Abstract
Previous research has found elevated levels of psychological distress (i.e., post-traumatic stress, depressive and anxiety symptoms) among veterans. Existing theory and evidence show how psychological distress is associated with marital disruptions. Only a few studies, however, have tested the link between psychological distress and couple communication quality in military couples, most of which were cross-sectional and employed self-report measures. The current study investigated whether psychological distress predicts changes in observed communication quality across one year in 228 couples consisting of male service members, who were deployed to Iraq and/or Afghanistan, and their non-deployed female partners. Psychological distress was indicated by self-reported post-traumatic stress disorder, depressive, and anxiety symptoms. Communication quality was assessed using observed couple interactions. The results of an actor-partner interdependence model showed that men’s psychological distress predicted men’s lower communication quality at one year after accounting for baseline communication quality. Women’s psychological distress did not predict their communication quality, and each partner’s psychological distress did not predict changes in their partner’s communication quality over time. Consistent with previous findings on civilian populations, our findings highlight the long-term effects of psychological distress among service members on their communication behaviors with their intimate partners, and emphasize the importance of targeting psychological symptoms of service members following deployment to war.
Keywords: Psychological distress, couple communication, actor-partner interdependence model, deployment
Introduction
Since 2001, over two million American soldiers, of whom nearly half are married, have experienced prolonged and repeated deployments to war zones in the Middle East (Department of Defense, 2015). Despite the idealized images of happy reunions after deployment, some military couples may deal with mental health issues associated with exposure to combat trauma (Milliken, Auchterlonie, & Hoge, 2007). For example, a 3-year prospective study showed that service members who experienced deployment trauma showed an increase in psychological distress, including post-traumatic stress disorder (PTSD), depressive and anxiety symptoms, from pre- to post-deployment (Meadows et al., 2016). These symptoms may persist even after deployment. Prospective data from a large group of National Guard/Reserve (NG/R) soldiers showed increases in post-traumatic stress symptoms (PTSS) and depressive symptoms from three to twelve months after the initial return; the proportion of individuals meeting criteria for PTSD increased from 21.5% to 30.5%, and rates of depressive symptoms increased from 11.5% to 15.9% (Thomas et al., 2010).
PTSD is one of the most common mental disorders among US veterans (Wisco et al., 2014), and it is likely to co-occur with depressive and anxiety symptoms (Smith, Goldstein, & Grant, 2016), especially in military populations (Rytwinski, Scur, Feeny, & Youngstrom, 2013). In fact, the highest rates of comorbidity for probable lifetime PTSD in US veterans were with major depression (72%) and anxiety disorder (49%) (Wisco et al., 2014). Co-occurrence of PTSD, and depressive and anxiety symptoms may reflect either overlapping diagnostic criteria between these disorders (Pietrzak, Goldstein, Southwick, & Grant, 2011), or preexisting genetic susceptibility to PTSD and other comorbid psychiatric disorders (Friedman & Yehuda, 1995).
Psychological distress, such as PTSS, depressive or anxiety symptoms, has far-reaching implications for the quality of life of service members and their intimate partners. Over the past three decades, research has identified inter- and intra-spousal effects of psychological distress on marital quality (Lambert, Engh, Hasbun, & Holzer, 2012) and dissatisfaction in service members (Erbes, Meis, Polusny, & Compton, 2011; Gewirtz, Polusny, DeGarmo, Khaylis, & Erbes, 2010) and their intimate partners (Renshaw, Rodrigues, & Jones, 2008). Moreover, emerging research indicated that PTSS can affect couple communication quality (Miller et al., 2013), the quality of behaviors occurring when a couple is interacting (Kelly, Fincham, & Beach, 2003). Communication, whether positive (e.g., warmth, affection, interest, empathy) or negative (e.g., hostility, contempt, criticism), has been repeatedly identified as a key predictor of relationship satisfaction (for reviews, see Heyman, 2001; Kelly et al., 2003).
The Couple Adaptation to Traumatic Stress model (CATS; Goff & Smith, 2005) describes the ways in which psychological symptoms, such as PTSD, depressive, and enxiety symptoms, hinder couple communication folowing exposure to trauma. The model highlights the bi-directional influences of psychological distress within dyad members, and the effects of each partner’s psychological distress on their own and their partner’s communication quality. Specifically, psychological distress of a partner who has been exposed to traumatic stress (called the primary partner) can intensify emotioanl distress in the other partner, the secondary partner, a phenomenon known as secondary traumatization. This phenomenon may be explained by various mechanisms, such as chronic stress resulting from living with a partner coping with psychological distress and/or identification with the primary partner’s traumatic experience. Moreover, secondary traumatization is bi-directional, such that emotioanl distress of the secondary partner can sequentially intensify the primary partner’s distress. The model postulates that elevated physiological arousal associated with emotioanl distress disrupts communication quality, which manifests in greater hostility, withdrawal, avoidance of intimacy, and aggressive behaviors. These behaviors impede the security needs of the other partner and consecutively disrupt his or her communication quality (Goff & Smith, 2005).
Research has yielded empirical evidence supporting the CATS model. First, psychological distress of service members was found to affect their intimate partners’ psychological functioning (Ben Arzi, Solomon, & Dekel, 2000). A recent meta-analysis found a medium effect size (r = .30) of the association between an individual’s PTSS and their partner’s psychological distress, including PTSD, depressive, and anxiety symptoms (Lambert at al., 2012). Prior studies indicated that 17% of non-deployed spouses met screening criteria for PTSD. Likewise, 22% of non-deployed wives met clinical criteria for depression (Gorman, Blow, Ames, & Reed, 2011), and 17.4% of spouses screened positive for generalized anxiety (Eaton et al., 2008).
Second, several studies have shown a link between PTSS and communication quality, including more aggressive behaviors, ineffective problem solving, invalidation and withdrawal, as well as lower self-disclosure and expressed affection (Allen, Rhoades, Stanley, & Markman, 2010; Taft, Watkins, Stafford, Street, & Monson, 2011). Furthermore, a meta-analysis revealed a medium effect size for the associations between PTSD symptomatology and self-reports of aggressive behaviors toward a partner (Taft et al., 2011). Whereas the above studies linking PTSS and lower communication quality relied on self-reports of communication (e.g., Allen et al., 2011), two recent studies used observations to assess couple communication in relation to PTSS. Miller et al. (2013) found that, among veterans, greater PTSS and depressive symptoms were each associated with more frequent displays of hostility and violence, and with fewer expressions of acceptance and humor. Similarly, PTSS among civilian men were associated with less supportive behaviors toward their intimate partners (Hanley, Leifker, Blandon, & Marshall, 2013).
