Abstract
The intestinal mucosal barrier, also referred to as intestinal barrier, is widely recognized as a critical player in gut homeostasis maintenance as it ensures the complex crosstalk between gut microbes (both commensals and pathogens) and the host immune system. Highly specialized epithelial cells constantly cope with several protective and harmful agents to maintain the multiple physiological functions of the barrier as well as its integrity. However, both genetic defects and environmental factors can break such equilibrium, thus promoting gut dysbiosis, dysregulated immune-inflammatory responses, and even the development of chronic pathological conditions. Here, we review and discuss the molecular and cellular pathways underlying intestinal barrier structural and functional homeostasis, focusing on potential alterations that may undermine this fine balance.
Keywords: intestinal epithelial cells, mucosal barrier, microbiota, inflammatory bowel diseases, diet, mucus layer, aryl hydrocarbon receptor, cell commitment, junctional complexes, Paneth cells
1. Introduction
The intestinal mucosal barrier, also referred to as intestinal barrier, is a selectively permeable structure that grants the absorption of water, electrolytes, and essential dietary nutrients from the intestinal lumen into the circulation [1,2]. Apart from this role, the intestinal barrier mediates the crosstalk between commensal gut microbes and the host immunity and constitutes a first line of defence against intraluminal pathogenic antigens and potentially harmful microorganisms [1,2]. The intestinal barrier is composed of several elements that aid in its function as a physical and immunological defence boundary. These mainly include: (i) the outer mucus layer, encompassing the commensal gut microbiota, antimicrobial proteins (AMPs), and secretory immunoglobulin A (SIgA) molecules; (ii) the central single layer of specialized epithelial cells, derived from a pool of pluripotent stem cells at the base of the crypts that can be ultimately committed to goblet cells (which secrete mucins), Paneth cells (which synthesize antimicrobial peptides such as lysozyme and defensins), enteroendocrine cells (producing enteric hormones), enterocytes (absorbing water and nutrients), and Microfold cells, also referred to as M cells, (which are specialized for antigen sampling), following the up- or down-regulation of specific transcription factors; (iii) the inner lamina propria where cells from both innate (e.g., natural killer, neutrophils) and adaptive (e.g., T cells, B cells) immunity reside (Figure 1).
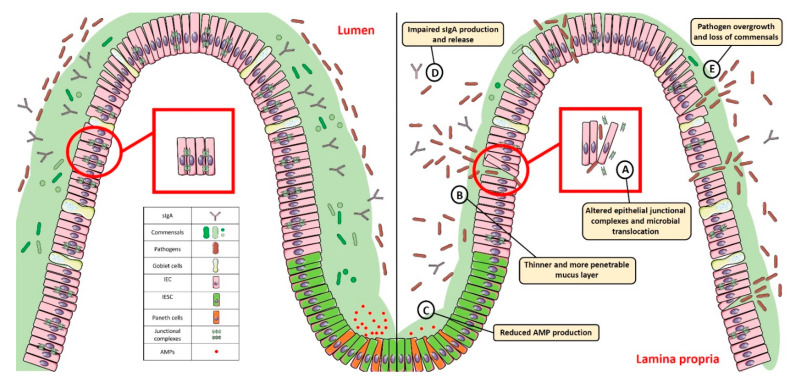
Figure 1.
Gut homeostasis is established and maintained by the intestinal mucosal barrier. Alterations in its integrity and function, characterized by: (A) dysregulated junctional complexes, (B) thinner mucus layer, (C,D) reduced AMP and IgA production, and (E) pathogen overgrowth and penetration across the epithelial barrier, may perturb this fine balance and lead to gut dysbiosis. SIgA: Secretory Immunoglobulin A; AMP: antimicrobial peptide; IEC: intestinal epithelial cell; IESC: intestinal epithelial stem cell.
The ability to regulate the physiological processes occurring in the gut to keep internal states steady and balanced, also referred to as intestinal homeostasis, depends on complex interactions between the microbiota, the intestinal epithelium, and the host immune system. In particular, intestinal epithelial cells (IECs) act as frontline sensors for microbial encounters, and their hyporesponsiveness is ensured by the host innate immune system that can discriminate between signals derived from either commensal bacteria or pathogens [3,4,5]. Increasing evidence in germ-free mice highlighted the importance of commensal microbiome in maintaining gut homeostasis by providing protective, structural, and metabolic effects on the host mucosal surfaces [6,7]. For instance, commensals can release anti-microbial peptides, synthetize vitamins, contribute to ion adsorption and fermentation of non-digestible dietary residues, control epithelial cell differentiation, induce IgA secretion, and favour the immune system development [8,9]. Maintenance of such intestinal homeostasis also requires the structural integrity of the intestinal epithelium, which is ensured by junctional protein complexes (i.e., tight junctions, adherens junctions and desmosomes) that finely regulate intestinal permeability and seal adjacent epithelial cells [10] (Figure 1).
Dysfunction of the barrier physical integrity and/or an impaired function of the highly specialized cells composing the epithelial layer may lead to pathogen invasion and mucosal dysbiosis, resulting in a disruption of gut homeostasis that may ultimately trigger pathologic conditions, such as inflammatory bowel diseases (IBD), celiac disease, Clostridioides difficile infection (CDI), irritable bowel syndrome, colorectal cancer, type 1 diabetes, and obesity (Table 1) [11,12,13,14].
Table 1.
Intestinal barrier alterations and related pathological conditions.
| Disease | Observation | Ref. |
|---|---|---|
| IBD |
|
[15,16,17,18,19] |
| Celiac disease |
|
[20,21,22,23,24] |
| CDI |
|
[25,26,27] |
| IBS |
|
[28,29,30,31,32,33,34] |
| CRC |
|
[35,36,37,38,39,40] |
| Obesity |
|
[41,42,43,44] |
| Type 1 diabetes |
|
[44,45,46,47,48,49,50] |
Abbreviations: IBD: Inflammatory Bowel Diseases; MyD88: Myeloid differentiation primary response 88; CXCR3: C-X-C Motif Chemokine Receptor 3; CDI: Clostridioides difficile infection; IBS: Irritable Bowel Syndrome; CRC: Colorectal cancer.
Here, we review and discuss the available experimental evidence about defects in epithelial barrier integrity and function and how they can compromise gut homeostasis, thus favouring microbial dysbiosis and disease development.
2. Breaking the Balance: Intestinal Barrier Dysfunction and Gut Dysbiosis
Both genetic defects and specific environmental factors are known to contribute to break the intestinal barrier balance and promote gut dysbiosis. In particular, impaired expression of genes related to cell commitment, junctional complexes, mucus production and secretion, Paneth cell activity, pathogen sensing, reactive oxygen species (ROS) production, xenobiotic response, and IgA secretion dramatically compromise intestinal epithelial barrier integrity and protective function (Table 2). Similarly, environmental factors—including bacterial infections; medication exposure (e.g., antibiotics) subsequent to pathogen infections or other diseases; and increased intake of high-fat compounds, sugars, and ethanol at the expense of fruits and vegetables—were reported to affect host microbiota composition and metabolic activities, leading to loss of commensals and overgrowth of pathogens (Table 3).
Table 2.
Genetic defects affecting intestinal barrier homeostasis.
| Category | Gene | Effects on Intestinal Barrier | Ref. |
|---|---|---|---|
| Cell commitment | Hes1 | Reduced production of AMPs and mucus, gut dysbiosis, and inflammation. Precocious differentiation of Paneth cells. Impaired specification of IECs into enterocytes. | [51,52,53] |
| Math1 | Decreased frequency of goblet cells. | [54] | |
| Stk11 | Impaired released of AMPs and IL-18. Colitogenic bacteria overgrowth. | [55] | |
| Cdx2 | Altered mucus production and increased intestinal permeability and susceptibility to DSS-induced colitis. | [15,56] | |
| Gata6 | Impaired stem cell proliferation, reduction in villus length, Paneth cell, and enterocyte and enteroendocrine cell frequency. Increased number of goblet-like cells. Decreased levels of ZO-1 and increased intestinal permeability and susceptibility to experimental colitis and ileitis. Gut dysbiosis. | [57,58,59] | |
| Sox9 | Lack of differentiated Paneth cells, crypt enlargement, gut dysbiosis. | [60,61] | |
| Junctional Complexes | Jam-A/F11R | Increased intestinal permeability, low-grade intestinal inflammation, and increased susceptibility to DSS-induced colitis. | [62] |
| Cldn-2 and Cldn-15 double-KO | Impaired paracellular Na+ flow and malnutrition. | [63] | |
| Tjp1 | Apical surface brush border membrane and crevasses at intercellular junctions between enterocytes. Increased susceptibility to experimental colitis, delayed cell division, and mucosal healing. | [64,65] | |
| P tpn2 | Increased claudin-2 expression, intestinal permeability, and inflammatory cytokine production. | [66] | |
| Mucus layer | Muc2 | ER stress and decreased frequency of goblet cells, altered mucus production, increased intestinal permeability, gut dysbiosis, and chronic intestinal inflammation. | [16,67,68] |
| Gfi1 | Accumulation of secretory progenitors, decrease in mucus and AMPs release. | [69] | |
| Foxo1 | Impaired mucus layer formation, overgrowth of mucin-degrading bacteria, and decrease of short-chain fatty acid-producing microbial species. Enhanced susceptibility to infection and inflammation. | [70] | |
| Paneth cells | Nod2 | Impaired α-defensins secretion. | [71,72] |
| Atg16l1 | Impaired autophagy in response to viral infection and decreased AMPs release. | [73,74] | |
| Xbp1 | Chronic ER stress in response to viral infection and decreased AMP release. | [75] | |
| Tcf4 | Reduced α-defensins secretion and CD development. | [76,77] | |
| PRRs | MyD88 | Increased stem cell proliferation. | [78] |
| Nod2 | Impaired pathogen sensing and clearance, and gut dysbiosis. No protection against oxidative stress-mediated cell death, and impaired epithelial regeneration. | [79,80,81,82,83] | |
| Oxidative Burst | Duox2 | Enhanced pathogen translocation to host lymphatic tissues. | [84] |
| Cyba | Decreased DUOX2 activity in response to Citrobacter rodentium. | [85] | |
| Xenobiotic Receptors | Pxr-Nr1I2 | Dysregulated TLR4-NF-κB signalling pathway, reduced ZO-1 and E-cadherin expression, increase in Claudin-2 levels. Higher susceptibility to IBD development. | [86,87,88] |
| AhR | Increased susceptibility to intestinal infection (Citrobacter rodentium), reduced mucus production, impaired tight junctions, and crypt hyperplasia. | [89,90,91] | |
| Secretory IgA | IgA | Gut dysbiosis. | [92] |
| pIgR | Impaired SIgA transcytosis across epithelial cells and gut dysbiosis. | [93,94] |
Abbreviations: Hes1: Hairy and enhancer of split 1; Math1: Mouse atonal homolog 1; Stk11: Serine threonine kinase 11; IL-18: Interleukin-18; Cdx2: Caudal type homeobox 2; DSS: Dextran Sodium Sulfate; Gata6: GATA binding factor 6; ZO1: Zonula Occludens-1; Sox9: SRY-Box Transcription Factor 9; Jam-A/F11R: Junctional adhesion molecules/F11 receptor; Cldn: claudin; Tjp1: Tight junction protein-1; Ptpn2: Protein tyrosine phosphatase non-receptor type 2; Muc2 Mucin-2; ER: Endoplasmic Reticulum; Gfi1: Growth factor independent 1; Foxo1: Forkhead box protein O1; Nod2: Nucleotide Binding Oligomerization Domain Containing 2; Atg16l1: Autophagy Related 16 Like 1; Xbp1: X-Box Binding Protein 1; Tcf4: transcription factor 4; CD: Crohn’s disease; MyD88: Myeloid differentiation primary response 88; Duox2: Dual oxidase 2; Cyba: Cytochrome B-245 Alpha Chain; Pxr/Nr1I2: Pregnane X receptor/Nuclear receptor subfamily 1 group I member 2; TLR4: Toll-like receptor-4; NF-kB: nuclear factor kappa-light-chain-enhancer of activated B cells; AhR: Aryl Hydrocarbon Receptor; IgA: Immunoglobulin A; pIgR: poly immunoglobulin receptor; AMP: Antimicrobial peptides; ZO-1: Zonula Occludens-1; ER: Endoplasmic reticulum; SIgA: Secretory immunoglobulin A.
Table 3.
Environmental factors affecting intestinal barrier homeostasis.
| Category | Diet | Effects on Intestinal Barrier | Ref. |
| Junctional Complexes | Gluten | Alterations in adherent junctions and desmosomes and increased intestinal permeability and susceptibility to experimental colitis. Disassembly of ZO-1 from the tight junctional complex. | [20,95] |
| Glucose/Fructose | TJ and AJ proteins dysfunction, increased susceptibility to pathogen infection, gut dysbiosis, metabolic syndrome, oxidative stress, and chronic inflammation | [44,96] | |
| High-fat diet | ER stress in IECs, impairment of Claudin-1 expression and mucus barrier, and increased endotoxin serum levels. Increased taurocholic bile acid production and gut dysbiosis. | [97,98] | |
| Ethanol | Altered ZO-1 and occludin localization and impaired paracellular permeability. | [99,100] | |
| Mucus Layer | Fiber-deprived diet | Thinner mucus layer, gut dysbiosis, and chronic intestinal inflammation. | [67,101] |
| Paneth cells | Vitamin D deficiency and exposure to high-fat diet | Impaired expression of α-defensins, MMP7, and tight junction-related proteins; increased intestinal permeability; gut dysbiosis; and metabolic syndrome. Indiction of ER stress and secretion of misfolded α-defensins. | [102,103] |
| High fat diet | Decreased AMP expression, ER stress and autophagy induction, and gut dysbiosis. | [104] | |
| Western diet (deoxycholic acid) | Excessive activation of the farnesoid X receptor and type I interferon signalling pathways. | [105] | |
| Xenobiotic receptors | AhR ligand-free diet | Higher susceptibility to experimental colitis and gut dysbiosis. | [106,107] |
| Category | Bacterial infection | Effects on intestinal barrier | Ref. |
| Junctional Complexes | Infection by Salmonella typhimurium | Increased claudin-2 expression and bacterial invasion. | [108] |
| Infection by Vibrio cholerae | Zonula occludes toxin production and altered paracellular permeability. | [109,110] | |
| PRRs | LPS | Increased intestinal permeability. | [111] |
| Category | Medication exposure | Effects on intestinal barrier | Ref. |
| Junctional Complexes | Antibiotic treatment | Decreased production of microbial-derived short-chain fatty acids. Gut dysbiosis. Reduced ZO-1, occludin, and claudin-1 expression, and increased intestinal permeability. Altered microvilli morphology and reduced rate of intestinal epithelial cell turnover. | [112,113] |
Abbreviations: ZO-1: Zonula Occludens-1; TJ: Tight junction; AJ: Adherent junction; ER: Endoplasmic Reticulum; IECs: Intestinal Epithelial Cells; MMP: Matrix Metallopeptidase; AMP: Antimicrobial peptide; AhR: aryl hydrocarbon receptor; PRR: Pattern recognition receptors; LPS: lipopolysaccharide; IECs: intestinal epithelial cells.
Such defects and factors, summarized in Table 2 and Table 3 respectively, are discussed below.
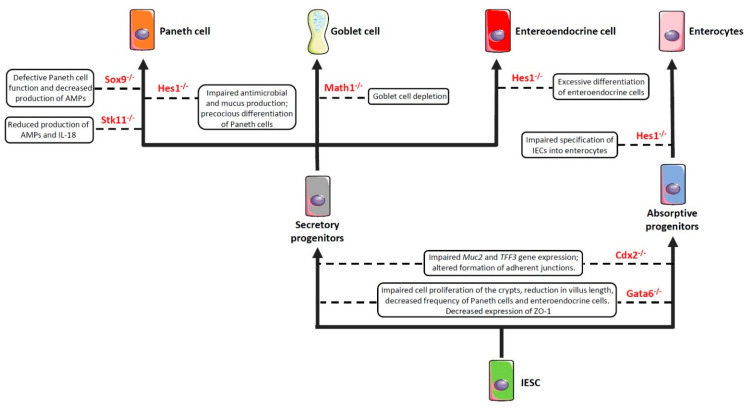
2.1. Impairment of Cell Commitment
As previously anticipated, the intestinal barrier is characterized by a self-renewing epithelium, organized in crypts and villi, including both stem cells and differentiated cells. As the epithelial barrier has to deal with multiple physiologic activities, it requires different specialized cells, some of which are able to produce and secrete several molecules—such as antimicrobial peptides, mucins and hormones—and others that are able to adsorb water and nutrients. To achieve this goal, stem cells, after multiple transit-amplifying (TA) divisions, terminally differentiate into either secretory or absorptive lineages depending on the tightly regulated expression/inhibition of specific transcription factors [114,115]. For instance, the cell surface receptor Notch drives the cell commitment process by binding to the Notch ligands Deltalike (Dll) and Jagged families [116]. A cell expressing the Notch ligands will differentiate into a secretory cell (e.g., goblet cell, Paneth cell) upon expression of the Atonal BHLH Transcription Factor 1 (Atoh1), whereas a neighbour cell expressing the activated Notch receptor will induce the expression of the target gene hairy and enhancer of split 1 (Hes1)—a Atoh1 inhibitor—and will differentiate into an absorptive cell (e.g., enterocyte) [54]. Obviously, a dysregulated expression of the above-mentioned proteins definitely compromises the intestinal epithelial cell commitment and, in turn, the intestinal barrier integrity and function, as demonstrated by the association of several polymorphisms in genes encoding commitment-related transcription factors with intestinal barrier dysfunctions and intestinal inflammatory diseases (Figure 2) [51,52,53,54,55]. In this context, by employing genetically engineered mouse models, Guo and colleagues demonstrated that deficiency of the Hes1 gene in IECs negatively affected antimicrobial peptides and mucus production, thus resulting in gut dysbiosis and inflammation [51]. Along the same line was the demonstration that mice deficient for Math1 (also referred to as Atoh1) displayed complete abrogation of goblet cells in the intestine [54]. Similar results were observed in mice with conditional deletion of the serine threonine kinase 11 (Stk11) gene, involved in the differentiation of stem cells into the secretory lineage cell types (e.g., goblet cells and Paneth cells), in IECs [55]. These animals displayed increased susceptibility to gut inflammation in association with reduced production of antimicrobial peptides and IL-18, as well as an uncontrolled expansion of colitogenic bacteria [55].
