Abstract
MicroRNAs (miRNAs) create systems networks and gene-expression circuits through molecular signaling and cell interactions that contribute to health imbalance and the emergence of cardiovascular disorders (CVDs). Because the clinical phenotypes of CVD patients present a diversity in their pathophysiology and heterogeneity at the molecular level, it is essential to establish genomic signatures to delineate multifactorial correlations, and to unveil the variability seen in therapeutic intervention outcomes. The clinically validated miRNA biomarkers, along with the relevant SNPs identified, have to be suitably implemented in the clinical setting in order to enhance patient stratification capacity, to contribute to a better understanding of the underlying pathophysiological mechanisms, to guide the selection of innovative therapeutic schemes, and to identify innovative drugs and delivery systems. In this article, the miRNA–gene networks and the genomic signatures resulting from the SNPs will be analyzed as a method of highlighting specific gene-signaling circuits as sources of molecular knowledge which is relevant to CVDs. In concordance with this concept, and as a case study, the design of the clinical trial GESS (NCT03150680) is referenced. The latter is presented in a manner to provide a direction for the improvement of the implementation of pharmacogenomics and precision cardiovascular medicine trials.
Keywords: miRNAs, biomarkers, gene networks, cardiovascular disorders, precision medicine, pharmacogenomics, SNPs, clinical trials
1. Introduction
Cardiovascular disorders (CVDs) represent a group of diseases which are associated with a large number of risk factors—including environmental, genomics and lifestyle risks—that contribute to both development and disease progression. CVDs are responsible for most noncommunicable disease (NCD) deaths, the number of which increased dramatically over the last two decades. According to the latest report from the World Health Organization (WHO) in 2019, NCDs accounted for 74% of all deaths globally (about 41 million people), while CVDs account for about 17.9 million deaths annually, for an estimated 32% of all deaths globally. Moreover, CVDs including coronary artery disease (CAD), myocardial infarction (MI), heart failure (HF) and cardiomyopathies rank among the leading causes of morbidity and mortality worldwide [1].
After the completion of the Human Genome Project, the efforts focusing on the clinical translation of the extracted molecular knowledge strengthened personalized medicine concepts to emerge and be applied in the healthcare system. Developments are currently being witnessed in the “-omics” methodologies, nanotechnological approaches and artificial intelligence capabilities, which now present greater accuracy, safety, and efficiency in the facilitation of disease prognosis and diagnosis, as well as the delivery of therapeutics in the clinical setting for specific populations and even individual patients [2,3]. In particular, for diseases and disorders exhibiting a complex and multifactorial status in their pathophysiology, like CVDs, such a capacity advances the improvement of clinical outcomes and offers more cost-effective disease management. Importantly, the clinical translation of the molecular knowledge has to be suitably implemented within existing therapeutic intervention guidelines, as well as laboratory tests and specific patient group handling procedures and protocols [4]. In order to move towards this direction, the molecular background reflecting the cardiovascular system’s physiology and pathophysiology must be clearly understood.
The genetic nature of CVDs is polygenetic, with a plethora of genes being involved in various signaling pathways that affect vital cellular decisions. Although the latter complicates a universal and easy exploitation of the genetic information, the validation of the clinical practical utility of specific identified biomarkers coming from genomic studies (e.g., single nucleotide polymorphisms (SNPs), differential gene and protein expression levels, and the identification of specific RNA molecules) offers such a capability. In previous years, evidence has shown that multiple such biomarkers often contribute cumulatively and generate polygenic risk scores that reflect an individual’s susceptibility to the emergence of disease before any symptoms appear. Moreover, by using predictive biomarkers for the early diagnosis of CVDs, medications may be delivered earlier to patients in order to ameliorate their risk and improve their clinical outcomes. Indeed, the administration of cardiovascular drugs offered in the clinical setting is based on pharmacological targets controlling the symptoms and thus minimizing the contribution of specific risk factors to CVDs’ emergence (e.g., high pressure and high cholesterol levels) [5,6,7,8,9].
The pathophysiology of CVDs is heterogeneous and involves various risk factors that contribute to the development and disease progression, whereas interindividual genetic differences further contribute to illness complexity and severity seen in the clinical phenotype”. Therefore, it is vital to analyze and clinically handle the extracted and validated genomic knowledge in a way which enables the identification of the most common molecular pathways derived from prognostic, diagnostic and pharmacogenomics biomarkers. MiRNAs represent crucial players at the molecular level that epigenetically modulate gene expression and function at the cellular and organismal level. Because miRNAs can target multiple genes, they can be valuable biomarkers in the management of various CVDs. In this context, the clinical utility of validated miRNA biomarkers in CVDs will be discussed by analyzing the miRNA-gene networks and correlating the molecular pathophysiology with pharmacogenomics knowledge. In particular, this review highlights the following for CVDs: (1) the role of miRNAs and their value in precision medicine, with special emphasis being given to atherosclerosis (arteriosclerosis); (2) the need for the implementation of pharmacogenomics to advance precision in CVD diagnosis and prognosis; (3) the power of biomarker miRNAs to advance pharmacogenomics knowledge by linking their gene networks with pathophysiology signaling pathways, SNPs, and drug targets. By combining the gene pharmacological targets of the marketed drugs used for the therapeutic management of CVDs within the miRNA–gene networks, the utility of different biomarkers (miRNAs, SNPs, pharmacogenomic) can be pinpointed across the pathway in order to guide clinical decisions. To this end, in silico methodologies, machine learning approaches and data-driven predictive risk models are needed to permit the validation and implementation of miRNA biomarkers in the care of CVDs for individual patients and populations.
The implementation of microRNAs and other biomarkers in the clinical setting and therapeutics of CVDs has been thoroughly covered in recently published reviews [10,11,12,13,14,15]. Moreover, the attempt to identify circulating microRNAs as biomarkers and the elucidation of the role of exosomes in carrying such critical molecules in the plasma of patients with CDVs has been additionally shown to present promises in diagnosis, therapy, and drug delivery [16,17,18,19]. To this end, the emerging role of circular RNAs (circRNAs) as potential biomarkers in CVDs has also been highlighted [20,21]. Furthermore, as recently pointed out, the long noncoding RNAs (lncRNAs) that represent a heterogenous group of noncoding transcripts are capable of regulating complex molecular networks, and are therefore considered as potential biomarkers in CVDs [22,23]. The main focus of our work relies on the development and application of bioinformatic methodologies capable to uncover pharmacogenomics relevant biomarkers in the miRNAs-gene correlation axis to guide cardiovascular medicine decisions. This is crucial as there are various types of genetic traits, (e.g., expression and mutational level, SNPs, epigenetic modifications, drug targets) within miRNA-gene networks that must be assessed and applied simultaneously in the clinical setting as biomarkers. Thus, the data presented in this article provides new insights into bioinformatics analysis of miRNA-gene interactions by presenting approaches to better achieve biomarker implementation for the diagnosis, treatment, and development of new drugs in CVDs. Overall, such direction contributes to efforts aiming to emphasize the importance of clinically-relevant correlations in the miRNA-genes axis that exhibit an importance to advance pharmacogenomics and cardiovascular precision medicine.
