Abstract
Objectives
Caring for patients with COVID-19 has resulted in a considerable strain on hospital capacity. One strategy to mitigate crowding is the use of ED-based observation units to care for patients who may have otherwise required hospitalization. We sought to create a COVID-19 Observation Protocol for our ED Observation Unit (EDOU) for patients with mild to moderate COVID-19 to allow emergency physicians (EP) to gather more data for or against admission and intervene in a timely manner to prevent clinical deterioration.
Methods
This was a retrospective cohort study which included all patients who were positive for SARS-CoV-2 at the time of EDOU placement for the primary purpose of monitoring COVID-19 disease. Our institution updated the ED Observation protocol partway into the study period. Descriptive statistics were used to characterize demographics. We assessed for differences in demographics, clinical characteristics, and outcomes between admitted and discharged patients. Multivariate logistic regression models were used to assess whether meeting criteria for the ED observation protocols predicted disposition.
Results
During the time period studied, 120 patients positive for SARS-CoV-2 were placed in the EDOU for the primary purpose of monitoring COVID-19 disease. The admission rate for patients in the EDOU during the study period was 35%. When limited to patients who met criteria for version 1 or version 2 of the protocol, this dropped to 21% and 25% respectively. Adherence to the observation protocol was 62% and 60% during the time of version 1 and version 2 implementation, respectively. Using a multivariate logistic regression, meeting criteria for either version 1 (OR = 3.17, 95% CI 1.34–7.53, p < 0.01) or version 2 (OR = 3.18, 95% CI 1.39–7.30, p < 0.01) of the protocol resulted in a higher likelihood of discharge. There was no difference in EDOU LOS between admitted and discharged patients.
Conclusion
An ED observation protocol can be successfully created and implemented for COVID-19 which allows the EP to determine which patients warrant hospitalization. Meeting protocol criteria results in an acceptable admission rate.
Keywords: SARS-CoV-2, Emergency department observation, Emergency department operations, COVID-19, Clinical observation units
1. Introduction
Caring for patients with COVID-19 has resulted in considerable strain on hospital capacity throughout the United States due to increased patient volumes, decreased number of beds available due to precautions, and increased numbers of patients requiring intensive care unit (ICU) beds [[1], [2], [3], [4]]. This has contributed to Emergency Department (ED) crowding in a system that was already stressed at baseline [5]. ED crowding is a well-established challenge in the United States with many deleterious effects on patient care outcomes and operational efficiency [[6], [7], [8], [9], [10], [11], [12]]. One way to mitigate ED crowding is the use of ED-based observation units to care for patients who may have otherwise required hospitalization [13,14].
ED-based observation units are well-equipped to care for patients who require further monitoring or testing to determine a need for inpatient admission, would benefit from specialty consultation not available during off-hours, or have a condition expected to require fewer than two midnights in the hospital [13,15,16]. Many protocols have been developed for common complaints that fit these criteria such as treatment of chest pain [[17], [18], [19], [20]], cellulitis [14,21], transient ischemic attacks [22], asthma [[23], [24], [25]], syncope [26], pulmonary embolism [27], and pyelonephritis [14,28,29].
Relatively few well-defined pathways have been established to care for patients with COVID-19. While those with severe COVID-19 clearly require hospitalization, a subset of patients with mild to moderate illness at the time of their ED presentation have a less predictable clinical course [30]. Emergency clinicians must decide whether to admit or discharge these patients with the limited information available at the time of the ED visit, with the risk of admitting too many – or too few – of them based on expected clinical course.
Applying lessons from the first COVID-19 surge in the spring of 2020, we sought to create a COVID-19 Observation Protocol for our ED Observation Unit (EDOU) for patients with mild to moderate COVID-19. Our goal was a protocol that would allow emergency physicians to further observe certain patients in the EDOU, gather more data for or against admission, and intervene in a timely manner to prevent clinical deterioration within 24–48 h.
2. Methods
This study was evaluated by our Institutional Human Research Committee and deemed exempt from institutional review board review.
