Abstract
SARS-CoV-2 by the direct cytopathic effect or indirectly through the propagation of pro-inflammatory cytokines could cause endothelial dysfunction (ED) and oxidative stress (OS). It has been reported that OS is triggered by various types of viral infections, including SARS-CoV-2. Into the bargain, allopurinol is regarded as a potent antioxidant that acts through inhibition of xanthine oxidase (XO), which is an essential enzyme of purine metabolism. Herein, the present study aimed to find the potential protective effects of allopurinol on the biomarkers of OS and ED in patients with severe Covid-19. This single-center cohort study recruited 39 patients with mild-moderate Covid-19 compared with 41 patients with severe Covid-19. Nineteen patients with severe Covid-19 were on the allopurinol treatment because of underlying chronic gout 3 years ago compared with 22 Covid-19 patients not on this treatment. The recruited patients were allocated into three groups: group I, mild-moderate Covid-19 on the standard therapy (n = 39); group II, severe Covid-19 patients on the standard therapy only (n = 22); and group III, severe Covid-19 patients on the standard therapy plus allopurinol (n = 19). The duration of the study was 3 weeks from the time of hospitalization till the time of recovery. In addition, inflammatory biomarkers (D-dimer, LDH, ferritin, CRP, procalcitonin), neutrophil–lymphocyte ratio (NLR), endothelin-1 (ET-1), uric acid and oxidative stress index (OSI), CT scan score, and clinical score were evaluated at the time of admission and discharge regarding the effect of allopurinol treatment adds to the standard treatment of Covid-19. Allopurinol plus standard treatment reduced LDH, ferritin, CRP, procalcitonin, and ET-1 serum level significantly (P < 0.05) compared with Covid-19 patients on standard treatment. Besides, neutrophil (%), lymphocyte (%), and neutrophil–lymphocyte ratio (NLR) were reduced in patients with severe Covid-19 on standard treatment plus allopurinol compared with Covid-19 patients on standard treatment alone (P < 0.01). OSI was higher in patients with severe Covid-19 than mild-moderate Covid-19 patients (P = 0.00001) at admission. At the time of discharge, the oxidative status of Covid-19 patients was significantly improved compared with that at admission (P = 0.01). In conclusion, Covid-19 severity is linked with high OS and inflammatory reaction with ED development. High uric acid in patients with severe Covid-19 is correlated with high OS and inflammatory biomarkers. Allopurinol with standard treatment in patients with severe Covid-19 reduced oxidative and inflammatory disorders with significant amelioration of ED and clinical outcomes.
KEY WORDS: SARS-CoV-2, oxidative stress, endothelial dysfunction, allopurinol, inflammatory disorders.
INTRODUCTION
The existence of coronavirus disease 2019 (Covid-19) is caused by a novel coronavirus known as a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and leads to worldwide diastrophic effects [1]. In this prudence, direct SARS-CoV-2 cytopathic damage and pro-inflammatory cytokines release could cause acute respiratory distress syndrome (ARDS) [2]. In Covid-19, SARS-CoV-2 mainly invades lung alveolar type II pneumocyte cells due to advanced expression of angiotensin-converting enzyme 2 (ACE2), a receptor involved for entry SARS-CoV-2 [3]. The majority of affected Covid-19 patients are asymptomatic and presented with mild respiratory symptoms, though a small proportion of Covid-19 patients may develop severe forms of respiratory symptoms due to the development of acute lung injury (ALI), which may progress to ARDS [4].
SARS-CoV-2 by the direct cytopathic effect or indirectly through the propagation of pro-inflammatory cytokines could cause endothelial dysfunction (ED) and various forms of vasculopathies [5]. Likewise, oxidative stress (OS) is induced during SARS-CoV-2 infection with ED development [6]. It has been reported that OS is triggered by various types of viral infections, including hepatitis viruses, human immune deficiency virus-1 (HIV-1), and most RNA viruses like coronavirus [7].
In general, viral infections increase the production of free radicals and reduction of endogenous antioxidant capacity through induction of mitochondrial dysfunction. Besides, Covid-19-induced cytokine storm and high pro-inflammatory cytokines with ferritin levels could induce the generation of reactive oxygen species via Fenton reaction [8]. In addition, pro-inflammatory cytokines activate inducible nitric oxide synthase (iNOS), which react with ROS and superoxide ions to form oxidizing peroxynitrite [9]. Hypoxia, tissue ischemia, hypertension, and diabetes mellitus commonly associated with Covid-19 reduce cellular antioxidant capacity [10, 11]. Reduction of antioxidant capacity in Covid-19 patients with underlying comorbidities predisposes to OS development [12].
On the other hand, ED is developed during the progression of OS through impairment synthesis and release of NO [13]. Moreover, deficiency of endothelial NO predisposes for activation of prothrombotic and pro-inflammatory cascades with noteworthy abnormal alterations of the endothelial lining, abnormal vascular tone, and development of ED [14]. Thus, mitigation of OS by antioxidants may attenuate the development of ED and associated vasculopathy in Covid-19 patients [15].
Into the bargain, allopurinol is regarded as a potent antioxidant that acts through inhibition of xanthine oxidase (XO), which is an essential enzyme of purine metabolism [16]. It is involved in the oxidation of xanthine and hypoxanthine for the generation of uric acid. In addition, XO induces ROS generation through calcium signaling and NO pathways [17]. Therefore, inhibition of XO by allopurinol and other XO inhibitors may reduce the risk of the development of ED [18]. In fact, allopurinol is metabolized by aldehyde oxidase and gives an active metabolite, oxipurinol, which has a long half-life and is regarded as a potent inhibitor of XO [19]. High xanthine and hypoxanthine concentration due to inhibition of XO by allopurinol may cause feedback inhibition of purine biosynthesis. Thus, allopurinol may inhibit both uric acid production and de novo purine synthesis [20].
It has been shown that expression of XO is induced by different respiratory RNA viral infections, including SARS-CoV-2 leading to the building of OS and production of uric acid [21]. Therefore, the rationale of the present study was that allopurinol might attenuate the induced XO by SARS-CoV-2 in patients with severe Covid-19 and associated inflammatory and oxidative changes.
Herein, the present study aimed to find the potential protective effects of allopurinol on the biomarkers of OS and ED in patients with severe Covid-19.
METHODS
In this single-center cohort prospective study, 39 non-hospitalized patients with mild-moderate Covid-19 compared with 41 hospitalized patients with severe Covid-19 were recruited according to the international diagnostic criteria from the Al-Atah Specialized Medical Center for Covid-19 Baghdad, Iraq, during a period from Feb 1 till March 2021. Nineteen patients with severe Covid-19 were on the allopurinol treatment 300 mg/day because of underlying chronic gout 3 years ago compared with 22 Covid-19 patients not on this treatment. Following the meticulous medical history, physical examination, and biochemical and serological investigations, the recruited patients were allocated into three groups:
Group I: Mild-moderate Covid-19 on the standard therapy (n = 39)
Group II: Severe Covid-19 patients on the standard therapy only (n = 22)
Group III: Severe Covid-19 patients on the standard therapy plus allopurinol (n = 19)
The duration of the study was 3 weeks from the time of hospitalization till the complete patient’s recovery. This study was approved by the Scientific Jury and Ethical Committee in College of Medicine, Al-Mustansiriyah University, in collaboration with the Al-Atah Specialized Medical Center for Covid-19 management, on Apr 10, 2021 (TRW34 in 2021).
The standard treatment of Covid-19 was acetaminophen tablet 2 g/day, famotidine tablet 40 mg/day, ivermectin tablet, subcutaneous enoxaparin 4000 iu/day, azithromycin 500 mg/day, and favipiravir 1800 mg/day. In addition, though, intravenous remdesivir 100 mg/day was used for severe cases.
Inclusion Criteria
Any Covid-19 patients of either gender with mild to severe presentation with/without concomitant use of allopurinol were included in this study.
Exclusion Criteria
The patients with chronic kidney diseases, hepatic disorders, endocrinopathy, lactation, pregnancy, autoimmune disorders, and mental and psychiatric disorders were excluded.
The primary outcomes of the present study were to evaluate the efficacy of allopurinol plus standard therapy on the discharging time and mortality. However, the secondary outcomes were to appraise the effectiveness of allopurinol plus standard therapy on the biomarkers of OS, inflammatory, and pro-inflammatory profiles, as well as radiological and clinical recoveries.
Biochemical and Serological Investigations
Real-time polymerase chain reaction (RT-PCR) was performed to confirm the recent SARS-CoV-2 infection for all recruited patients. Besides, anti-SARS-CoV-2 antibodies (Covid-19 test, NovaLisa, VROTECH, Germany), including IgM and IgG, were used to detect the recent SARS-CoV-2 infection. Complete blood count (CBC) was done by an auto-analyzer (Zhejiang Xinke Medical Technology Co., Ltd, China). Serum uric acid was measured by a colorimetric assay kit (E-BC-K016-M Abcam).
Furthermore, biomarkers of inflammations in Covid-19 were assessed by ELISA kit methods, including D-dimer, C-reactive protein (CRP), serum ferritin, lactate dehydrogenase (LDH), and procalcitonin. Assessment of endothelial function was done by measuring endothelin-1 (ET-1) by ELISA kit method (ET-1, ELISA ab133030, Abcam). In addition, total antioxidant status (TAS) and total oxidant status (TOS) were estimated by ELISA kit methods (human antioxidant MBS162650, MyBioSource, human total oxidant MBS 162650) that are expressed as mol/L). Then, oxidative stress index (OSI) can be calculated by a specific equation (OSI) = [22].
Measurement of Anthropometric Parameters
The patient’s body mass index (BMI) was measured depending on body weight (kg) and height (m2) as follows, [23]. In addition, the pressure profile of the recruited patients was measured at the supine position from the left arm by an automated sphygmomanometer. Diastolic blood pressure (DBP) and systolic blood pressure (SBP) were measured. From SBP and DBP, both pulse pressure (PP) and mean arterial pressure (MAP) were calculated by explicit equations. PP = SBP-DBP or (MAP-DBP)/0.33, while MAP = (SBP + 2 DBP)/3 [24].
Estimation of Lung Radiological Measures
Lung computed tomography (CT) scan and posterior-anterior chest X-ray were performed to detect lung involvement by Covid-19 pneumonia, which might be bilateral ground-glass opacity (GGO) in most cases (75%). However, unilateral lung GGO might be illustrated in 25% of patients with Covid-19 pneumonia [25]. The scoring of lung CT scan was also done according to Francone et al. method [26]: score 1, lung injury < 5%; score 2, lung injury 5–25%; score 3, lung injury 26–50%; score 4, lung injury 51–75%; and score 5, lung injury > 75%.
