressed patients: an outpatient, open-label, real-world study. Hum Psychopharmacol. 2016;31:412–418. doi: 10.1002/hup.2557 [DOI] [PubMed] [Google Scholar]
- 35.Di Giannantonio M, Martinotti G. Anhedonia and major depression: the role of agomelatine. Eur Neuropsychopharmacol. 2012;22(Suppl 3):S505–S10. doi: 10.1016/j.euroneuro.2012.07.004 [DOI] [PubMed] [Google Scholar]
- 36.McIntyre RS, Gommoll C, Chen C, et al. The efficacy of levomilnacipran ER across symptoms of major depressive disorder: a post hoc analysis of 5 randomized, double-blind, placebo-controlled trials. CNS Spectr. 2016;21:385–392. doi: 10.1017/S1092852915000899 [DOI] [PubMed] [Google Scholar]
- 37.Tran P, Skolnick P, Czobor P, et al. Efficacy and tolerability of the novel triple reuptake inhibitor amitifadine in the treatment of patients with major depressive disorder: a randomized, double-blind, placebo-controlled trial. J Psychiatr Res. 2012;46:64–71. doi: 10.1016/j.jpsychires.2011.09.003 [DOI] [PubMed] [Google Scholar]
- 38.Lally N, Nugent AC, Luckenbaugh DA, et al. Neural correlates of change in major depressive disorder anhedonia following open-label ketamine. J Psychopharmacol. 2015;29:596–607. doi: 10.1177/0269881114568041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rizvi SJ, Geraci J, Ravindran A, et al. Predictors of response to adjunctive osmotic-release methylphenidate or placebo in patients with major depressive disorder: effects of apathy/anhedonia and fatigue. J Clin Psychopharmacol. 2014;34:755–759. doi: 10.1097/JCP.0000000000000211 [DOI] [PubMed] [Google Scholar]
- 40.Carhart-Harris RL, Bolstridge M, Rucker J, et al. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. 2016;3:619–627. doi: 10.1016/S2215-0366(16)30065-7 [DOI] [PubMed] [Google Scholar]
- 41.Martinotti G, Sepede G, Gambi F, et al. Agomelatine versus venlafaxine XR in the treatment of anhedonia in major depressive disorder: a pilot study. J Clin Psychopharmacol. 2012;32:487–491. doi: 10.1097/JCP.0b013e31825d6c25 [DOI] [PubMed] [Google Scholar]
- 42.Costi S, Morris LS, Kirkwood KA, et al. Impact of the KCNQ2/3 channel opener ezogabine on reward circuit activity and clinical symptoms in depression: results from a randomized controlled trial. Am J Psychiatry. 2021;178:437–446. doi: 10.1176/appi.ajp.2020.20050653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lu Y, Ho CS, McIntyre RS, et al. Effects of vortioxetine and fluoxetine on the level of brain derived neurotrophic factors (BDNF) in the hippocampus of chronic unpredictable mild stress-induced depressive rats. Brain Res Bull. 2018;142:1–7. doi: 10.1016/j.brainresbull.2018.06.007 [DOI] [PubMed] [Google Scholar]
- 44.Pehrson AL, Pedersen CS, Tølbøl KS, et al. Vortioxetine treatment reverses subchronic PCP treatment-induced cognitive impairments: a potential role for serotonin receptor-mediated regulation of GABA neurotransmission. Front Pharmacol. 2018;9:162. doi: 10.3389/fphar.2018.00162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu CH, Tronick E. Prevalence and predictors of maternal postpartum depressed mood and anhedonia by race and ethnicity. Epidemiol Psychiatr Sci. 2014;23:201–209. doi: 10.1017/S2045796013000413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Iovieno N, Papakostas GI, Feeney A, et al. Vortioxetine versus placebo for major depressive disorder: a comprehensive analysis of the clinical trial dataset. J Clin Psychiatry. 2021;82. doi: 10.4088/JCP.20r13682 [DOI] [PubMed] [Google Scholar]
- 47.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. doi: 10.1192/bjp.134.4.382 [DOI] [PubMed] [Google Scholar]
- 48.Yee A, Chin SC, Hashim AH, et al. Anhedonia in depressed patients on treatment with selective serotonin reuptake inhibitor anti-depressant–a two-centered study in Malaysia. Int J Psychiatry Clin Pract. 2015;19:182–187. doi: 10.3109/13651501.2015.1031139 [DOI] [PubMed] [Google Scholar]
- 49.Dunlop K, Rizvi SJ, Kennedy SH, et al. Clinical, behavioral, and neural measures of reward processing correlate with escitalopram response in depression: a Canadian Biomarker Integration Network in Depression (CAN-BIND-1) report. Neuropsychopharmacology. 2020;45:1390–1397. doi: 10.1038/s41386-020-0688-x [DOI] [PMC free article] [PubMed] [Google Scholar]