Abstract
A). Purpose of Review
In this review, we provide a recent update on bioenergetic pathways in osteocytes and identify potential future areas of research interest. Studies have identified a role for regulation of bone formation and bone resorption through osteocyte mechanosensing and osteocyte secreted factors, placing an emphasis on the energy metabolism of bone cells like chondrocytes, osteoblasts and osteoclasts. Nevertheless, there is a paucity of studies on the bioenergetics and energy metabolism of osteocytes, which are required for the regulation of bone remodeling.
B). Recent findings
Osteocytes are cells of the osteoblast lineage embedded in bone. The osteocyte lacunocanalicular network within the skeletal matrix is exposed to a unique hypoxic environment. Therefore, the bioenergetic requirements of these cells could differ from other bone cells due to its location in the ossified matrix and its role in bone regulation transduced by mechanical signals. Recent findings provide some evidence that metabolism of these cells is dependent on their location due to the substrates present in the microenvironment and metabolic cues from stress pathways. Both glycolysis (glucose metabolism) and oxidative phosphorylation (mitochondrial dynamics, ROS generation) affect osteocyte function and viability.
C). Summary
There is some evidence that glucose metabolism in osteocytes can be driven by hypoxia. The role of PTH and PTHrP in bone anabolism and resorption, along with glucose transport and glycolytic mechanisms need to be explored further in osteocytes in homeostasis and disease models. Mitochondrial metabolism has a role in osteocyte bioenergetics through substrate utilization, location of the osteocyte in the bone cortex and mitochondrial biogenesis. While there are limitations in studying metabolic flux in traditional cell lines, there are now novel cell lines and sophisticated tools available to study osteocyte bioenergetics to help harness its potential in vivo in the future.
Keywords: Osteocytes, glycolysis, oxidative phosphorylation, mitochondria, metabolism
2). Introduction
To maintain skeletal architecture throughout adult life there is orchestrated coordination between osteoblasts, osteocytes, osteoclasts, hematopoietic stem cells and bone marrow adipocytes in the bone microenvironment [1]. The remodeling of bone architecture is mediated by the osteoclasts and the osteoblasts with regulation from the osteocytes. A study has estimated that there are on an average about ~42 billion osteocytes in an adult human skeleton [2], making them the most abundant skeletal cells. Osteocytes help maintain cortical and trabecular bone through coordinating bone resorption by osteoclasts and bone formation by osteoblasts in response to mechanical loading [3]. Osteocytes sense mechanical forces in bone and can coordinate both bone formation and resorption by secreting factors like sclerostin (SOST) and receptor activator of nuclear factor Кappa-B ligand (RANKL) among other cytokines [4]. Within the mineralized bone matrix, osteocytes occupy ossified and encased spaces called lacunae. Osteocytes network through small channels called canaliculi, which are established in the ossified bone, leading to the development of the lacunocanalicular system. This system enables communication between osteocytes and other bone cells, due to the dendritic projections of the osteocytes and their gap junctions, leading to integration of mechanical signals [4, 5]. They culminate in the periosteal and endocortical surfaces of cortical bone. Signaling between the osteocyte cells and secretion of factors is primarily through this network of lacunae and canaliculi.
Apart from morphological changes to osteocytes, there are also changes to their gene and protein expression patterns during differentiation. Genes that are primarily involved in osteoblast function like collagen I type A1 (COL1A1) and alkaline phosphatase (ALP) are downregulated while dentin matrix protein 1 (DMP1) and SOST, which are osteocyte specific genes, are upregulated. SOST is a negative regulator of the Wnt (Wingless) signaling pathway and controls Wnt induced bone formation [6, 7]. In bone, SOST production is mostly limited to osteocytes. It functions through reducing the availability of the co-receptor, low-density lipoprotein receptor-related protein 5/6 (LRP5/6 receptor) for Wnt ligands [8]. Loss of SOST causes sclerosteosis and Van Buchem disease, leading to increased bone mineral density [9]. SOST also increases adipogenesis and has a positive effect on bone marrow adipogenesis. Thus, SOST and Wnt have a bone–adipose interaction by enabling alterations in both catabolic and anabolic metabolism [10]. These observations have resulted in using anti-Sclerostin antibody therapy as a treatment for postmenopausal osteoporosis [11, 12]. Osteocyte secreted factors also regulate local and systemic calcium and phosphate metabolism to control mineralization. These include proteins like DMP1, matrix extracellular phosphoglycoprotein (MEPE), phosphate-regulating gene with homologies to endopeptidases on the X chromosome (PHEX), and fibroblast growth factor 23 (FGF23) [13–16].
Osteocytes control osteoclastogenesis through the RANKL/RANK signaling pathway. Osteocytes secrete RANKL [17] in response to parathyroid hormone (PTH), which is the primary factor initiating osteoclastogenesis. Osteocytes can also secrete a decoy receptor for RANKL called osteoprotegerin (OPG), which is upregulated by SOST, further controlling osteoclastogenesis [18]. Osteocytes release calcium from bone during lactation through the process of osteocytic osteolysis in a parathyroid hormone 1 receptor (PTHR1) dependent manner. The expression of Cathepsin K, carbonic anhydrases, and other osteoclast related enzymes, along with acidification help in this process [19]. How all of these functional aspects of the osteocyte interact with their energetic needs have not been fully characterized.
