Abstract
Introduction
Interventions to curb the spread of COVID-19 during the 2020–2021 influenza season essentially eliminated influenza during that season. Given waning antibody titers over time, future residual population immunity against influenza will be reduced. The implication for the subsequent 2021–2022 influenza season is unknown.
Methods
An agent-based model of influenza implemented in the Framework for Reconstructing Epidemiological Dynamics simulation platform was used to estimate cases and hospitalizations over 2 successive influenza seasons. The impact of reduced residual immunity owing to protective measures in the first season was estimated over varying levels of similarity (cross-immunity) between influenza strains over the seasons.
Results
When cross-immunity between first- and second-season strains was low, a decreased first season had limited impact on second-season cases. High levels of cross-immunity resulted in a greater impact on the second season. This impact was modified by the transmissibility of strains in the 2 seasons. The model estimated a possible increase of 13.52%–46.95% in cases relative to that in a normal season when strains have the same transmissibility and 40%–50% cross-immunity in a season after a very low one.
Conclusions
Given the light 2020–2021 influenza season, cases may increase by as much as 50% in 2021–2022, although the increase could be much less, depending on cross-immunity from past infection and transmissibility of strains. Enhanced vaccine coverage or continued interventions to reduce transmission could reduce this high season. Young children may have a higher risk in 2021–2022 owing to limited exposure to infection in the previous year.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) was declared a pandemic by the WHO on March 11, 2020. Cases were identified in the U.S. in early 2020, resulting in widespread interventions to reduce the spread of the virus, including school closure and measures to decrease social interactions. These interventions impacted not only COVID-19 transmission but also the transmission of other diseases that spread by the same mechanisms. Markedly decreased influenza activity was documented in many locations after the institution of COVID-19 interventions.1, 2, 3, 4, 5 Little influenza activity was detected by the Centers for Disease Control and Prevention (CDC) in the U.S. during the 2020–2021 influenza season.6
Previous-year vaccination is believed to provide little protection from subsequent-year influenza,7 but natural infection appears to provide measurable immunity for several seasons, particularly if the circulating strains are close antigenic matches.8 The limited number of influenza cases in the U.S. in 2020–2021 has raised concerns about the possibility of a higher burden of influenza illness in the 2021–2022 season owing to reduced immunity from previous-year natural infection. Children aged <2 years may be at increased risk after a season with limited influenza because they likely have never been exposed to natural infection and therefore have immunity only from vaccination.
Modeling has been applied to infectious diseases since the 1920s and is a well-established technique for analyzing and predicting influenza epidemics.9 Historically, compartmental models were applied extensively to estimate values for the reproduction number in past epidemics and pandemics and to estimate the possible impact of interventions if applied to past and hypothetical future epidemics.10, 11, 12, 13, 14, 15 Agent-based and individual-based modeling of infectious diseases became more common when high-performance computing became available.16, 17, 18, 19, 20 This type of model requires more computing resources but allows the setting of individual-based parameters and includes randomness so that a range of results are produced. Agent-based modeling can be used to perform highly detailed investigations of possible disease scenarios, for example, the effects of changes in strain transmissibility or the impact of vaccination.
The Framework for Reconstructing Epidemiologic Dynamics (FRED) simulation platform21 is an agent-based modeling platform that was developed in response to the 2009 influenza pandemic and has been used for modeling influenza as well as other infectious and noninfectious conditions.22, 23, 24, 25 FRED models use census-based synthetic populations whose agents have realistic demographics, locations, and interaction patterns and rates, allowing for targeting of parameters by those factors. The FRED influenza model was formerly limited to simulating a single season. This study expands the pandemic model to include immunity from previous infection and from vaccination and to allow for modeling of multiple consecutive seasons of influenza. It therefore represents a novel expansion of modeling capabilities in this area and provides a starting point for more complex simulations.
To explore the impact of limited influenza activity on subsequent-year influenza burden, FRED was used to model 2-season influenza scenarios under a variety of assumptions on the impact of natural infection on second-year immunity and a variable degree of antigenic relatedness of first- and second-year circulating strains. Simulations estimated the impact of increased vaccination, continued interventions to reduce respiratory disease transmission, and the specific impact on the youngest age group in the population.
