Abstract
Gastric cancer (GC) is one of the major causes of cancer-related mortality worldwide. The vast majority of GC cases are adenocarcinomas including intestinal and diffuse GC. The incidence of diffuse GCs, often associated with poor overall survival, has constantly increased in USA and Europe The molecular basis of diffuse GC aggressivity remains unclear. Using mRNA from diffuse and intestinal GC tumor samples of a Western cohort, this study reports the expression level of the immunomodulatory aryl-hydrocarbon receptor (AhR), and genes involved in immune suppression (PD1, PD-L1, PD-L2) and the early steps of tryptophan metabolism (IDO1, IDO2, TDO2). Strongly increased expression of IDO1 (p < 0.001) and PD1 (p < 0.003) was observed in the intestinal sub-type. The highest expression of IDO1 and PDL1 correlated with early clinical stage and absence of lymphatic invasion (×25 p = 0.004, ×3 p = 0.04, respectively). Our results suggest that kynurenine, produced by tryptophan catabolism, and AhR activation play a central role in creating an immunosuppressive environment. Correspondingly, as compared to intestinal GCs, expression levels of IDO1-TDO2 and PD-L1 were less prominent in diffuse GCs which also had less infiltration of immune cells, suggesting an inactive immune response in the advanced diffuse GC. Confirmation of these patterns of gene expression will require a larger cohort of early and advanced stages of diffuse GC samples.
Keywords: immune checkpoint, tryptophan metabolism, gastric cancers (GCs), diffuse GC, intestinal subtype GC, and aryl hydrocarbon receptor (AhR)
1. Introduction
Gastric cancer (GC) is a major health problem and one of the major causes of cancer-related mortality worldwide [1] with a high incidence in Asia [2]. However, GC is a highly heterogeneous disease in terms of classification, clinical presentation and epidemiology. The vast majority of GCs are adenocarcinomas, which can be further histologically classified in intestinal-, diffuse- and mixed types according to the Lauren classification [3]. The majority of intestinal subtype GC arises from chronic gastritis and is associated with infectious agents including Helicobacter pylori and Epstein-Barr virus (EBV). The incidence of intestinal subtype subtype of GC has been declined over the past 50 years, possibly as the result of the decreasing prevalence of Helicobacter pylori [4]. In contrast, the incidence of the diffuse subtype of GC has constantly increased among Western populations (0.1 to 1.4/year for 100,000 habitants between 1973 and 2000 in USA) [5,6]. The diffuse sub-population is unrelated to Helicobacter pylori and develops from morphological normal gastric mucosa without atrophic gastritis. Most patients with diffuse GC, especially so for the signet-ring cell carcinoma (SRCC), tend to present with an advanced-stage disease with lymphovascular invasion, frequent metastasis and poor overall survival [7,8,9,10]. Given the poor prognosis of diffuse cancer, advances in cancer biology and molecular profiling are needed to elucidate the molecular basis of growth and metastasis in advanced GCs.
Diffuse GCs were often associated with germ line mutation in CDH1 or RhoA amplification [11,12,13,14] and aggressive behavior [8,9,15,16]. Several studies have reported the activation of oncogenic signalling pathways in diffuse GC, such as hedgehog-EMT, Wnt/β catenin signalling, along with the expression of PI3K/Akt responsive genes [2,9,17]. Moreover, a TGFβ-associated supermodule of stroma-related genes associated with late stage diffuse type morphology has been reported [18]. Our group has also identified new genes including mesenchymal markers (IGF1, FGF7, TGFβ and ZEB2, CXCR4) whose expression is associated with aggressive phenotype of diffuse GC [14]. In this study we have explored two other signalling pathways, namely immunosuppressive genes and metabolic reprogramming in both intestinal and diffuse GCs.
Most of our knowledge of the immune context in cancer derives from studies on melanoma, lung, breast, colon, and prostate cancers, as well as from animal models. Cancer cells may exhibit immune inhibition to promote tumor progression and distant metastasis. One key mechanism is the Programmed Cell Death 1 (PD1)/PD1 ligand (PDL1) pathway [19,20]. PD1 is activated by its ligands PDL1 and PDL2 to suppress antigen-stimulated lymphocyte proliferation, migration and cytokine production, resulting in attenuation of effector T cells function and immunological tolerance [20]. Recent studies from Asian groups have reported the clinical implication of variations of the levels of immunosuppressive proteins such as PD-L1 and PD1 in patients with GCs [21,22,23]. A molecular characterization of clinical response to PD-1 inhibition in metastatic gastric cancer indicated a favourable response in EBV and MSI GC [22,24]. The last decade has also witnessed the emergence of novel therapeutic targets and combination strategies to address advanced HER2-positive GC [25]. In contrast little is known about the expression and role of immune cells in GC of the diffuse subtype GC.
Metabolic reprogramming is a hallmark of cancer and considered to be critical to support accelerated proliferation, progression and metastasis. Imbalance in tryptophan (Trp) metabolism is found in several cancers, and kynurenine (kyn) is recognized as a critical microenvironment factor that contributes to immune depression [26]. IDO1 (2,3-dioxygenase) and TDO2 are two intracellular enzymes that mediate the first and the rate-limiting step of tryptophan catabolism in the kynurenine pathway [27,28,29]. Activation of the IDO1 pathway induces the blocking of differentiation, affects the functional anergy of effector T cells and promotes the de novo differentiation of Treg. Moreover, the correlated expression of IDO1 and collagen genes synergistically enhances tumor cell migration and invasion in vivo and in vitro [30]. While TDO2 expression by tumor cells themselves has been reported in several carcinomas, the role of TDO2 remains unclear.
Aryl hydrocarbon receptor (AhR) is a ligand-activated member of the PAS family of basic-helix-loop helix transcription factor. Through binding to exogenous and endogenous ligands, AhR has been involved in important cellular and pathological processes, such as control of proliferation, migration, angiogenesis and tumorigenesis [31,32,33]. An important role has emerged for AhR as a receptor for the endogenous ligand kynurenine [27] and for environmental ligands, and as a modulator of cancer immunity [29,34,35,36,37,38,39]. The role of AhR in immune escape program remains to be investigated in GCs.
In this pilot study, the primary objective was to document the expression of genes involved in the immunosuppressive PD1/PDL1 pathway (PD1, PDL1, and PDL2), tryptophan metabolism (IDO1 and TDO2), along with the immunoregulator AhR in a cohort of GCs patients [14], comparing aggressive/diffuse and intestinal subtypes. We investigated the dynamic expression of these genes during GC progression. We also analysed a possible link between the immune checkpoint PD1/ PDL1, IDO1 and AhR expression in gastric cancers.
2. Material and Methods
2.1. Patients and Tissue Samples
The cohort of 29 GC patients has been previously described [14]. In addition to gender, age, tumor size and depth of tumor invasion, lymphatic invasion, TNM status and smoking were introduced. The malignancy of infiltrating carcinomas was scored according to the TNM staging system (Stage I to IV), first according to AJCC7, revised from IGCA and AJCC8. This TNM staging includes a T score in the primary tumor (T1-T4), N score (lymph node metastasis) and M (metastasis) (see Table 1).
Table 1.
Clinicopathological characteristics of gastric carcinoma patients: poorly cohesive adenocarcinoma and intestinal-subtype adenocarcinomas. Median (range) of gene mRNA expression levels; p value (a Chi2. b Mann Whitney). Significant p value < 0.05 (in bold), NS, not significant. Comparative basal levels of genes in normal tissue (×1) are as follow: PD1 (19), PDL1 (53), PDL2 (86), IDO1 (70), TDO2 (18) and IDO2 (1).
| Total GC (n = 29) | Poorly CohesiveGC (n = 13) (45%) |
Intestinal-Subtype GC (n = 16) (n = 55%) | p-Value | |
|---|---|---|---|---|
| Gender, n (%) | ||||
| male | 13/29 | 6/13 (46%) | 7/16 (43%) | 0.90 (NS) a |
| female | 16/29 | 7/13 (54%) | 9/16 (56%) | |
| Age (years, median) | 63 +/−17 | 57(27–71) | 75(59–82) | 0.0004 b |
| Tumor size (mm), n | ||||
| <50 | 10/27 | 4/11 (36%) | 6/16 (37%) | 0.10 (NS) b |
| >=50 | 17/27 | 7/11 (64%) | 10/16 (63%) | 0.95 (NS) a |
| Depth of tumor invasion | ||||
| T1-T2 | 6/29 | 2/13 (15%) | 4/16 (33%) | 0.5 (NS) a |
| T3-T4 | 23/29 | 11/13 (85%) | 12/16 (67%) | |
| Lymphatic invasion, n (%) | ||||
| negative | 11/28 | 1/13 (7%) | 10/15 (67%) | 0.0014 a |
| positive | 17/28 | 12/13 (92%) | 5/15 (33%) | |
| Vascular invasion, n + (%) | ||||
| negative | 9/29 | 3/13 (23%) | 6/16 (38%) | 0.67 (NS) a |
| positive | 20/29 | 10/13 (77%) | 10/16 (62%) | |
| Neural invasion, n (%) | ||||
| negative | 23/29 | 2/13 (15%) | 4/16 (25%) | 0.66 (NS) a |
| positive | 6/29 | 11/13 (68%) | 12/16 (75%) | |
| Metastasis (M), n (%) | ||||
| negative | 24/29 | 9/13 (69%) | 15/16 (94%) | 0.14 (NS) a |
| positive | 5/29 | 4/13 (31%) | 1/16 (6%) | |
| TNM status | ||||
| I-II | 16/29 | 5/13 (38.5%) | 11/16 (69%) | 0.10 (NS) a |
| III-IV | 13/29 | 8/13 (61.5%) | 5/16 (31%) | |
| Smoking | ||||
| negative | 12/22 | 4/12 | 8/12 | 0.77 (NS) a |
| positive | 10/22 | 3/10 | 7/10 |
2.2. Total RNA Preparation and Real-Time RT-PCR
The conditions for total RNA extraction, complementary cDNA synthesis and qRT-PCR conditions were as previouly described [14]. We used real-time quantitative PCR to analyse the expression of selected genes in the gastric tumors samples as compared to the non-tumoral samples. The theoretical and practical aspects of real-time quantitative PCR have been described in detail elsewhere [14]. using ABI Prism 7900 Sequence Detection System (Applied Biosystem; Thermo Fisher Scientific, Inc., Waltham, MA, USA). Reverse transcription PCR was conducted with the high capacity cDNA reverse transcriptase kit (Applied Biosystem; Thermo Fisher Scientific, Inc, Waltam, MA, USA). We quantified transcripts of the TBP gene (Genbank accession NM 003194) encoding the TATA box-binding protein (a component of the DNA-binding protein complex TFIID) as an endogenous housekeeping gene, and normalized each sample to the TBP content, as previously described.