2.1). Osteocyte Metabolism
As discussed in the above section, osteocyte function and activity are crucial for maintaining bone homeostasis and health through secreted factors that regulate osteoblasts and osteoclasts. RANKL and OPG secretion by osteocytes have an important role in mechanical unloading leading to bone resorption, while SOST and Dickkopf-related protein 1 (DKK1) , also derived from osteocytes, help regulate bone formation during mechanical loading [20]. Osteocytes have been implicated in regulating whole-body metabolism [21, 22]. Currently, however, not much is known about the metabolic pathways and substrates utilized by osteocytes. This section details the different energy sources used by osteocytes, including glucose, fatty acids, amino acids and intracellular substrates as energy sources to generate ATP.
2.2). Glucose Metabolism
Glucose catabolism is essential for the function and activity of chondrocytes, osteoblasts and osteoclasts. Based on the hypoxic nature of the osteocyte microenvironment, one could speculate that glucose metabolism and glycolysis could play an essential role in regulating osteocyte function. Cells in low oxygen environment upregulate molecular pathways that modulate metabolism by decreasing mitochondrial ATP generation, shifting metabolism to glycolysis and upregulating autophagy pathways [23–25]. In support of this, conditional mice lacking Von Hippel-Lindau (VHL) protein in osteocytes (10kb Dmp1-cre) exhibit a high bone mass phenotype (Figure 1) [26]. VHL is involved in oxygen dependent degradation of HIF1α. The role of this protein in osteocytes is thoroughly reviewed in [27, 28]. However, conditional deletion of Hif1α, a primary mediator of bone mass in osteoblasts did not result in high bone mass, suggesting that Hif2α or Hif independent pathways might play a role in the increased bone mass observed with VHL deletion [26]. Prolyl hydroxylase (PHD) involved in regulation of Hif-1α through detection of oxygen fluctuation, when targeted for knockout in osteocytes, has a role in high bone mass and bone formation (Figure 1) [29]. The effects of loss of VHL and PHD on osteocyte bioenergetic pathways, explicitly looking at glycolysis and oxidative phosphorylation and correlating the results with mitochondrial metabolic studies, should be informative. In a study by Yao et al., the authors generated a Hif1α conditional knock-out mouse line using Prxx1-cre to target mesenchymal stem cells involved in limb development and showed that Hif1α is required to maintain mitochondrial oxygen consumption at low levels by increasing glycolytic metabolism [30]. In the absence of Hif1α there is an increase in oxygen consumption that results in increased cell death in the growth plate. The phenotype observed with Prxx1-cre can be partially corrected by decreasing mitochondrial oxygen consumption with deletion of Tfam, a critical mitochondrial biogenesis transcriptional factor. They also identified a vital protein, BNIP3, as being upregulated in chondrocytes under hypoxic conditions [30]. BNIP3 is an important mitophagy receptor in many different tissues and we have recently shown its role in regulating intervertebral disc mitophagy pathways [31]. The potential role of this protein in autophagy pathways downstream of EphrinB2 signaling in osteocytes was recently described. In that paper, the dysregulated expression of several autophagy related genes resulted in increased secondary mineralization in the absence of EphrinB2 (Figure 1) [32]. Since BNIP3 expression is controlled by hypoxia in vitro in osteocytes [33], it will be essential to identify which factors control BNIP3 transcriptionally in the osteocyte and how it interacts with the bioenergetic program of an osteocyte.
Figure 1: Overview of bioenergetic pathways in the osteocyte:
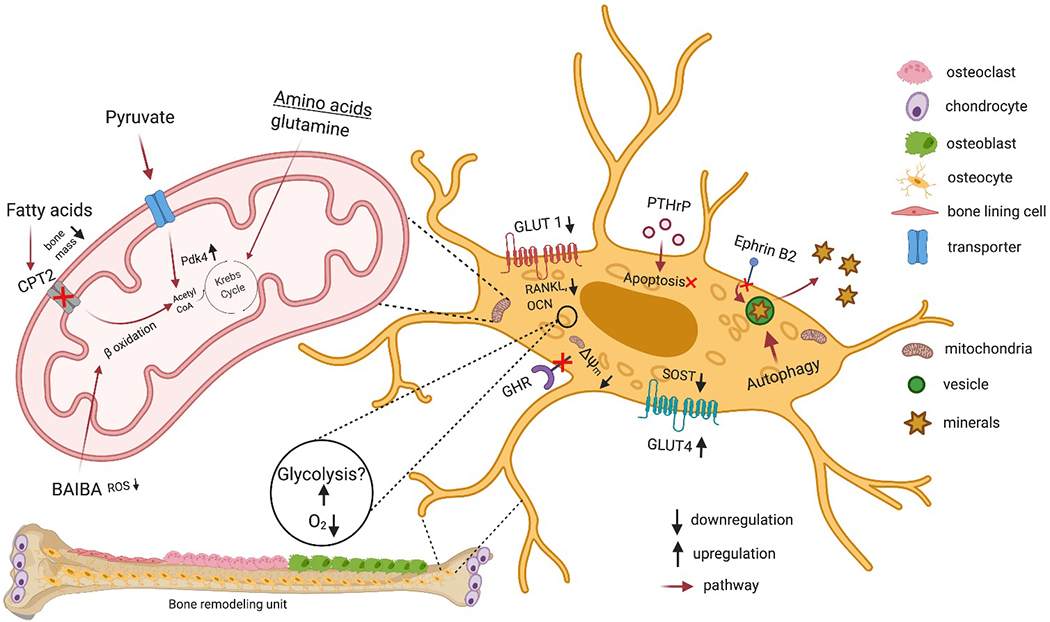