2.1. Setting
This study was conducted at a large academic medical center which has 1019 licensed operational beds and with level 1 trauma, STEMI-receiving center, and stroke center designations. Our ED has a dedicated EDOU with a capacity of 31 beds staffed by advanced practice providers (APPs) with attending emergency physician supervision.
2.2. Protocol
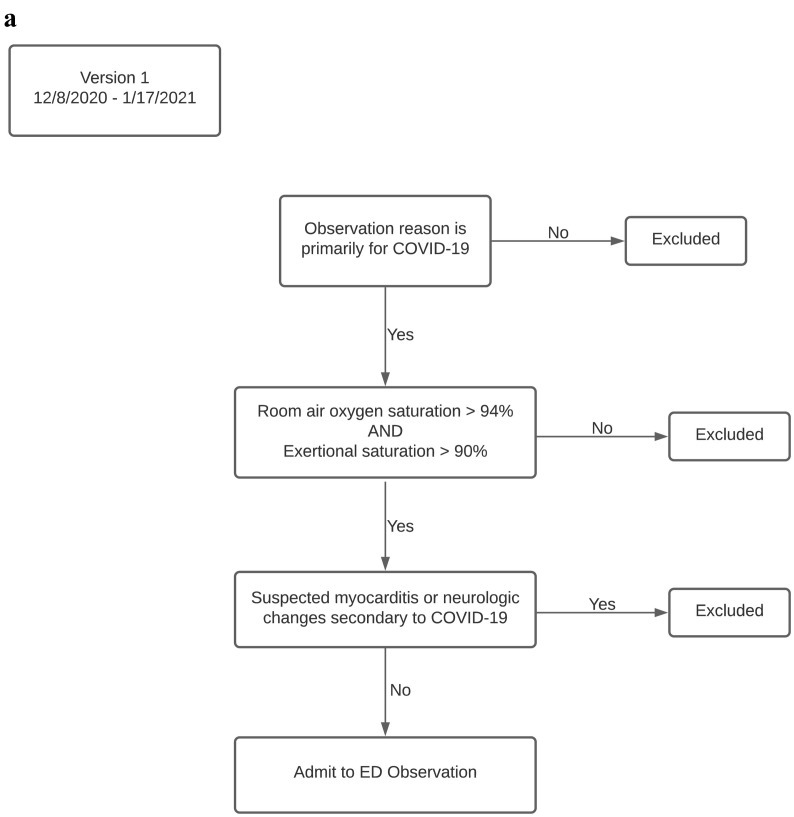
The COVID-19 ED Observation Protocol was launched on 12/8/20 (version 1) at our academic medical center (Fig. 1a). Inclusion criteria for version 1 were limited to patients with primary COVID-19 diagnosis as the reason for observation, room air oxygen saturation > 94% (or if always oxygen dependent, patients had to be at baseline oxygen therapy), and an exertional oxygen saturation > 90%. In addition to oxygen parameters, exclusion criteria included suspected myocarditis secondary to COVID-19 or neurological changes attributed to COVID-19.
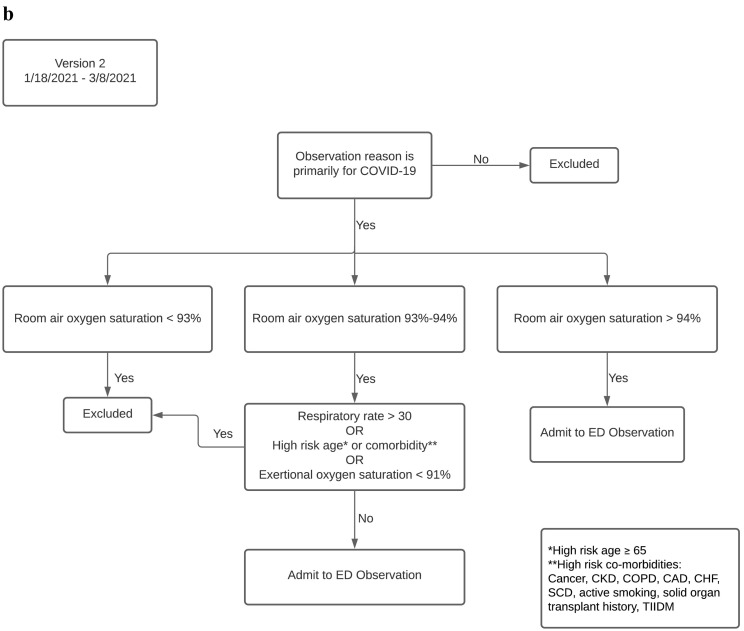
Fig. 1.
