Abstract
Objectives
To investigate the effect of Jintiange capsule on acute bone atrophy (vertebral height, Cobb's angle, bone mineral density, and visual analog score (VAS) in patients with osteoporotic vertebral compression fracture.
Methods
A total of 106 patients with osteoporotic vertebral compression fractures were selected and randomly divided into study and control group. Vertebral height ratio (VHR), Cobb's angle, bone mineral density (BMD), and VAS analyses were performed as study indexes. The study was performed from January 2019 to December 2019 as a double‐blind, randomized, controlled trial and all the participants were blinded throughout the study. There were 24 males and 29 females in the study group, with 14 cases of thoracic fractures and 39 cases of lumbar fractures. The age was 61–75 years, with an average of 67.5 ± 2.7 years, and the course of disease was 1–9 days, with an average of 2.7 ± 0.5 days. There were 22 males and 31 females in the control group, with 17 cases of thoracic fractures and 36 cases of lumbar fractures. Patients in the control group received conventional postoperative treatment, while patients in the study group were treated with Jintiange capsule. The treatment continued for 3 months. The ages of the participants were from 60 to 70 years, while the average ages of both groups were 67 ± 2.8 years and the study recruited participants of both sexes.
Results
The clinical efficacy, vertebral imaging indexes before and after treatment, as well as pain and daily activity dysfunction scores were compared. The effect of the Jintiange capsule was followed for 3 months and both the groups were compared. The total effective score of the study group was significantly increased (90.6%) in contrast to the control group (67.9) and the P value was less than the 0.5. The vertebral height and bone mineral density of the study group was significantly improved compared to the control group (P < 0.034) using t‐test. However, the Cobb's angle of the study group was significantly (P < 0.047) lower than the control group using t‐test after the treatment. On the other hand, the VAS score and Oswestry score of the study group were significantly lower than control group at 1 month and 3 months after treatment (P < 0.05). There was no significance difference (all P > 0.05) in term of gender and ages in both the recruited groups.
Conclusion
It can be concluded that Jintiange capsule can significantly improve the clinical efficacy rate, vertebral height, Cobb's angle, and bone mineral density, pain relief, and daily activity function.
Keywords: Anti‐osteoporosis drug, Jintiange capsule, Osteoporotic vertebral compression indexes
Jintiange capsules are a good choice for treating patients with osteoporosis in terms of improving bone mineral density, relieving pain, and reducing adverse events.

Introduction
In the United States alone, vertebral compression fractures affected approximately 25% of all postmenopausal women, while the prevalence increased with the age and reached 40% in women who were 80 years of age 1 , 2 . Furthermore, women who were diagnosed with vertebral compression fracture have high mortality rates, i.e. 15% compared to those who do not have vertebral fractures. While vertebral compression is reported less in older men than women, it is also a major health problem in this age group and the concern is increasing 1 , 2 . The annual medical cost of vertebral compression fractures was about US$749 mn in 1995 in the United States and the cost of the treatment has substantially increased during recent decades. Although treatment for vertebral compression fractures is less expensive compared with treatment for hip fracture, vertebral compression fracture significantly affects quality of life. The pain (acute and chronic) associated with the vertebral compression fractures is felt more severely and contributes to further disability 1 , 2 .
Jintiange capsule is a biomimetic medicine, and its components are derived from “non‐protected” animal bones with the same pharmacological attributes of tiger bone powder, so it is referred to as artificial tiger bone powder 3 . Recent studies indicated that the active ingredients of Jintiange capsules can improve the metabolism to absorb calcium and phosphorus. It is one of the natural tiger bone substitutes, which has analgesic and bone‐strengthening functions 3 . Furthermore, Jintiange capsules have been reported to promote bone fracture healing and improve osteoporosis 3 .