2. Role of miRNAs in Cardiovascular System Physiology and Pathophysiology
Atherosclerosis is a progressive, chronic, inflammatory disease of the artery walls caused by endothelial damage or injury. Blood cells and other substances such as fats, cholesterol and matrix proteins clump at the injury site, initiating atherosclerotic plaque formation and subsequent vessel stenosis. Although the exact cause of the plaque formation is still unclear, hypertension, hypercholesterolemia, diabetes, obesity, and smoking are considered to be major risk factors. Atherosclerosis is the main underlying cause of a plethora of CVDs, such as CAD, MI, stroke, carotid artery disease, and peripheral vascular disease.
Despite the significant advances in cardiovascular research, the current prognostic, diagnostic, and therapeutic tools have not been adequately improved, and fail to manage patients suffering from various CVDs. Thus, the need for the development of novel accurate prognostic and therapeutic tools remains a major challenge in cardiovascular medicine. Over the past few years, human genome sequencing studies have improved the characterization of non-coding RNAs, and have revealed their important roles in health and the pathophysiological pathways of many diseases, including cancer, diabetes, and CVDs [24,25]. Based on size, non-coding RNAs can be categorized into short non-coding RNAs (sncRNAs < 200 nucleotides) and long non-coding RNAs (lncRNAs > 200 nucleotides up to 100 kilobases). According to their function and structure, sncRNAs can be divided into: (a) functional RNAs, which play pivotal roles in transcription and translation, such as transfer-RNAs (t-RNAs), small nuclear RNAs (snRNAs), and ribosomal RNAs (rRNAs); and (b) regulatory RNAs, which differentially regulate gene expression, such as microRNAs (miRNAs), small interfering RNAs (siRNAs), and piwi-interacting RNAs (piwiRNAs) [26,27,28].
Among this wide variety of non-coding RNAs, much attention has been given to miRNAs which consist of 20–22 nucleotides, as they play key regulatory roles for molecular networks of cardiac development, lipid homeostasis and CVD pathogenesis [29,30]. MiRNAs regulate the expression of protein-coding genes through post-transcription mechanisms, mainly by inhibiting the translation of target mRNAs or inducing their destabilization. Specifically, a single miRNA may bind to complementary sequences of multiple target mRNAs, and a unique mRNA can be the target of several miRNAs, thus forming large-scale miRNA-mRNA regulatory networks. Besides their role in posttranscriptional regulation, miRNAs exert epigenetic regulatory roles [31].
Through their role in the regulation of gene expression, miRNAs can regulate the drug response by acting on genes encoding metabolic enzymes, protein carriers and pharmacological targets. At the same time, the presence of many miRNAs in the bloodstream has sparked a wealth of research into their role as potential biomarkers for use in precision approaches to patient stratification for various diseases, including CVDs [32,33,34]. It is noteworthy that circulating miRNAs share optimal biochemical properties to be excellent biomarkers; specifically, they (1) are highly stable in an extracellular environment, (2) are easily detected in plasma samples and serum, (3) can be obtained by standard laboratory techniques, and (4) are protected from degradation due to their binding to proteins or their encapsulation in microvesicles [35].
3. Clinical Relevance of miRNA Networks in the Clinical Practice of CVDs
During the last two decades, miRNAs have shown tremendous potential to serve as diagnostic and prognostic biomarkers in the cardiovascular field. Their organ- and cell-specific regulation allow them to be studied in a variety of disease entities within the CVD spectrum. Despite several studies having shed light to the properties of miRNAs in the classification and risk stratification of patients with CVD [11,36], the validation of the reported results in large-scale clinical trials is still needed, particularly with regard to the potential clinical utility of miRNAs as therapeutic agents.
Circulating miRNAs are extremely stable in the circulation, and can be easily detected with high sensitivity and specificity using sequence-specific amplification [37]. Hence, they are considered to be able to serve as potential clinical biomarkers with great diagnostic power (non-inferior to the established protein-based biomarkers) and promising prognostic value in lipid metabolism disorders, atherosclerosis, and cardiomyopathy [15]. For example, several studies concerning miRNAs as potential biomarkers in atherosclerosis and in cardiovascular risk factors were published in the last few years; likewise, genome sequence variations, including SNPs, could act as biological markers for the response to certain drugs [38,39,40]. However, genomics alone cannot provide a complete monitoring of the patient’s phenotype. The miRNA expression reflects changes to distinct pathological conditions and drug treatments, indicating a complex interaction between genetic and environmental factors, and providing functional insights in disease prediction [41]. For example, a correlation between platelet-derived miRNAs’ expression levels with P2Y12 receptor inhibitor (clopidogrel and prasugrel) responsiveness has been proposed [42,43,44], and this association could be influenced by the interaction of CYP2C19 genotype polymorphisms [45]. Thus, innovative and more accurate biomarkers are still an unmet need in the monitoring of cardiovascular therapies, and could lead to personalized therapies. Novel candidate miRNAs have to be extensively validated based on -omics sciences along with improvements in risk prediction algorithms, and hold the potential to provide very accurate predictions at an early stage of CVDs. The clinical relevance of miRNAs within these aspects of CVDs will be described below.
4. Experimental Data Collection of miRNA CVD Biomarkers and Bioinformatic Analysis
MiRNAs associated with CVDs were retrieved from the mir2disease [46] and phenomir [47] databases using multiMiR [48]. Specifically, disease terms associated with CVDs were manually selected as input for performing queries to retrieve CVD-associated miRNAs (Table S1). Validated target genes (VTGs) of the CVD-associated miRNAs were retrieved from the mirtarbase [49] and mirecords [50] databases using multiMiR. For increased accuracy, miRNA-gene target interactions were further filtered to include only those that were experimentally validated by Reporter gene assays (e.g., Luciferase assay), Immunoblot/Western blot, and Real-time (RT) qPCR. Furthermore, information of CVD-associated drugs and SNPs that target and/or affect VTGs were retrieved from the Cardiovascular Disease Systems Pharmacology (CVDSP) database (https://old.tcmsp-e.com/cvdsp.php (accessed on 27 September 2021)) [51] and the study of Vizirianakis et al. [52], respectively. According to our analysis, miR-155-5p is by far the most prominent in the list of CVD-associated miRNAs. As shown in Table 1, according to mirtarbase and mirecords databases, miR-155-5p interacts with 241 different genes playing a central role in regulating genes contributing to human cardiac hypertrophy and hypertension, as retrieved by the mir2disease database. The list of top ten overrepresented miRNAs involved in CVDs is further supplemented by miR-21-5p, miR-145-5p, miR-34a-5p, miR-125b-5p, miR-29a-3p, miR-24-3p, miR-29b-3p, miR-200c-3p, and miR-17-5p which have far fewer gene targets than miR-155-5p. Most of them are related to cardiomyopathy, cardiac hypertrophy and stroke (Table 1).
Table 1.