(a): Protocol Flow Chart Version 1 implemented from 12/8/2020–1/17/2021. (b): Protocol Flow Chart Version 2 implemented from 1/18/2021–3/8/2021.
The COVID-19 ED Observation Protocol was updated on 1/18/21 (version 2, Fig. 1b). Version 2 divided inclusion criteria by room air oxygen saturation and included patients with an oxygen saturation > 92%. For oxygen saturations 93–94% on room air, exclusion criteria included a respiratory rate > 30, high risk age or comorbidities, or an exertional oxygen saturation < 91%. For an oxygen saturation of 95% or greater there were no explicit exclusion criteria. If patients in this group were not of a high-risk age and did not have any high-risk comorbidities, discharge from the ED was encouraged but not required.
High risk age was defined as greater than or equal to 65 years [31]. High risk co-morbidities for severe COVID-19 were defined as cancer, chronic kidney disease (CKD), chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD) or congestive heart failure (CHF), sickle cell disease (SCD), active smoking, solid organ transplant history, or type II diabetes mellitus (TIIDM) [32].
Interventions offered during version 1 of the protocol included offering case management to set up visiting nursing services, offering appropriate patients rapid next-day paramedic assessment after discharge, and continuous oxygen and respiratory assessments. In version 1 of the protocol, disposition criteria were defined as admission to the hospital for anyone who develops a room air oxygen saturation ≤ 94%, a respiratory rate > 30, or worsening of COVID-19 symptoms. Discharge from the hospital was recommended if none of these criteria were met.
Interventions offered during version 2 of the protocol included offering case management to set up visiting nursing services, offering appropriate patients admission to the virtual observation unit for in-home monitoring, and continuous oxygen and respiratory assessments. In version 2 of the protocol, disposition criteria were defined as admission to the hospital for anyone who develops a new oxygen requirement, a respiratory rate > 30, or worsening of COVID-19 symptoms. Discharge from the hospital was recommended if none of these criteria were met.
2.3. Statistical analysis
This was a retrospective cohort study from 12/8/20 to 3/8/21. All patients who were positive for SARS-CoV-2 at time of EDOU placement for the primary purpose of monitoring COVID-19 disease were included. Patients who were incidentally positive for SARS-CoV-2 but placed in the EDOU for a different purpose (i.e., syncope, TIA, chest pain, etc.) were excluded. We retrospectively evaluated whether each patient met ED observation criteria for version 1 and version 2 of the protocol regardless of the date of their visit. Descriptive statistics were used to characterize patient demographics, clinical characteristics, and operational outcomes. We assessed for statistically significant differences between admitted and discharged patients using two-tailed t-tests for continuous variables and Chi-squared tests for categorical variables. Multivariate logistic regression models were used to assess whether meeting criteria for the ED observation protocols predicts disposition. All statistics were performed in R or Microsoft Excel.
2.4. Outcomes
The primary outcome was the admission rate from ED observation. Our goal admission rate was 30% as this was the first iteration of a protocol for observation of COVID-19 and no prior protocols existed. Secondary outcomes included adherence to the protocol, ED observation length of stay, 28-day mortality, and 14-day ED return visit.