A large body of research involving non-traumatized civilian population provides evidence of associations between depressive symptoms and observed couple communication (Hautzinger, Linden, & Hoffman, 1982). Compared to interactions of non-depressed couples, couples with a depressed partner exhibit higher frequency of dysfunctional interactions, including blame, withdrawal, verbal aggression, interruption, criticism and defensiveness (Gotlib & Whiffen, 1989; Rehman, Gollan, & Mortimer, 2008). In contrast, depressive symptoms are associated with less frequent positive communication patterns, both verbal and nonverbal, including less engagement in eye contact, less pleasant facial expressions, lower self-disclosure, and less effective problem-solving (Papp, Goeke-Morey, & Cummings, 2007; Rehman et al., 2008).
Finally, a few studies have documented the cross-partner associations of psychological distress with observed couple interaction. Specifically, greater PTSS of veterans and their partners were associated with more frequent partner expressions of hostility, and with fewer partner expressions of acceptance and humor (Miller et al., 2013). Likewise, among civilian couples, depressive and anxiety symptoms in one partner have been linked with ineffective communication behaviors, such as criticism and negativity, from their partners (Johnson & Jacob, 2000).
The Current Research
In sum, the CATS model suggests inter- and intra-partner effects linking psychological distress of each spouse with his/her partner communication (Goff & Smith, 2005). Indeed, Research has shown associations between psychological distress within intimate partners (Ben Arzi, Solomon, & Dekel, 2000), as well as inter- and intra-partner associations between psychological distress and communication behaviors (e.g., Miller et al., 2013). However, very few studies to date have tested effects of PTSS on communication quality (Hanley et al., 2013; Miller et al., 2013), and those that have relied almost exclusively on self-report data (Renshaw et al., 2008), which may be affected by social desirability and common method variance (Podsakoff, MacKenzie, Lee, & Podsakoff, 2003). Only two studies corroborating inter- and intra- personal associations between PTSS and observed couple communication (Hanley et al., 2013; Miller et al., 2013), from which only one sampled military couples and/or tested effects of depression and PTSD on couple interaction (Miller et al., 2013). Still, these studies were cross- sectional, which limits our understanding of how variables of interest change across time, and our ability to delineate causal effects. The current study aimed to replicate and extend previous findings by assessing whether psychological distress of each partner predicts his/her own and his/her partner’s observed communication behaviors over a course of one year in military couples. We hypothesized that greater psychological distress in service members and their partners will predict their own and their partners’ lower communication quality over time.
Method
Participants
A subsample of 228 couples was drawn from a randomized controlled prevention study for military parents, named After Deployment, Adaptive Parenting Tools (ADAPT; Gewirtz, DeGarmo, & Zamir, 2018). ADAPT aims to improve effective parenting practices by providing parents with evidence-based parenting tools combined with mindfulness training in 14-week group-based sessions. Couples in our study were married or cohabitating and the male partner had been deployed to recent conflicts in Iraq or Afghanistan. The vast majority of couples in this sample were married (97.8%), with only a few couples cohabitating (2.2%). The mean length of relationship to the current partner was 9.96 years (SD = 5.3), and ranged from 1 to 28 years. The number of children in a household ranged from 1 to 5 with a mean of 2.4 (SD = .92). Participants were predominantly white (88.6% of men and 95.9% of women). Women’s ages ranged from 23 to 51 (M = 35.5, SD = 5.86), and men’s ages ranged from 23 to 58 (M = 37.04, SD = 6.56). Household incomes ranged from $39,999 or less (11.5%) to $120,000 or more (15%), with most families reporting incomes between $40,000 to $79,999 (32.2 %) or $80,000 to $119,999 (41.4%). About half of participants (49.1% of husbands and 51.3% of wives) reported completing at least a Bachelor’s degree.
Most deployed partners were affiliated with Army National Guard (60.1%). The rest were affiliated with the Army Reserve (11.8%), Air National Guard (10.1%), Navy Reserve (3.9%), Air Force Reserve (3.9%), or other military units (10.2%). Participants reported one to ten combat deployments during recent conflicts (M = 2.01, SD = 1.2). Total number of months deployed were 1–6 months (6.1%), 7–12 months (26.8%), 13–24 months (32.9%), 25–36 months (24.6%), or longer than three years (9.6%).
Of the 228 couples who completed the baseline assessment, 160 (72%) couples completed the 12-month/ Time 2 (T2) assessment. There were no significant differences in most demographics (i.e., race, income, age, education, military affiliation) between women and men who completed the T2 assessment and those who dropped out. However, whereas 0.6% of couples who completed the T2 assessment were cohabitating, 5.9% of the couples who dropped out were cohabitating at baseline (χ2 (1) = 6.1, p = .03).
Procedure
Couples were recruited using multiple methods: events for National Guard and Reserve personnel, letters from the Minneapolis Veterans Affairs Medical Center, traditional and social media, and word of mouth. Couples who were interested in participating in the study were referred to an online screening survey. If they met eligibility criteria to participate in the study (i.e., at least one partner deployed to recent conflicts and they had a child aged five to twelve years old) and submitted their consent form, couples were asked to complete a confidential online survey. Following this, an in-home assessment was scheduled, where additional self- report and observational data were obtained (T1). A second in-home assessment was conducted at the 12-month post-baseline assessment, after the parenting intervention was delivered (T2)1.
Communication quality was assessed at the in-home assessments using a conflict discussion paradigm adapted from Bullard et al. (2010) for the Family Interaction Tasks (FITs) procedure (Forgatch & DeGarmo, 1999). Partners were asked to rate current conflicts from a checklist of frequent co-parenting conflicts related to deployment (e.g., getting back on the same page after deployment) in order of severity. The conflict that was ranked as most severe was selected for discussion by the interviewer. In the next phase, couples were instructed to attempt to solve the conflict in five minutes. Couples were left alone during the interactions, which were videotaped. Each couple received $50 for completing the in-home assessment, and each partner received an additional $25 for completing the online questionnaires. All study procedures of the ADAPT project were approved by the Institutional Review Board of the University of Minnesota (Study number 1005S82692, Title: Effectiveness of a web-enhanced parenting program for military families).
