Abstract
Peroxisomes are key regulators of cellular and metabolic homeostasis. These organelles play important roles in redox metabolism, the oxidation of very-long-chain fatty acids (VLCFAs), and the biosynthesis of ether phospholipids. Given the essential role of peroxisomes in cellular homeostasis, peroxisomal dysfunction has been linked to various pathological conditions, tissue functional decline, and aging. In the past few decades, a variety of cellular signaling and metabolic changes have been reported to be associated with defective peroxisomes, suggesting that many cellular processes and functions depend on peroxisomes. Peroxisomes communicate with other subcellular organelles, such as the nucleus, mitochondria, endoplasmic reticulum (ER), and lysosomes. These inter-organelle communications are highly linked to the key mechanisms by which cells surveil defective peroxisomes and mount adaptive responses to protect them from damages. In this review, we highlight the major cellular changes that accompany peroxisomal dysfunction and peroxisomal inter-organelle communication through membrane contact sites, metabolic signaling, and retrograde signaling. We also discuss the age-related decline of peroxisomal protein import and its role in animal aging and age-related diseases. Unlike other organelle stress response pathways, such as the unfolded protein response (UPR) in the ER and mitochondria, the cellular signaling pathways that mediate stress responses to malfunctioning peroxisomes have not been systematically studied and investigated. Here, we coin these signaling pathways as “peroxisomal stress response pathways”. Understanding peroxisomal stress response pathways and how peroxisomes communicate with other organelles are important and emerging areas of peroxisome research.
Keywords: peroxisome, reactive oxygen species, acetyl-CoA, plasmalogen, ER stress, mitochondrial dysfunction, apoptosis, pexophagy
1. Introduction
Eukaryotic cells contain a variety of membrane-enclosed organelles. Among them, peroxisomes are ubiquitous single membrane-bound organelles that play essential roles in cellular metabolism. Peroxisomes are the major site for both the production and degradation of hydrogen peroxide (H2O2) due to their high content of peroxisomal oxidases and antioxidant enzymes, such as catalase. Peroxisomes are also critical for the biosynthesis of ether phospholipids, cholesterol, bile acids, and polyunsaturated fatty acids (PUFAs). The importance of peroxisomes is evidenced by peroxisomal biogenesis disorders (PBDs), rare genetic diseases caused by mutations in any of the 13 different PEX genes encoding peroxins responsible for the import of membrane or matrix proteins to peroxisomes [1]. Zellweger syndrome (ZS) is the most severe PBD, and patients with ZS show severe brain, liver, kidney, and bone malfunctions [2].
Given the essential roles of peroxisomes in cellular and metabolic homeostasis [3,4], it is not surprising to find that peroxisomal dysfunction is strongly linked to the loss of redox homeostasis, dysregulated lipid metabolism, mitochondrial dysfunction, altered gene expression, and elevated ER stress and cell death. More recently, it has become clear that peroxisome deficiency can also alter functions of specific subcellular organelles [5,6,7], such as mitochondria, endoplasmic reticulum (ER), and lysosome. Peroxisomal stress signals can also be transduced from peroxisomes to the nucleus, as peroxisomal dysfunction often induces global transcriptional changes [8,9]. Thus, similar to other organelle stress pathways (e.g., ER stress), there are specific peroxisomal stress response pathways that allow eukaryotic cells to cope with malfunctioning peroxisomes [10].
Peroxisomes can communicate with other organelles through membrane contact sites, peroxisome-derived metabolites, as well as retrograde signaling. However, it remains largely unclear how peroxisomal stress response pathways are activated and how they protect cells from damages. Understanding peroxisomal stress response pathways and how peroxisomes communicate with other organelles are important areas of peroxisome research because of their vital role in cellular homeostasis, aging, and aging-related diseases [11,12,13,14]. In this review, we first describe peroxisomal biogenesis, the peroxisome protein import machinery, and peroxisome metabolic functions. Next, we summarize recent studies on the major cellular responses induced by peroxisomal dysfunction and the role of inter-organelle crosstalk in maintaining cellular homeostasis and organelle functions. Lastly, we discuss the potential roles of peroxisomes in aging and aging-related diseases.
2. Peroxisome Biogenesis and Peroxisomal Import Machinery
Peroxisomes are single membrane-bound organelles found in all eukaryotic cells and organisms, from yeast to plants and mammals [15]. Under normal conditions, the peroxisome has a half-life of 1.5 to 2 days [16], suggesting that peroxisome biogenesis and degradation are very dynamic processes. Peroxisomal biogenesis is mostly regulated by peroxins encoded by PEX genes. To date, more than 30 conserved peroxins have been identified in yeast, plants, and many animal species [17]. Peroxisomes can be formed by de novo biogenesis from the ER and mitochondria [17,18,19]. Pre-peroxisomal vesicles originating from the ER contain the peroxisomal membrane protein (PMP) PEX16, which binds to the PMP receptor PEX3. PEX3 functions as a docking receptor for the cytosolic chaperone and PMP receptor PEX19 [20,21]. Together, these peroxins recruit other PMPs containing membrane peroxisome targeting signals (PTS) to the peroxisomal membrane during the peroxisome maturation process.
Peroxisomal matrix proteins are transported into the organelle after synthesis in the cytosol [22]. PTSs are essential for the correct sorting of matrix proteins [23]. Most peroxisomal matrix proteins contain a PTS type 1 (PTS1) sequence at the C-terminus consisting of an S-K-L motif or a conservative variant [24,25]. A small set of matrix proteins contains a PTS type 2 (PTS2) sequence, a nonapeptide with the consensus sequence (R/K)-(L/I/V)-X5-(H/Q)-(L/A) (X = any amino acid) that is localized near or at the N-terminus of the protein [26,27]. PTS1 proteins are transported to the peroxisome by the shuttling receptor PEX5, whereas PTS2 proteins are delivered to the organelle by PEX5 and PEX7 [23]. The cargo-loaded receptor proteins bind to the peroxisomal membrane proteins PEX13 and PEX14 [28,29]. After docking, the cargo proteins are translocated across the peroxisomal membrane and imported into the organelle lumen, while receptor protein PEX5 is then mono- or polyubiquitinated by E3 ubiquitin ligases PEX2, PEX10, and PEX12 [23,30,31]. PEX5 monoubiquitination is required for its recycling to the cytosol, while polyubiquitinated PEX5 can be targeted to the proteasome for degradation [32,33,34]. Cytosolic AAA-ATPases PEX1 and PEX6 form a heterohexameric ring as a trimer of PEX1/PEX6 heterodimers, which is anchored to the peroxisome membrane by PEX26 in higher organisms [35,36,37,38,39]. The PEX1-PEX6-PEX26 complex is responsible for releasing ubiquitinated PEX5 from the peroxisomal membrane to the cytosol [33,34,35]. In the cytosol, PEX5 can be deubiquitinated by deubiquitylating (DUB) enzymes (Ubp15 in yeast [40] and USP9X in mammals [41]) for the next cycle of peroxisomal import.
Mature peroxisomes divide and grow by elongation, membrane constriction, and fission [22,42,43,44,45]. In mammals, the peroxisomal membrane protein PEX11β plays a critical role in peroxisomal proliferation [42,46,47]. Exogenous expression of PEX11β in mammalian cells enhances peroxisomal proliferation [42], whereas the genetic defects of human PEX11β decrease peroxisomal abundance [47]. Although the molecular mechanisms underlying the modulation of PEX11β activity are not fully understood, docosahexaenoic acid (DHA) is known to play an important role in the initiation of peroxisomal elongation and fission [48]. Itoyama et al. [48] demonstrated that DHA, a peroxisomal β-oxidation metabolite, induced peroxisomal division by augmenting the hyper-oligomerization of Pex11pβ and the formation of Pex11pβ-enriched regions on elongated peroxisomes. The function of Pex11β in peroxisome proliferation depends on the homo-oligomerization through its N-terminal domain [46,49]. In addition, Pex11β interacts with the membrane via the N-terminal amphipathic helix to deform the membrane into elongated tubular peroxisomes [50,51,52]. Subsequently, Pex11β forms a ternary fission machinery complex with mitochondrial fission factor (Mff) and dynamin-like protein 1 (DLP1) at the constricted membrane region of elongated peroxisomes, promoting the scission of the membrane [51,53].
3. Key Metabolic Functions of Peroxisome
Peroxisomes are multifunctional organelles that play essential roles in several key metabolic pathways, including the β-oxidation of very-long-chain fatty acids (VLCFAs, >C22), the α-oxidation of branched-chain fatty acids, the oxidation of D-amino acids and polyamines, and the synthesis of ether phospholipids, bile acids, and DHA [2,17]. During these metabolic processes (e.g., VLCFA β-oxidation), reactive oxygen species (ROS) are produced as byproducts and subsequently neutralized by several antioxidant enzymes such as catalase [54,55,56]. About 50 different enzymes are involved in peroxisomal metabolic functions [2,57], and some of them are shared with other subcellular compartments, including mitochondria [57]. Accordingly, cooperation with other organelles, including mitochondria, ER, lipid droplets, and lysosomes, is necessary for proper peroxisomal metabolic functions.
Most fatty acids (FAs) are catabolized by β-oxidation, which removes two carbons from their carboxyl terminus [58]. In all eukaryotic cells, fatty acid oxidation occurs in both mitochondria and peroxisomes. FAs (<C20) are oxidized in mitochondria and converted to CO2 and H2O through the mitochondrial citric acid cycle and oxidative phosphorylation. However, VLCFAs cannot be oxidized in mitochondria. Instead, VLCFAs translocate across the peroxisomal membrane via ATP-binding cassette (ABC) subfamily D half-transporters (ABCD) and are broken down to acetyl-CoA, propionyl-CoA, or medium-chain acyl-CoAs. These different acyl-CoAs can be further converted into acylcarnitines in the peroxisome and translocate to mitochondria through the mitochondrial carnitine/acylcarnitine translocase (CACT). Acylcarnitines are then converted back to acyl-CoAs in mitochondria and enter the citric acid cycle [59].
Ether phospholipids are particular classes of phospholipids containing a glycerol backbone with an ether or vinyl-ether bond at the sn-1 position [60]. Plasmalogen is one type of ether phospholipid containing a vinyl-ether bond that is widely found in the brain, heart, and white blood cells [17]. The biosynthesis of plasmalogen begins in peroxisomes [17,60,61]. Dihydroxyacetone (DHAP), a glycolysis intermediate, is used as a building block of the glycerol backbone of plasmalogen. The peroxisomal matrix enzyme glyceronephosphate O-acyltransferase (GNPAT) transfers the acyl chain of acyl-CoA to DHAP to generate acyl-DHAP. Then, alkyl dihydroxyacetone phosphate synthase (AGPS) exchanges the acyl chain for an alkyl group to form alkyl-DHAP. Recently, Honsho et al. [62] showed that acyl/alkyl-DHAP reductase (ADHAPR/DHRS7B) localizes in peroxisomes and the ER as a type I integral membrane protein in HeLa cells. The authors demonstrated that ER-localized ADHAPR reduces alkyl-DHAP, while peroxisomal ADHAPR preferentially reduces acyl-DHAP before the subsequent synthesis of alkyl-DHAP catalyzed by alkyl-DHAP synthase (ADAPS) [62]. The remaining steps of plasmalogen synthesis take place in the ER [63,64].
Peroxisomes are also important for ROS metabolism. The name “peroxisome” was first introduced by De Duve in 1965 to define an organelle containing several enzymes that produce or break down hydrogen peroxide (H2O2) [4,65]. Peroxisomes are responsible for up to 20% of the cell’s oxygen consumption and 35% of the H2O2 production in mammalian tissues [66]. Peroxisomes produce different ROS species such as superoxide, hydroxyl radicals, and hydrogen peroxide as byproducts of metabolic processes by multiple oxidases present in the organelle. Acyl-CoA oxidases (ACOX) are the most abundant ROS-generating enzymes in the peroxisome [59]. D-amino acid oxidase (DAO), D-aspartate oxidase (DDO), L-pipecolic acid oxidase (PIPOX), L-α-hydroxy acid oxidases (HAO), polyamine oxidase (PAOX), and xanthine oxidase (XDH) are also important H2O2 producers in human peroxisomes. To protect the organelle from oxidative damage, human peroxisomes have several antioxidant enzymes including catalase (CAT), copper/zinc-containing superoxide dismutase (SOD1), peroxiredoxin 5 (PRDX5), glutathione S-transferase kappa 1 (GSTK1), microsomal GST1 (MGST1), and epoxide hydrolase 2 (EPHX2) [67].
4. Cellular Responses to Peroxisomal Dysfunction
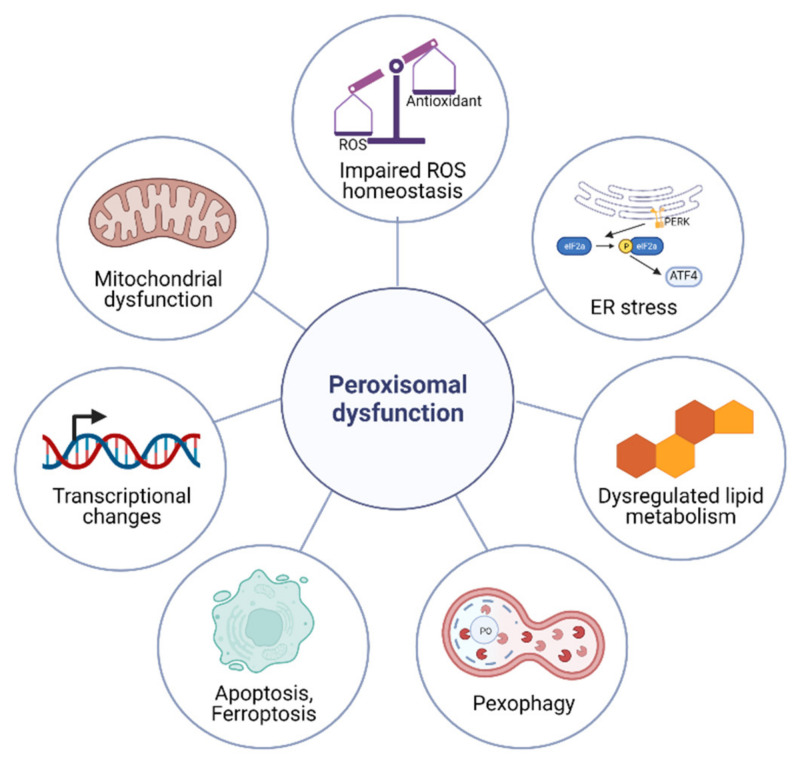
The metabolic functions of peroxisomes are critical for cellular homeostasis, and the impairment of proper peroxisomal function elicits a variety of cellular responses (Figure 1). Here, we propose that there is a signaling pathway that is responsible for sensing defective peroxisomes and activating cytoprotective mechanisms, which we coin as the peroxisomal stress response pathway. In this section, we categorize peroxisome stress responses into seven categories: transcriptional changes, impaired ROS homeostasis, dysregulated lipid metabolism, mitochondrial dysfunction, ER stress, apoptosis and ferroptosis, and pexophagy (Figure 1).
Figure 1.
Cellular responses to peroxisomal dysfunction. Impaired peroxisomal function elicits cellular responses such as the impaired ROS homeostasis, dysregulated lipid metabolism, mitochondrial dysfunction, altered gene expression, pexophagy, elevated ER stress, and apoptosis.
4.1. Transcriptional Changes upon Peroxisomal Dysfunction
Several lines of evidence suggest that an uncharacterized cellular stress response pathway might exist in eukaryotic cells to cope with peroxisomal dysfunction. Recent studies have revealed global transcriptional changes in PEX mutants with impaired peroxisomal import [9,68,69,70,71,72]. Peeters et al. [68] investigated the role of peroxisomes in liver carbohydrate metabolism through a microarray analysis using hepatocyte-specific Pex5 knockout mice (L-Pex5−/− mice). The depletion of Pex5 in hepatocytes significantly suppressed the mRNA levels of two enzymes involved in gluconeogenesis (Pck1, G6pc) as well as the mRNA level of glycogen synthase 2 (Gys2). However, some glycolysis genes (e.g., Aldoa, Pdk4) were upregulated in the Pex5 knockout hepatocytes. Follow-up experiments demonstrated that peroxisomal and mitochondrial abnormalities trigger energy deficits, evidenced by increased cellular AMP/ATP ratios and decreased NAD+/NADH ratios. This causes AMP-activated kinase (AMPK) activation and peroxisome proliferator-activated receptor γ coactivator 1α (PGC-1α) suppression, resulting in the down-regulation of glycogen synthesis and the induction of glycolysis [68].
