Too often, pediatric obesity clinical trials and interventions having an otherwise solid scientific premise and addressing highly relevant questions use the Centers for Disease Control and Prevention (CDC) BMI z score as the primary efficacy end point. The use of the CDC z scores has the potential to affect and lead to incorrect conclusions drawn by the authors of studies, particularly if many participants have BMI values above the 97th percentile, which reduces the rigor of these studies. Reporting on outcomes and predictors of treatment response within pediatric obesity clinical trials and interventions sheds light on vital clinical questions; therefore, the inclusion of multiple BMI metrics in clinical trials could advance the understanding of which metric is optimal for assessing change.
The use of the CDC BMI z score in children and adolescents (aged 2 to <20 years) with obesity has recently come under scrutiny because of limited utility when applied to cohorts that include participants with BMI values above the 97th percentile (1–3). The 97th percentile was the highest percentile directly estimated in the 2000 CDC growth charts (4), and all percentiles and z scores above the 97th were based on extrapolation, which can be inaccurate. Although difficult to determine from the data presented in some clinical trials and interventions, a relatively high proportion of participants in contemporary trials likely have BMI values well above the 97th percentile (~70% of children with obesity in National Health and Nutrition Examination Survey [NHANES] 2011–2018 had BMI > 97th percentile).
The compression of the CDC z scores among children with severe obesity, which resulted from the statistical method used to normalize the BMI distribution (4), further complicates their use. For example, if a 10-year-old boy with a BMI of 50 kg/m2 decreased by 10% over 6 months, the child’s BMI z score would decrease by only 0.07 standard deviations and would be considered unimportant (5). Several alternative metrics to the CDC BMI z score have been proposed without a consensus of the optimal metric; however, the literature has made clear that several alternative metrics are superior to the CDC BMI z score, especially for longitudinal tracking (1–3). Unfortunately, many publications that rely on the CDC BMI z score as the primary metric do not consistently report on other BMI or weight-related metrics (e.g., absolute BMI, BMI percentile, percentage of the 95th percentile, percentage of the median, distribution within each obesity category). Indeed, the conclusions drawn from many of these studies rely solely on using the CDC BMI z score.
Moreover, some researchers have supported their findings by using a weakly supported cut point of clinical treatment success of ≥0.20 CDC BMI z score unit reduction based on the United States Preventive Services Task Force (USPSTF) guidelines, which further clouds the interpretation of the findings (5). However, there is no consensus of an optimal pediatric obesity cut point for clinically meaningful weight loss. Indeed, the primary data source used by the USPSTF suggested that the cut point be placed higher (in the 0.25–0.50 CDC BMI z score range) if clinically meaningful improvements in cardiometabolic risk factors are to be expected (6). Furthermore, a meta-regression analysis placed this bar even higher (in the 0.7–1.2 CDC BMI z score unit reduction range) for improvement of cardiometabolic risk factors (7), which is near bariatric surgery levels of weight loss for most youth. Regardless, the use of z scores for pediatric obesity outcomes should be avoided because of scaling, interpretation, and bias issues (8,9).
One logical way to address this issue during this era of lack of consensus is to present various continuous BMI metrics as outcomes (e.g., absolute and percentage of change in BMI, change in percentage of the 95th BMI percentile, change in percentage of the median) along with the proportion meeting certain BMI thresholds as secondary outcomes to further support analyses of pediatric obesity intervention trial outcomes (Figure 1). Although the adult literature widely uses >5% and >10% BMI or weight reduction as cut points for clinical treatment success (10), similar thresholds are rarely used in the pediatric literature. It would lend great clarity to the data provided if several BMI-based metrics were used as continuous variables to support the conclusions made by authors of pediatric obesity clinical trials. In addition, it would allow for the comparison of treatments to be more easily conducted to move the field of pediatric obesity medicine forward in a meaningful way.
FIGURE 1.