Measures
Psychological distress.
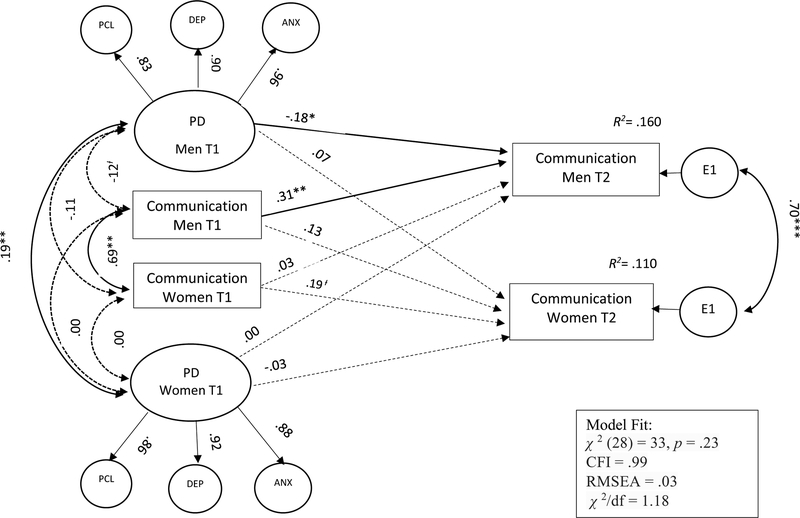
We treated PTSD, depressive, and anxiety symptoms measures as indicators of a latent variable reflecting psychological distress (see Figure 1).
Figure 1.
Actor and Partner Effects of Psychological Distress on Communication over One Year
Note. PD = psychological distress; PCL = post-traumatic stress symptoms; DEP=depressive symptoms; ANX=anxiety symptoms
Study control: intent to treat. Entries are standardized structural coefficients. Dashed paths were not found to be significant. All factor loadings were significant. Ɨ p= .08 *p <.05 **p < .01 ***p < .001.
Post-traumatic Stress symptoms.
The Post-Traumatic Stress Checklist (PCL; Weathers et al., 2013) is a 17-item standardized and clinically validated self-report measure assessing PTSD as defined by the DSM-IV (American Psychiatric Association, 1994). Deployed parents completed the PCL-M (military version), in which the items refer to a traumatic military experience, whereas non-deployed parents completed the PCL-C (civilian version), in which the items refer to any traumatic experience from the past. Respondents were asked to rate the extent to which they were bothered by each PTSD symptom in the past month using a 5-point scale from 1 (not at all) to 5 (extremely). Higher scores indicate greater PTSS. Cronbach’s alphas indicated good internal consistency for men (.95) and women (.90).
Depressive and anxiety symptoms.
We used the Hopkins Symptom Checklist-25 (HSCL 25; Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974), a well-known and widely used symptom inventory consisting of two scales: a 10-item scale assessing anxiety symptoms and a 15-item scale assessing depressive symptoms. All respondents rated each item on a 4-point Likert scale from 1 (not at all) to 4 (extremely). The total score is the average of the items of each sub-scale, such that higher scores indicate greater depressive or anxiety symptoms. Cronbach’s alphas indicated good internal consistency for men (.90) and women (.83) on the anxiety scale, and for men (.93) and women (.90) on the depression scale.
Communication quality.
A group of trained observers rated each partner’s positive and negative communication during the conflict discussion task. Communication was rated with a macro-coding system that assesses verbal and non-verbal behaviors (i.e., facial expression, body posture, tone of voice) (Zamir, Gewirtz, Labella, DeGarmo, & Snyder, 2017). Positive and negative communication of both partners was rated on 6-point Likert scales from 1 (never) to 6 (always). The positive communication scale included nine items indexing positive engagement in couple interaction, including humor, affection, empathy, interest in the partner, agreement, positive affect, positive involvement, and engaging body posture. The negative communication scale included nine items describing negative behaviors during couple interaction, including verbal aggression, withdrawal from the interaction, criticism, contempt, negative tone of voice, and interruptions (Zamir et al., 2017). Items were averaged to create summary scores of positive communication and negative communication.
Observers were trained for a total of 60 hours and underwent bi-weekly recalibration meetings to continue training and minimize observer drift. Inter-rater reliability was assessed for 15% of the videos. ICC’s for summary scales were very good for men’s (.92, .72) and women’s (.91, .70) positive communication, as well as for men’s (.86, .96) and women’s (.89, .86) negative communication at T1 and T2 respectively. In addition, Cronbach’s alphas indicated good internal consistency for men’s positive (.74, .76) and negative communication (.77, .80), and women’s positive (.72, .76), and negative communication (.79, .80) at T1 and T2. Codes were previously shown to have ecological, criterion, and construct validity in military couples (Zamir et al., 2017). Due to a strong correlation between partners’ positive and negative communication in men and women (rs = −.47 & −.56, respectively, ps < .05), we averaged the scores of the positive communication scale and the reversed scores of the negative communication scale to create a global communication quality composite for each partner.
Covariates.
We tested our model controlling for several contextual risk factors, all of which have previously shown to be associated with marital quality, including number of months deployed, combat exposure (Karney & Trail, 2017), economic status (Karney & Crown, 2007), length of relationship (Karney & Bradbury, 1995), and other negative life events experienced by men and women (Karney & Bradbury, 1995).
Family income was computed as the average of men’s and women’s reports on family income. Relationship duration was computed as the average of men’s and women’s reports of the number of years of marriage/cohabitation with the current spouse. Deployment duration was computed as the combined number of months the military partner was deployed. In addition, we also controlled for the effects of the intervention. Intent to treat (ITT) group was coded 1 for assignment to the treatment condition and 0 for controls.
Combat exposure.
The deployed spouses’ battle experiences were measured with the Deployment Risk and Resilience Inventory (DRRI; King, King, Vogt, Knight, & Samper, 2006). The DRRI measures a variety of military events and experiences among military personnel who have been deployed to war zones. The DRRI battle experience scale includes 15 items that are rated “yes” or “no”; examples include: “I or members of my unit received hostile incoming fire,” and “I or members of my unit were attacked by terrorists of civilians.” The DRRI has been validated with a large occupationally and demographically diverse sample of military personnel deployed to Operation Iraqi Freedom, and the instrument demonstrated criterion validity based on associations with measures of mental and physical health (Vogt, Proctor, King, King, & Vasterling, 2008). Cronbach’s alpha indicated good internal consistency (.87).