A recent transcriptome analysis was carried out to study the role of peroxisomes in pancreatic β-cell homeostasis using β-cell-selective Pex5 knockout mice (Rip-Pex5−/−) [69]. Similar to Pex5 knockout hepatocytes (L-Pex5−/−) [73], Pex5-deficient pancreatic β-cells exhibited abnormal mitochondrial shape and reduced complex I activity [69]. The genes involved in apoptosis and β-cell dysfunction, including Cdkn1a, Pmaip11, Pidd1, Txnip, Pitgs, and Thbs2, were up-regulated in the pancreatic β-cells of Pex5 knockout mice. The expression levels of genes with potential anti-apoptotic effects gene, including Sfrp1 and the insulin secretion promoting gene Alox5, were enhanced in islets of Rip-Pex5−/− mice, possibly as a compensatory mechanism [69].
X-linked adrenoleukodystrophy (X-ALD) is a peroxisomal disorder characterized by axonopathy and demyelination in the central nervous system and adrenal insufficiency [74]. The disease is caused by mutations in the ABCD1 gene mapped to chromosome Xq28, which functions as a transporter of VLCFAs and VLCFA-CoA esters into the peroxisome for β-oxidation [70,74]. The classical mouse model of X-ALD is the Abcd1 gene knockout (Abcd1−/−) [75]. Schluter et al. [71] performed a microarray-based functional genomics analysis of the spinal cord of Abcd1 knockout mice which revealed that several key metabolic and cell signaling pathways are involved in X-ALD pathogenesis. Based on this transcriptome analysis, the metabolic and cell signaling pathways involved in mitochondrial dysfunction, ROS production with antioxidant defense impairment, insulin and adipocytokine signaling dysregulation, impaired protein synthesis and turnover, as well as NF-κB mediated pro-inflammatory responses were found to play a potential role in X-ALD pathogenesis [71].
Catalase is an essential antioxidant enzyme predominantly located within peroxisomes that catalyzes the conversion of hydrogen peroxide to oxygen and water. The global knockout of catalase in mice (Cat−/−) resulted in increased oxidative stress and body weight [72]. The transcriptome analysis of liver tissue from Cat−/− mice revealed the differential expression of many metabolic genes, especially those involved in lipid metabolism. For example, catalase knockout resulted in the up-regulation of adipsin (Cfd), cell death-inducing DFFA-like effector C (Cidec), oxysterol binding protein-like 3 (Osbpl3), protein phosphatase 1 regulatory subunit 3G (Ppp1r3g), monoacylglycerol acyltransferase (Mogat1), fatty acid translocase (Cd36), fatty acid synthase (Fasn), endothelial lipase (Lipg), stearoyl-CoA desaturases (Scd1, Scd2, Scd3, Scd4), and alpha1A adrenoceptors (Adra1a). At the same time, the knockout of catalase down-regulated lipoprotein lipase (Lpl), beta2 adrenoceptors (Adrb2), and 3-hydroxy-3-methylglutaryl-CoA reductase (Hmgcr). In addition, the loss of catalase influenced the actions of insulin, down-regulating genes encoding insulin-like growth factor binding protein 1 (Igfbp1) and insulin receptor substrate 2 (Irs2) and up-regulating the insulin receptor substrate 3 (Irs3). These data provide evidence that catalase deficiency plays a vital role in insulin resistance and the development of a pre-diabetic state [72].
Recently, we performed a comparative transcriptomic analysis to interrogate the conserved peroxisomal stress responses between the fruit fly and humans. We generated stable human HEK293 cells with doxycycline-inducible expression of a mutated PEX5 (PEX5C11A), which blocks PEX5 recycling and PEX5-mediated peroxisomal import [9]. PEX5C11A expression decreased the mRNA level of genes involved in mitochondrial oxidative phosphorylation and increased the mRNA level of genes involved in MAPK signaling and Hippo signaling, presumably due to increased ROS production. To identify conserved responses, we performed a transcriptomic analysis on Drosophila with oenocyte-specific Pex1, Pex12, and Pex5 knockdowns (oenocytes are the fly hepatocytes). Our transcriptome analysis showed that oxidative phosphorylation genes were repressed, and the inflammation pathway was induced upon peroxisomal stress in both fly and human cells. Furthermore, we found that peroxisomal dysfunction in both fly and human cells repressed ribosome biogenesis and activated ER stress response pathways, especially the eIF2α-ATF4 pathway, suggesting potential crosstalk between peroxisomes and the ER [9].
Although further investigations are needed to determine the direct mechanisms underlying peroxisome-nucleus communication, recent transcriptomic studies strongly indicate that peroxisomal dysfunction can directly modulate transcriptional activities in the nucleus.
4.2. Impaired ROS Homeostasis
Peroxisomes play critical roles in both the production and scavenging of hydrogen peroxide. Given the essential role of peroxisomes in redox homeostasis, impaired peroxisomal function disrupts cellular ROS homeostasis. Several studies have reported excessive cellular ROS production upon peroxisomal dysfunction. For example, impaired peroxisomal import by knocking down Pex5 in adipocytes significantly elevated cytosolic ROS production [76]. Likewise, peroxisome disfunction associated with Pex13 [77] or Pex11b [78] deficiency led to higher ROS production in lung fibroblasts and neurons, respectively.
The major sources of elevated ROS levels upon peroxisomal dysfunction remain elusive. Presumably, mitochondria are the major contributor to overall cellular oxidative stress under peroxisomal impairment. Multiple studies have shown that mitochondrial ROS are elevated by peroxisomal dysfunction. For example, Walton and Pizzitelli [79] demonstrated that altered peroxisomal oxidative balance associated with the inhibition of catalase activity increased mitochondrial ROS production and decreased the activity of the mitochondrial enzyme aconitase, an enzyme that participates in the Krebs Cycle and is sensitive to oxidative stress. Moreover, the inhibition of catalase activity decreased the inner membrane potential in mitochondria, suggesting that ROS induced by impaired peroxisomal function contribute to mitochondrial dysfunction [79]. Importantly, Ivashchenko et al. [80] demonstrated that peroxisome-derived oxidative stress disturbed the mitochondrial redox balance. In their study, Ivashchenko et al. artificially induced the generation of excessive ROS exclusively inside peroxisomes by employing Killer Red, a genetically encoded photosensitizer that produces radicals and H2O2 upon green light illumination. In combination with a redox-sensitive green fluorescent protein (roGFP), the authors found that mitochondrial redox balance was disturbed by peroxisome-derived oxidative stress [80].
Whether animals with catalase deficiency show elevated ROS production inside peroxisomes themselves remains unclear. Hwang et al. [81] showed that the inhibition of catalase in hepatocytes significantly increased the peroxisomal H2O2 level, as measured by a peroxisome-targeted hydrogen peroxide probe (Hyper-P). However, another study reported that the redox environment of the peroxisomal matrix was not increased in catalase-deficient mouse embryonic fibroblast (MEF) cells [80]. The study measured the oxidation state using peroxisome-specific (roGFP2-PTS1) and mitochondria-specific (mt-roGFP2) ROS-detecting fusion proteins and found that only the redox status of mitochondria was significantly increased by either knocking out catalase activity or treating cells with the catalase inhibitor 3-amino-1,2,4-triazole (3-AT).
4.3. Dysregulated Lipid Metabolism
Peroxisomes contribute to cellular lipid metabolism including the β-oxidation of VLCFAs and the biosynthesis of cholesterol, bile acids, PUFAs, and ether phospholipids. Given the crucial roles of peroxisomes in lipid metabolism, accumulating evidence shows that lipid metabolism is largely altered in response to the impairment of peroxisomes.
VLCFAs are exclusively catabolized into a range of chain-shortened acyl-CoAs by peroxisomal β-oxidation, and the resulting acetyl-CoA, propionyl-CoA, and different medium-chain acyl-CoAs are delivered to mitochondria for further oxidation to CO2 and H2O [59]. Therefore, elevated plasma VLCFAs are associated with the clinical diagnosis of peroxisomal disorders, including X-linked adrenoleukodystrophy (X-ALD) [82,83]. Moser et al. [82] reported elevated plasma levels of VLCFA in patients with X-ALD, ZS, neonatal adrenoleukodystrophy (NALD), infantile Refsum’s disease (IRD), and in patients with deficiencies of peroxisomal acyl-coenzyme A oxidase (ACOX1), D-bifunctional protein (DBP), and 3-oxoacyl-coenzyme A thiolase. The levels of VLCFA in these patients were correlated with the severity of the disease [82]. Another study [84] showed that high levels of serum C26:0 were associated with a short survival time in patients with ZS, DBP, and mild ZS. However, it should be noted that dietary restriction of VLCFA in combination with oral supplementation with Lorenzo’s oil (a 4:1 mixture of glycerol trioleate and glycerol trierucate) reduced VLCFA plasma levels but did not result in clinical improvement [85] nor did it arrest the progression of the disease in X-ALD patients [86], suggesting that the correlation between serum VLCFA levels and clinical severity may not be direct.
Peroxisome deficiency mouse models recapitulate dysregulated lipid metabolism phenotypes seen in human PBD patients [87]. Pex2 knockout mice showed 10-fold increased plasma levels of VLCFAs [88]. Pex13 [89] and Pex5 [90] knockout mice exhibited increased levels of VLCFA in liver and brain tissue compared to wild-type animals. Additionally, the levels of plasmalogen, PUFAs, and DHA were significantly decreased in newborn Pex5 knockout mice compared to normal littermates [91]. Pex7 knockout mice also showed plasmalogen deficiency. Alkyl-glycerols supplementation to Pex7−/− mice restored plasmalogen levels in erythrocytes and several tissues including the kidney, heart, and eye, whereas only a marginal increase was observed in nervous tissues [92]. Hofer et al. [93] showed that peroxisomal fatty acid oxidation was decreased by the knockdown of Pex16 in adipocytes, resulting in the accumulation of VLCFAs and reduced levels of peroxisomal α-oxidation derived odd-chain fatty acids. Furthermore, the cellular oxygen consumption rate was reduced upon Pex16-silencing, suggesting impaired mitochondrial β-oxidation. These findings support the critical role of peroxisomes in lipid homeostasis.
Other model organisms show similar lipid metabolism phenotypes upon the loss of peroxisomes. Rackles et al. [10] showed that the knockdown of prx-5/PEX5 in Caenorhabditis elegans (C. elegans) resulted in increased levels of triacylglycerols with long acyl chains, suggesting reduced β-oxidation activity. In addition, the depletion of prx-5 resulted in reduced biosynthesis of ether phospholipids, which are generated exclusively in peroxisomes. Sellin et al. [94] reported that peroxisome loss in a Drosophila Pex19 mutant (Pex19ΔF7) was associated with the accumulation of VLCFAs.
Cholesterol is a major structural component of cellular membranes, and it serves as a precursor molecule for the synthesis of steroid hormones and bile acids [95]. The biosynthesis of cholesterol consists of multiple processes, beginning with acetyl-CoA. Plasmalogen and acetoacetyl-CoA are converted to 3-hydroxy-3-methylglutaryl-CoA (HMG-CoA) by HMG-CoA synthase. HMG-CoA is then converted to mevalonate by HMG-CoA reductase. Mevalonate is metabolized to farnesyl-diphosphate (farnesyl-PP) by a series of enzymatic reactions catalyzed by enzymes such as mevalonate kinase, phosphomevalonate kinase, mevalonate-PP decarboxylase, isopentenyl-PP isomerase, and farnesyl diphosphate synthase (for the comprehensive steps of cholesterol biosynthesis, see review [96]). All of the enzymes that convert acetyl-CoA to farnesyl-PP are cytosolic enzymes, except for HMG-CoA reductase, which is localized in the ER.
Several lines of evidence suggest that peroxisomes not only have a role in cholesterol oxidation but also in cholesterol biosynthesis. Krisans et al. [97] found that the liver tissue of ZS patients showed significantly decreased activities of enzymes involved in cholesterol biosynthesis, including HMG-CoA reductase, mevalonate kinase (MVK), and phosphomevalonate kinase. In line with these observations, Kovacs et al. [95] showed that Pex2 knockout mice (Pex2−/−) had decreased plasma levels of total and high-density lipoprotein cholesterol compared to wild-type mice. The cholesterol content in the liver tissue of Pex2−/− mice was reduced by about 40% relative to control mice. A follow-up study revealed that the loss of peroxisomes activates ER stress, which leads to the dysregulation of the endogenous sterol response pathway [98].
However, the role of peroxisomes in cholesterol biosynthesis is still debatable. Hogenboom et al. [99] found that the protein levels and activities of key enzymes of cholesterol biosynthesis in the liver homogenates of Pex5 knockout mice were normal. Likewise, cholesterol biosynthesis was not defective in the fibroblasts of ZS patients [100]. In addition, in contrast to the results obtained by Krisans et al. [97], Hogenboom et al. [101,102] found that mevalonate kinase, phosphomevalonate kinase, and mevalonate pyrophosphate decarboxylase were cytosolic, not peroxisomal enzymes.
Peroxisomal dysfunction also affects intracellular cholesterol trafficking from lysosomes to peroxisomes. Chu et al. [103] identified a number of proteins related to peroxisomal function and biogenesis that are required for the transport of low-density lipoprotein-derived cholesterol through genome-wide pooled shRNA screening. The disruption of critical peroxisomal genes, such as ABCD1 and PEX1, resulted in significant decreases in plasma membrane cholesterol levels and the accumulation of cholesterol in lysosomes. These findings reveal an unexpected role of peroxisomes in intracellular cholesterol transport. Furthermore, massive cholesterol accumulation was observed in human patient cells and mouse models of peroxisomal disorder [7,103], demonstrating the clinical relevance of cholesterol transport in peroxisomal disorders.
4.4. Mitochondrial Dysfunction
It has become clear that peroxisomes and mitochondria have a strong interconnection, as they show complementary activities and exchange many metabolites [59,73,104]. The coordinated interplay between peroxisomes and mitochondria is required for diverse metabolic and cellular processes such as the β-oxidation of fatty acids, redox homeostasis, as well as inflammatory and innate immune responses [104]. In line with the close relationship between the two organelles, multiple studies have reported that the loss of functional peroxisomes causes mitochondrial dysfunction [73,89,105,106,107,108,109,110].
Mitochondrial abnormalities have been widely reported in ZS patients. Although the detailed mechanisms remain unsolved, ZS patients exhibit altered structure of the inner mitochondrial membrane and decreased activities of respiratory chain complexes [111,112,113,114]. Accordingly, the depletion of functional peroxisomes in a Pex5 knockout mouse model (L-Pex5−/−) exhibiting selective elimination of liver peroxisomes resulted in mitochondrial abnormalities characterized by an altered inner mitochondrial membrane with twisted or irregular cristae, a dense matrix, and crystalline inclusions [106]. The ultrastructural changes of the mitochondrial inner membrane in Pex5 knockout mice were similar to those observed in ZS patients [114]. In addition, the knockout of Pex2 [107] or Pex13 [89] resulted in swollen mitochondria with abnormally shaped cristae in hepatocytes [73]. Besides the morphological changes, the depletion of Pex5 in hepatocytes reduced mitochondrial DNA content, inhibited the activities of the respiratory chain complex I, III, and V, reduced membrane potential, and increased ROS production [73].
Peroxisomal dysfunction has recently been linked to altered mitochondrial dynamics. Park et al. [110] studied the role of peroxisomes in mitochondrial dynamics and thermogenesis in adipose tissue. The authors demonstrated that the adipose-specific knockout of Pex16 in mice disrupted cold-induced mitochondrial fission, decreased the expression of mitochondrially encoded genes involved in oxidative phosphorylation, and reduced the rate of coupled and uncoupled respiration [110]. In Drosophila, Pex19 mutants showed increased mitochondrial size compared to wild-type flies and had increased levels of etomoxir-sensitive oxygen consumption, suggesting enhanced mitochondrial β-oxidation rates [109].
