Abstract
Background
Little is known about the longer-term impact of the Covid-19 pandemic beyond the first months of 2020, particularly for people with pre-existing mental health disorders. Studies including pre-pandemic data from large psychiatric cohorts are scarce.
Methods
Between April 2020 and February 2021, twelve successive online questionnaires were distributed among participants of the Netherlands Study of Depression and Anxiety, Netherlands Study of Depression in Older Persons, and Netherlands Obsessive Compulsive Disorder Association Study (N = 1714, response rate 62%). Outcomes were depressive symptoms, anxiety, worry, loneliness, perceived mental health impact of the pandemic, fear of Covid-19, positive coping, and happiness. Using linear mixed models we compared trajectories between subgroups with different pre-pandemic chronicity of disorders and healthy controls.
Results
Depressive, anxiety and worry symptoms were stable since April–May 2020 whereas happiness slightly decreased. Furthermore, positive coping steadily decreased and loneliness increased - exceeding pre-Covid and April–May 2020 levels. Perceived mental health impact and fear of Covid-19 fluctuated in accordance with national Covid-19 mortality rate changes. Absolute levels of all outcomes were poorer with higher chronicity of disorders, yet trajectories did not differ among subgroups.
Limitations
The most vulnerable psychiatric groups may have been underrepresented and results may not be generalizable to lower income countries.
Conclusions
After a year, levels of depressive and worry symptoms remained higher than before the pandemic in healthy control groups, yet not in psychiatric groups. Nevertheless, persistent high symptoms in psychiatric groups and increasing loneliness in all groups are specific points of concern for mental health care professionals.
Keywords: Affective disorder, Coronavirus, Epidemiology, Chronicity
1. Introduction
It has been over a year since the WHO declared the Covid-19 outbreak a pandemic, with about 300 million confirmed cases and 5,5 million deaths worldwide as of January 2022 (WHO, 2022). The impact of this crisis on mental health is a major concern, and collecting high-quality data to monitor longer-term developments and prepare for longer-term consequences for mental health has been deemed an immediate priority (Holmes et al., 2020; Marazziti and Stahl, 2020). In the general population, many cross-sectional studies reported a high prevalence of depression and anxiety in the initial phase of the pandemic (Bueno-Notivol et al., 2021; Xiong et al., 2020). However, longitudinal studies often found no or little change in symptoms of depression and anxiety compared to pre-pandemic levels (Connor et al., 2020; Wang et al., 2020), or observed that an initial increase in depressive and anxiety symptoms quickly waned off after the first wave of infections and deaths abated (Fancourt et al., 2021; Pierce et al., 2021), at least for the majority of the participants. A review based on 25 studies assessing psychological functioning before and after Covid-19 lockdowns in general population samples published between January and June 2020 (pooled n = 72,004) concluded that the psychological impact of the Covid-19 lockdowns was small on average, and suggested that most people were resilient during the first months of the pandemic (Prati and Mancini, 2021). Nevertheless, people with (pre-existing) psychopathology have been indicated as a group at particular risk for detrimental mental health effects of the pandemic (Holmes et al., 2020; Hotopf et al., 2020; Morgan and Rose, 2020; Pfefferbaum and North, 2020; Wang et al., 2021). Yet the few large-scale studies that included pre-pandemic data, including ours (Pan et al., 2021), found that groups with the highest mental health disorder burden showed no change or even a slight decrease in depressive, anxiety and worry symptoms and loneliness (Pan et al., 2021; Tsamakis et al., 2021). This slight decrease might be attributable to some sense of relaxation and shared cohesiveness in a world in lockdown (Mancini, 2020), although the overall levels of symptoms and the perceived impact of the pandemic on mental health were on average still much higher in people with compared to people without mental disorders (Pan et al., 2021; Pierce et al., 2021; Tsamakis et al., 2021).
Previous studies were based on the first wave of the pandemic. Since then, many countries have faced new and devastating waves of Covid-19-infections accompanied by comprehensive measures and lockdowns leading to a dramatic and long-lasting economic and societal burden (Chowdhury et al., 2021; Jackson et al., 2021). In the Netherlands, like in many other European countries, the spread of Covid-19 appeared to be under control after the first national lockdown in the spring of 2020, and the daily number of new Covid-19 infections during summer was minimal. However, in the fall of 2020 there was a new surge in Covid-19 infections, resulting in new lockdowns late 2020, including nighttime curfews in several countries. The duration of restrictions has been extended multiple times in light of a potential third wave of infections due to more transmissible Covid-19 variants. Although the initial mental health impact of the first Covid-19 wave may have been limited, the impact of subsequent waves may well be more pronounced for several reasons. The chronicity and comprehensiveness of the social restrictions may have brought along prolonged social isolation, physical distancing, fear, boredom, interrupted work and/or education, more severe economic consequences (e.g., reduced income) and discontent. These factors may have caused an upsurge in mental health problems and loneliness. This could be more problematic for persons with (pre-existing) mental disorders as they may have less psychological and social resources to prevent (further) mental health deterioration in the longer run. Also, mental health treatment services may have been discontinued or delivered less timely and effectively. In contrast, the recently commenced Covid-19 vaccination campaign may have brought a sense of hope and prospects of the end of the pandemic. To date, there are no longitudinal studies that have been able to map out how mental health in persons with and without mental health disorders has responded over the longer term, after the initial reaction to the Covid-19 pandemic relative to pre-Covid levels. Therefore, our objective was to examine changes in the perceived mental health impact, fear of Covid-19, positive coping, happiness and symptoms of depression, anxiety, worry, and loneliness in three ongoing cohorts of people with and without mental health disorders in the Netherlands from April 2020 to February 2021, including pre-pandemic data from the same participants.