3. Results
During the time period studied, 120 patients positive for SARS-CoV-2 were admitted to the EDOU for the primary purpose of monitoring COVID-19 disease (Table 1 ). Of these, 42 were subsequently admitted to the hospital for an admission rate of 35%. When limited to patients who met the criteria for version 1 or version 2 of the COVID-19 EDOU protocol, the admission rate dropped to 21% (15/71) and 25% (19/77) respectively (Table 2 ). The cohort consisted of 68 visits during the implementation of version 1 and 52 visits during version 2. Sixty-two percent of patients met version 1 criteria and 60% met version 2 criteria at the time each respective protocol was implemented (Table 2). Of the 26 patients who did not meet version 1 inclusion criteria, 24 should have been excluded from ED observation and directly admitted inpatient based on resting oxygen saturation less than 95%. Of the 21 patients who did not meet version 2 inclusion criteria, 16 should have been excluded from ED observation and directly admitted inpatient based on presence of a high-risk comorbidity and 9 of these should have also been excluded based on age alone.
Table 1.
Demographics and clinical characteristics. All clinical data reported from initial ED visit prior to decision made to place patient in EDOU. Bold indicates p < 0.05 for the difference between admitted and discharged patients. Two-tailed t-test used for continuous variables. Chi-squared test used for categorical variables.Abbreviations: CKD, Chronic Kidney Disease; COPD, Chronic Obstructive Pulmonary Disease; CAD, Coronary Artery Disease; CHF, Congestive Heart Failure; TIIDM, Type II Diabetes Mellitus (TIIDM)
| Full Cohort | Admitted | Discharged | P-value | |
|---|---|---|---|---|
| Number in Cohort | 120 | 42 | 78 | |
| Age median (Q1-Q3) in years | 60 (52–73) | 65 (56–77) | 59 (48–68) | 0.05 |
| Sex | 0.93 | |||
| Male | 50 (42%) | 20 (48%) | 30 (38%) | |
| Female | 70 (58%) | 22 (52%) | 48 (62%) | |
| Nadir SpO2 on RA: median (Q1-Q3) | 95 (94–96) | 94 (93–95) | 96 (94–97) | <0.01 |
| Nadir Exertional SpO2: median (Q1-Q3) | 94 (93–96) | 94 (93–95) | 95 (93–96) | 0.08 |
| Highest RR median (Q1-Q3) | 20 (20–24) | 21 (20–24) | 20 (20−22) | 0.79 |
| O2 Dependent at Baseline | 1 (1%) | 0 (0%) | 1 (1%) | – |
| Myocarditis | 0 (0%) | 0 (0%) | 0 (0%) | – |
| Neurologic Changes | 0 (0%) | 0 (0%) | 0 (0%) | – |
| Cancer | 21 (18%) | 8 (19%) | 13 (17%) | 0.94 |
| CKD | 8 (7%) | 4 (10%) | 4 (5%) | 0.59 |
| COPD | 7 (6%) | 4 (10%) | 3 (4%) | 0.39 |
| CAD/CHF | 20 (17%) | 8 (19%) | 12 (15%) | 0.79 |
| Obesity | 56 (47%) | 17 (40%) | 39 (50%) | 0.45 |
| Pregnant | 2 (2%) | 0 (0%) | 2 (3%) | – |
| Sickle Cell Disease | 0 (0%) | 0 (0%) | 0 (0%) | – |
| Current Smoker | 3 (3%) | 1 (1%) | 2 (3%) | – |
| Solid Organ Transplant | 1 (1%) | 0 (0%) | 1 (1%) | – |
| TIIDM | 26 (22%) | 8 (19%) | 18 (23%) | 0.78 |
Table 2.