Negative life events.
Negative life events were assessed using the Life Events Questionnaire (LEQ; Norbeck, 1984; Sarason, Johnson, & Siegel, 1978). The LEQ lists 82 items describing positive and negative events. For each item, participants indicated whether the event occurred in the last year, whether it was considered “good” or “bad”, and how strong the effect was (0 = “no effect”, 4 = “great effect”). For the current study we used the sum of the impact ratings for all items designated as “bad” by respondents. Alphas are not reported because the LEQ produces a count of negative life events rather than an internally consistent scale.
Analytic Strategy
Preliminary analysis was conducted with IBM SPSS 22. Hypotheses were tested using structural equation modeling (SEM) with IBM AMOS 22 (Arbuckle, 2013). SEM allows the testing of an Actor-Partner Interdependence Model (APIM), which tests simultaneously actor effects (whether the predictor score of an individual affects his/her outcomes) and partner effects (whether the predictor score of an individual affects his/her partner’s outcomes), while modeling the interdependence between dyad members (Kenny, Kashy, & Cook, 2006). Model fit was evaluated using recommended fit indices (Byrne, 2013): chi-square minimization p value above .05, comparative fit index (CFI) above .95, chi-square ratio (χ2/df) less than 2.0, and root mean square error of approximation (RMSEA) below .08.
Missing values.
Model parameters were estimated using full-information maximum likelihood (FIML), which uses all available information from the observed data in handling missing data. FIML estimates are computed by maximizing the likelihood of a missing value based on observed values in the data. FIML provides more reliable standard errors compared to imputation, listwise deletion, or pairwise deletion, and tends to produce unbiased parameter estimates (Enders, 2010).
Results
Preliminary Analysis
Means, standard deviations, and bivariate correlations for the study variables are presented in Table 1. Men’s combat exposure and negative life events were positively correlated with their psychological distress. Similarly, women’s negative life events were positively correlated with their psychological distress. Men’s depressive and anxiety symptoms were negatively associated with men’s observed communication quality at T2 and women’s PTSS were negatively associated with men’s T1 communication quality. Also, partners’ observed communication quality was highly correlated at T1 and at T22.
Table 1.
Means, Standard Deviations and Zero-Order Correlations of the Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Men’s PTSD | - | ||||||||||||||||
| 2. Men’s Anxiety | .80** | - | |||||||||||||||
| 3. Men’s Depression | .73** | .86** | - | ||||||||||||||
| 4. Men’s Communication (Time 1) | −.06 | −.13 | −.13 | - | |||||||||||||
| 5. Men’s Communication (Time 2) | −.15Ɨ | −.22** | −.26** | .35** | - | ||||||||||||
| 6. Women’s PTSD | .10 | .20** | .16* | −.15* | −.10 | - | |||||||||||
| 7. Women’s Anxiety | .10 | .14* | .15* | −.01 | −.06 | .57** | - | ||||||||||
| 8. Women’s Depression | .13 | .15* | .21* | .02 | −.08 | .61** | .81** | - | |||||||||
| 9. Women’s Communication (Time 1) | −.02 | −.10 | −.15* | .70** | .28** | −.12’ | .03 | .00 | - | ||||||||
| 10. Women’s Communication (Time 2) | −.08 | −.11 | −.15 | .28** | .73** | −.08 | −.06 | −.08 | .30** | - | |||||||
| 11. DRRI | .46** | 29** | 22** | −.02 | −.06 | .06 | .06 | .06 | .02 | .04 | - | ||||||
| 12. Men’s LEQ | .21** | .28** | .35** | −.14* | −.18* | .13 | .10 | .11 | −.12 | −.20* | .06 | - | |||||
| 13. Women’s LEQ | .11 | .11 | .13 | −.07 | −.08 | .34** | .39** | .37** | −.07 | −.13 | .04 | .27** | - | ||||
| 14. Deployment Duration | .10 | .00 | .01 | −.07 | −.08 | .01 | .02 | .02 | −.08 | −.03 | .36** | .07 | .08 | - | |||
| 15. Relationship Duration | −.14* | −.11 | −.06 | .07 | −.02 | −.06 | −.09 | −.03 | .11 | −.04 | −.09 | −.10 | −.12 | −.05 | - | ||
| 16. Family Income | −.08 | −.12 | −.05 | .11 | .03 | −.16* | −.15 | −.12 | .14* | .07 | .02 | −.02 | −.15* | −.03 | .33** | - | |
| 17. ITT | .04 | .04 | −.01 | −.05 | .02 | −.05 | −.07 | −.07 | .05 | .08 | .01 | −.01 | −.11 | .04 | −.01 | .06 | - |
| M | 29.78 | 1.48 | 1.51 | 3.9 | 3.94 | 26.84 | 1.42 | 1.52 | 3.91 | 3.94 | 9.12 | 4.58 | 5.22 | ||||
| SD | 12.41 | .48 | .52 | .48 | .49 | 8.65 | .37 | .46 | .46 | .48 | 7.65 | 3.05 | 4.9 |
Note.
p <.10
p < .05.
p < .01.
Actor and Partner Effects of Psychological Distress on Communication Quality
To test the actor and partner effects of psychological distress on communication quality, we ran an APIM analysis via SEM. This model included actor and partner regression paths going from men’s and women’s psychological distress at T1 directly to their own and their partner’s communication quality at T2. Each partner’s psychological distress was specified as a latent variable, with post-traumatic stress, depressive, and anxiety symptoms as measured indicators. This was done because of the high intercorrelations between the different distress measures (see Table 1). We controlled for ITT and the effects of family income, years married, deployment duration, combat exposure and negative life events of men and women at baseline on communication quality at T2. Finally, we controlled for actor and partner effects of communication quality at T1 on communication quality at T2 (see Figure 1).