Vertebral compression fractures are a common disease type, mainly due to accumulation, injury, labor, and inadequate prevention of osteoporosis. The incidence rate of this disease is relatively high in the elderly 3 . Most elderly patients are prone to thoracolumbar compression fractures after minor or unintentional injury, and some will have severe pain, which will have a serious impact on ground activities and turning over, thus posing a serious threat to their health 4 . At present, with the progress and development of medical technology, percutaneous balloon kyphoplasty (PKP) is gradually applied in clinical practice. In addition, during the surgical treatment of patients with osteoporotic vertebral compression fractures, the combination of drug treatment helps to promote fracture healing and improve clinical efficacy 5 . The percutaneous kyphoplasty (PKP) surgery has proved very effective in relieving pain and disability related with the vertebral compression fractures. However, in clinical practice the unilateral PKR procedure varies among different vertebral bodies in terms of intravertebral bone cement distribution. Moreover, it has been demonstrated that both cement volume and filling pattern following PKR leads to curative effects and surgical complications.
Acute bone atrophy is a kind of local osteoporosis but is often mistaken as a common fracture symptom, which leads to delayed diagnosis and treatment 1 , 2 . There is little information regarding the treatment and no specific medicine currently. For now, rehabilitation training and analgesic therapy are the main treatments. Acute bone atrophy is considered as local type of osteoporosis but is mistakenly regarded as a common fracture symptom, which significantly influences the diagnosis and treatment. Until now there is no effective therapy has been devised to treat bone dystrophy and osteoporosis; however, rehabilitation training and analgesic therapy remains the main approaches 1 , 2 . The clinical features associated with the osteoporotic vertebral compression fractures include acute or chronic back pain, physical disability, and distinct radiographic findings due to mechanical compression. The clinical management should aim to restore the physical and biomechanical resistance of the compromised spinal segment 1 , 2 .
In the current study, Jintiange capsules were used to assess the effect on vertebral height, bone mineral density, VAS, and Cobb's score. Based on previous reports, the current study anticipated that Jintiange capsules would improve the underlying conditions associated with the osteoporotic vertebral compression fracture.
Experimental
Participant Information
One hundred and six patients with osteoporotic vertebral compression fractures admitted to our hospital from January 2019 to December 2019 were selected and randomly divided into the study group and the control group. There were 24 males and 29 females in the study group, with 14 cases of thoracic fracture and 39 cases of lumbar fracture. The age was 61–75 years, with an average of 67.5 ± 2.7 years, and the course of disease was 1–9 days, with an average of 2.7 ± 0.5 days. There were 22 males and 31 females in the control group, with 17 cases of thoracic fracture and 36 cases of lumbar fracture. The age was 63–74 years, with an average of 67.8 ± 2.8 years, and the course of disease was 1–10 days, with an average of 2.9 ± 0.6 days. Figure 1 illustrates the flow chart and information about the participants of the study.
Fig. 1.
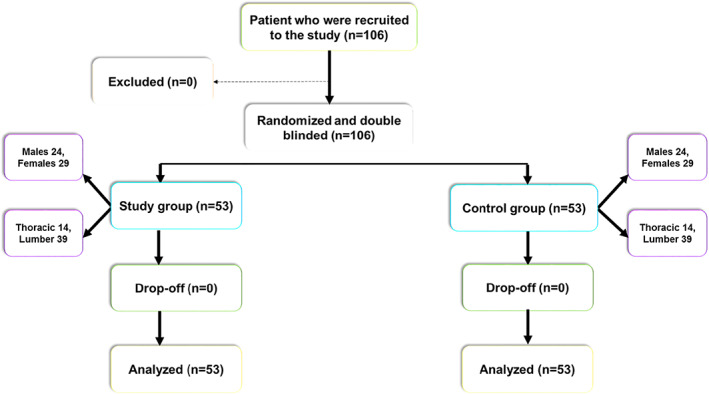
The illustrative diagram of the study design and the information about the participants. The Figure shows the number of patient recruited to the study, study design, and demographic data.
Inclusion Criteria
Participants were recruited in the study who fulfilled the following criteria:
Participants: Patients who were diagnosed with osteoporotic vertebral compression fractures by clinical examination were recruited.
Intervention and comparison: Two study groups were formed: control group and study group. The control group underwent surgery only, while the study group received Jintiange capsules in addition to the surgical intervention.