4.5. Endoplasmic Reticulum (ER) Stress
The ER is the site where secretory and membrane proteins are synthesized, folded, and matured. The accumulation of unfolded or misfolded proteins can activate the ER stress response. In mammalian cells, there are three ER stress pathways mediated through three stress sensors: protein kinase RNA-like ER kinase (PERK), inositol-requiring protein 1 (IRE1), and activating transcription factor 6 (ATF6) [115]. Upon ER stress, PERK phosphorylates eIF2α, leading to translation inhibition and the activation of the transcription factor ATF4 [116,117,118]. On the other hand, membrane-bound RNase IRE1 splices the transcription factor XBP1 pre-mRNA into its mature form, which is translocated to the nucleus to induce the transcription of ER-associated degradation (ERAD) genes [119]. Lastly, the transcription factor ATF6 is transported to the Golgi apparatus and sequentially cleaved by proteases such as S1P and S2P. The mature ATF6 translocates to the nucleus to induce the expression of ER chaperone genes [120].
Several recent studies reported that the impairment of peroxisomes induces ER stress [98,121,122,123]. Kovacs et al. [98] provided the first evidence that Pex2 knockout activated hepatic ER stress pathways in mice by showing increased mRNA expression of ATF4 and its transcriptional targets, such as ATF3, CHOP, and TRIB3. Another study from the same group showed that the phosphorylation of eIF2α was highly induced in newborn Pex2 knockout mice [121]. Accordingly, the silencing of PEX2 in human liver hepatocarcinoma cell lines induced the mRNA expression of ER stress markers such as PERK, Erol-Lα, PDI, and CHOP [122]. Our recent study also supports the link between peroxisomal dysfunction and ER stress [9]. We found that the ER-associated protein degradation (ERAD) pathway was induced in Pex1, Pex5, and Pex12 knockdowns in Drosophila. Similar to mouse studies, the phosphorylated eIF2α was significantly elevated in both peroxin knockdown flies and human PEX5C11A mutant cells. Interestingly, we observed that the level of spliced XBP1 was not altered in both Pex5 knockdown flies and PEX5C11A mutant human cells. Similarly, IRE1α signaling and its RNase activity were not significantly induced in the liver of Pex2 knockout mice [98]. Thus, these results suggest that peroxisomal deficiency activates a specific branch of ER stress pathways. It seems that the PERK-eIF2α-ATF4 branch, but not IRE1α-XBP1, is targeted by peroxisomal dysfunction. As eIF2α-ATF4 signaling is also involved in the integrated stress response (ISR) pathway, peroxisomal dysfunction can likely activate the ISR pathway. It has been proposed that ER stress might be induced by the metabolic changes associated with hepatic Pex2 knockout, such as the perturbed flux of mevalonate metabolites, dysregulated bile acid homeostasis, altered fatty acid levels and composition, and oxidative stress [123]. However, the exact mechanisms by which peroxisomal dysfunction controls ER stress and ISR signaling pathways remain to be determined.
4.6. Apoptosis and Ferroptosis
Peroxisomal dysfunction has been linked to apoptotic cell death. Peroxisome-deficient mice with Pex5 mutations showed elevated apoptotic cell death in the white matter and the cortical plate [90]. Transcriptomic profiling of Pex5 knockout pancreatic β-cells revealed the up-regulation of genes involved in apoptosis such as Cdkn1a, Pmaip11, and Pidd1. Results from the TUNEL assay further confirmed that apoptosis was increased in the β-cells of Pex5 mutants [69]. Similarly, knockout of Pex5 in the developing mouse cerebellum showed significantly higher numbers of caspase-3-positive cells, compared to control littermates [124]. Peroxisomal dysfunction associated with Pex16 deficiency in human skin fibroblast cells resulted in increased apoptotic cell death [125]. In addition, mouse embryonic fibroblast (MEF) with either Pex3 or Pex5 knockout showed elevated cytochrome c levels in the cytoplasm and an increase in the amounts of cleaved caspase-9 and caspase-3. The cell death phenotypes were rescued by the overexpression of Pex3 or Pex5 in the corresponding knockout MEFs, suggesting that peroxisomal dysfunction modulates caspase activity and apoptosis [126].
Recently, peroxisomes were shown to play an important role in ferroptosis, a unique process of nonapoptotic cell death caused by the accumulation of iron-dependent lipid peroxides [127]. Ferroptosis differs from other forms of cell death including apoptosis because it does not require caspase activation. Instead, increased activity of lipoxygenase and cytochrome P450 oxidoreductase is responsible for lipid peroxidation. In particular, the oxidation of PUFAs is a key driver of ferroptosis [127]. In a recent genome-wide CRISPR screen combined with lipidomic profiling, Zou et al. [128] reported that polyunsaturated ether phospholipids (PUFA-ePLs) synthesized in the peroxisome act as substrates for lipid peroxidation, resulting in the induction of ferroptosis in human renal and ovarian carcinoma cells. Carcinoma cells can evade ferroptosis through the downregulation of PUFA-ePLs. Although plasmalogens were previously described as cellular antioxidants, specific PUFA-ePLs may be pro-ferroptotic and act as key regulators in ferroptosis-associated pathologies [128].
4.7. Autophagy and Pexophagy
Peroxisomal homeostasis is maintained by the coordination of peroxisomal biogenesis and degradation. Peroxisomes have a half-life of 1.5 to 2 days, suggesting that peroxisomal homeostasis is very dynamic [129]. In mammals, three independent mechanisms have been proposed for peroxisome degradation, including Lon protease-mediated matrix protein removal, 15-lipoxygenase-mediated autolysis, and pexophagy [130]. Peroxisomal Lon protease 2 (LONP2) is a homo-oligomeric ATP-dependent protease with chaperone-like activity, and LONP2 is responsible for the degradation of excessive and unnecessary matrix proteins, such as β-oxidation enzymes [131,132]. 15-lipoxygenase (15-LOX) is responsible for the autolysis of the peroxisomal membrane by the peroxidation of membrane lipids [133].
However, the major degradation pathway of peroxisomes is pexophagy. Pexophagy is a type of macroautophagy, and 80% of peroxisomes are removed by this process [134]. Like other macroautophagy processes, pexophagy includes three major steps: (1) autophagy receptors NBR1 and p62 recognize ubiquitinated peroxisomal membrane proteins, (2) target peroxisomes are sequestered by autophagosome, and (3) sequestered peroxisomes are delivered to the lysosome for degradation [135].
The ubiquitination of PEX5 plays a key role in maintaining peroxisome homeostasis. Under normal conditions, PEX5 is usually ubiquitinated at conserved cysteine 11 residue by the RING (Really Interesting New Gene) E3 ligase complex that consists of PEX2, PEX10, and PEX12. Then, monoubiquitinated PEX5 facilitates its release from peroxisomes by the AAA-ATPase complex (PEX1, PEX6, and PEX26). The loss of peroxisomal AAA-complex function is commonly found in peroxisomal biogenesis disorders (PBDs) [136]. PBD patients with mutations in the AAA-complex show decreased peroxisomal number and function [2]. Law et al. [137] demonstrated that the loss of AAA-complex function in mammalian cells resulted in the accumulation of ubiquitinated PEX5 on the peroxisomal membrane that triggers peroxisomal degradation by NBR1-dependent pexophagy. In addition, the authors showed that autophagy inhibitors restored peroxisome number and matrix protein import in PEX1-mutated PBD fibroblasts, suggesting that the peroxisomal AAA-complex is required for peroxisomal quality control and the regulation of pexophagy [137]. However, conflicting findings were recently reported. Klouwer et al. [138] found that autophagy inhibitors, including hydroxychloroquine, did not improve peroxisomal metabolic functions and peroxisomal matrix protein import but, in fact, caused a further decrease of peroxisomal functions in the primary skin fibroblast cells of PBD patients. Thus, further investigations are needed to confirm the beneficial roles of autophagy inhibitors in PBD treatment [138].
Interestingly, the loss of peroxisomal function not only induces pexophagy but also alters other macroautophagy processes, such as lipophagy [139]. In the lipid metabolic process, besides cytosolic lipolysis, triglycerides can be hydrolyzed by lipophagy. Lipophagy plays a crucial role in lipid degradation through the engulfment of lipid droplets within the autophagosomes and hydrolysis of triglycerides by lysosomal acid lipase A (LIPA/LAL) to free fatty acid and glycerol [140,141]. Recently, He et al. [139] demonstrated that hepatocyte-specific knockout of the peroxisomal β-oxidation enzyme Acox1 induced autophagic degradation of lipid droplets and protected mice from hepatic steatosis induced by starvation or a high-fat diet. These results suggest that peroxisome-derived acetyl-CoA plays an important role in the regulation of lipophagy.
The role of peroxisomes in the regulation of the autophagic degradation of other organelles has just started to be uncovered. To date, several selective autophagic pathways have been discovered: mitophagy (mitochondria), proteaphagy (proteasomes), ribophagy (ribosomes), ER-phagy (ER), lysophagy (lysosome), nucleophagy (nuclei), and pexophagy (peroxisome) [142]. Since peroxisomes are functionally connected with other organelles, it would be interesting to further investigate whether and how peroxisomal dysfunction affects selective autophagic processes in organelle clearance and homeostasis.
5. Peroxisome-Organelle Communication
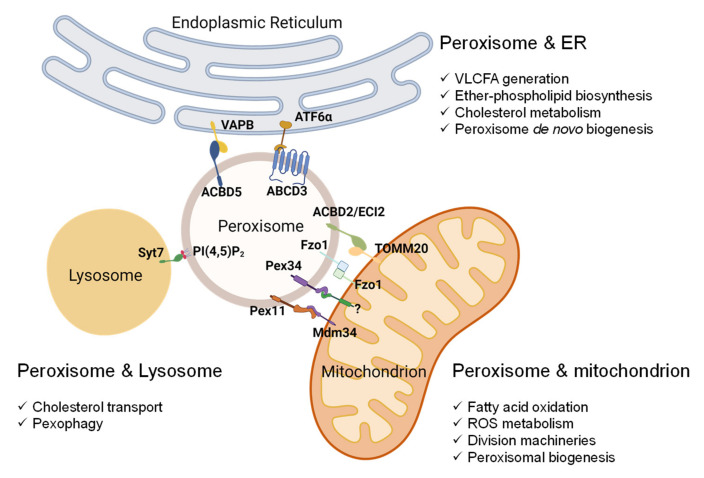
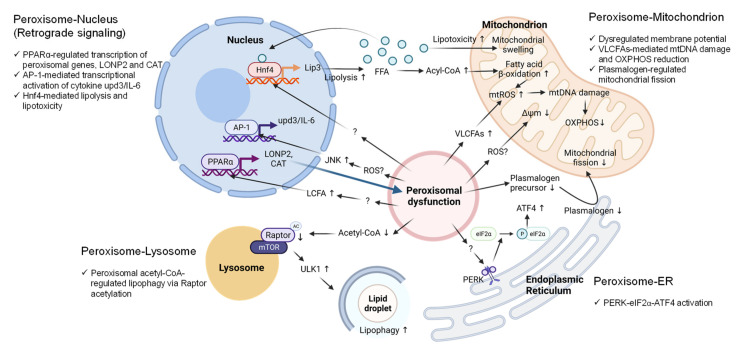
Peroxisomes are multifunctional and dynamic organelles that actively contribute to cellular signaling, cell fate, immunity and inflammation, and aging [6]. To accomplish these cellular activities, peroxisomes interact and coordinate with other subcellular organelles, such as mitochondria, ER, lysosomes, and lipid droplets [6,59,104]. The cellular changes that accompany peroxisomal dysfunction, discussed in Section 4, are strongly associated with peroxisome-organelle crosstalk. In this section, we summarize the current knowledge on peroxisome-organelle communication involving membrane contact sites, peroxisome-derived signaling metabolites, and retrograde signaling (Figure 2 and Figure 3). In addition, we highlight some of the potential mechanisms by which inter-organelle communication contributes to peroxisomal stress responses.
Figure 2.
Peroxisome-organelle membrane contact sites and their roles in organelle functions. Peroxisomes’ contact with mitochondria involves (1) peroxisomal Pex11 and mitochondrial Mdm34, (2) peroxisomal Pex34 and an unknown mitochondrial protein, (3) mitofusin Fzo1 on both peroxisome and mitochondria, and (4) peroxisomal ACBD2/ECI2 and mitochondrial TOMM20. The interaction between peroxisomes and the ER involves (1) peroxisomal ACBD5 and resident ER protein VAPB and (2) peroxisomal ABCD3 and ER protein ATF6α upon Ceapin treatment. In mammalian cells, the contact between peroxisomes and lysosomes involves phospholipid PI(4,5)P2 on the peroxisomal membrane and lysosomal Syt7. Abbreviations: Pex11, peroxin 11; Mdm34, mitochondrial distribution and morphology protein 34; Pex34, peroxin 34; Fzo1, mitofusin; ACBD2/ECI2, acyl-coenzyme A-binding domain or enoyl-CoA-δ isomerase 2; TOMM20, translocase of outer mitochondrial membrane 20; ACBD5, acyl-CoA binding domain-containing protein 5; VAPB, vesicle-associated membrane protein-associated protein B/C; ABCD3, ATP binding cassette subfamily D member 3; ATF6, activating transcription factor 6; PI(4,5)P2, phosphatidylinositol 4,5-bisphosphate; Syt7, synaptotagmin VII.
Figure 3.
Metabolic and molecular signaling pathways mediate peroxisome-organelle crosstalk in response to peroxisomal dysfunction. (1) Peroxisome-nucleus: Peroxisomal dysfunction activates nuclear gene transcription through the transcription factors PPARα, AP-1, or Hnf4. The accumulation of long-chain fatty acids (LCFAs) activates PPARα to upregulate LONP2 and CAT expression to restore peroxisomal function (Blue arrow). Elevated ROS activates JNK signaling and AP-1 to induce the transcription of the pro-inflammatory cytokine IL-6. Peroxisomal dysfunction activates Hnf4 through unknown mechanisms to induce the expression of lipase 3 (Lip3), which leads to excessive free fatty acids (FFA) in the cytoplasm. FFAs hyper-activate Hnf4 via a positive feedback loop. (2) Peroxisome-mitochondrion: Peroxisomal dysfunction causes mitochondrial swelling, mitochondrial ROS generation, mitochondrial DNA (mtDNA) damage, disruption of oxidative phosphorylation (OXPHOS), and decreased inner membrane potential. Excessive ROS and elevated VLCFA are the potential signaling molecules that mediate the peroxisome-mitochondrion crosstalk. Peroxisomal dysfunction decreases plasmalogen, resulting in the inhibition of mitochondrial fission. (3) Peroxisome-ER: Peroxisomal dysfunction activates PERK signaling through unknown mechanisms to increase the phosphorylation of eIF2α and ATF4 induction. (4) Peroxisome-lysosome: Peroxisomal dysfunction due to the loss of Acox1 decreases peroxisome-derived acetyl-CoA, resulting in Raptor acetylation and lysosome localization of mTOR, leading to ULK1 activation and elevated lipophagy. Abbreviations: PPARα, peroxisome proliferator activated receptor alpha; AP-1, activator protein-1; Hnf4, hepatocyte nuclear factor 4; LONP2, lon peptidase 2; CAT, catalase; upd3, unpaired 3; IL-6, interleukin 6; Lip3, lipase 3; ROS, reactive oxygen species; JNK, Jun N-terminal kinase; VLCFAs, very-long-chain fatty acids; PERK, protein kinase RNA-like endoplasmic reticulum kinase; eIF2α, eukaryotic translation initiation factor 2a, ATF4, activating transcription factor 4; mTOR, mechanistic target of rapamycin kinase; ULK1, Unc-51-like autophagy-activating kinase 1.
5.1. Peroxisome-Nucleus Crosstalk
All peroxisomal genes are encoded in the nucleus, and peroxisomal proteins are imported to either the peroxisomal membrane or matrix after well-coordinated transcription and translation processes [143]. In mammals, peroxisomal proliferation and lipid metabolism are regulated by nuclear transcription factors including the nuclear receptor peroxisomal proliferator-activated receptor alpha (PPARα) [144]. PPARα acts as a receptor for various compounds. It can be activated by natural fatty acids, such as acyl-CoAs, oxidized fatty acids, eicosanoids, and phytanic acid. PPARα can also be activated by synthetic compounds such as fibrates [144]. The activation of PPARα induces the expression of genes involved in peroxisomal fatty acid β-oxidation, as well as genes involved in peroxisomal biogenesis (PEX genes) [145].