Analysis of the structural equation model indicated an adequate fit to the data[χ2 (52) = 91.4, p = .01, CFI = .97, RMSEA = .05; χ2/df = 1.75]. None of the control variables were significantly related to T2 communication scores. Therefore, we ran the model controlling only for communication at T1 and ITT. The model fit the data very well [χ 2 (28) = 33, p = .23, CFI = .99, RMSEA = .03; χ 2/df = 1.18]. In total, the model explained 16 % of the variance in men’s communication quality and 11 % of the variance in women’s communication quality at T2. As shown in Figure 1, men’s and women’s psychological distress at T1 were positively correlated. Men’s communication quality at baseline predicted their own communication at T2 (β = .31, p = .02). Additionally, controlling for baseline levels of communication, more psychological distress in men predicted their own lower communication quality one year later (β = −.18, p = .02). No actor or partner effects were found for women’s psychological distress on communication quality, and no partner effect was found for men’s psychological distress on women’s communication quality. ITT did not predict a change in communication at T23.
Exploratory Post-hoc Analysis
To examine whether there is a difference between the significant actor effect of men’s psychological distress and the nonsignificant actor effect of women’s psychological distress, we conducted moderation analysis. This was done by constraining the two actor paths to be equal, and examining the resulting reduction in model fit (Kline, 2014). Model fit was not significantly reduced when the paths were constrained to be equal (Δχ2 (1) = 1.82, p = .18), indicating nonsignificant gender moderation of the actor effects.
Discussion
The current study tested actor and partner effects of psychological distress on communication quality among reintegrated military couples over a one-year span. We employed the CATS model postulating bi-directional and mutual influences of psychological distress on communication quality (Goff & Smith, 2005). Our results partially supported the CATS model, showing cross-partner correlations between the psychological distress of intimate partners, as well as effects of men’s psychological distress on their own lower communication quality while interacting with their partner one year after. However, we did not find intra-actor effect of women’s distress or inter-partner effects of men and women’s distress on communication quality over time.
Studies assessing the effects of PTSS or depressive symptoms on couple interaction in military couples are often limited by their cross-sectional design (e.g., Allen et al., 2010), and studies looking at the long-term effects of depression on couple interaction have been limited to civilian populations (e.g., Kouros & Cummings, 2011). The current study replicates and extends these prior findings and indicates there is a lasting effect of psychological distress on the communication behaviors of service members following deployment to war. Specifically, baseline psychological distress predicted lower communication quality in the following year, above and beyond baseline communication quality. Whereas the CATS model posits that psychological arousal associated with psychological distress explains the use of ineffective communication behaviors (Goff & Smith, 2005), in our analysis significant effects of psychological distress on communication were shown only over time. This long-term effect may be explained by factors involved in the link between baseline psychological distress and communication at T2. For instance, the double ABC-X model explains that stress may pile up over time, further eroding psychological resources, with potential downstream effects on family outcomes (McCubbin & Patterson, 1983). As such, it could be that other strains resulting from psychological distress, such as problems with children (Snyder et al., 2016), taxed mental resources over the course of a year, leading to lower communication quality. Likewise, it could be that psychological distress affected marital quality, a factor that has been found to be related to psychological distress (Lambert et al., 2012), and predicts communication quality over time (Lavner, Karney, & Bradbury, 2016). Our findings highlight the need to further explore longitudinal effects of psychological distress on the relationship quality of military couples.
Although we did not find cross-partner effects of psychological distress on communication behaviors, our findings suggest that psychological distress may reverberate throughout the couple. First, consistent with the concept of secondary traumatization and extant research (e.g., Lambert at al., 2012), we found bi-directional associations of psychological distress between intimate partners, suggesting transmission of psychological distress from one partner to the other. Second, the model suggested that men’s psychological distress is not directly associated with women’s communication, but rather indirectly linked with women’s communication through mutual interactional processes. Specifically, men’s psychological distress predicted their own lower communication quality, which was associated with lower communication quality in women. Indeed, couples may engage in cycles of escalation, such that hostility expressed by one partner triggers consecutive hostile reactions in the other, and so on (Gottman, Coan, Carrere, & Swanson, 1998). Thus, the effects of men’s psychological distress on women may be attributed to the negative behaviors expressed by their partner.
Prior studies have shown that the adverse effects of deployment on relationship outcomes are especially evident when service members were exposed to combat stress, such as exposure to physical (e.g., being injured) and psychological (e.g., seeing others injured or killed) trauma during deployment. For example, prospective data gathered from a large sample of military couples revealed that physical or psychological combat stressors predicted aggressive behaviors in men and women during the reintegration period (Meadows et al., 2016). Our study, however, indicated that psychological distress, which was associated with combat exposure, directly predicted communication quality in men one year later, above and beyond combat exposure or adverse life events. These findings elucidate the crucial role of subjective distress above and beyond exposure to traumatic or other stressors. They are in line with the Family Stress Model (Conger et al., 1992) and studies indicating that it is the psychological distress provoked by life adversity, rather than family stressors per se, that predict poorer couple interactions (Conger & Conger, 2002). Although depressive and anxiety symptoms are not unique to trauma, our model suggests that, consistent with existing knowledge, they represent co-occurring symptoms with PTSS (Smith et al., 2016), and are related to combat trauma in men.
Testing three commonly co-occurring symptoms, PTSD, depressive, and anxiety symptoms (Smith et al., 2016), the current study offers a broad understanding of the effects of psychological symptoms on communication quality in military couples. Looking closer at the role of each symptom, we found that men’s depressive and anxiety symptoms are associated with men’s observed communication at T2 and women’s PTSS are associated with men’s T1 communication. Whereas associations of depressive and PTSD symptoms with observed communication behaviors have been established in prior studies (Hanley et al., 2013; Miller et al., 2013), our data reveals that anxiety symptoms are also associated with couple communication. In addition, although the high covariation between psychological distress symptoms may bias the magnitude of zero-order correlations between each specific symptom and communication, the correlations between the study variables suggest that depressive and anxiety symptoms play a more significant role in men’s communication than PTSD symptoms. Altogether, our findings underscore the need to explore diverse psychological symptoms and their effects on couple communication following deployment to war.