Outcome: The outcome of the study was to assess the effect of the Jintiange capsules on the vertebral height, Cobb's angle, bone mineral density, and VAS.
Study design: The study was randomized, controlled, and double‐blind.
Exclusion Criteria
The exclusion criteria were as follows: (i) Combined with combined nerve root and spinal cord injury; (ii) combined with severe dysfunction of heart, liver, kidney, or other important functional organs; (iii) allergy to the drug used in this study; and (iv) with cognitive and language impairment and midway withdrawal.
There were no significant differences in the general information between the two groups (P > 0.05). The experiment was approved by the ethics committee.
Treatment Intervention
Anesthesia and Position
Patients in both groups received PKP surgery. In brief, the patient was placed in the prone position to keep their abdomen in the air (pillow could be placed in the front of bilateral ilium and under the chest). After routine disinfection of the surgical site, local anesthesia was carried out at both sides of the injured vertebral pedicle.
Approach and Exposure
Patients in the control group received conventional postoperative treatment including anti‐infection, and patients in the study group were treated with Jintiange capsules (manufacturer: Jinhua Enterprise Co., Ltd., z20030080), oral administration, three capsules, tris in a day (tid). Both the groups were treated for 3 months.
Pathological Changes and Resection
A 0.5 cm incision was made along the puncture site, and then the puncture needle with needle core was punctured to the vertebral body of the diseased vertebra at an angle of 15°–20° through the pedicle. To ensure that the puncture can reach the central position of the vertebral body, C‐type fluoroscopy machine could be used for assistance. After the core of the puncture needle was taken out, the contrast medium was injected, and the adjacent relationship between the internal vertebral vein and the puncture needle was observed carefully with the help of C‐arm fluoroscopy machine.
Fixation or Replacement of Prosthesis
After the guide pin is placed, the puncture needle is pulled out, and the expansion sleeve and working sleeve were placed along the guide pin. The fine drill was used to drill along the working sleeve to the corresponding designated position, and the balloon is placed in it, in a position located in the front 3/4 position of the vertebral body.
Reconstruction
The fracture reduction is observed carefully by fluoroscopy machine. After reduction to the appropriate position, stop balloon expansion and take it out, then inject bone cement into the vertebral body, and end the operation when the bone cement is about to overflow. The procedure of the surgical intervention has been illustrated in Fig. 2.
Fig. 2.

The Figure illustrates the overall surgical procedure and therapeutic intervention.
Observed Indexes
The total effective rate was compared between the two groups as: (i) completely effective: the clinical symptoms of pain and back soreness disappeared, and the daily functional activities returned to normal; (ii) effective: the symptoms of pain and back soreness almost disappeared, and there was mild dysfunction when carrying out daily activities; (iii) non‐effective: the above indexes were not reached, and there was a tendency of aggravation.
Vertebral Body Height
Definition
The vertebral body height is an important imaging parameter for determining the architecture, prognosis, and clinical outcome of the treatment on compression fractures.
Measuring Methods
The vertebral body height index was determined by the radiographic analysis before the commencement of intervention and 3 months after the intervention.
Clinical Significance of Vertebral Body Height
The vertebral body height (VBH) can be used to assess the effect of the any treatment on the compression fracture. The radiographic analysis provides critical insight into the vertebral body height based on the radiography and the compression of the vertebral fracture can be investigated. The increase in the VBH leads to increased vertebral instability.
Cobb's angle
Definition
The Cobb's angle is a measurement of greatest angle at a particular region of the vertebral column, when measured from the superior endplate of a superior vertebra to the inferior endplate of an inferior vertebra.
Measuring Methods
Cobb's angles are preferably measured while standing, since laying down decreases Cobb's angles by around 7°–10°. The Cobb's angle was assessed using X‐ray analysis and the results of the radiograph before treatment and 3 months after the therapy.
Clinical Significance of Cobb's Angle
The Cobb's angle was the preferred method to assess the vertebral abnormalities including vertebral compression fractures, kyphosis, scoliosis, etc. While radiographic analysis provides changes in the vertebral compression, the effect of the treatment modality outcome can be assessed.