The location of the osteocytes embedded in the lacunae creates a uniquely hypoxic environment that could lead to upregulation of glycolytic pathways. HIF-α regulation leads to increase in bone mass. In osteocytes when GLUT1 is inhibited it reduces osteocalcin and RANKL expression as depicted in the figure, while SOST inhibition leads to glucose uptake through GLUT4. Growth hormone receptor (GHR) is necessary for maintaining mitochondrial function and mitochondrial membrane potential (Δψm) in osteocytes. Based on the studies showing PTH effects on glycolysis and oxidative phosphorylation it will be important to study the role of PTH induced metabolism in osteocytes. The role of amino acids, pyruvate and fatty acids on mitochondrial metabolism in osteocytes need to be addressed. Intracellular substrates potentially generated through autophagy pathways can also regulate secondary mineralization pathways. BAIBA secreted by muscle acts on osteocytes to mitigate ROS generation, mitochondria breakdown and increase viability. Created with BioRender.com
It is currently not clear which of the glucose transporters is essential for osteocytes. Some recent studies have addressed this very question using specific glucose transporter inhibitors [34, 35]. In a study by Takeno et al., [34] the authors used phloretin to inhibit GLUT1 mediated glucose uptake in the murine osteocyte-like cell line, MLO-Y4. The authors suggest that lowering glucose uptake into osteocytes may contribute to maintaining blood glucose levels by decreasing osteocalcin expression and RANKL-induced bone resorption (Figure 1). Another study using Scriptaid, an HDAC co-repressor inhibitor, which suppressed SOST in osteocytes and increased genes involved in glucose uptake, showed upregulation in GLUT4 (Figure 1) [35]. There are now conditional alleles available for the various Glut transporters and these have been deleted in mesenchymal stem cells, chondrocytes, osteoblasts and osteoclasts [36–39]. Use of Dmp1-cre driver mice could help identify a role for the GLUT family of transporters and glucose metabolism in osteocytes.
PTH in osteoblasts increases glucose uptake and aerobic glycolysis, increasing lactate production [40]. The role of PTHR1 in lactation-induced acidification has been shown in osteocytes [19]. However, what is not known is if there is an increase in glycolysis driven ATP generation to fuel this process. It will be interesting to study if this process is similar to the lysosomal vacuolar ATPase driven bone resorption that uses both glycolysis and oxidative phosphorylation by osteoclasts [39].
One of the first studies to measure oxidative phosphorylation and glycolysis in osteocytes was from Liu et al; studying growth hormone receptor (GHR) signaling in mice [41]. In that study, they isolated primary osteocytes from bones of Ghr knockout mice and performed XF24 seahorse assays. They also performed multi-photon microscopy analysis to measure mitochondrial membrane potential in vivo, in primary osteocytes and metatarsals, and showed decreased mitochondrial membrane potential (Figure 1). Ghr knockout osteocytes overall exhibited decreased mitochondrial function [41]. This was one of the first studies to provide a comprehensive overview of the bioenergetic pathways of the osteocytes under different conditions.
Glucose metabolism in disease
Hyperglycemia affects not only the rate of glycolysis, but also osteocyte viability. SOST, a specific antagonist to Wnt pathway, increases during dysfunctional glycolytic metabolism involving high glucose and advanced glycation end products (AGEs) [42]. As hyperglycemia and oxidative stress are involved in AGE production and accumulation, it has been found in vitro that FOXO1 can mediate the AGE-induced osteocyte apoptosis along with osteoblast and osteoclast dysregulation [43]. A recent study also found that restricted glucose triggered the AMPK/PGC-1 pathway during differentiation of osteoblasts to osteocytes, which led to higher mitochondrial DNA levels and increased osteocyte gene expression [44]. The role of PTH on both glucose and fatty acid metabolism has been described in osteoblasts [40, 45]. PTHrP also upregulates mitochondrial metabolism in adipocytes [46]. In a study that used streptozotocin-induced T1D model in mice, treatment with parathyroid hormone-related protein (PTHrP) peptides attenuates osteocyte apoptosis and shows considerable improvement in bone mass and strength (Figure 1) [47]. The diabetic mice treated with different PTHrP peptides showed improvement, but blood glucose levels did not decrease. The mechanism through which PTHrP functioned was shown to be through regulating β-catenin and Erk mediated pathways [47]. It might be interesting to study how these treatments affected the bioenergetics profile and mitochondrial metabolism in osteocytes.
