Abstract
Objectives:
To investigate root resorption after 6 months of active orthodontic treatment and its relation to possible risk factors.
Materials and Methods:
Ninety-seven patients (10–18 years) with a Class I malocclusion and crowding treated with fixed appliance and premolar extractions were examined with cone beam computed tomography before and after 6 months of active treatment. The exposure covered all teeth from first molar to first molar in both jaws. The Malmgren index was used to evaluate the degree of root resorption. Irregular root contour (score 1) was seen in most teeth already before active treatment, and therefore resorptions were registered only as score 2 (<2 mm, minor resorption) or higher.
Results:
Minor root resorption was noted in 10% of the patients and severe root resorption, >2 mm (score 3) was found in four patients. Root resorption was more frequently seen in the upper jaw, especially the incisors. There was no statistically significant correlation of root resorption with any of the selected risk factors.
Conclusions:
After 6 months of treatment, clinically significant resorption was diagnosed in 4% of the patients, ie, in 96% of the patients the radiographic examination did not reveal any significant information. The selected risk factors did not have any impact on the amount of resorption after 6 months of active treatment.
Keywords: Root resorption, Orthodontics, Six months, Cone beam computed tomography, Risk factors
INTRODUCTION
Numerous studies have been published identifying orthodontics as a factor for external root resorption.1–3 Among treated patients, orthodontically induced root resorption (OIRR) incidences ranging from 1% to 100% have been reported.4,5 This large variation depends on several factors including for example, examination methods, definition of root resorption, type of appliance and forces used. In the literature the following factors have been claimed to be significant risk factors for the development of OIRR:
Radiography is the most commonly used tool for diagnosing root resorption and the majority of the clinical studies used intraoral periapical radiography.16 The technique has its shortcomings that are difficult to overcome.17–21 Radiographic detection of root shortening also requires a certain degree of resorption.22 Another radiographic technique that has been used to assess root shortening is panoramic radiography. This technique is sensitive to patient positioning because of its relatively narrow sharp layer and shape of focal trough. Even under optimal conditions and patient positioning panoramic radiographs are fraught with uncertainties, especially in the anterior regions. Use of a lateral radiograph in combination with a panoramic radiograph has been proposed to reduce the shortcomings in the anterior regions.23 Difficulty in identifying individual teeth on a lateral radiograph makes this, however, questionable.
Cone beam computed tomography (CBCT)24 was introduced in the late 1990s, and studies regarding radiation dosages show lower doses from CBCT units than from conventional CT examinations.25,26 The doses vary, however, between different brands, imaging areas, and exposure parameters used.27,28 Since its introduction, the CBCT technique has gained widespread use in various fields of dentistry, not least in orthodontics.29
In a study investigating the diagnostic accuracy of panoramic radiography in the detection of OIRR compared with CBCT examinations, Dudic et al.30 showed that using panoramic radiography, apical root resorption was diagnosed in 44% of teeth, whereas using CBCT, apical root resorption was diagnosed in 69%. The CBCT technique also has benefits compared with periapical radiography, such as providing images in all three planes, thus revealing resorption on surfaces not detectable with conventional radiography. Although, the foremost advantage over conventional radiography would be the high degree of reproducibility during the treatment course because multiplanar reconstructions can be made giving optimal visualization of each tooth despite changes in tooth position that occur during an orthodontic treatment.31
The literature poses significant correlation between the presence of minor root resorption at an early stage of treatment (3–9 months) and occurrence of severe resorption at the end of treatment.2,12,32 Levander et al.12 reported that after 3 months of treatment apical root resorption was detected only in a few teeth, but that the number increased significantly after 6 months of treatment. Patients with detectable root resorption during the first 6 months of active treatment have also been reported to be more likely to have resorption in the following 6-month period than those without.12,33 Mohandesan et al.34 found clinically significant resorption in 74% of the maxillary central incisors and 82% of the maxillary lateral incisors during a 12-month treatment period.