Bone Mineral Density
Definition
Bone mineral density (BMD) test can be used to determine the status of the bone and its alteration. It also provide information about the susceptibility of your bones to pathological conditions such as osteoporosis.
Measuring Methods
The radiographic analysis was compared between the two groups, i.e. control and study group before treatment and 3 months after the treatment.
Clinical Significance of the Bone Mineral Density (BMD)
The BMD serves as predictor of the future changes in vertebral structure and can be used to assess the effect of the treatment on the BMD. The risk of fractures increases two‐fold for each standard deviation decrease in the BMD.
Assessment of Visual Analog Scale (VAS)
Definition
“The visual analogue scale or visual analog scale (VAS) is a psychometric response scale which can be used in questionnaires.” It is commonly employed to assess functional outcomes in patients with back pain.
Measuring Methods
The pain scores of the two groups were evaluated and compared. The VAS was used to judge the pain before treatment and at 1 month and 3 months after treatment. The score of the scale was 0–10 points, which was directly proportional to the pain status of the patients.
Clinical Significance of the Parameters
VAS has a direct relation to subsequent disability in patients with back pain and/or spinal injury, . The VAS score directly influences the non‐operatively as well as operatively treated groups and is the most common scale for pain assessment in various conditions such as vertebral compression fractures, endometriosis, and chronic pelvic condition.
Assessment of Oswestry Disability Questionnaire (ODI)
Definition
The ODI is a questionnaire based survey that assess the influence of chronic low back pain on activities of daily living. The ODI survey is concise and straightforward, allowing patients to complete it quickly.
Measuring Methods
The ODI was used to evaluate and judge the degree of leg pain and low back pain before treatment, 1 month and 3 months after treatment. The 10 sections cover the pain and the daily function (including pain intensity, personal hygiene, lifting, walking, sitting, standing, sleeping, sexual activity, social activity, and traveling). Each item is rated on a six‐point scale (0–5); the higher the score, the higher the level of disability related to LBP. The present study used the traditional Chinese version of the ODI 2.1.
Clinical Significance of ODI
The ODI is widely used to assess the degenerative spine changes and consequently assess the impact of the treatment on this parameter.
Statistical Methods
The data were analyzed with SPSS_17.0 (SPSS Inc., USA). Measurement data were expressed in terms of mean and standard deviation (mean ± SD) and categorical data were expressed as percentages. A two‐independent sample t‐test was used to compare normally distributed data. The categorical data was analyzed with chi‐square test. P < 0.05 means the difference was statistically significant. Univariate analysis was conducted with chi‐square tests. The multivariate analysis results were reported as odds ratios (ORs) and 95% confidence intervals. The subgroup analysis was performed to assess the statistically significant difference of the studied groups.
Results
Comparison of the Total Effective Rate Between the Two Groups
Total effective rate, which includes completely effective, effective, and non‐effective, was compared between the two groups, i.e. control and study group. The chi‐square distribution was used to assess the P value between the two groups. The total effective score of the study group was significantly increased in contrast to the control group and the P value was less than the 0.5. Table 1 shows the various parameters of the two groups and respective X2 as well as P value.
Table 1.
Comparison of the total effective rate between the two groups (n = 53)
| Groups | Completely effective (%) | Effective (%) | Non‐effective (%) | Total effective rate (%) |
|---|---|---|---|---|
| Control | 20.8 | 47.2 | 32.1 | 67.9 |
| Study | 35.8 | 54.7 | 9.4 | 90.6 |
| χ2 | 4.610 | |||
| P | <0.043 | |||
| Multivariate analysis OR (95% CI) | 0.95 (0.92 to 1.01) | |||
Comparison of Vertebral Imaging Indexes Between the Two Groups
The vertebral height, Cobb's angle, and bone mineral density was assessed in both groups before treatment and 3 months after the treatment. The vertebral height and bone mineral density of the study group was significantly improved compared to the control group (P < 0.034) using t‐test. However, the Cobb's angle of the study group was significantly (P < 0.047) lower than the control group using t‐test after the treatment and the results are shown in Table 2.