Several transcriptomic studies have revealed that peroxisomal dysfunction triggers global transcriptional changes [9,68,69,70,71,72]. However, how cells relay the peroxisomal stress signal to the nucleus (retrograde signaling) remains largely unclear. Organelle retrograde signaling is well established in the case of mitochondria-nucleus and ER-nucleus crosstalk. A recent study suggests that peroxisomal retrograde signaling might also exist in eukaryotic cells [10]. Rackles et al. [10] found that peroxisomal import stress associated with prx-5/PEX5 knockdown in C. elegans induced the expression of peroxisomal Lon protease lonp-2/LONP2 and catalase ctl-2/CAT through the activation of NHR-49/PPARα and its co-factor MDT-15/MED15. Lipidomic analysis revealed that peroxisomal stress increased the levels of long-chain fatty acids due to reduced peroxisomal β-oxidation. Given that PPARα is activated by natural fatty acids, the authors proposed that excessive long-chain fatty acids associated with peroxisomal import stress might serve as the signal that relays peroxisomal stress to the nucleus [10].
In our recent study, we reported that the hepatocyte-specific knockdown of Pex5 in Drosophila induced the expression of the inflammatory cytokine upd3, the fly homolog of mammalian interleukin 6 (IL-6), in a JNK-dependent manner [14]. We further showed that the AP-1 transcription factors induced by Pex5 knockdown were required for the transcriptional activation of upd3/IL-6 and systemic inflammation in flies [14]. Elevated ROS in Pex5 knockdown flies likely activates JNK signaling, which promotes nuclear AP-1 activity and the transcriptional activation of AP-1 target genes, including genes involved in inflammation and oxidative stress.
In Drosophila, the loss of Pex19 enhanced mitochondrial β-oxidation and induced mitochondrial swelling [109]. The hepatocyte nuclear factor 4 (Hnf4) was identified as a key regulator of mitochondrial dysfunction in Pex19 mutant flies [109]. Hnf4 is an important transcription factor that regulates mitochondrial fatty acid β-oxidation [146] and insulin secretion [147]. Mutations in Pex19 activated Hnf4 and consequentially upregulated the expression of lipase 3 (Lip3) and lipolysis. The authors proposed that Hnf4-mediated lipotoxicity and accumulation of free fatty acids (FFAs) are the causes of mitochondrial damage (e.g., elevated ROS) in Pex19 mutant flies [109]. The study also revealed that peroxisome deficiency not only triggers the accumulation of VLCFAs but also causes the depletion of shorter fatty acids. Consequently, lipolysis is elevated to produce high levels of FFAs, which hyper-activates Hnf4 signaling, further enhancing lipolysis and lipotoxicity (Figure 3).
5.2. Peroxisome-Mitochondrion Crosstalk
Peroxisomes and mitochondria share many common features. They metabolically cooperate in fatty acid β-oxidation and ROS metabolism [104]. The two organelles contain distinct sets of substrate-specific enzymes for fatty acid β-oxidation: VLCFAs are chain-shortened in the peroxisome, and then the medium- or short-chain fatty acids metabolites are guided to the mitochondria for further oxidation to CO2 and H2O as well as ATP production [6,148]. Moreover, the two organelles share multiple components of their division machinery including DRP1, FIS1, MFF, and ganglioside-induced differentiation-associated protein (GDAP1) [104].
The crosstalk between peroxisome and mitochondria is also supported by physical interaction through membrane contact sites. Recently, Shai et al. [149] reported two novel tethers (Fzo1 and Pex34) for peroxisome-mitochondrion contact in yeast. The peroxisomal membrane protein Pex34 potentially contributes to the transfer of β-oxidation products to mitochondria through the interaction with an unknown mitochondrial protein. Fzo1 on mitochondria may mediate mitochondria–peroxisome tethering either by interacting with the Fzo1 on the peroxisome or with another peroxisomal protein [149]. Several other tethers between peroxisomes and mitochondria have also been identified. For example, Pex11 on peroxisome to Mdm34 on mitochondria [150]; ABCD1 on peroxisome to unknown mitochondrial protein [151]; and, in mammals, ECI2 (enoyl-CoA delta isomerase 2, also known as ACBD2) on peroxisome to TOMM20 (translocase of outer mitochondrial membrane 20) on mitochondria [152] (Figure 2).
Mitochondria-derived vesicles (MDVs) have been identified as an intracellular transport route between mitochondria and peroxisomes [153]. Neuspiel et al. [153] showed that MDVs were formed independently of DRP1. Interestingly, MDVs containing MAPL, a mitochondrial small ubiquitin-like modifier E3 ligase, are targeted to fuse with a subset of peroxisomes. This study provided the first evidence of a direct relationship between the two organelles. Furthermore, the same group recently demonstrated that MDVs fused with ER-derived pre-peroxisomes to form mature functional peroxisomes [18].
As VLCFAs are catabolized into a range of chain-shortened fatty acids in peroxisomes and then fully oxidized in mitochondria, the metabolic intermediates produced from fatty acid β-oxidation could serve as metabolic signals in the communication between peroxisome and mitochondria. ABCD1 is a key transporter that delivers VLCFAs into the peroxisome for β-oxidation. The loss of ABCD1 transporter in mice caused the accumulation of VLCFAs in the cytosol [75,154] accompanied by late-onset axonal degradation in the spinal cord and movement problems resembling the most common phenotype in X-ALD patients [155]. Lopez-Erauskin et al. [108] showed that impaired peroxisomal function due to the loss of Abcd1 in the spinal cord resulted in severe mitochondrial abnormalities, such as the down-regulation of oxidative phosphorylation and mtDNA damage [108]. The authors also demonstrated that exposure of human fibroblasts of X-ALD patients to C26:0 caused mitochondrial dysfunction by increasing mitochondrial ROS production, mitochondrial oxidative damage to DNA and proteins, and eventually the disruption of oxidative phosphorylation [108]. However, Oezen et al. [156] reported that mitochondrial respiration in the skeletal muscle cells of Abcd1-knockout mice was normal, regardless of the accumulation of cytosolic VLCFAs. Moreover, mitochondrial morphology parameters such as size and structure in the muscle cells of X-ALD and control mice did not differ [156]. Taken together, mitochondrial susceptibility to accumulated VLCFAs may vary among tissues and cell types.
Plasmalogen is the most common form of ether lipids, and the initial steps of ether lipid biosynthesis take place in peroxisomes. Peroxisome-derived plasmalogen is responsible for mitochondrial dynamics and function [110]. The inhibition of plasmalogen synthesis by knocking down GNPAT, an enzyme responsible for the first step in plasmalogen biosynthesis, resulted in altered mitochondrial morphology and decreased mtDNA content. Similar to Pex16 knockout, GNPAT knockdown resulted in elongated mitochondria, suggesting the potential disruption of mitochondrial fission [110]. Interestingly, high levels of plasmalogens were detected in the mitochondrial membrane [110], indicating that peroxisome-derived plasmalogen might be an important signal molecule that acts on the mitochondrial membrane to regulate mitochondrial membrane dynamics, especially the mitochondrial fission process (Figure 3).
5.3. Peroxisome-ER Crosstalk
Similar to peroxisome-mitochondrion crosstalk, the interaction between peroxisomes and ER was observed in the early years of peroxisome research [157,158]. Electron micrographs revealed that the two organelles are adjacent to each other, and peroxisomes are frequently seen wrapped around the ER membrane, implying a close connection between the two organelles [5,157,158]. Indeed, the membrane contact sites of peroxisome-ER have been recently discovered in mammalian cells [159,160]. Acyl-coenzyme A binding domain protein 5 (ACBD5) on the peroxisome membrane binds to the resident ER protein vesicle-associated membrane protein-associated protein B (VAPB). The interaction between the FFAT-like motif (two phenylalanines in an acidic tract) of ACBD5 and the MSP (major sperm protein) domain of the VAPB protein mediates the close association between the two organelles [161].
Peroxisome-ER communication plays an important role in maintaining lipid homeostasis, as the two organelles coordinate many lipid metabolic processes. For example, fatty acid oxidation in the peroxisome is strongly dependent on the crosstalk with the ER, since VLCFAs originate from the ER. Most of VLCFAs are not derived from dietary sources but synthesized from shorter-chain fatty acids through the fatty acid synthase (FAS) complex followed by the chain-elongation system localized in ER [162]. The physical interaction between peroxisome and ER is important for intracellular VLCFAs homeostasis since the genetic deficiency of ACBD5 results in the accumulation of VLCFAs [163]. In addition, peroxisome-ER interaction is also crucial for the biosynthesis of ether phospholipids, which is initiated in peroxisomes and completed in the ER. The loss of ACBD5 in fibroblasts resulted in a significant decrease in ether phospholipid biosynthesis, supporting the key roles of peroxisome-ER contact in the biosynthesis of ether phospholipids [164]. In addition, the disruption of peroxisome-ER contact inhibited peroxisomal membrane expansion and led to the formation of shorter peroxisomal membrane tubules and spherical organelles, suggesting a role for ACBD5-VAPB contact in peroxisomal membrane dynamics [160] (Figure 2).
Recently, Torres et al. [165] identified another peroxisome-ER tether mediated by the interaction between the peroxisomal fatty acid transporter ABCD3 and the ER-resident stress sensor ATF6α upon treatment with Ceapins, a new class of UPR inhibitor [165]. Treatment with Ceapins induced an ER-peroxisome association by tethering ATF6α to ABCD3, blocking its translocation to the Golgi apparatus [165,166,167] (Figure 2). As discussed in Section 4.5, recent studies show that peroxisomal dysfunction can activate ER stress response pathways, especially the PERK-eIF2α-ATF4 axis [98,121,122,123] (Figure 3). However, the underlying mechanisms for peroxisome-regulated ER stress response remain unknown. Does peroxisomal dysfunction activate PERK signaling through peroxisome-ER contact sites, similar to the interaction between ATF6α and ABCD3? Or is metabolic signaling (e.g., via VLCFAs) involved in the activation of PERK signaling? Future work is needed to address these possibilities.
5.4. Peroxisome-Lysosome Crosstalk
Lysosomes play an important role in the degradation of biomolecules, including unwanted fatty acids in cells. Several lines of evidence have demonstrated a strong link between peroxisomes and lysosomes. For instance, Chu et al. [103] demonstrated the physical interaction between lysosomes and peroxisomes mediated through the interaction between lysosomal synaptotagmin VII (Syt7) and the peroxisome membrane-bound phosphatidylinositol 4,5-bisphosphate (PI (4,5) P2) (Figure 2). These lysosome-peroxisome membrane contacts are essential for the transport of cholesterol from lysosomes to peroxisomes. Kleinecke et al. [168] provided in vivo evidence for functional interactions between peroxisomes and lysosomes. The authors showed that peroxisomal dysfunction associated with Schwann cell-specific Pex5 knockout caused the impairment of lysosomes in peripheral nerves, resulting in the perturbation of normal ganglioside turnover. This led to the abnormal distribution of potassium ion channels, possibly disturbing the proper signal transmission in the peripheral nerves of Schwann cell-specific Pex5 knockout mice [168].
Peroxisomes have also been shown to interact with the autophagy-lysosome system. He et al. [139] showed that hepatocyte-specific Acox1 knockout mice were protected from high-fat diet-induced liver steatosis and fatty liver diseases. The study further showed that the loss of Acox1 led to decreased acetyl-CoA levels and the acetylation of Raptor, a key subunit of mTORC1, which likely induced autophagy through Unc-51-like autophagy-activating kinase 1 (ULK1). These findings suggest that peroxisomal acetyl-CoA might act as an important signaling metabolite to regulate mTORC1, lipophagy, and lipid homeostasis [139] (Figure 3).
6. Peroxisomal Dysfunction in Aging and Aging-Related Diseases
Several lines of evidence suggest that peroxisomal dysfunction is an underappreciated cause of aging [11,12,13,14]. Peroxisomal protein import is known to be compromised in aged tissues [11,12,13,14], and almost all peroxisomal proteins are downregulated during aging [8,13]. In senescent human fibroblasts, catalase import was significantly reduced, leading to the accumulation of H2O2 and the further disruption of peroxisome import [11]. Conversely, the overexpression of Pex5 has been shown to restore peroxisomal import function and preserve cardiac health in aged oenocytes [14]. Importantly, Sebastiani et al. [169] studied the proteomic signatures of centenarians and identified that proteins encoding components of peroxisomes were significantly downregulated in centenarians’ serum compared with younger individuals. In addition, the bile acid metabolism pathway and cholesterol homeostasis pathway were also downregulated in centenarians. These studies provide strong evidence for a role of impaired peroxisomal homeostasis in aging.
As peroxisomal activities decline with age [170], it has been suggested that peroxisomal dysfunctions might be associated with the pathogenesis of age-related neurodegenerative disease, including Alzheimer’s disease [171], Parkinson’s disease [172], and amyotrophic lateral sclerosis [173]), as well as age-related metabolic disease, such as cardiovascular disease [174], obesity [76], diabetes [175], and nonalcoholic liver disease [176]. These age-related pathologies are likely due to increased oxidative stress [177,178] and decreased plasmalogen synthesis [179]. In this section, we summarize the current knowledge about the role of peroxisomes in several age-related diseases.
Alzheimer’s disease (AD) is the most common neurodegenerative disease in the elderly. It is characterized by the progressive loss of synapses and neurons especially in the frontal cortex and hippocampus accompanied by significant memory loss and cognitive impairment [180,181]. The pathological hallmarks of AD are the accumulation of the extracellular beta-amyloid (Aβ) plaques and intracellular fibrillary deposits of hyperphosphorylated tau protein (neurofibrillary tangles). Oxidative stress is thought to be a primary culprit in AD pathogenesis [182,183]. Accordingly, the hippocampus of AD mice was found to exhibit high levels of markers of lipid peroxidation and DNA/RNA oxidation [182]. Several lines of evidence suggest a link between peroxisomal dysfunction and AD pathogenesis. The accumulation of VLCFAs and decreased plasmalogen levels were observed in the cortical regions of AD patients [184]. Also, the levels of DHA in the brain and liver tissue of AD patients were reduced compared to those in control individuals [185]. Impaired peroxisomal function might also contribute to alterations of peroxisomal metabolites in AD pathology. Shi et al. [186] showed that the inhibition of peroxisomal β-oxidation increased the level of VLCFAs and Aβ contents in rat cerebral cortex. On the other hand, treatment with peroxisome proliferators attenuated AD-related pathology and improved spatial memory in transgenic mice models of AD [187]. Although peroxisomal dysfunction is associated with AD pathogenesis, whether decreased peroxisomal activity is the primary cause, bystander, or consequence in AD pathology remains to be determined [188].
Cardiovascular diseases (CVDs) are the major cause of death in elderly populations [189], and the prevalence of CVDs has been shown to increase with age [190]. Aging plays a critical role in the impairment of the cardiovascular system and increases the risk of CVDs [191]. Peroxisomal dysfunction has been implicated in CVDs. For instance, cardiac-specific overexpression of catalase, predominantly located in peroxisomes [192], was found to prevent the progression to overt heart failure [174]. In addition, catalase activity is significantly decreased in failing myocardium [193]. Refsum’s disease is a peroxisomal disorder caused by the impaired α-oxidation of branched-chain fatty acids, and patients with Refsum’s disease develop cardiac arrhythmia and heart failure later in life [194,195,196]. We recently demonstrated that peroxisomal dysfunction in Drosophila liver induced cardiac arrhythmia through the production of inflammatory cytokine upd3/IL-6 [14]. We showed that the production of upd3/IL-6 activated the cardiac JAK-STAT signaling pathway and induced cardiac arrhythmia. Our studies provide direct evidence connecting peroxisomal dysfunction to systemic inflammation and age-related cardiomyopathy [14].
Aging is accompanied by changes in the distribution and composition of adipose tissue, particularly an increase in fat deposition within the white adipose tissue (abdominal obesity), which is a major contributor to insulin resistance and metabolic syndrome [197,198,199]. As life expectancy increases, the prevalence of obesity has also risen steadily among the elderly [199]. A recent study demonstrated that peroxisomes play an important role in adipose dysfunction associated with obesity [76]. The authors found that obese mice exhibited downregulation of peroxisomal genes in white adipose tissue, and the knockdown of Pex5 increased ROS levels and inflammation in adipocytes. Accordingly, catalase knockout mice also showed accelerated obesity compared to control mice. These phenotypes were attenuated by improving peroxisomal biogenesis through treatment with the PPARα agonist fenofibrate [76]. Additionally, catalase-deficient patients frequently show diabetic pathology, presumably due to the accumulation of oxidative damage in pancreatic β-cells [200].