Primers for genes were selected using the Oligo 6.0 computer program (National Biosciences, Plymouth, MN, USA). We searched the dbEST and nr databases to confirm the absence of single nucleotide polymorphisms in the primer sequences and the total gene specificity of the nucleotide sequences chosen as primers. The nucleotide sequences of the primers used to amplify target genes are available on request. Each sample was normalized on the basis of its TBP content. Results, expressed as N-fold differences in target gene expressions relative to the TBP gene (and termed “Ntarget”), were determined as Ntarget = 2ΔCtsample, where the ΔCt value of the sample was determined by subtracting the average Ct value of the specific target gene from the average Ct value of the TBP gene. Ntarget values of the samples were subsequently normalized so that the median of Ntarget values for normal gastric tissues (n = 11) was 1. Preliminary analysis of gene expression have compared basal levels in normal samples in the same patients as their tumors (either diffuse- or intestinal- GC subtypes). We did not observe changes for most of the genes described in the study (ratio for the median levels ranging from 0.8 to 1.2). Moreover, to increase the reliability of the method of detection, gene expression was measured simultaneously. For each gene expression, normalized RNA values of 3 (or more) were considered to represent gene overexpression in tumor samples, and values 0.33 (or less) represented gene underexpression.
2.3. Statistical Analysis
For each gene, differences of expression between tumors versus normal tissues (fold change) were analyzed as previously described [14,29]. The relative expression of genes was characterized by the median and the range. Differences in the number of samples that over- (>3-fold) or under- (<3-fold) expressed were analyzed using the Chi2-square test. The relationships between expressions of genes in gastric cancer were determined using non parametric Spearman’s rank correlation test. Relationships between expression levels and clinical parameters were analyzed using non parametric Kruskal-Wallis (or Mann-Whitney) and Chi-square tests, as indicated in each Table. Statistical analyses were performed using Prism 5.03 software (GraphPad, San Diego, CA, USA). Differences were considered significant at confidence levels greater than 95% (p < 0.05).
2.4. Immunocytochemistry
Immunohistochemical labeling was performed on paraffin sections (4 mm) as previously described [29]. Immunohistochemical analysis for AhR (santaCruz) was performed using Ventana Autostainer (Roche Diagnostics, Indianapolis, IN, USA). AhR immunostaining was analyzed blindly by two specialists including a certified pathologist.
3. Results
3.1. Patient’s Characteristics
The clinicopathologic characteristics of the study population are shown in Table 1. The distribution of gastric tumor subtypes was as follows: diffuse (n = 13, 45%) and intestinal (n = 16, 55%) subtype GCs, according to the Lauren classification. Patients with diffuse adenocarcinoma are younger (p = 0.0004, Table 1), and harbor tumors with more aggressive characteristics, such as more lymphatic invasion (Table 1 p = 0.001), accompanied by massive stromal fibrosis [14] and metastasis than patients with the intestinal GC sub-type (Table 1). Vascular and neural invasion were not different (Table 1). In addition, when comparing the TNM stage, diffuse GC was present at TNM stages II, III and IV (38%, 31% and 31%, respectively), while intestinal subtype was more likely at stages I, II and III (26%, 44% and 25%, respectively).
3.2. Expression of PD-L1, PD-L2 and PD1 in Gastric Cancers
Significant higher expression of PD-L1 was observed in intestinal subtype vs. peri-tumoral samples (Table 2), along with overexpression (>3) in 30% of the cases (Table S1). Significant higher PD-L1 expression in the intestinal subtype occurred in the absence of lymphatic invasion (×3, p = 0.04) and in the early stages (TNM I-II, ×2, p = 0.03) as compared to non-tumoral tissue (Table 3). In contrast to the intestinal subtype, no significant modulation of PD-L1 expression was observed in diffuse GC vs. peri-tumoral samples (no overexpression and no change with clinical parameters) (Table 2, Table 3 and Table S1).
Table 2.
Statistical analysis of mRNA expression of genes involved in immunity and tryptophan metabolism in gastric cancers. Median (range) of gene mRNA expression levels GCs as compared to non tumoral gastric tissue (PT normalized to 1); p value a (Mann Whitney’s U test); Significant p-value a < 0.05 (in bold); median range of genes between GC subtypes, p value (Mann Withney pliciter le test). Significant p-value < 0.05 (in bold). NS, not significant. Comparative basal levels of genes in normal tissue (x1) are as follow: PD1 (19), PDL1 (53), PDL2 (86), IDO1 (70), TDO2 (18) and IDO2 (1).
| Genes | PT (n = 11) | All Tumors (n = 29) | p-Value a | Intestinal-GC vs. PT (n = 16) |
p-Value a | Diffuse-GC vs. PT (n = 13) |
p-Value a | p-Value subtypes |
|---|---|---|---|---|---|---|---|---|
| Immunity | ||||||||
| PD/PDCD1 | 1 (0.35–2.80) | 1.63 (0.81–5.3) | 0.001 | 1.71 (0.81–5.30) | 0.003 | 1.53 (0.87–3.08) | 0.009 | 0.35 (NS) |
| PDL1/CD274 | 1 (0.57–2.70) | 1.27 (0.52–6.63) | 0.33 (NS) | 1.46 (0.52–6.63) | 0.08 (NS) | 1.03 (0.57–1.56) | 0.84 (NS) | 0.018 |
| PDL2/PDCDL2 | 1 (0.54–1.63) | 1.52 (0.7–2.84) | 0.009 | 1.67 (0.70–2.79) | 0.014 | 1.21 (0.89–2.84) | 0.036 | 0.51 (NS) |
| Trypt metabolism | ||||||||
| IDO1 | 1 (0.19–1.46) | 2.17 (0.34–205) | <0.0001 | 3 (0.34–205) | 0.0006 | 1.96 (0.57–4.78) | 0.002 | 0.14 (NS) |
| TDO2 | 1 (0.45–2.95) | 5.41 (1.36–25.2) | <0.0001 | 7.45 (1.4–25.2) | <0.0001 | 3.33 (1.36–11.9) | 0.0002 | 0.049 |
| Arylhydrocarbon receptor | ||||||||
| AhR | 1 (0.37–1.64) | 1.94 (0.55–3.53) | 0.002 | 1.60 (0.65–3.53) | 0.003 | 2.12 (0.55–3.35) | 0.001 | 0.13 (NS) |
Table 3.
Correlation of genes involved in immune checkpoints (PD1, PD-L1 and PD-L2) with clinical parameters in all gastric tumors and subtypes. Median (range) of gene mRNA expression levels; p value (Mann Whitney). * Significant p value < 0.05 (in bold). ND, not determined, EPN, perineural invasion, TNM, tumor, node, metastasis.