METHODS
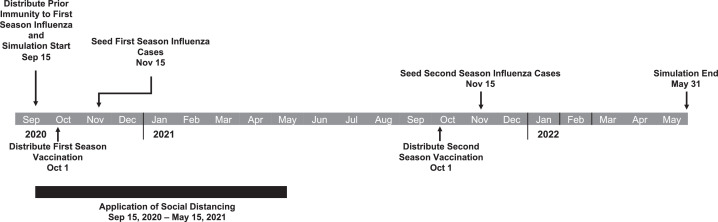
The FRED simulation platform has been described in detail previously.21 Details of simulations and the models used in this study as well as parameters used can be found in the Appendix (available online). A timeline is shown in Figure 1 . FRED uses a transmissibility parameter to represent the infectious ability of a transmissible condition. The transmissibility parameter contributes to producing R0 or Re in a simulation. A higher transmissibility parameter will produce a larger outbreak if no other parameters in the model change. Simulations were run with a low transmissibility parameter value (0.6, R0 ∼1.31, 95% CI=0.79, 1.83) and a high transmissibility parameter value (0.8, R0 ∼1.75, 95% CI=1.13, 2.37). Base model results are included in Appendix Table 1 (available online).
Figure 1.
Timeline of influenza simulation.
Apr, April; Aug, August; Dec, December; Feb, February; Jan, January; Jul, July; Jun, June; Mar, March; Nov, November; Oct, October; Sep, September
Population
Simulations were performed on a population representing Allegheny County, a medium-sized county in the southwest of Pennsylvania, with a population of approximately 1.2 million. It contains both urban and suburban areas and is large enough to capture the spread of influenza through a population. Simulations were performed with 100 repetitions to capture stochastic behavior.
Agents were immunized by age group as per CDC data using the following rates: age 0.5–17 years, probability=0.638; age 18–49 years, probability=0.384; age 50–64 years, probability=0.506; age ≥65 years, probability=0.698.26 In the model, vaccination reduces susceptibility to influenza by 40% (vaccination efficacy in CDC studies ranges between 10% and 60%) (Appendix Table 2, available online).27 , 28 Strain-specific vaccination occurs in October of the simulation year, and immunity wanes after vaccination at 7% per month.29
Immunity from previous infection was distributed by age group in the population using attack rates estimated by CDC for 2019–2020 (Appendix Table 2, available online).30
Reduced agent interactions at the population level were used to investigate the impact on second-season influenza cases. A simplified method of reducing contacts by isolating a proportion of agents in the simulation was used. Calibration runs with varied rates of isolation determined the percentage of the population needing to be isolated to prevent first-season influenza cases. Calibration results are in Appendix Section 7 (available online). The use of this method accomplishes the purpose of eliminating a first-season influenza epidemic. The method was not specifically focused on the impact of a particular social distancing intervention and does not address the nuances of various interventions (e.g., masking, work from home), which is not necessary for this study. Isolating 40% of the population was sufficient to reduce the first influenza epidemic to levels similar to those identified in the 2020–2021 influenza season (Appendix Section 7, available online, Model Validation Results). In 2-year simulations using the reduced interaction model, reductions were applied only in the first season. Additional simulations used a 40% reduction in the first season and lower levels of isolation (10% and 20%) in the second season.
To estimate the impact of increased vaccination, 1-year simulations with previous immunity were run with vaccination uptake by age group as reported by CDC and with 10% and 20% increases. Influenza vaccination levels as reported by CDC from 2010 to 2020 have increased by levels in the 10%–20% range.31
To orient the results to specific subtype/lineage scenarios in the modeled first and second influenza seasons, the level of reduction in susceptibility to infection by a subtype/lineage of influenza conferred by infection with the same or different subtype/lineage was estimated on the basis of discussions with experts in virology, influenza, and vaccination (Table 1). Support for expert opinion was identified in the literature.32 , 33 These estimates represent the ranges of possible strain cross-immunity.
Table 1.