2.3). Mitochondrial metabolism
Mitochondria are critical for the execution of multiple cellular metabolic processes. Through the Krebs cycle, pyruvate derived from glycolysis, fatty acids and amino acid breakdown takes place to generate adenosine triphosphate (ATP), reactive oxygen species (ROS) and small molecule metabolites necessary for maintaining calcium homeostasis and inter-organelle communication. All of these functions are dependent on the ability of mitochondria to engage in oxidative phosphorylation for ATP generation. However, control of mitochondrial respiration in skeletal cells in the bone marrow niche is dependent on oxygen levels, which are relatively low (hypoxia, <45mmHg) in the bone marrow niche (9-32 mmHg) [48]. Maintaining mitochondrial dynamics and function in this specialized niche ultimately controls cell fate and differentiation. For example, osteocyte mitochondrial-derived ROS plays a significant role in osteocyte viability [49].
Exercise-induced factors secreted by muscle, including β-aminoisobutyric acid (BAIBA), could mitigate ROS generation and mitochondrial breakdown in osteocytes and increase osteocyte viability (Figure 1) [50]. Transmission electron microscopy images of osteocytes indicate that that there are significant number of mitochondria in osteocytes and studies using labeled mitochondrial trackers show robust mitochondrial activity in osteocytes [51, 52]. Metabolic profiles and activity of the osteocyte is also dependent on location. Osteocytes at the cortical surface of the bone show a higher glycolytic profile. Multi-photon microscopy shows that there is a difference in mitochondrial content and activity based on the location of the osteocytes in the bone cortex. While there are active mitochondria in the osteocytes near the periosteum, many dysfunctional mitochondria are also found near the endosteum [23]. Differentiation of osteoblasts leads to osteocyte formation, which also brings about a bioenergetic metabolism shift, as shown by Lee et al., where differentiated osteocytes from periosteum-derived mesenchymal stem cells (POMSC) led to a higher mtDNA content and respiratory chain protein expression in the differentiated osteocytes, along with lower lactate levels [53]. Based on some of the above studies mitochondrial metabolism could be a key driver of bioenergetic pathways in an osteocyte.
One recent study suggested that glucose restriction resulted in an increase in mitochondrial biogenesis mediated by increased activity of the PGC1α transcriptional factor [44]. The cues for differentiation seem to be substrate restriction based on this study. Cyclophilin D, which regulates the mitochondrial permeability transition pore (MPTP), plays a significant role in aging by protecting against bone loss and osteocyte mitochondrial dysfunction. For example, in Cyclophilin D knockout mice, it has been shown that oxidative metabolism is impaired in aging bone leading to a glycolytic shift, poor nucleotide levels, and reduced NAD+/NADH ratio [54]. It is not clear if this is sufficient to regulate mitochondrial biogenesis, dynamics and turnover in osteocytes.
Based on the hypoxic environment osteocytes encounter especially in cortical bone [55], one can argue that the mechanisms that the chondrocytes in the growth plate employ can be used to understand osteocyte bioenergetics. However, there are significant differences in the vasculature, and based on some of the studies discussed above this could potentially be only a subset of osteocytes that are deeply embedded in the cortex. Osteoblasts seem to prefer aerobic glycolysis under certain conditions [56, 57], and if osteocytes show a similar metabolic profile, one could predict that mitochondrial metabolism should be modified to factor in those changes. These would include changes in mitochondrial substrate utilization, mitochondrial turnover and ATP generation. Studies performed to study osteocyte bioenergetics should include experiments to factor in all these different parameters to obtain a complete picture of the osteocyte metabolic profile.
Pyruvate
Pyruvate generated from glycolysis enters the mitochondria through mitochondrial pyruvate transporters, however, the role of these transporters in osteocytes is currently unknown. There is some information regarding the role of pyruvate dehydrogenase kinase 4 in regulating bone mass, specifically when the osteocyte network is dysfunctional (Figure 1) [58]. With the recent discovery of the pyruvate transporter genes and new mouse strains available, opportunities now exist to study how pyruvate affects osteocyte metabolism [59, 60].
Fatty acid metabolism
Skeletal tissue can uptake a significant amount of fatty acids [61]. Saturated fatty acids have been implicated in the induction of osteocyte apoptosis [62, 63]. A study in mice exploring the role of fatty acid oxidation in mitochondria found that by ablating the expression of carnitine palmitoyltransferase-2 (Cpt2) in osteoblasts and osteocytes resulted in low bone mass in females (Osteocalcin-cre was utilized in this study, which targets both osteoblasts and osteocytes) [64]. Labeled bromopalmitate and oleate uptake experiments showed that a significant amount of label was retained in the femur’s cortical bone envelope, suggesting utilization of fatty acids for catabolic process. CPT2 is one of the enzymes required for long-chain fatty acid β-oxidation. Deletion of Cpt2 and impaired fatty acid metabolism in osteoblasts and osteocytes also resulted in changes in whole-body adiposity [64] (Figure 1). It is difficult to interpret this result with relation to osteocytes as the Cre recombinase also targets mature osteoblasts; however, targeting some of the fatty acid metabolism genes specifically using the Dmp1-cre may provide more insights about osteocyte bioenergetics in the future.