| All Gastric Tumors (n = 29) | Intestinal Sub-Type (n = 16) | Diffuse Sub-Type (n = 13) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| PD1 | PDL1 | PDL2 | PD1 | PDL1 | PDL2 | PD1 | PDL1 | PDL2 | |||
| Gender. | p = 0.25 | p = 0.51 | p = 0.65 | Gender. | p = 0.11 | p = 0.58 | p = 0.15 | Gender. | p = 0.81 | p = 0.80 | p = 0.19 |
| Male (n = 13) | 1.5 (0.8–3.1) | 1.14 (0.5–6.6) | 1.21 (0.7–2.8) | Male (n = 7) | 1.5 (0.81–3.13) | 1.4 (0.52–6.63) | 1.17 (0.7–2.65) | Male (n = 6) | 1.51 (0.87–3.08) | 1.04 (0.62–1.27) | 1.71 (0.89–2.84) |
| Female (n = 16) | 1.7 (1.2–5.3) | 1.33 (0.6–5.5) | 1.53 (0.9–2.8) | Female (n = 9) | 2.18 (1.42–5.3) | 2.03 (0.78–5.55) | 1.83 (1.12–2.8) | Female (n = 7) | 1.58 (1.22–2.01) | 1.03 (0.57–1.56) | 1.16 (0.89–1.83) |
| Age | p = 0.08 | p = 0.18 | p = 0.20 | Age | ND | ND | ND | Age | p = 0.72 | p = 0.12 | p = 0.80 |
| <60 years (n = 9) | 1.49 (0.8–2.0) | 1.09 (0.5–1.6) | 1.21 (0.8–1.8) | <60 years (n = 1) | 0.81 | 0.52 | 0.76 | <60 years (n = 8) | 1.51 (0.87–2.01) | 1.11 (0.62–1.56) | 1.38 (0.89–1.83) |
| >60 years (n = 20) | 1.71 (0.9–5.3) | 1.33 (0.6–6.6) | 1.67 (0.7–2.8) | >60 years (n = 15) | 1.76 (0.94–5.3) | 1.52 (0.8–6.63) | 1.83 (0.7–2.8) | >60 years (n = 5) | 1.58 (1.22–3.08) | 0.78 (0.57–1.27) | 1.16 (0.90–2.84) |
| Tumor invasion | p = 0.74 | p = 0.72 | p = 0.32 | Tumor invasion | p = 0.86 | p > 0.9999 | p > 0.9999 | Tumor invasion | ND | ND | ND |
| T1-T2 (n = 6) | 1.42 (1–5.3) | 1.14 (0.6–85) | 0.93 (0.7–2.8) | T1-T2 (n = 4) | 2.85 (0.94–5.3) | 1.67 (0.96–4.25) | 1.66 (0.7–2.8) | T1-T2 (n = 2) | 1.42 (1.27–1.58) | 0.67 (0.57–0.78) | 0.93 (0.9–0.96) |
| T3-T4 (n = 23) | 1.65 (0.8–3.1) | 1.27 (0.5–6.6) | 1.55 (0.8–2.8) | T3-T4 (n = 12) | 1.71 (0.81–3.13) | 1.46 (0.52–6.63) | 1.67 (0.76–2.65) | T3-T4 (n = 11) | 1.53 (0.9–3.1) | 1.1 (0.62–1.56) | 1.55 (0.89–2.84) |
| Vascular invasion | p = 0.23 | p = 0.48 | p = 0.04 * | Vascular invasion | p = 0.14 | p = 0.56 | p = 0.03 * | Vascular invasion | p > 0.9999 | p = 0.83 | p = 0.79 |
| negative (n = 9) | 1.63 (1.3–5.3) | 1.56 (0.6–6.6) | 1.83 (1.2–2.8) | negative (n = 6) | 2.66 (1.42–5.3) | 3.07 (0.78–6.63) | 2.16 (1.21–2.8) | negative (n = 3) | 1.53 (1.32–1.63) | 0.88 (0.62–1.56) | 1.21 (1.18–1.72) |
| positive (n = 20) | 1.61 (3.1–5.3) | 1.22 (0.5–5.5) | 1.17 (0.7–2.8) | positive (n = 10) | 1.65 (0.81–2.5) | 1.37 (0.52–5.55) | 1.17 (0.7–2.65) | positive (n = 10) | 1.53 (0.87–3.08) | 1.06 (0.57–1.35) | 1.35 (0.89–2.84) |
| Lymphatic invasion | p = 0.05 | p = 0.009 * | p = 0.72 | Lymphatic invasion | p = 0.054 | p = 0.04 * | p = 0.39 | Lymphatic invasion | ND | ND | ND |
| negative (n = 11) | 2.18 (0.9–3.1) | 2.03 (0.6–6.6) | 1.21 (0.7–2.8) | negative (n = 10) | 2.24 (0.94–5.3) | 3.07 (0.96–6.63) | 1.36 (0.7–2.8) | negative (n = 1) | 1.53 | 0.62 | 1.18 |
| positive (n = 17) | 1.49 (0.8–3.1) | 1.03 (0.5–1.6) | 1.71 (0.8–2.9) | positive (n = 5) | 1.48 (0.81–1.66) | 0.87 (0.52–1.52) | 2.22 (0.76–2.65) | positive (n = 12) | 1.53 (0.87–3.08) | 1.06 (0.57–1.56) | 1.38 (0.89–2.84) |
| Metastasis | p = 0.25 | p = 0.15 | p = 0.20 | Metastasis | ND | ND | ND | Metastasis | p = 0.93 | p = 0.82 | p = 0.79 |
| negative (n = 24) | 1.65 (0.9–5.3) | 1.29 (0.6–6.6) | 1.71 (0.7–2.8) | negative (n = 15) | 1.76 (0.94–5.3) | 1.52 (0.8–6.63) | 1.83 (0.7–2.8) | negative (n = 9) | 1.49 (0.87–3.08) | 1.03 (0.57–1.32) | 1.71 (0.89–2.84) |
| positive (n = 5) | 1.53 (0.8–2) | 0.72 (0.5–1.6) | 1.18 (0.8–1.5) | positive (n = 1) | 0.81 | 0.52 | 0.76 | positive (n = 4) | 1.58 (1.22–2.01) | 1.03 (0.62–1.56) | 1.19 (1.16–1.55) |
| TNM | p = 0.37 | p = 0.008 * | p = 0.43 | TNM | p = 0.037 * | p = 0.03 * | p = 0.33 | TNM | p = 0.21 | p = 0.52 | p = 0.80 |
| I-II (n = 16) | 1.8 (0.9–5.3) | 1.33 (0.9–6.6) | 1.36 (0.7–2.8) | I-II (n = 11) | 2.18 (0.94–5.3) | 2.03 (0.96–6.63) | 1.21 (0.7–2.8) | I-II (n = 5) | 1.32 (0.87–1.9) | 1.09 (0.88–1.32) | 1.71 (0.89–1.83) |
| III-IV (n = 13) | 1.53 (0.8–3.1) | 0.87 (0.5–1.6) | 1.55 (0.76–2.8) | III-IV (n = 5) | 1.48 (0.81–1.66) | 0.87 (0.52–1.52) | 2.22 (0.76–2.65) | III-IV (n = 8) | 1.6 (1.22–3.08) | 0.88 (0.57–1.56) | 1.19 (0.9–2.84) |
| EPN | p = 0.13 | p > 0.999 | p = 0.54 | EPN | p = 0.02 * | p = 0.86 | p = 0.11 | EPN | ND | ND | ND |
| negative (n = 6) | 2.1 (1.3–5.3) | 1.26 (0.6–4.25) | 1.67 (0.9–2.8) | negative (n = 4) | 3.5 (1.76–5.3) | 1.69 (1.18–4.25) | 2.16 (1.52–2.8) | negative (n = 2) | 1.42 (1.27–1.58) | 0.67 (0.57–0.78) | 0.93 (0.9–0.96) |
| positive (n = 23) | 1.53 (0.8–3.1) | 1.29 (0.5–6.6) | 1.21 (0.7–2.8) | positive (n= 12) | 1.57 (0.81–3.13) | 1.46 (0.52–6.63) | 1.19 (0.7–2.65) | positive (n = 11) | 1.53 (0.9–3.1) | 1.1 (0.62–1.56) | 1.55 (0.89–2.84) |
| Smoking | p = 0.75 | p = 0.91 | p = 0.0006 * | Smoking | p = 0.45 | p = 0.46 | p = 0.0003 * | Smoking | p = 0.63 | p = 0.57 | p = 0.74 |
| negative (n = 12) | 1.58 (0.9–5.3) | 1.26 (0.6–4.2) | 1.83 (0.9–2.6) | negative (n = 8) | 1.71 (1.42–5.3) | 1.37 (0.78–4.25) | 2.05 (1.52–2.65) | negative (n = 4) | 1.51 (0.87–1.63) | 1.11 (0.62–1.56) | 1.19 (0.89–1.71) |
| positive (n = 10) | 1.61 (0.8–3.1) | 1.33 (0.5–6.6) | 1.04 (0.7–1.5) | positive (n = 7) | 1.65 (0.81–3.13) | 1.54 (0.52–6.63) | 1.12 (0.7–1.21) | positive (n = 3) | 1.58 (1.27–2.01) | 0.78 (0.57–1.35) | 0.96 (0.9–1.55) |
The expression of PD-L2, encoding another ligand for PD1, was increased in both intestinal and diffuse GC subtypes (×1.67, p = 0.014 and ×1.21 p = 0.036, respectively) (Table 2), but with no cases of high expression (>3) vs. their peri-tumoral samples (Table S1). In the intestinal subtype, a higher expression of PD-L2 correlated with the absence of vascular invasion (p = 0.03) and smoking (p < 0.001) (Table 3). PD-L2 was independent on clinical parameters in diffuse GCs (Table 3).
PD1 encodes the receptor for PD-L1 and PD-L2. Expression of PD1 significantly increased in gastric tumors vs. their peri-tumoral counterpart (×1.63, p = 0.001), both in intestinal and diffuse subtypes (×1.71, p = 0.003 and ×1.53 p = 0.009, respectively) (Table 2). Overexpression of PD1 (>3) was observed in 19% of intestinal and 8% of diffuse GC (Table S1). Interestingly, in intestinal GCs, a higher PD1 expression was observed in the absence of lymphatic invasion (×2.2, p = 0.05), absence of perineural invasion (×3.5, p = 0.02) and lower TNM stages (I-II) (×2.2, p = 0.037) (Table 3) that are clinical parameters of early stage GCs, i.e., less aggressive GCs. In contrast to the intestinal GC, PD1 expression was independent of clinical parameters in diffuse GCs (Table 3). Of note, in all GC subtypes, the mRNA expression levels of PD1 did not differ according to sex, age, or vascular invasion (Table 3).
Overall, in the intestinal GCs, expression of PD-L1 together with PD1 gradually decreased from the early stage to the advanced stage (lymphatic invasion and/or TNM III-IV), along with a decrease in PD-L2 expression with vascular invasion. In contrast, no correlation of PD1, PD-L1 or PD-L2 was observed with clinical parameters in diffuse GCs.
3.3. Expression of IDO1, IDO2 and TDO2 in Gastric Cancers
We further analyzed the expression of IDO1, IDO2 and TDO2, three genes that encode enzymes involved in the early steps of tryptophan metabolism leading to kynurenine, an endogenous AhR ligand [27]. The tryptophan (TRP) to kynurenine (KYN) metabolic pathway is now firmly established as a key regulator of innate and adaptative immunity [26].
As shown in Table 2, the expression of IDO1 was significantly increased in all gastric tumors vs. their peritumoral counterpart (×2.2, p < 0.0001), with IDO1 expression being significantly higher in both the intestinal (×3, p = 0.0006) and diffuse (×1.96, p = 0.002) GC subtypes as compared to non- tumoral gastric tissues (Table 2). Heterogeneous expression of IDO1 was observed in the intestinal subtype with a strong overexpression (>3) in 50% of cases, as compared to diffuse GC (23% of cases) (Table S1). In all GC tumors, higher IDO1 expression was significantly observed in less advanced stages, corresponding to absence of lymphatic invasion (×6.3, p = 0.005) and lower TNM stages (I and II, ×3.2, p = 0.036) (Table 4). Moreover, the higher expression of IDO1 in intestinal subtype corresponded to the absence of lymphatic invasion (×25.4, p = 0.004) and to lower TNM stage (×6.4, p = 0.02) (Table 4). In contrast to intestinal GC, IDO1 expression appeared independent of clinical parameters in our cohort of diffuse GCs (Table 4).