Estimation of Clinical Outcomes
The clinical scores were evaluated at the time of hospitalization and discharge for patients with severe Covid-19 in response to Gude et al. scoring system from 1–7 score [27].
Score 1: The patient does not need hospitalization with normal activity.
Score 2: The patient does not need hospitalization but not resumed usual activity.
Score 3: The patient needs hospitalization without need for oxygen supplementation.
Score 4: The patient needs hospitalization and oxygen supplementation.
Score 5: The patient needs hospitalization and oxygen supplementation by non-invasive method.
Score 6: The patient needs hospitalization and mechanical ventilation.
Score 7: Death.
Statistical Analysis
Data were analyzed using SPSS (IBM, Version 24.00, Armonk, IBM, NY, Corp, USA). Results are expressed and presented as number (n), percentages, and mean ± standard deviation (SD). An unpaired t-test was applied to find the statistical differences between two independent groups. In addition, Pearson correlation was done to discover the significance of correlations. P-value < 0.05 was regarded significant.
RESULTS
Characteristics of the Present Study
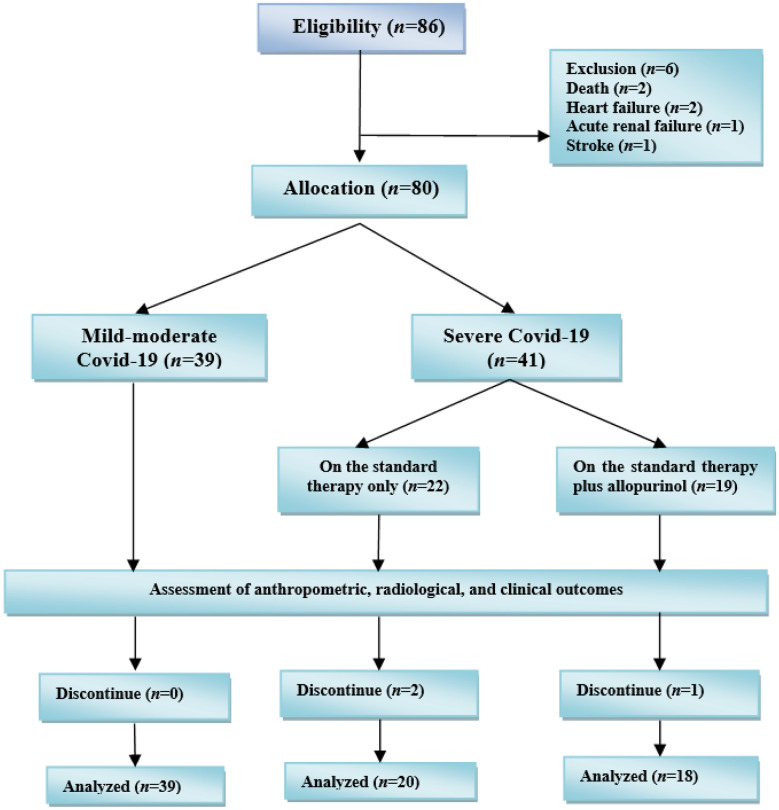
At the beginning of the present study, 86 Covid-19 were recruited, two patients died, and four patients were excluded because of heart failure (n = 2), acute renal failure (n = 1), and stroke (n = 1). Thus, only 80 patients continued the study and were subjected for investigations as 39 Covid-19 patients with mild-moderate and 41 patients with severe Covid-19. During the study, 3 patients died, and the rest continued the study (Fig. 1).
Fig. 1.
Consort flow-chart of the present study.
The characteristics of the present study revealed a total number of 80 Covid-19 patients with a mean age of 44.84 ± 8.12 years and a high male to female (M:F) ratio 57:23. Likewise, the race of recruited patients was predominantly white compared to the black race (73:7). The recruited patients were 39 (48.75%) of mild-moderate Covid-19, and 41 (51.25%) of them were severe Covid-19. The severe Covid-19 patients on the standard treatment only were 22 (27.50%), while 19 (23.75%) were on the standard treatment plus allopurinol. Some of the recruited Covid-19 patients had concomitant illnesses, including gout 19 (23.75%), hypertension 23 (28.75%), asthma 6 (7.50%), and ischemic heart disease 13 (16.25%). Besides, some of Covid-19 patients were on different treatments including allopurinol 19 (23.75%), indomethacin 3 (3.75%), clopidogrel 12 (15.00%), statins 3 (3.75%), montelukast 6 (7.50%), amlodipine 7 (8.75%), atenolol 9 (11.25%), metoprolol 5 (6.25%), and valsartan 2 (2.50%) (Table 1).
Table 1.
Characteristic of the Present Study
| The characteristics | Mean ± SD, n, % |
|---|---|
| n | 80 |
| Age (years) | 44.84 ± 8.12 |
| Gender (M:F) ratio | 57:23 |
| Race (white: black) ratio | 73:7 |
| Mild-moderate Covid-19 | 39 (48.75) |
| Severe Covid-19 | 41 (51.25) |
| On the standard treatment only | 22 (27.50) |
| On the standard treatment plus allopurinol | 19 (23.75) |
| Concomitant diseases | |
| Gout | 19 (23.75) |
| Hypertension | 23 (28.75) |
| Asthma | 6 (7.50) |
| Ischemic heart disease (IHD) | 13 (16.25) |
| Concomitant treatments | |
| Allopurinol | 19 (23.75) |
| Indomethacin | 3 (3.75) |
| Clopidogrel | 12 (15.00) |
| Statins | 3 (3.75) |
| Montelukast | 6 (7.50) |
| Amlodipine | 7 (8.75) |
| Atenolol | 9 (11.25) |
| Metoprolol | 5 (6.25) |
| Valsartan | 2 (2.50) |
Data expressed as mean ± SD, number (n), and percentages (%), M: F, male: female ratio
Evaluation of Covid-19 Patients at the Time of Admission
We analyzed the effects of allopurinol on the standard treatment of severe Covid-19 patients on the anthropometric and inflammatory variables, compared with the standard treatment alone in severe and mild to moderate Covid-19 patients. Both age and body mass index (BMI) were not significant (P = 0.95 and P = 0.68, respectively). Regarding pressure profile of patients, systolic blood pressure (SBP), diastolic blood pressure (DBP), and mean arterial pressure (MAP) were low in mild-moderate Covid-19 patients compared to patients with severe Covid-19 on standard treatment only (P = 0.006, P = 0.003, and P = 0.0001, respectively). However, MAP was lower in severe Covid-19 patients on standard treatment plus allopurinol compared with Covid-19 patients on standard treatment alone (P = 0.02). Oxygen saturation was reduced in Covid-19 patients on standard treatment alone compared with Covid-19 patients on standard treatment plus allopurinol (P = 0.002). In addition, MAP was lower in Covid-19 patients on standard treatment plus allopurinol than Covid-19 patients on standard treatment (P = 0.02). LDH and ferritin serum levels were higher in patients with severe Covid-19 than mild-moderate Covid-19 patients (P = 0.002 and P = 0.0001, respectively). So, allopurinol in patients with severe Covid-19 did not significantly affect LDH and ferritin serum levels compared to Covid-19 patients on standard treatment (P > 0.05). However, CRP and procalcitonin serum levels were lower in Covid-19 patients on standard treatment plus allopurinol than Covid-19 patients on standard treatment (P = 0.0001 and P = 0.002, respectively). Serum uric acid was low in patients with mild-moderate Covid-19 and patients with severe Covid-19 on allopurinol compared with severe Covid-19 on standard treatment alone (P = 0.002). Furthermore, endothelin-1 (ET-1) serum level was higher in patients with severe Covid-19 than mild-moderate Covid-19 patients (P = 0.00001) regardless of allopurinol treatment. Moreover, CT scores were higher in patients with severe Covid-19 compared with mild-moderate Covid-19 patients (P = 0.00001) without significant effect of allopurinol treatment. Concerning complete blood count (CBC), WBCs were higher in patients with severe Covid-19 than mild-moderate Covid-19 patients (P = 0.00001). Besides, neutrophil (%), lymphocyte (%), and neutrophil–lymphocyte ratio (NLR) were reduced in patients with severe Covid-19 on standard treatment plus allopurinol compared with Covid-19 patients on standard treatment alone (P < 0.01) (Table 2).
Table 2.