7. Concluding Remark
Aside from their role in metabolic regulation, peroxisomes have emerged as a regulatory hub for maintaining cellular and metabolic homeostasis. The perturbation of peroxisomal function has been linked to tissue functional decline and age-related diseases. Recent in vitro and in vivo studies have revealed a close connection between peroxisomes and other subcellular organelles. These inter-organelle communications, often through organelle membrane contact sites, are essential for maintaining normal peroxisome function, as well as the homeostasis of other organelles. It is evident that a homeostatic signaling pathway exists in eukaryotic cells to cope with malfunctioning peroxisomes and to protect cells from damages, as various cellular and metabolic changes are reported upon peroxisomal dysfunction. These findings open a new avenue for research on the “peroxisomal stress response pathway”.
Cellular stress responses are the mechanisms by which cells adapt to stressful conditions in order to restore normal cellular function [201]. Although peroxisome disfunction significantly contributes to the loss of cellular homeostasis and the activation of many cellular signaling pathways (e.g., ER stress), the cellular mechanisms by which the cell senses malfunctioning peroxisomes and activates the appropriate cytoprotective responses are still largely unknown. To fully characterize the peroxisomal stress response pathway, further research is needed to identify novel signaling molecules (including signaling metabolites) that relay peroxisomal stress to other parts of the cell and modulate the functions of other subcellular organelles. Advanced imaging techniques, including super-resolution live-cell imaging, will greatly facilitate the analysis of organelle membrane contact sites and membrane dynamics. Targeted lipidomics analysis of putative signaling metabolites will reveal new metabolic signaling pathways that mediate peroxisome-organelle crosstalk and metabolic homeostasis. Lastly, since peroxisomal dysfunction has been implicated in aging and aging-related diseases, such as Alzheimer’s disease, cardiovascular diseases, and diabetes, understanding peroxisomal stress responses will shed light on the potential of targeting the peroxisome as a therapeutic approach for aging-related diseases.
Acknowledgments
We apologize for those works that we could not include in this review article due to the space constriction. We sincerely thank the editor and anonymous peer-reviewers for the critical reading and helpful comments on earlier drafts of the manuscript.
Author Contributions
J.K. and H.B. wrote the paper. J.K. generated the figures with BioRender.com. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by NIH R01AG058741 and NSF CAREER 2046984.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Klouwer F.C., Berendse K., Ferdinandusse S., Wanders R.J., Engelen M. Zellweger spectrum disorders: Clinical overview and management approach. Orphanet J. Rare. Dis. 2015;10:151. doi: 10.1186/s13023-015-0368-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Waterham H.R., Ferdinandusse S., Wanders R.J. Human disorders of peroxisome metabolism and biogenesis. Biochim. Biophys. Acta. 2016;1863:922–933. doi: 10.1016/j.bbamcr.2015.11.015. [DOI] [PubMed] [Google Scholar]
- 3.He A., Dean J.M., Lodhi I.J. Peroxisomes as cellular adaptors to metabolic and environmental stress. Trends Cell Biol. 2021;31:656–670. doi: 10.1016/j.tcb.2021.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wanders R.J. Metabolic functions of peroxisomes in health and disease. Biochimie. 2014;98:36–44. doi: 10.1016/j.biochi.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 5.Schrader M., Kamoshita M., Islinger M. Organelle interplay-peroxisome interactions in health and disease. J. Inherit. Metab. Dis. 2020;43:71–89. doi: 10.1002/jimd.12083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lin T.K., Lin K.J., Lin K.L., Liou C.W., Chen S.D., Chuang Y.C., Wang P.W., Chuang J.H., Wang T.J. When Friendship Turns Sour: Effective Communication Between Mitochondria and Intracellular Organelles in Parkinson’s Disease. Front. Cell Dev. Biol. 2020;8:607392. doi: 10.3389/fcell.2020.607392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jin Y., Strunk B.S., Weisman L.S. Close encounters of the lysosome-peroxisome kind. Cell. 2015;161:197–198. doi: 10.1016/j.cell.2015.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Huang K., Chen W., Zhu F., Li P., Li P.W.-L., Kapahi P., Bai H. RiboTag translatomic profiling of Drosophila oenocytes under aging and induced oxidative stress. BMC Genom. 2019;20:50. doi: 10.1186/s12864-018-5404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang K., Kim J., Vo P., Miao T., Bai H. Peroxisome import stress impairs ribosome biogenesis and induces integrative stress response through eIF2α phosphorylation. bioRxiv. 2021 doi: 10.1101/2020.11.19.390609. [DOI] [Google Scholar]
- 10.Rackles E., Witting M., Forné I., Zhang X., Zacherl J., Schrott S., Fischer C., Ewbank J.J., Osman C., Imhof A., et al. Reduced peroxisomal import triggers peroxisomal retrograde signaling. Cell Rep. 2021;34:108653. doi: 10.1016/j.celrep.2020.108653. [DOI] [PubMed] [Google Scholar]
- 11.Legakis J.E., Koepke J.I., Jedeszko C., Barlaskar F., Terlecky L.J., Edwards H.J., Walton P.A., Terlecky S.R. Peroxisome senescence in human fibroblasts. Mol. Biol. Cell. 2002;13:4243–4255. doi: 10.1091/mbc.e02-06-0322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giordano C.R., Terlecky S.R. Peroxisomes, cell senescence, and rates of aging. Biochim. Biophys. Acta Mol. Basis Dis. 2012;1822:1358–1362. doi: 10.1016/j.bbadis.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Narayan V., Ly T., Pourkarimi E., Murillo A.B., Gartner A., Lamond A., Kenyon C. Deep Proteome Analysis Identifies Age-Related Processes in C. elegans. Cell Syst. 2016;3:144–159. doi: 10.1016/j.cels.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Huang K., Miao T., Chang K., Kim J., Kang P., Jiang Q., Simmonds A.J., Di Cara F., Bai H. Impaired peroxisomal import in Drosophila oenocytes causes cardiac dysfunction by inducing upd3 as a peroxikine. Nat. Commun. 2020;11:2943. doi: 10.1038/s41467-020-16781-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Islinger M., Cardoso M., Schrader M. Be different—The diversity of peroxisomes in the animal kingdom. Biochim. et Biophys. Acta. 2010;1803:881–897. doi: 10.1016/j.bbamcr.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 16.Huybrechts S.J., Van Veldhoven P.P., Brees C., Mannaerts G.P., Los G.V., Fransen M. Peroxisome Dynamics in Cultured Mammalian Cells. Traffic. 2009;10:1722–1733. doi: 10.1111/j.1600-0854.2009.00970.x. [DOI] [PubMed] [Google Scholar]
- 17.Lodhi I.J., Semenkovich C.F. Peroxisomes: A Nexus for Lipid Metabolism and Cellular Signaling. Cell Metab. 2014;19:380–392. doi: 10.1016/j.cmet.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sugiura A., Mattie S., Prudent J., McBride H.M. Newly born peroxisomes are a hybrid of mitochondrial and ER-derived pre-peroxisomes. Nature. 2017;542:251–254. doi: 10.1038/nature21375. [DOI] [PubMed] [Google Scholar]
- 19.Van der Zand A., Gent J., Braakman I., Tabak H.F. Biochemically distinct vesicles from the endoplasmic reticulum fuse to form peroxisomes. Cell. 2012;149:397–409. doi: 10.1016/j.cell.2012.01.054. [DOI] [PubMed] [Google Scholar]
- 20.Matsuzaki T., Fujiki Y. The peroxisomal membrane protein import receptor Pex3p is directly transported to peroxisomes by a novel Pex19p- and Pex16p-dependent pathway. J. Cell Biol. 2008;183:1275–1286. doi: 10.1083/jcb.200806062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fang Y., Morrell J.C., Jones J.M., Gould S.J. PEX3 functions as a PEX19 docking factor in the import of class I peroxisomal membrane proteins. J. Cell Biol. 2004;164:863–875. doi: 10.1083/jcb.200311131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lazarow P.B., Fujiki Y. Biogenesis of Peroxisomes. Annu. Rev. Cell Biol. 1985;1:489–530. doi: 10.1146/annurev.cb.01.110185.002421. [DOI] [PubMed] [Google Scholar]
- 23.Francisco T., Rodrigues T., Dias A.F., Barros-Barbosa A., Bicho D., Azevedo J.E. Protein transport into peroxisomes: Knowns and unknowns. BioEssays. 2017;39:39. doi: 10.1002/bies.201700047. [DOI] [PubMed] [Google Scholar]
- 24.Platta H., Erdmann R. The peroxisomal protein import machinery. FEBS Lett. 2007;581:2811–2819. doi: 10.1016/j.febslet.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Gould S.J., Keller G.-A., Hosken N., Wilkinson J., Subramani S. A conserved tripeptide sorts proteins to peroxisomes. J. Cell Biol. 1989;108:1657–1664. doi: 10.1083/jcb.108.5.1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lazarow P.B. Chapter 3.1.7. The import receptor Pex7p and the PTS2 targeting sequence. Biochim. Biophys. Acta Bioenerg. 2006;1763:1599–1604. doi: 10.1016/j.bbamcr.2006.08.011. [DOI] [PubMed] [Google Scholar]
- 27.Swinkels B.W., Gould S.J., Bodnar A.G., Rachubinski R.A., Subramani S. A novel, cleavable peroxisomal targeting signal at the amino-terminus of the rat 3-ketoacyl-CoA thiolase. EMBO J. 1991;10:3255–3262. doi: 10.1002/j.1460-2075.1991.tb04889.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meinecke M., Cizmowski C., Schliebs W., Krüger V., Beck S., Wagner R.H., Erdmann R. The peroxisomal importomer constitutes a large and highly dynamic pore. Nat. Cell Biol. 2010;12:273–277. doi: 10.1038/ncb2027. [DOI] [PubMed] [Google Scholar]
- 29.Rucktäschel R., Girzalsky W., Erdmann R. Protein import machineries of peroxisomes. Biochim. Biophys. Acta Biomembr. 2011;1808:892–900. doi: 10.1016/j.bbamem.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 30.Platta H.W., El Magraoui F., Baumer B.E., Schlee D., Girzalsky W., Erdmann R. Pex2 and Pex12 Function as Protein-Ubiquitin Ligases in Peroxisomal Protein Import. Mol. Cell. Biol. 2009;29:5505–5516. doi: 10.1128/MCB.00388-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Platta H.W., Brinkmeier R., Reidick C., Galiani S., Clausen M.P., Eggeling C. Regulation of peroxisomal matrix protein import by ubiquitination. Biochim. Biophys. Acta Bioenerg. 2016;1863:838–849. doi: 10.1016/j.bbamcr.2015.09.010. [DOI] [PubMed] [Google Scholar]
- 32.Thoms S., Erdmann R. Peroxisomal matrix protein receptor ubiquitination and recycling. Biochim. Biophys. Acta Bioenerg. 2006;1763:1620–1628. doi: 10.1016/j.bbamcr.2006.08.046. [DOI] [PubMed] [Google Scholar]
- 33.Carvalho A.F., Pinto M.P., Grou C.P., Alencastre I.S., Fransen M., Sa-Miranda C., Azevedo J.E. Ubiquitination of Mammalian Pex5p, the Peroxisomal Import Receptor. J. Biol. Chem. 2007;282:31267–31272. doi: 10.1074/jbc.M706325200. [DOI] [PubMed] [Google Scholar]
- 34.Grou C.P., Carvalho A.F., Pinto M.P., Alencastre I.S., Rodrigues T.A., Freitas M.O., Francisco T., Sá-Miranda C., Azevedo J.E. The peroxisomal protein import machinery—A case report of transient ubiquitination with a new flavor. Cell. Mol. Life Sci. 2008;66:254–262. doi: 10.1007/s00018-008-8415-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Matsumoto N., Tamura S., Fujiki Y. The pathogenic peroxin Pex26p recruits the Pex1p–Pex6p AAA ATPase complexes to peroxisomes. Nat. Cell Biol. 2003;5:454–460. doi: 10.1038/ncb982. [DOI] [PubMed] [Google Scholar]
- 36.Blok N.B., Tan D., Wang R.Y., Penczek P.A., Baker D., DiMaio F., Rapoport T.A., Walz T. Unique double-ring structure of the peroxisomal Pex1/Pex6 ATPase complex revealed by cryo-electron microscopy. Proc. Natl. Acad. Sci. USA. 2015;112:E4017–E4025. doi: 10.1073/pnas.1500257112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ciniawsky S., Grimm I., Saffian D., Girzalsky W., Erdmann R., Wendler P. Molecular snapshots of the Pex1/6 AAA+ complex in action. Nat. Commun. 2015;6:7331. doi: 10.1038/ncomms8331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tan D., Blok N.B., Rapoport T.A., Walz T. Structures of the double-ring AAA ATPase Pex1-Pex6 involved in peroxisome biogenesis. FEBS J. 2015;283:986–992. doi: 10.1111/febs.13569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gardner B.M., Chowdhury S., Lander G.C., Martin A. The Pex1/Pex6 complex is a heterohexameric AAA+ motor with alternating and highly coordinated subunits. J. Mol. Biol. 2015;427:1375–1388. doi: 10.1016/j.jmb.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Debelyy M., Platta H., Saffian D., Hensel A., Thoms S., Meyer H.E., Warscheid B., Girzalsky W., Erdmann R. Ubp15p, a Ubiquitin Hydrolase Associated with the Peroxisomal Export Machinery. J. Biol. Chem. 2011;286:28223–28234. doi: 10.1074/jbc.M111.238600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Grou C.P., Francisco T., Rodrigues T.A., Freitas M.O., Pinto M.P., Carvalho A.F., Domingues P., Wood S.A., Rodríguez-Borges J.E., Sá-Miranda C., et al. Identification of Ubiquitin-specific Protease 9X (USP9X) as a Deubiquitinase Acting on Ubiquitin-Peroxin 5 (PEX5) Thioester Conjugate. J. Biol. Chem. 2012;287:12815–12827. doi: 10.1074/jbc.M112.340158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schrader M., Reuber B.E., Morrell J.C., Jimenez-Sanchez G., Obie C., Stroh T.A., Valle D., Schroer T.A., Gould S.J. Expression of PEX11beta mediates peroxisome proliferation in the absence of extracellular stimuli. J. Biol. Chem. 1998;273:29607–29614. doi: 10.1074/jbc.273.45.29607. [DOI] [PubMed] [Google Scholar]
- 43.Schrader M., Fahimi H.D. Growth and Division of Peroxisomes. Adv. Appl. Microbiol. 2006;255:237–290. doi: 10.1016/S0074-7696(06)55005-3. [DOI] [PubMed] [Google Scholar]
- 44.Fagarasanu A., Fagarasanu M., Rachubinski R.A. Maintaining peroxisome populations: A story of division and inheritance. Annu. Rev. Cell Dev. Biol. 2007;23:321–344. doi: 10.1146/annurev.cellbio.23.090506.123456. [DOI] [PubMed] [Google Scholar]
- 45.Thoms S., Erdmann R. Dynamin-related proteins and Pex11 proteins in peroxisome division and proliferation. FEBS J. 2005;272:5169–5181. doi: 10.1111/j.1742-4658.2005.04939.x. [DOI] [PubMed] [Google Scholar]
- 46.Okumoto K., Tamura S., Honsho M., Fujiki Y. Peroxisome: Metabolic Functions and Biogenesis. Adv. Exp. Med. Biol. 2020;1299:3–17. doi: 10.1007/978-3-030-60204-8_1. [DOI] [PubMed] [Google Scholar]