Theoretical Percent Cross-Immunity Between Influenza Subtypes/Lineages
| Influenza subtype/lineage | Immunity to reinfection within the current year |
Immunity to infection after 1-year waninga |
||||||
|---|---|---|---|---|---|---|---|---|
| H1N1 | H3N2 | BYam | BVic | H1N1 | H3N2 | BYam | BVic | |
| H1N1 | 0.85‒1.0 | 0 | 0 | 0 | 0.49‒0.64 | 0 | 0 | 0 |
| H3N2 | 0 | 0.65‒1.0 | 0 | 0 | 0 | 0.29‒0.64 | 0 | 0 |
| BYam | 0 | 0 | 0.90‒1.0 | 0.40‒0.60 | 0 | 0 | 0.54‒0.64 | 0.04‒0.24 |
| BVic | 0 | 0 | 0.40‒0.60 | 0.90‒1.0 | 0 | 0 | 0.04‒0.24 | 0.54‒0.64 |
Waning is modeled at 3% per month, 36% between seasons.
The University of Pittsburgh IRB determined that this study was not human subject research. It was therefore an exempt study design.
RESULTS
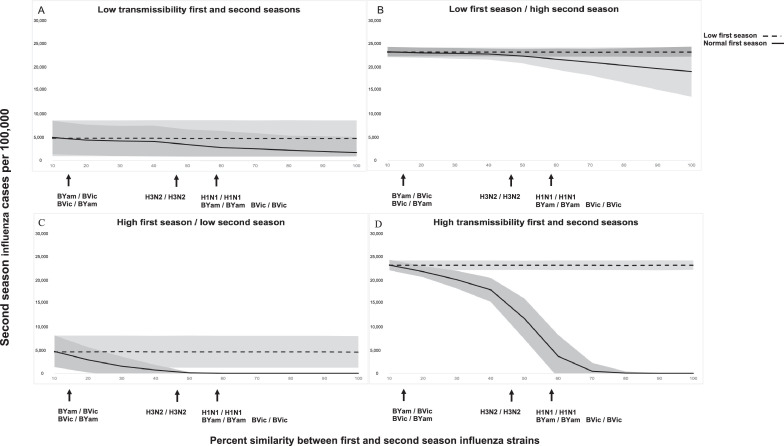
Model validation results are included in Appendix Section 7 (available online). In a 2-strain, 2-season model, normal first-season cases prevented second-season influenza cases and hospitalizations in all 4 transmissibility scenarios. A low first season would cause second-season case increases equal to the reductions caused by a normal first season. The impact varied by the transmissibility of the first- and second-year strains and by the similarity (cross-immunity) between those strains (Figure 2 and Appendix Table 4, available online). After waning, highly similar strains might have approximately 50%–60% cross-immunity (Table 1 ). Using 50% cross-immunity, if both season strains had lower transmissibility, the difference between second-season cases after a normal first season and a low first season was 26.29% (29.99% hospitalizations) (Figure 2A). A lower transmissibility strain in the first season had less impact on second-season cases when the second-season strain was more transmissible (difference of 3.83% cases and 4.31% hospitalizations) (Figure 2B). When the first-season strain had greater transmissibility than the second-season strain, there was a difference of 97.72% in cases (96.98% hospitalizations) (Figure 2C). When both the first-season and second-season strains were more transmissible, case difference in the second season was 49.47% for cases (56.81% hospitalizations) (Figure 2D). Higher transmissibility strains in the first season cause higher case numbers, contributing more to second-season immunity. When this immunity is removed, there is a larger increase in the second season. In the low transmissibility scenarios, Re is approximately 1 in a model with previous immunity and vaccination; therefore, a greater impact of an intervention is not unexpected.
Figure 2.
Influence of cross-immunity between annual strains on second season influenza cases.
Note: Second-season cases per 100,000 are depicted by the burden of the first season (low versus normal) and by the amount of viral transmissibility (low versus high). x-axis is % cross-immunity between first- and second-year strains; y-axis is mean second season cases per 100,000. The shaded area represents 95% CIs of model results. Arrows indicate likely cross-immunity values for first-season/second-season strain pairs. For example, H1N1/H1N1 means that the first season and second season strains are both H1N1. The dashed line is second-season cases after a low first season. The solid line is second-season cases after a normal first season. The difference between dashed and solid lines indicates an increase in second-season cases when first-season cases are very low.