Effects of Allopurinol add on the Standard Treatment of Severe Covid-19 Patients on the Anthropometric and Inflammatory Variable Compared with Severe Covid-19 Patients on the Standard Treatment Alone and Mild to Moderate Covid-19 Patients at the Time of Admission
| The parameters | A (n = 39) | B (n = 22) | C (n = 19) | I | II | III | ANOVA |
|---|---|---|---|---|---|---|---|
| Age (years) | 44.53 ± 8.73 | 44.23 ± 8.93 | 43.81 ± 8.49 | Ns | Ns | Ns | 0.95 |
| BMI (kg/m2) | 35.61 ± 3.91 | 34.82 ± 3.77 | 34.91 ± 3.91 | Ns | Ns | Ns | 0.68 |
| SBP (mmHg) | 132.80 ± 7.05 | 139.63 ± 8.91 | 135.05 ± 9.31 | 0.006 | Ns | Ns | 0.009 |
| DBP(mmHg) | 83.95 ± 8.31 | 90.53 ± 6.47 | 86.29 ± 5.99 | 0.003 | Ns | Ns | 0.005 |
| PP(mmHg) | 48.85 ± 6.93 | 49.10 ± 6.88 | 48.76 ± 7.31 | Ns | Ns | Ns | 0.98 |
| MAP(mmHg) | 100.23 ± 4.31 | 106.90 ± 6.29 | 102.54 ± 4.91 | 0.00001 | Ns | 0.02 | 0.00001 |
| SaO2 (%) | 96.83 ± 2.41 | 87.09 ± 3.71 | 90.56 ± 3.85 | 0.00001 | 0.00001 | 0.002 | 0.00001 |
| D-dimer (ng/mL) | 238.93 ± 11.78 | 643.94 ± 23.95 | 521.73 ± 12.72 | Ns | Ns | 0.02 | 0.00001 |
| LDH (U/L) | 296.81 ± 9.21 | 495.72 ± 29.53 | 275.12 ± 15.49 | Ns | 0.002 | Ns | 0.00001 |
| Ferritin(ng/mL) | 276.80 ± 11.03 | 503.61 ± 26.41 | 312.67 ± 12.92 | Ns | 0.0001 | Ns | 0.00001 |
| CRP (mg/L) | 11.79 ± 2.91 | 25.73 ± 4.81 | 12.30 ± 3.95 | 0.0001 | Ns | 0.0001 | 0.00001 |
| Procalcitonin (ng/mL) | 0.19 ± 0.03 | 0.24 ± 0.04 | 0.20 ± 0.01 | 0.0001 | Ns | 0.002 | 0.00001 |
| Uric acid (mg/dL) | 7.52 ± 1.95 | 9.56 ± 2.07 | 7.59 ± 2.83 | 0.002 | Ns | 0.01 | 0.002 |
| ET-1(pg/mL) | 25.07 ± 8.05 | 43.86 ± 9.12 | 34.63 ± 7.22 | 0.00001 | 0.00001 | 0.001 | 0.00001 |
| CT scan score (%) | 2.12 ± 1.33 | 4.68 ± 1.04 | 4.11 ± 1.09 | 0.00001 | 0.00001 | Ns | 0.00001 |
| WBC (103/µL) | 11.59 ± 2.84 | 14.37 ± 2.99 | 13.63 ± 3.61 | 0.003 | Ns | Ns | 0.002 |
| Neutrophil (%) | 66.73 ± 4.01 | 87.94 ± 8.45 | 81.91 ± 5.04 | 0.00001 | 0.00001 | 0.003 | 0.00001 |
| Lymphocytes (%) | 21.71 ± 2.75 | 12.23 ± 6.95 | 17.53 ± 5.04 | 0.00001 | 0.007 | 0.001 | 0.00001 |
| NLR | 3.07 ± 1.71 | 7.19 ± 2.97 | 4.67 ± 2.30 | 0.00001 | 0.03 | 0.001 | 0.00001 |
Data presented as mean ± SD. A: Patients with mild-moderate Covid-19. B: Patients with severe Covid-19 on the standard treatment only. C: Patients with severe Covid-19 on the standard treatment plus allopurinol. I: A vs. B, II: A vs. C, III: B vs. C. Ns not significant, BMI body mass index, SBP systolic blood pressure, DBP diastolic blood pressure, PP pulse pressure, MAP mean arterial pressure, SaO2 oxygen saturation, LDH lactate dehydrogenase, CRP C-reactive protein, ET-1 endothelin-1, NLR neutrophil–lymphocyte ratio
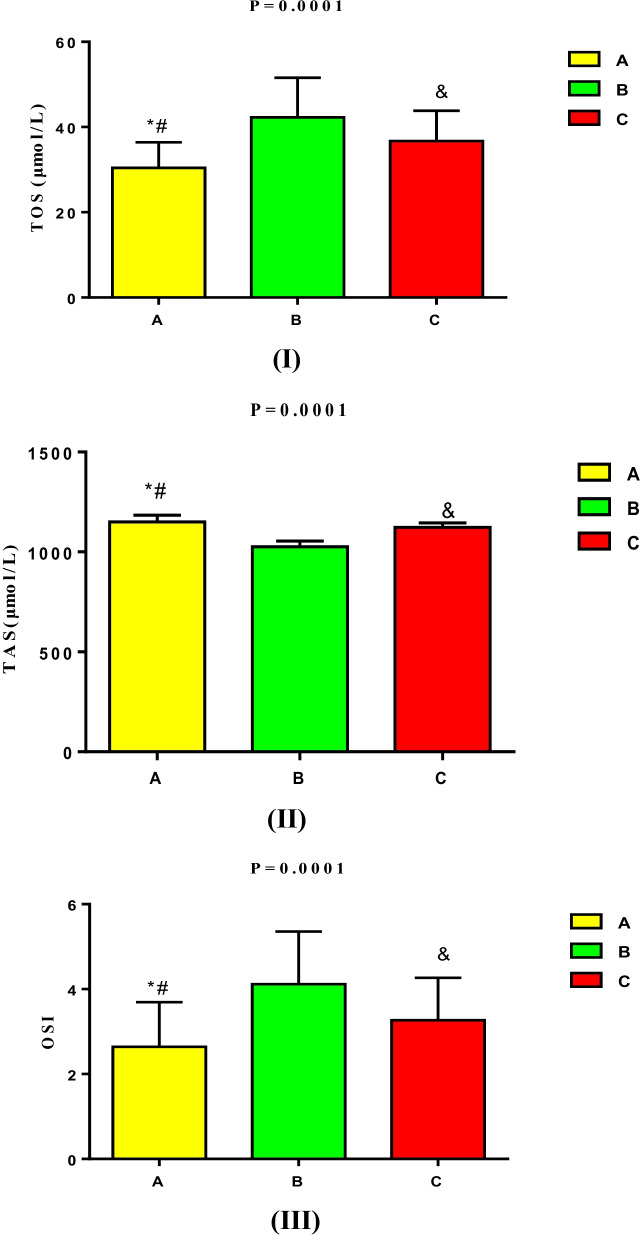
Regarding oxidative status, TOS and OSI were higher in patients with severe Covid-19 than mild-moderate Covid-19 patients (P = 0.00001). TOS was low in mild-moderate Covid-19 patients (30.42 ± 6.01 µmol/L) compared with patients with severe Covid-19 on standard treatment only (42.29 ± 9.2901 µmol/L) (P = 0.0001). However, TOS was lower in patients with severe Covid-19 treated by standard treatment plus allopurinol (36.73 ± 7.08 µmol/L) as compared with severe Covid-19 treated by standard alone (P = 0.04) (Fig. 2).
Fig. 2.
Oxidative statue in Covid-19 regarding effect of allopurinol treatment: (I): total oxidant status (TOS) was lower in mild-moderate Covid-19 patients as compared with severely Covid-19 patients on standard treatment alone (*P = 0.0001 and #P = 0.007) as compared with severely affected Covid-19 patients on standard treatment plus allopurinol. TOS was lower in severely affected Covid-19 patients on standard treatment plus allopurinol than severely affected Covid-19 patients on standard treatment alone (&P = 0.04). (II): Total antioxidant status (TAS) was higher in mild-moderate Covid-19 patients as compared with severely Covid-19 patients on standard treatment alone (*P = 0.0001 and #P = 0.007) as compared with severely affected Covid-19 patients on standard treatment plus allopurinol. TAS was higher in severely affected Covid-19 patients on standard treatment plus allopurinol than severely affected Covid-19 patients on standard treatment alone (&P = 0.005). (III): Oxidative stress index (OSI) was lower in mild-moderate Covid-19 patients as compared with severely Covid-19 patients on standard treatment alone (*P = 0.0001), but not significant as compared with severely affected Covid-19 patients on standard treatment plus allopurinol (#P = 0.08). OSI was lower in severely affected Covid-19 patients on standard treatment plus allopurinol than severely affected Covid-19 patients on standard treatment alone (&P = 0.04).
Evaluation of Covid-19 Patients at the Time of Discharge
Following 3 weeks of management with either standard treatment alone or standard treatment plus allopurinol, most anthropometric and inflammatory variables returned to near normal values, mainly in mild-moderate Covid-19 patients. The clinical score was better in mild-moderate Covid-19 patients (1.11 ± 0.63) as compared with patients with severe Covid-19. The clinical score was also better in patients with severe Covid-19 on standard treatment plus allopurinol than those on the standard treatment alone (P = 0. 00,001). The mortality rate was zero in mild-moderate Covid-19 patients; however, the mortality rate was 2 (10.0%) in patients with severe Covid-19 on standard treatment and 5.5% in patients with severe Covid-19 on standard treatment plus allopurinol (Table 3).
Table 3.