The aim of this study was to investigate prevalence and degree of OIRR after 6 months of active treatment with fixed appliances and to study correlation of early root resorption with some risk factors.
MATERIALs AND METHODS
Subjects
One hundred seventy-one patients from the Department of Orthodontics, University Clinics of Odontology, Gothenburg, Sweden, participated in a study on root resorption between March 2005 and June 2008. The patients had to fulfill predefined inclusion criteria: Class I malocclusion (super Class I to cusp to cusp distal molar relationship) with crowding and an overjet <5 mm. Further, the crowding had to be so severe that the treatment plan should comprise extraction of one premolar in each jaw quadrant. Informed consent from the parents as well as an ethical approval from the Ethics Committee and from the Radiation Protection Committee, Sahlgrenska Academy at University of Gothenburg, Sweden was obtained.
The treatment protocol was standardized using an MBT preadjusted appliance (3M Unitek, Monrovia, CA) with 0.022-inch slots. The initial leveling and alignment were done using round heat activated nickel titanium wires, and space closure was performed with rectangular 0.019 × 0.021-inch stainless steel wires. For each patient, a protocol was added to the records with notations of known risk factors (Table 1).
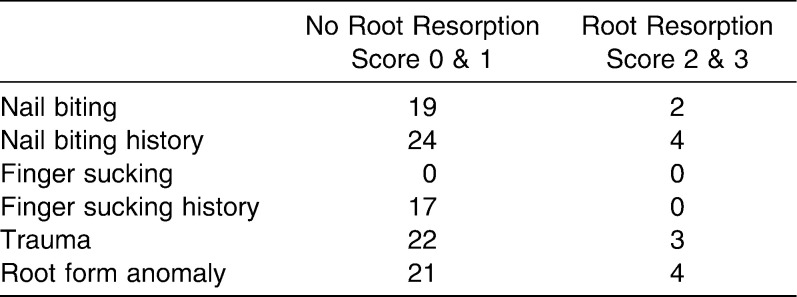
Table 1.
Prevalence of Risk Factors Among 97 Patients With and Without Root Resorption (number of patients)
Radiographic Examination
A radiographic examination (CBCT) was performed on all subjects before treatment, and in 97 randomly selected patients (57 female, 40 male) after 6 months of active treatment. The mean age of the patients was 15.2 years (SD 1.5, range 11.4–18.3 years). The randomization of the 6-month radiographic examination, among the 171 patients, was performed with a random number list generated in an Excel spreadsheet. All examinations were performed with three-dimensional Accuitomo FPD (J Morita Mfg Corp, Kyoto, Japan). Exposure parameters were 75 kV, 4–5.5 mA based on patient size, and volume 60 mm × 60 mm with a full 17.5-second scan rotation. Positioning of the patients was made according to standard operating procedure, and adjustments of the x-ray beam positioning were made so that all teeth in both jaws, from the incisors to the first molars, were included in one imaged volume.
All reformatting was performed according to a procedure previously described by Lund et al.31 The reformatting was made in line with the long axis of the tooth/root, thus an optimal visualization of the tooth/root in axial, coronal, and sagittal planes was obtained. The accuracy and precision of the method have been described elsewhere.31
In order to describe root shortening, changes in tooth length between the pretreatment examination and the 6-month examination were subjectively converted into an index originally designed for intraoral radiography by Malmgren et al.35 The index (Figure 1) comprises four different scores: 1 = irregular root contour, 2 = root resorption apically amounting to less than 2 mm (minor resorption), 3 = root resorption apically from 2 mm to 1/3 of the original root length (severe resorption), and 4 = root resorption exceeding 1/3 of the original root length (extreme resorption). All assessments were made by one of the authors.
Figure 1.