Top 10 miRNAs implicated in CVDs.
| Mature_Mirna | Targeted Genes | SNPs | Drugs | Disease_Drug | |
|---|---|---|---|---|---|
| 1 | miR-155-5p | 241 | 5 | 15 | Cardiac hypertrophy; hypertension |
| 2 | miR-21-5p | 153 | 4 | 11 | Myocardial infarction; heart failure; vascular disease; cardiac hypertrophy; cardiomyopathy, dilated; stroke |
| 3 | miR-145-5p | 151 | 3 | 9 | Vascular disease; supravalvar aortic stenosis |
| 4 | miR-34a-5p | 148 | 4 | 31 | Stroke |
| 5 | miR-125b-5p | 126 | 5 | 4 | Cardiac hypertrophy; heart failure; vascular disease; cardiomyopathy, dilated; supravalvar aortic stenosis; cardiovascular; cardiomyopathy, idiopathic dilated; stroke |
| 6 | miR-29a-3p | 123 | 7 | 28 | Cardiac hypertrophy; cardiomyopathy, dilated; stroke |
| 7 | miR-24-3p | 110 | 4 | 1 | Cardiac hypertrophy; heart failure; cardiovascular; cardiomyopathy, dilated; supravalvar aortic stenosis; stroke |
| 8 | miR-29b-3p | 109 | 6 | 15 | Cardiac hypertrophy; myocardial infarction; cardiomyopathy, dilated; stroke |
| 9 | miR-200c-3p | 98 | 3 | 5 | Cardiomyopathy, dilated |
| 10 | miR-17-5p | 95 | 3 | 8 | Cardiomyopathy, dilated; stroke |
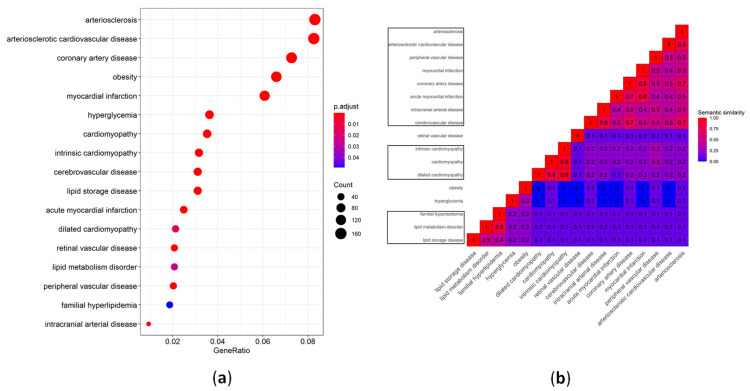
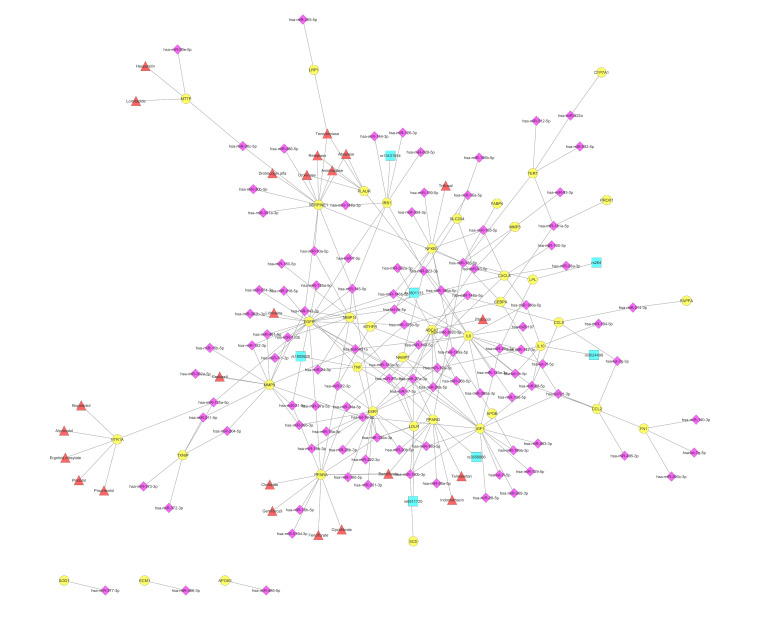
Over-representation analysis on VTGs was performed for disease ontology (DOSE) terms (Table S2) and Reactome pathways (Table S3), using DOSE [53], ReactomePA [54] and clusterProfiler [55,56]. The selected CVD-associated DOSE terms that were enriched in the VTGs of CVD-associated miRNAs are shown in Figure 1. In particular, as presented in Figure 1a, a larger number of genes (about 160) are associated with the terms “arteriosclerosis”, and “arteriosclerotic cardiovascular disease”. The top five categories identified are related to the terms “arteriosclerosis”, “arteriosclerotic cardiovascular disease”, “coronary artery disease”, “obesity”, and “myocardial infraction” (Figure 1a). The subsequently executed similarity analysis between the CVD-associated DOSE terms revealed three major clusters (Figure 1b) that will be further presented and discussed under the terms “atherosclerosis”, “cardiomyopathy”, and “lipid metabolism disorder”. As far as the pharmacogenomic association of the genes identified is concerned, the in silico analysis of the top ten most drug-targeted genes is shown in Figure 2.
Figure 1.
Selected CVD-associated DOSE terms that are enriched in the validated gene targets of CVD-associated miRNAs. (a) Dot plot of statistically significant, CVD-associated DOSE terms, displaying the gene ratio and statistical significance (p-value < 0.05, following Bonferroni adjustment). (b) Heat map displaying the semantic similarity between the CVD-associated DOSE terms. The DOSE term similarity measurements were performed using the method of Wang et al. [57] and clusterProfiler [55,56]. The DOSE terms were clustered using hierarchical clustering. Clusters with two or more terms are specified with black-colored borders. The heat map was created using ComplexHeatmap [58].
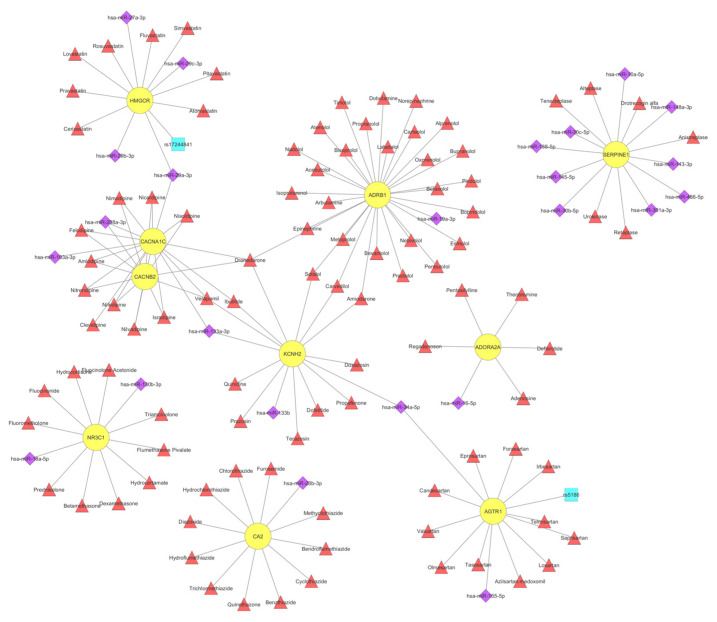
Figure 2.