Effects of Allopurinol add on the Standard Treatment of Severe Covid-19 Patients on the Anthropometric and Inflammatory Variable Compared with Severe Covid-19 Patients on the Standard Treatment Alone and Mild to Moderate Covid-19 Patients at the Time of Discharge
| The parameters | A (n = 39) | B (n = 20) | C (n = 18) | I | II | III | ANOVA |
|---|---|---|---|---|---|---|---|
| SBP (mmHg) | 130.780 ± 6.03 | 138.21 ± 7.21 | 134.05 ± 7.314 | 0.0004 | Ns | Ns | 0.0005 |
| DBP (mmHg) | 78.22 ± 7.31 | 87.51 ± 6.12 | 85.28 ± 5.43 | 0.00001 | 0.001 | Ns | 0.00001 |
| PP (mmHg) | 52.56 ± 6.72 | 50.70 ± 6.88 | 48.77 ± 7.31 | Ns | Ns | Ns | 0.15 |
| MAP (mmHg) | 95.74 ± 4.31 | 104.40 ± 6.29 | 101.54 ± 5.91 | 0.00001 | 0.0007 | Ns | 0.00001 |
| SaO2 (%) | 97.93 ± 1.30 | 91.95 ± 2.52 | 95.92 ± 2.11 | 0.00001 | 0.001 | 0.00001 | 0.00001 |
| D-dimer (ng/mL) | 210.12 ± 9.42 | 321.30 ± 11.05 | 281.17 ± 10.81 | Ns | 0.04 | 0.00001 | 0.00001 |
| LDH (U/L) | 216.21 ± 12.05 | 395.03 ± 13.71 | 235.33 ± 11.81 | Ns | 0.00001 | Ns | 0.00001 |
| Ferritin (ng/mL) | 233.38 ± 12.93 | 331.73 ± 13.94 | 255.61 ± 9.03 | Ns | 0.00001 | 0.00001 | 0.00001 |
| CRP (mg/L) | 6.24 ± 1.05 | 13.96 ± 2.04 | 8.62 ± 2.72 | 0.00001 | 0.0001 | 0.00001 | 0.00001 |
| Procalcitonin (ng/mL) | 0.17 ± 0.031 | 0.19 ± 0.01 | 0.18 ± 0.01 | 0.007 | Ns | Ns | 0.009 |
| Uric acid (mg/dL) | 6.73 ± 1.77 | 8.56 ± 2.06 | 7.01 ± 1.33 | 0.009 | Ns | 0.02 | 0.001 |
| ET-1 (pg/mL) | 21.09 ± 4.33 | 33.12 ± 4.12 | 24.11 ± 4.99 | 0.00001 | 0.05 | 0.00001 | 0.00001 |
| CT scan score (%) | 0.19 ± 0.05 | 2.01 ± 0.09 | 1.08 ± 0.01 | Ns | Ns | Ns | Ns |
| WBC (103/µL) | 9.22 ± 2.51 | 11.07 ± 2.08 | 9.51 ± 3.86 | Ns | Ns | Ns | Ns |
| Neutrophil (%) | 61.09 ± 7.94 | 72.94 ± 6.49 | 65.18 ± 6.64 | 0.00001 | 0.12 | 0.004 | 0.00001 |
| Lymphocytes (%) | 34.68 ± 4.92 | 22.97 ± 5.03 | 30.85 ± 5.97 | 0.00001 | 0.00001 | 0.03 | 0.00001 |
| NLR | 1.67 ± 0.56 | 3.17 ± 0.98 | 2.11 ± 0.44 | 0.00001 | 0.06 | 0.00001 | 0.00001 |
| Clinical score (0–7) | 1.11 ± 0.63 | 3.05 ± 0.83 | 2.03 ± 0.39 | 0.00001 | 0.00001 | 0.00001 | 0.00001 |
| Mortality rate (%) | 0% | 2(10%) | 1(5.56%) | ………. | ………. | Ns | ……… |
Data presented as mean ± SD. A: Patients with mild-moderate Covid-19. B: Patients with severe Covid-19 on the standard treatment only. C: Patients with severe Covid-19 on the standard treatment plus allopurinol. I: A vs. B, II: A vs. C, III: B vs. C. Ns not significant, SBP systolic blood pressure, DBP diastolic blood pressure, PP pulse pressure, MAP mean arterial pressure, SaO2 oxygen saturation, LDH lactate dehydrogenase, CRP C-reactive protein, ET-1 endothelin-1, NLR neutrophil–lymphocyte ratio
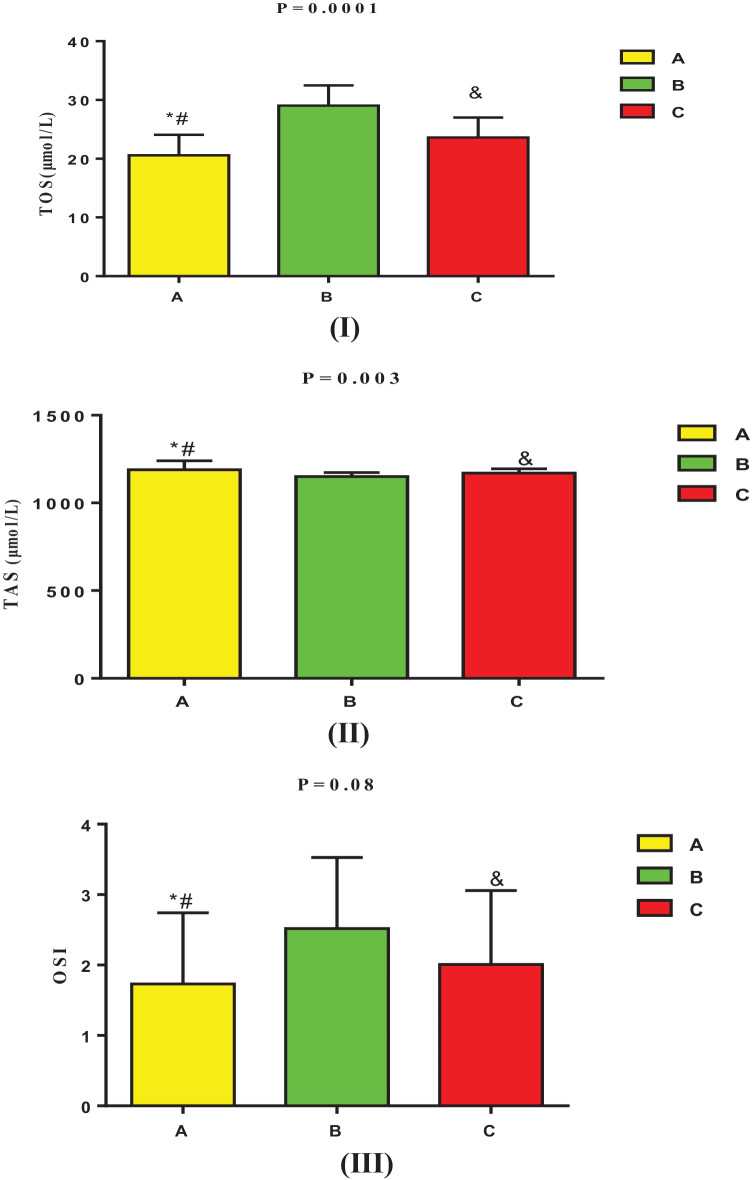
Regarding oxidative status at the time of discharge, TOS was low in mild-moderate Covid-19 patients (20.57 ± 3.51 µmol/L) compared to the severely affected patients (P = 0.00001). As well, TOS was lower in patients with severe Covid-19 on standard treatment plus allopurinol (23.61 ± 3.41 µmol/L) compared with patients with severe Covid-19 on standard treatment (29.04 ± 3.45 µmol/L) (P = 0.00001). The TAS was better in mild-moderate Covid-19 (1188.94 ± 51.62 µmol/L) as compared with severely affected patients. There was an insignificant difference between patients with severe Covid-19 on standard treatment with or without allopurinol (P = 0.86). OSI at the time of discharge was not significantly different among treated patients (P = 0.09) (Fig. 3). At the time of discharge, the oxidative status of Covid-19 patients was significantly improved compared with that at admission (P = 0.01).
Fig. 3.
Oxidative statue in Covid-19 regarding the effect of allopurinol treatment at time of discharge: (I): total oxidant status (TOS) was lower in mild-moderate Covid-19 patients as compared with severely Covid-19 patients on standard treatment alone (*P = 0.0001 and #P = 0.0008) as compared with severely affected Covid-19 patients on standard treatment plus allopurinol. TOS was lower in severely affected Covid-19 patients on standard treatment plus allopurinol than severely affected Covid-19 patients on standard treatment alone (&P = 0.0001). (II): Total antioxidant status (TAS) was higher in mild-moderate Covid-19 patients as compared with severely Covid-19 patients on standard treatment alone (*P = 0.002), and not significant (#P = 0.87) as compared with severely affected Covid-19 patients on standard treatment plus allopurinol. TAS was higher in severely affected Covid-19 patients on standard treatment plus allopurinol than severely affected Covid-19 patients on standard treatment alone but was not significant (&P = 0.09). (III): Oxidative stress index (OSI) was lower but insignificant in mild-moderate Covid-19 patients as compared with severely Covid-19 patients on standard treatment alone (*P = 0.07), but not significant as compared with severely affected Covid-19 patients on standard treatment plus allopurinol (#P = 0.08). OSI was lower in severely affected Covid-19 patients on standard treatment plus allopurinol than severely affected Covid-19 patients on standard treatment alone, but was insignificant (&P = 0.09).
Indeed, the present study revealed that uric acid serum level was significantly correlated with inflammatory and oxidative stress biomarkers in Covid-19 patients at admission. However, this correlation was reduced slightly in Covid-19 patients at discharge time (Table 4).
Table 4.
Correlation of Uric Acid with Inflammatory and Oxidative Stress Biomarkers in Covid-19 Patients
| Variables | At time of admission (n = 80) | At time of discharge(n = 77) | ||||
|---|---|---|---|---|---|---|
| r | P | 95% CI | r | P | 95% CI | |
| SBP (mmHg) | 0.19 | 0.09 | −0.031–0.393 | 0.16 | 0.16 | −0.06–0.371 |
| DBP(mmHg) | 0.20 | 0.07 | −0.021–0.402 | 0.20 | 0.08 | −0.025–0.406 |
| PP(mmHg) | 0.21 | 0.06 | −0.162–0.276 | 0.19 | 0.09 | −0.035–0.397 |
| MAP(mmHg) | 0.23 | 0.04 | −0.01–0.411 | 0.12 | 0.29 | −0.107–0.335 |
| SaO2 (%) | −0.22 | 0.04 | −0.419–0.00 | −0.27 | 0.01 | −0.466–0.994 |
| D-dimer (ng/mL) | 0.51 | 0.001 | 0.327–0.656 | 0.33 | 0.003 | 0.114–0.516 |
| LDH (U/L) | 0.48 | 0.001 | 0.291–633 | 0.29 | 0.01 | 0.071–0.483 |
| Ferritin(ng/mL) | 0.51 | 0.001 | 0.327–656 | 0.35 | 0.001 | 0.137–0.532 |
| CRP (mg/L) | 0.61 | 0.001 | 0.451–0.732 | 0.33 | 0.003 | 0.114–0.516 |
| Procalcitonin (ng/mL) | 0.49 | 0.001 | 0.303–0.641 | 0.28 | 0.01 | 0.06–0.474 |
| ET-1(pg/mL) | 0.72 | 0.00001 | 0.594–0.811 | 0.36 | 0.001 | 0.148–0.540 |
| CT scan score (%) | 0.53 | 0.001 | 0.351–0.672 | 0.13 | 0.25 | −0.097–0.344 |
| WBC (103/µL) | 0.39 | 0.001 | 0.186–0.562 | 0.21 | 0.06 | −0.015–0.414 |
| Neutrophil (%) | 0.61 | 0.0001 | 0.451–0.732 | 0.30 | 0.008 | 0.081–0.491 |
| Lymphocytes (%) | −0.64 | 0.001 | −0.754–489 | −0.53 | 0.0001 | −0.694–0.347 |
| NLR (%) | 0.58 | 0.001 | 0.413–0.709 | 0.21 | 0.06 | −0.015–0.414 |
| TAS(µmol/L) | −0.75 | 0.0001 | −0.833–635 | −0.31 | 0.006 | −0.499–0.92 |
| TOS(µmol/L) | 0.56 | 0.001 | 0.388–694 | 0.29 | 0.01 | 0.071–0.483 |
| OSI | 0.84 | 0.00001 | 0.761–0.895 | 0.36 | 0.001 | 0.148–0.540 |
| Clinical score (0–7) | ……. | ………… | ………… | −0.33 | 0.003 | 0.114–0.516 |
| Mortality rate (%) | ……. | ……… | …………… | 0.20 | 0.08 | −0.025–0.406 |
SBP systolic blood pressure, DBP diastolic blood pressure, PP pulse pressure, MAP mean arterial pressure, SaO2 oxygen saturation, LDH lactate dehydrogenase, CRP C-reactive protein, ET-1 endothelin-1, NLR neutrophil-lymphocyte ratio, OSI oxidative stress index
Furthermore, OSI in the present study was significantly correlated with the inflammatory and oxidative stress biomarkers, uric acid, a biomarker of ED, and biomarkers of lung injury biomarkers in Covid-19 patients at the time of admission. Following 3 weeks of treatment with standard treatment and/or allopurinol, reduction of OSI was associated with improvement of the clinical score at the time of discharge of Covid-19 patients (Table 5).