Table 4.
Correlation of genes involved in tryptophan metabolism with clinical parameters in all gastric tumors and subtypes. Median (range) of gene mRNA expression levels; p value (Mann Whitney). * Significant p value <0.05 (in bold). ND, not determined.
| All Gastric Tumors | IDO1 | TDO2 | Intestinal Sub-Type (n = 16) | IDO1 | TDO2 | Diffuse Sub-Type (n = 13) | IDO1 | TDO2 |
|---|---|---|---|---|---|---|---|---|
| Gender. | p = 0.23 | p = 0.08 | Gender. | p = 0.09 | p = 0.53 | Gender. | p = 0.71 | p = 0.035 * |
| Male (n = 13) | 2 (0.34–44.5) | 8.5 (1.4–25) | Male (n = 7) | 1.77 (0.34–44.5) | 9.45 (1.38–25) | Male (n = 6) | 2.37(0.57–4.78) | 6.82 (1.92–1.9) |
| Female (n = 16) | 2.25 (1.3–205) | 4.23 (1.4–20) | Female (n = 9) | 6.36 (1.43–205) | 6.19 (2.33–20) | Female (n = 7) | 1.75(1.31–3.43) | 2.42 (1.36–5.26) |
| Age | p = 0.06 | p = 0.045 * | Age | ND | ND | Age | p = 0.72 | p = 0.78 |
| <60 years (n = 9) | 1.96 (0.3–3.4) | 3.33 (1.4–7.2) | <60 years (n = 1) | 0.34 | 1.38 | <60 years (n = 8) | 1.98 (0.57–0.43) | 4.16 (1.92–7.17) |
| >60 years (n = 20) | 2.85 (1–205) | 7.45 (1.4–25.2) | >60 years (n = 15) | 3.15 (0.98–205) | 8.5 (2.33–25.2) | >60 years (n = 5) | 1.75 (1.32–4.78) | 2.42(1.36–11.9) |
| Tumor invasion | p = 0.38 | p = 0.74 | Tumor invasion | p = 0.32 | p > 0.9999 | Tumor invasion | ND | ND |
| T1–T2 (n = 6) | 3.53 (1.3–53) | 5.1 (1.6–20) | T1–T2 (n = 4) | 5.14 (3.15–53) | 6.95 (4.73–20) | T1–T2 (n = 2) | 1.4 (1.32–1.5) | 2 (1.6–2.4) |
| T3–T4 (n = 23) | 2 (0.3–205) | 6.19 (1.4–25.2) | T3–T4 (n = 12) | 2.05 (0.34–205) | 7.7 (1.38–25) | T3–T4 (n = 11) | 2 (0.57–4.8) | 5 (1.36–11.9) |
| Vascular invasion | p = 0.33 | p = 0.39 | Vascular invasion | p = 0.18 | p = 0.22 | Vascular invasion | p = 0.32 | p = 0.50 |
| negative (n = 9) | 3.43 (0.6–205) | 6.19 (1.9–20) | negative (n = 6) | 25.4 (1.43–205) | 9.22 (5.4–20) | negative (n = 3) | 0.81 (0.57–3.43) | 2.91 (1.92–5.0) |
| positive (n = 20) | 1.98 (0.3–141) | 5.19 (1.4–25.2) | positive (n = 10) | 2.05 (0.34–141) | 5.78 (1.38–25) | positive (n = 10) | 1.98(1.31–4.78) | 4.29 (1.36–11.9) |
| Lymphatic invasion | p = 0.005 * | p = 0.85 | Lymphatic invasion | p = 0.004 * | p = 0.37 | Lymphatic invasion | ND | ND |
| negative (n = 11) | 6.3 (0.57–205) | 5.4 (1.9–20) | negative (n = 10) | 25.4 (1.74–205) | 5.91 (2.33–20) | negative (n = 1) | 0.57 | 1.92 |
| positive (n = 17) | 1.77 (0.3–4.8) | 5.2 (1.4–25.2) | positive (n = 5) | 1.43 (0.34–2.96) | 12.47 (1.38–25) | positive (n = 12) | 1.98 (0.8–4.8) | 4.16 (1.36–11.9) |
| Metastasis | p = 0.12 | p = 0.005 * | Metastasis | ND | ND | Metastasis | p = 0.75 | p = 0.034 * |
| negative (n = 24) | 2.53 (0.8–205) | 6.44 (1.6–25) | negative (n = 15) | 3.15 (0.98–205) | 8.5 (2.33–25) | negative (n = 9) | 2 (0.81–4.78) | 5.26 (1.58–11.9) |
| positive (n = 5) | 1.75 (0.3–3.4) | 1.92 (1.4–2.9) | positive (n = 1) | 0.34 | 1.38 | positive (n = 4) | 0.85 (0.57–3.43) | 2 (1.36–2.91) |
| TNM | p = 0.035 * | p = 0.44 | TNM | p = 0.02 * | p = 0.38 | TNM | p = 0.78 | p = 0.17 |
| I–II (n = 16) | 3.25 (0.8–205) | 5.91 (2.3–20) | I–II (n = 11) | 6.36 (0.98–205) | 6.41 (2.33–20) | I–II (n = 5) | 2 (0.81–3.35) | 5.26 (3.33–7.17) |
| III–IV (n = 13) | 1.75 (0.3–4.8) | 2.91 (1.4–25.2) | III–IV (n = 5) | 1.43 (0.34–2.96) | 12.47 (1.38–25) | III–IV (n = 8) | 1.85(0.57–4.78) | 2.24(1.36–11.9) |
| EPN | p = 0.94 | p = 0.22 | EPN | p = 0.86 | p = 0.34 | EPN | ND | ND |
| negative (n= 6) | 2.03 (1.3–53) | 2.49 (1.6–20) | negative (n= 4) | 4.34 (1.74–53) | 3.99 (2.33–20) | negative (n = 2) | 1.4 (1.32–1.5) | 2 (1.6–2.4) |
| positive (n= 23) | 2.17 (0.3–205) | 6.41 (1.4–25.2) | positive (n= 12) | 3.05 (0.34–205) | 8.75 (1.38–25) | positive (n = 11) | 2 (0.57–4.8) | 5 (1.36–11.9) |
| Smoking | p = 0.97 | p = 0.18 | Smoking | p = 0.68 | p = 0.28 | Smoking | p = 0.40 | p = 0.23 |
| negative (n = 12) | 2.16 (0.6–205) | 6.82 (1.9–25) | negative (n = 8) | 2.05 (1.3–205) | 10.74 (2.33–25) | negative (n = 4) | 2.67(0.57–3.43) | 4.69(1.92–7.17) |
| positive (n = 10) | 2.55 (0.3–141) | 4.93 (1.4–10) | positive (n = 7) | 3.92 (0.34–141) | 6.41 (1.38–10) | positive (n = 3) | 1.48(1.32–1.96) | 2.07(1.58–2.42) |
A significant increase of TDO2 expression was observed in all GC tumors (×5.4, p < 0.0001), both in intestinal and diffuse GC subtypes (×7.4, p < 0.0001 and ×3.3, p = 0.0002, respectively), as compared to non-tumoral gastric tissues (Table 2). Strong overexpression (>3) of TDO2 was preferentially observed in intestinal subtype (80% of cases, especially in the absence of lymphatic invasion (Table 4 and Table S1). In the diffuse GCs, the highest expression of TDO2 (with 50% of overexpression) was observed in males (p = 0.035) and in the absence of metastasis (p = 0.034) (Table 4). IDO2 was expressed at very low basal level in non-tumoral gastric tissues.
3.4. Correlation of Expression between PD-L1 and IDO1 in Gastric Cancers
As an exploratory analysis, we conducted non-parametric Spearman rank correlation tests to assess the associations of PD1/PD-L1 and IDO1 expression in gastric cancers (see Materials and Methods). The expression levels of PD-L1 and IDO1 were correlated in all GCs (r = 0.65, p = 0.0001) (Table S2), both in the intestinal (r = 0.68, p = 0.004) and diffuse (r = 0.63, p < 0.05) GCs (Tables S3 and S4). The correlation between PD-L1 and TDO2 was lower in all GCs (r = 0.50, p = 0.006) (Table S2), in the intestinal subtype (r = 0.32, p = 0.23) or in diffuse GCs (r = 0.48, p > 0.05) (Tables S3 and S4). Moreover, strong PD1 and PD-L1 correlated in intestinal subtype, while PD1 and PD-L2 correlated in diffuse subtype (Tables S3 and S4).