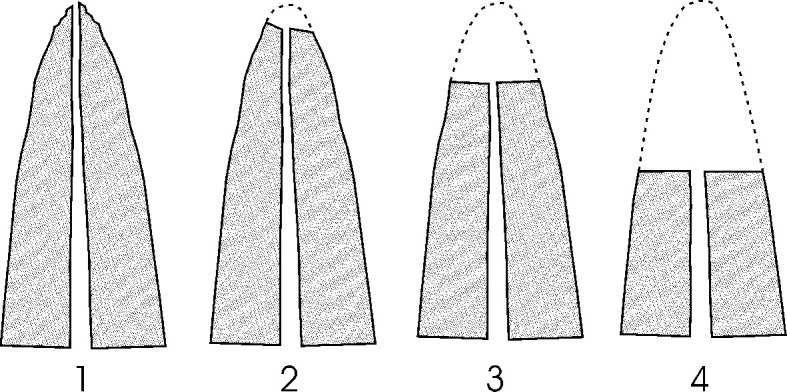
Index for subjective scoring of root resorption according to Malmgren et al.35 (1) Irregular root contour. (2) Apical root resorption less than 2 mm of original root length. (3) Apical root resorption from 2 mm to 1/3 of original root length. (4) Apical root resorption exceeding 1/3 of original root length.
Statistics
Root resorption was dichotomized in root resorption (Y) and no root resorption (N). The incidence of patients with root resorption (Y/N) and the presence of risk factors groups (Y/N) were investigated by using the Fisher exact test. P ≥ .05 was considered not statistically significant.
RESULTS
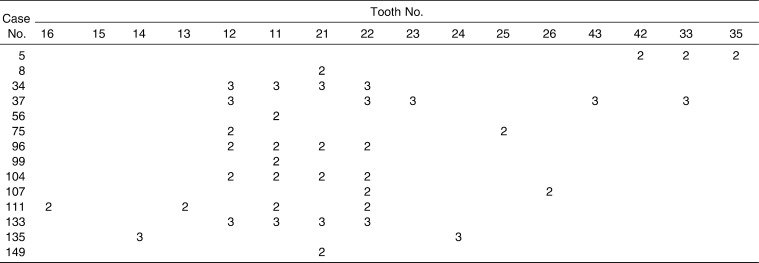
Irregular root contour (score 1) was seen in most teeth already before active treatment. Thus, root resorption was only considered present if scores of 2 or higher were registered. Minor resorption (score 2), was noted in 10 patients and score 3 was found in four patients (Table 2). Figure 2 shows images of an upper canine judged as score 3 (case 37). No teeth showed score 4. Root resorption was more frequently seen in the upper jaw, especially in the incisors (Table 2). In the lower jaw, root resorption was only detected in two patients. In one patient there was no detectable root resorption in the upper jaw, but in the other patient root resorption was also seen on the maxillary laterals and left canine (Table 2).
Table 2.
Distribution of Affected Teeth and Their Severity of Root Resorption, Index Scores 2 (II) and 3 (III) According to the Index Described by Malmgren et al.35
Figure 2.