Network representation of ten gene-targets of CVD-associated miRNAs, which were also found to be targeted by most CVD-associated drugs from the CVDSP database [51]. The network displays 10 validated gene targets (circles in yellow), as well as 24 miRNAs (diamonds in purple), two SNPs (squares in turquoise) and 98 drugs (triangles in red) that are CVD-associated, and which target and/or affect them. The network was created using Cytoscape [59].
5. Atherosclerosis
Accumulating evidence from numerous studies have demonstrated the significant role of miRNAs in the development of atherosclerosis, controlling the molecular and cellular mechanism of onset and progression of atherosclerosis by acting in different vascular cells. The major cell categories affected by miRNAs are endothelial cells (EC), inflammatory cells, mainly macrophages and monocytes and vascular smooth muscle cells (VSMC). Although the vast majority of miRNAs are expressed in all atherosclerosis-associated cell types (ECs, macrophages and VSMCs), a small group of them were expressed in a cell-type specific manner [60]. In addition, their expression is highly regulated at a post-transcriptional level as evidenced by the inconsistency between pri-miRNA and mature miRNA expression [60] and by the fact that many pri-miRNAs fail to produce mature miRNAs due to their processing [61].
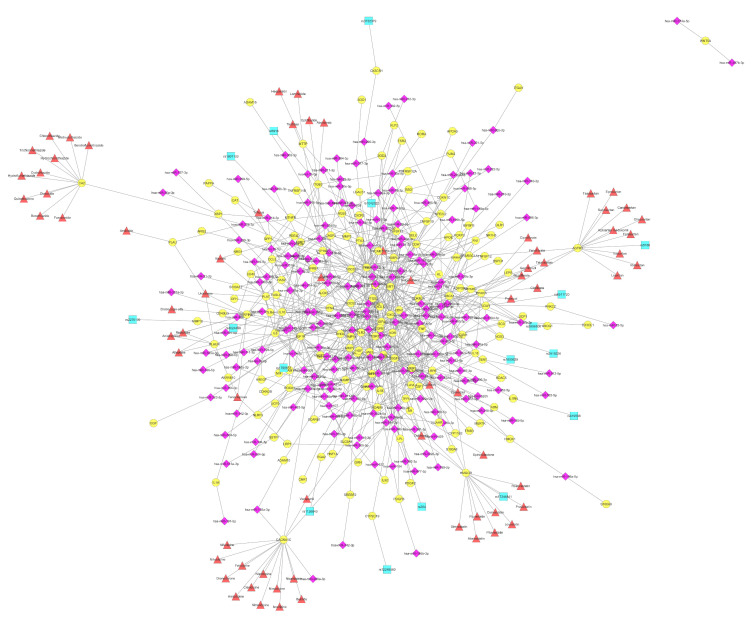
In our analysis, under the term “atherosclerosis”, many different terms with high similarity have been grouped and discussed together. These terms are: “arteriosclerotic cardiovascular disease”, “arteriosclerosis”, “retinal vascular disease”, “coronary artery disease”, “hyperglycemia”, “myocardial infarction”, “obesity”, “peripheral vascular disease”, “cerebrovascular disease”, “acute myocardial infarction”, “cardiomyopathy”, and “intracranial arterial disease” (Figure 1b). As shown in Figure 3, the complicated network describing the interactions of VTGs with CVD-associated miRNAs consists of 724 connections. More than 190 miRNAs have been found to be involved in the regulation of 160 different genes in all phases of atherosclerosis (Figure 3). In particular, the average number of connections found between a VTG and miRNAs is 4.5, while the vast majority of them (114 out of 160; 71.25%) had less than five connections, and 17 out of 160 (10.63%) interacted with more than 10 candidate miRNAs. Of the 196 different miRNAs associated with atherosclerosis, the ten with the most gene interactions are presented in Table 2. Of these, the most abundant, miR-146a-5p, as well as miR-143-3p, miR-221-3p, miR-126-3p, and miR-138-5p are absent from the list of miRNAs with the most gene interactions implicated in CVDs (Table 1). MiR-146a-5p was found to target 18 genes—namely CCL5, CD40LG, CFH, CXCL12, ELAVL1, ICAM1, IL6, MIF, NFKB1, PLAUR, PTGS2, RHOA, ROCK1, S100A12, SPP1, TGFB1, TLR2, and TLR4—associated with the development of atherosclerosis. The role of miR-146a in atherosclerosis has been described; its increased expression has been correlated with an increased risk of atherosclerosis in patients with CAD [62]. Moreover, in patients with hypothyroidism, it counts as a potential predictor for atherosclerosis [63].
Figure 3.
Network of VTGs enriched within the DOSE term arteriosclerosis. The network displays 160 arteriosclerosis-associated VTGs (circles in yellow), as well as 196 miRNAs (diamonds in purple), 17 SNPs (squares in turquoise) and 70 drugs (triangles in red) that are CVD-associated, and target and/or affect them. The network was created using Cytoscape [59].
Table 2.
Top 10 miRNAs implicated in atherosclerosis, cardiomyopathy and lipid metabolism disorder.
| Atherosclerosis | Cardiomyopathy | Lipid Metabolism Disorder | ||||
|---|---|---|---|---|---|---|
| Mature_Mirna | Targeted Genes | Mature_Mirna | Targeted Genes | Mature_Mirna | Targeted Genes | |
| 1 | miR-146a-5p * | 18 | miR-21-5p | 10 | miR-138-5p * | 8 |
| 2 | miR-155-5p | 15 | miR-24-3p | 9 | miR-146a-5p * | 6 |
| 3 | miR-21-5p | 15 | miR-145-5p | 7 | miR-26a-5p * | 5 |
| 4 | miR-24-3p | 15 | miR-138-5p * | 7 | miR-27a-3p * | 5 |
| 5 | miR-29b-3p | 13 | miR-143-3p * | 7 | miR-145-5p | 5 |
| 6 | miR-143-3p * | 12 | miR-17-5p | 7 | miR-130a-3p * | 5 |
| 7 | miR-145-5p | 12 | miR-155-5p | 6 | miR-98-5p * | 5 |
| 8 | miR-221-3p * | 12 | miR-125b-5p | 6 | miR-130b-3p * | 5 |
| 9 | miR-126-3p * | 11 | miR-146a-5p * | 6 | miR-223-3p * | 4 |
| 10 | miR-138-5p * | 11 | miR-133b * | 5 | miR-1-3p * | 4 |
* miRNAs not listed in top 10 miRs implicated in CVDs (Table 1).