Table 5.
Correlation of Oxidative Stress Index with Inflammatory and Oxidative Stress Biomarkers in Covid-19 Patients
| Variables | At time of admission (n = 80) | At time of discharge (n = 77) | ||||
|---|---|---|---|---|---|---|
| r | P | 95% CI | r | P | 95% CI | |
| SBP (mmHg) | 0.18 | 0.11 | −0.041–0.385 | 0.16 | 0.16 | −0.066–0.371 |
| DBP (mmHg) | 0.21 | 0.06 | −0.01–0.411 | 0.20 | 0.08 | −0.025–0.406 |
| PP (mmHg) | 0.20 | 0.07 | −0.021–0.402 | 0.14 | 0.22 | −0.004–0.423 |
| MAP (mmHg) | 0.22 | 0.04 | 0.00–0.419 | 0.17 | 0.13 | −0.056–0.380 |
| SaO2 (%) | −0.23 | 0.04 | −0.428–0.011 | −0.29 | 0.01 | 0.483–0.071 |
| D-dimer (ng/mL) | 0.37 | 0.007 | 0.164–545 | 0.30 | 0.008 | 0.081–0.491 |
| LDH (U/L) | 0.29 | 0.009 | 0.075–0.497 | 0.19 | 0.09 | −0.035–0.397 |
| Ferritin (ng/mL) | 0.44 | 0.00004 | 0.244–0.602 | 0.15 | 0.19 | −0.077–0.362 |
| CRP (mg/L) | 0.42 | 0.0001 | 0.221–0.586 | 0.30 | 0.008 | 0.081–0.491 |
| Procalcitonin (ng/mL) | 0.49 | 0.0001 | 0.303–0.641 | 0.21 | 0.06 | −0.015–0.414 |
| ET-1 (pg/mL) | 0.70 | 0.0001 | 0.568–0.797 | 0.30 | 0.008 | 0.081–0.491 |
| CT scan score (%) | 0.33 | 0.002 | 0.119–0.513 | 0.19 | 0.09 | −0.035–0.397 |
| WBC (103/µL) | 0.30 | 0.006 | 0.086–0.488 | 0.20 | 0.08 | −0.025–0.406 |
| Neutrophil (%) | 0.60 | 0.0001 | 0.438–0.724 | 0.31 | 0.006 | 0.092–0.499 |
| Lymphocytes (%) | −0.34 | 0.002 | 0.521–0.613 | −0.43 | 0.0001 | −0.597–0.228 |
| NLR (%) | 0.48 | 0.0001 | 0.291–0.633 | 0.25 | 0.02 | 0.028–0.499 |
| TAS (µmol/L) | −0.45 | 0.0001 | −0.609–0.256 | −0.29 | 0.01 | −0.483–0.710 |
| TOS (µmol/L) | 0.58 | 0.0001 | 0.413–0.709 | 0.25 | 0.02 | 0.028–0.499 |
| Uric acid (mg/dL) | 0.84 | 0.0001 | 0.761–0.895 | 0.36 | 0.001 | 0.148–0.540 |
| Clinical score (0–7) | ……… | ……… | −0.30 | 0.008 | 0.081–0.491 | |
| Mortality rate (%) | ……. | ………… | 0.19 | 0.09 | −0.035–0.397 | |
SBP systolic blood pressure, DBP diastolic blood pressure, PP pulse pressure, MAP mean arterial pressure, SaO2 oxygen saturation, LDH lactate dehydrogenase, CRP C-reactive protein, ET-1 endothelin-1, NLR neutrophil-lymphocyte ratio
DISCUSSION
The present study illustrated that most of the recruited Covid-19 patients either of mild-moderate or severe form had underlying comorbidities like hypertension and IHD, which are regarded as risk factors for Covid-19 severity as reported by a recent study [28]. The present findings revealed that SBP, DBP, and MAP were higher in patients with severe Covid-19 than mild-moderate Covid-19 patients that might be due to SARS-CoV-2-induced cardio-metabolic changes. Increasing Ang II level due to downregulation of ACE2 and linked peripheral vasoconstriction could be the proposed mechanism for developing Covid-19-mediated hypertension [29]. In addition, severe hypertension increases Covid-19 severity due to delay of viral clearance and exacerbation of pulmonary inflammation [30].
The present study also showed that the inflammatory biomarkers and biomarkers of lung injury were higher in patients with severe Covid-19 than mild-moderate Covid-19 patients. Martinez-Mesa et al. observed that inflammatory and lung injury biomarkers are linked with ARDS development and Covid-19 severity [31]. In addition, oxidative stress was augmented in patients with severe Covid-19 as measured by oxidative stress index (OSI). Different studies revealed that OS is correlated with Covid-19 due to ROS generation and the reduction of endogenous antioxidant capacity [32]. Besides, NLR was also increased in patients with severe Covid-19 since NLR is linked with ARDS development and Covid-19 severity [33].
The main context of the present study is the potential effects of allopurinol on the inflammatory biomarkers and oxidative stress in Covid-19 patients. Patients with severe Covid-19 experienced lower inflammatory biomarkers and OS levels when treated with allopurinol. Furthermore, it has been reported that allopurinol has critical anti-inflammatory effects [34]. This anti-inflammatory effect is mediated through inhibition of inflammatory signaling pathways such as nuclear factor kappa B (NF-κB) and nod-like receptor pyrin 3(NLRP3) inflammasome [34]. Both NF-κB and NLRP3 inflammasome are directly activated by SARS-CoV-2 and associated with the release of pro-inflammatory cytokines and the development of ALI/ARDS [35]. Herein, allopurinol in the present study reduced lung CT scan scores percentage, reflecting the severity of ALI/ARDS in patients with severe Covid-19 compared to mild-moderate Covid-19. However, allopurinol did not reduce lung CT scan scores compared to patients with severe Covid-19 on standard treatment only.
Furthermore, Kuipers et al. reported that pre-treatment with allopurinol reduces ventilator-induced-ALI by attenuating lung barrier dysfunction [36]. Therefore, SaO2% was improved in allopurinol-treated patients compared with severe Covid-19 on standard treatment alone due to its pulmo-protective effect as reported previously [37]. Likewise, exaggerated XO and high uric serum are linked with the development of ALI due to activation of NF-κB and NLRP3 inflammasome with the high building of ROS [38, 39].
Thus, the inflammatory biomarkers CRP and procalcitonin declined in patients with severe Covid-19 on standard treatment plus allopurinol compared with standard treatment only. However, LDH and ferritin were significantly reduced in patients with severe Covid-19 on standard treatment plus allopurinol compared with that on the standard treatment only, as allopurinol does not affect LDH ferritin as reported by various studies [40].
On the other hand, OS was reduced in patients with severe Covid-19 on allopurinol treatment compared with the standard treatment only as evaluated by OSI. It has been reported that allopurinol reduces OS through activation of nuclear factor erythroid 2-related factor 2 (Nrf2), which maintains homeostasis of inner redox and attenuates activated autophagy [41]. Furthermore, Okafor and colleagues observed that the antioxidant effect of allopurinol is through inhibition of vascular ion channel and mitochondrial abnormalities [42].
High OS in Covid-19 is associated with the development of ED, as evident by the high serum level of ET-1, a biomarker of endothelial function [13]. Patients with severe Covid-19 with allopurinol treatment experienced a lower level of ET-1 than severe Covid-19 patients on the standard treatment only. It has been shown that allopurinol reduces ET-1 by reducing uric acid serum level, a potent activator of ET-1, as evident in the present study [43]. Furthermore, both OS and ED are linked with the progression of coagulopathy and thrombosis-mediated ALI/ARDS [44]. Recently, Lucijanic et al. revealed that hyperuricemia predisposes for severe arterial and venous thrombosis, and the use of allopurinol is associated with a low risk of thrombosis [45]. In the present study, high serum uric acid was significantly correlated with D-dimer, a biomarker of coagulopathy. Besides, high serum uric acid in patients with severe Covid-19 was significantly correlated with TOS and OSI and was negatively correlated with TAS. These findings of the present study suggest that a high uric serum level is implicated in the pathogenesis and progression of ED, OS, and coagulopathy.
Of note, hyperuricemia may induce ED through activation of the transition of vascular endothelial cells to mesenchymal one by induction of OS [46]. This effect is substantially blocked by the effect of allopurinol, probenecid, and antioxidant agents [ 46]. Cai et al. observed that hyperuricemia-induced ED is mediated through activation expression of high mobility group box protein-1 (HMGB-1) and receptor for advanced glycation end-product (RAGE) [47]. Taken together, activated HMGB-1 and RAGE are linked with the development of ED and Covid-19 severity [48]. Furthermore, hyperuricemia may trigger a prothrombotic status due to the development of ED, OS, and endothelial inflammation [49]. Otani et al. observed that hyperuricemia is linked with ED through inhibition of endothelial NO [50]. A previous study confirmed that allopurinol improves ED by regulating endothelial NO synthesis and release [49, 51]. Therefore, allopurinol reduces uric acid or independently reduces the risk of ED, OS, and coagulopathy, as revealed in the present study.
Furthermore, following 3 weeks of treatment of Covid-19 patients with either of standard treatment alone or with allopurinol, the clinical score was mainly improved in patients on allopurinol treatment. These results suggest that allopurinol has a protective effect against ALI/ARDS by attenuating SARS-CoV-2-induced ALI as reported by different studies [21, 52]. In addition, allopurinol and other XO inhibitors like febuxostat have antiviral effects mainly against the herpes simplex virus, so it is effective for recurrent herpes labialis [18]. The antiviral mechanism of allopurinol might be through inhibition of neutrophils to release of IL-2, with attenuation of polyclonal T- cell activation t hat involved in the propagation of cytokine storm in viral infections [53]. Furthermore, different studies illustrated that allopurinol reduces viral infection-induced exaggerated inflammatory reactions by inhibiting the release of IL-1β and IL-6 [54] linked with Covid-19 severity.