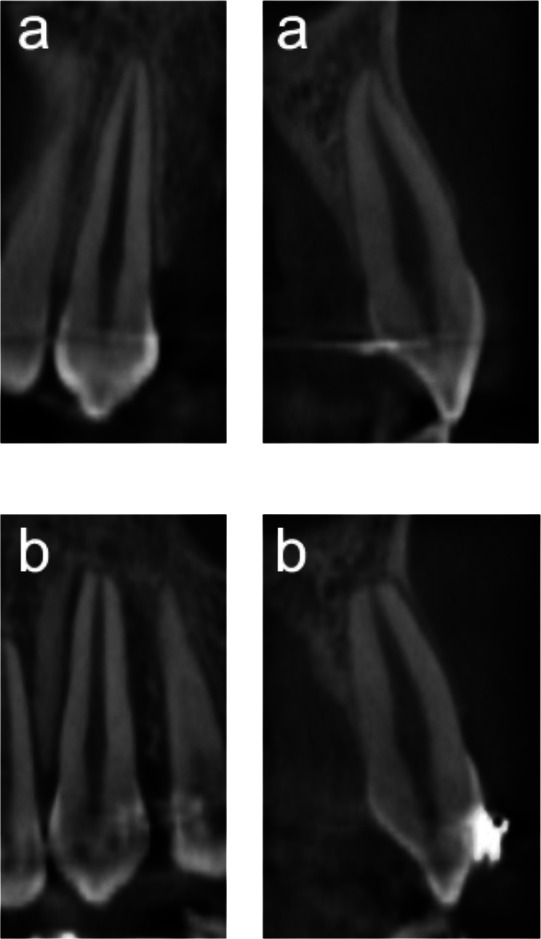
Reformatted CBCT images (cropped) of upper left canine in frontal and sagittal views obtained at baseline (a) and after 6 months of treatment (b). Resorption index was judged to be score 3 after the 6 months of treatment.
Table 1 shows the prevalence of risk factors among the 97 patients. None of them had any endodontically treated teeth and none of them were still finger-sucking individuals. There was no statistically significant relationship of root resorption with any of the selected risk factors (Table 1).
DISCUSSION
This study is part of a larger survey where an extensive radiographic examination is performed on a number of patients with the same type of malocclusion and a comparable treatment plan. The aim was to study early signs of root resorption and relation to certain predictive factors.
To get a correct evaluation of the amount of OIRR and to minimize the errors in the radiographic evaluation, the study design included the use of a CBCT examination before treatment, 6 months after the start of treatment, and at the end of treatment. CBCT has a fairly low radiation dosage compared with other advanced radiographic methods,25,26 and the amount of radiation could be considered similar to that of eight panoramic radiographs.36
The “Malmgren index”35 was originally adopted for use with intraoral periapical radiography. The advantage of the index is that it sets a threshold that is clinically relevant and is fairly easy to apply in the daily practice. The CBCT technique revealed that almost every tooth had some irregularity in the apical root contour even in images obtained before treatment. Hence, there would have been an overestimation of presence of OIRR if score 1 had been included. Further, irregular root contours are perhaps not clinically significant. Score 2 (<2 mm) on the other hand is a small but clear resorption, and from a clinical point of view a useful threshold for defining minor root shortening.
There are few, if any, studies published investigating OIRR in all teeth in both jaws during the initial phase of orthodontic treatment. In agreement with previous studies investigating maxillary incisors,12,32,37 the present study confirmed that some patients developed signs of OIRR during the first stage of treatment with fixed appliances. However, the number of patients with more evident resorption was small. Four of 97 patients had teeth with resorption classified as score 3. In one of these patients, the resorption was found on the first maxillary premolars (Table 2), a tooth type that normally is not monitored with radiography during an orthodontic treatment or included in scientific papers on early root resorption. Resorption was, however, almost exclusively seen in the upper jaw, especially in the incisor region; only one patient was noted to have resorption with an index score 3 in the lower canine (Table 2).