The maximum number of interactions with different miRNAs was 42, and was observed for the vascular endothelial growth factor (VEGFA) gene. VEGFA is the most functionally important member of the Vegf family [64], and was initially identified as an inducer of vascular permeability (vascular permeability factor, VPF). VEGFA is a proangiogenic factor [65] that—through binding to its receptor, mainly Vegfr-2/Flk1/Kdr—stimulates haematopoietic cell proliferation, survival, differentiation and migration [66]. Indeed, numerous miRNAs—including miR-15a, miR-200b, miR-20b, miR-1, miR-206, and miR-93—have been discussed extensively in the literature to target VEGFA, and have been validated with multiple methods (Table S4). Additionally, 17 different SNPs have been identified in an equal number of genes (Table S1). Regarding the therapeutic drugs, 24 genes are serving as targets for 70 different compounds (Table S1). The largest group of drugs (13), mainly containing calcium channel blockers, target the CACNA1C gene. This gene encodes for the alpha-1 subunit of a voltage-dependent calcium channel that controls the flow of calcium ions into cardiomyocytes. In parallel, CACNA1C was found to interact with miR-103a-3p, miR-133a-3p, miR-208a-3p, and miR-29a-3p (Figure 3). CACNA1C has been validated as a target of miR-103a-3p, one of the most important miRNAs associated with recurrent venous thromboembolism [67]. Moreover, the overexpression of miR-29a-3p was associated with the reduced expression of CACNA1C in patients with atrial fibrillation, enhancing its potential therapeutic role in its treatment [68].
According to our analysis, the four genes—AGTR1, HMGCR, ITGB3, and PPARG—shown to be influenced by specific miRNAs, or targeted by drugs and SNPs in their sequence are also associated with atherosclerosis (Figure 3). Notably based on this fact, rs5186 (Chromosome 3:148742201) in the AGTR1 gene, rs17244841 (Chromosome 5:75347030) in the HMGCR gene, rs5918 (Chromosome 17:47283364) in the ITGB3 gene, and rs3856806 (Chromosome 3:12434058) in the PPARG gene were also included in our clinical trial GESS (NCT03150680), in order to assess any potential predictive value with the SYNTAX score; this outcome, if exists upon the completion of the study, it will be of great interest in the clinical setting of CVDs.
Angiotensin II receptor type 1 (AGTR1, AT1R) encodes for multiple transcript variants of the type 1 receptor of angiotensin II, which is an important effector controlling blood pressure and volume in the cardiovascular system. AGTR1 expression levels are largely regulated by post-transcriptional mechanisms [69]. MiR-155 was found overexpressed in human umbilical vein endothelial cells (HUVECs) and vascular smooth muscle cells (VSMCs) and by using Western blot, it was confirmed that AT1R is a target of miR-155 in HUVECs [70] (Table S4). Zheng et al demonstrated that overexpression of miR-155 in rat’s aortic adventitial fibroblasts significantly reduced AT1R protein expression despite that mRNA levels remained unaffected [71]. Luciferase reporter assays further confirmed that miR-155 interacts directly with the AT1R 3′-UTR and translationally represses the expression of this protein in vivo [71]. Of interest, the SNP +1166A/C or A1166C (rs5186), which is located in the 3’ UTR of AT1R gene is recognized by miR-155 [72] and results in altered AT1R protein expression in a cohort of hypertensive patients [73] or in patients with advanced carotid atherosclerosis [74]. The drugs related to AGTR1 gene, such as candesartan, eprosartan and olmesartan, are angiotensin II receptor blockers (ARBs) that are widely used to treat high blood pressure (Figure 2 and Figure 3).
3-hydroxy-3-methylglutaryl coenzyme A reductase (HMGCR) is an atheroprotective enzyme that limits cholesterol biosynthesis, preventing CVD and other atherosclerotic diseases [75]. MiR-29 directly targets HMGCR as evidenced by decreased levels of luciferase activity in the presence of a miR-29a mimic [76] (Table S4). Using Dicer1-knockout mice, Liu et al found that miR-29a/b/c significantly suppressed HMGCR expression (by targeting the HMGCR mRNA 3′-UTR) revealing the importance of miR-29 in regulating hepatic cholesterol homeostasis and as a potential therapeutic target [77]. In addition, miR-27 was found capable of significantly suppressing cholesterol biosynthesis by regulating HMGCR gene [78]. The genetic polymorphism rs17244841 in HMGCR gene, although relatively rare, caused a significant reduction in total cholesterol and LDL-c levels in heterozygous CAD patients treated with statins [79].
As mentioned above, one of the three vital cell categories in atherosclerotic plaque formation is smooth muscle cells (SMCs). Particularly in rupture caps, fewer SMCs are present, indicating an unstable plaque prone to rupture [80,81]. As was demonstrated by Misra et al., the reduction of integrin β3 (Itgb3, GPIIIa) levels in SMCs induces TLR4 expression, consequently enhancing Cd36 levels [82]. Moreover, the Itgb3 mutant phenotype resulted in the recruitment of multiple pre-existing SMCs into plaques, while a medium conditioned with Itgb3(−/−) macrophages increased SMC migration and proliferation [82]. Altogether, the important contribution of Itgb3 in atherogenesis has been highlighted. Several miRNAs have been found in our analysis to interact with ITGB3, namely let-7a-5p, let-7c-5p, miR-17-3p, miR-30a-5p, miR-30c-5p, and miR-98-5p (Table S4). Moreover, the rs5918 (PlA1/A2) polymorphism in the integrin β3 gene is a well-established risk factor for acute coronary thrombosis and premature myocardial infarction [83,84]. Carriers of the Leu33Pro polymorphism have been linked to an increased risk of atherosclerotic plaque rupture in an ARIC study in a Caucasian population [85]. Three therapeutic choices were found to target GPIIIa in order to prevent platelet aggregation (Figure 3). Abciximab is a monoclonal anti-glycoprotein IIb/IIIa receptor antibody, while eptifibatide and tirofiban are a peptide-based antagonist and a non-peptide reversible antagonist of the platelet glycoprotein IIb/IIIa receptor, respectively.
