Abstract
Objective:
To identify the risk factors for periodontal changes in adult patients during orthodontic treatment by evaluating the periodontal status of banded second molars using the gingival index (GI).
Material and Methods:
The sample consisted of 100 adult patients divided into two groups: the Orthodontics group, undergoing corrective treatment with fixed appliances and bands cemented to the four second molars, and the Control group, with no prior history of orthodontic treatment, age and sex matched. Group GI values were compared using the Wilcoxon test. Additionally, a multivariate logistic regression was performed to study the risk factors for increases in the GI.
Results:
Individuals in the Orthodontics group showed a significantly higher GI than those in the Control group. Logistic regression revealed that among the risk factors found to increase GI, the following proved significant (in order of importance): plaque index, subgingival encroachment of the cervical margins of bands, probing depth, and length of orthodontic treatment.
Conclusions:
Banded second molars of adult patients during orthodontic treatment showed more clinical signs of gingival inflammation than those of untreated individuals. Moreover, major risk factors identified included the presence of plaque and the presence of subgingival band margins.
Keywords: Orthodontic appliance, Molar, Periodontium, Adult, Risk factors
INTRODUCTION
Any patient undergoing orthodontic treatment should be extra careful with their oral hygiene,1–3 especially adults.2 The number of adult patients in treatment increased significantly during the 1980s,4,5 bringing with it malocclusions with their attendant age limitations6 and various aggravating periodontal conditions, ranging from lesions on one single tooth surface to generalized periodontal disease.2,4,5
However, it has been argued that age is not in itself a contraindication for orthodontic treatment4 because adult patients, in certain situations, may exhibit less plaque build-up and gingival inflammation than adolescents.6 Various factors have been suggested to explain these observations, such as the larger size of the clinical crown of adult teeth resulting from passive eruption, which allows brackets to be positioned farther away from the gingival margin.2 On the other hand, orthodontic appliances and accessories (bands, brackets, archwires, elastics, and springs) increase the number of areas of dental plaque retention and consequently hinder hygiene,7–13 particularly in the posterior segments of the oral cavity, given their difficult access. Permanent second molars are often misaligned and therefore are included in the treatment plan, thus increasing the potential for gingival inflammation.7,14 Technical and bonding difficulties often arise, leading professionals to resort to the use of bands.2,7,14
Gingivitis, especially in the region of the interdental papilla, has been observed in teeth banded for orthodontic purposes.4,15 These have been associated with higher plaque rates,3,7,9,14 gingival rates3,7,9,11,16–18 and probing depth,3,7,10,11,17,18 more often than in patients with bonded brackets or no orthodontic appliance.7,11,16 However, apparently gingival reactions are transient, and they do not cause permanent damage to periodontal tissues; rather, cases are rapidly resolved and treatment completed.10
Given that orthodontic appliances favor dental plaque retention, and that the number of adults undergoing orthodontic treatment has been growing considerably (which creates peculiar periodontal conditions), this study aimed to analyze the gingival index (GI) of banded second molars in adult patients and compare it with that of a control group. Additionally, investigators aimed specifically to detect the presence of possible predictive factors for increases in GI in patients treated with orthodontic bands on the second molars.
MATERIALS AND METHODS
A cross-sectional clinical study was conducted by examining maxillary and mandibular second molars of 100 adults (54 women, mean age 26 ± 7.5 years, and 46 men, mean age 23 ± 4.8 years). A group of 50 patients in orthodontic treatment at the Specialization Program in Orthodontics, Federal University of Bahia (UFBA), was randomly selected for participation in the study. All had been wearing fixed standard edgewise orthodontic appliances for at least a year (to ensure that subjects had established an oral hygiene routine and that periodontal conditions were stable) and orthodontic bands (Dental Morelli Ltda, Sorocaba, Brazil) cemented with glass ionomer cement (Ketac-Cem, Espe, Germany) on the four second molars (Orthodontics group). The Control group, comprising 50 individuals undergoing restorative treatment in teeth other than the second molars at the Department of Integrated Clinic, School of Dentistry (UFBA), was age and sex matched with those wearing fixed appliances.
Before treatment, the groups received equivalent guidelines with regard to oral hygiene and motivation. Additional oral hygiene instructions were given during orthodontic treatment only if necessary. Other inclusion criteria included the following: absence of chronic medical disease or condition that could affect their periodontium (such as diabetes mellitus, juvenile periodontitis, congenital heart disease, blood dyscrasias, or history of rheumatic fever), did not take antibiotics in the 3 months preceding the study, and had fully erupted second molars in the oral cavity. Informed consent was obtained from each member of the sample, and the study protocol was approved by Committee on Research Involving Human Subjects at the School of Dentistry at Salvador, Bahia Federal University, UFBA, Brazil.