3.5. High AhR Expression in Gastric Cancers
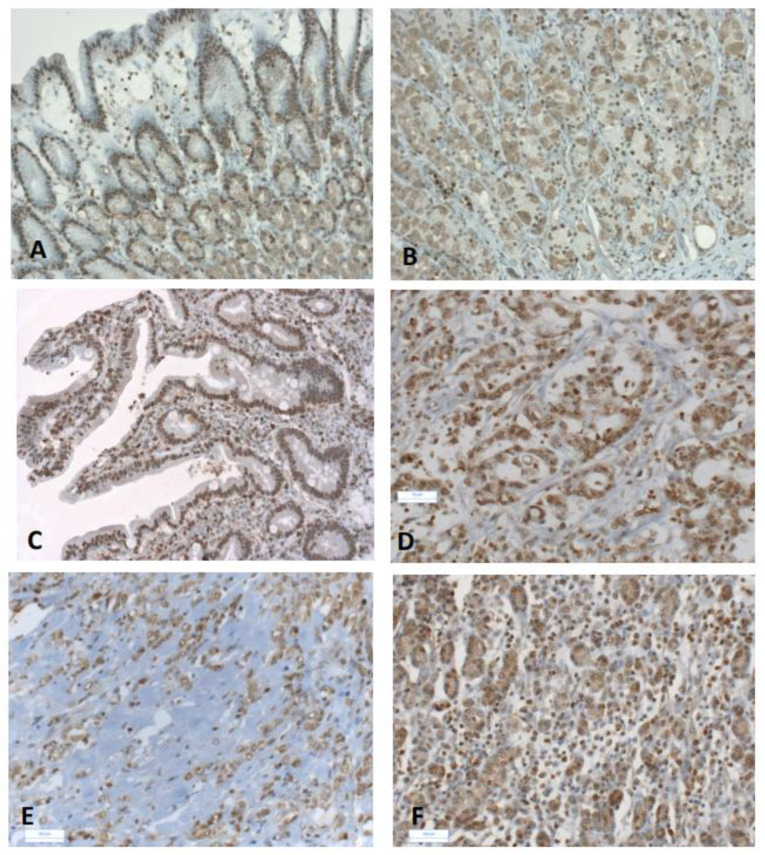
Both IDO1 and TDO2 are a source of kynurenine, an activated ligand of AhR [26,27]. Therefore, since we observed a higher expression of IDO1 and TDO2 in gastric cancers as compared to non-tumoral tissue, we further analyzed AhR expression and protein localization in gastric tumors (see Materials and Methods). Increased AhR expression was found in GCs, both in intestinal and diffuse subtypes (×1.6, p = 0.003, and ×2.1, p = 0.001, respectively) (Table 2), with few cases of overexpression (8–12%, Table S1). Moreover, AhR expression was independent of clinical parameters in all tumors, either intestinal or diffuse GCs (Table 5). AhR was present in tumor epithelial and stromal cells (Figure 1), including fibroblasts, endothelial and immune cells (such as lymphocytes).
Table 5.
Relationship between AhR transcript levels and classical clinical parameters in all GCs and subtypes. Median (range) of gene mRNA expression levels; p value (Mann Whitney). ND, not determined.
| All Tumors n = 29 | Intestinal Sub-Type n = 16 | Diffuse Sub- Type n = 13 |
|||
|---|---|---|---|---|---|
| AhR | AhR | AhR | |||
| Gender. | p = 0.51 | Gender. | p = 0.19 | Gender. | p = 0.81 |
| Male (n = 13) | 1.54 (0.55–3.33) | Male (n = 7) | 1.71 (0.89–2.84) | Male (n = 6) | 1.51 (0.87–3.08) |
| Female (n = 16) | 1.35 (0.65–3.53) | Female (n = 9) | 1.16 (0.89–1.83) | Female (n = 7) | 1.58 (1.22–2.01) |
| Age | p = 0.82 | Age | ND | Age | p = 0.72 |
| <60 years (n = 9) | 1.94 (0.55–3.35) | <60 years (n = 1) | 1.38 (0.89–1.83) | <60 years (n = 8) | 1.51 (0.87–2.01) |
| >60 years (n = 20) | 1.80 (0.65–3.53) | >60 years (n = 15) | 1.16 (0.90–2.84) | >60 years (n = 5) | 1.58 (1.22–3.08) |
| Tumor invasion | p = 0.21 | Tumor invasion | ND | Tumor invasion | ND |
| T1–T2 (n = 6) | 1.45 (0.65–2.86) | T1–T2 (n = 4) | 0.93 (0.9–0.96) | T1–T2 (n = 2) | 1.42 (1.27–1.58) |
| T3–T4 (n = 23) | 1.94 (0.55–3.53) | T3–T4 (n = 12) | 1.55 (0.89–2.84) | T3–T4 (n = 11) | 1.53 (0.9–3.1) |
| Vascular invasion | p = 0.14 | Vascular invasion | p = 0.79 | Vascular invasion | p>0.9999 |
| negative (n = 9) | 1.25 (0.82–2.96) | negative (n = 6) | 1.21 (1.18–1.72) | negative (n = 3) | 1.53 (1.32–1.63) |
| positive (n = 20) | 2.05 (0.55–3.53) | positive (n = 10) | 1.35 (0.89–2.84) | positive (n = 10) | 1.53 (0.87–3.08) |
| Lymphatic invasion | p = 0.11 | Lymphatic invasion | ND | Lymphatic invasion | ND |
| negative (n = 11) | 1.25 (0.65–3.18) | negative (n = 10) | 1.18 | negative (n = 1) | 1.53 |
| positive (n = 17) | 2.11 (0.55–3.53) | positive (n = 5) | 1.38 (0.89–2.84) | positive (n = 12) | 1.53 (0.87–3.08) |
| Metastasis | p = 0.92 | Metastasis | ND | Metastasis | p = 0.93 |
| negative (n = 24) | 1.96 (0.55–3.53) | negative (n = 15) | 1.71 (0.89–2.84) | negative (n = 9) | 1.49 (0.87–3.08) |
| positive (n = 5) | 2.1 (0.82–2.55) | positive (n = 1) | 1.19 (1.16–1.55) | positive (n = 4) | 1.58 (1.22–2.01) |
| TNM | p = 0.30 | TNM | p = 0.80 | TNM | p = 0.21 |
| I–II (n = 16) | 1.77 (0.54–3.35) | I–II (n = 11) | 1.71 (0.89–1.83) | I–II (n = 5) | 1.32 (0.87–1.9) |
| III–IV (n = 13) | 2.11 (0.82–3.53) | III–IV (n = 5) | 1.19 (0.9–2.84) | III–IV (n = 8) | 1.6 (1.22–3.08) |
| EPN | p = 0.47 | EPN | ND | EPN | ND |
| negative (n = 6) | 1.58 (0.90–2.86) | negative (n = 4) | 0.93 (0.9–0.96) | negative (n = 2) | 1.42 (1.27–1.58) |
| positive (n = 23) | 1.94 (0.55–3.53) | positive (n = 12) | 1.55 (0.89–2.84) | positive (n = 11) | 1.53 (0.9–3.1) |
| Smoking | p = 0.85 | Smoking | p = 0.74 | Smoking | p = 0.63 |
| negative (n = 12) | 1.77 (0.55–3.35) | negative (n = 8) | 1.19 (0.89–1.71) | negative (n = 4) | 1.51 (0.87–1.63) |
| positive (n = 10) | 1.85 (0.82–3.53) | positive (n = 7) | 0.96 (0.9–1.55) | positive (n = 3) | 1.58 (1.27–2.01) |
Figure 1.
Immunohistochemical staining of AhR in gastric cancers. Representative immunostaining of AhR in non-tumoral gastric mucosa (A,B) and in gastric cancers (C–F). Weak cytoplasmic and nuclear expression of AhR were observed in epithelial cells (A,B). Intestinal subtype GC with metaplasia (TNM 2a) (C); strong nuclear AhR staining in epithelial and stromal cells (C). Moderately differentiated intestinal subtype (TNM2a) showing nuclear AhR staining in tubular glands and stroma (D). Advanced diffuse GC (TNM4) (E): the intensity of AhR immunostaining was lower in the scattered cells of single ring cell component (SRCC). Early diffuse GC (TNM2a) (F): AhR immunostaining in epithelial and stromal cells. Original magnification ×10 (A,C,E); ×20 (B,D,F).
4. Discussion
Intestinal and diffuse GCs are two gastric cancers with different aggressivity and prognosis. Intestinal GCs are more commonly diagnosed in aged patients, and are strongly associated with gastric mucosal atrophy and intestinal metaplasia, both of which are induced by chronic Helicobacter pylori infection. The diffuse subtype which represents a small minority of gastric cancer, is genomically stable and associated with decreased expression of CDH1 (E-cadherin), higher expression of RhoA and prominent mesenchymal features, thus resulting in tumor aggressiveness [11,12,13,14,15,17]. Diffuse GCs are associated with frequent metastasis in lymph nodes and the peritoneum, contributing to their poor prognosis. Most anti-cancer therapies have failed to substantially improve prognosis of GC patients. The molecular driver of anti-tumor immunity in GCs is still poorly understood, posing a major obstacle for selection of GC patients for immunotherapy trials. Although the expression of immunosuppressive markers including PD-L1 has been reported for various tumor types [21,40,41], it remains unclear for GCs and their associated subtypes in the Western population. In this retrospective analysis of tumor samples from 29 intestinal and diffuse GCs patients, from patients who underwent primary surgery at Lariboisiere Hospital (Paris, France), we report for the first time, the expression levels of AhR, and of several genes involved in immune gene signature (PD1, PD-L1 and PD-L2) and in tryptophan metabolism (IDO1/IDO2, TDO2). Association (or absence of association) with various clinical parameters are also described.
Escape from anti-tumor immunity is a second generation cancer hallmark. One key mechanism in the heterogeneous immune response is the PD1-PD-L1/PD-L2 axis. Immune checkpoints have been identified on both immune cells and tumor cells. PD1 is expressed on the surface of activated CD4+ and CD8+ T lymphocytes, B lymphocytes, but also on NK and dendritic cells [20]. PD-L1 is expressed on the surface of cancer cells and in cells of the tumor environment (T and B cells, macrophages and dendritic cells), while PD-L2 expression is more restricted to activated dendritic cells and macrophages [42]. The interaction of PD1 with ligands PDL1 and PDL2 provides an immune effector T cells and immune tolerance [20]. To date, data regarding the expression of PD1 /PDL1 in GC have been mostly evaluated in Asian populations [21,22,23]; studies in Caucasians are urgently needed.
In the present study, we present gene signatures associated with the PD-1-PD-L1/PD-L2 axis in GCs, including intestinal and diffuse subtypes. Selected gene expression differed between subtypes of GCs. A higher expression of PD-L1 along with PD-1 expression was observed in patients with intestinal GC, interestingly at a less advanced time (without lymphatic invasion and at the lower TNM). PD-L1 expression was correlated with PD1 expression. While the relevance of the PD1-PDL1 pathway in cancer has been extensively studied, the relevance of PD-L2 has received less attention. As compared to patients with a history of smoking, nonsmoking patients exhibit higher expression of PD-L2 in intestinal GC, an observation that has been recently reported for PD-L1 in lung cancer [43]. Therapy targeting both PD1 ligands may provide clinical benefit in these patients [44]. PD-L1 positive immune cells revealed by immunocytochemistry and infiltration of immune (CD3+ /or CD8+) cells correlated with survival outcome in Asian GC patients that include EBV-positive and MSI GCs [21,22,23,45]. More prevalent PD-L1 expression and better patient outcome was also observed in Western patients with EBV and MSI [46]. EBV and MSI were the most infiltrated GCs, harboring 30–50% T cells and 20% macrophages, while intestinal GC contained fewer T cells and more macrophages [9,47,48].