The peroxisome proliferator activated receptor gamma (PPARγ) gene is located in chromosome 3 (3p25), and encodes for a protein that is a member of the PPAR family. The three members of the PPARs—namely PPARα, PPARγ and PPARβ/δ—are ligand-activated transcription factors of nuclear hormone receptor that play a vital role in the regulation of energy homeostasis and metabolism, but each of them performs unique functions in these processes and displays tissue-specific expression patterns [86,87,88]. PPARγ is an essential regulator of adipocyte differentiation and glucose homeostasis, and is highly expressed—in addition to adipocytes—in VSMCs, in ECs, and in macrophages [89]. The significant contribution of PPARγ in the limitation of the progression of atherosclerosis through multiple mechanisms is well studied and reviewed elsewhere [89]. Our in silico analysis revealed seven miRNAs that interact with PPARγ (Figure 3, Table S4). MiR-130 strongly suppresses PPARγ expression, resulting in the inhibition of adipocyte differentiation. Their interaction was both in the PPARγ mRNA-coding region and in 3′ UTR, as shown by Lee et al [90]. Interestingly, in the same study, obese women showed significantly lower miR-130 levels and increased PPARγ mRNA levels in comparison with lean women [90]. Similarly, an upregulation of miR-27b, miR-130b and miR-138 in obese colorectal cancer patients was observed, while PPARγ was downregulated [91]. Likewise, miR-130 and miR-27a/b are known adipogenic inhibitors that directly target the major regulators of adipogenesis, PPARγ and C/EBPα by suppressing their expression [92]. MiR-20 has been shown to promote osteogenic differentiation in mesenchymal stem cells (MSCs), and it was confirmed using different assays that PPARγ, Bambi (BMP and activin membrane-bound inhibitor) and Crim1 (Cysteine-rich motor neuron 1) are direct targets of miR-20a [93]. Regarding the role of the PPARγ polymorphism rs3856806 at the onset of atherosclerosis, the results are contradictory. In a study with 787 Iranian individuals with CAD and dyslipidemia, it was shown that C1431T polymorphism was significantly associated with fasted serum lipid levels [94], while in a study with 2102 children from Greece, the CT+TT genotypes of C1431T polymorphism were associated with increased adiposity [95]. In addition, a meta-analysis study of eight studies confirmed the association of C161T polymorphism with an increased risk of [96]. On the contrary, the meta-analysis by Wang et al involving 29 studies failed to support a significant correlation of rs3856806 with the risk of atherosclerotic disease in general, except for the Caucasian and myocardial infarction subgroups [97]. Considering the current literature, further investigation is needed to shed light on the importance of rs3856806 in the development of atherosclerosis.
6. Cardiomyopathy
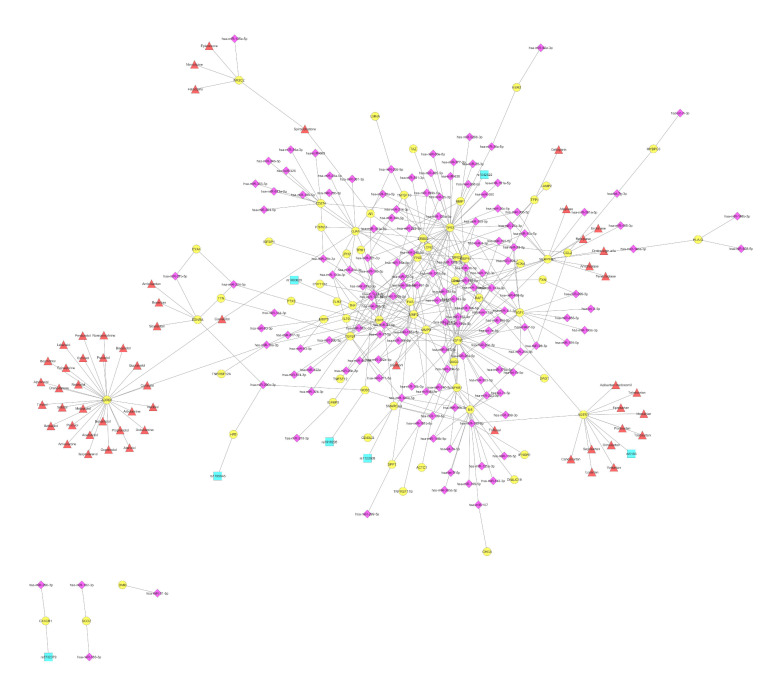
Cardiomyopathy refers to a collection of disorders of the heart muscle that lead to a reduced ability to pump blood efficiently. According to our in silico analysis, in this category the terms “cardiomyopathy”, “intrinsic cardiomyopathy”, and “dilated cardiomyopathy” are grouped together (Figure 1b). In general, 340 interactions between 67 genes and 145 unique miRNAs were identified, which is substantially fewer than those described for atherosclerosis, although the number of miRNAs remained roughly equal (Figure 4). Moreover, the average number of connections found between a VTG and miRNAs was 5.1, while most of the genes (47 out of 67; 70.15%) had less than five connections, and 10 out of 67 (14.93%) interacted with more than 10 candidate miRNAs. As shown in Table 2, the miRNAs that target most of the genes associated with cardiomyopathy are miR-21-5p, miR-24-3p, miR-145-5p, miR-138-5p, miR-143-3p, miR-17-5p, miR-155-5p, miR-125b-5p, miR-146a-5p, and miR-133b and six of them are also in the list of the most abundant in CVDs in general (Table 1). Of the 145 different miRNAs implicated in cardiomyopathy, miR-21-5p was found to target 10 genes, namely ERBB2, IGF1R, IL1B, MMP2, MMP9, PTX3, SMARCA4, TGFB1, TLR3, and TPM1 (Figure 4). MiR-21 has gained great attention because of its involvement in many biological processes and clinical conditions, and has also received increased attention due to its involvement in many biological processes, primarily in CVD. The increased expression of miR-21 was observed in the left ventricles of patients with dilated cardiomyopathy (DCM), but not in hypertrophic cardiomyopathy (HCM) [98]. In addition, there was no significant difference in the circulating miR-21 levels in patients with ischemic cardiomyopathy and DCM, but they were found to be significantly increased compared with the control group [99], suggesting their value as a biomarker for heart failure.
Figure 4.
Network of VTGs enriched within the DOSE term cardiomyopathy. The network displays 67 cardiomyopathy-associated VTGs (circles in yellow), as well as 145 miRNAs (diamonds in purple), seven SNPs (squares in turquoise) and 56 drugs (triangles in red) that are associated with CVD, and which target and/or affect it. The network was created using Cytoscape [59].
The Beta-1 adrenergic receptor (ADRB1) gene is by far the most drug-targeted gene, with 29 different compounds from the total 56 different drugs that have been identified to interact with genes associated with cardiomyopathies (Figure 4). Ser49Gly genetic polymorphism in the ADRB1 gene was associated with a low mean resting heart rate in a cohort study of >1000 individuals from China and Japan [100], while in another study Ser49Gly polymorphism was associated with reduced mortality risk in patients with congestive heart failure, probably through myocardial protection [101]. As shown in Figure 2, beta-adrenergic receptors are principal targets for beta-blockers, such as bisoprolol, metoprolol, propranolol and atenolol to treat angina, hypertension and heart failure.
Tumor protein P53 (TP53), which encodes for a tumor suppressor protein which is responsible for the regulation of the tumor-free survival of organisms, is regulated by 34 miRs (Table S4), which represent the highest number of miRNA-VTGs interactions (Figure 4). In cardiomyocytes, Tp53 plays a critical role in the regulation of the cardiac transcriptome [102], while elevated Tp53 levels have been associated with cardiac hypertrophy and remodeling [103]. Among the identified miRNAs, miR-34s has been extensively studied and recognized as the most prevalent miRNA induced by p53, not only in cancer where it suppresses tumor growth and metastasis, but also in non-cancerous diseases such as brain disorders, metabolic and cardiovascular diseases [104]. One of the most important miRNAs, miR-125b, which was the first discovered miRNA [105], has been also found to interact with TP53. In the latest study of Chen et al, cardiac-specific miR-125b-1 knockout mice were generated that displayed dysregulated fatty acid metabolism, leading to perinatal death and cardiac hypertrophy [106], a condition that eventually leads to cardiomyopathy and heart failure.