When agent interactions were reduced in the second season as well as in the first season (40% reduction first season), cases were reduced in the second season. Reduction of interactions by 20% in the second season resulted in a 98.6% reduction in cases (95% CI=98.5, 98.7) for the low transmissibility scenario and 85.3% reduction (95% CI=84.8, 85.8) for the high transmissibility scenario. Reduction of interactions by 10% resulted in a 68.6% reduction in cases (95% CI=67.7, 69.4) for the low transmissibility scenario and 32.1% reduction (95% CI=30.4, 33.9) for the high transmissibility scenario.
Increasing vaccination rates above those reported by CDC by 10% and 20% decreased the number of cases and hospitalizations in a single-season simulation. Increased vaccination rates had a greater impact on simulations with a lower transmissibility strain (10% increase in vaccination caused a 31.5% decrease in cases and 32.9% decrease in hospitalizations; 20% increase in vaccination caused a 45.5% decrease in cases and 47.4% decrease in hospitalizations). For simulations with a more transmissible strain, increased vaccination resulted in a more modest effect (10% increase in vaccination caused a 2.3% decrease in cases and 3.3% decrease in hospitalizations; 20% increase in vaccination caused a 5.0% decrease in cases and 8.5% decrease in hospitalizations). In the low transmissibility scenario, increased vaccination rates may have a greater impact owing to vaccination levels reducing the reproduction number in that model to approximately 1 (Re=0.93, 95% CI=0.57, 1.30 in a model including previous immunity and vaccination at CDC-reported rates). Relatively low vaccination effectiveness in this model (40%) may decrease the impact of vaccination in a high transmissibility scenario. Single-year simulations include previous immunity, as described in Methods and Appendix (available online).
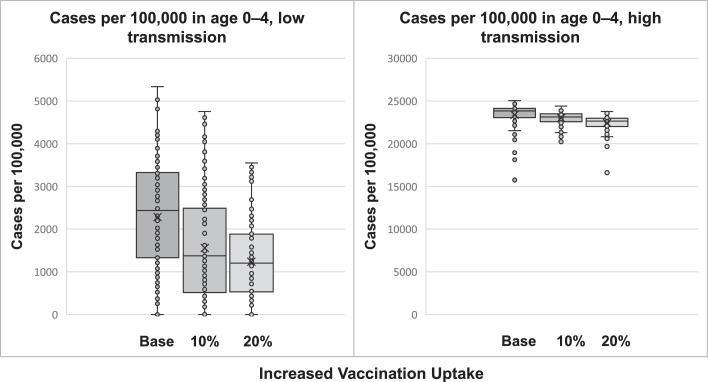
The age group 0–4 years comprised 5.2% of the simulation population and accounted for approximately 6% of cases in the simulation (5.8%–6.2% of cases). Increasing vaccination coverage by 10% decreased cases in this age group by 31.7% in the lower transmissibility scenario but only 1.7% in a higher transmissibility scenario (Figure 3 ). A 20% increase in vaccination coverage resulted in 45.7% fewer cases for a lower transmissibility strain but only 4.1% fewer cases for a more transmissible strain. Hospitalizations decreased by similar amounts (for the low transmissibility scenario, 33.7% decrease with 10% uptake increase and 49.0% with 20% increase; for the high transmissibility scenario, 3.1% decrease with 10% uptake increase and 5.4% decrease with 20% increase). Low Re may enhance the effects of vaccination in the low transmissibility scenarios.
Figure 3.
Change in total infections per 100,000 children aged 0‒4 years with an increase in vaccination coverage rate in a single season simulation.
Note: Base vaccination from reported rates. Coverage rates were increased by 10% and 20%. A proportion of agents had immunity at the start of the simulation to reflect immunity from previous-year infection, as described in Methods and Appendix (available online).