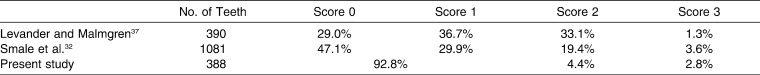
Our findings are thus less severe than those found by Smale et al.32 who reported that 8.5% of their patients had one or more maxillary incisors with index score 3 after 3 to 9 months of treatment. The corresponding number of maxillary incisors in our study was 3.1% (Table 2). The difference is even larger for the less severe resorption where Smale et al.32 found score 2 in one or more incisors in 40% of the patients, whereas score 2 was registered on maxillary incisors in 9.3% of the patients in the present study (Table 2). Levander and Malmgren37 also investigated OIRR during initial orthodontic treatment. Their results, presented on tooth level, showed a higher number of resorbed teeth with score 2 than the present study. On a tooth level, which however is a less correct way of presenting clinical data due to the influence of the individual, the number of teeth with more severe resorption (score 3) in the present study is quite similar to the numbers of teeth in the studies of Smale et al.,32 Levander and Malmgren,37 and the present study (Table 3). The lower numbers of teeth with minor resorption (score 2) found in the present study compared to Smale32 and Levander and Malmgren37 (Table 3) might be explained by the different radiographic techniques used. Projection error is a great problem in intraoral radiography, especially in orthodontics where teeth are moved and the angulations of the teeth are changing during treatment, making periodical identical radiographs more or less impossible. The CBCT technique, however, controls projection geometry for each individual tooth,31 so that projection errors are minimized for tooth length variations of 2 mm; this might explain the low number of score 2 resorption in the present study. More severe root resorption is probably not as sensitive to technique, and thus the findings in the three studies are more alike (Table 3).
Table 3.
Root Resorption in Maxillary Incisors on Tooth Level in Three Different Studies. In the Present Study 388 Maxillary Incisors in 97 Patients Were Studied Before and After 6 Months of Treatment. Resorbed Teeth in Per Cent of Total
No correlation between OIRR and selected predisposing factors was found, probably due to the small number of patients with evident root resorption. In a systematic review, Weltman et al.2 reported that previous trauma and tooth morphology are unlikely causative factors for OIRR, which supports our findings. The results from the present study showed that almost 50% of the patients with OIRR score 3 (>2mm) had abnormal shaped roots, but no statistically significant correlation was found. Levander et al.12 also reported a higher degree of OIRR in teeth with blunt and pipette-shaped roots, and these findings were also reported in other studies.9–11
In conclusion, 96% of the patients during the first phase of orthodontic treatment did not reveal any clinically significant changes of the root length. With this in mind one could question if it is justified to make radiographic examinations of all patients after 3–6 months of treatment. However, when the final results of this project are complete and the numbers and severity of root resorption can be analyzed in detail after the orthodontic treatment, the benefits of an intermediate radiographic examination can be evaluated.
CONCLUSIONS
After 6 months of treatment, clinically significant resorption was diagnosed in 4% of the patients, ie, the radiographic examination did not reveal any clinically significant information in 96% of the patients.
The selected predisposing risk factors for root resorption did not have any impact on the amount of resorption after 6 months of active treatment.
REFERENCES
- 1.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 1. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:62–66. doi: 10.1016/0889-5406(93)70106-X. [DOI] [PubMed] [Google Scholar]