AGTR1 is the only gene out of the 67 cardiomyopathy-associated genes that revealed a connection with at least one miRNA, drug, and SNP. In particular, in full accordance with what is described in the atherosclerosis section, AGTR1 is a target for miR-155-5p, miR-34a-5p, and 11 drugs acting as angiotensin II receptor type 1 (AT1) antagonists, with its most widely studied polymorphism, rs5186, to be also associated in the connection map (Figure 4).
7. Lipid Metabolism Disorder
Dyslipidemia is one of the most important risk factors in the pathophysiological basis of CVDs and the development of atherosclerosis. Blood lipids are a complex environment that includes cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), lipoprotein A (Lp(a)), triglycerides and fatty acids. The most important lipid disorders affecting CAD occurrence risk are those related to an increased serum LDL level or a reduced HDL level. Despite the extensive research in the field and the development of lipid-lowering therapeutics such as statins that inhibit cholesterol synthesis, alternative treatment options and therefore novel pharmacological targets need to be discovered. According to our analysis under the term “lipid metabolism disorder”, the terms “lipid storage disease”, “lipid metabolism disorder” and “familial hyperlipidemia” are clustered (Figure 1b). The network presenting the correlations between VTGs associated with lipid metabolism disorder and miRNAs consists of 215 interactions, as shown in Figure 5. In general, 40 genes were recognized to interact with 109 different miRNAs, while 24 therapeutics target 11 of them. The most common miRNA in the lipid metabolism network is hsa-miR-138-5p, which is found to target eight different genes, namely CEBPA, FABP4, LPL, MMP3, NFKB1, SERPINE1, PPARG and TERT. In addition to miR-138-5p, the list of miRNAs with the most interactions with genes involved in lipid metabolism disorders is complete with miR-146a-5p, miR-26a-5p, miR-27a-3p, miR-145-5p, miR-130a-3p, miR-98-5p, miR-130b-3p, miR-223-3p, and miR-1-3p (Table 2). Except of miR-145-5p, all other miRNAs are not listed in Table 1 with most abundant miRNAs being involved in CVDs (Table 1). The most interactions were observed between epidermal growth factor receptor (EGFR) and 20 miRNAs (Table S4). Among them, miR-125a-5p and miR-7 were recently verified, by Western blot analysis, to target EGFR and thereby stimulate the growth, migration and invasion of VSMCs [107]. On the contrary, the study of Prasad et al, on the explanted hearts of transplant recipients with a diagnosis of DCM showed that the overexpression of miR-7 significantly reduces the expression of ERBB2 but not EGFR, in contrast to cancer cells [108,109]. Most of the myocardial energetic requirements in adults are derived from the oxidation of free fatty acids. In CVDs, the myocardial energy metabolism is disrupted, and a lack of energy or excessive fat accumulation is observed [110]. As was mentioned above, PPARγ is a major regulator of adipogenesis. According to our in silico analysis, PPARγ is the only VTG associated with lipid metabolism disorder that revealed interactions with miRNAs and is also a potential therapeutic target.
Figure 5.
Network of the VTGs enriched within the DOSE term lipid metabolism disorder. The network displays 40 lipid metabolism disorder-associated VTGs (circles in yellow), as well as 109 miRNAs (diamonds in purple), seven SNPs (squares in turquoise) and 24 drugs (triangles in red) that are associated with CVDs, and target and/or affect them. The network was created using Cytoscape [59].
Following this, the existing knowledge concerning miRNA biomarkers within each cluster of the three CVD terms—namely (a) atherosclerosis and coronary disease, (b) cardiomyopathy and heart failure, and (c) lipid metabolism disorders—will be discussed separately. This direction could advance pharmacogenomics-guided decisions and practical clinical utility by easily facilitating correlations between common CVD pathophysiological features, drug-gene targets, SNPs, and miRNA-genomic networks in different CVD clinical conditions.
8. The Clinical Implementation of the Biomarker miRNA Networks in the CVD Cluster of Atherosclerosis and Coronary Artery Disease
Atherosclerosis, the main cause of CAD, is a progressive inflammatory disease of the arterial wall, leading to endothelial dysfunction and apoptosis, lipid accumulation, and the subsequent formation of atheromatous plaques [111,112]. The occlusion of a coronary artery as a result of an atherosclerotic process can lead to acute MI, and to cell death due to the prolonged deprivation of the oxygen supply.
Despite miRNAs’ infancy in the research community, their ability to regulate protein expression has led to their implementation as a means to achieve earlier diagnoses and better therapeutics to combat the initiation, progression, and complications of atherosclerosis [113]. To date, the accumulated evidence has associated specific miRNA expression patterns with the development of atherosclerosis and CAD, which are two closely related conditions. This occurs due to miRNA’s participation in relevant molecular pathways, including endothelial dysfunction, cellular adhesion, proliferation, lipid uptake and efflux, the generation of inflammatory mediators, platelet and VSMC activation, and plaque formation [37,38]. A recent systematic review supported the hypothesis that some miRNAs may be involved in atherosclerotic expression in specific territories (carotid, inferior limbs/arteriosclerosis obliterans, renal artery), while others may be involved in the common mechanisms of atherosclerosis [114]. Several miRNAs can be delivered by apoptotic bodies to the atherosclerotic lesions [115]; therefore, the reduction of circulating miRNAs in patients with atherosclerosis/CAD might be attributed to an uptake of circulating miRNAs into atherosclerotic lesions [116,117].
Plenty of studies on patients with CAD, have demonstrated the downregulated expression of endothelial cell-enriched miRNAs (miR-126, miR-17, and miR-92a), and VSMC-enriched miRNAs (miR-145) [118,119]. In contrast, cardiomyocyte-enriched miRNAs (miR-133 and miR-208a) were upregulated [118]. The expression of pro-inflammatory cell-enriched miRNAs (miR-155) was reported to be either increased or reduced in patients with atherosclerosis [118,120].
Other research groups showed that patients with CAD had higher plasma levels of miR-133a, miR-150, miR-34a, miR-21, miR-30a, miR-146a, miR-146b, miR-106b, miR-206, miR-574-5p, miR-221, and miR-222 when compared to controls, while the ratio of miR-135a to miR-147 concentration was 19-fold higher in patients with CAD in comparison with healthy individuals [121,122,123,124]. On the contrary, patients with CAD had lower levels of miR-126-5p, miR-17-92, miR-31, and miR-720 when compared to healthy patients [125,126,127].
Nowadays, miRNA diagnostic panels have been developed to enhance discriminatory power for the detection of patients with atherosclerosis and CAD. In particular, miR-765, miR-149, and miR-424 were useful to discriminate both patients with stable and unstable CAD from controls [128]. Other combined panels comprise of: i. miR-24, miR-33, miR-103a, and miR-122 [129], ii. miR-155, -145, and let-7c [130] and iii. miR-132, miR-150, and miR-186 [131], which can provide a high diagnostic accuracy on CAD even in higher levels than cardiac TroponinI (cTnI) alone.