Indeed, XO plays a potential role in various viral infections since activating intracellular stress signaling by viral virions induces pro-free radical enzymes, including XO [55]. Excessive activation of XO during viral infections, including SARS-CoV-2, is connected with the generation of free radicals and induction of oxidative stress [56]. As well, XO, through the generation of free radicals, may cause damage and necrosis of T lymphocyte leading to lymphopenia, a hallmark of Covid-19 severity [57, 58]. Besides, over-activated XO triggers the release of pr o-inflammatory cytokines with the development of cytokine storms causing multi-organ failure [38]. The experimental study of Jacob et al. illustrated that activation of XO contributes to sustained respiratory epithelial injury through oxidative-dependent pathway [38]. These findings suggest that XO stimulation during SARS-CoV-2 infection leads to respiratory injury through direct production of ROS or indirectly by induction release of pro-inflammatory cytokines [59, 60]. Undeniably, exaggerated XO activity in respiratory syncytial virus infection is associated with increased uric acid in the bronchoalveolar lavages on days 2–8 post-infection [61]. Likewise, a high uric acid serum level is linked with Covid-19 severity and mortality and is regarded as a prognostic risk factor for ARDS development [62].
In addition, XO induces neutrophil recruitment by releasing chemokines and cytokines, causing more inflammation and oxidative reaction due to the production of superoxide anions from activated neutrophils in Covid-19 patients [63]. This finding might explain a higher NLR in patients with severe Covid-19, as revealed in the present study. Unfortunately, XO activity was not measured in the present study.
Both uric acid and superoxide anions, products of XO, activate macrophages, endothelial cells, and epithelial cells to form and release pro-inflammatory cytokines [64]. As well, neutrophil migrations and recruitments around infected alveolar epithelial cells may trigger formation and accumulations of neutrophils extracellular trap (NETs) and, together with platelets, may induce thrombus formation [65]. In addition, micro-pulmonary thrombosis may provoke the development of hypoxic injury and the development of ALI/ARDS in patients with severe Covid-19 [66]. Therefore, XO inhibitor allopurinol may reduce the recruitment of neutrophils and inhibit the formation of NETs and the release of pro-inflammatory cytokines.
Moreover, circulating XO can bind endothelial cells catalyzing the formation of superoxide anion and uric acid, which trigger the release of pro-inflammatory cytokines and subsequent apoptosis of endothelial cells [67]. These changes lead to disrupting function and permeability of endothelial cell barriers with the development of ED. Therefore, inhibition of XO by allopurinol attenuates ED in diabetic patients [22]. Thus, allopurinol may inhibit the development of SAR-CoV-2-induced ED in Covid-19 patients through mitigation of inflammation and oxidative stress-induced ED [68].
Regarding the development of hypoxia in Covid-19, at first, pulmonary vasoconstriction is developed due to high circulating Ang II, leading to high pressure in the pulmonary vessels and leakage of fluids into the alveoli causing pulmonary edema and atelectasis with the development of ARDS [69]. As a result, left to right shunting (LRS) will develop, causing an incomplete gas exchange and persistence hypoxia not responding to the oxygen supplement [70]. However, NET formation and lung inflammation may cause pulmonary vasodilatation due to loss of response to the hypoxia. Pulmonary vasodilatation increases LRS with the development of silent hypoxia [71]. Daly et al. illustrated that SAR-CoV-2 binds neuropilin-1, which activates vascular endothelial growth factor (VEGF) receptors leading to pulmonary vasodilatations with an intensification of LRS [71]. Therefore, XO-induced NETs formation with free radical production contributes to hypoxic pulmonary endothelial injury progression and loss of hypoxic response. Allopurinol inhibits NETs formation by reducing citrullinated histone [72], so allopurinol inhibits NETs-induced ALI and pulmonary ED.
Taken together, these findings indicate that allopurinol has potential effects in the reduction of hypoxia, as confirmed in the present study. Thus, the present study illustrated that allopurinol had pleiotropic effects, which reduced Covid-19 severity. Furthermore, the present findings confirmed that allopurinol treatment mitigated ED, inflammatory, and OS disorders in patients with severe Covid-19. The primary outcomes of the present study revealed that allopurinol had a significant effect on the improvement of the clinical score without a significant effect on the mortality rate compared to patients with severe Covid-19 on the standard treatment alone, though the secondary outcomes (OS, inflammatory disorders, radiological and clinical recoveries) were significantly ameliorated at the time of discharge.
Of interest, the present study had limitations, including small sample size, XO activity was not evaluated, and pro-inflammatory cytokines like IL-6 and TNF-α were not estimated. However, despite these limitations, this study, to our knowledge, is regarded as a novel study that describes the potential role of allopurinol in treating Covid-19. Therefore, in view of these results, clinical trial and large sample size prospective are recommended in this regard.
CONCLUSION
Covid-19 severity is linked with high OS and inflammatory reaction with ED development. Furthermore, high uric acid in patients with severe Covid-19 is correlated with high OS and inflammatory biomarkers. Allopurinol with standard treatment in patients with severe Covid-19 reduced oxidative and inflammatory disorders with significant amelioration of ED and clinical outcomes. In the sight of these results, clinical trial and large sample size perspective are suggested in this regard to observe the clinical efficacy of allopurinol in treating Covid-19 patients.
Acknowledgements
The authors extend their appreciation to the Researchers Supporting Project number (RSP2022R418), King Saud University, Riyadh, Saudi Arabia
Author Contribution
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by all the authors. The first draft of the manuscript was written by Ali I. Al-Gareeb and Hayder M. Al-kuraishy. All authors read and approved the final manuscript.
Data Availability
All the available data are included in the manuscript.
Declarations
Ethics Approval
This study was approved by the Scientific Jury and Ethical Committee in College of Medicine, Al-Mustansiriyah University, in collaboration with Al-Atah Specialized Medical Center for Covid-19 management, on Apr 10, 2021 (TRW34 in 2021).
Consent to Participate
Informed consent was obtained from all individual participants included in the study according to the international diagnostic criteria from Al-Atah Specialized Medical Center for Covid-19 Baghdad, Iraq.
Consent to Publish
Not applicable.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Hayder M. Al-kuraishy, Email: Hayderm36@yahoo.com
Ali I. Al-Gareeb, Email: Dr.alialgareeb78@yahoo.com
Marwa S. Al-Niemi, Email: marwasalih83@yahoo.com
Reem M. Aljowaie, Email: raljowaie@ksu.edu.sa
Saeedah Musaed Almutairi, Email: alsaeedah@ksu.edu.sa.
Athanasios Alexiou, Email: alexiou@ngcef.net.
Gaber El-Saber Batiha, Email: gaberbatiha@gmail.com, Email: dr_gaber_batiha@vetmed.dmu.edu.eg.
References
- 1.Moubarak M, Kasozi KI, Hetta HF, Shaheen HM, Rauf A, Al-kuraishy HM, Qusti S, Alshammari EM, Ayikobua ET, Ssempijja F, Afodun AM. The rise of SARS-CoV-2 variants and the role of convalescent plasma therapy for management of infections. Life. 2021;11(8):734. doi: 10.3390/life11080734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Kuraishy, H.M., A.I. Al-Gareeb, N. Qusty, N. Cruz-Martins, and G.E. Batiha. 2021. Sequential doxycycline and colchicine combination therapy in Covid-19: The salutary effects. Pulmonary Pharmacology & Therapeutics. 67:102008. [DOI] [PMC free article] [PubMed]
- 3.Al-Kuraishy HM, Al-Gareeb AI, Alblihed M, Cruz-Martins N, Batiha GE. COVID-19 and risk of acute ischemic stroke and acute lung injury in patients with type ii diabetes mellitus: The anti-inflammatory role of metformin. Frontiers in Medicine. 2021;19(8):110. doi: 10.3389/fmed.2021.644295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Kuraishy, H.M., A.I Al-Gareeb, H. Faidah, T.J. Al-Maiahy, N. and Cruz-Martins, G.E. Batiha. 2021. The looming effects of estrogen in Covid-19: a Rocky Rollout. Frontiers in Nutrition. 8. [DOI] [PMC free article] [PubMed]
- 5.Al-Kuraishy HM, Al-Gareeb AI, Alzahrani KJ, Cruz-Martins N, Batiha GE. The potential role of neopterin in Covid-19: A new perspective. Molecular and Cellular Biochemistry. 2021;28:1–6. doi: 10.1007/s11010-021-04232-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Kuraishy HM, Al-Gareeb AI, Cruz-Martins N, Batiha GE. Hyperbilirubinemia in Gilbert syndrome attenuates Covid-19 induced-metabolic disturbances: A case-report study. Frontiers in cardiovascular medicine. 2021;8:71. doi: 10.3389/fcvm.2021.642181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pincemail J, Cavalier E, Charlier C, Cheramy-Bien JP, Brevers E, Courtois A, Fadeur M, Meziane S, Goff CL, Misset B, Albert A. Oxidative stress status in COVID-19 patients hospitalized in intensive care unit for severe pneumonia. A pilot study. Antioxidants. 2021;10(2):257. doi: 10.3390/antiox10020257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muhammad Y, Kani YA, Iliya S, Muhammad JB, Binji A, El-Fulaty Ahmad A, Kabir MB, Umar Bindawa K, Ahmed AU. Deficiency of antioxidants and increased oxidative stress in COVID-19 patients: A cross-sectional comparative study in Jigawa. Northwestern Nigeria. SAGE open medicine. 2021;9:2050312121991246. doi: 10.1177/2050312121991246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mete, A.Ö., K. Kocak, A. Saracaloglu, S. Demiryürek, Ö. Altınbaş, and A.T. Demiryürek. 2021. Effects of antiviral drug therapy on dynamic thiol/disulphide homeostasis and nitric oxide levels in COVID-19 patients. European journal of pharmacology. 7:174306. [DOI] [PMC free article] [PubMed]
- 10.Wang M, Liu Y, Liang Y, Naruse K, Takahashi K. Systematic understanding of pathophysiological mechanisms of oxidative stress-related conditions—diabetes mellitus, cardiovascular diseases, and ischemia–reperfusion injury. Frontiers in Cardiovascular Medicine. 2021;13(8):295. doi: 10.3389/fcvm.2021.649785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ogunlana, O.O., B.O. Adetuyi, M. Rotimi, A. Adeyemi, J. Akinyele, O.E. Ogunlana, O.A. Adetuyi, O.A. Adebisi, E.K. Opata, R.S. Baty, and G.E. Batiha. 2021. Hypoglycemic and antioxidative activities of ethanol seed extract of Hunteria umbellate (Hallier F.) on streptozotocin-induced diabetic rats. Clinical Phytoscience. 7(1):1–9.