In contrast to the intestinal subtype, lower expression of PD-L1 was observed in diffuse GC (p = 0.02). Diffuse GC was the least infiltrated subtype GC. In particular, CD8+ T cells (CD8+ TILs) and circulating NK cells and Tregs were significantly lower in diffuse advanced gastric cancer compared to the intestinal type (p = 0.009) [9,49]. Low infiltration of immune cells, associated with low expression of PD-L1 in diffuse gastric cancers, suggests an underdeveloped immune resistance. Taken into account that the rate of diffuse GCs has strongly increased among Western populations [6], this immune signature may suggest that individual evaluation of PD1, PD-L1 or PD-L2 would be ineffective.
Mice overexpressing an active AhR exhibit enhanced stomach cancer [50], suggesting a role of AhR in carcinogenesis [51,52,53]. We observed significant increased AhR expression in GCs as compared to non-cancerous tissues, independently of intestinal or diffuse GC subtypes and clinical parameters. Nuclear AhR present in GC tumor and immune cells, fibroblasts and endothelial cells (Figure 1), suggests an activation of AhR, as previously reported in breast cancer [29]. In the past several years, AhR has been established as a critical ligand-dependent transcription factor involved in the regulation of the immune system and inflammatory response [29,54,55]. A large variety of exogenous (present in food and environment) and endogenous AhR ligands provide a complex scenario of the impact of AhR on tumorigenesis and immune homeostasis [33,56]. The effect of AhR ligands on differentiation of Th17 and Treg occurs through different mechanisms [57]. Considering AhR ligands, tryptophan catabolism plays a central role in creating an immunosuppressive environment [28,34,36,58,59,60].
The levels of expression of IDO1, IDO2 and TDO2 involved in the early steps of tryptophan metabolism leading to the AhR ligand kynurenine, were analysed [27,28,29]. Interestingly, IDO1 levels, but not IDO2 levels (not expressed), were significantly elevated in high AhR expressing gastric tumors. Increased IDO1 expression was mainly observed in the intestinal GC subtype, with an overexpression (>3) in 50% of the cases, along with a less advanced stage characterized by an absence of lymphatic invasion (p = 0.004) and lower TNM (p = 0.02)]. Higher IDO1 expression in early stage intestinal GC subtype (Table 4) is consistent with a previous study [21]. IDO1 can be overexpressed in tumor cells and dendritic cells, macrophages and endothelial cells [60]. IDO1 has been shown to be upregulated in an inflammatory microenvironment (e.g., in the presence of IFNγ, the most potent IDO inducer, LPS and pathogens) [61,62]. In other cancers, IDO1 expression may be constitutive with IDO-producing tumors cells surrounded by a lower number of lymphocytes. Our results suggest that the lower IDO1 expression observed in diffuse GC as compared to the intestinal subtype (p = 0.009) may be related to the significantly lower circulating NK cells and Tregs described in (advanced) diffuse GCs [9]. IDO enzyme activity may lead to a local amino-acid starvation response. T cells and NK cells are very sensitive to tryptophan deprivation and downstream metabolites from IDO activity (kynurenine) in their microenvironment [60,63]. Two related populations of CD4+T cells (Th17/CD4+/CD25+ and regulatory T (Treg) cells), with opposing functions during immune responses, shifted from TH17-dominant (through inflammation) to Treg-dominant (TGFβ) according to GC progression [64,65].
We report for the first time significant TDO2 up-regulation in GCs, both in intestinal (p = 0.014) and diffuse (p = 0.05) subtypes. The non-redundant role of IDO1 and TDO2 still remain unclear [66]. TDO2 was found in several cancers including lung, bladder, breast and ovarian carcinoma [29,67]. TDO2 is expressed in tumor cells that produce sufficient intracellular kynurenine concentrations to chronically activate the AhR, and by pro-inflammatory cytokines such as IL-6 in triple-negative breast cancer [67]. Notably, in triple negative breast cancer, the TDO2-AhR signaling axis promotes metastasis and resistance to anoikis [67]. The correlations between the expression of TDO2 and other genes (e.g., IDO1, TGFβ, and MMP9) observed in diffuse GC, but not intestinal GC (Sup Table 3 and Table 4), suggests a role of tumor and immune cells that merits further consideration using a larger sample of patients.
Our study has some limitations. First, the small number of tumor samples (30) could be a limiting factor and could induce a bias between intestinal and diffuse subtypes. However, in a previous study with the same Western cohort [14], we observed comparable decrease or increases of the gene expression, notably CDH1, CXCR4 and TGFβ, which are involved in epithelial mesenchymal transition and chemotaxis) in diffuse gastric cancers, as now well described. Second, we have not differentiated the subpopulation of diffusely infiltrating type of GC associated with extensive fibrosis (linitis or SRCC) [5,6] as compared to non linitis diffuse GC.
In conclusion, the results reported here document for the first time the time-dependent expression of PD-L1 and the IDO1-TDO2-kyn-AhR signaling pathway in diffuse and intestinal GCs. Our previous results in the same cohort of patients have suggested that mesenchymal features are more prominent in diffuse GC, resulting in tumor aggressiveness and fibrosis [14]. The present study suggests an inactive immune response in the advanced diffuse GC in patients undergoing surgery (no adaptive immune resistance). Further studies in a larger series of gastric tumor samples, especially with different clinical characteristics (-early diffuse subpopulation, and -SRCC known as an increased risk of developing peritoneal metastasis [68]), would offer opportunity to confirm genes of interest in aggressive GC. The nature of the signal (exogenous or endogenous) that drives AhR activation in diffuse GC has yet to be understood. The role of the surrounding tumor environment in gastric cancer is particularly important in tumor progression and metastasis. Actually, the microenvironment is a limitation factor for any drug penetration. The more we will be able to understand the different mechanisms implicated, the more we will be able to develop new therapeutic solutions. We can hope that in 5 years the classification of gastric cancer will be changed and the clinician could offer a specific microenvironment dedicated drug for the patient.
Acknowledgments
The authors would like to thank JP Brouland and P Castagnet (Department of Pathology, Lariboisiere Hospital, Paris, France), S Durieux (INSERM) for their technical help.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/biomedicines10020240/s1, Table S1: mRNA expression of selected genes in intestinal- and diffuse- GC relative to non-tumoral tissue, Table S2: Correlation of selected genes analysed in the study in relation to immunity and tryptophan metabolism in all GCs. r, Spearman ‘rank test (relation between two parameters), Table S3: Correlation of selected genes analysed in the study in relation to immunity and tryptophan metabolism in intestinal GCs, and Table S4: Correlation of selected genes analysed in the study in relation to immunity and tryptophan metabolism in diffuse GCs.
Author Contributions
Conceptualization: M.P.-A.; Methodology: C.P., S.V., I.B., M.P.-A.; Software: C.P., S.V., M.P.-A., Data curation: M.P., M.P.-A. collected the clinical samples and data from patients; Writing-original draft: M.P.-A., V.B.; Writing-Review and Editing: M.P.-A., V.B.; Funding acquisition: M.P.-A., M.P. All authors have read and agreed to the published version of the manuscript.
Funding
The present study was supported by grants from Institut National de la Santé et de la Recherche Médicale, and Centre National de la Recherche Scientifique.