Applying model results specifically to influenza subtypes/lineages, the greatest impacts would be expected for seasons in which the current predominant strain was closely related to the previous-year strain, and cross-immunity is generally high between strains in succeeding years. A 40%–50% reduction in susceptibility could be expected for similar strains in succeeding years in cases where strains share subtype/lineage. Strain transmissibility would be expected to be similar in highly similar strains. The model estimated an increase of 13.52%–46.95% in cases and 15.43%–56.81% in hospitalizations in strains with the same transmissibility and 40%–50% cross-immunity (Appendix Table 4, available online). In the population used for simulation (Allegheny County, PA, synthetic population of 1,218,695) these values correspond to an increase of 8,225 (95% CI=2,241, 14,209) to 139,205 (95% CI=98,836, 179,575) cases and 31 (95% CI=10, 53) to 369 (95% CI=610, 982) hospitalizations over the influenza season. Cases numbers include asymptomatic cases, which make up 25% of those occurring in the model.
DISCUSSION
Agent-based modeling was used to predict the impact of a light influenza season on infection rates in the following season. Results indicate that a light first season (such as 2020–2021) could result in a large, compensatory second season (such as what might occur in 2021–2022). This increase could be as large as a doubling of cases. Enhanced vaccine coverage could reduce but not eliminate this predicted severe season. Continuation of interventions to reduce infectious contacts in the population could have a larger impact.
Influenza immunity is complex. Strains are highly variable, with genetic drift antigens contributing to emergence of new variants that escape immunity and enable yearly seasonal outbreaks with widely varying case rates despite population immunity and vaccination.34 Subtype switching of the predominant circulating strain is not consistently correlated with increases in infection rates.35
The northern hemisphere 2020–2021 season lacked the usual seasonal outbreak, likely because of COVID-19 interventions to reduce transmission. That outcome was beneficial because healthcare systems were already strained by the COVID-19 pandemic, but there is concern that the lack of residual immunity resulting from infection in 2020–2021 will cause a more severe influenza season in 2021–2022. Vaccination is an effective tool to prevent influenza, but vaccination rates are typically suboptimal, and vaccination does not confer complete immunity to infection.
An agent-based model of influenza was used to help in understanding the impact of a very low influenza season on the succeeding season. Reductions in interactions in a proportion of the population were sufficient to essentially eliminate influenza. Normal interaction levels in a second season caused an increase in second-season cases beyond what was predicted using the same model with no first-year reduction in interactions.
The model accounts for situations in which highly related and less related strains circulate in successive seasons. With a low level of cross-immunity, similar to an influenza A subtype switch, a low first season has limited impact on second-season cases. If there is a good antigenic match between seasons (high level of cross-immunity), the model predicts a large impact on second-season cases from first-season infections.
Increased vaccination could help offset the reduced population immunity resulting from the lack of influenza in 2020–2021. This could be particularly important for young children, who may be especially at risk in 2021–2022. Very few very young children had influenza in 2020–2021, so essentially all immunity in that age group would be from vaccination, which wanes relatively quickly.
Several factors suggest that although cases may increase after a very low first season, disease burden will not reach pandemic levels. The most prevalent influenza subtype often switches from one season to the next—for example, H1N1 predominated in the 2013–2014 season, whereas H3N2 predominated in the 2 preceding seasons— and these influenza subtype switches do not always cause increased intensity.36 Immunity owing to infection is believed to persist for 3–7 years, so substantial immunity can be expected to remain from previous seasons.8 Immunity from exposure to infection early in life is believed to confer a level of lifetime immunity to related strains, possibly including some immunity to conserved epitopes,37 and this could assist in limiting 2021–2022 influenza case rates.
Models are simplified representations of reality and therefore can never be perfect. Their intent is simply to provide useful and actionable information. The validity of a model is determined in part by how closely its design reflects reality and how accurately the parameters it uses are estimated. The FRED influenza model was designed to simulate pandemic influenza and has been used in previous studies to model influenza interventions, so model validity has been assessed in the past.21, 22, 23 The model now includes previous immunity in the first season and residual immunity from first-season infection in the second season and can be expanded to include an arbitrary number of seasons.