Table 2.
Comparison of vertebral imaging indexes between the two groups (n = 53)
| Groups | Vertebral height (mm) | Cobb's angle (°) | Bone mineral density (g/cm) | |||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||||
| Before treatment | After treatment | Before treatment | After treatment | Before treatment | After treatment | |
| Control | 13.7 ± 1.5 | 24.0 ± 1.4 | 25.2 ± 3.2 | 14.0 ± 1.6 | 0.33 ± 0.07 | 0.33 ± 0.05 |
| Study | 13.9 ± 1.3 | 30.1 ± 1.7 | 25.4 ± 3.3 | 8.5 ± 1.2 | 0.34 ± 0.08 | 0.37 ± 0.10 |
| t value | 1.301 | 11.527 | 1.935 | 12.201 | 1.437 | 10.008 |
| P value | >0.034 | >0.047 | >0.029 | |||
| Multivariate analysis | 0.57 | 0.94 | 0.64 | 0.97 | 0.69 | 0.98 |
| OR (95% CI) | (0.14 to 3.21) | (0.94 to 1.03) | (0.34 to 1.41) | (0.93 to 1.02) | (0.12 to 3.15) | (0.43 to 2.15) |
Comparison of VAS between the Two Groups
VAS was used to assess the effect of the Jintiange capsules on the treatment outcomes in the osteoporotic vertebral compression fractures. VAS was significantly lowered by the Jintiange capsule in the study group compared to the control group 1 and 3 months after the treatment using t‐test and the P value was recorded lower than 0.05 as shown in Table 3.
Table 3.
Comparison of the VAS score between the two groups (n = 53, mean ± SD)
| Groups | Before treatment | 1 month after treatment | 3 months after treatment |
|---|---|---|---|
| Control | 8.4 ± 2.9 | 4.2 ± 1.3 | 2.0 ± 0.9 |
| Study | 8.5 ± 2.8 | 3.4 ± 1.0 | 0.5 ± 0.3 |
| t value | 1.638 | 10.819 | 10.116 |
| P value | >0.038 | <0.042 | <0.047 |
| Multivariate analysis | 0.81 | 0.97 | 0.94 |
| OR (95% CI) | (0.19 to 3.12) | (0.94 to 1.01) | (0.91 to 1.02) |
Comparison of the ODI between the Two Groups
The ODI was determined before and after the treatment in both the groups. The ODI was significantly lower in the study group following treatment with the Jintiange capsules compared to the control that underwent only surgical intervention and did not receive Jintiange capsules 1 and 3 months after treatment. The study group showed significant statistical difference from the control group, and P value was less than 0.05 as evident in Table 4.
Table 4.
Comparison of the Oswestry score between the two groups (n = 53) (mean ± SD)
| Groups | Before treatment | 1 month after treatment | 3 months after treatment |
|---|---|---|---|
| Control | 69.8 ± 8.1 | 25.0 ± 2.3 | 15.1 ± 2.1 |
| Study | 68.6 ± 7.8 | 13.4 ± 2.1 | 6.8 ± 1.0 |
| t value | 2.001 | 12.546 | 12.130 |
| P value | >0.035 | <0.038 | <0.032 |
| Multivariate analysis | 0.76 | 0.96 | 0.98 |
| OR (95% CI) | (0.23 to 3.40) | (0.93 to 1.02) | (0.49 to 2.18) |
Subgroup Analysis
The subgroup analysis was performed to assess the statistically significant difference of the participants in different groups. The various variables were analyzed during the subgroup analysis and the results are shown in Table 5.
Table 5.