Figure 2.
Impaired expression of genes encoding commitment-related transcription factors compromises epithelial cell differentiation and intestinal barrier function. Boxes enclose the effect/s of the knockdown of the genes depicted in red on the indicated cell commitment. Abbreviations: Sox9: SRY-Box Transcription Factor 9; Hes1: Hairy and enhancer of split 1; Stk11: Serine threonine kinase 11; Math1: Mouse atonal homolog 1; Cdx2: Caudal type homeobox 2; Gata6: GATA binding factor 6; Muc2: Mucin 2; TFF3: Trefoil factor 3; ZO-1: Zonula Occludens-1; AMPs: Antimicrobial peptides; IESC: Intestinal epithelial stem cells.
Another important transcription factor involved in the commitment of IECs is the caudal type homeobox 2 (Cdx2) gene [117]. Indeed, CDX2 is a positive regulator of the Muc2 and Trefoil Factor 3 (TFF3) genes [56,118] involved in the production and stabilization of the mucus layer, respectively, and whose deficiency induces hypersensitivity to chemically-induced colitis (such as that induced by dextran sulfate sodium (DSS)) [15,56]. In addition, CDX2 controls cell-cell interactions and the expression of cadherins, which are important in the formation of the adherens junctions [119,120,121]. In support of this view is the evidence that mice bearing one non-functional Cdx2 allele (Cdx2+/− mice) displayed increased intestinal permeability and were more susceptible to the abrasive effect of DSS [117].
The GATA binding factor 6 (GATA6) is a zinc finger transcription factor that regulates cell proliferation, differentiation, and gene expression in several tissues [122]. For instance, GATA6 is involved in cell proliferation and differentiation along the gastrointestinal tract [57,58]. In particular, conditional deletion of Gata6 in IECs resulted in impaired cell proliferation of the crypts, reduction in villus length, decreased frequency of Paneth cells and enteroendocrine cells, increased number of goblet-like cells, and dysregulated expression of enterocyte-related genes in the ileum [57]. Similar alterations were observed in the colon, where Gata6 deficiency affected stem cell proliferation and differentiation into Paneth cells, enteroendocrine cells, and enterocytes [58]. Our study has recently demonstrated that conditional deletion of Gata6 in the gut epithelium significantly affected intestinal barrier integrity, leading to decreased expression of the tight junction-related protein zonula occludens-1 (ZO-1), and resulting in increased paracellular permeability, microbial dysbiosis, and susceptibility to gut inflammation [59]. Interestingly, we also reported a decreased expression of GATA6 in the intestinal epithelium of IBD patients, thus suggesting that a reduced expression of this transcription factor may contribute to intestinal barrier dysfunction in these subjects [59]. In the intestinal epithelium, defects in Paneth cell function—and the consequent decrease in the antimicrobial peptide production—may also result from the deletion of Sox9 [60]. Indeed, by generating mice that harbored a conditional Sox9 gene and a Villin-Cre transgene, Mori-Akiyama et al. reported that lack of Sox9 expression in the intestinal epithelium of Sox9fl/fl Villin-Cre+ mice resulted in the complete absence of differentiated Paneth cells, although the differentiation of other intestinal epithelial cell subsets (e.g., goblet cells, enterocytes) was not affected. Moreover, Sox9 deficiency also lead to crypt enlargement, a marked increase in cell proliferation throughout the crypts, as well as a replacement of the Paneth cells by proliferating epithelial cells [60]. More recently, by employing the same conditional mouse model, Riba and colleagues showed that Sox9 deletion in the intestinal epithelium reduced lysozyme production. This effect resulted in significant microbial dysbiosis, characterized by E. coli overgrowth and ultimately leading to visceral hypersensitivity [61].
2.2. Impairment of Epithelial Junctional Complexes
The intestinal epithelial barrier’s main function is to protect the host from luminal antigens, pathogens, and toxins, while allowing selective permeability to water, nutrients, and electrolytes. In particular, transcellular permeability, involved in solute transport through the epithelial cells, is mediated by selective transporters for amino acids, electrolytes, short chain fatty acids, and sugars [123]. Paracellular permeability, instead, occurs through intercellular junctional complexes encompassing adherens junctions (AJs), tight junctions (TJs), and desmosomes [124,125]. These transmembrane proteins, localized both at the apical-lateral membrane junction and along the lateral membrane, mediate the contact between adjacent IECs, thus sealing the intracellular spaces. The AJs (e.g., catenins, cadherins) and desmosomes (e.g., desmoglein, desmocollins) regulate the mechanical linkage of adjacent cells, while the TJs (e.g., ZO-1, claudin-2, occludins, Junctional Adhesion Molecule) form an apical junctional complex that seals the intercellular space and modulates selective paracellular permeability [124,125,126,127,128].
Alterations in the formation/distribution of the intercellular junctional complexes, which may occur in men with specific genetic susceptibilities, as well as in response to dietary factors and bacterial infections, may result in intestinal epithelial barrier breakdown and translocation of the luminal content into the lamina propria, leading to gut dysbiosis, uncontrolled immune/inflammatory responses, and, ultimately, pathological conditions [10].
For instance, gliadin (a glycoprotein representing the major component of wheat gluten) has been reported to deeply affect the expression and distribution of several junctional complexes in the small intestine of celiac patients by binding to CXC motif receptor 3 (CXCR3) on epithelial cells [20]. This interaction induces the release of zonulin, a human protein analogue of the Zonula occludens toxin (ZOT) from Vibrio cholerae, through the recruitment of Myeloid differentiation primary response (MyD)-88 [20,21,129,130]. Increased levels of zonulin were detected in the intestinal tissues taken from celiac disease patients during the acute phase compared to those taken from healthy controls. Once released, Zonulin leads to transactivation of EGF receptor (EGFR) via proteinase-activated receptor 2 (PAR2) activation in the intestinal epithelium and subsequent tight junction disassembly [20,21,129,130].
The impairment of the epithelial junctional complexes importantly contributes to the development of other chronic inflammatory conditions, such as IBD. For example, increased expression of claudin-2, as well as impaired expression and redistribution of claudin-5, -8 and occludin were reported in Crohn’s disease patients, leading to increased intestinal permeability and bacterial translocation [131]. A similar severe condition was described also in the colonic mucosa of patients with ulcerative colitis, in association with the dysregulated expression of occludin, ZO-1, claudin-1, JAM, beta-catenin, E-cadherin, and the consequent transepithelial migration of neutrophils [132].
The above-mentioned chronic inflammatory conditions importantly contribute to the development and progress of colorectal carcinogenesis. Interestingly, increased expression of claudin-1 and claudin-2 was found to correlate with inflammatory activity, IBD-associated dysplasia, and sporadic adenomas [36]. Similarly, Dhawan et al. observed that claudin-1 expression was increased in colon carcinomas and metastatic lesions and played a key role for tumorigenesis and invasiveness of colonic epithelial cells [35]. Claudin-2 was also reported to be increased in tissues taken from CRC and IBD-associated CRC patients and to promote and sustain cell proliferation and tumor growth in cultured cells and experimental models [133].
Dysfunctions of the epithelial junctional complexes and the consequent increase of intestinal permeability and gut dysbiosis correlate with the development and progression of other pathological conditions. In particular, increased intestinal permeability was seen to precede and/or to be an early biomarker of diabetes development in patients, as well as in experimental models of the disease [45,134,135]. Moreover, increased serum levels of zonulin, in association with altered intestinal permeability, were described in a subgroup of patients with type 1 diabetes and their first-degree relatives, suggesting this molecule as a valid early biomarker of disease development [49].
Animal models employing genetically engineered mice have helped to better understand the link between junctional complex dysregulation and the development of dysbiosis and pathologic conditions. In this context, Laukoetter et al. reported a role for Junctional Adhesion Molecule (JAM)-A, a TJ component contributing to the control of barrier function and leukocyte migration, in regulating intestinal permeability and inflammation in vivo [62]. Indeed, despite showing normal epithelial architecture, JAM-A knockout mice developed low-grade colonic inflammation (characterized by enhanced polymorphonuclear leukocyte infiltration and large lymphoid aggregates not seen in sham mice) [62]. Barrier function experiments revealed increased mucosal permeability, as indicated by enhanced dextran flux, and decreased transepithelial electrical resistance in JAM-A knockout mice compared to wild-type control mice [62]. Consistently, JAM-A deficiency increased the permeability of in vitro monolayers derived from the human colonic epithelial cell line SK-CO15 compared with control. Moreover, JAM-A deficient mice were more susceptible to the DSS-driven experimental colitis compared to controls, although the colonic mucosa showed less injury and increased epithelial proliferation [62]. Analyses of other TJ-related proteins showed increased expression of claudin-10 and -15, both of which tune TJ barrier function by the formation of ion-selective pores, following JAM-A knockdown in the colonic mucosa of mice and in SK-CO15 cell monolayers [62].
In a later article, Wada and colleagues reported that mice with the double knockdown of claudin-2 (Cldn-2) and claudin-15 (Cldn-15) genes had impaired paracellular Na+ flow and subsequent malnutrition, leading to infant death [63].
By employing cultured epithelial cells and an intestinal epithelial-specific knockout mouse (that is, Tjp1fl/fl Villin-Cre+ mouse), Odenwald and co-workers showed that the TJ scaffolding protein ZO-1 was essential for development of unified apical surfaces in vitro and in vivo. In detail, conditional deletion of ZO-1 in IECs of Tjp1fl/fl Villin-Cre+ mice did not significantly alter crypt-villus architecture, whereas it affected apical tissue continuity, which is by characterized apical surface brush border membrane, and the presence of crevasses at intercellular junctions between enterocytes, likely by modulating actomyosin contraction and membrane traffic [64]. Recently, Kuo and colleagues reported decreased ZO-1 expression, both at RNA and protein level, in intestinal mucosal biopsies isolated from IBD patients as compared with those isolated from healthy controls [65]. Loss of ZO-1 expression in epithelial cells in Tjp1fl/fl Villin-Cre+ mice did not promote spontaneous disease, but it exacerbated tissue damage and weight loss during experimental colitis, as well as delayed the mucosal healing [65]. The authors also reported that ZO-1 is critically involved in the cell division phase upon damage. In particular, by associating with the centriole and mitotic spindle, ZO-1 contributed to both Wnt–β-catenin signaling and mitotic spindle orientation, suggesting that ZO-1 may actively contribute to the intestinal epithelial barrier restoration [65]. In line with these observations, we recently found that loss of Gata6 expression in IECs of genetically engineered mice resulted in increased intestinal permeability, gut dysbiosis, and microbial-driven intestinal inflammation. These effects were associated with decreased ZO-1 expression and epithelial damage both in the ileum and colon. Experiments in cultured cells suggested that ZO-1 expression could be directly modulated by GATA6 [59]. Recently, Marchelletta and colleagues reported that the impaired function of T cell protein tyrosine phosphatase (TCPTP), encoded by the protein tyrosine phosphatase non-receptor type 2 (PTPN2) gene, contributed to the epithelial tight junction protein remodeling and increased intestinal permeability [66]. In particular, Tcptp-deficient mice showed increased claudin-2 expression, intestinal permeability, and inflammatory cytokine production [66]. In detail, TCPTP was able to maintain the localization of ZO-1 and occludin at apical tight junctions, as well as to modulate the turn-over of claudin-2, a cation pore-forming transmembrane protein, by upregulating the serine metalloproteinase matriptase, which promoted claudin-2 proteosomal degradation [66].
Apart from defects in the above-mentioned epithelial junction-related molecules, several dietary factors may contribute to increase intestinal permeability and trigger/amplify pathologic conditions [136]. A good example in this regard is given by gluten, which, in addition to its well-known detrimental effects on barrier integrity and TJ protein activity in celiac disease, can actively promote dysregulation of intestinal barrier function in non-celiac patients. Of note, mice exposed to a gluten-rich diet showed alterations in adherent junctions and desmosomes, resulting in increased intestinal permeability and susceptibility to DSS-driven experimental colitis [95].
Glucose and fructose are additional macronutrients found to trigger TJ and AJ protein dysfunction, thus promoting changes in microbiota composition, increased susceptibility to pathogen infection, as well as metabolic syndrome [44]. In mouse experimental models, uncontrolled metabolism of fructose in the liver and in the small intestine, due to the excessive delivery of this sugar (15% in water for 3 weeks), induced the transcriptional expression of fructokinase (a protein involved in fructose metabolism), TJ alterations, energy depletion, oxidative stress, and chronic inflammation [96]. On the other hand, mice deficient of the fructokinase isoforms A and C (KHK-A, KHK-C) were protected from such detrimental effects. Notably, loss of KHK-A function only did not prevent alterations in TJs, thus suggesting that intestinal barrier impairment was mainly mediated by KHK-C activity [96].
Detrimental effects of dietary fats on the epithelial junctional complexes have been also reported by several studies. In particular, mice exposed to a high-fat diet for 3, 11, and 22 weeks showed induction of endoplasmic reticulum (ER) stress in IECs, as well as an impairment of Claudin-1 expression and mucus barrier, with the consequent increase of endotoxin serum levels and gut dysbiosis [97]. Similarly, Devkota and colleagues demonstrated that the increased availability of taurocholic bile acid, due to the consumption of a diet high in saturated (milk derived)-fat, promoted the expansion of the low abundance pathobiont Bilophila wadsworthia (a member of the Deltaproteobacteria), which, in turn, was able to impair intestinal barrier integrity in genetically susceptible Il-10−/− mice due to its sulphite-reducing activity [98]. Another dietary habit found to affect TJ activity is ethanol consumption. Exposure to non-cytotoxic doses of ethanol (as those detected in the blood of moderate drinkers) impaired paracellular permeability in vitro due to alterations in ZO-1 and occludin localization [99,100].
Both localization and activity of epithelial junctional complexes can also be affected by pathogen invasion and toxin secretion. For instance, Salmonella typhimurium was found to up-regulate the colonic expression of the leaky protein claudin-2, which plays an opposite role in the modulation of intestinal permeability compared to other TJ proteins involved in barrier maintenance, thus facilitating bacterial invasion [108]. Vibrio cholerae, instead, was reported to target the intestinal epithelial barrier by producing the zonula occludens toxin (ZOT), which transiently affects the paracellular permeability in the small intestine by opening TJs through a protein kinase C-dependent actin reorganization [109,110].
On its side, antibiotic treatment dramatically influences intestinal permeability by compromising host microbial ecology. In particular, mice exposed to antibiotics for 2 weeks developed mucosal dysbiosis characterized by decreased production of short-chain fatty acids, such as butyrate (known to sustain barrier function and integrity), by commensals [112]. Moreover, antibiotic treatment hampered intestinal TJ function and increased intestinal permeability by reducing the expression of ZO-1, occluding, and claudin-1 [112]. Similar results were obtained in antibiotic-treated germ-free mice, which presented altered microvilli morphology and reduced rate of intestinal epithelial cell turnover compared to sham mice [113]. Altogether, these results indicate a key role for commensal microbiota in preserving epithelial junctional complexes and gut barrier integrity, highlighting a possible detrimental effect of antibiotic exposure on such a fine balance.
2.3. Thinning/Depletion of the Mucus Layer
Goblet cells are specialized IECs able to synthetize and secrete mucin proteins into the lumen. Mucin proteins are pivotal in creating a protective mucus layer acting against pathogens, chemicals, and mechanical stress in order to maintain gut homeostasis and protect the inner mucosal surface [137]. The mucus layer, mainly composed of water, electrolytes, lipids, and glycosylated mucins [138], represents an important source of antimicrobial peptides and immunoglobulins and can directly interact with commensals, providing nutrients and attachment sites depending on the mucin glycosylation profile [139].