- 47.Ebberink M.S., Koster J., Visser G., van Spronsen F., Stolte-Dijkstra I., Smit G.P., Fock J.M., Kemp S., Wanders R.J., Waterham H.R. A novel defect of peroxisome division due to a homozygous non-sense mutation in the PEX11β gene. J. Med. Genet. 2012;49:307–313. doi: 10.1136/jmedgenet-2012-100778. [DOI] [PubMed] [Google Scholar]
- 48.Itoyama A., Honsho M., Abe Y., Moser A., Yoshida Y., Fujiki Y. Docosahexaenoic acid mediates peroxisomal elongation, a prerequisite for peroxisome division. J. Cell Sci. 2012;125:589–602. doi: 10.1242/jcs.087452. [DOI] [PubMed] [Google Scholar]
- 49.Kobayashi S., Tanaka A., Fujiki Y. Fis1, DLP1, and Pex11p coordinately regulate peroxisome morphogenesis. Exp. Cell Res. 2007;313:1675–1686. doi: 10.1016/j.yexcr.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 50.Opaliński Ł., Kiel J.A., Williams C., Veenhuis M., Van Der Klei I.J. Membrane curvature during peroxisome fission requires Pex11. EMBO J. 2011;30:5–16. doi: 10.1038/emboj.2010.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yoshida Y., Niwa H., Honsho M., Itoyama A., Fujiki Y. Pex11mediates peroxisomal proliferation by promoting deformation of the lipid membrane. Biol. Open. 2015;4:710–721. doi: 10.1242/bio.201410801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Su J., Thomas A.S., Grabietz T., Landgraf C., Volkmer R., Marrink S.J., Williams C., Melo M.N. The N-terminal amphipathic helix of Pex11p self-interacts to induce membrane remodelling during peroxisome fission. Biochim. Biophys. Acta Biomembr. 2018;1860:1292–1300. doi: 10.1016/j.bbamem.2018.02.029. [DOI] [PubMed] [Google Scholar]
- 53.Itoyama A., Michiyuki S., Honsho M., Yamamoto T., Moser A., Yoshida Y., Fujiki Y. Mff functions with Pex11pβ and DLP1 in peroxisomal fission. Biol. Open. 2013;2:998–1006. doi: 10.1242/bio.20135298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bonekamp N.A., Völkl A., Fahimi H.D., Schrader M. Reactive oxygen species and peroxisomes: Struggling for balance. BioFactors. 2009;35:346–355. doi: 10.1002/biof.48. [DOI] [PubMed] [Google Scholar]
- 55.Islinger M., Li K.W., Seitz J., Völkl A., Lüers G.H. Hitchhiking of Cu/Zn Superoxide Dismutase to Peroxisomes–Evidence for a Natural Piggyback Import Mechanism in Mammals. Traffic. 2009;10:1711–1721. doi: 10.1111/j.1600-0854.2009.00966.x. [DOI] [PubMed] [Google Scholar]
- 56.del Río L.A., Corpas F.J., Sandalio L.M., Palma J.M., Gómez M., Barroso J.B. Reactive oxygen species, antioxidant systems and nitric oxide in peroxisomes. J. Exp. Bot. 2002;53:1255–1272. doi: 10.1093/jxb/53.372.1255. [DOI] [PubMed] [Google Scholar]
- 57.Wanders R.J., Waterham H.R. Biochemistry of Mammalian Peroxisomes Revisited. Annu. Rev. Biochem. 2006;75:295–332. doi: 10.1146/annurev.biochem.74.082803.133329. [DOI] [PubMed] [Google Scholar]
- 58.Cipolla C.M., Lodhi I.J. Peroxisomal Dysfunction in Age-Related Diseases. Trends Endocrinol. Metab. 2017;28:297–308. doi: 10.1016/j.tem.2016.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wanders R.J.A., Waterham H.R., Ferdinandusse S. Metabolic Interplay between Peroxisomes and Other Subcellular Organelles Including Mitochondria and the Endoplasmic Reticulum. Front. Cell Dev. Biol. 2016;3:83. doi: 10.3389/fcell.2015.00083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nagan N., Zoeller R.A. Plasmalogens: Biosynthesis and functions. Prog. Lipid Res. 2001;40:199–229. doi: 10.1016/S0163-7827(01)00003-0. [DOI] [PubMed] [Google Scholar]
- 61.Dean J.M., Lodhi I.J. Structural and functional roles of ether lipids. Protein Cell. 2018;9:196–206. doi: 10.1007/s13238-017-0423-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Honsho M., Tanaka M., Zoeller R.A., Fujiki Y. Distinct Functions of Acyl/Alkyl Dihydroxyacetonephosphate Reductase in Peroxisomes and Endoplasmic Reticulum. Front. Cell Dev. Biol. 2020;8:855. doi: 10.3389/fcell.2020.00855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gallego-García A., Monera-Girona A.J., Pajares-Martínez E., Bastida-Martínez E., Pérez-Castaño R., Iniesta A.A., Fontes M., Padmanabhan S., Elías-Arnanz M. A bacterial light response reveals an orphan desaturase for human plasmalogen synthesis. Science. 2019;366:128–132. doi: 10.1126/science.aay1436. [DOI] [PubMed] [Google Scholar]
- 64.Werner E.R., Keller M.A., Sailer S., Lackner K., Koch J., Hermann M., Coassin S., Golderer G., Werner-Felmayer G., Zo-eller R.A., et al. The TMEM189 gene encodes plasmanylethanolamine desaturase which introduces the characteristic vinyl ether double bond into plasmalogens. Proc. Natl. Acad. Sci. USA. 2020;117:7792–7798. doi: 10.1073/pnas.1917461117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.De Duve C., Baudhuin P. Peroxisomes (microbodies and related particles) Physiol. Rev. 1966;46:323–357. doi: 10.1152/physrev.1966.46.2.323. [DOI] [PubMed] [Google Scholar]
- 66.Boveris A., Oshino N., Chance B. The cellular production of hydrogen peroxide. Biochem. J. 1972;128:617–630. doi: 10.1042/bj1280617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fransen M., Nordgren M., Wang B., Apanasets O. Role of peroxisomes in ROS/RNS-metabolism: Implications for human disease. Biochim. et Biophys. Acta Mol. Basis Dis. 2011;1822:1363–1373. doi: 10.1016/j.bbadis.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 68.Peeters A., Fraisl P., Berg S.V.D., van Themaat E.V.L., Van Kampen A., Rider M.H., Takemori H., van Dijk K.W., Van Veldhoven P.P., Carmeliet P., et al. Carbohydrate Metabolism Is Perturbed in Peroxisome-deficient Hepatocytes Due to Mitochondrial Dysfunction, AMP-activated Protein Kinase (AMPK) Activation, and Peroxisome Proliferator-activated Receptor γ Coactivator 1α (PGC-1α) Suppression. J. Biol. Chem. 2011;286:42162–42179. doi: 10.1074/jbc.M111.299727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Baboota R.K., Shinde A.B., Lemaire K., Fransen M., Vinckier S., Van Veldhoven P.P., Schuit F., Baes M. Functional peroxisomes are required for beta-cell integrity in mice. Mol. Metab. 2019;22:71–83. doi: 10.1016/j.molmet.2019.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mosser J., Douar A.-M., Sarde C.-O., Kioschis P., Feil R., Moser H., Poustka A.-M., Mandel J.-L., Aubourg P. Putative X-linked adrenoleukodystrophy gene shares unexpected homology with ABC transporters. Nature. 1993;361:726–730. doi: 10.1038/361726a0. [DOI] [PubMed] [Google Scholar]
- 71.Schluter A., Espinosa L., Fourcade S., Galino J., López E., Ilieva E., Morató L., Asheuer M., Cook T., McLaren A., et al. Functional genomic analysis unravels a metabolic-inflammatory interplay in adrenoleukodystrophy. Hum. Mol. Genet. 2011;21:1062–1077. doi: 10.1093/hmg/ddr536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Heit C., Marshall S., Singh S., Yu X., Charkoftaki G., Zhao H., Orlicky D.J., Fritz K., Thompson D.C., Vasiliou V. Catalase deletion promotes prediabetic phenotype in mice. Free Radic. Biol. Med. 2017;103:48–56. doi: 10.1016/j.freeradbiomed.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Peeters A., Shinde A.B., Dirkx R., Smet J., De Bock K., Espeel M., Vanhorebeek I., Vanlander A., Van Coster R., Carmeliet P., et al. Mitochondria in peroxisome-deficient hepatocytes exhibit impaired respiration, depleted DNA, and PGC-1α independent proliferation. Biochim. Biophys. Acta Bioenerg. 2015;1853:285–298. doi: 10.1016/j.bbamcr.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 74.Ferrer I., Aubourg P., Pujol A. General Aspects and Neuropathology of X-Linked Adrenoleukodystrophy. Brain Pathol. 2009;20:817–830. doi: 10.1111/j.1750-3639.2010.00390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lu J.-F., Lawler A.M., Watkins P.A., Powers J.M., Moser A.B., Moser H.W., Smith K.D. A mouse model for X-linked adrenoleukodystrophy. Proc. Natl. Acad. Sci. USA. 1997;94:9366–9371. doi: 10.1073/pnas.94.17.9366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Piao L., Dorotea D., Jiang S., Koh E.H., Oh G.T., Ha H. Impaired Peroxisomal Fitness in Obese Mice, a Vicious Cycle Exacerbating Adipocyte Dysfunction via Oxidative Stress. Antioxid. Redox Signal. 2019;31:1339–1351. doi: 10.1089/ars.2018.7614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Oruqaj G., Karnati S., Vijayan V., Kotarkonda L.K., Boateng E., Zhang W., Ruppert C., Günther A., Shi W., Baumgart-Vogt E. Compromised peroxisomes in idiopathic pulmonary fibrosis, a vicious cycle inducing a higher fibrotic response via TGF-β signaling. Proc. Natl. Acad. Sci. USA. 2015;112:E2048–E2057. doi: 10.1073/pnas.1415111112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ahlemeyer B., Gottwald M., Baumgart-Vogt E. Deletion of a single allele of the Pex11β gene is sufficient to cause oxidative stress, delayed differentiation and neuronal death in mouse brain. Dis. Model. Mech. 2012;5:125–140. doi: 10.1242/dmm.007708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Walton P.A., Pizzitelli M. Effects of peroxisomal catalase inhibition on mitochondrial function. Front. Physiol. 2012;3:108. doi: 10.3389/fphys.2012.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ivashchenko O., Van Veldhoven P.P., Brees C., Ho Y.-S., Terlecky S.R., Fransen M. Intraperoxisomal redox balance in mammalian cells: Oxidative stress and interorganellar cross-talk. Mol. Biol. Cell. 2011;22:1440–1451. doi: 10.1091/mbc.e10-11-0919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hwang I., Uddin J., Pak E.S., Kang H., Jin E.-J., Jo S., Kang D., Lee H., Ha H. The impaired redox balance in peroxisomes of catalase knockout mice accelerates nonalcoholic fatty liver disease through endoplasmic reticulum stress. Free. Radic. Biol. Med. 2020;148:22–32. doi: 10.1016/j.freeradbiomed.2019.12.025. [DOI] [PubMed] [Google Scholar]
- 82.Moser A.B., Kreiter N., Bezman L., Lu S.-E., Raymond G.V., Naidu S., Moser H.W. Plasma very long chain fatty acids in 3,000 peroxisome disease patients and 29,000 controls. Ann. Neurol. 1999;45:100–110. doi: 10.1002/1531-8249(199901)45:1<100::AID-ART16>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 83.Dasouki M. Chapter 11-Peroxisomal disorders: Clinical and biochemical laboratory aspects. Biomark. Inborn Errors Metab. 2017;2:80087–80096. [Google Scholar]
- 84.Stradomska T.J., Syczewska M., Jamroz E., Pleskaczyńska A., Kruczek P., Ciara E., Tylki-Szymanska A. Serum very long-chain fatty acids (VLCFA) levels as predictive biomarkers of diseases severity and probability of survival in peroxisomal disorders. PLoS ONE. 2020;15:e0238796. doi: 10.1371/journal.pone.0238796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Aubourg P., Adamsbaum C., Lavallard-Rousseau M.C., Rocchiccioli F., Cartier N., Jambaque I., Jakobezak C., Lemaitre A., Boureau F., Wolf C., et al. A two-year trial of oleic and erucic acids (“Lorenzo’s oil”) as treatment for adrenomyeloneuropathy. N. Engl. J. Med. 1993;329:745–752. doi: 10.1056/NEJM199309093291101. [DOI] [PubMed] [Google Scholar]
- 86.van Geel B.M., Assies J., Haverkort E.B., Koelman J.H., Verbeeten B.W., Wanders R.J., Barth P.G. Progression of abnormalities in adrenomyeloneuropathy and neurologically asymptomatic X-linked adrenoleukodystrophy despite treatment with “Lorenzo’s oil”. J. Neurol. Neurosurg. Psychiatry. 1999;67:290–299. doi: 10.1136/jnnp.67.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Baes M., Van Veldhoven P.P. Generalised and conditional inactivation of Pex genes in mice. Biochim. Biophys. Acta. 2006;1763:1785–1793. doi: 10.1016/j.bbamcr.2006.08.018. [DOI] [PubMed] [Google Scholar]
- 88.Faust P.L., Hatten M.E. Targeted Deletion of the PEX2 Peroxisome Assembly Gene in Mice Provides a Model for Zellweger Syndrome, a Human Neuronal Migration Disorder. J. Cell Biol. 1997;139:1293–1305. doi: 10.1083/jcb.139.5.1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Maxwell M., Bjorkman J., Nguyen T., Sharp P., Finnie J., Paterson C., Tonks I., Paton B.C., Kay G.F., Crane D.I. Pex13 Inactivation in the Mouse Disrupts Peroxisome Biogenesis and Leads to a Zellweger Syndrome Phenotype. Mol. Cell. Biol. 2003;23:5947–5957. doi: 10.1128/MCB.23.16.5947-5957.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Baes M., Gressens P., Baumgart-Vogt E., Carmeliet P., Casteels M., Fransen M., Evrard P., Fahimi D., Declercq P.E., Collen D., et al. A mouse model for Zellweger syndrome. Nat. Genet. 1997;17:49–57. doi: 10.1038/ng0997-49. [DOI] [PubMed] [Google Scholar]
- 91.Janssen A., Baes M., Gressens P., Mannaerts G.P., Declercq P., Van Veldhoven P.P. Docosahexaenoic Acid Deficit Is Not a Major Pathogenic Factor in Peroxisome-Deficient Mice. Lab. Investig. 2000;80:31–35. doi: 10.1038/labinvest.3780005. [DOI] [PubMed] [Google Scholar]
- 92.Brites P., Ferreira A.S., da Silva T.F., Sousa V.F., Malheiro A.R., Duran M., Waterham H.R., Baes M., Wanders R.J.A. Alkyl-Glycerol Rescues Plasmalogen Levels and Pathology of Ether-Phospholipid Deficient Mice. PLoS ONE. 2011;6:e28539. doi: 10.1371/journal.pone.0028539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Hofer D., Pessentheiner A., Pelzmann H.J., Schlager S., Madreiter-Sokolowski C.T., Kolb D., Eichmann T.O., Rechberger G., Bilban M., Graier W., et al. Critical role of the peroxisomal protein PEX16 in white adipocyte development and lipid homeostasis. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2017;1862:358–368. doi: 10.1016/j.bbalip.2016.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sellin J., Wingen C., Gosejacob D., Senyilmaz D., Hänschke L., Büttner S., Meyer K., Bano D., Nicotera P., Teleman A., et al. Dietary rescue of lipotoxicity-induced mitochondrial damage in Peroxin19 mutants. PLoS Biol. 2018;16:e2004893. doi: 10.1371/journal.pbio.2004893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Kovacs W.J., Shackelford J.E., Tape K.N., Richards M.J., Faust P.L., Fliesler S.J., Krisans S.K. Disturbed Cholesterol Homeostasis in a Peroxisome-Deficient PEX2 Knockout Mouse Model. Mol. Cell. Biol. 2004;24:1–13. doi: 10.1128/MCB.24.1.1-13.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ridgway N., McLeod R. Biochemistry of Lipids, Lipoproteins and Membranes. Elsevier Science; Amsterdam, The Netherlands: 2008. [Google Scholar]
- 97.Krisans S.K., Ericsson J., Edwards P.A., Keller G.A. Farnesyl-diphosphate synthase is localized in peroxisomes. J. Biol. Chem. 1994;269:14165–14169. doi: 10.1016/S0021-9258(17)36769-8. [DOI] [PubMed] [Google Scholar]