Amino acid metabolism
The role of dietary proteins on bone mass in humans and rodents has been studied previously [65–67]. Osteoblasts and osteoclasts can respond to amino acids by increasing uptake and utilizing them for both energy generation and protein synthesis. The role of glutamine, a non-essential amino acid has recently been shown to be crucial for chondrocyte growth and survival. Glutamine metabolism stimulated by the master chondrogenic transcriptional factor SOX9 controlled multiple aspects of chondrocytes, including gene expression, matrix production, proliferation, and ROS mitigation [68]. A study from the Karner laboratory has shown that skeletal stem cells require glutamine metabolism for proper lineage allocation and osteoblast differentiation [69]. The role of glutamine metabolism in osteocytes could potentially be an interesting area to investigate. A study by Shen et al., have identified γ(+)-LAT1 and ASCT2 as primary glutamine transporters that are necessary for osteoblast differentiation [70]. Nevertheless, it is currently not clear how osteocytes utilize amino acids for energy needs. More recently, a study identified an increase in the receptor for taurine uptake during osteocyte differentiation. Increased taurine uptake through taurine transporters in an in vitro osteocyte cell model IDGSW3 is protective from oxidative damage [71]. This study also identified an increase in taurine synthesis by osteocytes during differentiation with a decrease in methionine, a precursor for taurine.
Intracellular substrates as energy sources
Studies have highlighted the reliance of osteoblasts on autophagy [72–74] to not only fuel bioenergetic demands of osteoblasts but also favor mineralization [75]. Autophagy, the process through which cellular components are recycled in response to starvation or stress, plays a significant role in osteoblast to osteocyte transition [25, 76]. Initial studies deleting ATG7, an essential autophagy gene using the Dmp1-cre driver resulted in a low bone mass phenotype [77]. More recently, autophagy in the osteocyte has been shown to be crucial to regulate secondary mineralization [32]. In vitro studies assessing the role of autophagy in cell viability of osteocytes have been shown [78, 79]. Both studies concluded that induction of autophagy was necessary for cell viability; either to offset damage due to mechanical stress [78], or induction of apoptosis due to glucocorticoid administration [79]. The role proposed for mitochondrial- associated autophagy (mitophagy) and lysosomal acidification for mineralization in osteoblast-like cells [80, 81], and the role of exosome derived vesicles from different organelles and how they affect metabolism needs more attention.
3). Conclusions and future directions:
The importance of osteocyte to maintain skeletal health has been established over the last two decades. There is now emerging interest in identifying the metabolic pathways in these cells and if they have any unique properties based on their location in a specialized niche. Current research is ongoing to identify the metabolic pathways active in the osteocytes, looking at both glycolytic and mitochondrial metabolism, but more work needs to be done to identify the bioenergetics pathways in these cells to get a complete picture of their metabolism. Some of the challenges that we have come across when studying cell lines in vitro on an XF96 Agilent seahorse platform is the difficulty in having an adherent monolayer of cells for a sufficient amount of time to complete an experimental run. With the recent generation of cell lines that are GFP tagged and can form 3-dimensional bone like structures with the osteocytes embedded in them might yield better results [82].
There are currently many new sophisticated techniques that have been used to study osteocyte function in vivo using two-photon and three-photon microscopy techniques [83, 84]. Coupled with metabolomics, we may be able to identify metabolic pathways engaged by osteocytes during differentiation and gain a clearer understanding of osteocyte bioenergetics. It will be important to harness these techniques to study osteocyte bioenergetics in vivo in the future.
4). Acknowledgements:
This work was funded by NIGMS to A.R.G. through P20GM121301, Phase I: Mesenchymal and Neural Regulation of Metabolic Networks, Lucy Liaw, PhD, Program Director and start up research fund from MMCRI to A.R.G. We would also like to apologize to all the authors whose work could not be cited due to space constraints.
Footnotes
Disclosure Statement: The authors have nothing to disclose
References
- 1.Capulli M, Paone R, and Rucci N, Osteoblast and osteocyte: games without frontiers. Arch Biochem Biophys, 2014. 561: p. 3–12. [DOI] [PubMed] [Google Scholar]
- 2.Buenzli PR and Sims NA, Quantifying the osteocyte network in the human skeleton. Bone, 2015. 75: p. 144–50. [DOI] [PubMed] [Google Scholar]
- 3.Bakker AD, et al. , IL-6 alters osteocyte signaling toward osteoblasts but not osteoclasts. J Dent Res, 2014. 93(4): p. 394–9. [DOI] [PubMed] [Google Scholar]
- 4.Bonewald LF, The amazing osteocyte. J Bone Miner Res, 2011. 26(2): p. 229–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dallas SL, Prideaux M, and Bonewald LF, The osteocyte: an endocrine cell ... and more. Endocr Rev, 2013. 34(5): p. 658–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winkler DG, et al. , Osteocyte control of bone formation via sclerostin, a novel BMP antagonist. EMBO J, 2003. 22(23): p. 6267–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin C, et al. , Sclerostin mediates bone response to mechanical unloading through antagonizing Wnt/beta-catenin signaling. J Bone Miner Res, 2009. 24(10): p. 1651–61. [DOI] [PubMed] [Google Scholar]