Mucolytic bacteria (e.g., Akkermansia muciniphila, Bacteroides thetaiotaomicron, Ruminococcus gnavus, Ruminococcus torques) represent an important class of commensals as they are able to digest glycans (from dietary fibers) and mucins through glycosidase enzymes, and to produce, in turn, short chain fatty acids (such as acetate and butyrate) acting as energy source for colonocytes and contributing to protect the intestinal barrier integrity [139]. However, the fine balance between goblet cell-mediated replenishment of mucus and its degradation by commensals can be affected by a fiber-deprived diet, as indicated by the fact that mice subjected to intermittent dietary fiber deprivation presented a thinner mucus layer due to O-linked glycan digestion by the fiber-deprived microbiota [101]. Thus, enrichment in mucus-degrading bacteria may impair the mucus layer thickness and viscosity and promote enteric pathogens adherence and penetration, ultimately causing gut dysbiosis and chronic intestinal inflammation [67,101]. These pathological alterations were observed in the Winnie murine model of spontaneous colitis, characterized by a missense mutation in the Muc2 gene [16,67]. The phenotype of Winnie mice was characterized by altered mucus production as early as 4 weeks of age, with ensuing intestinal barrier dysfunction, gut dysbiosis, and inflammation [16,67]. In particular, impaired Muc2 expression affected the number of goblet cells, which underwent unresolved ER stress and accumulation of mucin precursors [16,67]. All these processes were associated with apoptotic cell death, increased intestinal permeability, pathogen penetration into the inner mucus layer, and adherence to epithelial cells, as well as bacterial translocation into the lamina propria [16,67]. The subsequent uncontrolled immune response towards pathogens (e.g., enhanced dendritic cell activation, T-helper cytokine production) promoted chronic intestinal inflammation and gut dysbiosis, characterized by the outgrowth of Bacteroidetes and Verrucomicrobia (such as Akkermansia muciniphila) [67,68].
Impaired mucus layer integrity can also depend on mutations in the Gfi1 gene. Gfi1 functions downstream of Math1 in the intestinal epithelium and encodes molecules involved in the stem cell differentiation into the different secretory cell lineages [69]. In particular, Gfi1-deficient mice displayed alterations in terminal differentiation and morphology of goblet cells and Paneth cells, together with accumulation of immature secretory progenitors, as well as a decrease in mucin and antimicrobial peptide release [69]. Recently, the Foxo1 trascription factor was described to be critically involved in mucin granule release through autophagy [70]. In particular, Foxo1fl/fl Villin-Cre+ mice showed impaired mucus layer formation and subsequent dysbiosis, resulting in disrupted intestinal barrier integrity and enhanced susceptibility to infection and tissue inflammation. Moreover, Foxo1 deficiency in IECs resulted in the overgrowth of mucin-degrading bacteria and a decrease of short-chain fatty acid-producing microbial species, which further affected the intestinal barrier function [70].
In addition to mucus production and degradation, gut microbiota composition is able to influence the mucus properties. In this regard, Jakobsson and colleagues reported that the mucus layer of germ-free mice was characterized by a higher mucus penetrability as compared to conventional mice [111]. Moreover, mice with identical genetic background, but hosted in two rooms of the same specific pathogen-free animal facility, showed different mucus properties, evidenced by the fact that one colony had an impenetrable inner mucus layer, whereas the other showed opposite features [111]. The authors suggested that these differences relied on changes in the gut microbiota composition as the different mucus phenotypes were acquired by germ-free mice upon faecal microbiota transplantation [111]. In particular, mice with an impenetrable inner mucus layer showed increased frequency of the Erysipelotrichi class, whereas Proteobacteria and TM7 expanded in mice with more penetrable mucus [111]. Hence, even genetically identical animals housed in the same facility may have distinct microbiotas and barrier structures [111].
Taken together, these results highlight the mutualistic effects between the gut microbial community and the mucus layer and their consequences on intestinal barrier integrity and function.
2.4. Paneth Cell Dysfunction
Intestinal epithelial cells include Paneth cells, a particular group of secretory cells located at the base of the crypts of Lieberkühn in the small intestine. As previously described, Paneth cells, together with goblet cells and enteroendocrine cells, originate from a common progenitor that expresses the Math1 gene [54]. Further differentiation of the secretory lineage into Paneth cells and goblet cells requires additional key transcription factors, such as: (1) Gfi1, a zinc-finger protein family member that functions downstream of Math1; (2) Sox9, which controls an early step of Paneth cell differentiation; (3) Fz5, which is crucial for the late step of cell commitment toward the Paneth cell phenotype; and (4) Cdk5rap3, which is involved in both fate decision and cell development [60]. Once differentiated, Paneth cells migrate to the base of crypts, instead of out of crypts onto adjacent villi. These specialized epithelial cells are able to produce and secrete granules enclosing AMPs (e.g., α-defensin, Reg3 lectins, lysozyme, and secretory phospholipase A2 isotype II) that shape the composition of commensals and protect the host from pathogen colonization [140,141]. Interestingly, mice with deficiency for vitamin D and exposed to high-fat diet showed decreased expression of Paneth cell-specific alpha-defensins, including α-defensin 5 (DEFA5), Matrix metalloproteinase 7 (MMP7), and tight junction genes [102]. Such defects resulted in enhanced gut permeability, microbial translocation, and consequent gut dysbiosis, as well as chronic inflammation and metabolic syndrome [102]. In addition, an increased fraction of abnormal Paneth cells that exhibit ER stress and accumulate reduced-form α-defensins were observed in SAMP1/YitFc mice, representing an animal model of Crohn’s disease-like ileitis [103]. In particular, secretion of misfolded α-defensins resulted in mucosal dysbiosis characterized by loss of Lachnospiraceae and Ruminococcaceae and increased abundance of Bacteroidaceae and Rikenellaceae [103]. Interestingly, administration of reduced-form α-defensins to wild-type mice induced similar microbial alterations, thus suggesting that Paneth cell activity was crucial to keep/ensure gut homeostasis [103].
Paneth cell dysfunction and consequent intestinal dysbiosis may also derive from the presence of risk alleles that commonly associate with chronic inflammatory pathologies, such as Crohn’s disease. In particular, the Nod2 gene encodes the nucleotide-binding oligomerization domain 2 (NOD2), a cytoplasmic muramyl dipeptide receptor able to recognize both Gram-positive and negative pathogens. NOD2 is highly expressed by Paneth cells and impaired NOD2 expression compromises α-defensins secretion, affecting gut homeostasis and promoting increased susceptibility to infections [71,72]. Other genetic polymorphisms associated with Paneth cell dysfunction (such as Xbp1 and Atg16l1 polymorphisms) are related to chronic ER stress and impaired autophagy in response to viral infection, leading to decreased AMP secretion [73,74,75]. Moreover, susceptibility polymorphisms in the promoter region of the Tcf4 gene also associate with Paneth cell dysfunction and Crohn’s disease development [76,77].
Paneth cell activity can also be hampered by dietary compounds. For instance, a high-fat diet is able to enhance the secretion of bile acids which, in turn, promote the upregulation of the G protein-coupled bile acid receptor (TGR5) on Paneth cell membrane [104]. The interaction between bile acids and TGR5 resulted in decreased expression of anti-microbial peptide-related genes (such as α-defensin 5 and 6) and induction of ER stress, autophagy, and DNA damage. Moreover, gut microbiota composition was significantly affected, with reduced abundance in Firmicutes and Lactobacillaceae, whereas Verrucomicrobiaceae, Akkermansia muciniphila, Clostridium XIVa, Ruminococcaceae, and Lachnospiraceae resulted to be increased [104]. Mice exposed to high-fat diet and orally treated with Cholestyramine (a bile acid sequestrant) or 4-Phenylbutyric acid (a ER stress inhibitor) prevented these changes as both molecules reduced serum bile acid levels and decreased TGR5 expression on Paneth cells without altering microbiota composition [104]. Finally, a Western diet has been suggested to indirectly impact on Paneth cell activity through the Clostridium-mediated conversion of the secondary bile acid deoxycholic acid. In detail, increased level of deoxycholic acid in the ileum induced excessive activation of the farnesoid X receptor (FXR) and type I interferon (IFN) signalling pathways, ultimately leading to Paneth cell defects [105].
Thus, impaired Paneth cell activity, induced by bile acid toxicity following a high-fat diet or other triggers, can deeply impact on host microbial composition and gut homeostasis, ultimately leading to the onset and development of gut dysbiosis and several chronic pathologic conditions.
2.5. Impairment of Microbial Sensing by Pattern Recognition Receptors (PRRs)
The efficient interaction/crosstalk between host and commensals across the intestinal epithelial barrier involves several inducible mechanisms that are able to discriminate endogenous and exogenous luminal antigens and to modulate the host immune response accordingly. These mechanisms require the presence on epithelial cells of specific receptors termed “pattern recognition receptors” (PRRs), which drive the sensing of pathogens and the consequent initiation of innate inflammatory immune responses, while maintaining an immune tolerance towards resident gut microbiota [142].
Toll-like receptors (TLRs) represent an important class of microbial-induced proteins expressed in different cell compartments including cells of the intestinal lining (e.g., stem cells, enterocytes), which are able to recognize microbial-related molecules—such as flagellin and lipopolysaccharide (LPS)—as well as single- and double-stranded RNAs. Once activated, TLRs trigger specific signalling pathways, ultimately inducing the expression/activation of transcription factors (e.g., NF-kB, AP-1, IRF3) involved in the orchestration of pro-inflammatory responses [143].
TLR-mediated pathways play an important role in the regulation of intestinal barrier function and integrity. For instance, the activation of the TLR4/MyD88 signal transduction pathway by LPS was seen to increase the intestinal permeability by promoting IL-1 receptor-associated kinase (IRAK)-4 function and the phosphorylation of transforming growth factor-β–activating kinase (TAK)-1, followed by the activation of the canonical NF-kB pathway and the up-regulation of myosin light chain kinase (MLCK) [144]. Deficiency in MyD88 signalling increased intestinal epithelial cell proliferation, whereas activation of TLR4 by LPS triggered apoptotic cell death in murine intestinal organoids [78]. Further, TLRs actively contribute to the secretion of both mucus and antimicrobial peptides, IgA class switching, the expression of polymeric immunoglobulin receptor, translocation of ZO-1 and occludin to the tight junctions, as well as to the expression of nicotinamide-adenine dinucleotide phosphate (NADPH) oxidase and release of ROS [145,146,147,148].
Increasing evidence suggests that TLR function may be critically involved in the intestinal epithelial restitution. Indeed, TLR activity in enterocytes, goblet cells, and mesenchymal stem cells induces the expression of molecules (e.g., trefoil factor 3, prostaglandin E2) and downstream pathways (e.g., Wnt–β-catenin), promoting the proliferation of enterocytes in the crypts adjacent to the wound [149]. On the other hand, TLR function is regulated by specific molecules (e.g., IRAK3, SIGIRR), and impairment of this control system results in excessive TLR activity and consequent gut dysbiosis and detrimental inflammatory response [150]. Thus, it is clear that TLR activation has to be tightly regulated in order to prevent excessive/impaired epithelial TLR signalling, which could compromise microbial–host interaction and lead to inefficient pathogen clearance, increased intestinal permeability, gut dysbiosis, and chronic inflammation. Another PRR significantly contributing to gut homeostasis is NOD2, a cytosolic receptor expressed by both epithelial (e.g., Paneth cells, stem cells) and immune cells. Loss-of-function mutations in Nod2 gene associate with increased susceptibility to Crohn’s disease due to impaired pathogen clearance by dendritic cells [79,80,81]. However, NOD2 function in epithelial cells is also crucial in order to maintain microbial ecology. In particular, upon sensing the bacterial muramyl dipeptide, N-acetylmuramyl-L-alanyl-D-isoglutamine (MDP) present in Gram-positive and -negative bacteria, NOD2 is able to trigger host defences through the production of antimicrobial peptides, cytokines, mucins, and the activation of immune responses, thus ensuring a balanced host-microbial crosstalk [151,152]. Given that, Nod2-deficient mice showed a decreased antimicrobial activity of Paneth cells and enhanced intestinal colonization by pathogens that could easily penetrate through the intestinal barrier and induce gut dysbiosis [82]. In addition to the above-mentioned functions, NOD2 exerts a protective effect against oxidative stress-mediated cell death on stem cells and sustains epithelial regeneration [83], thus contributing to the intestinal barrier integrity.
2.6. Modulation of Epithelial Oxidative Burst
TLR ligands are critical actors in the defence system against luminal pathogens as they promote the transcription of NADPH oxidase-related genes and the production/release of ROS by phagocytes in the lamina propria. In addition, ROS can be produced by IECs through the activity of the NADPH oxidases DUOX2 and NOX1 [153,154]. The former, in particular, is expressed at the apical membrane of enterocytes and dimerizes with DUOXA2 for maturation and cell membrane trafficking [153,154]. The main function of DUOX2 is to protect the host mucosal surfaces by releasing hydrogen peroxide in response to pathogens (e.g., Salmonella typhimurium, Listeria monocytogenes, Campylobacter jejun), thus contributing to the maintenance of gut homeostasis [153,155,156,157]. Given that, loss of DUOX2 activity results in enhanced pathogen translocation to host lymphatic tissue and activation of compensatory defence mechanisms [84]. Interestingly, Grasberger and colleagues identified a significant association between DUOX2 loss-of-function variants and IL-17C induction in IBD mucosal biopsies in response to Gram-negative bacteria, suggesting that DUOX2 variants may increase the risk of developing IBD [84]. However, it is worth underlining that chronic activation of DUOX2 in the inflamed tissues of IBD patients may sustain harmful inflammatory responses [158,159]. In this context, DUOX2 expression was not limited to apical surface of epithelial cells, but widely expressed along the crypt epithelium of IBD patients [158]. Moreover, enhanced DUOX2 expression in inflamed intestinal tissue associated with gut dysbiosis is characterized by Proteobacteria expansion in Crohn’s disease patients [160]. Altogether, these evidences suggest that a dysregulated DUOX2 function may be considered a sensitive marker of gut dysbiosis and intestinal inflammation in IBD patients [161].
During an infection process, DUOX2 activity can be modulated by another intestinal epithelium NADPH oxidase, namely NADPH Oxidase 1 (NOX1) [85]. In particular, lack of Cyba protein, which normally dimerizes with NOX1 to form a superoxide-generating NADPH oxidase, was seen to compromise DUOX2 activity in response to intestinal infection by Citrobacter rodentium in mice [85]. Interestingly, loss of mucosal NOX1 function did not exacerbate intestinal inflammation by Citrobacter rodentium as several commensal, including Lactobacilli such as Lactobacillus leuteri and Lactobacillus murinus, started producing hydrogen peroxide and downregulating C. rodentium-related virulence factors to ensure host protection and gut homeostasis [85]. Both NOX1 and DUOX2 function can be also triggered by TLR-4 expressed on IECs [145]. In this regard, using Tlr-4fl/fl-Villin-Cre+ mice, Burgueño and colleagues observed that dysregulated TLR-4 signalling in IECs led to NOX1 and DUOX2 overexpression [145]. Further, dysregulated hydrogen peroxide synthesis altered gut microbiota and induced increased susceptibility to dysplasia and colon tumorigenesis once transplanted into recipient germ-free mice [145]. Hence, NOX1 and DUOX2 activity have to be tightly regulated in order to ensure pathogen clearance and prevent mucosal dysbiosis, as well as harmful intestinal inflammatory responses.
2.7. Modulation of Xenobiotic Receptors
Among their functions, IECs can also provide protection against xenobiotic substances (e.g., environmental pollutants, chemicals, drugs) thanks to a detoxification system encompassing specific enzymes involved in the elimination of toxic compounds from the host [162]. These detoxification enzymes are regulated by specific transcription factors, such as the nuclear receptor pregnane X receptor (PXR) and the drug receptor aryl hydrocarbon receptor (AhR), which are mainly expressed in the liver, small intestine, and colon [163,164]. Accumulating evidence suggests that these receptors are actively involved in the modulation of several physiologic functions (e.g., cell proliferation, cell death, inflammatory immune response) by recognizing food components and endogenous ligands [165,166]. In particular, PXR can regulate the expression of drug-metabolizing and drug-transporter enzymes, such as UDP glucuronosyltransferases (UGTs), glutathione S-transferases (GSTs), the cytochrome P450 (CYP) family, the multidrug resistance protein 1 (MDR1), and the multidrug-resistant associated proteins (MRPs) [167]. PXR is also a critical regulator of mucosal surfaces, known to recognize several endobiotic compounds (e.g., bilirubin, bile acids) [168]. PXR was seen to exert anti-inflammatory functions by preventing Iκ-Bα degradation, thus limiting the activity of the transcription factor NF-κB [169,170]. Moreover, PXR actively contributes to the intestinal barrier integrity and function. Indeed, Pxr-deficient mice showed increased intestinal permeability due to a reduction in ZO-1 and E-cadherin expression, as well as an increase in claudin-2 levels [86]. The dysregulated TLR4-NF-κB signalling pathway derived from the absence of PXR expression resulted in TNF-α over-production that further contributed to the increased paracellular transport across the epithelial barrier [86]. In detail, TNF-α induced ZO-1 relocalization through the upregulation of Myosin Light Chain Kinase (MLCK) expression, which, in turn, phosphorylates myosin II regulatory light chain (MLC), a protein involved in the junctional complex arrangement. PXR, instead, was seen to limit the MLCK upregulation by targeting NF-κB activation [165].