Clinical examination was performed by a single examiner, duly calibrated (kappa >0.90) periodontics specialist using a conventional “Williams”-type periodontal probe (Trinity Periodontics, Jaraguá, Brazil) and a dental mirror.) The midbuccal sites of the four second molars were evaluated, and the data were noted in individual clinical charts for each study group.
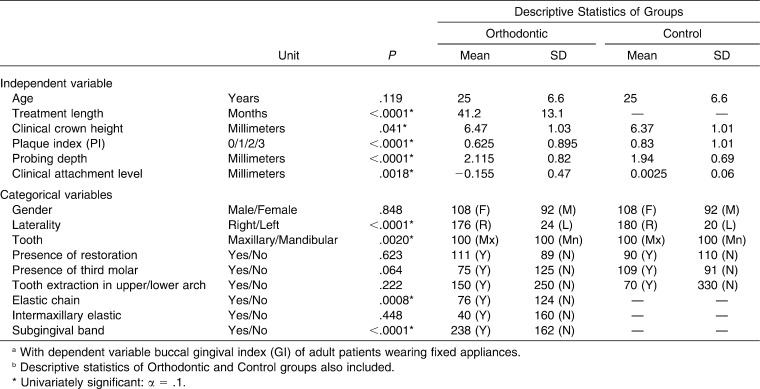
The independent variables described in Table 1, such as the Silness and Löe19 plaque index (PI), were recorded for each participant. The dependent variable used in this study was the Löe and Silness20 GI, used for periodontal status assessment, with the following classification: 0, absence of inflammation; 1, mild inflammation, with slight change in color and little change in texture; 2, moderate inflammation, with reddish appearance, mild edema, and hypertrophy and bleeding on probing; and 3, severe inflammation, with marked reddish appearance and hypertrophy, ulceration, and tendency to spontaneous bleeding.
Table 1.
Independent Variables Used in Univariate Logistic Regressions and Results of These Regressions in Selection of Variables for Multivariate Modela,b
Statistical Analysis
The midbuccal GI of the Orthodontics and Control groups was compared using the Wilcoxon test at a 5% significance level. Next, to study potential risk factors that might account for increased GI in patients with fixed orthodontic appliances, a series of logistic regressions were performed. Initially, univariate logistic regressions were carried out using as a dependent variable the midbuccal GI of patients in the Orthodontics group, and as independent variables those contained in Table 1. The significance of univariate models was 10%. Only those that proved statistically significant using univariate analysis were included in a stepwise multivariate model with the same level of significance (5%). Statistically significant variables in the multivariate model were found to be the odds ratios. Their respective 95% confidence intervals were therefore recorded.
RESULTS
The midbuccal GI of second molars in the Orthodontics group ( : 0.94 ± 1.0; n = 200) was significantly higher than in the Control group (0.54 ± 0.89, n = 200, P < .0001).
: 0.94 ± 1.0; n = 200) was significantly higher than in the Control group (0.54 ± 0.89, n = 200, P < .0001).
Risk factors for increases in GI in the Orthodontics group were studied by means of a series of logistic regressions. Results of univariate logistic regressions performed for selecting variables that entered the multivariate model are presented in Table 1, along with the descriptive statistics for these variables. None of the bands used on teeth that were evaluated showed excess cement or poor occlusal or cervical adjustment. Only significant variables were included in the multivariate model, whose selection was held by the stepwise method.
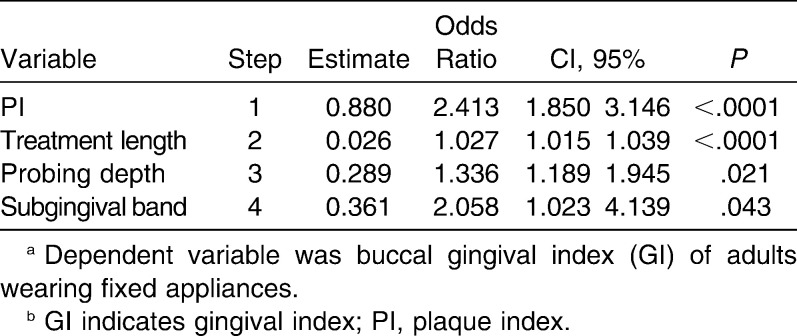
Selected variables generated a significant multivariate model ( = 92.34; P < .0001); those included in the model are presented in Table 2, along with odds ratio and 95% confidence intervals. The following were identified as possible risk factors for increased GI (in order of odds ratio importance): PI, subgingival cervical margin of the bands, probing depth, and length of orthodontic treatment.