2. Methods
2.1. Participants
We recruited participants from three Dutch prospective cohort studies with largely identical pre-pandemic data: the Netherlands Study of Depression and Anxiety (NESDA (Penninx et al., 2008)), The Netherlands Study of Depression in Older Persons (NESDO (Comijs et al., 2011)) and Netherlands Obsessive Compulsive Disorder Association Study (NOCDA (Schuurmans et al., 2012)).
NESDA includes individuals with a depressive or anxiety disorder (n = 2329), their biological siblings (n = 367), and controls without mental health disorder (n = 652). Participants were aged between 18 and 65 years at baseline in 2004–2007, and recruited from specialized mental health care, primary care (based on a random sample from 65 General Practitioners (GPs) across three regions), and the community (based on two pre-existing cohort studies). Controls were mainly recruited from the same primary care settings as the cases (for more details see Penninx et al., 2008). Follow-up measurements took place in 2008–11, 2010–13, and 2014–16.
NESDO includes individuals with a primary diagnosis of depressive disorder (n = 378) aged 60–93 years at baseline in 2007–10, recruited from out- and inpatient mental health care and 14 GPs across three regions. Non-depressed controls without lifetime diagnoses of mental health disorders were recruited from the same 14 GPs (n = 132). Follow-up measurements took place in 2008–12 and 2012–16.
NOCDA includes individuals with a lifetime diagnosis of obsessive-compulsive disorder (n = 419), aged 18–65 years at baseline in 2004–2009, recruited from seven mental health-care institutions across the Netherlands. Follow-up measurements took place in 2006–11, 2008–13, and 2012–16.
Participants from these cohorts who gave permission to be contacted for further research activities (n = 2748) were invited via e-mail from April 1, 2020 onwards to participate in a repeated online questionnaire on the mental health impact of the Covid-19 pandemic, i.e. the “Covid-19 questionnaire”. Online informed consent was obtained from 55all participants. Participants received no incentives for participation in the study. We used data from twelve measurement waves conducted between April 12,020 and February 22, 2021, held two to eight weeks apart.
All study procedures were approved by the Institutional Review Board of the Vrije Universiteit Medical Center, Amsterdam (reference number 2020.166). The online questionnaire was built in Survalyzer, 3000 edition.
2.2. Measures
2.2.1. Mental health outcomes
Three validated symptom severity scales were included in pre-pandemic waves and the Covid-19 questionnaires. For depressive symptoms we used the 16-item Quick Inventory of Depressive Symptoms (QIDS (Rush et al., 2003)); for anxiety symptoms the 21-item Beck Anxiety Inventory (BAI (Aaron T. Beck et al., 1988)); for worry the 11-item Penn State Worry Questionnaire (PSWQ (Meyer, 1990)). Additionally, we included loneliness, based on the six-item De Jong Gierveld Loneliness Scale (De Jong Q; de Jong-Gierveld and Kamphuis, 1985). Additionally, happiness was based on a single question asking how happy or unhappy participants were with their life. Answer options ranged from 1 (completely unhappy) to 7 (completely happy). For descriptive purposes, we included pre-pandemic levels of these five outcomes, by computing the mean of available waves between 2006 and 2016, as done previously (Pan et al., 2021). As pre-pandemic happiness was not available in NESDO and NOCDA, the pre-pandemic level was based on NESDA-participants only.
The Covid-19 questionnaires also included three Covid-specific measures, based on 20 items about participants' perceptions of the consequences of the pandemic, answered on a five-point Likert scale (1-completely disagree to 5-completely agree). Using exploratory factor analysis, we previously derived three dimensions from these items (for details see Pan et al., 2021), which we again include in the present study. Perceived mental health impact had 9 items (e.g. “In this period I feel more emotional”; Cronbach's α = 0.84–0.89 across measurements). Higher scores indicate a more detrimental perceived mental health impact. Fear of Covid-19 was had 6 items (e.g., “I fear to become infected with Covid-19”; Cronbach's α = 0.71–0.78). Higher scores indicate more fear of Covid-19. Positive coping had 5 items (e.g., “I actively maintain contacts with friends via phone or online”; Cronbach's α = 0.59–0.66). Higher scores indicate more positive coping with the Covid-19 pandemic.
2.2.2. Mental health disorder burden
In previous work (Pan et al., 2021) we found that the chronicity of disorders based on pre-pandemic data was strongly predictive of mental health levels and changes in the initial month of the pandemic, whereas type of disorder was not. Therefore, we used Chronicity of disorders as indicator of mental health disorder burden. We calculated the percentage of waves between 2006 and 2016 at which participants had a current (6-month recency) diagnosed mental health disorder. We included only the waves from 2006 onwards to harmonize the baseline year among the three cohorts. Chronicity was categorized into: No Lifetime Disorder (i.e. ‘healthy controls’); Remitted Disorder (applying to NOCDA and NESDA participants who had mental disorder(s) at baseline that persistently remitted at the remaining measurements); Low-medium Chronicity (1–50% of previous waves with disorders); and High Chronicity (51–100% of previous waves with disorders). Disorders included major depressive disorder, dysthymia, general anxiety disorder, panic disorder, social phobia, and agoraphobia for all three cohorts, and additionally obsessive-compulsive disorder in NOCDA. In NESDA and NESDO, diagnoses were based on the Composite Interview Diagnostic Interview (CIDI (Wittchen, 1994)), using DSM-IV criteria. In NOCDA, diagnoses were based on the Structured Clinical Interview for DSM-IV axis-I disorders (SCID (First et al., 1996)).