- 2.Weltman B, Vig K. W, Fields H. W, Shanker S, Kaizar E. E. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 3.Ottolengui R. The physiological and pathological resorption of tooth roots. Items of Interest. 1914;36:332–362. [Google Scholar]
- 4.Mayoral G. Treatment results with light wires studied by panoramic radiography. Am J Orthod. 1982;81:489–497. doi: 10.1016/0002-9416(82)90428-6. [DOI] [PubMed] [Google Scholar]
- 5.Harry M. R, Sims M. R. Root resorption in bicuspid intrusion. A scanning electron microscope study. Angle Orthod. 1982;52:235–258. doi: 10.1043/0003-3219(1982)052<0235:RRIBI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 6.Linge L, Linge B. O. Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;99:35–43. doi: 10.1016/S0889-5406(05)81678-6. [DOI] [PubMed] [Google Scholar]
- 7.Odenrick L, Brattstrom V. The effect of nail biting on root resorption during orthodontic treatment. Eur J Orthod. 1983;5:185–188. doi: 10.1093/ejo/5.3.185. [DOI] [PubMed] [Google Scholar]
- 8.Rupp R. Root resorption related to orthodontics and other factors: a review of the literature. J Gen Orthod. 1995;6:25–29. [PubMed] [Google Scholar]
- 9.Mirabella A. D, Artun J. Risk factors for apical root resorption of maxillary anterior teeth in adult orthodontic patients. Am J Orthod Dentofacial Orthop. 1995;108:48–55. doi: 10.1016/s0889-5406(95)70065-x. [DOI] [PubMed] [Google Scholar]
- 10.Nigul K, Jagomagi T. Factors related to apical root resorption of maxillary incisors in orthodontic patients. Stomatologija. 2006;8:76–79. [PubMed] [Google Scholar]
- 11.Thongudomporn U, Freer T. J. Anomalous dental morphology and root resorption during orthodontic treatment: a pilot study. Aust Orthod J. 1998;15:162–167. [PubMed] [Google Scholar]
- 12.Levander E, Bajka R, Malmgren O. Early radiographic diagnosis of apical root resorption during orthodontic treatment: a study of maxillary incisors. Eur J Orthod. 1998;20:57–63. doi: 10.1093/ejo/20.1.57. [DOI] [PubMed] [Google Scholar]
- 13.Linge B. O, Linge L. Apical root resorption in upper anterior teeth. Eur J Orthod. 1983;5:173–183. doi: 10.1093/ejo/5.3.173. [DOI] [PubMed] [Google Scholar]
- 14.de Freitas M. R, Beltrao R. T, Janson G, Henriques J. F, Chiqueto K. Evaluation of root resorption after open bite treatment with and without extractions. Am J Orthod Dentofacial Orthop. 2007;132:143.e15–e22. doi: 10.1016/j.ajodo.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Segal G. R, Schiffman P. H, Tuncay O. C. Meta analysis of the treatment-related factors of external apical root resorption. Orthod Craniofac Res. 2004;7:71–78. doi: 10.1111/j.1601-6343.2004.00286.x. [DOI] [PubMed] [Google Scholar]
- 16.Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: part 2. Literature review. Am J Orthod Dentofacial Orthop. 1993;103:138–146. doi: 10.1016/S0889-5406(05)81763-9. [DOI] [PubMed] [Google Scholar]
- 17.Brezniak N, Goren S, Zoizner R, Dinbar A, Arad A, Wasserstein A, et al. A comparison of three methods to accurately measure root length. Angle Orthod. 2004;74:786–791. doi: 10.1043/0003-3219(2004)074<0786:ACOTMT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Brezniak N, Goren S, Zoizner R, Dinbar A, Arad A, Wasserstein A, et al. The use of an individual jig in measuring tooth length changes. Angle Orthod. 2004;74:780–785. doi: 10.1043/0003-3219(2004)074<0780:TUOAIJ>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 19.Gegler A, Fontanella V. In vitro evaluation of a method for obtaining periapical radiographs for diagnosis of external apical root resorption. Eur J Orthod. 2008;30:315–319. doi: 10.1093/ejo/cjm125. [DOI] [PubMed] [Google Scholar]
- 20.Heo M. S, Lee S. S, Lee K. H, Choi H. M, Choi S. C, Park T. W. Quantitative analysis of apical root resorption by means of digital subtraction radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:369–373. doi: 10.1067/moe.2001.113592. [DOI] [PubMed] [Google Scholar]