- 8.Li X, et al. , Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling. J Biol Chem, 2005. 280(20): p. 19883–7. [DOI] [PubMed] [Google Scholar]
- 9.Balemans W, et al. , Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Human Molecular Genetics, 2001. 10(5): p. 537–544. [DOI] [PubMed] [Google Scholar]
- 10.Kim SP, et al. , Sclerostin influences body composition by regulating catabolic and anabolic metabolism in adipocytes. Proc Natl Acad Sci U S A, 2017. 114(52): p. E11238–E11247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McClung MR, et al. , Effects of 24 months of treatment with romosozumab followed by 12 months of denosumab or placebo in postmenopausal women with low bone mineral density: a randomized, double-blind, phase 2, parallel group study. J Bone Miner Res, 2018. 33(8): p. 1397–1406. [DOI] [PubMed] [Google Scholar]
- 12.Geusens P, et al. , The effect of 1 year of romosozumab on the incidence of clinical vertebral fractures in postmenopausal women with osteoporosis: results from the FRAME study. JBMR Plus, 2019. 3(10): p. e10211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nampei A, et al. , Matrix extracellular phosphoglycoprotein (MEPE) is highly expressed in osteocytes in human bone. J Bone Miner Metab, 2004. 22(3): p. 176–84. [DOI] [PubMed] [Google Scholar]
- 14.Toyosawa S, et al. , Dentin matrix protein 1 is predominantly expressed in chicken and rat osteocytes but not in osteoblasts. J Bone Miner Res, 2001. 16(11): p. 2017–26. [DOI] [PubMed] [Google Scholar]
- 15.Ubaidus S, et al. , FGF23 is mainly synthesized by osteocytes in the regularly distributed osteocytic lacunar canalicular system established after physiological bone remodeling. J Electron Microsc (Tokyo), 2009. 58(6): p. 381–92. [DOI] [PubMed] [Google Scholar]
- 16.Miyagawa K, et al. , Dysregulated gene expression in the primary osteoblasts and osteocytes isolated from hypophosphatemic Hyp mice. PLoS One, 2014. 9(4): p. e93840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakashima T, et al. , Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med, 2011. 17(10): p. 1231–4. [DOI] [PubMed] [Google Scholar]
- 18.Wijenayaka AR, et al. , Sclerostin stimulates osteocyte support of osteoclast activity by a RANKL-dependent pathway. PLoS One, 2011. 6(10): p. e25900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **19.Jähn K, et al. , Osteocytes acidify their microenvironment in response to PTHrP in vitro and in lactating mice in vivo. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research, 2017. 32(8): p. 1761–1772. [DOI] [PMC free article] [PubMed] [Google Scholar]; This interesting study points to a potential role for glycolytic pathways in regulating osteolytic osteolysis
- 20.Goldring SR, The osteocyte: key player in regulating bone turnover. RMD Open, 2015. 1(Suppl 1): p. e000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brun J, et al. , Bone regulates browning and energy metabolism through mature osteoblast/osteocyte PPARgamma expression. Diabetes, 2017. 66(10): p. 2541–2554. [DOI] [PubMed] [Google Scholar]
- 22.Sato M, et al. , Osteocytes regulate primary lymphoid organs and fat metabolism. Cell Metab, 2013. 18(5): p. 749–58. [DOI] [PubMed] [Google Scholar]
- 23.Frikha-Benayed D, et al. , Regional differences in oxidative metabolism and mitochondrial activity among cortical bone osteocytes. Bone, 2016. 90: p. 15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo D, et al. , Identification of osteocyte-selective proteins. Proteomics, 2010. 10(20): p. 3688–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zahm AM, et al. , Bone cell autophagy is regulated by environmental factors. Cells Tissues Organs, 2011. 194(2–4): p. 274–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **26.Loots GG, et al. , Vhl deficiency in osteocytes produces high bone mass and hematopoietic defects. Bone, 2018. 116: p. 307–314. [DOI] [PubMed] [Google Scholar]; This is the first study to target the oxygen sensing system in osteocytes.
- 27.Maxwell PH, et al. , The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature, 1999. 399(6733): p. 271–5. [DOI] [PubMed] [Google Scholar]
- 28.Yellowley CE and Genetos DC, Hypoxia signaling in the skeleton: implications for bone health. Current osteoporosis reports, 2019. 17(1): p. 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stegen S, et al. , Osteocytic oxygen sensing controls bone mass through epigenetic regulation of sclerostin. Nat Commun, 2018. 9(1): p. 2557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yao Q, et al. , Suppressing mitochondrial respiration is critical for hypoxia tolerance in the fetal growth plate. Dev Cell, 2019. 49(5): p. 748–763 e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Madhu V, et al. , Hypoxic regulation of mitochondrial metabolism and mitophagy in nucleus pulposus cells is dependent on HIF-1alpha-BNIP3 Axis. J Bone Miner Res, 2020. 35(8): p. 1504–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **32.Vrahnas C, et al. , Increased autophagy in EphrinB2-deficient osteocytes is associated with elevated secondary mineralization and brittle bone. Nat Commun, 2019. 10(1): p. 3436. [DOI] [PMC free article] [PubMed] [Google Scholar]; This interesting study points to a potential role for autophagy in regulating secondary mineralization.