2.2.3. Covariates
We included age, gender (based on biological sex: female, male) and education (basic [elementary school], intermediate [lower vocational to general secondary education], and high [college or university]) as covariates in all analyses. For descriptive purposes, from the Covid-19 questionnaires we included whether participants or a household member had been diagnosed with Covid-19 and whether a close contact had died from Covid-19. The latter question was included from the 8th wave (October 2020) onwards. Furthermore, we asked whether participants were currently in treatment for mental health problems, were not in treatment but felt a need for treatment, or neither of these. Variables expressed whether participants reported these situations at least once.
2.3. Statistical analysis
Characteristics and outcomes were summarized as means with standard deviations (SD) for continuous variables, and as proportions for categorical variables. In order to assess average trajectories in QIDS, BAI, PSWQ, Loneliness, Happiness, Perceived mental health impact, Fear of Covid-19 and Positive coping, we estimated marginal mean scores at each wave using linear mixed models, with a random intercept for participants and adjusting for age, gender and education level. We used wave number as a categorical variable to examine absolute and relative changes in outcomes between each Covid-19 measurement and the Covid-19 baseline (April 1, 2020). Relative change was based on z-standardized values with Covid-19 baseline as reference. To examine statistical significance of differences in outcome trajectories between groups with different chronicity of disorders, we tested whether the change between one wave to the next differed between these subgroups using Chi-square tests. Furthermore, in our previous work focusing on the first month of the pandemic we found that compared to pre-pandemic levels, depressive symptoms and loneliness increased in the control group and depressive symptoms decreased somewhat only in the group with high chronicity of pre-pandemic disorders. Other groups remained stable (Pan et al., 2021). To extend this previous analysis, we tested whether mental health at each of the twelve Covid-19 measurements significantly differed from the pre-pandemic level, stratified for each chronicity of disorders subgroup and healthy controls. Missing data was handled by Full Information Maximum Likelihood estimation.
We performed descriptive analyses in SPSS (v26), and mixed model analyses in R (v3.6.0), packages ‘lme4’ (v1.1–26) and ‘emmeans’ (v1.5.4). Given the larger chance of type I errors with our relatively high number of outcomes, we considered p-values <.01 as statistically significant.
2.4. Sensitivity analyses
We conducted two sensitivity analyses. First, to consider potential bias by including participants who participated in few Covid-19 measurements, we repeated analyses in those who provided data on at least five measurements. Second, we repeated analyses in those who were not explicitly exposed to Covid-19, i.e. who had not been infected, nor had household members being infected, nor had a close contact who died from Covid-19.
3. Results
3.1. Attrition and response rates
There were n = 2748 persons who participated in the last pre-Covid waves of the three cohort studies and indicated they could be approached for new data collections. This is 64.7% of the total baseline participants (NESDA: 69.7%; NESDO: 22.7% (largely due to high mortality rates); NOCDA: 71.6%). For NESDA, the percentage of eligible controls was about 10% lower than for cases, whereas in NESDO, this percentage was about 20% higher. Of the n = 2748 we included 1714 participants with data on all mental health outcomes for at least one wave (overall response rate 62.4%; NESDA: 64%; NESDO: 67.2%; NOCDA: 48%, p = .02). The response rates did not differ between cases and controls.
Within the group eligible for the Covid-study, the 1714 respondents were older (43 versus 40.5 years, p < .001) and more likely to be high educated than non-responders (42% versus 38%, p < .001). We found no significant differences in sex (p = .68) and the chronicity of disorders (p = .054).
Within the total cohorts, the 1714 participants were on average younger than all non-participants combined (43 versus 47 years, p < .001), more likely to be high educated (42% versus 31%, p < .001) and less likely to have a history of psychopathology (76% versus 80%, p = .002). These groups did not differ in sex (p = .92).
In the included sample, the median number of Covid-measurements participated was 5 (IQR 2–10); 16.7% (n = 286) participated only once; 7.4% (n = 126) participated at all waves. This number did not significantly differ between cases and controls.
3.2. Descriptive statistics
Of the 1714 included participants, n = 428 had Remitted Disorders across 2006–2016, n = 444 had Low-medium Chronicity of disorders, n = 464 had High Chronicity, and n = 378 were persons without lifetime disorders (Table 1 ). Participants with higher chronicity of mental health disorders were on average younger, more likely to be female and lower educated, and more likely to indicate that they were in mental health treatment or felt a need for treatment. We found no significant subgroup differences in the number of waves participated, the percentage being diagnosed with Covid-19, having a household member diagnosed with Covid-19 or knowing a close contact who died from Covid-19. Over 60% of participants with Low-medium chronicity and High chronicity had a six-month MDD diagnosis at one or more pre-Covid measurements. The prevalence of OCD was lowest of the included types of disorders, namely 4.7% (n = 21) in the Low-medium chronicity and 21.6% (n = 100) in the High chronicity subgroups.