- 21.Reukers E, Sanderink G, Kuijpers-Jagtman A. M, van't Hof M. Assessment of apical root resorption using digital reconstruction. Dentomaxillofac Radiol. 1998;27:25–29. doi: 10.1038/sj.dmfr.4600313. [DOI] [PubMed] [Google Scholar]
- 22.Chan E. K, Darendeliler M. A. Exploring the third dimension in root resorption. Orthod Craniofac Res. 2004;7:64–70. doi: 10.1111/j.1601-6343.2004.00280.x. [DOI] [PubMed] [Google Scholar]
- 23.Leach H. A, Ireland A. J, Whaites E. J. Radiographic diagnosis of root resorption in relation to orthodontics. Br Dent J. 2001;190:16–22. doi: 10.1038/sj.bdj.4800870. [DOI] [PubMed] [Google Scholar]
- 24.Arai Y, Tammisalo E, Iwai K, Hashimoto K, Shinoda K. Development of a compact computed tomographic apparatus for dental use. Dentomaxillofac Radiol. 1999;28:245–248. doi: 10.1038/sj/dmfr/4600448. [DOI] [PubMed] [Google Scholar]
- 25.Schulze D, Heiland M, Thurmann H, Adam G. Radiation exposure during midfacial imaging using 4- and 16-slice computed tomography, cone beam computed tomography systems and conventional radiography. Dentomaxillofac Radiol. 2004;33:83–86. doi: 10.1259/dmfr/28403350. [DOI] [PubMed] [Google Scholar]
- 26.Tsiklakis K, Donta C, Gavala S, Karayianni K, Kamenopoulou V, Hourdakis C. J. Dose reduction in maxillofacial imaging using low dose cone beam CT. Eur J Radiol. 2005;56:413–417. doi: 10.1016/j.ejrad.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Lofthag-Hansen S, Thilander-Klang A, Ekestubbe A, Helmrot E, Grondahl K. Calculating effective dose on a cone beam computed tomography device: 3D Accuitomo and 3D Accuitomo FPD. Dentomaxillofac Radiol. 2008;37:72–79. doi: 10.1259/dmfr/60375385. [DOI] [PubMed] [Google Scholar]
- 28.Ludlow J. B, Davies-Ludlow L. E, Brooks S. L, Howerton W. B. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol. 2006;35:219–226. doi: 10.1259/dmfr/14340323. [DOI] [PubMed] [Google Scholar]
- 29.Kau C. H, Richmond S, Palomo J. M, Hans M. G. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 30.Dudic A, Giannopoulou C, Leuzinger M, Kiliaridis S. Detection of apical root resorption after orthodontic treatment by using panoramic radiography and cone-beam computed tomography of super-high resolution. Am J Orthod Dentofacial Orthop. 2009;135:434–437. doi: 10.1016/j.ajodo.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 31.Lund H, Grondahl K, Grondahl H. G. Cone beam computed tomography for assessment of root length and marginal bone level during orthodontic treatment. Angle Orthod. 2010;80:466–473. doi: 10.2319/072909-427.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smale I, Artun J, Behbehani F, Doppel D, van't Hof M, Kuijpers-Jagtman A. M. Apical root resorption 6 months after initiation of fixed orthodontic appliance therapy. Am J Orthod Dentofacial Orthop. 2005;128:57–67. doi: 10.1016/j.ajodo.2003.12.030. [DOI] [PubMed] [Google Scholar]
- 33.Artun J, Smale I, Behbehani F, Doppel D, Van't Hof M, Kuijpers-Jagtman A. M. Apical root resorption six and 12 months after initiation of fixed orthodontic appliance therapy. Angle Orthod. 2005;75:919–926. doi: 10.1043/0003-3219(2005)75[919:ARRSAM]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Mohandesan H, Ravanmehr H, Valaei N. A radiographic analysis of external apical root resorption of maxillary incisors during active orthodontic treatment. Eur J Orthod. 2007;29:134–139. doi: 10.1093/ejo/cjl090. [DOI] [PubMed] [Google Scholar]
- 35.Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod. 1982;82:487–491. doi: 10.1016/0002-9416(82)90317-7. [DOI] [PubMed] [Google Scholar]
- 36.Helmrot E, Thilander-Klang A. Methods for monitoring patient dose in dental radiology. Radiat Prot Dosimetry. 2010;139:303–305. doi: 10.1093/rpd/ncq095. [DOI] [PubMed] [Google Scholar]
- 37.Levander E, Malmgren O. Evaluation of the risk of root resorption during orthodontic treatment: a study of upper incisors. Eur J Orthod. 1988;10:30–38. doi: 10.1093/ejo/10.1.30. [DOI] [PubMed] [Google Scholar]