Results. Bold indicates p < 0.05 for the difference between admitted and discharged patients. Two-tailed t-test used for continuous variables. Chi-squared test used for categorical variables. Abbreviations: ED LOS, Emergency Department Length of Stay; ED OBS LOS, Emergency Department Observation Unit Length of Stay; IP LOS, Inpatient Length of Stay; ED, Emergency Department
| Full Cohort | Admitted | Discharged | P-value | |
|---|---|---|---|---|
| Number in Cohort | 120 | 42 | 78 | |
| ED LOS: median (Q1-Q3) in hours | 3.8 (3.0–5.3) | 3.7 (3.0–5.0) | 3.8 (2.9–5.4) | 0.89 |
| ED OBS LOS: median (Q1-Q3) in hours | 22.5 (17.1–28.8) | 23.8 (18.4–31.8) | 21.6 (16.7–26.2) | 0.30 |
| IP LOS: median (Q1-Q3) in days | 2.9 (2.2–4.2) | 2.9 (2.2–4.2) | N/A | – |
| Meets Version 1 Criteria | 71 (59%) | 15 (36%) | 56 (72%) | <0.01 |
| Meets Version 2 Criteria | 77 (64%) | 19 (45%) | 58 (74%) | <0.01 |
| 28 Day Mortality | 1 (1%) | 1 (2%) | 0 (0%) | – |
| 14 Day ED Return | 22 (18%) | 5 (12%) | 17 (22%) | – |
| Admitted after repeat ED visit | 17 (14%) | 4 (10%) | 13 (17%) | – |
Admitted patients were slightly older (Table 1, 65 years vs. 59 years, p = 0.05) and had a lower median resting oxygen saturation on room air (Table 1, 94% vs. 96%, p < 0.01). Discharged patients were significantly more likely to have met criteria for version 1 (Table 2, 72% vs. 36%, p < 0.01) and version 2 (Table 2, 74% vs. 45%, p < 0.01) of the protocol. Using a multivariate logistic regression with disposition as the outcome while controlling for age and sex, meeting criteria for either version 1 (OR = 3.17, 95% CI 1.34–7.53, p < 0.01) or version 2 (OR = 3.18, 95% CI 1.39–7.30, p < 0.01) of the protocol resulted in a higher likelihood of discharge.
Of the 22 patients who returned to our emergency department within 14 days of initial visit, 17 were admitted directly from the ED on their second visit. There was one death within 28-days of initial ED visit and that patient did not meet version 1 or version 2 criteria.
Our median EDOU LOS was 22.5 h for the full cohort with no statistically significant difference between those patients ultimately admitted (23.8 h) or discharged (21.6 h). Similarly, the median ED LOS was 3.8 h for the full cohort with no statistically significant difference between those patients ultimately admitted from the EDOU (3.7 h) or discharged (3.8 h).
4. Discussion
Our ED successfully created and implemented a COVID-19 ED Observation Protocol for our EDOU. While there are patients with COVID-19 for whom appropriate disposition is clear at the time of initial ED evaluation, there is a proportion of patients for whom disposition is not immediately apparent. A brief observation period allows the emergency physician to gather more data for or against admission.
While ED-based observation units have been well studied for many chief complaints, this is the first example we are aware of where a COVID-19 protocol was developed for ED-based observation. Moreover, this is the first ED-based observation protocol we are aware of that has been created and implemented in real time for a novel disease with rapidly changing treatment guidelines. This protocol was developed and implemented nine months after the initial cases of COVID-19 were seen in our ED, and in time to capture much of the second surge seen during the winter of 2020–2021.
Our overall adherence to the observation protocols was 62% (version 1) and 60% (version 2). For the purpose of our analysis, we assessed compliance with the protocol using the lowest documented room air saturation at rest prior to the decision being made to admit the patient to the EDOU. It is likely that some of the deviation from the protocols can be explained by clinicians using clinical judgement when pulse oximeter readings were borderline. It is also possible that during the implementation of version 2 clinicians did not account for common high-risk comorbidies.
Our overall admission rate from the EDOU was 35%, slightly exceeding our goal of 30%. On subgroup analysis of patients who strictly met criteria for either version of the protocol, the admission rate drops to 21% (version 1) and 25% (version 2). Although version 2 of the protocol liberalized EDOU placement criteria, the admission rate did not significantly change. While goal admission rates from EDOU should be less than 20% according to expert consensus, [13] we anticipated a higher admission rate in our first iteration of designing a protocol for COVID-19, which was a novel disease for which no prior observation protocols existed. The median EDOU LOS was 22.5 h, with no statistically significant difference between admitted (23.5 h) and discharged (21.6 h) patients. Our standard goal for ED observation is to observe the patient for up to 48 h to determine a disposition and intervene as necessary. Nearly all patients met this target.