= 92.34; P < .0001); those included in the model are presented in Table 2, along with odds ratio and 95% confidence intervals. The following were identified as possible risk factors for increased GI (in order of odds ratio importance): PI, subgingival cervical margin of the bands, probing depth, and length of orthodontic treatment.
Table 2.
Variables Included in Multivariate Model, Input String, Odds Ratio, and 95% Confidence Intervala,b
DISCUSSION
An increased GI index in teeth with orthodontic bands, as found in the present study, constitutes a relatively frequent event.3,7,9,11,16–18 This variable was selected for the study because bleeding on probing is the most reliable clinical indicator of significant gingival inflammation,2,6 and its absence indicates a high likelihood of maintaining periodontal health.21 For this reason, it can be considered a parameter for use in daily practice.
As stated earlier, PI was the most important risk factor for an increased GI in adult orthodontic patients because plaque builds up given the difficulty involved in removing the different orthodontic appliance components.7–13 The quantity and quality of plaque are influenced by many factors, including surface characteristics. Moreover, surface roughness is positively correlated with plaque growth and maturation.17 The role of this primary etiologic factor in gingivitis and periodontitis has been extensively documented in the literature, as has periodontal breakdown resulting from an imbalance between their constituents and the host's defense mechanisms.17,18,22–24
The subgingival cervical margin of the bands was another key factor (ie, bands that encroach into the sulcus substantially increased the odds [odds ratio {OR} = 2.058] for developing inflammation). Apparently, significant advantages are associated with not allowing the cervical margins of orthodontic bands to encroach into the gingival sulcus.1,7
Given the importance of PI, the difficulty in removing plaque from the subgingival margin of bands,1,7,15,21 often quoted in the literature, can explain its prominence as a risk factor. Arguably, another reason for this periodontal reaction is mechanical injury to adjacent tissues during the band placement procedure,1,16 or even the fact that attachment fibers are torn during the adaptation procedure, thus violating the biological space25 and leading to loss of attachment.7 This trauma may be more severe in clinical situations in which the teeth are improperly positioned or are not completely erupted.7 It is also conceivable that the cytotoxic effects of cement1 and/or band material1,16 can partially explain the gingival response. Nickel can have an influence over the periodontal status of allergic orthodontic patients, leading to local and systemic inflammatory reactions that are correlated with the gingival index.13 Such effects, although not evaluated in this study, deserve further investigation. Because of these reactions, it would be interesting to conduct a comparative study involving second molars with bonded accessories. According to some authors, this method would be preferable to banding.1,11,12,16
Probing depth appeared as another risk factor for increases in GI. It was determined that for every additional 1.0 mm, there is an increase of 1.336 in the odds ratio toward an increase in the gingival index. This association between GI and probing depth has been explained by decreased effectiveness in oral hygiene and, consequently, changes in subgingival microbiota at these sites.10,26 Increases in probing depth can be related to the presence of subgingival bands in two different ways. If encroachment into the gingival sulcus exceeds 0.5 mm, the risk that violation of the biological space will occur is increased, and this might cause recession and/or apical migration of the junctional epithelium and consequent periodontal pocket formation.27 Another explanation is the formation of hyperplasia or gingival edema, with a pseudopocket caused by local irritation of the bands and the proliferation of periodontopathogenic bacteria.7,9,17 Gingival hyperplasia (of inflammatory origin) affecting orthodontic patients is usually characterized by gingival tissue growth, localized or generalized, starting at the interdental papillae 1 to 2 months into treatment.28
Finally, treatment time showed only a slight influence on the occurrence of gingival inflammation. This is probably a result of the fact that, as treatment progresses, the number of orthodontic accessories (rubber bands, springs, and hooks) tends to increase, and, as already seen, this further compromises hygiene.7–13 It is therefore necessary that orthodontists provide their patients with oral hygiene instructions and constant motivation,10,12,29 while acting as objectively as possible and applying strategies to reduce the number of accessories12 and to shorten treatment time.