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are all contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray F. Cancer incidence and mortality worldwide: Sources, methods and mfajor patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Shi J., Qu Y.P., Hou P. Pathogenetic mechanisms in gastric cancer. World J. Gastroenterol. 2014;20:13804–13819. doi: 10.3748/wjg.v20.i38.13804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lauren P. The Two Histological Main Types of Gastric Carcinoma: Diffuse and So-Called Intestinal-Type Carcinoma. An Attempt at a Histo-Clinical Classification. Acta Pathol. Microbiol. Scand. 1965;64:31–49. doi: 10.1111/apm.1965.64.1.31. [DOI] [PubMed] [Google Scholar]
- 4.Uemura N., Okamoto S., Yamamoto S., Matsumura N., Yamaguchi S., Yamakido M., Taniyama K., Sasaki N., Schlemper R.J. Helicobacter pylori infection and the development of gastric cancer. N. Engl. J. Med. 2001;345:784–789. doi: 10.1056/NEJMoa001999. [DOI] [PubMed] [Google Scholar]
- 5.Henson D.E., Dittus C., Younes M., Nguyen H., Albores-Saavedra J. Differential trends in the intestinal and diffuse types of gastric carcinoma in the United States, 1973–2000: Increase in the signet ring cell type. Arch. Pathol. Lab. Med. 2004;128:765–770. doi: 10.5858/2004-128-765-DTITIA. [DOI] [PubMed] [Google Scholar]
- 6.Jezequel J., Bessaguet C., Verveur C., Faycal J., Richert Z., Metges J.P., Volant A., Nousbaum J.B., Robaszkiewicz M. Trends in incidence, management, and survival of gastric and cardia carcinomas in the area of Finistere (France) between 1984 and 2003. Eur. J. Gastroenterol. Hepatol. 2010;22:1412–1419. doi: 10.1097/MEG.0b013e3283408865. [DOI] [PubMed] [Google Scholar]
- 7.Li C., Kim S., Lai J.F., Hyung W.J., Choi W.H., Choi S.H., Noh S.H. Advanced gastric carcinoma with signet ring cell histology. Oncology. 2007;72:64–68. doi: 10.1159/000111096. [DOI] [PubMed] [Google Scholar]
- 8.Taghavi S., Jayarajan S.N., Davey A., Willis A.I. Prognostic significance of signet ring gastric cancer. J. Clin. Oncol. 2012;30:3493–3498. doi: 10.1200/JCO.2012.42.6635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pernot S., Voron T., Perkins G., Lagorce-Pages C., Berger A., Taieb J. Signet-ring cell carcinoma of the stomach: Impact on prognosis and specific therapeutic challenge. World J. Gastroenterol. 2015;21:11428–11438. doi: 10.3748/wjg.v21.i40.11428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Voron T., Messager M., Duhamel A., Lefevre J., Mabrut J.Y., Goere D., Meunier B., Brigand C., Hamy A., Glehen O., et al. Is signet-ring cell carcinoma a specific entity among gastric cancers? Gastric Cancer. 2016;19:1027–1040. doi: 10.1007/s10120-015-0564-2. [DOI] [PubMed] [Google Scholar]
- 11.Guilford P., Hopkins J., Harraway J., McLeod M., McLeod N., Harawira P., Taite H., Scoular R., Miller A., Reeve A.E. E-cadherin germline mutations in familial gastric cancer. Nature. 1998;392:402–405. doi: 10.1038/32918. [DOI] [PubMed] [Google Scholar]
- 12.Humar B., Blair V., Charlton A., More H., Martin I., Guilford P. E-cadherin deficiency initiates gastric signet-ring cell carcinoma in mice and man. Cancer Res. 2009;69:2050–2056. doi: 10.1158/0008-5472.CAN-08-2457. [DOI] [PubMed] [Google Scholar]
- 13.Kakiuchi M., Nishizawa T., Ueda H., Gotoh K., Tanaka A., Hayashi A., Yamamoto S., Tatsuno K., Katoh H., Watanabe Y., et al. Recurrent gain-of-function mutations of RHOA in diffuse-type gastric carcinoma. Nat. Genet. 2014;46:583–587. doi: 10.1038/ng.2984. [DOI] [PubMed] [Google Scholar]
- 14.Perrot-Applanat M., Vacher S., Pimpie C., Chemlali W., Derieux S., Pocard M., Bieche I. Differential gene expression in growth factors, epithelial mesenchymal transition and chemotaxis in the diffuse type compared with the intestinal type of gastric cancer. Oncol. Lett. 2019;18:674–686. doi: 10.3892/ol.2019.10392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Piessen G., Messager M., Leteurtre E., Jean-Pierre T., Mariette C. Signet ring cell histology is an independent predictor of poor prognosis in gastric adenocarcinoma regardless of tumoral clinical presentation. Ann. Surg. 2009;250:878–887. doi: 10.1097/SLA.0b013e3181b21c7b. [DOI] [PubMed] [Google Scholar]
- 16.Messager M., Lefevre J.H., Pichot-Delahaye V., Souadka A., Piessen G., Mariette C., FREGAT Working Group The impact of perioperative chemotherapy on survival in patients with gastric signet ring cell adenocarcinoma: A multicenter comparative study. Ann. Surg. 2011;254:684–693. doi: 10.1097/SLA.0b013e3182352647. discussion 693. [DOI] [PubMed] [Google Scholar]
- 17.Ohta H., Aoyagi K., Fukaya M., Danjoh I., Ohta A., Isohata N., Saeki N., Taniguchi H., Sakamoto H., Shimoda T., et al. Cross talk between hedgehog and epithelial-mesenchymal transition pathways in gastric pit cells and in diffuse-type gastric cancers. Br. J. Cancer. 2009;100:389–398. doi: 10.1038/sj.bjc.6604846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ishimoto T., Miyake K., Nandi T., Yashiro M., Onishi N., Huang K.K., Joyce L.S., Kalpana R., Tay S.T., Suzuki Y., et al. Activation of Transforming Growth Factor Beta 1 Signaling in Gastric Cancer-associated Fibroblasts Increases Their Motility, via Expression of Rhomboid 5 Homolog 2, and Ability to Induce Invasiveness of Gastric Cancer Cells. Gastroenterology. 2017;153:191–204.e16. doi: 10.1053/j.gastro.2017.03.046. [DOI] [PubMed] [Google Scholar]
- 19.Ayers M., Lunceford J., Nebozhyn M., Murphy E., Loboda A., Kaufman D.R., Albright A., Cheng J.D., Kang S.P., Shankaran V., et al. IFN-gamma-related mRNA profile predicts clinical response to PD-1 blockade. J. Clin. Investig. 2017;127:2930–2940. doi: 10.1172/JCI91190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Seliger B. Basis of PD1/PD-L1 Therapies. J. Clin. Med. 2019;8:2168. doi: 10.3390/jcm8122168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kim J.W., Nam K.H., Ahn S.H., Park D.J., Kim H.H., Kim S.H., Chang H., Lee J.O., Kim Y.J., Lee H.S., et al. Prognostic implications of immunosuppressive protein expression in tumors as well as immune cell infiltration within the tumor microenvironment in gastric cancer. Gastric Cancer. 2016;19:42–52. doi: 10.1007/s10120-014-0440-5. [DOI] [PubMed] [Google Scholar]
- 22.Koh J., Ock C.Y., Kim J.W., Nam S.K., Kwak Y., Yun S., Ahn S.H., Park D.J., Kim H.H., Kim W.H., et al. Clinicopathologic implications of immune classification by PD-L1 expression and CD8-positive tumor-infiltrating lymphocytes in stage II and III gastric cancer patients. Oncotarget. 2017;8:26356–26367. doi: 10.18632/oncotarget.15465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Xing X., Guo J., Ding G., Li B., Dong B., Feng Q., Li S., Zhang J., Ying X., Cheng X., et al. Analysis of PD1, PDL1, PDL2 expression and T cells infiltration in 1014 gastric cancer patients. Oncoimmunology. 2018;7:e1356144. doi: 10.1080/2162402X.2017.1356144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim S.T., Cristescu R., Bass A.J., Kim K.M., Odegaard J.I., Kim K., Liu X.Q., Sher X., Jung H., Lee M., et al. Comprehensive molecular characterization of clinical responses to PD-1 inhibition in metastatic gastric cancer. Nat. Med. 2018;24:1449–1458. doi: 10.1038/s41591-018-0101-z. [DOI] [PubMed] [Google Scholar]
- 25.Ricci A.D., Rizzo A., Rojas Llimpe F.L., Di Fabio F., De Biase D., Rihawi K. Novel HER2-Directed Treatments in Advanced Gastric Carcinoma: AnotHER Paradigm Shift? Cancers. 2021;13:1664. doi: 10.3390/cancers13071664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Platten M., von Knebel Doeberitz N., Oezen I., Wick W., Ochs K. Cancer Immunotherapy by Targeting IDO1/TDO and Their Downstream Effectors. Front. Immunol. 2014;5:673. doi: 10.3389/fimmu.2014.00673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Opitz C.A., Litzenburger U.M., Sahm F., Ott M., Tritschler I., Trump S., Schumacher T., Jestaedt L., Schrenk D., Weller M., et al. An endogenous tumour-promoting ligand of the human aryl hydrocarbon receptor. Nature. 2011;478:197–203. doi: 10.1038/nature10491. [DOI] [PubMed] [Google Scholar]
- 28.Mezrich J.D., Fechner J.H., Zhang X., Johnson B.P., Burlingham W.J., Bradfield C.A. An interaction between kynurenine and the aryl hydrocarbon receptor can generate regulatory T cells. J. Immunol. 2010;185:3190–3198. doi: 10.4049/jimmunol.0903670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vacher S., Castagnet P., Chemlali W., Lallemand F., Meseure D., Pocard M., Bieche I., Perrot-Applanat M. High AHR expression in breast tumors correlates with expression of genes from several signaling pathways namely inflammation and endogenous tryptophan metabolism. PLoS ONE. 2018;13:e0190619. doi: 10.1371/journal.pone.0190619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiang Z., Li J., Song S., Wang J., Cai W., Hu W., Ji J., Zhu Z., Zang L., Yan R., et al. A positive feedback between IDO1 metabolite and COL12A1 via MAPK pathway to promote gastric cancer metastasis. J. Exp. Clin. Cancer Res. 2019;38:314. doi: 10.1186/s13046-019-1318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feng S., Cao Z., Wang X. Role of aryl hydrocarbon receptor in cancer. Biochim. Biophys. Acta. 2013;1836:197–210. doi: 10.1016/j.bbcan.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Schlezinger J.J., Liu D., Farago M., Seldin D.C., Belguise K., Sonenshein G.E., Sherr D.H. A role for the aryl hydrocarbon receptor in mammary gland tumorigenesis. Biol. Chem. 2006;387:1175–1187. doi: 10.1515/BC.2006.145. [DOI] [PubMed] [Google Scholar]