While our sample size was modest at 120, our protocol successfully demonstrated that ED observation can be safely used to care for patients with COVID-19 who do not clearly have an appropriate disposition at the time of their initial evaluation. Rather than having high-risk and potentially unsafe discharges or using scarce hospital resources for unnecessary admissions in an already strained environment, our protocol allowed the emergency physician to gather more clinical data for determining an appropriately disposition. COVID-19 is an illness known to progress over a multi-week course, sometimes with acute deteriorations that can prompt re-presentation [33]. Our study found that 18% of patients returned to the ED within 14 days of their original hospital visit. Of those 22 patients, 17 (77%) were admitted during their second hospital visit.
The primary limitation of our study is a small sample size of 120 patients at a single center. This particularly limited any subgroup analysis on the impact of high-risk comorbidities on final disposition. Additionally, as this was a retrospective study, our analysis was limited to available data within the electronic medical record, which may have obscured clinical judgement regarding individual cases. Additional limitations include a change in protocol partway through the study period, heterogenous methods for calculation of exertional oxygen saturation, and the addition of new alternative pathways to admission implemented during version 2 of the protocol. The addition of new potential disposition pathways during version 2, including a virtual observation unit, likely drew a small fraction of the patients who would have otherwise been placed in the EDOU for COVID-19.
This study serves as an initial proof of concept that an ED-based observation protocol can be successfully created and implemented for COVID-19. Furthermore, our study serves as an initial proof of concept that it is possible to rapidly create, implement, and improve an ED-based observation protocol for a novel disease with satisfactory operational outcomes. Meeting criteria for the protocol resulted in an acceptable admission rate and a higher likelihood of discharge. Further studies with larger sample sizes are needed to refine and validate the protocol. Future research might also examine operational outcomes such as cost savings and reduction in admissions achieved through a COVID-19 observation protocol, whether such an approach can reduce strain on hospital capacity, and how to optimally utilize the EDOU given the recent creation of multiple innovative alternative care pathways available for patients with COVID-19.
Sources of support/funding
Brian Yun received support by the Massachusetts General Hospital Department of Emergency Medicine Fellowship Eleanor and Miles Shore Fellowship Program for Scholars in Medicine.
Summary conflict of interest statement
None.
Prior abstract publication/presentation
None.
CRediT authorship contribution statement
Yosef Berlyand: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis. Joshua J. Baugh: Data curation, Investigation, Writing – original draft, Writing – review & editing, Conceptualization. Andy Hung-Yi Lee: Writing – review & editing, Methodology, Data curation. Stephen Dorner: Data curation, Writing – review & editing. Susan R. Wilcox: Writing – review & editing, Data curation, Conceptualization. Ali S. Raja: Data curation, Writing – review & editing. Brian J. Yun: Writing – review & editing, Writing – original draft, Supervision, Methodology, Investigation, Data curation, Conceptualization.
Declaration of Competing Interest
All authors report no conflict of interest.