Our results suggests that when orthodontic bands are required on second molars, factors such as plaque control, cervical margin height, probing depth, and treatment time play an important role in increasing the GI index. This means that the clinician should take protective measures to minimize periodontal risk. These measures include monitoring and motivating patients' oral hygiene,10,12,29 maintaining supragingival band margins,1,7 and optimizing treatment, with minimal use of accessories.12 Thus, possibly, we will improve the periodontal condition of patients in treatment and their oral health.
CONCLUSIONS
Orthodontic treatment in adult patients showed more clinical signs of gingival inflammation than were seen in those with no appliance.
Potential risk factors identified for increased gingival index, in decreasing order of importance, include the following: plaque index, subgingival encroachment of the cervical margin of bands, probing depth, and length of orthodontic treatment.
Study results suggests that these factors depend on the professional responsible for treatment, adaptation of the bands during appliance set-up, and duration of orthodontic correction, as well as the patient's plaque control to prevent deposits from building up around appliance components.
REFERENCES
- 1.Diedrich P, Rudzki-Janson I, Wehrbein H, Fritz U. Effects of orthodontic bands on marginal periodontal tissues: a histologic study on two human specimens. J Orofac Orthop. 2001;62:146–156. doi: 10.1007/pl00001923. [DOI] [PubMed] [Google Scholar]
- 2.Proffit W. R, Fields H. W, Jr, Sarver D. M. Contemporary Orthodontics 4th ed. St Louis, Mo: Mosby; 2007. Contemporary orthodontic appliances and special considerations in treatment for adults; pp. 395–430, 635–685. [Google Scholar]
- 3.Rego R. O, Oliveira C. A, dos Santos-Pinto A, Jordam S. F, Zambon J. J, Cirelli J. A, Haraszthy V. I. Clinical and microbiological studies of children and adolescents receiving orthodontic treatment. Am J Dent. 2010;23:317–323. [PubMed] [Google Scholar]
- 4.Ong M. M. A, Wang H. Periodontic and orthodontic treatment in adults. Am J Orthod Dentofacial Orthop. 2002;122:420–428. doi: 10.1067/mod.2002.126597. [DOI] [PubMed] [Google Scholar]
- 5.Carvalho R. S, Nelson D, Kelderson H, Wise R. Guided bone regeneration to repair an osseous defect. Am J Orthod Dentofacial Orthop. 2003;123:455–467. doi: 10.1067/mod.2003.59. [DOI] [PubMed] [Google Scholar]
- 6.Vanarsdall R. L, Jr, Musich D. R. Adult orthodontics: diagnosis and treatment. In: Graber T. M, Vanarsdall R. L Jr, editors. Orthodontics Current Principles and Techniques 3rd ed. St Louis, Mo: Mosby; 2000. pp. 839–915. [Google Scholar]
- 7.Alexander S. A. Effects of orthodontic attachments in the gingival health of permanent second molars. Am J Orthod Dentofacial Orthop. 1991;100:337–340. doi: 10.1016/0889-5406(91)70071-4. [DOI] [PubMed] [Google Scholar]
- 8.Olympio K. P. K, Bardal P. A. P, Henriques J. F. C, de Bastos J. R. Prevenção de cárie dentária e doença periodontal em Ortodontia: uma necessidade imprescindível. R Dental Press Ortodon Ortop Facial. 2006;11:110–119. [Google Scholar]
- 9.Demling A, Heuer W, Elter C, et al. Analysis of supra- and subgingival long term biofilm formation on orthodontic bands. Eur J Orthod. 2009;31:202–206. doi: 10.1093/ejo/cjn090. [DOI] [PubMed] [Google Scholar]
- 10.Ristic M, Svabic M. V, Sasic M, Zelic O. Effects of fixed orthodontic appliances on subgingival microflora. Int J Dent Hyg. 2008;6:129–136. doi: 10.1111/j.1601-5037.2008.00283.x. [DOI] [PubMed] [Google Scholar]
- 11.Paschos E, Limbach M, Teichmann M, Huth K. C, Folwaczny M, Hickel R, Rudzki-Janson I. Orthodontic attachments and chlorhexidine-containing varnish effects on gingival health. Angle Orthod. 2008;78:908–916. doi: 10.2319/090707-422.1. [DOI] [PubMed] [Google Scholar]