The study suggested that the association between psychological distress and observed communication is particularly strong in men. These results are consistent with research suggesting men are more likely to spillover their distress into the relationships than women. For example, depressive symptoms were more strongly related to negative communication among men compared with women in civilian couples (Du Rocher Schudlich, Papp, & Cummings, 2004). In addition, among military couples, only men exhibited more negative communication in relation to depressive symptoms (Miller et al., 2013). In the current sample, the fact that men, but not women, experienced combat deployment may have intensified this tendency. In contrast, women are theorized to be more invested in maintaining and improving relationships (Cross & Madson, 1997), and are believed to show greater resiliency to their partners’ distress, especially when they can recognize the source of distress (Thompson & Bolger, 1999). For example, among military couples, spouses’ marital satisfaction was negatively linked to service members’ self-reported symptom severity only when spouses perceived their partner had experienced low levels of combat activity, but not when high levels of combat exposure were perceived (Renshaw et al., 2008). Theory suggests that when a partner can attribute negative affect to external stressors they are likely to tolerate negative emotions (Thompson & Bolger, 1999). Perhaps women in the present study, who enrolled in a parenting study for military families following deployment, were more likely to be aware of their partners’ combat experience and its complications, and therefore managed to maintain effective communication in spite of their own and their partners’ distress.
Limitation and Future Directions
The current research needs to be interpreted with several limitations in mind. First, the study sample included relatively high-functioning, well-educated, middle class, Caucasian, non- clinical military couples. Caution is warranted when generalizing our results to other populations, including clinical, more representative community samples, or civilian couples dealing with other forms of traumatic stress. Specifically, low socio-economic status has been identified as a major predictor of negative couple interaction (Conger et al., 1992). Therefore, it is important to explore our research question with more socioeconomically diverse populations. Although a meta-analysis indicated stronger associations between PTSD symptomatology and reports of aggressive behaviors toward the partner in non-clinical populations, and when post- traumatic stress is conceptualized in terms of symptom severity rather than diagnosis (Taft et al., 2011), more research is needed with clinical populations diagnosed with PTSD, who may exhibit more prominent disruptions in communication quality. Furthermore, although prior research indicated associations between PTSD and/or depressive symptoms and couple communication in civilian populations (Gabriel et al., 2010; Heene, Buysse, & van Oost, 2007), generalizability of the results of this study may be limited to military populations dealing with the specific challenges associated with reintegration (e.g., combat trauma, transitional stressors). Replicating our study with civilian couples dealing with other types of trauma, such as interpersonal trauma, will reinforce the generalizability of our model.
Second, although observations are considered a preferred method to assess communication behaviors, it should be acknowledged that couples tend to display less negativity during observations compared with naturalistic settings (Heyman, 2001).
Third, we tested our theoretical model using data drawn from a randomized controlled prevention trial, which targeted maladaptation that may unfold over time following deployment. Effects of prevention intervention may be reflected in stabilization rather than decline in functioning, and they may be involved in changes in targeted variables and processes. Despite these difficulties, the use of data from a prevention study with repeated longitudinal measures provided an opportunity to examine the impact of causally distal variables that may generate long-term and accumulating effects (e.g., Snyder et al., 2016). The intervention was incorporated into the model as a covariate to control for its effects on communication at T2, and these effects were not significant.
Clinical Implications
The hundreds of thousands of couples exposed to the war in the Middle East and the persistent political conflicts around the globe highlight the crucial need to develop and implement programs designed to help military couples. Our findings suggest that interventions targeting psychological distress may help support reintegrating couples, as could the delivery of couple therapy tailored for populations affected by traumatic stress. To date, very few short-term cognitive behavioral interventions providing couple communication training have been developed for couples dealing with PTSD, some of which have shown promising results in improving relationship satisfaction (for a review see Monson, Taft, & Fredman, 2009). For example, a recent short-term intervention integrating communication training in cognitive- behavioral conjoint therapy for military couples coping with PTSD found improvements in relationship satisfaction from pre- to post-treatment (Monson et al., 2009). More efforts should be invested in the development and implementation of such programs.
Conclusion
In conclusion, we tested the CATS model with 228 couples reintegrating after combat deployment in a prospective longitudinal study assessing observed couple communication at two time points over a year. Our study offers new evidence regarding the role of psychological distress in disrupting male military spouses’ communication behaviors over time. These results emphasize the need for interventions targeting healthy intimate relationships following exposure to combat trauma.
Supplementary Material
Acknowledgments
This research was funded in part by a grant from NIDA’s prevention branch to the second author (R01DA 030114) and a grand by Warburg Fund to the first Author
Footnotes
The model was presented in the International Association for Relationship Research (IARR) Conference (July, 2018) in Forth Collins, Colorado, USA.
The study included an online survey conducted six months post baseline, which is normally considered the T2 assessment. Because the 6-month assessment is not included in the current analysis, in the current manuscript we termed the one-year follow-up in the study as T2.
Please note that psychological distress was also measured at T2, but was not included in the analysis due to the complexity of the model and sample size restrictions. For the sake of completeness, the correlations of psychological distress measures at T2 with psychological distress measures at T1 and communication at T2 are given in the supplemental materials - Table 2.
The sample of non-cohabitating couples was too small to include marital status as a variable in the model (only 6 couples were not cohabitating). Moreover, combat experience does not moderate the actor and partner effects of psychological distress on communication. These additional analyses are available from the authors upon request.
Contributor Information
Osnat Zamir, The Paul Baerwald School of Social Work and Social Welfare. The Hebrew University,.
Abigail H. Gewirtz, Department of Family Social Science & Institute of Child Development, & Institute for Translational Research in Children’s Mental Health, University of Minnesota.
Cheuk Hei Cheng, Department of Family Social Science, University of Minnesota.
Na Zhang, Department of Family Social Science, University of Minnesota.
Yoav Lavee, School of Social Work, The Max Stren Yeraeel Valley College.