References
- 1.COVID-19 Impact on Nurse Staffing and ICU Beds. 2021. https://ehrn.org/articles/covid-19-impact-on-nurse-staffing-and-icu-beds (accessed 15 Apr 2021)
- 2.Weissman G.E., Crane-Droesch A., Chivers C., et al. Locally informed simulation to predict hospital capacity needs during the COVID-19 pandemic. Ann Intern Med. 2020;173:21–28. doi: 10.7326/M20-1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bravata D.M., Perkins A.J., Myers L.J., et al. Association of Intensive Care Unit Patient Load and Demand with Mortality Rates in US Department of veterans affairs hospitals during the COVID-19 pandemic. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2020.34266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.‘There's No Place for Them to Go’: I.C.U. Beds Near Capacity Across U.S. - The New York Times. 2020. https://www.nytimes.com/interactive/2020/12/09/us/covid-hospitals-icu-capacity.html
- 5.Drumheller Byron C., Mareiniss Darren P., Overberger Ryan C., Sabolick Erin E. 2020. Design and implementation of a temporary emergency department-intensive care unit patient care model during the COVID-19 pandemic surge. Published Online First. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernstein S.L., Aronsky D., Duseja R., et al. The effect of emergency department crowding on clinically oriented outcomes. Acad Emerg Med. 2009;16:1–10. doi: 10.1111/j.1553-2712.2008.00295.x. [DOI] [PubMed] [Google Scholar]
- 7.Miro O., Antonio M., Jimenez S., et al. Decreased health care quality associated with emergency department overcrowding. europepmc.org. 1999;6(2):105–107. doi: 10.1097/00063110-199906000-00003. https://europepmc.org/abstract/med/10461551 (accessed 4 Dec 2019) [DOI] [PubMed] [Google Scholar]
- 8.Medicine I of. Hospital-Based Emergency Care. National Academies Press; 2007. [DOI] [Google Scholar]
- 9.Sikka R., Mehta S., Kaucky C., et al. ED crowding is associated with an increased time to pneumonia treatment. Am J Emerg Med. 2010;28:809–812. doi: 10.1016/j.ajem.2009.06.023. [DOI] [PubMed] [Google Scholar]
- 10.Chatterjee P., Cucchiara B.L., Lazarciuc N., et al. Emergency department crowding and time to care in patients with acute stroke. Stroke. 2011;42:1074–1080. doi: 10.1161/STROKEAHA.110.586610. [DOI] [PubMed] [Google Scholar]
- 11.McCarthy M.L., Zeger S.L., Ding R., et al. Crowding delays treatment and lengthens emergency department length of stay, even among high-acuity patients. Ann Emerg Med. 2009;54 doi: 10.1016/j.annemergmed.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 12.Fee C., Weber E., Maak C., et al. Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Elsevier. 2006 doi: 10.1016/j.annemergmed.2007.08.003. https://www.sciencedirect.com/science/article/pii/S0196064407013820 (accessed 4 Dec 2019) [DOI] [PubMed] [Google Scholar]
- 13.Conley J., Bohan J.S., Baugh C.W. The establishment and Management of an Observation Unit. Emerg Med Clin N Am. 2017;35:519–533. doi: 10.1016/j.emc.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 14.Ross M.A., Hockenberry J.M., Mutter R., et al. Protocol-driven emergency department observation units offer savings, shorter stays, and reduced admissions. Health Aff. 2013;32:2149–2156. doi: 10.1377/hlthaff.2013.0662. [DOI] [PubMed] [Google Scholar]
- 15.Medicare Program: Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs; Short Inpatient Hospital Stays; Transition for Certain Medicare-Dependent, Small Rural Hospitals Under the Hospital Inpatient Prospective Payment System; Provider Administrative Appeals and Judicial Review. http://www.cms.gov/ [PubMed]
- 16.Reviewing short stay hospital claims for patient status: admissions on or after medical review of inpatient hospital claims. 2016. http://qioprogram.org/announcementscms.govhttps://www.cms.gov/research-statistics-data-and-systems/monitoring-programs/medicare-ffs-compliance-programs/medical-review/inpatienthospitalreviews.html [accessed 15 Apr 2021] [Google Scholar]