- 12.Opsahl Vital S, Haignere-Rubinstein C, Lasfargues J. J, Chaussain C. Caries risk and orthodontic treatment. Int Orthod. 2010;8:28–45. doi: 10.1016/j.ortho.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 13.Pazzini C. A, Pereira L. J, Carlos R. G, de Melo G. E, Zampini M. A, Marques L. S. Nickel: periodontal status and blood parameters in allergic orthodontic patients. Am J Orthod Dentofacial Orthop. 2011;139:55–59. doi: 10.1016/j.ajodo.2009.02.036. [DOI] [PubMed] [Google Scholar]
- 14.Banks P, Macfarlane T. V. Bonded versus banded first molar attachments: a randomized controlled clinical trial. J Orthod. 2007;34:128–136. doi: 10.1179/146531207225022032. [DOI] [PubMed] [Google Scholar]
- 15.Chambrone L, Goldenberg F. C. Resposta dos tecidos mucogengivais em dentes submetidos a tratamento ortodôntico. J Bras Ortodon Ortop Facial. 2006;11:315–321. [Google Scholar]
- 16.Matos M, Vianna M. I. P, Pitta A. Controle químico e mecânico de placa em pacientes ortodônticos. Uma análise por grupo de dentes de acordo com o acessório ortodôntico empregado. R Dental Press Ortodon Ortop Facial. 2003;8:87–93. [Google Scholar]
- 17.Gastel J. V, Quirynen M, Teughe W, Coucke W, Carels C. Longitudinal changes in microbiology and clinical periodontal variables after placement of fixed orthodontic appliances. J Periodontol. 2008;79:2078–2086. doi: 10.1902/jop.2008.080153. [DOI] [PubMed] [Google Scholar]
- 18.Kim K, Heimisdottir K, Gebauer U, Persson G. R. Clinical and microbiological findings at sites treated with orthodontic fixed appliances in adolescents. Am J Orthod Dentofacial Orthop. 2010;137:223–228. doi: 10.1016/j.ajodo.2008.03.027. [DOI] [PubMed] [Google Scholar]
- 19.Silness J, Löe H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1964;22(suppl 1):121–135. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 20.Löe H, Silness J. Periodontal disease in pregnancy. I: prevalence and severity. Acta Odontol Scand. 1963;21(suppl 3):533–551. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 21.Lang N. P, Adler R, Joss A, Nyman S. Absence of bleeding on probing: an indicator of periodontal stability. J Clin Periodontol. 1990;17:714–721. doi: 10.1111/j.1600-051x.1990.tb01059.x. [DOI] [PubMed] [Google Scholar]
- 22.Löe H, Theilade E, Jensen S. B. Experimental gingivitis in man. J Periodontol. 1965;36:177–187. doi: 10.1902/jop.1965.36.3.177. [DOI] [PubMed] [Google Scholar]
- 23.Theilade E, Wright W. H, Jensen S. B. Experimental gingivitis in man. II: a longitudinal clinical and bacteriological investigation. J Periodontal Res. 1966;1:1–13. doi: 10.1111/j.1600-0765.1966.tb01842.x. [DOI] [PubMed] [Google Scholar]
- 24.Newman M. G. Currents concepts of the pathogenesis of periodontal disease: microbiology emphasis. J Periodontol. 1985;56:734–739. doi: 10.1902/jop.1985.56.12.734. [DOI] [PubMed] [Google Scholar]
- 25.Gargiulo A. W, Wentz F. M, Orban B. Dimensions and relations of the dentogingival junction in humans. J Periodontol. 1961;32:261–267. [Google Scholar]
- 26.Greenstein G. Contemporary interpretation of probing depth assessments: diagnostic and therapeutic implications. A literature review. J Periodontol. 1997;68:1194–1205. doi: 10.1902/jop.1997.68.12.1194. [DOI] [PubMed] [Google Scholar]
- 27.Wylson R. D, Maynard G. Intracrevicular restorative dentistry. Int J Periodontics Restorative Dent. 1981;1:35–45. [PubMed] [Google Scholar]
- 28.Romero M, Albi M, Bravo L. A. Surgical solutions to periodontal complications of orthodontic therapy. J Clin Pediatr Dent. 2000;24:159–163. [PubMed] [Google Scholar]
- 29.Lovrov S, Hertrich K, Hirschfelder U. Enamel demineralization during fixed orthodontic treatment: incidence and correlation to various oral-hygiene parameters. J Orofac Orthop. 2007;68:353–363. doi: 10.1007/s00056-007-0714-1. [DOI] [PubMed] [Google Scholar]