Moreover, PXR is also able to limit the phosphorylation and activation of C-jun N-terminal kinase (JNK) 1/2 by inducing the expression of the JNK1/2 inhibitory molecule GADD45β (growth arrest and DNA damage inducible 45β) [171]. Terc and colleagues also reported that PXR activation can mediate the intestinal epithelial cell migration and proliferation, as well as the repair of the intestinal barrier by inducing p38 mitogen-activated protein kinase (MAPK) activation following experimental colitis [165]. Decreased levels of PXR were observed in the inflamed tissue of IBD patients and polymorphisms of the PXR-encoding gene Nr1I2, which is significantly associated with increased susceptibility to disease [87,88].
In conclusion, PXR is a critical player in gut homeostasis maintenance and, for this reason, it should be considered a potential therapeutic target to manage chronic intestinal inflammation, gut dysbiosis, and epithelial damage.
Aryl hydrocarbon receptor (AhR) is a member of the basic helix–loop–helix (bHLH)–PAS family of transcription factors that act as environmental sensors (e.g., circadian rhythm, hypoxia, xenobiotic response) [172,173]. Aryl hydrocarbon receptor expression was originally characterized in the intestinal immune cells (e.g., Th17 cells, intraepithelial lymphocytes) where AhR-dependent signalling was crucial for immune cell survival and functional activity [174]. However, increasing evidence confirmed that AhR is also widely expressed in the intestinal microenvironment by non-hematopoietic cells (e.g., IECs) and its activation by natural ligands, such as dietary and microbial metabolites, results in the maintenance of gut homeostasis at the barrier sites (e.g., lung and gut) [175,176]. In particular, AhR deficiency in IECs causes increased susceptibility to the intestinal infection despite a normal immune compartment. Moreover, mice with dysregulated AhR expression in the epithelium showed dysfunctional barrier, characterized by reduced mucus production and impaired TJs, as well as chronic low-grade inflammation and crypt hyperplasia [89,90,91]. AhR was also seen to take part in the modulation of crypt stem cell proliferation, wound healing processes, and cell commitment. In particular, Ahrfl/fl-Villin-Cre+ mice showed impaired resistance against Citrobacter rodentium infection characterized by bacterial dissemination in the liver and in the spleen, increased epithelial damage, and decreased expression of Muc2 and Car4 genes, thus confirming a crucial role of AhR in the maintenance of gut homeostasis [90]. Furthermore, mice exposed to AhR ligand-free diet (e.g., high fat diet) developed gut dysbiosis, characterized by higher susceptibility to experimental colitis and overgrowth of Erysipelotrichaceae family compared to mice receiving the dietary AhR ligand indole-3-carbinol (I3C) [106,107]. Another important source of AhR natural ligands is represented by commensal microbiota. For example, the induction of AhR transcriptional targets was observed in IECs upon challenge with butyrate derived from Proteobacteria, Firmicutes, and Fusobacteria, and in part from Actinobacteria [177]. Overall, these observations indicate AhR activation in IECs by either xenobiotic compounds or natural ligands as a crucial step to ensure barrier integrity and host microbial ecology.
2.8. Impairment of Secretory IgA
Immunoglobulin A (IgA), the major immunoglobulin isotype secreted at the mucosal surfaces, provides the first line of defence against pathogens and toxins [178]. Maternal milk-derived secretory immunoglobulin A (SIgA) can mediate the protection at mucosal surfaces in neonates [179]. Moreover, SIgA is crucial in the regulation of host immune homeostasis as it can shape the composition and function of gut microbiota and promote bacteria–mucus and bacteria–bacteria interactions, leading to the release of metabolites enforcing mucosal barrier functions [180,181]. SIgA is mainly produced by plasma cells in the lamina propria, transported across the IECs through a transcytosis mechanism mediated by poly Ig receptor (pIgR), and released into the lumen in order to neutralize invading pathogens and related products via different mechanisms [182,183]. SIgA can modulate gut homeostasis by binding and excluding invading pathogens from the mucosal surface through a process called “agglutination”, thus preventing them from breaching the epithelial barrier and limiting consequent unwanted immune responses (immune exclusion) [184]. Moreover, SIgA are able to intercept incoming antigens intracellulary, thus generating immune complexes that are then transported by pIgR across the epithelial cells in order to be cleared [179,184]. Finally, SIgA immune complexes can be internalized by microfold cells (M cells) in the mucosal-associated lymphoid tissue and recognized by tolerogenic DCs, which, in turn, may secrete IL-10 and TGF-β cytokines and promote Foxp3+ regulatory T cells expansion, thus limiting potential detrimental inflammatory immune responses [185,186].
Given the above-mentioned functions, it is clear that impaired SIgA production and release can deeply impact on gut homeostasis, leading to decreased microbial diversity and mucosal dysbiosis [92]. Even though secretory IgM (SIgM) can be released into the gut lumen in response to IgA deficiency, this counteracting mechanism can only partially compensate such a defect. In particular, subjects with selective IgA deficiency exhibited alterations of microbial ecology with reduced alpha diversity [187,188]. Similar results have been reported in mice lacking pIgR, where SIgA levels were decreased at the mucosal surfaces due to impaired transcytosis across epithelial cells [93,94]. Again, microbial community was significantly altered in these mice, though compensatory mechanisms occurred to limit potential detrimental effects (e.g., increase of serum IgA levels and B cells, and increase of the frequency of macrophages, dendritic cells, and intraepithelial lymphocytes) [189,190,191,192].
3. Discussion and Therapeutic Perspectives
The maintenance of the intestinal barrier integrity and functions requires a fine-tuned balance among different specialized cells in order to ensure the physiological and protective crosstalk between intestinal microbes and host immune response, protection against xenobiotic substances, as well as nutrient absorption.
Nowadays, much effort has been made to explore the mechanisms underlying an altered intestinal barrier and gut dysbiosis in subjects carrying genetic polymorphisms or exposed to infections, medications and specific diets. In this regard, the recent advent of integrative multi-omic analyses has become a valid and promising means to better characterize the pivotal contribution of genetic defects and environmental factors in the impairment of gut homeostasis. For instance, metataxonomic and metagenomic data have helped to characterize microbiota profiles in different pathological conditions (such as IBD) and, in addition, highly contributed to uncover the dynamics and functional interactions among bacteria, metabolite pools, and host genetics [193,194,195]. Similarly, transcriptomic, proteomic, and metabolomic techniques have strongly helped to better define the impact of gut dysbiosis in IBD pathogenesis as well as in the development and progression of other chronic diseases [196,197,198,199,200]. Altogether, these approaches have definitely provided important knowledge to predict the onset and progression of pathological conditions, as well as their response to treatments, thus representing a key tool for the development of new diagnostic, prognostic, and therapeutic strategies [197,198,201,202,203].
Restoring the intestinal barrier physiological functions following a perturbation has always been considered a fascinating and promising approach to treat chronic inflammatory diseases such as IBD, and, indeed, multiple attempts have been made in this direction.
Over the past decades, it was found that flavonoids, which are phytochemicals with biological activity ubiquitously distributed in edible plants, can directly treat IBD through various mechanisms, including anti-inflammatory and antioxidant actions, which preserve the epithelial barrier; immunomodulatory functions in the intestine, which shape the composition and function of the microbiota; and the modulation of specific enterohormones (such as glucagon-like peptide 1 and dipeptidyl peptidase-4 inhibitors) [204,205,206]. Taken together, these observations suggest that the maintenance of gut homeostasis can be modulated by such bioactive compounds. Further studies on the basic functional role of flavonoids in IBD could contribute to establish new effective therapeutic options for the treatment of this disease in the future.
Accumulating evidence has shown the importance of the JAK-STAT signaling pathway in the pathogenesis of IBD by inducing, both directly and via the modulation of inflammatory cytokines, changes in intestinal paracellular permeability through the regulation of tight junction protein expression and localization. Given that, inhibitors of the JAK-STAT pathway are currently a therapeutic option for IBD patients. However, these compounds may present potential risks, including non-specificity and toxicity [207].
As decreased microbial diversity, overgrowth of pathogens, and uncontrolled immune/inflammatory response characterizing IBD were seen to further sustain defective barrier function (although most often these events are just a direct consequence of barrier impairment), other curative possibilities aim at treating these aspects.
In this context, change in dietary habits is one of the most powerful ways to alter the gut microbiome [208,209]. For instance, high-fiber diets (e.g., vegetarian, vegan, Mediterranean), which are low in red meat and higher in unsaturated fatty acids, are associated with a more beneficial microbiome composition, an increased microbial diversity, and more health-promoting bacteria (e.g., Bifidobacteria, Lactobacillus), as well as higher levels of small chain fatty acids (especially butyrate) [210,211,212,213]. These modulations result in a more thick mucus layer and an improved function of the intestinal barrier. Nevertheless, although dietary interventions aimed at reducing inflammatory chronic diseases and improving the microbiome are promising, the field is still evolving and, due to a large heterogeneity of the studies, drawing definitive conclusions has proved difficult in the past.
Finally, it should be mentioned that some IBD medications (e.g., steroids, aminosalicylates, and anti-TNF-α agents), as well as the use of probiotics/prebiotics have been reported to positively affect either the composition/metabolism of gut microbiota or the metabolic status of intestinal cells by altering the intestinal biota [214]. These drugs/strategies may thus represent valid therapeutic options.
A different and more fascinating approach is aimed at targeting the primary genetic defects undermining the intestinal barrier homeostasis with the delivery of therapeutic genetic information through viral vectors (e.g., lentiviruses, adenoviruses). However, it is worth underlining that, in this regard, no therapies have been validated in clinical studies so far, due to a number of drawbacks. For instance, the viral access to transduce intestinal epithelial cells with the gene of interest can be damped by the mucosal barrier itself as the mucus layer and/or the tight junctions may interfere with this process [215,216,217,218,219,220,221].
In addition, as enterocytes are characterized by a high turnover, this precludes their long-term transduction [222,223]. Finally, multiple treatments with viral vectors may trigger unwanted host immune responses that could compromise the efficacy of this therapeutic approach [224].
4. Conclusions
In conclusion, targeting intestinal barrier dysfunctions, and in particular those related to primary genetic defects, represents a very interesting and challenging approach to treat gut-related diseases. However, further efforts are necessary to transfer experimental findings on this complex topic into clinical practice.
Author Contributions
C.S.: literature search, writing—original draft preparation; C.M.: literature search, figure and table preparation; G.M.: review and editing; F.L.: conceptualization, literature search, writing—review, and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Peterson L.W., Artis D. Intestinal epithelial cells: Regulators of barrier function and immune homeostasis. Nat. Rev. Immunol. 2014;14:141–153. doi: 10.1038/nri3608. [DOI] [PubMed] [Google Scholar]
- 2.Goto Y., Kiyono H. Epithelial barrier: An interface for the cross-communication between gut flora and immune system. Immunol. Rev. 2012;245:147–163. doi: 10.1111/j.1600-065X.2011.01078.x. [DOI] [PubMed] [Google Scholar]
- 3.Okumura R., Takeda K. Roles of intestinal epithelial cells in the maintenance of gut homeostasis. Exp. Mol. Med. 2017;49:e338. doi: 10.1038/emm.2017.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hooper L.V., Macpherson A.J. Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat. Rev. Immunol. 2010;10:159–169. doi: 10.1038/nri2710. [DOI] [PubMed] [Google Scholar]
- 5.Martens E.C., Neumann M., Desai M.S. Interactions of commensal and pathogenic microorganisms with the intestinal mucosal barrier. Nat. Rev. Microbiol. 2018;16:457–470. doi: 10.1038/s41579-018-0036-x. [DOI] [PubMed] [Google Scholar]
- 6.Pickard J.M., Zeng M.Y., Caruso R., Nunez G. Gut microbiota: Role in pathogen colonization, immune responses, and inflammatory disease. Immunol. Rev. 2017;279:70–89. doi: 10.1111/imr.12567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Round J.L., Mazmanian S.K. The gut microbiota shapes intestinal immune responses during health and disease. Nat. Rev. Immunol. 2009;9:313–323. doi: 10.1038/nri2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hayes C.L., Dong J., Galipeau H.J., Jury J., McCarville J., Huang X., Wang X.Y., Naidoo A., Anbazhagan A.N., Libertucci J., et al. Commensal microbiota induces colonic barrier structure and functions that contribute to homeostasis. Sci. Rep. 2018;8:14184. doi: 10.1038/s41598-018-32366-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghosh S., Whitley C.S., Haribabu B., Jala V.R. Regulation of Intestinal Barrier Function by Microbial Metabolites. Cell. Mol. Gastroenterol. Hepatol. 2021;11:1463–1482. doi: 10.1016/j.jcmgh.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Su L., Shen L., Clayburgh D.R., Nalle S.C., Sullivan E.A., Meddings J.B., Abraham C., Turner J.R. Targeted epithelial tight junction dysfunction causes immune activation and contributes to development of experimental colitis. Gastroenterology. 2009;136:551–563. doi: 10.1053/j.gastro.2008.10.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Groschwitz K.R., Hogan S.P. Intestinal barrier function: Molecular regulation and disease pathogenesis. J. Allergy Clin. Immunol. 2009;124:3–20. doi: 10.1016/j.jaci.2009.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mankertz J., Schulzke J.D. Altered permeability in inflammatory bowel disease: Pathophysiology and clinical implications. Curr. Opin. Gastroenterol. 2007;23:379–383. doi: 10.1097/MOG.0b013e32816aa392. [DOI] [PubMed] [Google Scholar]
- 13.Martini E., Krug S.M., Siegmund B., Neurath M.F., Becker C. Mend Your Fences: The Epithelial Barrier and its Relationship with Mucosal Immunity in Inflammatory Bowel Disease. Cell. Mol. Gastroenterol. Hepatol. 2017;4:33–46. doi: 10.1016/j.jcmgh.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gitter A.H., Wullstein F., Fromm M., Schulzke J.D. Epithelial barrier defects in ulcerative colitis: Characterization and quantification by electrophysiological imaging. Gastroenterology. 2001;121:1320–1328. doi: 10.1053/gast.2001.29694. [DOI] [PubMed] [Google Scholar]