Table 1.
Included participants' characteristics (n = 1714) by chronicity of mental health disorders.
| n | Chronicity of mental health disordersa |
p valueb | ||||
|---|---|---|---|---|---|---|
| No lifetime disorder n = 378 |
Remitted disorder(s) n = 428 |
Low-medium chronicity n = 444 |
High chronicity n = 464 |
|||
| m/% (SD) | m/% (SD) | m/% (SD) | m/% (SD) | |||
| Pre-Covid characteristics | ||||||
| Age in April 2020 (Years) | 1714 | 58.2 (14.5) | 55.9 (13.0) | 56.4 (13.0) | 55.1 (12.5) | 0.0078 |
| Gender (Woman) | 1714 | 55.0 | 65.9 | 68.7 | 65.5 | <0.0001 |
| Education | 1710 | |||||
| Basic | 55 | 2.1 | 3.1 | 2.9 | 4.5 | |
| Intermediate | 943 | 47.2 | 56.7 | 55.9 | 59.5 | |
| High | 712 | 50.7 | 40.2 | 41.2 | 36.0 | 0.0016 |
| Source study | 1714 | |||||
| NESDA | 1492 | 90.7 | 95.1 | 90.8 | 73.1 | |
| NESDO | 78 | 9.3 | 0.0 | 4.1 | 5.4 | |
| NOCDA | 144 | 0.0 | 4.9 | 5.2 | 21.6 | |
| Type of current (6-month) disorders present since 2006d | ||||||
| Major Depressive Disorder | 1714 | .. | .. | 61.0 | 66.8 | |
| Dysthymia | 1714 | .. | .. | 15.5 | 32.5 | |
| Generalized Anxiety Disorder | 1714 | .. | .. | 18.9 | 33.8 | |
| Panic Disorder | 1714 | .. | .. | 21.6 | 44.2 | |
| Social Phobia | 1714 | .. | .. | 26.4 | 51.5 | |
| Obsessive-Compulsive Disorder | 1714 | .. | .. | 4.7 | 21.6 | |
| Characteristics during Covid follow-up | ||||||
| Number of waves participatedc | 1714 | 6 (3−10) | 5 (2–9) | 6 (2−10) | 5 (2–9) | 0.096 |
| Covid-19 diagnosis participant | 1687 | 4.8 | 6.0 | 4.1 | 4.2 | 0.55 |
| Covid-19 diagnosis household member | 1697 | 31.4 | 33.3 | 34.7 | 39.9 | 0.055 |
| Close contact died from Covid-19 | 1228 | 5.0 | 9.9 | 7.8 | 9.6 | 0.12 |
| Mental health treatment | 1612 | |||||
| Yes, currently | 940 | 6.7 | 27.2 | 45.2 | 68.8 | |
| No, but felt need for treatment | 53 | 1.4 | 3.2 | 4.3 | 4.0 | |
| No, and did not feel need | 619 | 91.9 | 69.6 | 50.6 | 27.3 | <0.0001 |
Percentage of previous waves since 2006 with ‘current’ (6-month) mental disorders.
F-test, Chi-square test or Mood's median test as appropriate.
Median (25th percentile – 75th percentile).
Obsessive-Compulsive Disorder only ascertained in NOCDA.
3.3. Average changes in outcomes over time
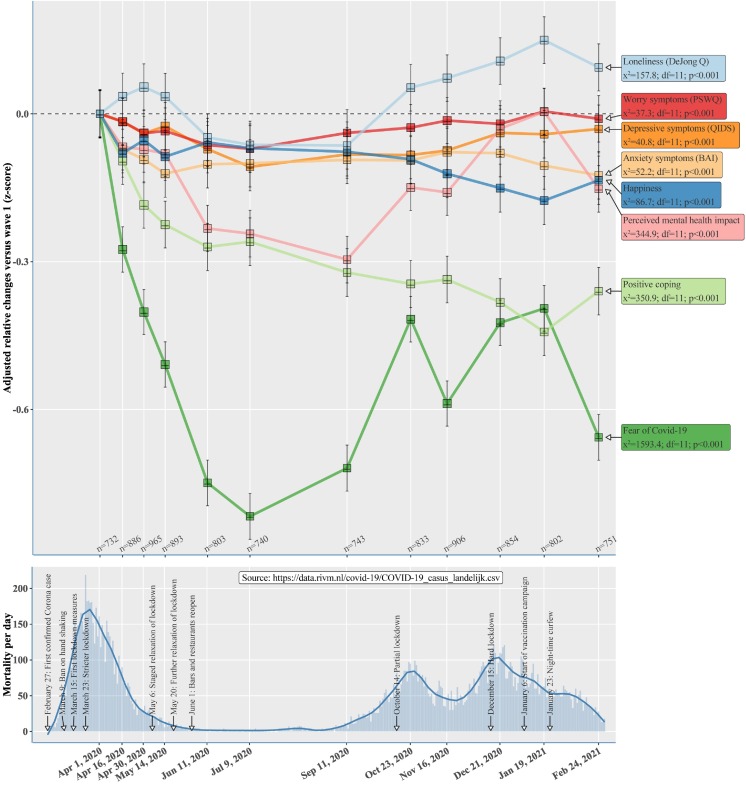
The upper panel of Fig. 1 shows average relative differences in mental health outcomes at each measurement compared to the Covid-19 baseline in April 2020. The lower panel shows national Covid-19 mortality per day across the same observation period, and indicates key transitions such as lockdowns, alleviations of measures and the start of Covid-19 vaccinations in the Netherlands. The mean change in all outcomes was statistically significant, yet there were substantial differences in the change patterns between outcomes.