- 12.Karkhanei, B., E.T. Ghane, and F. Mehri. 2021. Evaluation of oxidative stress level: total antioxidant capacity, total oxidant status and glutathione activity in patients with Covid-19. New Microbes and New Infections. 42:100897. [DOI] [PMC free article] [PubMed]
- 13.Kadhim SS, Al-Windy SA, Al-Kuraishy HM, Al-Gareeb AI. Endothelin-1 is a surrogate biomarker link severe periodontitis and endothelial dysfunction in hypertensive patients: The potential nexus. Journal of International Oral Health. 2019;11(6):369. doi: 10.4103/jioh.jioh_158_19. [DOI] [Google Scholar]
- 14.Al-Kuraishy, H.M., A.H. Al-Kuraishi, S. Al-Windy, and A.I. Al-Gareeb. 2019. Toxoplasmosis and risk of endothelial dysfunction: role of oxidative stress and pro-inflammatory mediators. Archives of Clinical Infectious Diseases. 14(6).
- 15.Chang, R., A.D. Abrar Mamun, and N.T. Le. 2020. SARS-CoV-2 mediated endothelial dysfunction: the potential role of chronic oxidative stress. Frontiers in Physiology. 11. [DOI] [PMC free article] [PubMed]
- 16.Zhang S, Xu T, Shi Q, Li S, Wang L, An Z, Su N. Cardiovascular safety of febuxostat and allopurinol in hyperuricemic patients with or without gout: A network meta-analysis. Frontiers in medicine. 2021;8:891. doi: 10.3389/fmed.2021.698437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Axton ER, Cristobal E, Choi J, Miranda CL, Stevens JF. Metabolomics-driven elucidation of cellular nitrate tolerance reveals ascorbic acid prevents nitroglycerin-induced inactivation of xanthine oxidase. Frontiers in pharmacology. 2018;25(9):1085. doi: 10.3389/fphar.2018.01085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pérez-Mazliah D, Albareda MC, Alvarez MG, Lococo BE, Bertocchi GL, Petti M, Viotti R, Laucella SA. Allopurinol reduces antigen-specific and polyclonal activation of human T cells. Frontiers in immunology. 2012;21(3):295. doi: 10.3389/fimmu.2012.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams CD, McGill MR, Lebofsky M, Bajt ML, Jaeschke H. Protection against acetaminophen-induced liver injury by allopurinol is dependent on aldehyde oxidase-mediated liver preconditioning. Toxicology and applied pharmacology. 2014;274(3):417–424. doi: 10.1016/j.taap.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Masson E, Synold TW, Relling MV, Schuetz JD, Sandlund JT, Pui CH, Evans WE. Allopurinol inhibits de novo purine synthesis in lymphoblasts of children with acute lymphoblastic leukemia. Leukemia. 1996;10(1):56–60. [PubMed] [Google Scholar]
- 21.Pratomo IP, Noor DR, Kusmardi K, Rukmana A, Paramita RI, Erlina L, Fadilah F, Gayatri A, Fitriani M, Purnomo TT, Ariane A. Xanthine oxidase-induced inflammatory responses in respiratory epithelial cells: A review in immunopathology of COVID-19. International Journal of Inflammation. 2021;6:2021. doi: 10.1155/2021/1653392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-Kuraishy HM, Sami OM, Hussain NR, Al-Gareeb AI. Metformin and/or vildagliptin mitigate type II diabetes mellitus induced-oxidative stress: The intriguing effect. Journal of Advanced Pharmaceutical Technology & Research. 2020;11(3):142. doi: 10.4103/japtr.JAPTR_18_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Nami MS, Al-Kuraishy HM, Al-Gareeb AI, Al-Mamoori F. Metabolic profile and prolactin serum levels in men with type 2 diabetes mellitus: Old-new rubric. International journal of critical illness and injury science. 2019;9(3):120. doi: 10.4103/IJCIIS.IJCIIS_40_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Nami MS, Al-Kuraishy HM, Al-Gareeb AI. Impact of thioctic acid on glycemic indices and associated inflammatory-induced endothelial dysfunction in patients with type 2 diabetes mellitus: A case control study. International Journal of Critical Illness and Injury Science. 2020;10(5):21. doi: 10.4103/IJCIIS.IJCIIS_62_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shi H, Han X, Jiang N, Cao Y, Alwalid O, Gu J, Fan Y, Zheng C. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: A descriptive study. The Lancet infectious diseases. 2020;20(4):425–434. doi: 10.1016/S1473-3099(20)30086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Francone M, Iafrate F, Masci GM, Coco S, Cilia F, Manganaro L, Panebianco V, Andreoli C, Colaiacomo MC, Zingaropoli MA, Ciardi MR. Chest CT score in COVID-19 patients: Correlation with disease severity and short-term prognosis. European radiology. 2020;30(12):6808–6817. doi: 10.1007/s00330-020-07033-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gude F, Riveiro V, Rodríguez-Núñez N, Ricoy J, Lado-Baleato Ó, Lourido T, Rábade C, Lama A, Casal A, Abelleira-París R, Ferreiro L. Development and validation of a clinical score to estimate progression to severe or critical state in COVID-19 pneumonia hospitalized patients. Scientific reports. 2020;10(1):1. doi: 10.1038/s41598-020-75651-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Batchu SN, Kaur H, Yerra VG, Advani SL, Kabir MG, Liu Y, Klein T, Advani A. Lung and kidney ACE2 and TMPRSS2 in renin-angiotensin system blocker–treated comorbid diabetic mice mimicking host factors that have been linked to severe COVID-19. Diabetes. 2021;70(3):759–771. doi: 10.2337/db20-0765. [DOI] [PubMed] [Google Scholar]
- 29.Batiha, G.E., A. Gari, N. Elshony, H.M. Shaheen, M.B. Abubakar, S.B. Adeyemi, and H.M. Al-Kuraishy. 2021. Hypertension and its management in COVID-19 patients: the assorted view. International Journal of Cardiology Cardiovascular Risk and Prevention.11:200121. [DOI] [PMC free article] [PubMed]
- 30.Trump S, Lukassen S, Anker MS, Chua RL, Liebig J, Thürmann L, Corman VM, Binder M, Loske J, Klasa C, Krieger T. Hypertension delays viral clearance and exacerbates airway hyperinflammation in patients with COVID-19. Nature Biotechnology. 2021;39(6):705–716. doi: 10.1038/s41587-020-00796-1. [DOI] [PubMed] [Google Scholar]
- 31.Martinez Mesa A, Cabrera César E, Martín-Montañez E, Sanchez Alvarez E, Lopez PM, Romero-Zerbo Y, Garcia-Fernandez M, Velasco Garrido JL. Acute lung injury biomarkers in the prediction of COVID-19 severity: Total thiol, ferritin and lactate dehydrogenase. Antioxidants. 2021;10(8):1221. doi: 10.3390/antiox10081221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fodor A, Tiperciuc B, Login C, Orasan OH, Lazar AL, Buchman C, Hanghicel P, Sitar-Taut A, Suharoschi R, Vulturar R, Cozma A. Endothelial Dysfunction, Inflammation, and Oxidative Stress in COVID-19—Mechanisms and Therapeutic Targets. Oxidative Medicine and Cellular Longevity. 2021;21:2021. doi: 10.1155/2021/8671713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Root-Bernstein R. Innate receptor activation patterns involving TLR and NLR synergisms in COVID-19, ALI/ARDS and sepsis cytokine storms: A review and model making novel predictions and therapeutic suggestions. International Journal of Molecular Sciences. 2021;22(4):2108. doi: 10.3390/ijms22042108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schlesinger, N., and L. Brunetti. 2020. Beyond urate lowering: Analgesic and anti-inflammatory properties of allopurinol. InSeminars in Arthritis and Rheumatism. 50(3): 444–450. WB Saunders. [DOI] [PubMed]
- 35.Batiha, G.E., A.I Al-Gareeb, S. Qusti, E.M. Alshammari, D. Rotimi, O.S. Adeyemi, and H.M. Al-Kuraishy. 2021. Common NLRP3 inflammasome inhibitors and Covid-19: Divide and Conquer. Scientific African. 18:e01084. [DOI] [PMC free article] [PubMed]
- 36.Kuipers, M.T., H. Aslami, A.P. Vlaar, N.P. Juffermans, A.M. Tuip-de Boer, M.A. Hegeman, G. Jongsma, J.J. Roelofs, T. van der Poll, M.J. Schultz, and C.W. Wieland. 2012. Pre-treatment with allopurinol or uricase attenuates barrier dysfunction but not inflammation during murine ventilator-induced lung injury. PloS one. 30;7(11):e50559. [DOI] [PMC free article] [PubMed]
- 37.Abdallah, M.A., and D.A. Mohame. 2014. Effect of acute pancreatitis on lung structure of adult male albino rats and role of allopurinol administration. Life Science Journal. 11(3).