- 15.Van der Sluis M., De Koning B.A., De Bruijn A.C., Velcich A., Meijerink J.P., Van Goudoever J.B., Buller H.A., Dekker J., Van Seuningen I., Renes I.B., et al. Muc2-deficient mice spontaneously develop colitis, indicating that MUC2 is critical for colonic protection. Gastroenterology. 2006;131:117–129. doi: 10.1053/j.gastro.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 16.Heazlewood C.K., Cook M.C., Eri R., Price G.R., Tauro S.B., Taupin D., Thornton D.J., Png C.W., Crockford T.L., Cornall R.J., et al. Aberrant mucin assembly in mice causes endoplasmic reticulum stress and spontaneous inflammation resembling ulcerative colitis. PLoS Med. 2008;5:e54. doi: 10.1371/journal.pmed.0050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Braun A., Treede I., Gotthardt D., Tietje A., Zahn A., Ruhwald R., Schoenfeld U., Welsch T., Kienle P., Erben G., et al. Alterations of phospholipid concentration and species composition of the intestinal mucus barrier in ulcerative colitis: A clue to pathogenesis. Inflamm. Bowel Dis. 2009;15:1705–1720. doi: 10.1002/ibd.20993. [DOI] [PubMed] [Google Scholar]
- 18.Larsson J.M., Karlsson H., Crespo J.G., Johansson M.E., Eklund L., Sjovall H., Hansson G.C. Altered O-glycosylation profile of MUC2 mucin occurs in active ulcerative colitis and is associated with increased inflammation. Inflamm. Bowel Dis. 2011;17:2299–2307. doi: 10.1002/ibd.21625. [DOI] [PubMed] [Google Scholar]
- 19.Heller F., Florian P., Bojarski C., Richter J., Christ M., Hillenbrand B., Mankertz J., Gitter A.H., Burgel N., Fromm M., et al. Interleukin-13 is the key effector Th2 cytokine in ulcerative colitis that affects epithelial tight junctions, apoptosis, and cell restitution. Gastroenterology. 2005;129:550–564. doi: 10.1016/j.gastro.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 20.Lammers K.M., Lu R., Brownley J., Lu B., Gerard C., Thomas K., Rallabhandi P., Shea-Donohue T., Tamiz A., Alkan S., et al. Gliadin induces an increase in intestinal permeability and zonulin release by binding to the chemokine receptor CXCR3. Gastroenterology. 2008;135:194–204.e3. doi: 10.1053/j.gastro.2008.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fasano A., Not T., Wang W., Uzzau S., Berti I., Tommasini A., Goldblum S.E. Zonulin, a newly discovered modulator of intestinal permeability, and its expression in coeliac disease. Lancet. 2000;355:1518–1519. doi: 10.1016/S0140-6736(00)02169-3. [DOI] [PubMed] [Google Scholar]
- 22.El Asmar R., Panigrahi P., Bamford P., Berti I., Not T., Coppa G.V., Catassi C., Fasano A. Host-dependent zonulin secretion causes the impairment of the small intestine barrier function after bacterial exposure. Gastroenterology. 2002;123:1607–1615. doi: 10.1053/gast.2002.36578. [DOI] [PubMed] [Google Scholar]
- 23.Szakal D.N., Gyorffy H., Arato A., Cseh A., Molnar K., Papp M., Dezsofi A., Veres G. Mucosal expression of claudins 2, 3 and 4 in proximal and distal part of duodenum in children with coeliac disease. Virchows Arch. Int. J. Pathol. 2010;456:245–250. doi: 10.1007/s00428-009-0879-7. [DOI] [PubMed] [Google Scholar]
- 24.Ciccocioppo R., Finamore A., Ara C., Di Sabatino A., Mengheri E., Corazza G.R. Altered expression, localization, and phosphorylation of epithelial junctional proteins in celiac disease. Am. J. Clin. Pathol. 2006;125:502–511. doi: 10.1309/DTYRA91G8R0KTM8M. [DOI] [PubMed] [Google Scholar]
- 25.Theriot C.M., Koenigsknecht M.J., Carlson P.E., Jr., Hatton G.E., Nelson A.M., Li B., Huffnagle G.B., Li J.Z., Young V.B. Antibiotic-induced shifts in the mouse gut microbiome and metabolome increase susceptibility to Clostridium difficile infection. Nat. Commun. 2014;5:3114. doi: 10.1038/ncomms4114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Theriot C.M., Young V.B. Microbial and metabolic interactions between the gastrointestinal tract and Clostridium difficile infection. Gut Microbes. 2014;5:86–95. doi: 10.4161/gmic.27131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kachrimanidou M., Tsintarakis E. Insights into the Role of Human Gut Microbiota in Clostridioides difficile Infection. Microorganisms. 2020;8:200. doi: 10.3390/microorganisms8020200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hanning N., Edwinson A.L., Ceuleers H., Peters S.A., De Man J.G., Hassett L.C., De Winter B.Y., Grover M. Intestinal barrier dysfunction in irritable bowel syndrome: A systematic review. Ther. Adv. Gastroenterol. 2021;14:1756284821993586. doi: 10.1177/1756284821993586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Martinez C., Vicario M., Ramos L., Lobo B., Mosquera J.L., Alonso C., Sanchez A., Guilarte M., Antolin M., de Torres I., et al. The jejunum of diarrhea-predominant irritable bowel syndrome shows molecular alterations in the tight junction signaling pathway that are associated with mucosal pathobiology and clinical manifestations. Am. J. Gastroenterol. 2012;107:736–746. doi: 10.1038/ajg.2011.472. [DOI] [PubMed] [Google Scholar]
- 30.Martinez C., Lobo B., Pigrau M., Ramos L., Gonzalez-Castro A.M., Alonso C., Guilarte M., Guila M., de Torres I., Azpiroz F., et al. Diarrhoea-predominant irritable bowel syndrome: An organic disorder with structural abnormalities in the jejunal epithelial barrier. Gut. 2013;62:1160–1168. doi: 10.1136/gutjnl-2012-302093. [DOI] [PubMed] [Google Scholar]
- 31.Martinez C., Rodino-Janeiro B.K., Lobo B., Stanifer M.L., Klaus B., Granzow M., Gonzalez-Castro A.M., Salvo-Romero E., Alonso-Cotoner C., Pigrau M., et al. miR-16 and miR-125b are involved in barrier function dysregulation through the modulation of claudin-2 and cingulin expression in the jejunum in IBS with diarrhoea. Gut. 2017;66:1537–1538. doi: 10.1136/gutjnl-2016-311477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dunlop S.P., Hebden J., Campbell E., Naesdal J., Olbe L., Perkins A.C., Spiller R.C. Abnormal intestinal permeability in subgroups of diarrhea-predominant irritable bowel syndromes. Am. J. Gastroenterol. 2006;101:1288–1294. doi: 10.1111/j.1572-0241.2006.00672.x. [DOI] [PubMed] [Google Scholar]
- 33.Long Y., Du L., Kim J.J., Chen B., Zhu Y., Zhang Y., Yao S., He H., Zheng X., Huang Z., et al. MLCK-mediated intestinal permeability promotes immune activation and visceral hypersensitivity in PI-IBS mice. Neurogastroenterol. Motil. Off. J. Eur. Gastrointest. Motil. Soc. 2018;30:e13348. doi: 10.1111/nmo.13348. [DOI] [PubMed] [Google Scholar]
- 34.Zhou Q., Verne M.L., Fields J.Z., Lefante J.J., Basra S., Salameh H., Verne G.N. Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome. Gut. 2019;68:996–1002. doi: 10.1136/gutjnl-2017-315136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dhawan P., Singh A.B., Deane N.G., No Y., Shiou S.R., Schmidt C., Neff J., Washington M.K., Beauchamp R.D. Claudin-1 regulates cellular transformation and metastatic behavior in colon cancer. J. Clin. Investig. 2005;115:1765–1776. doi: 10.1172/JCI24543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Weber C.R., Nalle S.C., Tretiakova M., Rubin D.T., Turner J.R. Claudin-1 and claudin-2 expression is elevated in inflammatory bowel disease and may contribute to early neoplastic transformation. Lab. Investig. A J. Tech. Methods Pathol. 2008;88:1110–1120. doi: 10.1038/labinvest.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kostic A.D., Chun E., Robertson L., Glickman J.N., Gallini C.A., Michaud M., Clancy T.E., Chung D.C., Lochhead P., Hold G.L., et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe. 2013;14:207–215. doi: 10.1016/j.chom.2013.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Buc E., Dubois D., Sauvanet P., Raisch J., Delmas J., Darfeuille-Michaud A., Pezet D., Bonnet R. High prevalence of mucosa-associated E. coli producing cyclomodulin and genotoxin in colon cancer. PLoS ONE. 2013;8:e56964. doi: 10.1371/journal.pone.0056964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Boleij A., Hechenbleikner E.M., Goodwin A.C., Badani R., Stein E.M., Lazarev M.G., Ellis B., Carroll K.C., Albesiano E., Wick E.C., et al. The Bacteroides fragilis toxin gene is prevalent in the colon mucosa of colorectal cancer patients. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2015;60:208–215. doi: 10.1093/cid/ciu787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Biarc J., Nguyen I.S., Pini A., Gosse F., Richert S., Thierse D., Van Dorsselaer A., Leize-Wagner E., Raul F., Klein J.P., et al. Carcinogenic properties of proteins with pro-inflammatory activity from Streptococcus infantarius (formerly S.bovis) Carcinogenesis. 2004;25:1477–1484. doi: 10.1093/carcin/bgh091. [DOI] [PubMed] [Google Scholar]
- 41.Genser L., Aguanno D., Soula H.A., Dong L., Trystram L., Assmann K., Salem J.E., Vaillant J.C., Oppert J.M., Laugerette F., et al. Increased jejunal permeability in human obesity is revealed by a lipid challenge and is linked to inflammation and type 2 diabetes. J. Pathol. 2018;246:217–230. doi: 10.1002/path.5134. [DOI] [PubMed] [Google Scholar]
- 42.Cani P.D., Bibiloni R., Knauf C., Waget A., Neyrinck A.M., Delzenne N.M., Burcelin R. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes. 2008;57:1470–1481. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 43.Pendyala S., Walker J.M., Holt P.R. A high-fat diet is associated with endotoxemia that originates from the gut. Gastroenterology. 2012;142:1100–1101.e2. doi: 10.1053/j.gastro.2012.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Thaiss C.A., Levy M., Grosheva I., Zheng D., Soffer E., Blacher E., Braverman S., Tengeler A.C., Barak O., Elazar M., et al. Hyperglycemia drives intestinal barrier dysfunction and risk for enteric infection. Science. 2018;359:1376–1383. doi: 10.1126/science.aar3318. [DOI] [PubMed] [Google Scholar]
- 45.Meddings J.B., Jarand J., Urbanski S.J., Hardin J., Gall D.G. Increased gastrointestinal permeability is an early lesion in the spontaneously diabetic BB rat. Am. J. Physiol. 1999;276:G951–G957. doi: 10.1152/ajpgi.1999.276.4.G951. [DOI] [PubMed] [Google Scholar]
- 46.Neu J., Reverte C.M., Mackey A.D., Liboni K., Tuhacek-Tenace L.M., Hatch M., Li N., Caicedo R.A., Schatz D.A., Atkinson M. Changes in intestinal morphology and permeability in the biobreeding rat before the onset of type 1 diabetes. J. Pediatric Gastroenterol. Nutr. 2005;40:589–595. doi: 10.1097/01.MPG.0000159636.19346.C1. [DOI] [PubMed] [Google Scholar]
- 47.Bosi E., Molteni L., Radaelli M.G., Folini L., Fermo I., Bazzigaluppi E., Piemonti L., Pastore M.R., Paroni R. Increased intestinal permeability precedes clinical onset of type 1 diabetes. Diabetologia. 2006;49:2824–2827. doi: 10.1007/s00125-006-0465-3. [DOI] [PubMed] [Google Scholar]
- 48.Watts T., Berti I., Sapone A., Gerarduzzi T., Not T., Zielke R., Fasano A. Role of the intestinal tight junction modulator zonulin in the pathogenesis of type I diabetes in BB diabetic-prone rats. Proc. Natl. Acad. Sci. USA. 2005;102:2916–2921. doi: 10.1073/pnas.0500178102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sapone A., de Magistris L., Pietzak M., Clemente M.G., Tripathi A., Cucca F., Lampis R., Kryszak D., Carteni M., Generoso M., et al. Zonulin upregulation is associated with increased gut permeability in subjects with type 1 diabetes and their relatives. Diabetes. 2006;55:1443–1449. doi: 10.2337/db05-1593. [DOI] [PubMed] [Google Scholar]
- 50.Visser J.T., Lammers K., Hoogendijk A., Boer M.W., Brugman S., Beijer-Liefers S., Zandvoort A., Harmsen H., Welling G., Stellaard F., et al. Restoration of impaired intestinal barrier function by the hydrolysed casein diet contributes to the prevention of type 1 diabetes in the diabetes-prone BioBreeding rat. Diabetologia. 2010;53:2621–2628. doi: 10.1007/s00125-010-1903-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guo X.K., Ou J., Liang S., Zhou X., Hu X. Epithelial Hes1 maintains gut homeostasis by preventing microbial dysbiosis. Mucosal Immunol. 2018;11:716–726. doi: 10.1038/mi.2017.111. [DOI] [PubMed] [Google Scholar]
- 52.Jensen J., Pedersen E.E., Galante P., Hald J., Heller R.S., Ishibashi M., Kageyama R., Guillemot F., Serup P., Madsen O.D. Control of endodermal endocrine development by Hes-1. Nat. Genet. 2000;24:36–44. doi: 10.1038/71657. [DOI] [PubMed] [Google Scholar]
- 53.Suzuki K., Fukui H., Kayahara T., Sawada M., Seno H., Hiai H., Kageyama R., Okano H., Chiba T. Hes1-deficient mice show precocious differentiation of Paneth cells in the small intestine. Biochem. Biophys. Res. Commun. 2005;328:348–352. doi: 10.1016/j.bbrc.2004.12.174. [DOI] [PubMed] [Google Scholar]
- 54.Yang Q., Bermingham N.A., Finegold M.J., Zoghbi H.Y. Requirement of Math1 for secretory cell lineage commitment in the mouse intestine. Science. 2001;294:2155–2158. doi: 10.1126/science.1065718. [DOI] [PubMed] [Google Scholar]
- 55.Liu X., Lu J., Liu Z., Zhao J., Sun H., Wu N., Liu H., Liu W., Hu Z., Meng G., et al. Intestinal Epithelial Cell-Derived LKB1 Suppresses Colitogenic Microbiota. J. Immunol. 2018;200:1889–1900. doi: 10.4049/jimmunol.1700547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shimada T., Koike T., Yamagata M., Yoneda M., Hiraishi H. Regulation of TFF3 expression by homeodomain protein CDX2. Regul. Pept. 2007;140:81–87. doi: 10.1016/j.regpep.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 57.Beuling E., Baffour-Awuah N.Y., Stapleton K.A., Aronson B.E., Noah T.K., Shroyer N.F., Duncan S.A., Fleet J.C., Krasinski S.D. GATA factors regulate proliferation, differentiation, and gene expression in small intestine of mature mice. Gastroenterology. 2011;140:1219–1229.e2. doi: 10.1053/j.gastro.2011.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Beuling E., Aronson B.E., Tran L.M., Stapleton K.A., ter Horst E.N., Vissers L.A., Verzi M.P., Krasinski S.D. GATA6 is required for proliferation, migration, secretory cell maturation, and gene expression in the mature mouse colon. Mol. Cell. Biol. 2012;32:3392–3402. doi: 10.1128/MCB.00070-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laudisi F., Stolfi C., Bevivino G., Maresca C., Franze E., Troncone E., Lolli E., Marafini I., Pietrucci D., Teofani A., et al. GATA6 deficiency leads to epithelial barrier dysfunction and enhances susceptibility to gut inflammation. J. Crohn’s Colitis. 2021:jjab145. doi: 10.1093/ecco-jcc/jjab145. [DOI] [PubMed] [Google Scholar]
- 60.Mori-Akiyama Y., van den Born M., van Es J.H., Hamilton S.R., Adams H.P., Zhang J., Clevers H., de Crombrugghe B. SOX9 is required for the differentiation of paneth cells in the intestinal epithelium. Gastroenterology. 2007;133:539–546. doi: 10.1053/j.gastro.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 61.Riba A., Olier M., Lacroix-Lamande S., Lencina C., Bacquie V., Harkat C., Gillet M., Baron M., Sommer C., Mallet V., et al. Paneth Cell Defects Induce Microbiota Dysbiosis in Mice and Promote Visceral Hypersensitivity. Gastroenterology. 2017;153:1594–1606.e2. doi: 10.1053/j.gastro.2017.08.044. [DOI] [PubMed] [Google Scholar]
- 62.Laukoetter M.G., Nava P., Lee W.Y., Severson E.A., Capaldo C.T., Babbin B.A., Williams I.R., Koval M., Peatman E., Campbell J.A., et al. JAM-A regulates permeability and inflammation in the intestine in vivo. J. Exp. Med. 2007;204:3067–3076. doi: 10.1084/jem.20071416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wada M., Tamura A., Takahashi N., Tsukita S. Loss of claudins 2 and 15 from mice causes defects in paracellular Na+ flow and nutrient transport in gut and leads to death from malnutrition. Gastroenterology. 2013;144:369–380. doi: 10.1053/j.gastro.2012.10.035. [DOI] [PubMed] [Google Scholar]