The subgroup analysis of the control and study groups
| Control group | Study group | ||||
|---|---|---|---|---|---|
| Subgroups | Total | Total | OR (95% CI) | ||
| Age (years) | |||||
| 61–68 | 25/53 | 25 | 21/53 | 21 | 0.84 (0.54, 1.10) |
| 69–75 | 28/53 | 28 | 32/53 | 32 | 0.79 (0.64, 1.3) |
| Male | 22/53 | 22 | 24/53 | 24 | 0.82 (0.67, 1.09) |
| Female | 31/53 | 31 | 29/53 | 29 | 1.34 (0.72, 2.17) |
| Thoracic fracture | 17/53 | 17 | 14/53 | 14 | 0.89 (0.51, 1.72) |
| Lumber fracture | 36/53 | 36 | 39/53 | 39 | 0.73 (0.56, 1.86) |
Complication
The thoracolumbar spine compression fractures involve flexion compression mechanism of injury and the first column, i.e. anterior longitudinal ligament and anterior half of the vertebral body is commonly implicated. The vertebral compression fractures of the vertebral bodies are particularly troublesome for osteoporosis patients and trivial events such as weightlifting, vigorous cough, or turning in bed can cause problems. It has been hypothesized that fractures in vertebral bodies occur because of an increased load on the spine caused by contraction of paraspinal muscles. It has been suggested that approximately 30% of compression fractures in patients with severe osteoporosis occur while the patient is in bed 1 , 2 . Furthermore, it has been hypothesized that the vertebral body's fractures are often triggered by the increased load on spinal cord by the contraction of the paraspinal muscles. It has been reported that about 30% of the vertebral compression fractures occur in severe osteoporosis patients while the patient is in bed, while the moderate osteoporotic patient experiences vertebral compression fractures due to falling from a chair, tripping or lifting weights, and in people without osteoporosis the vertebral compression fractures commonly occur due to accident or falling from a height. For vertebral compression fractures in people younger than 55 years, malignancy can possibly be involved 2 .
Discussion
General Overview
Osteoporotic fracture is a kind of systemic bone metabolism disease and has a high incidence rate in postmenopausal women and elderly people 6 , 7 . The main clinical manifestations of osteoporotic fracture are bone mass decrease, bone fragility increase, and bone microstructure damage 6 , 7 . In the past, the combination of long‐term bed rest and drug therapy is mostly used, but its long‐term effect is not ideal. After the patient stands, it is easy to cause vertebral body height reduction, which has a serious impact on quality of life 8 . In recent years, with the progress and development of medical technology, minimally invasive treatments, such as PBK, have been gradually applied and promoted in the treatment of patients with osteoporotic fractures. For patients with spinal canal stenosis, spinal nerve disorders, and vertebral fracture instability, minimally invasive PBK is helpful to promote the effective recovery of injured vertebral body height and effectively maintain the stability of a fractured spine 8 , 9 . In addition, through the effective regulation of spinal cord nerve compression, it is helpful to promote the rapid recovery of spinal nerve function and the prognosis of patients. However, clinical practice shows that PBK has a good therapeutic effect only for patients with local vertebral fractures, but for patients with primary osteoporosis, its treatment has certain limitations 8 . In the theory of traditional Chinese medicine, osteoporosis belongs to the scope of bone flaccidity. Therefore, during the treatment of patients with osteoporotic compression fracture, in order to ensure its therapeutic effect, it should also be combined with the treatment of tonifying the kidney and strengthening the bone.
Significance of PKP in the Vertebral Compression Fractures
At present, PKP has the characteristics of less trauma and exact treatment effect, which makes it widely used in the treatment of osteoporotic vertebral compression fractures. The indications of PKP in the treatment of osteoporotic vertebral compression fractures are relatively broad, except for patients with nerve root injury, spinal cord injury, intolerance to surgery, and coagulation dysfunction caused by vertebral fracture 9 , 10 . In PKB, through the establishment of the corresponding pedicle working channel 2 into the injured vertebrae, the balloon device was placed in the area and expanded accordingly, so as to effectively restore the height of the injured vertebrae and significantly correct the convex deformity. After the satisfactory correction effect is achieved, the bone cement is injected into the cavity formed by the expansion of the balloon. The bearing capacity of the bone cement after solidification can provide reliable support for the injured vertebrae 9 , 10 , 11 .