References
- Allen ES, Rhoades GK, Stanley SM, & Markman HJ (2010). Hitting home: Relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. Journal of Family Psychology, 24, 280–288. doi: 10.1037/a0019405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arbuckle J (2013). IBM® SPSS® Amos™ 22 User’s Guide. Chicago, IL: IBM. [Google Scholar]
- Ben Arzi N, Solomon Z, & Dekel R (2000). Secondary traumatization among wives of PTSD and post-concussion casualties: distress, caregiver burden and psychological separation. Brain Injury, 14, 725–736. doi: 10.1080/026990500413759 [DOI] [PubMed] [Google Scholar]
- Bullard L, Wachlarowicz M, DeLeeuw J, Snyder J, Low S, Forgatch M, & DeGarmo D (2010). Effects of the Oregon model of Parent Management Training (PMTO) on marital adjustment in new stepfamilies: A randomized trial. Journal of Family Psychology, 24, 485–496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne BM (2013). Structural equation modeling with EQS: Basic concepts, applications, and programming. New Jersey: Routledge. [Google Scholar]
- Conger RD, & Conger KJ (2002). Resilience in midwestern families: Selected findings from the first decade of a prospective, longitudinal study. Journal of Marriage and Family, 64, 361–373. doi: 10.1111/j.1741-3737.2002.00361.x [DOI] [Google Scholar]
- Conger RD, Conger KJ, Elder GH, Lorenz FO, Simons RL, & Whitbeck LB (1992). A family process model of economic hardship and adjustment of early adolescent boys. Child Development, 63, 526–541. doi: 10.1111/j.1467-8624.1992.tb01644.x [DOI] [PubMed] [Google Scholar]
- Cross SE, & Madson L (1997). Models of the self: self-construals and gender. Psychological Bulletin, 122, 5–37. doi: 10.1037/0033-2909.122.1.5 [DOI] [PubMed] [Google Scholar]
- Department of Defense. (2015). Demographics: Profile of the Military Community Retrieved from http://download.militaryonesource.mil/12038/MOS/Reports/2015-Demographics-Report.pdf
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, & Covi L (1974). The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behavioral Science, 19, 1–15. doi: 10.1002/bs.3830190102 [DOI] [PubMed] [Google Scholar]
- Du Rocher Schudlich TD, Papp LM, & Cummings EM (2004). Relations of Husbands’ and Wives’ Dysphoria to Marital Conflict Resolution Strategies. Journal of Family Psychology, 18, 171–183. doi: 10.1037/0893-3200.18.1.171 [DOI] [PubMed] [Google Scholar]
- Eaton KM, Hoge CW, Messer SC, Whitt AA, Cabrera OA, McGurk D, … Castro CA (2008). Prevalence of mental health problems, yreatment need, and barriers to care among primary care-seeking spouses of military service members involved in Iraq and Afghanistan deployments. Military Medicine, 173, 1051–1056. doi: 10.7205/MILMED.173.11.1051 [DOI] [PubMed] [Google Scholar]
- Enders CK (2010). Applied missing data analysis. New York, NY: : Guilford Press. [Google Scholar]
- Erbes CR, Meis LA, Polusny MA, & Compton JS (2011). Couple adjustment and posttraumatic stress disorder symptoms in National Guard veterans of the Iraq war. Journal of Family Psychology, 25(4), 479–487. doi: 10.1037/a0024007 [DOI] [PubMed] [Google Scholar]
- Forgatch MS, & DeGarmo DS (1999). Parenting through change: An effective prevention program for single mothers. Journal of Consulting and Clinical Psychology, 67, 711–724. doi: 10.1037/0022-006X.67.5.711 [DOI] [PubMed] [Google Scholar]
- Friedman MJ, & Yehuda R (1995). Post-traumatic stress disorder and comorbidity: Psychobiological approaches to differential diagnosis Neurobiological and clinical consequences of stress: From normal adaptation to post-traumatic stress disorder. (pp. 429–445). Philadelphia, PA, US: Lippincott Williams & Wilkins Publishers. [Google Scholar]
- Gewirtz AH, DeGarmo DS, & Zamir O (2018). After Deployment, Adaptive Parenting Tools: 1-Year outcomes of an evidence-based parenting program for military families following deployment. Prevention Science, 19, 589–599. doi: 10.1007/s11121-017-0839-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gewirtz AH, Polusny MA, DeGarmo DS, Khaylis A, & Erbes CR (2010). Posttraumatic stress symptoms among National Guard soldiers deployed to Iraq: Associations with parenting behaviors and couple adjustment. Journal of Consulting and Clinical Psychology, 78(5), 599–610. doi: 10.1037/a0020571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff BSN, & Smith DB (2005). Systemic traumatic stress: The Couple Adaptation to Traumatic Stress Model. Journal of Marital and Family Therapy, 31, 145–157. doi: 10.1111/j.1752-0606.2005.tb01552.x [DOI] [PubMed] [Google Scholar]
- Gorman L,A, Blow A,J, Ames B,D, & Reed P,L. (2011). National guard families after combat: Mental health, use of mental health services, and perceived treatment barriers. Psychiatric Services, 62, 28–34. doi: 10.1176/ps.62.1.pss6201_0028 [DOI] [PubMed] [Google Scholar]
- Gotlib IH, & Whiffen VE (1989). Depression and marital functioning: An examination of specificity and gender differences. 98, 23–30. doi: 10.1037/0021-843X.98.1.23 [DOI] [PubMed] [Google Scholar]
- Gottman JM, Coan J, Carrere S, & Swanson C (1998). Predicting marital happiness and stability from newlywed interactions. Journal of Marriage and Family, 60, 5–22. doi: 10.2307/353438 [DOI] [Google Scholar]
- Hanley KE, Leifker FR, Blandon AY, & Marshall AD (2013). Gender differences in the impact of posttraumatic stress disorder symptoms on community couples’ intimacy behaviors. Journal of Family Psychology, 27, 525–530. doi: 10.1037/a0032890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heene E, Buysse A, & van Oost P (2007). An interpersonal perspective on depression: The role of marital adjustment, conflict communication, attributions, and attachment within a clinical sample. Family Process, 46, 499–514. doi:doi: 10.1111/j.1545-5300.2007.00228.x [DOI] [PubMed] [Google Scholar]
- Heyman RE (2001). Observation of couple conflicts: Clinical assessment applications, stubborn truths, and shaky foundations. Psychological Assessment, 13, 5–35. doi: 10.1037/1040-3590.13.1.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, & Jacob T (2000). Sequential interactions in the marital communication of depressed men and women. Journal of Consulting and Clinical Psychology, 68, 4–12. doi: 10.1037/0022-006X.68.1.4 [DOI] [PubMed] [Google Scholar]
- Karney BR, & Bradbury TN (1995). The longitudinal course of marital quality and stability: A review of theory, methods, and research. Psychological Bulletin, 118, 3–34. doi: 10.1037/0033-2909.118.1.3 [DOI] [PubMed] [Google Scholar]
- Karney BR, & Crown JS (2007). Families under stress: An assessment of data, theory, and reseach on marriage and divorce in the military (Vol. 599): Rand Corporation. [Google Scholar]