Limitations
Reliable and appropriate sources were used for parameter estimation; however, there are limitations on those estimates. Previous immunity is based on a CDC-modeled disease burden estimate,29 which may be affected by fluctuations in disease reporting because of a variety of factors. Vaccination efficacy is estimated from surveillance data and may be an overestimate or underestimate. The parameters for the waning of both natural and vaccine immunity are based on the literature and expert opinion. Cross-immunity between strains of influenza is most difficult to quantitate when the strains differ by antigenic drift only, and this is a major source of uncertainty. The model uses a range of values to account for this uncertainty. Parameter uncertainty can cause model results to be higher or lower than what would be encountered in reality.
Transmission in this model is caused by the interaction of agents, specifically the geographic proximity of infectious and susceptible agents, simulating respiratory transmission. There is no inclusion of fomites or other nonrespiratory modes of transmission. Rates of interaction between agents are age dependent and were calibrated to match data from influenza studies.21
This set of simulations was designed to address a specific problem concerning the possible impact of loss of immunity because of a low influenza season on the following season. It assumes that the second season will behave as a normal influenza season, having no additional interventions. Additional simulations were performed to assess the impact of possible continued interventions and pandemic-induced changes in behavior on transmission. Other circumstances may also impact the 2021–2022 season. Low levels of circulating influenza worldwide and in the Southern Hemisphere may limit the seasonal introduction of influenza to the U.S., thereby limiting the season. The low level of influenza circulation since March 2020 may have limited influenza evolution in the interim; however, the circulation of influenza in animal hosts also provides the potential for the development and introduction of novel strains. These additional scenarios have not been modeled specifically. Model results must be interpreted in the context of model design, uncertainty in model parameters, and limitations of modeling in general.
CONCLUSIONS
Given the light 2020–2021 influenza season, the 2021–2022 season may see increased case rates of up to 50%, depending on cross-immunity from past infection and transmissibility of strains. Enhanced vaccine coverage as well as continued interventions and behaviors that decrease population interactions could reduce this high season. Vaccination in the very young may be particularly important in 2021–2022, given the lack of immunity from previous infections in that age group.
Acknowledgments
ACKNOWLEDGMENTS
The authors would like to acknowledge Donald S. Burke, MD for valuable contributions to the development of this project. The authors would also like to thank John V. Williams, MD and Lee H. Harrison, MD for valuable discussion and comments.
The study sponsor had no role in study design; collection, analysis, or interpretation of data; writing of the report; or the decision to submit the report for publication.
This work was supported by the Center for Disease Control and Prevention U01-IP001141-01. The University of Pittsburgh IRB has determined that this study was not human subject research and is therefore an exempt study design.
A version of this study has been posted on the preprint server MedRxiv.
RKZ and JMR have research grant funding from Sanofi Pasteur on an unrelated vaccine topic. No other financial disclosures were reported.
CRediT AUTHOR STATEMENT
Mary G. Krauland: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Resources; Software; Validation; Visualization; Writing - original draft; Writing - review and editing. David D. Galloway: Data curation; Investigation; Methodology; Resources; Software; Writing - review and editing. Jonathan M. Raviotta: Data curation; Investigation; Validation; Writing - review and editing. Richard K. Zimmerman: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Validation; Writing - review and editing. Mark S. Roberts: Conceptualization; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Writing - review and editing.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2021.11.007.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.Adlhoch C, Mook P, Lamb F, et al. Very little influenza in the WHO European Region during the 2020/21 season, weeks 40 2020 to 8 2021. Euro Surveill. 2021;26(11) doi: 10.2807/1560-7917.ES.2021.26.11.2100221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children - a nationwide register study in Finland. EClinicalMedicine. 2021;34 doi: 10.1016/j.eclinm.2021.100807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee L, Butt K, Buckrell S, Nwosu A, Sevenhuysen C, Bancej C. National influenza mid-season report, 2020-2021. Can Commun Dis Rep. 2021;47(1):1–4. doi: 10.14745/ccdr.v47i01a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID-19 pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(37):1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Partridge E, McCleery E, Cheema R, et al. Evaluation of seasonal respiratory virus activity before and after the statewide COVID-19 shelter-in-place order in Northern California. JAMA Netw Open. 2021;4(1) doi: 10.1001/jamanetworkopen.2020.35281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.2020-2021 Flu Season Summary. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/season/faq-flu-season-2020-2021.htm. Updated October 25, 2021. Accessed January 3, 2022.