- 33.Zahm AM, et al. , Oxygen tension regulates preosteocyte maturation and mineralization. Bone, 2008. 43(1): p. 25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takeno A, et al. , Glucose uptake inhibition decreases expressions of receptor activator of nuclear factor-kappa B ligand (RANKL) and osteocalcin in osteocytic MLO-Y4-A2 cells. Am J Physiol Endocrinol Metab, 2018. 314(2): p. E115–E123. [DOI] [PubMed] [Google Scholar]
- 35.Sun N, et al. , Effects of histone deacetylase inhibitor Scriptaid and parathyroid hormone on osteocyte functions and metabolism. J Biol Chem, 2019. 294(25): p. 9722–9733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fidler TP, et al. , Deletion of GLUT1 and GLUT3 reveals multiple roles for glucose metabolism in platelet and megakaryocyte function. Cell Rep, 2017. 21(6): p. 1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wei J, et al. , Glucose uptake and Runx2 synergize to orchestrate osteoblast differentiation and bone formation. Cell, 2015. 161(7): p. 1576–1591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee S-Y, Abel ED, and Long F, Glucose metabolism induced by Bmp signaling is essential for murine skeletal development. Nature Communications, 2018. 9(1): p. 4831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Li B, et al. , Both aerobic glycolysis and mitochondrial respiration are required for osteoclast differentiation. Faseb j, 2020. [DOI] [PubMed] [Google Scholar]
- 40.Esen E, et al. , PTH promotes bone anabolism by stimulating aerobic glycolysis via IGF signaling. Journal of bone and mineral research : the official journal of the American Society for Bone and Mineral Research, 2015. 30(11): p. 1959–1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **41.Liu Z, et al. , Mitochondrial function is compromised in cortical bone osteocytes of long-lived growth hormone receptor null mice. J Bone Miner Res, 2019. 34(1): p. 106–122. [DOI] [PMC free article] [PubMed] [Google Scholar]; One of the first published reports studying energetics in osteocytes.
- 42.Tanaka K, et al. , Effects of high glucose and advanced glycation end products on the expressions of sclerostin and RANKL as well as apoptosis in osteocyte-like MLO-Y4-A2 cells. Biochem Biophys Res Commun, 2015. 461(2): p. 193–9. [DOI] [PubMed] [Google Scholar]
- 43.Zhang C, et al. , FOXO1 mediates advanced glycation end products induced mouse osteocyte-like MLO-Y4 cell apoptosis and dysfunctions. J Diabetes Res, 2019. 2019: p. 6757428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sanchez-de-Diego C, et al. , Glucose restriction promotes osteocyte specification by activating a PGC-1alpha-dependent transcriptional program. iScience, 2019. 15: p. 79–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maridas DE, et al. , Progenitor recruitment and adipogenic lipolysis contribute to the anabolic actions of parathyroid hormone on the skeleton. Faseb j, 2019. 33(2): p. 2885–2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kir S, et al. , Tumour-derived PTH-related protein triggers adipose tissue browning and cancer cachexia. Nature, 2014. 513(7516): p. 100–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maycas M, et al. , PTHrP-derived peptides restore bone mass and strength in diabetic mice: Additive Effect of Mechanical Loading. J Bone Miner Res, 2017. 32(3): p. 486–497. [DOI] [PubMed] [Google Scholar]
- 48.Spencer JA, et al. , Direct measurement of local oxygen concentration in the bone marrow of live animals. Nature, 2014. 508(7495): p. 269–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kobayashi K, et al. , Mitochondrial superoxide in osteocytes perturbs canalicular networks in the setting of age-related osteoporosis. Sci Rep, 2015. 5: p. 9148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kitase Y, et al. , Beta-aminoisobutyric Acid, l-BAIBA, is a muscle-derived osteocyte survival factor. Cell Rep, 2018. 22(6): p. 1531–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boivin G, Anthoine-Terrier C, and Obrant KJ, Transmission electron microscopy of bone tissue. A review. Acta Orthop Scand, 1990. 61(2): p. 170–80. [DOI] [PubMed] [Google Scholar]
- 52.Gao J, et al. , Endoplasmic reticulum mediates mitochondrial transfer within the osteocyte dendritic network. Sci Adv, 2019. 5(11): p. eaaw7215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee AR, et al. , Involvement of mitochondrial biogenesis during the differentiation of human periosteum-derived mesenchymal stem cells into adipocytes, chondrocytes and osteocytes. Arch Pharm Res, 2019. 42(12): p. 1052–1062. [DOI] [PubMed] [Google Scholar]
- 54.Shum LC, et al. , Cyclophilin D knock-out mice show enhanced resistance to osteoporosis and to metabolic changes observed in aging bone. PLoS One, 2016. 11(5): p. e0155709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spencer JA, et al. , Direct measurement of local oxygen concentration in the bone marrow of live animals. Nature, 2014. 508(7495): p. 269–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guntur AR, et al. , Osteoblast-like MC3T3-E1 cells prefer glycolysis for ATP production but adipocyte-like 3T3-L1 cells prefer oxidative phosphorylation. J Bone Miner Res, 2018. 33(6): p. 1052–1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lee WC, et al. , Malic enzyme couples mitochondria with aerobic glycolysis in osteoblasts. Cell Rep, 2020. 32(10): p. 108108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang Y, et al. , Pyruvate dehydrogenase kinase 4 induces bone loss at unloading by promoting osteoclastogenesis. Bone, 2012. 50(1): p. 409–19. [DOI] [PubMed] [Google Scholar]