- 64.Odenwald M.A., Choi W., Kuo W.T., Singh G., Sailer A., Wang Y., Shen L., Fanning A.S., Turner J.R. The scaffolding protein ZO-1 coordinates actomyosin and epithelial apical specializations in vitro and in vivo. J. Biol. Chem. 2018;293:17317–17335. doi: 10.1074/jbc.RA118.003908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kuo W.T., Zuo L., Odenwald M.A., Madha S., Singh G., Gurniak C.B., Abraham C., Turner J.R. The Tight Junction Protein ZO-1 Is Dispensable for Barrier Function but Critical for Effective Mucosal Repair. Gastroenterology. 2021;161:1924–1939. doi: 10.1053/j.gastro.2021.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Marchelletta R.R., Krishnan M., Spalinger M.R., Placone T.W., Alvarez R., Sayoc-Becerra A., Canale V., Shawki A., Park Y.S., Bernts L.H., et al. T cell protein tyrosine phosphatase protects intestinal barrier function by restricting epithelial tight junction remodeling. J. Clin. Investig. 2021;131:e138230. doi: 10.1172/JCI138230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liso M., De Santis S., Verna G., Dicarlo M., Calasso M., Santino A., Gigante I., Eri R., Raveenthiraraj S., Sobolewski A., et al. A Specific Mutation in Muc2 Determines Early Dysbiosis in Colitis-Prone Winnie Mice. Inflamm. Bowel Dis. 2020;26:546–556. doi: 10.1093/ibd/izz279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Eri R.D., Adams R.J., Tran T.V., Tong H., Das I., Roche D.K., Oancea I., Png C.W., Jeffery P.L., Radford-Smith G.L., et al. An intestinal epithelial defect conferring ER stress results in inflammation involving both innate and adaptive immunity. Mucosal Immunol. 2011;4:354–364. doi: 10.1038/mi.2010.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shroyer N.F., Wallis D., Venken K.J., Bellen H.J., Zoghbi H.Y. Gfi1 functions downstream of Math1 to control intestinal secretory cell subtype allocation and differentiation. Genes Dev. 2005;19:2412–2417. doi: 10.1101/gad.1353905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Chen Z., Luo J., Li J., Kim G., Chen E.S., Xiao S., Snapper S.B., Bao B., An D., Blumberg R.S., et al. Foxo1 controls gut homeostasis and commensalism by regulating mucus secretion. J. Exp. Med. 2021;218:e20210324. doi: 10.1084/jem.20210324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Simms L.A., Doecke J.D., Walsh M.D., Huang N., Fowler E.V., Radford-Smith G.L. Reduced alpha-defensin expression is associated with inflammation and not NOD2 mutation status in ileal Crohn’s disease. Gut. 2008;57:903–910. doi: 10.1136/gut.2007.142588. [DOI] [PubMed] [Google Scholar]
- 72.Wehkamp J., Harder J., Weichenthal M., Schwab M., Schaffeler E., Schlee M., Herrlinger K.R., Stallmach A., Noack F., Fritz P., et al. NOD2 (CARD15) mutations in Crohn’s disease are associated with diminished mucosal alpha-defensin expression. Gut. 2004;53:1658–1664. doi: 10.1136/gut.2003.032805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cadwell K., Liu J.Y., Brown S.L., Miyoshi H., Loh J., Lennerz J.K., Kishi C., Kc W., Carrero J.A., Hunt S., et al. A key role for autophagy and the autophagy gene Atg16l1 in mouse and human intestinal Paneth cells. Nature. 2008;456:259–263. doi: 10.1038/nature07416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cadwell K., Patel K.K., Maloney N.S., Liu T.C., Ng A.C., Storer C.E., Head R.D., Xavier R., Stappenbeck T.S., Virgin H.W. Virus-plus-susceptibility gene interaction determines Crohn’s disease gene Atg16L1 phenotypes in intestine. Cell. 2010;141:1135–1145. doi: 10.1016/j.cell.2010.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Adolph T.E., Tomczak M.F., Niederreiter L., Ko H.J., Bock J., Martinez-Naves E., Glickman J.N., Tschurtschenthaler M., Hartwig J., Hosomi S., et al. Paneth cells as a site of origin for intestinal inflammation. Nature. 2013;503:272–276. doi: 10.1038/nature12599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Koslowski M.J., Kubler I., Chamaillard M., Schaeffeler E., Reinisch W., Wang G., Beisner J., Teml A., Peyrin-Biroulet L., Winter S., et al. Genetic variants of Wnt transcription factor TCF-4 (TCF7L2) putative promoter region are associated with small intestinal Crohn’s disease. PLoS ONE. 2009;4:e4496. doi: 10.1371/journal.pone.0004496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wehkamp J., Wang G., Kubler I., Nuding S., Gregorieff A., Schnabel A., Kays R.J., Fellermann K., Burk O., Schwab M., et al. The Paneth cell alpha-defensin deficiency of ileal Crohn’s disease is linked to Wnt/Tcf-4. J. Immunol. 2007;179:3109–3118. doi: 10.4049/jimmunol.179.5.3109. [DOI] [PubMed] [Google Scholar]
- 78.Neal M.D., Sodhi C.P., Jia H., Dyer M., Egan C.E., Yazji I., Good M., Afrazi A., Marino R., Slagle D., et al. Toll-like receptor 4 is expressed on intestinal stem cells and regulates their proliferation and apoptosis via the p53 up-regulated modulator of apoptosis. J. Biol. Chem. 2012;287:37296–37308. doi: 10.1074/jbc.M112.375881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hugot J.P., Chamaillard M., Zouali H., Lesage S., Cezard J.P., Belaiche J., Almer S., Tysk C., O’Morain C.A., Gassull M., et al. Association of NOD2 leucine-rich repeat variants with susceptibility to Crohn’s disease. Nature. 2001;411:599–603. doi: 10.1038/35079107. [DOI] [PubMed] [Google Scholar]
- 80.Ogura Y., Bonen D.K., Inohara N., Nicolae D.L., Chen F.F., Ramos R., Britton H., Moran T., Karaliuskas R., Duerr R.H., et al. A frameshift mutation in NOD2 associated with susceptibility to Crohn’s disease. Nature. 2001;411:603–606. doi: 10.1038/35079114. [DOI] [PubMed] [Google Scholar]
- 81.Cooney R., Baker J., Brain O., Danis B., Pichulik T., Allan P., Ferguson D.J., Campbell B.J., Jewell D., Simmons A. NOD2 stimulation induces autophagy in dendritic cells influencing bacterial handling and antigen presentation. Nat. Med. 2010;16:90–97. doi: 10.1038/nm.2069. [DOI] [PubMed] [Google Scholar]
- 82.Petnicki-Ocwieja T., Hrncir T., Liu Y.J., Biswas A., Hudcovic T., Tlaskalova-Hogenova H., Kobayashi K.S. Nod2 is required for the regulation of commensal microbiota in the intestine. Proc. Natl. Acad. Sci. USA. 2009;106:15813–15818. doi: 10.1073/pnas.0907722106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nigro G., Rossi R., Commere P.H., Jay P., Sansonetti P.J. The cytosolic bacterial peptidoglycan sensor Nod2 affords stem cell protection and links microbes to gut epithelial regeneration. Cell Host Microbe. 2014;15:792–798. doi: 10.1016/j.chom.2014.05.003. [DOI] [PubMed] [Google Scholar]
- 84.Grasberger H., Magis A.T., Sheng E., Conomos M.P., Zhang M., Garzotto L.S., Hou G., Bishu S., Nagao-Kitamoto H., El-Zaatari M., et al. DUOX2 variants associate with preclinical disturbances in microbiota-immune homeostasis and increased inflammatory bowel disease risk. J. Clin. Investig. 2021;131:e141676. doi: 10.1172/JCI141676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Pircalabioru G., Aviello G., Kubica M., Zhdanov A., Paclet M.H., Brennan L., Hertzberger R., Papkovsky D., Bourke B., Knaus U.G. Defensive Mutualism Rescues NADPH Oxidase Inactivation in Gut Infection. Cell Host Microbe. 2016;19:651–663. doi: 10.1016/j.chom.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 86.Venkatesh M., Mukherjee S., Wang H., Li H., Sun K., Benechet A.P., Qiu Z., Maher L., Redinbo M.R., Phillips R.S., et al. Symbiotic bacterial metabolites regulate gastrointestinal barrier function via the xenobiotic sensor PXR and Toll-like receptor 4. Immunity. 2014;41:296–310. doi: 10.1016/j.immuni.2014.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dring M.M., Goulding C.A., Trimble V.I., Keegan D., Ryan A.W., Brophy K.M., Smyth C.M., Keeling P.W., O’Donoghue D., O’Sullivan M., et al. The pregnane X receptor locus is associated with susceptibility to inflammatory bowel disease. Gastroenterology. 2006;130:341–348. doi: 10.1053/j.gastro.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 88.Martinez A., Marquez A., Mendoza J., Taxonera C., Fernandez-Arquero M., Diaz-Rubio M., de la Concha E.G., Urcelay E. Role of the PXR gene locus in inflammatory bowel diseases. Inflamm. Bowel Dis. 2007;13:1484–1487. doi: 10.1002/ibd.20252. [DOI] [PubMed] [Google Scholar]
- 89.Alvarado D.M., Chen B., Iticovici M., Thaker A.I., Dai N., VanDussen K.L., Shaikh N., Lim C.K., Guillemin G.J., Tarr P.I., et al. Epithelial Indoleamine 2,3-Dioxygenase 1 Modulates Aryl Hydrocarbon Receptor and Notch Signaling to Increase Differentiation of Secretory Cells and Alter Mucus-Associated Microbiota. Gastroenterology. 2019;157:1093–1108.e11. doi: 10.1053/j.gastro.2019.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Metidji A., Omenetti S., Crotta S., Li Y., Nye E., Ross E., Li V., Maradana M.R., Schiering C., Stockinger B. The Environmental Sensor AHR Protects from Inflammatory Damage by Maintaining Intestinal Stem Cell Homeostasis and Barrier Integrity. Immunity. 2018;49:353–362.e5. doi: 10.1016/j.immuni.2018.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Yu M., Wang Q., Ma Y., Li L., Yu K., Zhang Z., Chen G., Li X., Xiao W., Xu P., et al. Aryl Hydrocarbon Receptor Activation Modulates Intestinal Epithelial Barrier Function by Maintaining Tight Junction Integrity. Int. J. Biol. Sci. 2018;14:69–77. doi: 10.7150/ijbs.22259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Catanzaro J.R., Strauss J.D., Bielecka A., Porto A.F., Lobo F.M., Urban A., Schofield W.B., Palm N.W. IgA-deficient humans exhibit gut microbiota dysbiosis despite secretion of compensatory IgM. Sci. Rep. 2019;9:13574. doi: 10.1038/s41598-019-49923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Johansen F.E., Pekna M., Norderhaug I.N., Haneberg B., Hietala M.A., Krajci P., Betsholtz C., Brandtzaeg P. Absence of epithelial immunoglobulin A transport, with increased mucosal leakiness, in polymeric immunoglobulin receptor/secretory component-deficient mice. J. Exp. Med. 1999;190:915–922. doi: 10.1084/jem.190.7.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shimada S., Kawaguchi-Miyashita M., Kushiro A., Sato T., Nanno M., Sako T., Matsuoka Y., Sudo K., Tagawa Y., Iwakura Y., et al. Generation of polymeric immunoglobulin receptor-deficient mouse with marked reduction of secretory IgA. J. Immunol. 1999;163:5367–5373. [PubMed] [Google Scholar]
- 95.Menta P.L.R., Andrade M.E.R., Leocadio P.C.L., Fraga J.R., Dias M.T.S., Cara D.C., Cardoso V.N., Borges L.F., Capettini L.S.A., Aguilar E.C., et al. Wheat gluten intake increases the severity of experimental colitis and bacterial translocation by weakening of the proteins of the junctional complex. Br. J. Nutr. 2019;121:361–373. doi: 10.1017/S0007114518003422. [DOI] [PubMed] [Google Scholar]
- 96.Johnson R.J., Rivard C., Lanaspa M.A., Otabachian-Smith S., Ishimoto T., Cicerchi C., Cheeke P.R., Macintosh B., Hess T. Fructokinase, Fructans, Intestinal Permeability, and Metabolic Syndrome: An Equine Connection? J. Equine Vet. Sci. 2013;33:120–126. doi: 10.1016/j.jevs.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gulhane M., Murray L., Lourie R., Tong H., Sheng Y.H., Wang R., Kang A., Schreiber V., Wong K.Y., Magor G., et al. High Fat Diets Induce Colonic Epithelial Cell Stress and Inflammation that is Reversed by IL-22. Sci. Rep. 2016;6:28990. doi: 10.1038/srep28990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Devkota S., Wang Y., Musch M.W., Leone V., Fehlner-Peach H., Nadimpalli A., Antonopoulos D.A., Jabri B., Chang E.B. Dietary-fat-induced taurocholic acid promotes pathobiont expansion and colitis in Il10−/− mice. Nature. 2012;487:104–108. doi: 10.1038/nature11225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ma T.Y., Nguyen D., Bui V., Nguyen H., Hoa N. Ethanol modulation of intestinal epithelial tight junction barrier. Am. J. Physiol. 1999;276:G965–G974. doi: 10.1152/ajpgi.1999.276.4.G965. [DOI] [PubMed] [Google Scholar]
- 100.Elamin E., Jonkers D., Juuti-Uusitalo K., van Ijzendoorn S., Troost F., Duimel H., Broers J., Verheyen F., Dekker J., Masclee A. Effects of ethanol and acetaldehyde on tight junction integrity: In vitro study in a three dimensional intestinal epithelial cell culture model. PLoS ONE. 2012;7:e35008. doi: 10.1371/journal.pone.0035008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Desai M.S., Seekatz A.M., Koropatkin N.M., Kamada N., Hickey C.A., Wolter M., Pudlo N.A., Kitamoto S., Terrapon N., Muller A., et al. A Dietary Fiber-Deprived Gut Microbiota Degrades the Colonic Mucus Barrier and Enhances Pathogen Susceptibility. Cell. 2016;167:1339–1353.e21. doi: 10.1016/j.cell.2016.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Sankaran-Walters S., Hart R., Dills C. Guardians of the Gut: Enteric Defensins. Front. Microbiol. 2017;8:647. doi: 10.3389/fmicb.2017.00647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Shimizu Y., Nakamura K., Yoshii A., Yokoi Y., Kikuchi M., Shinozaki R., Nakamura S., Ohira S., Sugimoto R., Ayabe T. Paneth cell alpha-defensin misfolding correlates with dysbiosis and ileitis in Crohn’s disease model mice. Life Sci. Alliance. 2020;3:e201900592. doi: 10.26508/lsa.201900592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhou H., Zhou S.Y., Gillilland M., 3rd, Li J.Y., Lee A., Gao J., Zhang G., Xu X., Owyang C. Bile acid toxicity in Paneth cells contributes to gut dysbiosis induced by high-fat feeding. JCI Insight. 2020;5:e138881. doi: 10.1172/jci.insight.138881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Liu T.C., Kern J.T., Jain U., Sonnek N.M., Xiong S., Simpson K.F., VanDussen K.L., Winkler E.S., Haritunians T., Malique A., et al. Western diet induces Paneth cell defects through microbiome alterations and farnesoid X receptor and type I interferon activation. Cell Host Microbe. 2021;29:988–1001.e6. doi: 10.1016/j.chom.2021.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Brawner K.M., Yeramilli V.A., Duck L.W., Van Der Pol W., Smythies L.E., Morrow C.D., Elson C.O., Martin C.A. Depletion of dietary aryl hydrocarbon receptor ligands alters microbiota composition and function. Sci. Rep. 2019;9:14724. doi: 10.1038/s41598-019-51194-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Schanz O., Chijiiwa R., Cengiz S.C., Majlesain Y., Weighardt H., Takeyama H., Forster I. Dietary AhR Ligands Regulate AhRR Expression in Intestinal Immune Cells and Intestinal Microbiota Composition. Int. J. Mol. Sci. 2020;21:3189. doi: 10.3390/ijms21093189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Zhang Y.G., Wu S., Xia Y., Sun J. Salmonella infection upregulates the leaky protein claudin-2 in intestinal epithelial cells. PLoS ONE. 2013;8:e58606. doi: 10.1371/journal.pone.0058606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Fasano A., Baudry B., Pumplin D.W., Wasserman S.S., Tall B.D., Ketley J.M., Kaper J.B. Vibrio cholerae produces a second enterotoxin, which affects intestinal tight junctions. Proc. Natl. Acad. Sci. USA. 1991;88:5242–5246. doi: 10.1073/pnas.88.12.5242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Fasano A., Fiorentini C., Donelli G., Uzzau S., Kaper J.B., Margaretten K., Ding X., Guandalini S., Comstock L., Goldblum S.E. Zonula occludens toxin modulates tight junctions through protein kinase C-dependent actin reorganization, in vitro. J. Clin. Investig. 1995;96:710–720. doi: 10.1172/JCI118114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Jakobsson H.E., Rodriguez-Pineiro A.M., Schutte A., Ermund A., Boysen P., Bemark M., Sommer F., Backhed F., Hansson G.C., Johansson M.E. The composition of the gut microbiota shapes the colon mucus barrier. EMBO Rep. 2015;16:164–177. doi: 10.15252/embr.201439263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Feng Y., Huang Y., Wang Y., Wang P., Song H., Wang F. Antibiotics induced intestinal tight junction barrier dysfunction is associated with microbiota dysbiosis, activated NLRP3 inflammasome and autophagy. PLoS ONE. 2019;14:e0218384. doi: 10.1371/journal.pone.0218384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sharma R., Young C., Neu J. Molecular modulation of intestinal epithelial barrier: Contribution of microbiota. J. Biomed. Biotechnol. 2010;2010:305879. doi: 10.1155/2010/305879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.van der Flier L.G., Clevers H. Stem cells, self-renewal, and differentiation in the intestinal epithelium. Annu. Rev. Physiol. 2009;71:241–260. doi: 10.1146/annurev.physiol.010908.163145. [DOI] [PubMed] [Google Scholar]