- 33.Murray I.A., Patterson A.D., Perdew G.H. Aryl hydrocarbon receptor ligands in cancer: Friend and foe. Nat. Rev. Cancer. 2014;14:801–814. doi: 10.1038/nrc3846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Quintana F.J., Sherr D.H. Aryl hydrocarbon receptor control of adaptive immunity. Pharmacol. Rev. 2013;65:1148–1161. doi: 10.1124/pr.113.007823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fernandez-Salguero P., Pineau T., Hilbert D.M., McPhail T., Lee S.S., Kimura S., Nebert D.W., Rudikoff S., Ward J.M., Gonzalez F.J. Immune system impairment and hepatic fibrosis in mice lacking the dioxin-binding Ah receptor. Science. 1995;268:722–726. doi: 10.1126/science.7732381. [DOI] [PubMed] [Google Scholar]
- 36.Stockinger B., Di Meglio P., Gialitakis M., Duarte J.H. The aryl hydrocarbon receptor: Multitasking in the immune system. Annu. Rev. Immunol. 2014;32:403–432. doi: 10.1146/annurev-immunol-032713-120245. [DOI] [PubMed] [Google Scholar]
- 37.Cella M., Colonna M. Aryl hydrocarbon receptor: Linking environment to immunity. Semin. Immunol. 2015;27:310–314. doi: 10.1016/j.smim.2015.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou L. AHR Function in Lymphocytes: Emerging Concepts. Trends Immunol. 2016;37:17–31. doi: 10.1016/j.it.2015.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mulero-Navarro S., Fernandez-Salguero P.M. New Trends in Aryl Hydrocarbon Receptor Biology. Front. Cell Dev. Biol. 2016;4:45. doi: 10.3389/fcell.2016.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sun J., Xu K., Wu C., Wang Y., Hu Y., Zhu Y., Chen Y., Shi Q., Yu G., Zhang X. PD-L1 expression analysis in gastric carcinoma tissue and blocking of tumor-associated PD-L1 signaling by two functional monoclonal antibodies. Tissue Antigens. 2007;69:19–27. doi: 10.1111/j.1399-0039.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 41.Soliman H., Khalil F., Antonia S. PD-L1 expression is increased in a subset of basal type breast cancer cells. PLoS ONE. 2014;9:e88557. doi: 10.1371/journal.pone.0088557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Masugi Y., Nishihara R., Hamada T., Song M., da Silva A., Kosumi K., Gu M., Shi Y., Li W., Liu L., et al. Tumor PDCD1LG2 (PD-L2) Expression and the Lymphocytic Reaction to Colorectal Cancer. Cancer Immunol. Res. 2017;5:1046–1055. doi: 10.1158/2326-6066.CIR-17-0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang G.Z., Zhang L., Zhao X.C., Gao S.H., Qu L.W., Yu H., Fang W.F., Zhou Y.C., Liang F., Zhang C., et al. The Aryl hydrocarbon receptor mediates tobacco-induced PD-L1 expression and is associated with response to immunotherapy. Nat. Commun. 2019;10:1125. doi: 10.1038/s41467-019-08887-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yearley J.H., Gibson C., Yu N., Moon C., Murphy E., Juco J., Lunceford J., Cheng J., Chow L.Q.M., Seiwert T.Y., et al. PD-L2 Expression in Human Tumors: Relevance to Anti-PD-1 Therapy in Cancer. Clin. Cancer Res. 2017;23:3158–3167. doi: 10.1158/1078-0432.CCR-16-1761. [DOI] [PubMed] [Google Scholar]
- 45.Ma C., Patel K., Singhi A.D., Ren B., Zhu B., Shaikh F., Sun W. Programmed Death-Ligand 1 Expression Is Common in Gastric Cancer Associated with Epstein-Barr Virus or Microsatellite Instability. Am. J. Surg. Pathol. 2016;40:1496–1506. doi: 10.1097/PAS.0000000000000698. [DOI] [PubMed] [Google Scholar]
- 46.Boger C., Behrens H.M., Mathiak M., Kruger S., Kalthoff H., Rocken C. PD-L1 is an independent prognostic predictor in gastric cancer of Western patients. Oncotarget. 2016;7:24269–24283. doi: 10.18632/oncotarget.8169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Haas M., Dimmler A., Hohenberger W., Grabenbauer G.G., Niedobitek G., Distel L.V. Stromal regulatory T-cells are associated with a favourable prognosis in gastric cancer of the cardia. BMC Gastroenterol. 2009;9:65. doi: 10.1186/1471-230X-9-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kim T.S., da Silva E., Coit D.G., Tang L.H. Intratumoral Immune Response to Gastric Cancer Varies by Molecular and Histologic Subtype. Am. J. Surg. Pathol. 2019;43:851–860. doi: 10.1097/PAS.0000000000001253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pernot S., Terme M., Radosevic-Robin N., Castan F., Badoual C., Marcheteau E., Penault-Llorca F., Bouche O., Bennouna J., Francois E., et al. Infiltrating and peripheral immune cell analysis in advanced gastric cancer according to the Lauren classification and its prognostic significance. Gastric Cancer. 2020;23:73–81. doi: 10.1007/s10120-019-00983-3. [DOI] [PubMed] [Google Scholar]
- 50.Andersson P., McGuire J., Rubio C., Gradin K., Whitelaw M.L., Pettersson S., Hanberg A., Poellinger L. A constitutively active dioxin/aryl hydrocarbon receptor induces stomach tumors. Proc. Nat. Acad. Sci. USA. 2002;99:9990–9995. doi: 10.1073/pnas.152706299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Safe S., Lee S.O., Jin U.H. Role of the aryl hydrocarbon receptor in carcinogenesis and potential as a drug target. Toxicol. Sci. 2013;135:1–16. doi: 10.1093/toxsci/kft128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yin X.F., Chen J., Mao W., Wang Y.H., Chen M.H. Downregulation of aryl hydrocarbon receptor expression decreases gastric cancer cell growth and invasion. Oncol. Rep. 2013;30:364–370. doi: 10.3892/or.2013.2410. [DOI] [PubMed] [Google Scholar]
- 53.Peng T.L., Chen J., Mao W., Liu X., Tao Y., Chen L.Z., Chen M.H. Potential therapeutic significance of increased expression of aryl hydrocarbon receptor in human gastric cancer. World J. Gastroenterol. 2009;15:1719–1729. doi: 10.3748/wjg.15.1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nguyen N.T., Hanieh H., Nakahama T., Kishimoto T. The roles of aryl hydrocarbon receptor in immune responses. Int. Immunol. 2013;25:335–343. doi: 10.1093/intimm/dxt011. [DOI] [PubMed] [Google Scholar]
- 55.Julliard W., Fechner J.H., Mezrich J.D. The aryl hydrocarbon receptor meets immunology: Friend or foe? A little of both. Front. Immunol. 2014;5:458. doi: 10.3389/fimmu.2014.00458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zelante T., Iannitti R.G., Fallarino F., Gargaro M., De Luca A., Moretti S., Bartoli A., Romani L. Tryptophan Feeding of the IDO1-AhR Axis in Host-Microbial Symbiosis. Front. Immunol. 2014;5:640. doi: 10.3389/fimmu.2014.00640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mohinta S., Kannan A.K., Gowda K., Amin S.G., Perdew G.H., August A. Differential regulation of Th17 and T regulatory cell differentiation by aryl hydrocarbon receptor dependent xenobiotic response element dependent and independent pathways. Toxicol. Sci. 2015;145:233–243. doi: 10.1093/toxsci/kfv046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Munn D.H., Mellor A.L. IDO in the Tumor Microenvironment: Inflammation, Counter-Regulation, and Tolerance. Trends Immunol. 2016;37:193–207. doi: 10.1016/j.it.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Prendergast G.C., Smith C., Thomas S., Mandik-Nayak L., Laury-Kleintop L., Metz R., Muller A.J. Indoleamine 2,3-dioxygenase pathways of pathogenic inflammation and immune escape in cancer. Cancer Immunol. Immunother. 2014;63:721–735. doi: 10.1007/s00262-014-1549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Domblides C., Lartigue L., Faustin B. Control of the Antitumor Immune Response by Cancer Metabolism. Cells. 2019;8:104. doi: 10.3390/cells8020104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Takikawa O., Kuroiwa T., Yamazaki F., Kido R. Mechanism of interferon-gamma action. Characterization of indoleamine 2,3-dioxygenase in cultured human cells induced by interferon-gamma and evaluation of the enzyme-mediated tryptophan degradation in its anticellular activity. J. Biol. Chem. 1988;263:2041–2048. doi: 10.1016/S0021-9258(19)77982-4. [DOI] [PubMed] [Google Scholar]
- 62.Litzenburger U.M., Opitz C.A., Sahm F., Rauschenbach K.J., Trump S., Winter M., Ott M., Ochs K., Lutz C., Liu X., et al. Constitutive IDO expression in human cancer is sustained by an autocrine signaling loop involving IL-6, STAT3 and the AHR. Oncotarget. 2014;5:1038–1051. doi: 10.18632/oncotarget.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Platten M., Wick W., Van den Eynde B.J. Tryptophan catabolism in cancer: Beyond IDO and tryptophan depletion. Cancer Res. 2012;72:5435–5440. doi: 10.1158/0008-5472.CAN-12-0569. [DOI] [PubMed] [Google Scholar]
- 64.Maruyama T., Kono K., Mizukami Y., Kawaguchi Y., Mimura K., Watanabe M., Izawa S., Fujii H. Distribution of Th17 cells and FoxP3(+) regulatory T cells in tumor-infiltrating lymphocytes, tumor-draining lymph nodes and peripheral blood lymphocytes in patients with gastric cancer. Cancer Sci. 2010;101:1947–1954. doi: 10.1111/j.1349-7006.2010.01624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Li Q., Li Q., Chen J., Liu Y., Zhao X., Tan B., Ai J., Zhang Z., Song J., Shan B. Prevalence of Th17 and Treg cells in gastric cancer patients and its correlation with clinical parameters. Oncol. Rep. 2013;30:1215–1222. doi: 10.3892/or.2013.2570. [DOI] [PubMed] [Google Scholar]
- 66.Puccetti P. On the Non-Redundant Roles of TDO2 and IDO1. Front. Immunol. 2014;5:522. doi: 10.3389/fimmu.2014.00522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.D’Amato N.C., Rogers T.J., Gordon M.A., Greene L.I., Cochrane D.R., Spoelstra N.S., Nemkov T.G., D’Alessandro A., Hansen K.C., Richer J.K. A TDO2-AhR signaling axis facilitates anoikis resistance and metastasis in triple-negative breast cancer. Cancer Res. 2015;75:4651–4664. doi: 10.1158/0008-5472.CAN-15-2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Honore C., Goere D., Messager M., Souadka A., Dumont F., Piessen G., Elias D., Mariette C., FRENCH F.W.G. Risk factors of peritoneal recurrence in eso-gastric signet ring cell adenocarcinoma: Results of a multicentre retrospective study. Eur. J. Surg. Oncol. 2013;39:235–241. doi: 10.1016/j.ejso.2012.12.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are all contained within the article.