- Karney BR, & Trail TE (2017). Associations between prior deployments and marital aatisfaction among army couples. Journal of Marriage and Family, 79, 147–160. doi:doi: 10.1111/jomf.12329 [DOI] [Google Scholar]
- Kelly AB, Fincham FD, & Beach SR (2003). Communication skills in couples: A review and discussion of emerging perspectives. In Burleson BR & Green JO (Eds.), Handbook of communication and social interaction skills (pp. 723–751). Mahwah, NJ: Erlbaum. [Google Scholar]
- Kenny D, Kashy D, & Cook W (2006). Dyadic data analysis. New York, NY: Guilford Press. [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, & Samper RE (2006). Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology, 18(2), 89–120. [Google Scholar]
- Kline RB (2014). Principles and practice of structural equation modeling. New York, NY: Guilford Publications. [Google Scholar]
- Kouros CD, & Cummings EM (2011). Transactional Relations Between Marital Functioning and Depressive Symptoms. American Journal of Orthopsychiatry, 81, 128–138. doi: 10.1111/j.1939-0025.2010.01080.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert JE, Engh R, Hasbun A, & Holzer J (2012). Impact of posttraumatic stress disorder on the relationship quality and psychological distress of intimate partners: A meta-analytic review. Journal of Family Psychology, 26, 729–737. doi: 10.1037/a0029341 [DOI] [PubMed] [Google Scholar]
- Lavner JA, Karney BR, & Bradbury TN (2016). Does couples’ communication predict marital satisfaction, or does marital satisfaction predict communication? Journal of Marriage and Family, 78, 680–694. doi: 10.1111/jomf.12301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCubbin HI, & Patterson JM (1983). The family stress process. Marriage & Family Review, 6, 7–37. doi: 10.1300/J002v06n01_02 [DOI] [Google Scholar]
- Meadows SO, Tanielian T, Karney BR, Ayer L, Chandra A, Friedman EM, … Schell TL (2016). The deployment life study: Longitudinal analysis of military families across the deployment cycle. Retrieved from http://www.dtic.mil/dtic/tr/fulltext/u2/1014454.pdf [PMC free article] [PubMed] [Google Scholar]
- Miller MW, Wolf EJ, Reardon AF, Harrington KM, Ryabchenko K, Castillo D, … Heyman RE (2013). PTSD and conflict behavior between veterans and their intimate partners. Journal of Anxiety Disorders, 27, 240–251. doi: 10.1016/j.janxdis.2013.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, & Hoge CW (2007). Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the iraq war. Journal of the American Medical Association, 298, 2141–2148. doi: 10.1001/jama.298.18.2141 [DOI] [PubMed] [Google Scholar]
- Monson CM, Taft CT, & Fredman SJ (2009). Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clinical Psychology Review, 29, 707–714. doi: 10.1016/j.cpr.2009.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norbeck JS (1984). Modification of recent life event questionnaires for use with female respondents. Research on Nursing and Health, 7, 61–71. [DOI] [PubMed] [Google Scholar]
- Papp LM, Goeke-Morey MC, & Cummings EM (2007). Linkages between spouses’ psychological distress and marital conflict in the home. Journal of Family Psychology, 21, 533–537. doi: 10.1037/0893-3200.21.3.533 [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, & Grant BF (2011). Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Anxiety Disorders, 25, 456–465. doi: 10.1016/j.janxdis.2010.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee J-Y, & Podsakoff NP (2003). Common method biases in behavioral research: A critical review of the literature and recommended remedies. Journal of Applied Psychology, 88, 879–903. doi: 10.1037/0021-9010.88.5.879 [DOI] [PubMed] [Google Scholar]
- Rehman US, Gollan J, & Mortimer AR (2008). The marital context of depression: Research, limitations, and new directions. Clinical Psychology Review, 28, 179–198. doi: 10.1016/j.cpr.2007.04.007 [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Rodrigues CS, & Jones DH (2008). Psychological symptoms and marital satisfaction in spouses of Operation Iraqi Freedom veterans: Relationships with spouses’ perceptions of veterans’ experiences and symptoms. Journal of Family Psychology, 22, 586–594. doi: 10.1037/0893-3200.22.3.586 [DOI] [PubMed] [Google Scholar]
- Rytwinski NK, Scur MD, Feeny NC, & Youngstrom EA (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A Meta- analysis. Journal of Traumatic Stress, 26, 299–309. doi:doi: 10.1002/jts.21814 [DOI] [PubMed] [Google Scholar]
- Sarason IG, Johnson JH, & Siegel JM (1978). Assessing the impact of life changes: Development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology, 46, 932–946. [DOI] [PubMed] [Google Scholar]
- Smith SM, Goldstein RB, & Grant BF (2016). The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Journal of Psychiatric Research, 82, 16–22. doi: 10.1016/j.jpsychires.2016.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snyder J, Gewirtz A, Schrepferman L, Gird SR, Quattlebaum J, Pauldine MR, … Hayes C (2016). Parent–child relationship quality and family transmission of parent posttraumatic stress disorder symptoms and child externalizing and internalizing symptoms following fathers’ exposure to combat trauma. Development and Psychopathology, 28, 947–969. doi: 10.1017/S095457941600064X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, & Monson CM (2011). Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology, 79, 22–33. doi: 10.1037/a0022196 [DOI] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, & Hoge CW (2010). Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of general psychiatry, 67(6), 614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- Thompson A, & Bolger N (1999). Emotional transmission in couples under stress. Journal of Marriage and Family, 61, 38–48. doi: 10.2307/353881 [DOI] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, & Vasterling JJ (2008). Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment, 15(4), 391–403. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Wisco BE, Marx BP, Wolf EJ, Miller MW, Southwick SM, & Pietrzak RH (2014). Posttraumatic stress disorder in the US veteran population: results from the National Health and Resilience in Veterans Study. The Journal of clinical psychiatry, 75, 1338–1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamir O, Gewirtz A, Labella M, DeGarmo D, & Snyder J (2017). Experiential avoidance, dyadic interaction and relationship quality in the lives of veterans and their partners Journal of Family Issues. doi: 10.1177/0192513X17698182 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.