- 115.Beumer J., Clevers H. Cell fate specification and differentiation in the adult mammalian intestine. Nat. Rev. Mol. Cell Biol. 2021;22:39–53. doi: 10.1038/s41580-020-0278-0. [DOI] [PubMed] [Google Scholar]
- 116.Fre S., Huyghe M., Mourikis P., Robine S., Louvard D., Artavanis-Tsakonas S. Notch signals control the fate of immature progenitor cells in the intestine. Nature. 2005;435:964–968. doi: 10.1038/nature03589. [DOI] [PubMed] [Google Scholar]
- 117.Calon A., Gross I., Lhermitte B., Martin E., Beck F., Duclos B., Kedinger M., Duluc I., Domon-Dell C., Freund J.N. Different effects of the Cdx1 and Cdx2 homeobox genes in a murine model of intestinal inflammation. Gut. 2007;56:1688–1695. doi: 10.1136/gut.2007.125542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Mesquita P., Jonckheere N., Almeida R., Ducourouble M.P., Serpa J., Silva E., Pigny P., Silva F.S., Reis C., Silberg D., et al. Human MUC2 mucin gene is transcriptionally regulated by Cdx homeodomain proteins in gastrointestinal carcinoma cell lines. J. Biol. Chem. 2003;278:51549–51556. doi: 10.1074/jbc.M309019200. [DOI] [PubMed] [Google Scholar]
- 119.Lorentz O., Duluc I., Arcangelis A.D., Simon-Assmann P., Kedinger M., Freund J.N. Key role of the Cdx2 homeobox gene in extracellular matrix-mediated intestinal cell differentiation. J. Cell Biol. 1997;139:1553–1565. doi: 10.1083/jcb.139.6.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hinoi T., Lucas P.C., Kuick R., Hanash S., Cho K.R., Fearon E.R. CDX2 regulates liver intestine-cadherin expression in normal and malignant colon epithelium and intestinal metaplasia. Gastroenterology. 2002;123:1565–1577. doi: 10.1053/gast.2002.36598. [DOI] [PubMed] [Google Scholar]
- 121.Keller M.S., Ezaki T., Guo R.J., Lynch J.P. Cdx1 or Cdx2 expression activates E-cadherin-mediated cell-cell adhesion and compaction in human COLO 205 cells. Am. J. Physiol. Gastrointest. Liver Physiol. 2004;287:G104–G114. doi: 10.1152/ajpgi.00484.2003. [DOI] [PubMed] [Google Scholar]
- 122.Morrisey E.E., Ip H.S., Lu M.M., Parmacek M.S. GATA-6: A zinc finger transcription factor that is expressed in multiple cell lineages derived from lateral mesoderm. Dev. Biol. 1996;177:309–322. doi: 10.1006/dbio.1996.0165. [DOI] [PubMed] [Google Scholar]
- 123.Menard S., Cerf-Bensussan N., Heyman M. Multiple facets of intestinal permeability and epithelial handling of dietary antigens. Mucosal Immunol. 2010;3:247–259. doi: 10.1038/mi.2010.5. [DOI] [PubMed] [Google Scholar]
- 124.Schneeberger E.E., Lynch R.D. Structure, function, and regulation of cellular tight junctions. Am. J. Physiol. 1992;262:L647–L661. doi: 10.1152/ajplung.1992.262.6.L647. [DOI] [PubMed] [Google Scholar]
- 125.Gumbiner B.M. Breaking through the tight junction barrier. J. Cell Biol. 1993;123:1631–1633. doi: 10.1083/jcb.123.6.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tsukita S., Furuse M. The structure and function of claudins, cell adhesion molecules at tight junctions. Ann. N. Y. Acad. Sci. 2000;915:129–135. doi: 10.1111/j.1749-6632.2000.tb05235.x. [DOI] [PubMed] [Google Scholar]
- 127.Harhaj N.S., Antonetti D.A. Regulation of tight junctions and loss of barrier function in pathophysiology. Int. J. Biochem. Cell Biol. 2004;36:1206–1237. doi: 10.1016/j.biocel.2003.08.007. [DOI] [PubMed] [Google Scholar]
- 128.Hartsock A., Nelson W.J. Adherens and tight junctions: Structure, function and connections to the actin cytoskeleton. Biochim. Et Biophys. Acta. 2008;1778:660–669. doi: 10.1016/j.bbamem.2007.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Clemente M.G., De Virgiliis S., Kang J.S., Macatagney R., Musu M.P., Di Pierro M.R., Drago S., Congia M., Fasano A. Early effects of gliadin on enterocyte intracellular signalling involved in intestinal barrier function. Gut. 2003;52:218–223. doi: 10.1136/gut.52.2.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Tripathi A., Lammers K.M., Goldblum S., Shea-Donohue T., Netzel-Arnett S., Buzza M.S., Antalis T.M., Vogel S.N., Zhao A., Yang S., et al. Identification of human zonulin, a physiological modulator of tight junctions, as prehaptoglobin-2. Proc. Natl. Acad. Sci. USA. 2009;106:16799–16804. doi: 10.1073/pnas.0906773106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zeissig S., Burgel N., Gunzel D., Richter J., Mankertz J., Wahnschaffe U., Kroesen A.J., Zeitz M., Fromm M., Schulzke J.D. Changes in expression and distribution of claudin 2, 5 and 8 lead to discontinuous tight junctions and barrier dysfunction in active Crohn’s disease. Gut. 2007;56:61–72. doi: 10.1136/gut.2006.094375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kucharzik T., Walsh S.V., Chen J., Parkos C.A., Nusrat A. Neutrophil transmigration in inflammatory bowel disease is associated with differential expression of epithelial intercellular junction proteins. Am. J. Pathol. 2001;159:2001–2009. doi: 10.1016/S0002-9440(10)63051-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Dhawan P., Ahmad R., Chaturvedi R., Smith J.J., Midha R., Mittal M.K., Krishnan M., Chen X., Eschrich S., Yeatman T.J., et al. Claudin-2 expression increases tumorigenicity of colon cancer cells: Role of epidermal growth factor receptor activation. Oncogene. 2011;30:3234–3247. doi: 10.1038/onc.2011.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Damci T., Nuhoglu I., Devranoglu G., Osar Z., Demir M., Ilkova H. Increased intestinal permeability as a cause of fluctuating postprandial blood glucose levels in Type 1 diabetic patients. Eur. J. Clin. Investig. 2003;33:397–401. doi: 10.1046/j.1365-2362.2003.01161.x. [DOI] [PubMed] [Google Scholar]
- 135.Carratu R., Secondulfo M., de Magistris L., Iafusco D., Urio A., Carbone M.G., Pontoni G., Carteni M., Prisco F. Altered intestinal permeability to mannitol in diabetes mellitus type I. J. Pediatric Gastroenterol. Nutr. 1999;28:264–269. doi: 10.1097/00005176-199903000-00010. [DOI] [PubMed] [Google Scholar]
- 136.Khoshbin K., Camilleri M. Effects of dietary components on intestinal permeability in health and disease. Am. J. Physiol. Gastrointest. Liver Physiol. 2020;319:G589–G608. doi: 10.1152/ajpgi.00245.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Johansson M.E., Sjovall H., Hansson G.C. The gastrointestinal mucus system in health and disease. Nat. Rev. Gastroenterol. Hepatol. 2013;10:352–361. doi: 10.1038/nrgastro.2013.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Johansson M.E., Ambort D., Pelaseyed T., Schutte A., Gustafsson J.K., Ermund A., Subramani D.B., Holmen-Larsson J.M., Thomsson K.A., Bergstrom J.H., et al. Composition and functional role of the mucus layers in the intestine. Cell. Mol. Life Sci. CMLS. 2011;68:3635–3641. doi: 10.1007/s00018-011-0822-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Arike L., Hansson G.C. The Densely O-Glycosylated MUC2 Mucin Protects the Intestine and Provides Food for the Commensal Bacteria. J. Mol. Biol. 2016;428:3221–3229. doi: 10.1016/j.jmb.2016.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ayabe T., Satchell D.P., Wilson C.L., Parks W.C., Selsted M.E., Ouellette A.J. Secretion of microbicidal alpha-defensins by intestinal Paneth cells in response to bacteria. Nat. Immunol. 2000;1:113–118. doi: 10.1038/77783. [DOI] [PubMed] [Google Scholar]
- 141.Ouellette A.J. Paneth cells and innate immunity in the crypt microenvironment. Gastroenterology. 1997;113:1779–1784. doi: 10.1053/gast.1997.v113.pm9352884. [DOI] [PubMed] [Google Scholar]
- 142.Wells J.M., Rossi O., Meijerink M., van Baarlen P. Epithelial crosstalk at the microbiota-mucosal interface. Proc. Natl. Acad. Sci. USA. 2011;108((Suppl. 1)):4607–4614. doi: 10.1073/pnas.1000092107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Burgueno J.F., Abreu M.T. Epithelial Toll-like receptors and their role in gut homeostasis and disease. Nat. Rev. Gastroenterol. Hepatol. 2020;17:263–278. doi: 10.1038/s41575-019-0261-4. [DOI] [PubMed] [Google Scholar]
- 144.Nighot M., Rawat M., Al-Sadi R., Castillo E.F., Nighot P., Ma T.Y. Lipopolysaccharide-Induced Increase in Intestinal Permeability Is Mediated by TAK-1 Activation of IKK and MLCK/MYLK Gene. Am. J. Pathol. 2019;189:797–812. doi: 10.1016/j.ajpath.2018.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Burgueno J.F., Fritsch J., Gonzalez E.E., Landau K.S., Santander A.M., Fernandez I., Hazime H., Davies J.M., Santaolalla R., Phillips M.C., et al. Epithelial TLR4 Signaling Activates DUOX2 to Induce Microbiota-Driven Tumorigenesis. Gastroenterology. 2021;160:797–808.e6. doi: 10.1053/j.gastro.2020.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.He B., Xu W., Santini P.A., Polydorides A.D., Chiu A., Estrella J., Shan M., Chadburn A., Villanacci V., Plebani A., et al. Intestinal bacteria trigger T cell-independent immunoglobulin A(2) class switching by inducing epithelial-cell secretion of the cytokine APRIL. Immunity. 2007;26:812–826. doi: 10.1016/j.immuni.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 147.Cario E., Gerken G., Podolsky D.K. Toll-like receptor 2 controls mucosal inflammation by regulating epithelial barrier function. Gastroenterology. 2007;132:1359–1374. doi: 10.1053/j.gastro.2007.02.056. [DOI] [PubMed] [Google Scholar]
- 148.Cario E., Gerken G., Podolsky D.K. Toll-like receptor 2 enhances ZO-1-associated intestinal epithelial barrier integrity via protein kinase C. Gastroenterology. 2004;127:224–238. doi: 10.1053/j.gastro.2004.04.015. [DOI] [PubMed] [Google Scholar]
- 149.Podolsky D.K., Gerken G., Eyking A., Cario E. Colitis-associated variant of TLR2 causes impaired mucosal repair because of TFF3 deficiency. Gastroenterology. 2009;137:209–220. doi: 10.1053/j.gastro.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Xiao H., Gulen M.F., Qin J., Yao J., Bulek K., Kish D., Altuntas C.Z., Wald D., Ma C., Zhou H., et al. The Toll-interleukin-1 receptor member SIGIRR regulates colonic epithelial homeostasis, inflammation, and tumorigenesis. Immunity. 2007;26:461–475. doi: 10.1016/j.immuni.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 151.Werts C., Rubino S., Ling A., Girardin S.E., Philpott D.J. Nod-like receptors in intestinal homeostasis, inflammation, and cancer. J. Leukoc. Biol. 2011;90:471–482. doi: 10.1189/jlb.0411183. [DOI] [PubMed] [Google Scholar]
- 152.Claes A.K., Zhou J.Y., Philpott D.J. NOD-Like Receptors: Guardians of Intestinal Mucosal Barriers. Physiology. 2015;30:241–250. doi: 10.1152/physiol.00025.2014. [DOI] [PubMed] [Google Scholar]
- 153.Grasberger H., Gao J., Nagao-Kitamoto H., Kitamoto S., Zhang M., Kamada N., Eaton K.A., El-Zaatari M., Shreiner A.B., Merchant J.L., et al. Increased Expression of DUOX2 Is an Epithelial Response to Mucosal Dysbiosis Required for Immune Homeostasis in Mouse Intestine. Gastroenterology. 2015;149:1849–1859. doi: 10.1053/j.gastro.2015.07.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Lambeth J.D., Neish A.S. Nox enzymes and new thinking on reactive oxygen: A double-edged sword revisited. Annu. Rev. Pathol. 2014;9:119–145. doi: 10.1146/annurev-pathol-012513-104651. [DOI] [PubMed] [Google Scholar]
- 155.Lipinski S., Till A., Sina C., Arlt A., Grasberger H., Schreiber S., Rosenstiel P. DUOX2-derived reactive oxygen species are effectors of NOD2-mediated antibacterial responses. J. Cell Sci. 2009;122:3522–3530. doi: 10.1242/jcs.050690. [DOI] [PubMed] [Google Scholar]
- 156.Botteaux A., Hoste C., Dumont J.E., Van Sande J., Allaoui A. Potential role of Noxes in the protection of mucosae: H2O2 as a bacterial repellent. Microbes Infect. 2009;11:537–544. doi: 10.1016/j.micinf.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 157.Corcionivoschi N., Alvarez L.A., Sharp T.H., Strengert M., Alemka A., Mantell J., Verkade P., Knaus U.G., Bourke B. Mucosal reactive oxygen species decrease virulence by disrupting Campylobacter jejuni phosphotyrosine signaling. Cell Host Microbe. 2012;12:47–59. doi: 10.1016/j.chom.2012.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Chu F.F., Esworthy R.S., Doroshow J.H., Grasberger H., Donko A., Leto T.L., Gao Q., Shen B. Deficiency in Duox2 activity alleviates ileitis in GPx1- and GPx2-knockout mice without affecting apoptosis incidence in the crypt epithelium. Redox Biol. 2017;11:144–156. doi: 10.1016/j.redox.2016.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.MacFie T.S., Poulsom R., Parker A., Warnes G., Boitsova T., Nijhuis A., Suraweera N., Poehlmann A., Szary J., Feakins R., et al. DUOX2 and DUOXA2 form the predominant enzyme system capable of producing the reactive oxygen species H2O2 in active ulcerative colitis and are modulated by 5-aminosalicylic acid. Inflamm. Bowel Dis. 2014;20:514–524. doi: 10.1097/01.MIB.0000442012.45038.0e. [DOI] [PubMed] [Google Scholar]
- 160.Haberman Y., Tickle T.L., Dexheimer P.J., Kim M.O., Tang D., Karns R., Baldassano R.N., Noe J.D., Rosh J., Markowitz J., et al. Pediatric Crohn disease patients exhibit specific ileal transcriptome and microbiome signature. J. Clin. Investig. 2014;124:3617–3633. doi: 10.1172/JCI75436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hayes P., Dhillon S., O’Neill K., Thoeni C., Hui K.Y., Elkadri A., Guo C.H., Kovacic L., Aviello G., Alvarez L.A., et al. Defects in NADPH Oxidase Genes NOX1 and DUOX2 in Very Early Onset Inflammatory Bowel Disease. Cell. Mol. Gastroenterol. Hepatol. 2015;1:489–502. doi: 10.1016/j.jcmgh.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Cheng J., Shah Y.M., Gonzalez F.J. Pregnane X receptor as a target for treatment of inflammatory bowel disorders. Trends Pharmacol. Sci. 2012;33:323–330. doi: 10.1016/j.tips.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Gao J., Xie W. Pregnane X receptor and constitutive androstane receptor at the crossroads of drug metabolism and energy metabolism. Drug Metab. Dispos. Biol. Fate Chem. 2010;38:2091–2095. doi: 10.1124/dmd.110.035568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Frericks M., Meissner M., Esser C. Microarray analysis of the AHR system: Tissue-specific flexibility in signal and target genes. Toxicol. Appl. Pharmacol. 2007;220:320–332. doi: 10.1016/j.taap.2007.01.014. [DOI] [PubMed] [Google Scholar]
- 165.Terc J., Hansen A., Alston L., Hirota S.A. Pregnane X receptor agonists enhance intestinal epithelial wound healing and repair of the intestinal barrier following the induction of experimental colitis. Eur. J. Pharm. Sci. Off. J. Eur. Fed. Pharm. Sci. 2014;55:12–19. doi: 10.1016/j.ejps.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 166.Stockinger B., Shah K., Wincent E. AHR in the intestinal microenvironment: Safeguarding barrier function. Nat. Rev. Gastroenterol. Hepatol. 2021;18:559–570. doi: 10.1038/s41575-021-00430-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Chen Y., Tang Y., Guo C., Wang J., Boral D., Nie D. Nuclear receptors in the multidrug resistance through the regulation of drug-metabolizing enzymes and drug transporters. Biochem. Pharmacol. 2012;83:1112–1126. doi: 10.1016/j.bcp.2012.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Satsu H., Hiura Y., Mochizuki K., Hamada M., Shimizu M. Activation of pregnane X receptor and induction of MDR1 by dietary phytochemicals. J. Agric. Food Chem. 2008;56:5366–5373. doi: 10.1021/jf073350e. [DOI] [PubMed] [Google Scholar]