- 59.Vanderperre B, et al. , Embryonic lethality of mitochondrial pyruvate carrier 1 deficient mouse can be rescued by a ketogenic diet. PLoS Genet, 2016. 12(5): p. e1006056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vigueira PA, et al. , Mitochondrial pyruvate carrier 2 hypomorphism in mice leads to defects in glucose-stimulated insulin secretion. Cell Rep, 2014. 7(6): p. 2042–2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alekos NS, Moorer MC, and Riddle RC, Dual effects of lipid metabolism on osteoblast function. Front Endocrinol (Lausanne), 2020. 11: p. 578194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sekar S, et al. , Saturated fatty acids induce development of both metabolic syndrome and osteoarthritis in rats. Sci Rep, 2017. 7: p. 46457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Al Saedi A, et al. , Mechanisms of palmitate-induced lipotoxicity in osteocytes. Bone, 2019. 127: p. 353–359. [DOI] [PubMed] [Google Scholar]
- 64.Kim SP, et al. , Fatty acid oxidation by the osteoblast is required for normal bone acquisition in a sex- and diet-dependent manner. JCI Insight, 2017. 2(16). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Shams-White MM, et al. , Dietary protein and bone health: a systematic review and meta-analysis from the National Osteoporosis Foundation. Am J Clin Nutr, 2017. 105(6): p. 1528–1543. [DOI] [PubMed] [Google Scholar]
- 66.Rizzoli R, et al. , The role of dietary protein and vitamin D in maintaining musculoskeletal health in postmenopausal women: a consensus statement from the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). Maturitas, 2014. 79(1): p. 122–32. [DOI] [PubMed] [Google Scholar]
- 67.Rouy E, et al. , Protein quality affects bone status during moderate protein restriction in growing mice. Bone, 2014. 59: p. 7–13. [DOI] [PubMed] [Google Scholar]
- 68.Stegen S, et al. , Glutamine metabolism controls chondrocyte identity and function. Dev Cell, 2020. 53(5): p. 530–544 e8. [DOI] [PubMed] [Google Scholar]
- 69.Yu Y, et al. , Glutamine metabolism regulates proliferation and lineage allocation in skeletal stem cells. Cell Metab, 2019. 29(4): p. 966–978 e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shen L, et al. , Biphasic regulation of glutamine consumption by WNT during osteoblast differentiation. J Cell Sci, 2021. 134(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Prideaux M, et al. , Taurine, an osteocyte metabolite, protects against oxidative stress-induced cell death and decreases inhibitors of the Wnt/beta-catenin signaling pathway. Bone, 2020. 137: p. 115374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yang YH, et al. , Oxidative damage to osteoblasts can be alleviated by early autophagy through the endoplasmic reticulum stress pathway--implications for the treatment of osteoporosis. Free Radic Biol Med, 2014. 77: p. 10–20. [DOI] [PubMed] [Google Scholar]
- 73.Li H, et al. , Defective autophagy in osteoblasts induces endoplasmic reticulum stress and causes remarkable bone loss. Autophagy, 2018. 14(10): p. 1726–1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Xi G, Rosen CJ, and Clemmons DR, IGF-I and IGFBP-2 stimulate AMPK activation and autophagy, which are required for osteoblast differentiation. Endocrinology, 2016. 157(1): p. 268–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nollet M, et al. , Autophagy in osteoblasts is involved in mineralization and bone homeostasis. Autophagy, 2014. 10(11): p. 1965–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Piemontese M, et al. , Low bone mass and changes in the osteocyte network in mice lacking autophagy in the osteoblast lineage. Sci Rep, 2016. 6: p. 24262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Onal M, et al. , Suppression of autophagy in osteocytes mimics skeletal aging. J Biol Chem, 2013. 288(24): p. 17432–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang B, et al. , Mechanically induced autophagy is associated with ATP metabolism and cellular viability in osteocytes in vitro. Redox Biol, 2018. 14: p. 492–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zhu L, et al. , Parathyroid hormone (PTH) induces autophagy to protect osteocyte cell survival from dexamethasone damage. Med Sci Monit, 2017. 23: p. 4034–4040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pei DD, et al. , Contribution of mitophagy to cell-mediated mineralization: revisiting a 50-year-old conundrum. Adv Sci (Weinh), 2018. 5(10): p. 1800873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Iwayama T, et al. , Osteoblastic lysosome plays a central role in mineralization. Sci Adv, 2019. 5(7): p. eaax0672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **82.Wang K, et al. , A novel osteogenic cell line that differentiates into GFP-tagged osteocytes and forms mineral with a bone-like lacunocanalicular structure. J Bone Miner Res, 2019. 34(6): p. 979–995. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study provides a new cell model to test some of the bioenergtic pathways.
- 83.Tokarz D, et al. , Intravital imaging of osteocytes in mouse calvaria using third harmonic generation microscopy. PLoS One, 2017. 12(10): p. e0186846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Genthial R, et al. , Label-free imaging of bone multiscale porosity and interfaces using third-harmonic generation microscopy. Sci Rep, 2017. 7(1): p. 3419. [DOI] [PMC free article] [PubMed] [Google Scholar]