- 7.Ferdinands JM, Fry AM, Reynolds S, et al. Intraseason waning of influenza vaccine protection: evidence from the U.S. Influenza Vaccine Effectiveness Network, 2011-12 through 2014-15. Clin Infect Dis. 2017;64(5):544–550. doi: 10.1093/cid/ciw816. [DOI] [PubMed] [Google Scholar]
- 8.Ranjeva S, Subramanian R, Fang VJ, et al. Age-specific differences in the dynamics of protective immunity to influenza. Nat Commun. 2019;10(1):1660. doi: 10.1038/s41467-019-09652-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kermack WO, McKendrick AG. Contributions to the mathematical theory of epidemics–I. 1927. Bull Math Biol. 1991;53(1–2):33–55. doi: 10.1007/BF02464423. [DOI] [PubMed] [Google Scholar]
- 10.Bootsma MC, Ferguson NM. The effect of public health measures on the 1918 influenza pandemic in U.S. cities. Proc Natl Acad Sci U S A. 2007;104(18):7588–7593. doi: 10.1073/pnas.0611071104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chowell G, Ammon CE, Hengartner NW, Hyman JM. Transmission dynamics of the great influenza pandemic of 1918 in Geneva, Switzerland: assessing the effects of hypothetical interventions. J Theor Biol. 2006;241(2):193–204. doi: 10.1016/j.jtbi.2005.11.026. [DOI] [PubMed] [Google Scholar]
- 12.Chowell G, Miller MA, Viboud C. Seasonal influenza in the United States, France, and Australia: transmission and prospects for control. Epidemiol Infect. 2008;136(6):852–864. doi: 10.1017/S0950268807009144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dushoff J, Plotkin JB, Levin SA, Earn DJ. Dynamical resonance can account for seasonality of influenza epidemics. Proc Natl Acad Sci USA. 2004;101(48):16915–16916. doi: 10.1073/pnas.0407293101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferguson NM, Cummings DA, Fraser C, Cajka JC, Cooley PC, Burke DS. Strategies for mitigating an influenza pandemic. Nature. 2006;442(7101):448–452. doi: 10.1038/nature04795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mills CE, Robins JM, Lipsitch M. Transmissibility of 1918 pandemic influenza. Nature. 2004;432(7019):904–906. doi: 10.1038/nature03063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DePasse JV, Nowalk MP, Smith KJ, et al. Does cost-effectiveness of influenza vaccine choice vary across the U.S.? An agent-based modeling study. Vaccine. 2017;35(32):3974–3981. doi: 10.1016/j.vaccine.2017.05.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guo D, Li KC, Peters TR, Snively BM, Poehling KA, Zhou X. Multi-scale modeling for the transmission of influenza and the evaluation of interventions toward it. Sci Rep. 2015;5:8980. doi: 10.1038/srep08980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.O'Neil CA, Sattenspiel L. Agent-based modeling of the spread of the 1918-1919 flu in three Canadian fur trading communities. Am J Hum Biol. 2010;22(6):757–767. doi: 10.1002/ajhb.21077. [DOI] [PubMed] [Google Scholar]
- 19.Whitman J, Jayaprakash C. Stochastic modeling of influenza spread dynamics with recurrences. PLoS One. 2020;15(4) doi: 10.1371/journal.pone.0231521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Halloran ME, Ferguson NM, Eubank S, et al. Modeling targeted layered containment of an influenza pandemic in the United States. Proc Natl Acad Sci U S A. 2008;105(12):4639–4644. doi: 10.1073/pnas.0706849105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grefenstette JJ, Brown ST, Rosenfeld R, et al. FRED (a Framework for Reconstructing Epidemic Dynamics): an open-source software system for modeling infectious diseases and control strategies using census-based populations. BMC Public Health. 2013;13:940. doi: 10.1186/1471-2458-13-940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kumar S, Grefenstette JJ, Galloway D, Albert SM, Burke DS. Policies to reduce influenza in the workplace: impact assessments using an agent-based model. Am J Public Health. 