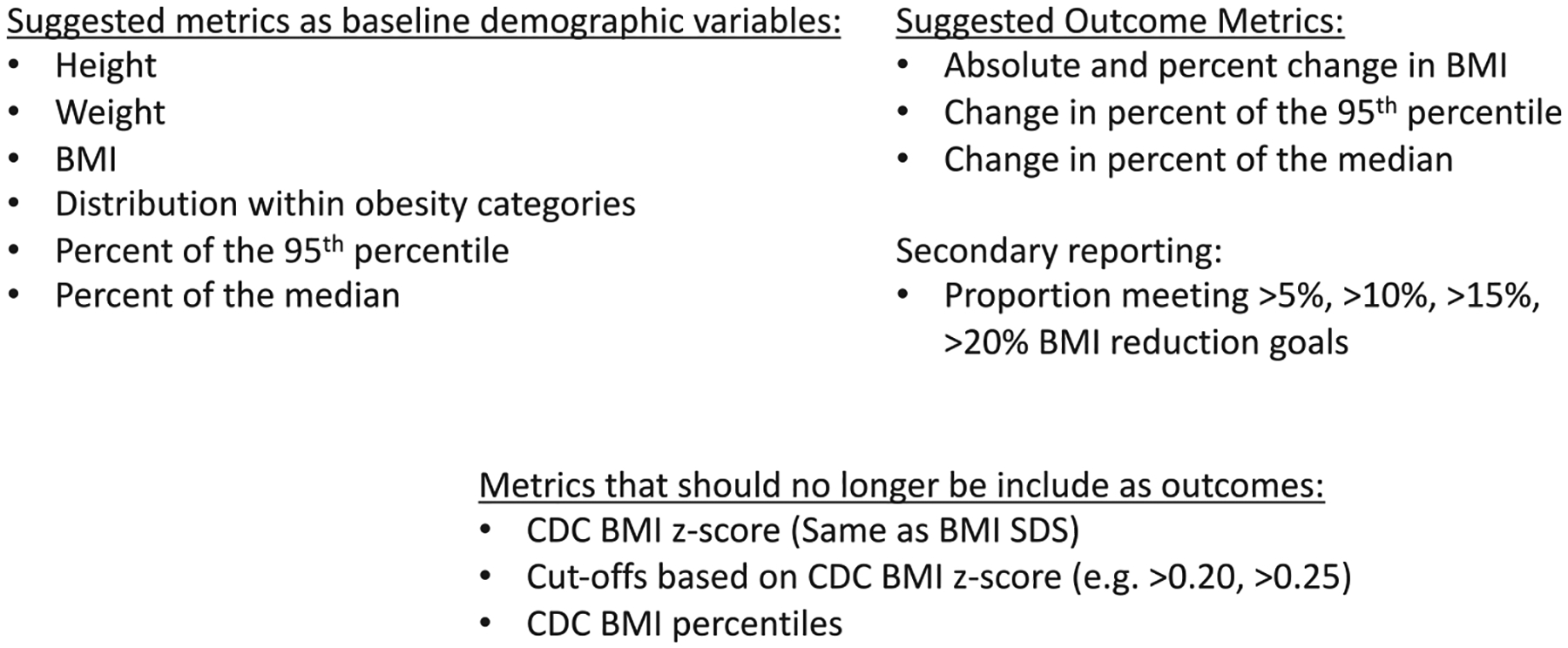
Suggested reporting of outcome metrics for pediatric obesity clinical trials and interventions. CDC, Centers for Disease Control and Prevention
The larger point of discussion for pediatric obesity is that the metrics used to determine success and interpret findings of pediatric obesity treatments matter. Agreement on which measures are optimal and what threshold constitutes clinical treatment success would help researchers know which measures to report and help practitioners understand the potential impact of different interventions. Until widespread agreement can be reached, investigators can consider consistently reporting more metrics (e.g., absolute and percentage of change in BMI, change in percentage of the 95th BMI percentile, change in percentage of the median) and demonstrating robust findings with multiple outcomes for sufficient conclusions to be drawn and comparisons to be made. This applies not only to pediatric obesity researchers but also to the journals in the field, which could emphasize consistent reporting of a wide variety of metrics to enhance scientific rigor. Metrics matter.
CONFLICT OF INTEREST
JRR receives support from Boehringer Ingelheim Pharmaceuticals in the form of drug/placebo. JRR serves as a consultant for Novo Nordisk A/S and Eli Lilly and Company; he does not accept personal or professional income for his services. ASK serves as a consultant for Novo Nordisk A/S, Vivus, and Eli Lilly and Company; he does not accept personal or professional income for his services. ASK also receives research support from Vivus in the form of drug/placebo. The other authors declared no conflict of interest. This report’s findings and conclusions are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Freedman DS, Butte NF, Taveras EM, Goodman AB, Ogden CL, Blanck HM. The limitations of transforming very high body mass indexes into z-scores among 8.7 million 2-to 4-year-old children. J Pediatr. 2017;188:50–56.e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman DS, Butte NF, Taveras EM, et al. BMI z-scores are a poor indicator of adiposity among 2-to 19-year-olds with very high BMIs, NHANES 1999–2000 to 2013–2014. Obesity (Silver Spring). 2017;25:739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wei R, Ogden CL, Parsons VL, Freedman DS, Hales CM. A method for calculating BMI z-scores and percentiles above the 95(th) percentile of the CDC growth charts. Ann Hum Biol. 2020;47:514–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Flegal KM, Cole TJ. Construction of LMS parameters for the Centers for Disease Control and Prevention 2000 growth charts. Natl Health Stat Report. 2013;63:1–3. [PubMed] [Google Scholar]
- 5.Grossman DC, Bibbins-Domingo K, Curry SJ, et al. Screening for obesity in children and adolescents: US preventive services task force recommendation statement. JAMA. 2017;317:2417–2426. [DOI] [PubMed] [Google Scholar]
- 6.Reinehr T, Lass N, Toschke C, Rothermel J, Lanzinger S, Holl RW. Which amount of BMI-SDS reduction is necessary to improve cardiovascular risk factors in overweight children? J Clin Endocrinol Metab. 2016;101:3171–3179. [DOI] [PubMed] [Google Scholar]
- 7.El-Medany AYM, Birch L, Hunt LP, et al. What change in body mass index is required to improve cardiovascular outcomes in childhood and adolescent obesity through lifestyle interventions: a meta-regression. Child Obes. 2020;16:449–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berkey CS, Colditz GA. Adiposity in adolescents: change in actual BMI works better than change in BMI z score for longitudinal studies. Ann Epidemiol. 2007;17:44–50. [DOI] [PubMed] [Google Scholar]
- 9.Cole TJ, Faith MS, Pietrobelli A, Heo M. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr. 2005;59:419–425. [DOI] [PubMed] [Google Scholar]
- 10.Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384:989–1002. [DOI] [PubMed] [Google Scholar]