Effect of Jintinage Capsules on Cobb's Angle, Vertebral Height, and Bone Mineral Density
In the present study, compared with the control group, the total effective rate of the study group was significantly increased. The vertebral height and bone mineral density were higher while the Cobb's angle was lower in the study group than in the control group after treatment. The results showed that for patients with osteoporotic vertebral compression fracture after PKP treatment, Jintange capsules can effectively restore the vertebral height, have a good correction effect on Cobb's angle, and can significantly improve bone mineral density, which is conducive to the prognosis of patients. The results of the current study are consistent with the previously reported studies in which the Jintiange capsules improved the bone mineral density and facilitate the healing process 1 , 2 .
In the theory of traditional Chinese medicine, renal anomalies are the main pathogenesis of fracture caused by osteoporosis. Due to the invasion of exogenous pathogenic factors, the deficiency of kidney essence leads to the failure of its function of storing essence and generating marrow. Bone and bone marrow lose nutrition, which can easily lead to fracture 12 , 13 . Jintiange capsules are one of the natural tiger bone substitutes. They are effective for dispelling wind, relieving pain, and strengthening bone. At the same time, they can promote the significant increase of bone mineral density and significantly improve the maximum stress, load, and bone mineral salt of femur, so as to strengthen the effect of bone resistance to external force impact 12 , 13 . In addition, Jintiange capsules can also promote the significant improvement of serum calcium, osteocalcin, and alkaline phosphatase, thus accelerating bone formation. Besides, they can significantly reduce the level of urinary hydroxyproline, prevent bone absorption, and significantly reduce the collagen decomposition 13 . Some scholars believed that as animal bone is the main raw material of Jintiange capsules, its bone collagen and calcium content are relatively rich, so it can have a better anti‐osteoporosis effect 13 , 14 , 15 .
Effect of Jintinage Capsules on VAS and ODI
In the present study, compared with the control group, the VAS and ODI of the study group were lower than the control group at 1 month and 3 months after treatment. The results showed that for patients with osteoporotic vertebral compression fracture after PKP treatment, Jintiange capsules can reduce the pain of patients, significantly improve the dysfunction of daily activities, and the long‐term effect is relatively good. The results of the present study showed a similar pattern in term of VAS and ODI improvement following treatment with the Jintiange capsules in different osteoporotic models 1 , 2 .
In treating patients with osteoporotic vertebral compression fracture after PKP treatment, the pharmacological effects of Jintiange capsules mainly include the following aspects: the content of bone collagen polypeptide in Jintange capsules is relatively high, which can promote the obvious improvement of bone, and this is conducive to joint health and can promote the significant relief of pain; Jintange capsules can effectively stimulate the proliferation of osteoblasts and enhance their activity, having a good inhibitory effect on osteoclasts; the contents of organic calcium and microelements needed by bone are relatively high in this drug and are easily absorbed; Jintange capsules have good remission effect for upper limb numbness, low back pain, and dizziness caused by osteoarthritis; Jintange capsules are easy to take, and their adverse reactions are small, so that the patient's tolerance is high, thus promoting the significant improvement of patient's medication compliance 16 , 17 , 18 .
Clinical Outcome
For the treatment of osteoporotic vertebral compression fracture, the use of Jintiange capsules is helpful to improve clinical symptoms and treatment effect, and they have high clinical application value.
Limitation of the Study
As for the limitations of the study, the adverse effect of the Jintiange capsules was not properly conceptualized in the present study. Furthermore, the study population and follow‐up should be increased to draw a clear conclusion.
Conclusion
In conclusion, for patients with osteoporotic vertebral compression fracture, Jintiange capsules can significantly improve the clinical efficacy rate, improve vertebral height, Cobb's angle, and bone mineral density, relieve pain, and promote daily activity function, which is conducive to clinical application and promotion.