Fig. 1.
Upper panel: average relative changes in eight mental health outcomes across 12 Covid-assessments compared to the first assessment, in n = 1714 participants who participated in at least one Covid-assessment. Data are marginal means obtained from mixed models with random intercepts, adjusted for age, gender and level of education. The box sizes are proportional to the number of participants during each wave, ranging from n = 732 through n = 965. Error bars represent standard errors. Lower panel: daily number of Covid-19 deaths during the pandemic in the Netherlands, with a sliding mean in dark blue. Key dates with regard to Covid-19 and its Dutch (lockdown) measures are given. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Depressive and worry symptoms only slightly decreased until July 2020 and then gradually increased to the initial level, while anxiety symptoms and happiness gradually decreased and ended at about only 0.2 SD below the initial level. Still, in contrast to loneliness and the COVID-specific measures (overall χ2-values between 158 and 1593), these outcomes were relatively stable over time (χ2-values between 37 and 87). Specifically, after some fluctuation since the Covid-baseline, loneliness steadily increased after summer 2020, when new lockdowns came into effect, exceeding Covid-baseline levels. The perceived mental health impact of Covid-19 initially sharply decreased until the end of summer 2020, meaning that participants perceived a less detrimental mental health burden in summer than in the initial month of the pandemic. However, it then increased again to initial levels in January 2021. Fear of Covid-19 decreased and increased in accordance with national rates of Covid-19 mortality rates, yet stayed well below the initial level. The extent to which participants perceived they could cope in a positive way with the pandemic gradually declined throughout the entire period, ending at about −0.4 SD. However, between the January and February 2021 measurements this somewhat increased again. Similarly, perceived mental health impact and loneliness somewhat decreased. For more detailed descriptive statistics of each wave see Supplementary Table 1.
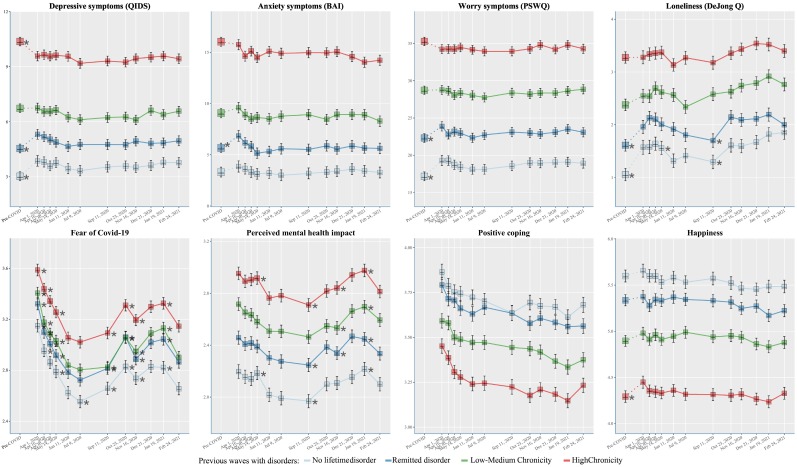
3.4. Differences between chronicity of disorders subgroups
Although groups with higher chronicity of disorders reported worse absolute mean levels for every outcome, the patterns of change over time relative to the COVID-baseline were very similar across subgroups (Fig. 2 ; see Supplementary Fig. 1 for relative changes). Changes in-between two subsequent time points differed significantly differed between subgroups for only two out of 88 comparisons (2.3%). Furthermore, we found that in groups with High Chronicity of disorders, depressive, anxiety and worry symptoms were slightly yet persistently lower during the pandemic than pre-Covid (see Supplementary Fig. 4). In the later measurement waves, loneliness was higher and happiness somewhat lower. In contrast, in persons without lifetime disorders, depressive and worry symptoms and loneliness were persistently higher during-Covid than pre-Covid. In groups with Remitted disorders and 1–50% chronicity of disorders, loneliness was higher at almost all Covid-measurements than pre-Covid.
Fig. 2.
Changes according to the four groups of chronicity of psychiatric disorders. Marginal mean levels obtained with mixed models are shown during the 12 Covid-assessment in eight mental health outcomes, in n = 1714 participants who participated in at least one Covid-assessment. For the QIDS, BAI, PSWQ, Happiness, and Loneliness, the mean values before the Covid-19 pandemic (years 2006–2016) are provided and connected with dotted lines. Data are adjusted for age, gender and level of education. The box sizes are proportional to the number of participants during each wave. Error bars represent standard errors. Asterisks indicate a statistically significant change from one wave to the subsequent one (p < .01).
3.5. Sensitivity analyses
Compared to findings in the complete study sample (n = 1714), findings were similar when analyses were restricted to participants with at least five waves of data (n = 925; Supplementary Fig. 2), and when restricted to participants not explicitly exposed to Covid-19 (n = 1030; Supplementary Fig. 3).