- 17.Goodacre S.W. Should we establish chest pain observation units in the UK? A systemic review and critical appraisal of the literature. J Accid Emerg Med. 2000;17:1–6. doi: 10.1136/emj.17.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Farkouh M.E., Smars P.A., Reeder G.S., et al. A clinical trial of a chest-pain observation unit for patients with unstable angina. N Engl J Med. 1998;339:1882–1888. doi: 10.1056/nejm199812243392603. [DOI] [PubMed] [Google Scholar]
- 19.Gomez M.A., Anderson J.L., Karagounis L.A., et al. An emergency department-based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO) J Am Coll Cardiol. 1996;28:25–33. doi: 10.1016/0735-1097(96)00093-9. [DOI] [PubMed] [Google Scholar]
- 20.Roberts R.R. Costs of an emergency department—based accelerated diagnostic protocol vs hospitalization in patients with chest pain. JAMA. 1997;278:1670. doi: 10.1001/jama.1997.03550200046030. [DOI] [PubMed] [Google Scholar]
- 21.Volz K.A., Canham L., Kaplan E., et al. Identifying patients with cellulitis who are likely to require inpatient admission after a stay in an ED observation unit. Am J Emerg Med. 2013;31:360–364. doi: 10.1016/j.ajem.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 22.Ross M.A., Compton S., Medado P., et al. An emergency department diagnostic protocol for patients with transient ischemic attack: a randomized controlled trial. Ann Emerg Med. 2007;50:109–119. doi: 10.1016/j.annemergmed.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 23.McDermott M.F. A comparison between emergency diagnostic and treatment unit and inpatient Care in the Management of acute asthma. Arch Intern Med. 1997;157:2055. doi: 10.1001/archinte.1997.00440390041006. [DOI] [PubMed] [Google Scholar]
- 24.Zwicke D.L., Donohue J.F., Wagner E.H. Use of the emergency department observation unit in the treatment of acute asthma. Ann Emerg Med. 1982;11:77–83. doi: 10.1016/S0196-0644(82)80301-6. [DOI] [PubMed] [Google Scholar]
- 25.O’Brien S.R., Hein E.W., Sly R.M. Treatment of acute asthmatic attacks in a holding unit of a pediatric emergency room. Ann Allergy. 1980;45:159–162. https://europepmc.org/article/med/7416560 [PubMed] [Google Scholar]
- 26.Shen W.K., Decker W.W., Smars P.A., et al. Syncope evaluation in the emergency department study (seeds): a multidistiplinary approach to syncope management. Circulation. 2004;110:3636–3645. doi: 10.1161/01.CIR.0000149236.92822.07. [DOI] [PubMed] [Google Scholar]
- 27.Stewart M., Bledsoe J., Madsen T., et al. Utilization and safety of a pulmonary embolism treatment protocol in an emergency department observation unit. Crit Pathways Cardiol A J Evidence-Based Med. 2015;14:87–89. doi: 10.1097/HPC.0000000000000046. [DOI] [PubMed] [Google Scholar]
- 28.Ward G., Jorden R.C., Severance H.W. Treatment of pyelonephritis in an observation unit. Ann Emerg Med. 1991;20:258–261. doi: 10.1016/S0196-0644(05)80935-7. [DOI] [PubMed] [Google Scholar]
- 29.Scott Israel M.R., Lowenstein S.R., Marx J.A., et al. Management of acute pyelonephritis in an emergency department observation unit. Ann Emerg Med. 1991;20:253–257. doi: 10.1016/S0196-0644(05)80934-5. [DOI] [PubMed] [Google Scholar]
- 30.Kilaru A.S., Lee K., Snider C.K., et al. Return hospital admissions among 1419 COVID-19 patients discharged from five U.S. emergency departments. Acad Emerg Med. 2020;27:1039–1042. doi: 10.1111/acem.14117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Older Adults and COVID-19 | CDCCenters Dis. Control Prev. 2021 https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html (accessed 15 Apr 2021) [Google Scholar]
- 32.Science Brief: Evidence used to update the list of underlying medical conditions that increase a person's risk of severe illness from COVID-19. Centers Dis Control Prev. 2021 https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlying-evidence-table.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fneed-extra-precautions%2Fevidence-table.html [PubMed] [Google Scholar]
- 33.Cohen P.A., Hall L.E., John J.N., et al. The early natural history of SARS-CoV-2 infection: clinical observations from an urban, ambulatory COVID-19 clinic. Mayo Clin Proc. 2020;95:1124–1126. doi: 10.1016/j.mayocp.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]