2013;103(8):1406–1411. doi: 10.2105/AJPH.2013.301269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumar S, Piper K, Galloway DD, Hadler JL, Grefenstette JJ. Is population structure sufficient to generate area-level inequalities in influenza rates? An examination using agent-based models. BMC Public Health. 2015;15:947. doi: 10.1186/s12889-015-2284-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chu KH, Shensa A, Colditz JB, et al. Integrating social dynamics into modeling cigarette and e-cigarette use. Health Educ Behav. 2020;47(2):191–201. doi: 10.1177/1090198119876242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu F, Enanoria WT, Zipprich J, et al. The role of vaccination coverage, individual behaviors, and the public health response in the control of measles epidemics: an agent-based simulation for California. BMC Public Health. 2015;15:447. doi: 10.1186/s12889-015-1766-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Influenza. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/fastats/flu.htm. Updated August 3, 2021. Accessed August 9, 2021.
- 27.U.S. flu VE data for 2019-20. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/vaccines-work/2019-2020.html. Updated December 22, 2020. Accessed May 20, 2021.
- 28.Past seasons vaccine effectiveness estimates. Centers for Disease Control and Prevention. https://www.cdc.gov/flu/vaccines-work/past-seasons-estimates.html. Updated January 29, 2020. Accessed August 9, 2021.
- 29.Centers for Disease Control and Prevention; 2021. Estimated influenza illnesses, medical visits, hospitalizations, and deaths in the United States - 2019–2020 flu Season. https://www.cdc.gov/flu/about/burden/2019-2020.html. Updated June 2, 2021. Accessed August 11, 2021. [Google Scholar]
- 30.Ferdinands JM, Alyanak E, Reed C, Fry AM. Waning of influenza vaccine protection: exploring the trade-offs of changes in vaccination timing among older adults. Clin Infect Dis. 2020;70(8):1550–1559. doi: 10.1093/cid/ciz452. [DOI] [PubMed] [Google Scholar]
- 31.Flu vaccination coverage . Centers for Disease Control and Prevention; 2020. United States, 2019–20 influenza season.https://www.cdc.gov/flu/fluvaxview/coverage-1920estimates.htm Updated October 1Accessed August 13, 2021. [Google Scholar]
- 32.Carlock MA, Ingram JG, Clutter EF, et al. Impact of age and pre-existing immunity on the induction of human antibody responses against influenza B viruses. Hum Vaccin Immunother. 2019;15(9):2030–2043. doi: 10.1080/21645515.2019.1642056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nuñez IA, Carlock MA, Allen JD, et al. Impact of age and pre-existing influenza immune responses in humans receiving split inactivated influenza vaccine on the induction of the breadth of antibodies to influenza A strains. PLoS One. 2017;12(11) doi: 10.1371/journal.pone.0185666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention; 2020. Past seasons estimated influenza disease burden.https://www.cdc.gov/flu/about/burden/past-seasons.html Updated October 1Accessed August 9, 2021. [Google Scholar]
- 35.Biggerstaff M, Kniss K, Jernigan DB, et al. Systematic assessment of multiple routine and near real-time indicators to classify the severity of influenza seasons and pandemics in the United States, 2003-2004 through 2015-2016. Am J Epidemiol. 2018;187(5):1040–1050. doi: 10.1093/aje/kwx334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention; 2018. How CDC classifies flu severity.https://www.cdc.gov/flu/about/classifies-flu-severity.htm Updated September 14Accessed July 21, 2021. [Google Scholar]
- 37.Arevalo CP, Le Sage V, Bolton MJ, et al. Original antigenic sin priming of influenza virus hemagglutinin stalk antibodies. Proc Natl Acad Sci U S A. 2020;117(29):17221–17227. doi: 10.1073/pnas.1920321117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.