4. Discussion
In this study we examined changes in eight mental health outcomes during the initial year of the Covid-19 pandemic in three Dutch cohorts of persons with and without depressive, anxiety and obsessive compulsive disorders. We found that patterns of change over time differed among outcomes: whereas depressive, anxiety and worry symptoms were remarkably stable over time, the perceived mental health impact and fear of Covid-19 substantially fluctuated in concordance with decreases and increases in Covid-19 mortality and social restrictions. At the same time, participants' self-perceived ability to positively cope with the situation steadily declined since the start of the pandemic, and loneliness increased since autumn 2020, exceeding levels observed in April 2020. We found that absolute levels of all outcomes were substantially poorer in participants with higher burden of mental disorders, yet, the relative changes in these outcomes over time did not differ between persons without lifetime mental disorders or patients with different chronicity levels. Furthermore, our earlier observation that in the initial two months of the pandemic, symptoms and levels of loneliness were elevated specifically in groups with a low or no burden of disorders (Pan et al., 2021), persisted across the subsequent course of the pandemic.
The strong changes in the perceived impact of the pandemic indicate that pandemic-specific situations and events indeed elicit emotional reactions and behaviour changes (e.g. drinking more alcohol or consuming more snacks and sweets) that could be considered natural responses to external stressors (Morgan and Rose, 2020). According to our findings, these responses tended to be transient. In contrast, depressive, anxiety and worry symptoms captured by validated questionnaires were stable. This may be because these questionnaires tap into more chronic and general mood states, which appeared not to be affected by pandemic-related changes and uncertainties, at least on the group level.
This stability in depressive, anxiety and worry symptoms also pertained to participants with mental disorders. Moreover, in the group with the highest chronicity of disorders, these symptoms remained somewhat lower than before the pandemic. This does not support the expectation that the mental health of persons with mental disorders is particularly vulnerable during the Covid-19 pandemic (Holmes et al., 2020; Hotopf et al., 2020; Morgan and Rose, 2020; Pfefferbaum and North, 2020). Similar to our previous reflections based on data from the initial months of the pandemic (Pan et al., 2021), this may partly be due to the observation that symptom levels were already high in psychiatric groups, making further deterioration less likely. It might also be that aspects such as a reduction in social obligations and less exposure to crowded environments may have helped to alleviate existing symptoms of social anxiety, agoraphobia or obsessive compulsive disorder. In contrast, in persons without lifetime disorders and persons with remitted disorders, mental health symptoms remained elevated compared to pre-pandemic levels, though on average not near the threshold of clinical significance.
Nevertheless, the increase in loneliness during the initial months of the pandemic compared to pre-pandemic levels, was further exacerbated since the onset of the second wave of Covid-19 infections and deaths starting in October 2020, particularly in persons without lifetime mental health disorders. Furthermore, participants' self-reported ability to positively cope with the pandemic, which was partly based on questions about maintaining social contacts, gradually decreased. This suggests that in the long run, the pandemic reduces individuals' sense of social connectedness, which may in turn have detrimental effects on physical and mental health outcomes (Hawkley and Cacioppo, 2010), although in our sample we did not observe an average change in depressive symptoms. Moreover, intervening on loneliness may be more challenging with the profound restrictions on face-to-face contacts resulting from measures to curb the Covid-19 pandemic (Brooks et al., 2020). Therefore, it has been argued that in creating a “new normal” after the pandemic, the long-term consequences of potential loneliness-reinforcing measures that became new norms during the pandemic and are likely to persist, such as remote working, should be taken into account (Holt-Lunstad, 2021). In sum, our findings suggest that it is important to distinguish between COVID-specific emotions, fears and worries that are sensitive to the lockdowns and restrictions, and more chronic affective mood states that seem less prone to be quickly affected by specific events (Gross, 2015).
A strength of our study is that we included repeated observations in well-phenotyped psychiatric cohorts including longitudinal pre-pandemic data and healthy controls. Furthermore, we included multiple validated symptom scales and COVID-specific scales enabling assessment of changes in various dimensions of mental health and wellbeing. Limitations firstly include limits to the generalizability of our sample, including healthy controls, to the Dutch population. Comparison of responders to non-responders suggests that the most vulnerable groups may have been underrepresented. Furthermore, although our sample includes sufficient variation in mental health burden, it consists of persons who have been participating in a cohort study for a long time, and these might differ from the overall population of persons with (a history of) psychopathology. In addition, although 50% of the participants provided data for five or more waves, only about 7% participated in all twelve of them and the missing data may not fully conform to the missing-at-random assumption underlying mixed models estimation. Secondly, the Netherlands are a rich country with relatively generous social welfare arrangements and opportunities for economic compensation for Covid-19 related losses. The mental health impact may thus have been less severe than in low- and middle-income countries (Kola et al., 2021). Thirdly, our self-developed COVID-specific questionnaires have not been validated yet, and the positive coping scale had relatively low reliability. In addition, coping is a complex concept and encompasses not only positive coping, but also maladaptive coping and its associations with patient distress, which we did not capture. Nevertheless, our data may be useful to further develop instruments that accurately capture subjective mental health responses to pandemics such as Covid-19. Finally, our findings mainly pertain to groups of individuals, yet there may be large interindividual heterogeneity in Covid-19 mental health responses depending on individual characteristics (Mancini, 2020). Examining this heterogeneity is a key topic for further research.