- 38.Jacob S, Herndon DN, Hawkins HK, Enkhbaatar P, Cox RA. Xanthine oxidase contributes to sustained airway epithelial oxidative stress after scald burn. International journal of burns and trauma. 2017;7(6):98. [PMC free article] [PubMed] [Google Scholar]
- 39.Gasse P, Riteau N, Charron S, Girre S, Fick L, Pétrilli V, Tschopp J, Lagente V, Quesniaux VF, Ryffel B, Couillin I. Uric acid is a danger signal activating NALP3 inflammasome in lung injury inflammation and fibrosis. American journal of respiratory and critical care medicine. 2009;179(10):903–913. doi: 10.1164/rccm.200808-1274OC. [DOI] [PubMed] [Google Scholar]
- 40.Smith, L.T., and K. Venella. 2017. Cytokine release syndrome. Clinical Journal of Oncology Nursing. 21(2). [DOI] [PubMed]
- 41.Luo J, Yan D, Li S, Liu S, Zeng F, Cheung CW, Liu H, Irwin MG, Huang H, Xia Z. Allopurinol reduces oxidative stress and activates Nrf2/p62 to attenuate diabetic cardiomyopathy in rats. Journal of cellular and molecular medicine. 2020;24(2):1760–1773. doi: 10.1111/jcmm.14870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Okafor ON, Farrington K, Gorog DA. Allopurinol as a therapeutic option in cardiovascular disease. Pharmacology & therapeutics. 2017;1(172):139–150. doi: 10.1016/j.pharmthera.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 43.Romi MM, Arfian N, Tranggono U, Setyaningsih WA, Sari DC. Uric acid causes kidney injury through inducing fibroblast expansion, Endothelin-1 expression, and inflammation. BMC nephrology. 2017;18(1):1–8. doi: 10.1186/s12882-017-0736-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Al-Kuraishy, H.M., A.I. Al-Gareeb, M. Alblihed, N. Cruz-Martins, and G.E. Batiha. 2021. COVID-19 and risk of acute ischemic stroke and acute lung injury in patients with type ii diabetes mellitus: the anti-inflammatory role of metformin. Frontiers in Medicine. 19(8): 110 [DOI] [PMC free article] [PubMed]
- 45.Lucijanic M, Krecak I, Galusic D, Sedinic M, Holik H, Perisa V, Peric MM, Zekanovic I, Stoos-Veic T, Pejsa V, Kusec R. Higher serum uric acid is associated with higher risks of thrombosis and death in patients with primary myelofibrosis. Wiener klinische Wochenschrift. 2021;19:1–7. doi: 10.1007/s00508-020-01802-x. [DOI] [PubMed] [Google Scholar]
- 46.Ko J, Kang HJ, Kim DA, Kim MJ, Ryu ES, Lee S, Ryu JH, Roncal C, Johnson RJ, Kang DH. Uric acid induced the phenotype transition of vascular endothelial cells via induction of oxidative stress and glycocalyx shedding. The FASEB Journal. 2019;33(12):13334–13345. doi: 10.1096/fj.201901148R. [DOI] [PubMed] [Google Scholar]
- 47.Cai W, Duan XM, Liu Y, Yu J, Tang YL, Liu ZL, Jiang S, Zhang CP, Liu JY, Xu JX. Uric acid induces endothelial dysfunction by activating the HMGB1/RAGE signaling pathway. BioMed research international. 2017;1:2017. doi: 10.1155/2017/4391920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Al-kuraishy, H., A.I. Al-Gareeb, S.G. Guerreiro, N. Cruz-Martins, and G.G. Batiha. 2021. COVID-19 in relation to hyperglycemia and diabetes mellitus. Frontiers in cardiovascular medicine. 8: 335. [DOI] [PMC free article] [PubMed]
- 49.Akahane HG, Gomes RZ, Paludo KS, Linhares F, Lopes L. The influence of allopurinol and post-conditioning on lung injuries induced by lower-limb ischemia and reperfusion in Wistar rats 1. Acta cirurgica brasileira. 2017;32:746–754. doi: 10.1590/s0102-865020170090000007. [DOI] [PubMed] [Google Scholar]
- 50.Otani N, Toyoda S, Sakuma M, Hayashi K, Ouchi M, Fujita T, Anzai N, Tanaka A, Node K, Uemura N, Inoue T. Effects of uric acid on vascular endothelial function from bedside to bench. Hypertension Research. 2018;41(11):923–931. doi: 10.1038/s41440-018-0095-4. [DOI] [PubMed] [Google Scholar]
- 51.El Solh AA, Saliba R, Bosinski T, Grant BJ, Berbary E, Miller N. Allopurinol improves endothelial function in sleep apnoea: A randomised controlled study. European Respiratory Journal. 2006;27(5):997–1002. doi: 10.1183/09031936.06.00101005. [DOI] [PubMed] [Google Scholar]
- 52.El-Farrash MA, Jilan MY, El-Mongy SE. Allopurinol as a potential therapeutic agent for recurrent herpes labialis. Journal of medical and dental sciences. 2003;50(2):147–154. [PubMed] [Google Scholar]
- 53.Prieto-Moure B, Lloris-Carsí JM, Belda-Antolí M, Toledo-Pereyra LH, Cejalvo-Lapeña D. Allopurinol protective effect of renal ischemia by downregulating TNF-α, IL-1β, and IL-6 response. Journal of Investigative Surgery. 2017;30(3):143–151. doi: 10.1080/08941939.2016.1230658. [DOI] [PubMed] [Google Scholar]
- 54.Okamura Y, Inada M, Elshopakey GE, Itami T. Characterization of xanthine dehydrogenase and aldehyde oxidase of Marsupenaeus japonicus and their response to microbial pathogen. Molecular biology reports. 2018;45(4):419–432. doi: 10.1007/s11033-018-4177-9. [DOI] [PubMed] [Google Scholar]
- 55.López-Iranzo FJ, López-Rodas AM, Franco L, López-Rodas G. Pentoxifylline and oxypurinol: Potential drugs to prevent the “cytokine release (storm) syndrome” caused by SARS-CoV-2? Current pharmaceutical design. 2020;26(35):4515–4521. doi: 10.2174/1381612826666200811180232. [DOI] [PubMed] [Google Scholar]
- 56.Battelli MG, Musiani S, Tazzari PL, Stirpe F. Oxidative stress to human lymphocytes by xanthine oxidoreductase activity. Free radical research. 2001;35(6):665–679. doi: 10.1080/10715760100301191. [DOI] [PubMed] [Google Scholar]
- 57.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, Xie C, Ma K, Shang K, Wang W, Tian DS. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan. China. Clinical infectious diseases. 2020;71(15):762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ty, M.C., M. Zuniga, A. Götz, S. Kayal, P.K. Sahu, A. Mohanty, S. Mohanty, S.C. Wassmer, and A. Rodriguez. 2019. Malaria inflammation by xanthine oxidase‐produced reactive oxygen species. EMBO Molecular Medicine. 11(8):e9903. [DOI] [PMC free article] [PubMed]
- 59.Wang, D., S. Bai, Y. Cui, N. Zhao, F. Qi, J. Liu, S. Zeng, L. Xu, H. Hu, and B. Liu. 2018. Respiratory syncytial virus prevents the subsequent development of ovalbumin-induced allergic responses by inhibiting ILC2 via the IL- 33/ST2 pathway. Immunotherapy, 10(12): 1065–1076. 10.2217/imt-2018-0059 [DOI] [PubMed]
- 60.Fonseca W., C.A. Malinczak, C.F. Schuler, S.K. Best, A.J. Rasky, S.B. Morris, T.X. Cui, A.P. Popova, N.W. Lukacs. 2020. Jul Uric acid pathway activation during respiratory virus infection promotes Th2 immune response via innate cytokine production and ILC2 accumulation. Mucosal Immunology. 13(4):691-701. [DOI] [PMC free article] [PubMed]
- 61.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z. Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China. The lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alon R, Sportiello M, Kozlovski S, Kumar A, Reilly EC, Zarbock A, Garbi N, Topham DJ. Leukocyte trafficking to the lungs and beyond: Lessons from influenza for COVID-19. Nature Reviews Immunology. 2021;21(1):49–64. doi: 10.1038/s41577-020-00470-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Tang L, Xu YE, Wei Y, He X. Uric acid induces the expression of TNF-α via the ROS-MAPK-NF-κB signaling pathway in rat vascular smooth muscle cells. Molecular medicine reports. 2017;16(5):6928–6933. doi: 10.3892/mmr.2017.7405. [DOI] [PubMed] [Google Scholar]
- 64.Zhang Y, Han K, Du C, Li R, Liu J, Zeng H, Zhu L, Li A. Carboxypeptidase B blocks ex vivo activation of the anaphylatoxin-neutrophil extracellular trap axis in neutrophils from COVID-19 patients. Critical Care. 2021;25(1):1–1. doi: 10.1186/s13054-021-03482-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Al-Kuraishy, H.M., A.I. Al-Gareeb, H.A. Al-Hussaniy, N.A. Al-Harcan, A. Alexiou, and G.E. Batiha. 2021. Neutrophil Extracellular Traps (NETs) and Covid-19: a new frontiers for therapeutic modality. International Immunopharmacology. 6:108516. [DOI] [PMC free article] [PubMed]
- 66.Al-Kuraishy HM, A.I. Al-Gareeb, and G.E. Batiha. 2022. The possible role of ursolic acid in Covid-19: a real game changer. Clinical Nutrition ESPEN. [DOI] [PMC free article] [PubMed]
- 67.Al-Kuraishy, H.M., A.I. Al-Gareeb, and M.S. Al-Nami. 2020. Irbesartan attenuates gentamicin-induced nephrotoxicity in rats through modulation of oxidative stress and endogenous antioxidant capacity. International Journal of Preventive Medicine. 11. [DOI] [PMC free article] [PubMed]
- 68.Munch, M.W., A. Granholm, S.N. Myatra, B.K. Vijayaraghavan, M. Cronhjort, R.R. Wahlin, S,M. Jakob, L. Cioccari, M.N. Kjaer, G.K. Vesterlund, and T.S. Meyhoff. 2021. Higher vs lower doses of dexamethasone in patients with COVID‐19 and severe hypoxia (COVID STEROID 2) trial: Protocol and statistical analysis plan. Acta Anaesthesiologica Scandinavica. [DOI] [PMC free article] [PubMed]
- 69.Al-Kuraishy HM, Al-Gareeb AI, Alzahrani KJ, Cruz-Martins N, Batiha GE. The potential role of neopterin in Covid-19: A new perspective. Molecular and Cellular Biochemistry. 2021;476(11):4161–4166. doi: 10.1007/s11010-021-04232-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gopal, A.B., S. Chakraborty, P.K. Padha PK, A. Barik, P. Dixit, D. Chakraborty, I. Poira, S. Samal, A. Sarkar, and A. Bhattacharyya. 2021. Silent hypoxia in COVID-19: a gut microbiota connection. Current Opinion in Physiology. [DOI] [PMC free article] [PubMed]
- 71.Daly JL, Simonetti B, Klein K, Chen KE, Williamson MK, Antón-Plágaro C, Shoemark DK, Simón-Gracia L, Bauer M, Hollandi R, Greber UF. Neuropilin-1 is a host factor for SARS-CoV-2 infection. Science. 2020;370(6518):861–865. doi: 10.1126/science.abd3072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Al-Khafaji AB, Tohme S, Yazdani HO, Miller D, Huang H, Tsung A. Superoxide induces neutrophil extracellular trap formation in a TLR-4 and NOX-dependent mechanism. Molecular medicine. 2016;22(1):621–631. doi: 10.2119/molmed.2016.00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All the available data are included in the manuscript.