- 98.Kovacs W.J., Tape K.N., Shackelford J.E., Wikander T.M., Richards M.J., Fliesler S.J., Krisans S.K., Faust P.L. Peroxisome Deficiency Causes a Complex Phenotype because of Hepatic SREBP/Insig Dysregulation Associated with Endoplasmic Reticulum Stress. J. Biol. Chem. 2009;284:7232–7245. doi: 10.1074/jbc.M809064200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hogenboom S., Romeijn G.J., Houten S.M., Baes M., Wanders R.J.A., Waterham H.R. Absence of functional peroxisomes does not lead to deficiency of enzymes involved in cholesterol biosynthesis. J. Lipid Res. 2002;43:90–98. doi: 10.1016/S0022-2275(20)30191-7. [DOI] [PubMed] [Google Scholar]
- 100.Hogenboom S., Wanders R.J., Waterham H.R. Cholesterol biosynthesis is not defective in peroxisome biogenesis defective fibroblasts. Mol. Genet. Metab. 2003;80:290–295. doi: 10.1016/S1096-7192(03)00143-4. [DOI] [PubMed] [Google Scholar]
- 101.Hogenboom S., Tuyp J.J.M., Espeel M., Koster J., Wanders R.J.A., Waterham H.R. Mevalonate kinase is a cytosolic enzyme in humans. J. Cell Sci. 2004;117:631–639. doi: 10.1242/jcs.00910. [DOI] [PubMed] [Google Scholar]
- 102.Hogenboom S., Tuyp J.J.M., Espeel M., Koster J., Wanders R.J.A., Waterham H.R. Phosphomevalonate kinase is a cytosolic protein in humans. J. Lipid Res. 2004;45:697–705. doi: 10.1194/jlr.M300373-JLR200. [DOI] [PubMed] [Google Scholar]
- 103.Chu B.-B., Liao Y.-C., Qi W., Xie C., Du X., Wang J., Yang H., Miao H.-H., Li B.-L., Song B.-L. Cholesterol Transport through Lysosome-Peroxisome Membrane Contacts. Cell. 2015;161:291–306. doi: 10.1016/j.cell.2015.02.019. [DOI] [PubMed] [Google Scholar]
- 104.Fransen M., Lismont C., Walton P. The Peroxisome-Mitochondria Connection: How and Why? Int. J. Mol. Sci. 2017;18:1126. doi: 10.3390/ijms18061126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Baes M., Van Veldhoven P.P. Hepatic dysfunction in peroxisomal disorders. Biochim. Biophys. Acta Bioenerg. 2016;1863:956–970. doi: 10.1016/j.bbamcr.2015.09.035. [DOI] [PubMed] [Google Scholar]
- 106.Dirkx R., Vanhorebeek I., Martens K., Schad A., Grabenbauer M., Fahimi D., Declercq P., Van Veldhoven P.P., Baes M. Absence of peroxisomes in mouse hepatocytes causes mitochondrial and ER abnormalities. Hepatology. 2005;41:868–878. doi: 10.1002/hep.20628. [DOI] [PubMed] [Google Scholar]
- 107.Keane M.H., Overmars H., Wikander T.M., Ferdinandusse S., Duran M., Wanders R.J.A., Faust P.L. Bile acid treatment alters hepatic disease and bile acid transport in peroxisome-deficientPEX2Zellweger mice. Hepatology. 2007;45:982–997. doi: 10.1002/hep.21532. [DOI] [PubMed] [Google Scholar]
- 108.López-Erauskin J., Galino J., Ruiz M., Cuezva J., Fabregat I., Cacabelos D., Boada J., Martínez J., Ferrer I., Pamplona R., et al. Impaired mitochondrial oxidative phosphorylation in the peroxisomal disease X-linked adrenoleukodystrophy. Hum. Mol. Genet. 2013;22:3296–3305. doi: 10.1093/hmg/ddt186. [DOI] [PubMed] [Google Scholar]
- 109.Bülow M.H., Wingen C., Senyilmaz D., Gosejacob D., Sociale M., Bauer R., Schulze H., Sandhoff K., Teleman A.A., Hoch M., et al. Unbalanced lipolysis results in lipotoxicity and mitochondrial damage in peroxisome-deficient Pex19 mutants. Mol. Biol. Cell. 2018;29:396–407. doi: 10.1091/mbc.E17-08-0535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Park H., He A., Tan M., Johnson J., Dean J.M., Pietka T.A., Chen Y., Zhang X., Hsu F.-F., Razani B., et al. Peroxisome-derived lipids regulate adipose thermogenesis by mediating cold-induced mitochondrial fission. J. Clin. Investig. 2019;129:694–711. doi: 10.1172/JCI120606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mathis R.K., Watkins J.B., Leeuwen P.S.-V., Lott I.T. Liver in the cerebro-hepato-renal syndrome: Defective bile acid synthesis and abnormal mitochondria. Gastroenterology. 1980;79:1311–1317. doi: 10.1016/0016-5085(80)90931-2. [DOI] [PubMed] [Google Scholar]
- 112.Trijbels J.M.F., A Berden J., Monnens L.A.H., Willems J.L., Janssen A.J.M., Schutgens R.B.H., Essen M.V.D.B.-V. Biochemical Studies in the Liver and Muscle of Patients with Zellweger Syndrome. Pediatr. Res. 1983;17:514–517. doi: 10.1203/00006450-198306000-00018. [DOI] [PubMed] [Google Scholar]
- 113.Goldfischer S., Moore C.L., Johnson A.B., Spiro A.J., Valsamis M.P., Wisniewski H.K., Ritch R.H., Norton W.T., Rapin I., Gartner L.M. Peroxisomal and Mitochondrial Defects in the Cerebro-Hepato-Renal Syndrome. Science. 1973;182:62–64. doi: 10.1126/science.182.4107.62. [DOI] [PubMed] [Google Scholar]
- 114.Hughes J.L., Poulos A., Robertson E., Chow C.W., Sheffield L.J., Christodoulou J., Carter R.F. Pathology of hepatic peroxisomes and mitochondria in patients with peroxisomal disorders. Virchows Arch. A. 1990;416:255–264. doi: 10.1007/BF01678985. [DOI] [PubMed] [Google Scholar]
- 115.Yoshida H. ER stress and diseases. FEBS J. 2007;274:630–658. doi: 10.1111/j.1742-4658.2007.05639.x. [DOI] [PubMed] [Google Scholar]
- 116.Harding H., Zhang Y., Bertolotti A., Zeng H., Ron D. Perk Is Essential for Translational Regulation and Cell Survival during the Unfolded Protein Response. Mol. Cell. 2000;5:897–904. doi: 10.1016/S1097-2765(00)80330-5. [DOI] [PubMed] [Google Scholar]
- 117.Harding H., Novoa I., Zhang Y., Zeng H., Wek R., Schapira M., Ron D. Regulated Translation Initiation Controls Stress-Induced Gene Expression in Mammalian Cells. Mol. Cell. 2000;6:1099–1108. doi: 10.1016/S1097-2765(00)00108-8. [DOI] [PubMed] [Google Scholar]
- 118.Baird T., Wek R.C. Eukaryotic Initiation Factor 2 Phosphorylation and Translational Control in Metabolism. Adv. Nutr. Int. Rev. J. 2012;3:307–321. doi: 10.3945/an.112.002113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cox J.S., Shamu C.E., Walter P. Transcriptional induction of genes encoding endoplasmic reticulum resident proteins requires a transmembrane protein kinase. Cell. 1993;73:1197–1206. doi: 10.1016/0092-8674(93)90648-A. [DOI] [PubMed] [Google Scholar]
- 120.Haze K., Yoshida H., Yanagi H., Yura T., Mori K. Mammalian Transcription Factor ATF6 Is Synthesized as a Transmembrane Protein and Activated by Proteolysis in Response to Endoplasmic Reticulum Stress. Mol. Biol. Cell. 1999;10:3787–3799. doi: 10.1091/mbc.10.11.3787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kovacs W.J., Charles K.N., Walter K.M., Shackelford J.E., Wikander T.M., Richards M.J., Fliesler S.J., Krisans S.K., Faust P.L. Peroxisome deficiency-induced ER stress and SREBP-2 pathway activation in the liver of newborn PEX2 knock-out mice. Biochim. Biophys. Acta Mol. Cell Biol. Lipids. 2012;1821:895–907. doi: 10.1016/j.bbalip.2012.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cai M., Sun X., Wang W., Lian Z., Wu P., Han S., Chen H., Zhang P. Disruption of peroxisome function leads to metabolic stress, mTOR inhibition, and lethality in liver cancer cells. Cancer Lett. 2018;421:82–93. doi: 10.1016/j.canlet.2018.02.021. [DOI] [PubMed] [Google Scholar]
- 123.Faust P.L., Kovacs W.J. Cholesterol biosynthesis and ER stress in peroxisome deficiency. Biochimie. 2014;98:75–85. doi: 10.1016/j.biochi.2013.10.019. [DOI] [PubMed] [Google Scholar]
- 124.Krysko O., Hulshagen L., Janssen A., Schütz G., Klein R., De Bruycker M., Espeel M., Gressens P., Baes M. Neocortical and cerebellar developmental abnormalities in conditions of selective elimination of peroxisomes from brain or from liver. J. Neurosci. Res. 2007;85:58–72. doi: 10.1002/jnr.21097. [DOI] [PubMed] [Google Scholar]
- 125.Kim D., Song J., Ahn C., Kang Y., Chun C.-H., Jin E.-J. Peroxisomal dysfunction is associated with up-regulation of apoptotic cell death via miR-223 induction in knee osteoarthritis patients with type 2 diabetes mellitus. Bone. 2014;64:124–131. doi: 10.1016/j.bone.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 126.Tanaka H., Okazaki T., Aoyama S., Yokota M., Koike M., Okada Y., Fujiki Y., Gotoh Y. Peroxisomes control mitochondrial dynamics and the mitochondrion-dependent apoptosis pathway. J. Cell Sci. 2019;132:jcs224766. doi: 10.1242/jcs.224766. [DOI] [PubMed] [Google Scholar]
- 127.Dixon S.J., Lemberg K.M., Lamprecht M.R., Skouta R., Zaitsev E.M., Gleason C.E., Patel D.N., Bauer A.J., Cantley A.M., Yang W.S., et al. Ferroptosis: An Iron-Dependent Form of Nonapoptotic Cell Death. Cell. 2012;149:1060–1072. doi: 10.1016/j.cell.2012.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zou Y., Henry W.S., Ricq E.L., Graham E.T., Phadnis V.V., Maretich P., Paradkar S., Boehnke N., Deik A.A., Reinhardt F., et al. Plasticity of ether lipids promotes ferroptosis susceptibility and evasion. Nature. 2020;585:603–608. doi: 10.1038/s41586-020-2732-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Germain K., Kim P.K. Pexophagy: A Model for Selective Autophagy. Int. J. Mol. Sci. 2020;21:578. doi: 10.3390/ijms21020578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zientara-Rytter K., Subramani S. Autophagic degradation of peroxisomes in mammals. Biochem. Soc. Trans. 2016;44:431–440. doi: 10.1042/BST20150268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Yokota S., Haraguchi C.M., Oda T. Induction of peroxisomal Lon protease in rat liver after di-(2-ethylhexyl)phthalate treatment. Histochem. Cell Biol. 2007;129:73–83. doi: 10.1007/s00418-007-0328-0. [DOI] [PubMed] [Google Scholar]
- 132.Yokota S., Fahimi H.D. Degradation of excess peroxisomes in mammalian liver cells by autophagy and other mechanisms. Histochem. Cell Biol. 2009;131:455–458. doi: 10.1007/s00418-009-0564-6. [DOI] [PubMed] [Google Scholar]
- 133.Van Leyen K., Duvoisin R.M., Engelhardt H., Wiedmann M. A function for lipoxygenase in programmed organelle degradation. Nature. 1998;395:392–395. doi: 10.1038/26500. [DOI] [PubMed] [Google Scholar]
- 134.Komatsu M., Waguri S., Ueno T., Iwata J., Murata S., Tanida I., Ezaki J., Mizushima N., Ohsumi Y., Uchiyama Y., et al. Impairment of starvation-induced and constitutive autophagy in Atg7-deficient mice. J. Cell Biol. 2005;169:425–434. doi: 10.1083/jcb.200412022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Li J., Wang W. Mechanisms and Functions of Pexophagy in Mammalian Cells. Cells. 2021;10:1094. doi: 10.3390/cells10051094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Steinberg S.J., Dodt G., Raymond G.V., Braverman N.E., Moser A.B., Moser H.W. Peroxisome biogenesis disorders. Biochim. Biophys. Acta Mol. Cell Res. 2006;1763:1733–1748. doi: 10.1016/j.bbamcr.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 137.Law K.B., Bronte-Tinkew D., Di Pietro E., Snowden A., Jones R.O., Moser A., Brumell J.H., Braverman N., Kim P.K. The peroxisomal AAA ATPase complex prevents pexophagy and development of peroxisome biogenesis disorders. Autophagy. 2017;13:868–884. doi: 10.1080/15548627.2017.1291470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Klouwer F.C.C., Falkenberg K.D., Ofman R., Koster J., van Gent D., Ferdinandusse S., Wanders R.J.A., Waterham H.R. Autophagy Inhibitors Do Not Restore Peroxisomal Functions in Cells with the Most Common Peroxisome Biogenesis Defect. Front. Cell Dev. Biol. 2021;9:661298. doi: 10.3389/fcell.2021.661298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.He A., Chen X., Tan M., Chen Y., Lu D., Zhang X., Dean J.M., Razani B., Lodhi I.J. Acetyl-CoA Derived from Hepatic Peroxisomal β-Oxidation Inhibits Autophagy and Promotes Steatosis via mTORC1 Activation. Mol. Cell. 2020;79:30–42. doi: 10.1016/j.molcel.2020.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.He A., Dean J.M., Lu D., Chen Y., Lodhi I.J. Hepatic peroxisomal β-oxidation suppresses lipophagy via RPTOR acetylation and MTOR activation. Autophagy. 2020;16:1727–1728. doi: 10.1080/15548627.2020.1797288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Zechner R., Madeo F., Kratky D. Cytosolic lipolysis and lipophagy: Two sides of the same coin. Nat. Rev. Mol. Cell Biol. 2017;18:671–684. doi: 10.1038/nrm.2017.76. [DOI] [PubMed] [Google Scholar]
- 142.Li W., He P., Huang Y., Li Y.-F., Lu J., Li M., Kurihara H., Luo Z., Meng T., Onishi M., et al. Selective autophagy of intracellular organelles: Recent research advances. Theranostics. 2021;11:222–256. doi: 10.7150/thno.49860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Schrader M., Grille S., Fahimi H.D., Islinger M. Peroxisome Interactions and Cross-Talk with Other Subcellular Compartments in Animal Cells. Subcell. Biochem. 2013;69:1–22. doi: 10.1007/978-94-007-6889-5_1. [DOI] [PubMed] [Google Scholar]
- 144.Rakhshandehroo M., Knoch B., Müller M., Kersten S. Peroxisome Proliferator-Activated Receptor Alpha Target Genes. PPAR Res. 2010;2010:393–416. doi: 10.1155/2010/612089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Rakhshandehroo M., Hooiveld G., Müller M., Kersten S. Comparative analysis of gene regulation by the transcription factor PPARalpha between mouse and human. PLoS ONE. 2009;4:e6796. doi: 10.1371/journal.pone.0006796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Palanker L., Tennessen J.M., Lam G., Thummel C.S. Drosophila HNF4 regulates lipid mobilization and beta-oxidation. Cell Metab. 2009;9:228–239. doi: 10.1016/j.cmet.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.E Barry W., Thummel C.S. The Drosophila HNF4 nuclear receptor promotes glucose-stimulated insulin secretion and mitochondrial function in adults. eLife. 2016;5:e11183. doi: 10.7554/eLife.11183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Poirier Y., Antonenkov V.D., Glumoff T., Hiltunen J.K. Peroxisomal beta-oxidation-a metabolic pathway with multiple functions. Biochim. Et Biophys. Acta Mol. Cell Res. 2006;1763:1413–1426. doi: 10.1016/j.bbamcr.2006.08.034. [DOI] [PubMed] [Google Scholar]
- 149.Shai N., Yifrach E., Van Roermund C.W.T., Cohen N., Bibi C., Ijlst L., Cavellini L., Meurisse J., Schuster R., Zada L., et al. Systematic mapping of contact sites reveals tethers and a function for the peroxisome-mitochondria contact. Nat. Commun. 2018;9:1761. doi: 10.1038/s41467-018-03957-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Usaj M.M., Brložnik M., Kaferle P., Žitnik M., Wolinski H., Leitner F., Kohlwein S.D., Zupan B., Petrovič U. Genome-Wide Localization Study of Yeast Pex11 Identifies Peroxisome–Mitochondria Interactions through the ERMES Complex. J. Mol. Biol. 2015;427:2072–2087. doi: 10.1016/j.jmb.2015.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.McGuinness M.C., Lu J.-F., Zhang H.-P., Dong G.-X., Heinzer A.K., Watkins P.A., Powers J., Smith K.D. Role of ALDP (ABCD1) and Mitochondria in X-Linked Adrenoleukodystrophy. Mol. Cell. Biol. 2003;23:744–753. doi: 10.1128/MCB.23.2.744-753.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fan J., Li X., Issop L., Culty M. ACBD2/ECI2-Mediated Peroxisome-Mitochondria Interactions in Leydig Cell Steroid Biosynthesis. Mol. Endocrinol. 2016;30:763–782. doi: 10.1210/me.2016-1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Neuspiel M., Schauss A.C., Braschi E., Zunino R., Rippstein P., Rachubinski R.A., Andrade-Navarro M.A., McBride H.M. Cargo-Selected Transport from the Mitochondria to Peroxisomes Is Mediated by Vesicular Carriers. Curr. Biol. 2008;18:102–108. doi: 10.1016/j.cub.2007.12.038. [DOI] [PubMed] [Google Scholar]