Our study answered to the call for examining longer-term mental health consequences of the Covid-19 pandemic in psychiatric groups. After almost a year and according to our data, levels of depressive and worry symptoms remained higher than before the pandemic in healthy control groups, yet not in psychiatric groups. Loneliness was persistently higher during the pandemic in almost all groups except those with the most chronic psychiatric disorders, although also in this groups loneliness further increased in the second half of 2020. The apparent increasing mental health burden in groups without a history of psychopathology coupled with the persisting high symptoms and a relatively strong perceived Covid-19 mental health impact in psychiatric groups are important points of concern for mental health practitioners and emphasize the need for effective (online) interventions.
CRediT authorship contribution statement
All authors contributed to formulating the research question and designing the study. AALK, K-YP and EJG analysed the data. AALK wrote the initial draft of the manuscript, which was commented on and edited by all co-authors. EJG produced the figures. BWJHP obtained research funding. All authors had access to all data, have approved the final manuscript and accept responsibility for submission for publication. Funders had no role in study design, data collection, analysis, interpretation, or writing.
Declaration of competing interest
BWJHP reports grants from Janssen Research and Boehringer Ingelheim, outside of the submitted work. All other authors declare no competing interests.
Acknowledgments
Acknowledgements
We thank all NESDA, NESDO and NOCDA participants for their valuable contributions to the studies as participants.
Data availability
According to European law (General Data Protection Regulation), data containing potentially identifying or sensitive patients' information are restricted. However, for academic researchers, data can be made available on request via the NESDA (nesda@ggzingeest.nl), NESDO (d.rhebergen@ggzcentraal.nl), and NOCDA (p.vanoppen@ggzingeest.nl) data access committees.
Funding sources
COVID online data collection and analyses were partly funded by a ‘fast track grant’ from the Dutch Research Council (grant no 440.20.009) and by the RESPOND project which has received funding from the European Union's Horizon 2020 research and innovation programme Societal Challenges under grant agreement No 101016127. The infrastructure for the NESDA study is funded through the Geestkracht programme of the Netherlands Organisation for Health Research and Development (grant no 10-000-1002) and financial contributions by participating universities and mental health-care organisations (VU University Medical Center, Geestelijke Gezondheidszorg (GGZ) inGeest, Leiden University Medical Center, Leiden University, GGZ Rivierduinen, University Medical Center Groningen, University of Groningen, Lentis, GGZ Friesland, GGZ Drenthe, Rob Giel Onderzoekscentrum). The infrastructure for the NESDO study is funded through the Fonds NutsOhra (project 0701-065), Stichting tot Steun VCVGZ, NARSAD The Brain and Behaviour Research Fund (grant id 41080), and by participating universities and mental health-care organisations (VU University Medical Center, Leiden University Medical Center, University Medical Center Groningen, University Medical Center St Radboud, GGZ inGeest, GGNet, GGZ Nijmegen, GGZ Rivierduinen, Lentis, and Parnassia). The infrastructure for the NOCDA study is funded by participating universities and mental health-care organisations (Academic Department VU Medical Center, GGZ inGeest, Innova Research Centre, Mental Health Care Institute GGZ Centraal, Marina de Wolf Anxiety Research Centre, Center for Anxiety Disorders Overwaal, Dimence, GGZ Overijssel, Department of Psychiatry at Leiden University Medical Center, Vincent van Gogh Institute Mental Health Care Centre, Academic Anxiety Center, PsyQ Maastricht University, Division Mental Health and Neuroscience, and Stichting tot Steun VCVGZ).
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2022.02.056.
Appendix A. Supplementary data
Supplementary material
References
- Beck Aaron T., Brown Gary, Kiyosaki R.T., Lechter S.L. An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bueno-Notivol J., Gracia-García P., Olaya B., Lasheras I., López-Antón R., Santabárbara J. Prevalence of depression during the COVID-19 outbreak: a meta-analysis of community-based studies. Int. J. Clin. Health Psychol. 2021;21 doi: 10.1016/j.ijchp.2020.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chowdhury E.K., Khan I.I., Dhar B.K. Catastrophic impact of COVID-19 on the global stock markets and economic activities. Bus. Soc. Rev. 2021 doi: 10.1111/basr.12219. [DOI] [Google Scholar]
- Comijs H.C., Van Marwijk H.W., Van Der Mast R.C., Naarding P., Oude Voshaar R.C., Beekman A.T.F., Boshuisen M., Dekker J., Kok R., De Waal M.W.M., Penninx B.W.J.H., Stek M.L., Smit J.H. The Netherlands study of depression in older persons (NESDO); a prospective cohort study. BMC Res. Notes. 2011;4 doi: 10.1186/1756-0500-4-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor R.C.O., Wetherall K., Cleare S., Mcclelland H., Melson A.J., Claire L., Carroll R.E.O., Connor D.B.O., Platt S., Scowcroft E., Watson B., Ferguson E., Robb K.A. Mental health and wellbeing during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br. J. Psychiatry. 2020 doi: 10.1192/bjp.2020.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong-Gierveld J., Kamphuis F. The development of a Rasch-type loneliness scale. Appl. Psychol. Meas. 1985;9:289–299. doi: 10.1177/014662168500900307. [DOI] [Google Scholar]