References
- 1. Lin J, Qian L, Jiang C, et al. Bone cement distribution is a potential predictor to the reconstructive effects of unilateral percutaneous kyphoplasty in OVCFs: a retrospective study. J Orthop Surg Res, 2018, 13: 140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sun J, Yang XG, Hu YC. Efficacy of Jintiange capsules in the treatment of osteoporosis: a network meta‐analysis. Orthop Surg, 2019, 11: 176–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Li‐You W, Hong‐Wei Z, Jin‐Zeng Z, Su‐Miao X, Liang L, et al. Effect of Jintiange capsule on acute bone atrophy resulting from wrist fractures: a randomized controlled trial. J Acute Dis, 2020, 9: 51–55. [Google Scholar]
- 4. Wang Y, Liu J, Hou YX. Correlation between microangiopathy and bone mineral density in patients with type 2 diabetes. Chin J Osteoporosis, 2018, 24: 239–243. [Google Scholar]
- 5. Liu KC, Li SL, Zhao XY. Effect of Bushen Jiangu Decoction assisted vertebroplasty on bone mineral density and lumbar function in elderly patients with osteoporotic compression fracture. Liaoning J Traditi Chin Med, 2018, 45: 765–767. [Google Scholar]
- 6. Huang C, Huang H, AI Z. Chinese herbal medicines for rheumatoid arthritis. Chin Arch Tradit Chin Med, 2018, 36: 719–722. [Google Scholar]
- 7. Wang WF, Lin CW, Xie CN. The association between sarcopenia and osteoporotic vertebral compression refracture. Osteoporos Int, 2019, 30: 2459–2467. [DOI] [PubMed] [Google Scholar]
- 8. Zhao L, Zhang K, Cao C. Treatment of severe osteoporotic vertebral compression fractures with internal medicine by unilateral approach in lateral decubitus position. Chin J Trauma, 2019, 35: 693–699. [Google Scholar]
- 9. Zhu D, Shang CF, Liu HJ. Kyphoplasty with movement and secondary enlargement of balloon for compression fracture of vertebral body with im‐complete posterior wall. Chin J Orthop, 2019, 39: 737–746. [Google Scholar]
- 10. Yang CC, Chien JT, Tsai TY. Earlier Vertebroplasty for osteoporotic thoracolumbar compression fracture may minimize the subsequent development of adjacent fractures: a retrospective study. Pain Physician, 2018, 21: 483–491. [PubMed] [Google Scholar]
- 11. Liang X, Zhong W, Luo X, Quan Z. Risk factors of adjacent segmental fractures when percutaneous vertebroplasty is performed for the treatment of osteoporotic thoracolumbar fractures. Sci Rep, 2020, 10: 399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhao Y, Li A, Ni L, Wang W, Shi X. The research progress of tiger bone and artificial tiger bone for the treatment of osteoporosis. Chin J Osteoporosis, 2012, 16: 95–98. [Google Scholar]
- 13. Chen XW, Yang JS, Guo JH. Analysis of the curative effect of vertebroplasty with unilateral and bilateral hydraulic conveying high viscosity bone cement in the treatment of osteoporotic vertebral compression fracture. Guangdong Med J, 2019, 40: 941–946. [Google Scholar]
- 14. Yehong L, Lin W. Changes in inflammatory factors in patients with osteoporotic vertebral compression fracture and influences of rehabilitation training on postoperative functional recovery and inflammation. J Musculoskelet Neuronal Interact, 2018, 18: 272–279. [PMC free article] [PubMed] [Google Scholar]
- 15. Li Q, Chen C, Ma X. Progress of orthopaedic research in China over the last decade. Chin J Orthop Trauma, 2020, 22: 355–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Huang ZF, Xiao SX, Liu K. Effectiveness analysis of percutaneous kyphoplasty combined with zoledronic acid in treatment of primary osteoporotic vertebral compression fractures. Pain Physician, 2019, 22: 63–68. [PubMed] [Google Scholar]
- 17. Zhagn M, Liu Y, Tan JF. Comparison of percutaneous kyphoplasty, zoledronic acid or both in the treatment of senile osteoporotic lumbar vertebral compression fractures. Chin J Tissue Eng Res, 2019, 23: 2479–2485. [Google Scholar]
- 18. Arabmotlagh M, Nikoleiski SC, Schmidt S, Rauschmann M, Rickert M, Fleege C. Radiological evaluation of kyphoplasty with an intravertebral expander after osteoporotic vertebral fracture. J Orthop Res, 2019, 37: 457–465. [DOI] [PubMed] [Google Scholar]