- 154.Forss-Petter S., Werner H., Berger J., Lassmann H., Molzer B., Schwab M.H., Bernheimer H., Zimmermann F., Nave K.A. Targeted inactivation of the X-linked adrenoleukodystrophy gene in mice. J. Neurosci. Res. 1997;50:829–843. doi: 10.1002/(SICI)1097-4547(19971201)50:5<829::AID-JNR19>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 155.Pujol A., Hindelang C., Callizot N., Bartsch U., Schachner M., Mandel J.L. Late onset neurological phenotype of the X-ALD gene inactivation in mice: A mouse model for adrenomyeloneuropathy. Hum. Mol. Genet. 2002;11:499–505. doi: 10.1093/hmg/11.5.499. [DOI] [PubMed] [Google Scholar]
- 156.Oezen I., Rossmanith W., Forss-Petter S., Kemp S., Voigtländer T., Moser-Thier K., Wanders R.J., Bittner R.E., Berger J. Accumulation of very long-chain fatty acids does not affect mitochondrial function in adrenoleukodystrophy protein deficiency. Hum. Mol. Genet. 2005;14:1127–1137. doi: 10.1093/hmg/ddi125. [DOI] [PubMed] [Google Scholar]
- 157.Novikoff P.M., Novikoff A.B. Peroxisomes in absorptive cells of mammalian small intestine. J. Cell Biol. 1972;53:532–560. doi: 10.1083/jcb.53.2.532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zaar K., Völkl A., Fahimi H. Association of isolated bovine kidney cortex peroxisomes with endoplasmic reticulum. Biochim. Biophys. Acta Biomembr. 1987;897:135–142. doi: 10.1016/0005-2736(87)90321-X. [DOI] [PubMed] [Google Scholar]
- 159.Gronemeyer T., Wiese S., Ofman R., Bunse C., Pawlas M., Hayen H., Eisenacher M., Stephan C., Meyer H.E., Waterham H.R., et al. The proteome of human liver peroxisomes: Identification of five new peroxisomal constituents by a label-free quantitative proteomics survey. PLoS ONE. 2013;8:e57395. doi: 10.1371/annotation/3552e5c7-88d1-42c5-844d-4c2f2d722533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Costello J., Castro I.G., Hacker C., Schrader T.A., Metz J., Zeuschner D., Azadi A.S., Godinho L.F., Costina V., Findeisen P., et al. ACBD5 and VAPB mediate membrane associations between peroxisomes and the ER. J. Cell Biol. 2017;216:331–342. doi: 10.1083/jcb.201607055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hua R., Cheng D., Coyaud É., Freeman S., Di Pietro E., Wang Y., Vissa A., Yip C.M., Fairn G.D., Braverman N., et al. VAPs and ACBD5 tether peroxisomes to the ER for peroxisome maintenance and lipid homeostasis. J. Cell Biol. 2017;216:367–377. doi: 10.1083/jcb.201608128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wanders R.J.A., Vaz F.M., Waterham H.R., Ferdinandusse S. Fatty Acid Oxidation in Peroxisomes: Enzymology, Metabolic Crosstalk with Other Organelles and Peroxisomal Disorders. Adv. Exp. Med. Biol. 2020;1299:55–70. doi: 10.1007/978-3-030-60204-8_5. [DOI] [PubMed] [Google Scholar]
- 163.Ferdinandusse S., Falkenberg K., Koster J., Mooyer P.A., Jones R., Van Roermund C.W.T., A Pizzino A., Schrader M., Wanders R.J.A., Vanderver A., et al. ACBD5 deficiency causes a defect in peroxisomal very long-chain fatty acid metabolism. J. Med Genet. 2017;54:330–337. doi: 10.1136/jmedgenet-2016-104132. [DOI] [PubMed] [Google Scholar]
- 164.Herzog K., Pras-Raves M.L., Ferdinandusse S., Vervaart M.A.T., Luyf A.C.M., van Kampen A.H.C., Wanders R.J.A., Waterham H.R., Vaz F.M. Functional characterisation of peroxisomal β-oxidation disorders in fibroblasts using lipidomics. J. Inherit. Metab. Dis. 2018;41:479–487. doi: 10.1007/s10545-017-0076-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Torres S.E., Gallagher C.M., Plate L., Gupta M., Liem C.R., Guo X., Tian R., Stroud R.M., Kampmann M., Weissman J.S., et al. Ceapins block the unfolded protein response sensor ATF6α by inducing a neomorphic inter-organelle tether. eLife. 2019;8:e46595. doi: 10.7554/eLife.46595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Gallagher C.M., Walter P. Ceapins inhibit ATF6α signaling by selectively preventing transport of ATF6α to the Golgi apparatus during ER stress. eLife. 2016;5:e11880. doi: 10.7554/eLife.11880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Gallagher C.M., Garri C., Cain E.L., Ang K.K.-H., Wilson C.G., Chen S., Hearn B., Jaishankar P., Aranda-Diaz A., Arkin M.R., et al. Ceapins are a new class of unfolded protein response inhibitors, selectively targeting the ATF6α branch. eLife. 2016;5:e11878. doi: 10.7554/eLife.11878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kleinecke S., Richert S., De Hoz L., Brügger B., Kungl T., Asadollahi E., Quintes S., Blanz J., McGonigal R., Naseri K., et al. Peroxisomal dysfunctions cause lysosomal storage and axonal Kv1 channel redistribution in peripheral neuropathy. eLife. 2017;6:e23332. doi: 10.7554/eLife.23332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Sebastiani P., Federico A., Morris M., Gurinovich A., Tanaka T., Chandler K.B., Andersen S.L., Denis G., Costello C.E., Ferrucci L., et al. Protein signatures of centenarians and their offspring suggest centenarians age slower than other humans. Aging Cell. 2021;20:e13290. doi: 10.1111/acel.13290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Titorenko V.I., Terlecky S.R. Peroxisome Metabolism and Cellular Aging. Traffic. 2010;12:252–259. doi: 10.1111/j.1600-0854.2010.01144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Lizard G., Rouaud O., Demarquoy J., Cherkaoui-Malki M., Iuliano L. Potential roles of peroxisomes in Alzheimer’s disease and in dementia of the Alzheimer’s type. J. Alzheimer Dis. 2012;29:241–254. doi: 10.3233/JAD-2011-111163. [DOI] [PubMed] [Google Scholar]
- 172.Jo D.S., Park N.Y., Cho D.-H. Peroxisome quality control and dysregulated lipid metabolism in neurodegenerative diseases. Exp. Mol. Med. 2020;52:1486–1495. doi: 10.1038/s12276-020-00503-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Pharaoh G., Sataranatarajan K., Street K., Hill S., Gregston J., Ahn B., Kinter C., Kinter M., Van Remmen H. Metabolic and Stress Response Changes Precede Disease Onset in the Spinal Cord of Mutant SOD1 ALS Mice. Front. Neurosci. 2019;13:487. doi: 10.3389/fnins.2019.00487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Qin F., Lennon-Edwards S., Lancel S., Biolo A., Siwik D.A., Pimentel D.R., Dorn G.W., Kang Y.J., Colucci W.S. Cardiac-specific overexpression of catalase identifies hydrogen peroxide-dependent and -independent phases of myocardial remodeling and prevents the progression to overt heart failure in G(alpha)q-overexpressing transgenic mice. Circ. Heart Fail. 2010;3:306–313. doi: 10.1161/CIRCHEARTFAILURE.109.864785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Hwang I., Lee J., Huh J.Y., Park J., Lee H.B., Ho Y.-S., Ha H. Catalase Deficiency Accelerates Diabetic Renal Injury Through Peroxisomal Dysfunction. Diabetes. 2012;61:728–738. doi: 10.2337/db11-0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Francque S., Szabo G., Abdelmalek M.F., Byrne C.D., Cusi K., Dufour J.-F., Roden M., Sacks F., Tacke F. Nonalcoholic steatohepatitis: The role of peroxisome proliferator-activated receptors. Nat. Rev. Gastroenterol. Hepatol. 2021;18:24–39. doi: 10.1038/s41575-020-00366-5. [DOI] [PubMed] [Google Scholar]
- 177.Marcus D.L., Thomas C., Rodriguez C., Simberkoff K., Tsai J.S., Strafaci J.A., Freedman M.L. Increased peroxidation and reduced antioxidant enzyme activity in Alzheimer’s disease. Exp. Neurol. 1998;150:40–44. doi: 10.1006/exnr.1997.6750. [DOI] [PubMed] [Google Scholar]
- 178.Sheikh F.G., Pahan K., Khan M., Barbosa E., Singh I. Abnormality in catalase import into peroxisomes leads to severe neurological disorder. Proc. Natl. Acad. Sci. USA. 1998;95:2961–2966. doi: 10.1073/pnas.95.6.2961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Goodenowe D.B., Cook L.L., Liu J., Lu Y., Jayasinghe D.A., Ahiahonu P.W., Heath D., Yamazaki Y., Flax J., Krenitsky K.F., et al. Peripheral ethanolamine plasmalogen deficiency: A logical causative factor in Alzheimer’s disease and dementia. J. Lipid Res. 2007;48:2485–2498. doi: 10.1194/jlr.P700023-JLR200. [DOI] [PubMed] [Google Scholar]
- 180.Graham W.V., Bonito-Oliva A., Sakmar T.P. Update on Alzheimer’s Disease Therapy and Prevention Strategies. Annu. Rev. Med. 2017;68:413–430. doi: 10.1146/annurev-med-042915-103753. [DOI] [PubMed] [Google Scholar]
- 181.Cimini A., Moreno S., D’Amelio M., Cristiano L., D’Angelo B., Falone S., Benedetti E., Carrara P., Fanelli F., Cecconi F., et al. Early biochemical and morphological modifications in the brain of a transgenic mouse model of Alzheimer’s disease: A role for peroxisomes. J. Alzheimer Dis. 2009;18:935–952. doi: 10.3233/JAD-2009-1199. [DOI] [PubMed] [Google Scholar]
- 182.Fanelli F., Sepe S., D’Amelio M., Bernardi C., Cristiano L., Cimini A., Cecconi F., Ceru’ M.P., Moreno S. Age-dependent roles of peroxisomes in the hippocampus of a transgenic mouse model of Alzheimer’s disease. Mol. Neurodegener. 2013;8:8. doi: 10.1186/1750-1326-8-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Nunomura A., Tamaoki T., Motohashi N., Nakamura M., McKeel D.W., Jr., Tabaton M., Lee H.-G., Smith M.A., Perry G., Zhu X. The Earliest Stage of Cognitive Impairment in Transition from Normal Aging to Alzheimer Disease Is Marked by Prominent RNA Oxidation in Vulnerable Neurons. J. Neuropathol. Exp. Neurol. 2012;71:233–241. doi: 10.1097/NEN.0b013e318248e614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Kou J., Kovacs G.G., Höftberger R., Kulik W., Brodde A., Forss-Petter S., Hönigschnabl S., Gleiss A., Brügger B., Wanders R., et al. Peroxisomal alterations in Alzheimer’s disease. Acta Neuropathol. 2011;122:271–283. doi: 10.1007/s00401-011-0836-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Astarita G., Jung K.M., Berchtold N.C., Nguyen V.Q., Gillen D.L., Head E., Cotman C.W., Piomelli D. Deficient liver biosynthesis of docosahexaenoic acid correlates with cognitive impairment in Alzheimer’s disease. PLoS ONE. 2010;5:e12538. doi: 10.1371/journal.pone.0012538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Shi R., Zhang Y., Shi Y., Shi S., Jiang L. Inhibition of peroxisomal β-oxidation by thioridazine increases the amount of VLCFAs and Aβ generation in the rat brain. Neurosci. Lett. 2012;528:6–10. doi: 10.1016/j.neulet.2012.08.086. [DOI] [PubMed] [Google Scholar]
- 187.Inestrosa N.C., Carvajal F.J., Zolezzi J.M., Tapia-Rojas C., Serrano F., Karmelic D., Toledo E.M., Toro A., Toro J., Santos M.J. Peroxisome proliferators reduce spatial memory impairment, synaptic failure, and neurodegeneration in brains of a double transgenic mice model of Alzheimer’s disease. J. Alzheimer Dis. 2013;33:941–959. doi: 10.3233/JAD-2012-120397. [DOI] [PubMed] [Google Scholar]
- 188.Berger J., Dorninger F., Forss-Petter S., Kunze M. Peroxisomes in brain development and function. Biochim. Biophys. Acta. 2016;1863:934–955. doi: 10.1016/j.bbamcr.2015.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Dai D.-F., Chen T., Johnson S., Szeto H., Rabinovitch P.S. Cardiac Aging: From Molecular Mechanisms to Significance in Human Health and Disease. Antioxid. Redox Signal. 2012;16:1492–1526. doi: 10.1089/ars.2011.4179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Yazdanyar A., Newman A.B. The Burden of Cardiovascular Disease in the Elderly: Morbidity, Mortality, and Costs. Clin. Geriatr. Med. 2009;25:563–577. doi: 10.1016/j.cger.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Rodgers J.L., Jones J., Bolleddu S.I., Vanthenapalli S., Rodgers L.E., Shah K., Karia K., Panguluri S.K. Cardiovascular Risks Associated with Gender and Aging. J. Cardiovasc. Dev. Dis. 2019;6:19. doi: 10.3390/jcdd6020019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Mittler R. Oxidative stress, antioxidants and stress tolerance. Trends Plant Sci. 2002;7:405–410. doi: 10.1016/S1360-1385(02)02312-9. [DOI] [PubMed] [Google Scholar]
- 193.Bäumer A.T., Flesch M., Wang X., Shen Q., Feuerstein G.Z., Böhm M. Antioxidative Enzymes in Human Hearts with Idiopathic Dilated Cardiomyopathy. J. Mol. Cell. Cardiol. 2000;32:121–130. doi: 10.1006/jmcc.1999.1061. [DOI] [PubMed] [Google Scholar]
- 194.Colasante C., Chen J., Ahlemeyer B., Baumgart-Vogt E. Peroxisomes in cardiomyocytes and the peroxisome/peroxisome proliferator-activated receptor-loop. Thromb. Haemost. 2015;113:452–463. doi: 10.1160/TH14-06-0497. [DOI] [PubMed] [Google Scholar]
- 195.Koh J.T., Choi H.H., Ahn K.Y., Kim J.U., Kim J.H., Chun J.-Y., Baik Y.H., Kim K.K. Cardiac Characteristics of Transgenic Mice Overexpressing Refsum Disease Gene-Associated Protein within the Heart. Biochem. Biophys. Res. Commun. 2001;286:1107–1116. doi: 10.1006/bbrc.2001.5510. [DOI] [PubMed] [Google Scholar]
- 196.Wanders R.J., Komen J.C. Peroxisomes, Refsum’s disease and the alpha- and omega-oxidation of phytanic acid. Biochem. Soc. Trans. 2007;35:865–869. doi: 10.1042/BST0350865. [DOI] [PubMed] [Google Scholar]
- 197.Miard S., Picard F. Obesity and aging have divergent genomic fingerprints. Int. J. Obes. 2008;32:1873–1874. doi: 10.1038/ijo.2008.214. [DOI] [PubMed] [Google Scholar]
- 198.Barzilai N., Huffman D.M., Muzumdar R.H., Bartke A. The Critical Role of Metabolic Pathways in Aging. Diabetes. 2012;61:1315–1322. doi: 10.2337/db11-1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Jura M., Kozak L. Obesity and related consequences to ageing. AGE. 2016;38:23. doi: 10.1007/s11357-016-9884-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Goth L., Eaton J.W. Hereditary catalase deficiencies and increased risk of diabetes. Lancet. 2000;356:1820–1821. doi: 10.1016/S0140-6736(00)03238-4. [DOI] [PubMed] [Google Scholar]
- 201.Milisav I., Poljsak B., Suput D. Adaptive response, evidence of cross-resistance and its potential clinical use. Int. J. Mol. Sci. 2012;13:10771–10806. doi: 10.3390/ijms130910771. [DOI] [PMC free article] [PubMed] [Google Scholar]