- Fancourt D., Steptoe A., Bu F. Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry. 2021;8:141–149. doi: 10.1016/S2215-0366(20)30482-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L., Gibbon M., Williams J.B.W. American Psychiatric Press; New York, NY: 1996. User's Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I): Clinician Version. [Google Scholar]
- Gross J.J. Emotion regulation: current status and future prospects. Psychol. Inq. 2015;26:1–26. doi: 10.1080/1047840X.2014.940781. [DOI] [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010;40:218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O’Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad A pandemic of social isolation? World Psychiatry. 2021;20:55–56. doi: 10.1002/wps.20839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotopf M., Bullmore E., O’Connor R.C., Holmes E.A. The scope of mental health research during the COVID-19 pandemic and its aftermath. Br. J. Psychiatry. 2020;217:540–542. doi: 10.1192/bjp.2020.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson J., Weiss M., Schwarzenberg A., Nelson R. Congr. Res. Serv. R46270; 2021. Global Economic Effects of COVID-19. [Google Scholar]
- Kola L., Kohrt B.A., Hanlon C., Naslund J.A., Sikander S., Balaji M., Benjet C., Cheung E.Y.L., Eaton J., Gonsalves P., Hailemariam M., Luitel N.P., Machado D.B., Misganaw E., Omigbodun O., Roberts T., Salisbury T.T., Shidhaye R., Sunkel C., Ugo V., van Rensburg A.J., Gureje O., Pathare S., Saxena S., Thornicroft G., Patel V. COVID-19 mental health impact and responses in low-income and middle-income countries: reimagining global mental health. Lancet Psychiatry. 2021;0366:1–16. doi: 10.1016/S2215-0366(21)00025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini A.D. Heterogeneous mental health consequences of COVID-19: costs and benefits. Psychol. Trauma TheoryRes. Pract. Policy. 2020;12:15–16. doi: 10.1037/tra0000894. [DOI] [PubMed] [Google Scholar]
- Marazziti D., Stahl S.M. The relevance of COVID-19 pandemic to psychiatry. World Psychiatry. 2020;19:261. doi: 10.1002/wps.20764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer T.J. Development and validation of the Penn State Worry Questionnaire. Behav. Res. Ther. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Morgan C., Rose N. Multidisciplinary research priorities for the COVID-19 pandemic. Lancet Psychiatry. 2020;7 doi: 10.1016/S2215-0366(20)30230-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan K., Kok A.A.L., Eikelenboom M., Horsfall M., Jörg F., Luteijn R.A., Rhebergen D., Oppen P.Van, Giltay E.J. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: a longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry. 2021;8:121–129. doi: 10.1016/S2215-0366(20)30491-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penninx B.W.J.H., Beekman A.T.F., Smit J.H., Zitman F.G., Nolen W.A., Spinhoven P., Cuijpers P., de Jong P.J., van Marwijk H.W.J., Assendelft W.J.J., van der Meer K. The Netherlands Study of Depression and Anxiety (NESDA): rationale, objectives and methods. Int. J. Methods Psychiatr. Res. 2008;17:121–140. doi: 10.1002/mpr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020;383:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pierce M., McManus S., Hope H., Hotopf M., Ford T., Hatch S., John A., Kontopantelis E., Webb R.T., Wessely S., Abel K.M. Different mental health responses to the COVID-19 pandemic: latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021 doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021 doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rush A.J., Trivedi M.H., Ibrahim H.M., Carmody T.J., Arnow B., Klein D.N., Markowitz J.C., Ninan P.T., Kornstein S., Manber R., Thase M.E., Kocsis J.H., Keller M.B. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol. Psychiatry. 2003;54:573–583. doi: 10.1016/S0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- Schuurmans J., van Balkom A.J.L.M., van Megen H.J.G.M., Smit J.H., Eikelenboom M., Cath D.C., Kaarsemaker M., Oosterbaan D., Hendriks G.-J., Schruers K.R.J., van der Wee N.J.A., Glas G., van Oppen P. The Netherlands Obsessive Compulsive Disorder Association (NOCDA) study: design and rationale of a longitudinal naturalistic study of the course of OCD and clinical characteristics of the sample at baseline. Int. J. Methods Psychiatr. Res. 2012;21:273–285. doi: 10.1002/mpr.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsamakis K., Tsiptsios D., Ouranidis A., Mueller C., Schizas D., Terniotis C., Nikolakakis N., Tyros G., Kympouropoulos S., Lazaris A., Spandidos D., Smyrnis N., Rizos E. COVID-19 and its consequences on mental health (review) Exp. Ther. Med. 2021;21 doi: 10.3892/etm.2021.9675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20:124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO WHO COVID-19 dashboard [WWW Document] 2022. https://covid19.who.int/ URL.
- Wittchen H.U. Reliability and validity studies of the WHO-Composite International Diagnostic Interview (CIDI): a critical review. J. Psychiatr. Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
According to European law (General Data Protection Regulation), data containing potentially identifying or sensitive patients' information are restricted. However, for academic researchers, data can be made available on request via the NESDA (nesda@ggzingeest.nl), NESDO (d.rhebergen@ggzcentraal.nl), and NOCDA (p.vanoppen@ggzingeest.nl) data access committees.