- 169.Ren Y., Yue B., Ren G., Yu Z., Luo X., Sun A., Zhang J., Han M., Wang Z., Dou W. Activation of PXR by alantolactone ameliorates DSS-induced experimental colitis via suppressing NF-kappaB signaling pathway. Sci. Rep. 2019;9:16636. doi: 10.1038/s41598-019-53305-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Shah Y.M., Ma X., Morimura K., Kim I., Gonzalez F.J. Pregnane X receptor activation ameliorates DSS-induced inflammatory bowel disease via inhibition of NF-kappaB target gene expression. Am. J. Physiol. Gastrointest. Liver Physiol. 2007;292:G1114–G1122. doi: 10.1152/ajpgi.00528.2006. [DOI] [PubMed] [Google Scholar]
- 171.Garg A., Zhao A., Erickson S.L., Mukherjee S., Lau A.J., Alston L., Chang T.K., Mani S., Hirota S.A. Pregnane X Receptor Activation Attenuates Inflammation-Associated Intestinal Epithelial Barrier Dysfunction by Inhibiting Cytokine-Induced Myosin Light-Chain Kinase Expression and c-Jun N-Terminal Kinase 1/2 Activation. J. Pharmacol. Exp. Ther. 2016;359:91–101. doi: 10.1124/jpet.116.234096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hankinson O. The aryl hydrocarbon receptor complex. Annu. Rev. Pharmacol. Toxicol. 1995;35:307–340. doi: 10.1146/annurev.pa.35.040195.001515. [DOI] [PubMed] [Google Scholar]
- 173.Mulero-Navarro S., Fernandez-Salguero P.M. New Trends in Aryl Hydrocarbon Receptor Biology. Front. Cell Dev. Biol. 2016;4:45. doi: 10.3389/fcell.2016.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Lee J.S., Cella M., McDonald K.G., Garlanda C., Kennedy G.D., Nukaya M., Mantovani A., Kopan R., Bradfield C.A., Newberry R.D., et al. AHR drives the development of gut ILC22 cells and postnatal lymphoid tissues via pathways dependent on and independent of Notch. Nat. Immunol. 2011;13:144–151. doi: 10.1038/ni.2187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Schiering C., Wincent E., Metidji A., Iseppon A., Li Y., Potocnik A.J., Omenetti S., Henderson C.J., Wolf C.R., Nebert D.W., et al. Feedback control of AHR signalling regulates intestinal immunity. Nature. 2017;542:242–245. doi: 10.1038/nature21080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Scott S.A., Fu J., Chang P.V. Microbial tryptophan metabolites regulate gut barrier function via the aryl hydrocarbon receptor. Proc. Natl. Acad. Sci. USA. 2020;117:19376–19387. doi: 10.1073/pnas.2000047117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Marinelli L., Martin-Gallausiaux C., Bourhis J.M., Beguet-Crespel F., Blottiere H.M., Lapaque N. Identification of the novel role of butyrate as AhR ligand in human intestinal epithelial cells. Sci. Rep. 2019;9:643. doi: 10.1038/s41598-018-37019-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Fagarasan S., Honjo T. Intestinal IgA synthesis: Regulation of front-line body defences. Nat. Rev. Immunol. 2003;3:63–72. doi: 10.1038/nri982. [DOI] [PubMed] [Google Scholar]
- 179.Corthesy B. Multi-faceted functions of secretory IgA at mucosal surfaces. Front. Immunol. 2013;4:185. doi: 10.3389/fimmu.2013.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Pabst O., Slack E. IgA and the intestinal microbiota: The importance of being specific. Mucosal Immunol. 2020;13:12–21. doi: 10.1038/s41385-019-0227-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Suzuki K. Diversified IgA-Bacteria Interaction in Gut Homeostasis. Adv. Exp. Med. Biol. 2020;1254:105–116. doi: 10.1007/978-981-15-3532-1_9. [DOI] [PubMed] [Google Scholar]
- 182.Turula H., Wobus C.E. The Role of the Polymeric Immunoglobulin Receptor and Secretory Immunoglobulins during Mucosal Infection and Immunity. Viruses. 2018;10:237. doi: 10.3390/v10050237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Johansen F.E., Kaetzel C.S. Regulation of the polymeric immunoglobulin receptor and IgA transport: New advances in environmental factors that stimulate pIgR expression and its role in mucosal immunity. Mucosal Immunol. 2011;4:598–602. doi: 10.1038/mi.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Mantis N.J., Rol N., Corthesy B. Secretory IgA’s complex roles in immunity and mucosal homeostasis in the gut. Mucosal Immunol. 2011;4:603–611. doi: 10.1038/mi.2011.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Diana J., Moura I.C., Vaugier C., Gestin A., Tissandie E., Beaudoin L., Corthesy B., Hocini H., Lehuen A., Monteiro R.C. Secretory IgA induces tolerogenic dendritic cells through SIGNR1 dampening autoimmunity in mice. J. Immunol. 2013;191:2335–2343. doi: 10.4049/jimmunol.1300864. [DOI] [PubMed] [Google Scholar]
- 186.Baumann J., Park C.G., Mantis N.J. Recognition of secretory IgA by DC-SIGN: Implications for immune surveillance in the intestine. Immunol. Lett. 2010;131:59–66. doi: 10.1016/j.imlet.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ludvigsson J.F., Neovius M., Hammarstrom L. Association between IgA deficiency & other autoimmune conditions: A population-based matched cohort study. J. Clin. Immunol. 2014;34:444–451. doi: 10.1007/s10875-014-0009-4. [DOI] [PubMed] [Google Scholar]
- 188.Aghamohammadi A., Cheraghi T., Gharagozlou M., Movahedi M., Rezaei N., Yeganeh M., Parvaneh N., Abolhassani H., Pourpak Z., Moin M. IgA deficiency: Correlation between clinical and immunological phenotypes. J. Clin. Immunol. 2009;29:130–136. doi: 10.1007/s10875-008-9229-9. [DOI] [PubMed] [Google Scholar]
- 189.Reikvam D.H., Derrien M., Islam R., Erofeev A., Grcic V., Sandvik A., Gaustad P., Meza-Zepeda L.A., Jahnsen F.L., Smidt H., et al. Epithelial-microbial crosstalk in polymeric Ig receptor deficient mice. Eur. J. Immunol. 2012;42:2959–2970. doi: 10.1002/eji.201242543. [DOI] [PubMed] [Google Scholar]
- 190.Kato-Nagaoka N., Shimada S., Yamakawa Y., Tsujibe S., Naito T., Setoyama H., Watanabe Y., Shida K., Matsumoto S., Nanno M. Enhanced differentiation of intraepithelial lymphocytes in the intestine of polymeric immunoglobulin receptor-deficient mice. Immunology. 2015;146:59–69. doi: 10.1111/imm.12480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Yamazaki K., Shimada S., Kato-Nagaoka N., Soga H., Itoh T., Nanno M. Accumulation of intestinal intraepithelial lymphocytes in association with lack of polymeric immunoglobulin receptor. Eur. J. Immunol. 2005;35:1211–1219. doi: 10.1002/eji.200425627. [DOI] [PubMed] [Google Scholar]
- 192.Uren T.K., Johansen F.E., Wijburg O.L., Koentgen F., Brandtzaeg P., Strugnell R.A. Role of the polymeric Ig receptor in mucosal B cell homeostasis. J. Immunol. 2003;170:2531–2539. doi: 10.4049/jimmunol.170.5.2531. [DOI] [PubMed] [Google Scholar]
- 193.Manichanh C., Rigottier-Gois L., Bonnaud E., Gloux K., Pelletier E., Frangeul L., Nalin R., Jarrin C., Chardon P., Marteau P., et al. Reduced diversity of faecal microbiota in Crohn’s disease revealed by a metagenomic approach. Gut. 2006;55:205–211. doi: 10.1136/gut.2005.073817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Frank D.N., St Amand A.L., Feldman R.A., Boedeker E.C., Harpaz N., Pace N.R. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc. Natl. Acad. Sci. USA. 2007;104:13780–13785. doi: 10.1073/pnas.0706625104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Halfvarson J., Brislawn C.J., Lamendella R., Vazquez-Baeza Y., Walters W.A., Bramer L.M., D’Amato M., Bonfiglio F., McDonald D., Gonzalez A., et al. Dynamics of the human gut microbiome in inflammatory bowel disease. Nat. Microbiol. 2017;2:17004. doi: 10.1038/nmicrobiol.2017.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Lloyd-Price J., Arze C., Ananthakrishnan A.N., Schirmer M., Avila-Pacheco J., Poon T.W., Andrews E., Ajami N.J., Bonham K.S., Brislawn C.J., et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature. 2019;569:655–662. doi: 10.1038/s41586-019-1237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Schirmer M., Franzosa E.A., Lloyd-Price J., McIver L.J., Schwager R., Poon T.W., Ananthakrishnan A.N., Andrews E., Barron G., Lake K., et al. Dynamics of metatranscription in the inflammatory bowel disease gut microbiome. Nat. Microbiol. 2018;3:337–346. doi: 10.1038/s41564-017-0089-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Yachida S., Mizutani S., Shiroma H., Shiba S., Nakajima T., Sakamoto T., Watanabe H., Masuda K., Nishimoto Y., Kubo M., et al. Metagenomic and metabolomic analyses reveal distinct stage-specific phenotypes of the gut microbiota in colorectal cancer. Nat. Med. 2019;25:968–976. doi: 10.1038/s41591-019-0458-7. [DOI] [PubMed] [Google Scholar]
- 199.Erickson A.R., Cantarel B.L., Lamendella R., Darzi Y., Mongodin E.F., Pan C., Shah M., Halfvarson J., Tysk C., Henrissat B., et al. Integrated metagenomics/metaproteomics reveals human host-microbiota signatures of Crohn’s disease. PLoS ONE. 2012;7:e49138. doi: 10.1371/journal.pone.0049138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Heintz-Buschart A., May P., Laczny C.C., Lebrun L.A., Bellora C., Krishna A., Wampach L., Schneider J.G., Hogan A., de Beaufort C., et al. Integrated multi-omics of the human gut microbiome in a case study of familial type 1 diabetes. Nat. Microbiol. 2016;2:16180. doi: 10.1038/nmicrobiol.2016.180. [DOI] [PubMed] [Google Scholar]
- 201.Martinez C., Antolin M., Santos J., Torrejon A., Casellas F., Borruel N., Guarner F., Malagelada J.R. Unstable composition of the fecal microbiota in ulcerative colitis during clinical remission. Am. J. Gastroenterol. 2008;103:643–648. doi: 10.1111/j.1572-0241.2007.01592.x. [DOI] [PubMed] [Google Scholar]
- 202.Rajca S., Grondin V., Louis E., Vernier-Massouille G., Grimaud J.C., Bouhnik Y., Laharie D., Dupas J.L., Pillant H., Picon L., et al. Alterations in the intestinal microbiome (dysbiosis) as a predictor of relapse after infliximab withdrawal in Crohn’s disease. Inflamm. Bowel Dis. 2014;20:978–986. doi: 10.1097/MIB.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 203.Yu J., Feng Q., Wong S.H., Zhang D., Liang Q.Y., Qin Y., Tang L., Zhao H., Stenvang J., Li Y., et al. Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut. 2017;66:70–78. doi: 10.1136/gutjnl-2015-309800. [DOI] [PubMed] [Google Scholar]
- 204.Li H., Christman L.M., Li R., Gu L. Synergic interactions between polyphenols and gut microbiota in mitigating inflammatory bowel diseases. Food Funct. 2020;11:4878–4891. doi: 10.1039/D0FO00713G. [DOI] [PubMed] [Google Scholar]
- 205.Vezza T., Rodriguez-Nogales A., Algieri F., Utrilla M.P., Rodriguez-Cabezas M.E., Galvez J. Flavonoids in Inflammatory Bowel Disease: A Review. Nutrients. 2016;8:211. doi: 10.3390/nu8040211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Li M., Weigmann B. A Novel Pathway of Flavonoids Protecting against Inflammatory Bowel Disease: Modulating Enteroendocrine System. Metabolites. 2022;12:31. doi: 10.3390/metabo12010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Lei H., Crawford M.S., McCole D.F. JAK-STAT Pathway Regulation of Intestinal Permeability: Pathogenic Roles and Therapeutic Opportunities in Inflammatory Bowel Disease. Pharmaceuticals. 2021;14:840. doi: 10.3390/ph14090840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Wagenaar C.A., van de Put M., Bisschops M., Walrabenstein W., de Jonge C.S., Herrema H., van Schaardenburg D. The Effect of Dietary Interventions on Chronic Inflammatory Diseases in Relation to the Microbiome: A Systematic Review. Nutrients. 2021;13:3208. doi: 10.3390/nu13093208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Wark G., Samocha-Bonet D., Ghaly S., Danta M. The Role of Diet in the Pathogenesis and Management of Inflammatory Bowel Disease: A Review. Nutrients. 2020;13:135. doi: 10.3390/nu13010135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.De Filippo C., Cavalieri D., Di Paola M., Ramazzotti M., Poullet J.B., Massart S., Collini S., Pieraccini G., Lionetti P. Impact of diet in shaping gut microbiota revealed by a comparative study in children from Europe and rural Africa. Proc. Natl. Acad. Sci. USA. 2010;107:14691–14696. doi: 10.1073/pnas.1005963107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Tomova A., Bukovsky I., Rembert E., Yonas W., Alwarith J., Barnard N.D., Kahleova H. The Effects of Vegetarian and Vegan Diets on Gut Microbiota. Front. Nutr. 2019;6:47. doi: 10.3389/fnut.2019.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Singh R.K., Chang H.W., Yan D., Lee K.M., Ucmak D., Wong K., Abrouk M., Farahnik B., Nakamura M., Zhu T.H., et al. Influence of diet on the gut microbiome and implications for human health. J. Transl. Med. 2017;15:73. doi: 10.1186/s12967-017-1175-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.De Filippis F., Pellegrini N., Vannini L., Jeffery I.B., La Storia A., Laghi L., Serrazanetti D.I., Di Cagno R., Ferrocino I., Lazzi C., et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016;65:1812–1821. doi: 10.1136/gutjnl-2015-309957. [DOI] [PubMed] [Google Scholar]
- 214.Sultan S., El-Mowafy M., Elgaml A., Ahmed T.A.E., Hassan H., Mottawea W. Metabolic Influences of Gut Microbiota Dysbiosis on Inflammatory Bowel Disease. Front. Physiol. 2021;12:715506. doi: 10.3389/fphys.2021.715506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Sandberg J.W., Lau C., Jacomino M., Finegold M., Henning S.J. Improving access to intestinal stem cells as a step toward intestinal gene transfer. Hum. Gene Ther. 1994;5:323–329. doi: 10.1089/hum.1994.5.3-323. [DOI] [PubMed] [Google Scholar]
- 216.Ferrari S., Kitson C., Farley R., Steel R., Marriott C., Parkins D.A., Scarpa M., Wainwright B., Evans M.J., Colledge W.H., et al. Mucus altering agents as adjuncts for nonviral gene transfer to airway epithelium. Gene Ther. 2001;8:1380–1386. doi: 10.1038/sj.gt.3301525. [DOI] [PubMed] [Google Scholar]
- 217.Pickles R.J., Fahrner J.A., Petrella J.M., Boucher R.C., Bergelson J.M. Retargeting the coxsackievirus and adenovirus receptor to the apical surface of polarized epithelial cells reveals the glycocalyx as a barrier to adenovirus-mediated gene transfer. J. Virol. 2000;74:6050–6057. doi: 10.1128/JVI.74.13.6050-6057.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Matsumoto H., Kimura T., Haga K., Kasahara N., Anton P., McGowan I. Effective in vivo and ex vivo gene transfer to intestinal mucosa by VSV-G-pseudotyped lentiviral vectors. BMC Gastroenterol. 2010;10:44. doi: 10.1186/1471-230X-10-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Matsumoto H., Haga K., Ohno I., Hiraoka K., Kimura T., Hermann K., Kasahara N., Anton P., McGowan I. Mucosal gene therapy using a pseudotyped lentivirus vector encoding murine interleukin-10 (mIL-10) suppresses the development and relapse of experimental murine colitis. BMC Gastroenterol. 2014;14:68. doi: 10.1186/1471-230X-14-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Lindsay J., Van Montfrans C., Brennan F., Van Deventer S., Drillenburg P., Hodgson H., Te Velde A., Sol Rodriguez Pena M. IL-10 gene therapy prevents TNBS-induced colitis. Gene Ther. 2002;9:1715–1721. doi: 10.1038/sj.gt.3301841. [DOI] [PubMed] [Google Scholar]
- 221.Buckinx R., Timmermans J.P. Targeting the gastrointestinal tract with viral vectors: State of the art and possible applications in research and therapy. Histochem. Cell Biol. 2016;146:709–720. doi: 10.1007/s00418-016-1496-6. [DOI] [PubMed] [Google Scholar]
- 222.Wirtz S., Galle P.R., Neurath M.F. Efficient gene delivery to the inflamed colon by local administration of recombinant adenoviruses with normal or modified fibre structure. Gut. 1999;44:800–807. doi: 10.1136/gut.44.6.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Kovalenko P.L., Yuan L., Sun K., Kunovska L., Seregin S., Amalfitano A., Basson M.D. Regulation of epithelial differentiation in rat intestine by intraluminal delivery of an adenoviral vector or silencing RNA coding for Schlafen 3. PLoS ONE. 2013;8:e79745. doi: 10.1371/journal.pone.0079745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Brown G.R., Thiele D.L., Silva M., Beutler B. Adenoviral vectors given intravenously to immunocompromised mice yield stable transduction of the colonic epithelium. Gastroenterology. 1997;112:1586–1594. doi: 10.1016/S0016-5085(97)70040-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.