Additionally, miRNAs can also serve as the biomarkers which are required to differentiate Type I MI–due to atherosclerotic-plaque rupture (upregulated miR-1, miR-133a, miR-133b, and miR-499-5p, and downregulated miR-122 and miR-375) from Type II–MI due to supply/demand mismatch [132,133,134]. With regard to the subtype of MI, Ward et al. reported that miR-25-3p, miR-221-3p, and miR-374b-5p were strongly correlated with ST-Elevation Myocardial Infarction (STEMI), while miRs-221-3p and -483-5p were highly associated with non-ST-Elevation Myocardial Infarction (NSTEMI) [135]. The upregulation of a few other miRNAs (miR-134, miR-198, and miR-370) was uniquely linked to unstable angina (UA) compared to stable CAD, and can facilitate the diagnosis of UA, which can be elusive in some patients with normal troponin values [136].
Furthermore, a combined model of miR-483-5p and miR-451a can differentiate plaque rupture [125], while circulating miR-133a, miR-208a, miR-155, miR-145, miR-214, and miR-223 were strongly correlated with the severity of CAD [137,138,139,140]. Other studies suggest that circulating miRNAs (miR-19a, miR-208a, miR-133, and miR-499) might be detectable even earlier than the traditional prognostic biomarkers (cTnI, creatine kinase-MB (CK-MB), and brain natriuretic peptide (BNP)) [118,141]. Thus, in the near future, an miRNA panel, probably in conjunction with traditional biomarkers, might have a role to play in the emergency department, leading to the diagnosis of acute coronary syndrome with great sensitivity and accuracy.
The current miRNA therapeutics for atherosclerosis treatment is focused on the systemic administration of either anti-miRNAs (antagomirs) or synthetic miRNA mimics (miRNA mimetics), by using viral and non-viral delivery platforms as vehicles [142]. The delivery of miR-126 by apoptotic bodies was shown to counteract atherosclerosis, inducing vascular protection and facilitating the “fine-tuning” of atherosclerotic disease [143]. Other well-performed studies have demonstrated the cardioprotective potential of intercellular communication mechanisms by miRNA-containing extracellular vesicles [144]. Therapeutic miR-210 delivery has also been linked with the decreasing of the infarct size, as well as the improvement of angiogenesis and cardiac function [145].
Moreover, miRNAs may pave the way for personalized therapy in patients with atherosclerosis/CAD. They could potentially be used to identify patients who could benefit from antiplatelet treatment. This was evaluated in studies by measuring plasma miRNA’s response to antiplatelet treatment and platelet activation markers at different moments in the course of the treatment. Several platelet-related miRNAs (miR-223, miR-191, miR-126, and miR-150) were decreased as a result of platelet inhibition in the plasma (via P2Y12 expression pathway modulation) [35,43]. Hence, circulating miRNAs can provide tailored, effective antiplatelet therapy by monitoring its efficiency and detecting non-respondent patients.
9. The Clinical Implementation of the Biomarker miRNA Networks in the CVD Cluster of Cardiomyopathy and Heart Failure
Despite BNP and N-terminal (NT)-pro hormone BNP (NT-proBNP) being well-established gold-standard biomarkers for the evaluation of HF and cardiomyopathy progress, miRNAs seem to be able to play a role in the management of HF that frequently occurs in patients with cardiomyopathies [36,116,146]. Recently emerging evidence suggested, for the first time, that miRNA expression patterns (miR-1, miR-16, miR-21, miR-26a, miR-133, miR-146a, and miR-192) could differ in various forms of cardiomyopathy (hypertrophic, dilated, ischemic, diabetic, Tako-tsubo, peripartum, and pressure overload), especially when compared to that of normal hearts, thereby constituting biomarkers of high diagnostic and discriminatory value [147,148,149,150,151,152,153,154,155,156,157,158,159]. Moreover, upregulated miR-192 expression was independently associated with decreased survival rates in patients with ischemic cardiomyopathy but not in patients with non-ischemic cardiomyopathy [160], while left ventricular assist device treatment has succeeded in normalizing abnormal miRNAs expression in ischemic cardiomyopathy [161].
In particular, DCM is a complex disease with a common phenotype but heterogeneous pathological mechanisms, and early etiological diagnosis and risk stratification seems to be crucial for the clinical course of the disease. Despite the state-of-the-art imaging technology and genetic tests provided, novel non-invasive markers are still needed to guide the clinical decision-making [162]. To that end, miRNAs are emerging as a promising tool for the clinical management of DCM because it is intimately associated with an altered intracellular and circulating miRNA profile. MiR-21 was upregulated, and miR-29a, miR-29b, miR-29c, miR-133a, and miR-133b were downregulated in the apex, left, and right ventricles of patients with DCM compared with normal cardiac tissues [163]. MiR-1-3p and miR-27a were differentially expressed among the left ventricles of HCM and DCM patients with an optimal discrimination performance, with an area under the receiver operating characteristic curve (AUC) > 0.850 [98]. With regard to the DCM prognosis, patients with end-stage DCM showed a consistent miRNA pattern, with a downregulation of miR-7 and miR-378, and an upregulation of miR-214, miR-181b, and miR-423-5p [164]. In DCM, some myocardial miRNAs were found to predict the time-dependent reverse-remodeling response to β-blocker treatment [165]. Finally, anti-miR-34a therapy was shown to be more effective in females with moderate DCM than in males [166].
Mounting evidence suggests that miRNAs are involved in the development and progression of HF in general. Findings from different studies in patients with HF revealed an upregulation of some miRNAs (miR-21, miR-23a, miR-125b, miR-195, miR-199A, miR-214, and miR-342) and a downregulation of others (miR-1, miR-7, miR-29b, miR-30, miR-133, miR-150, and miR-378) [167]. Analogous to atherosclerosis, the combination of two or more miRNAs as a defined set (an miRNA signature) enhances the discriminatory power in HF as well. A study on HF with a reduced ejection fraction (HFrEF) identified eight miRNAs (miR-520d-5p, miR-558, miR-122, miR-200b, miR-622, miR-519e, miR-1231, and miR-1228) that reliably predicted the diagnosis of HFrEF (AUC = 0.81), and demonstrated a potential superiority of miRNA signatures over the quantification of single miRNA for diagnostic purposes [167,168].
As for HF with a preserved ejection fraction (HFpEF), three recent clinical studies assessed the capacity of circulating miRNAs to predict the differentiated diagnosis of HFPEF vs HFREF [169,170,171]. However, none of the identified miRNAs were reported more than once, and no validating results could be presented so far [169]. This emphasizes the need for the further development of larger clinical trials evaluating miRNAs in this disease entity. In particular, the exploration of signaling pathways and validation analyses in further clinical cohorts are of utmost importance [172].
10. The Clinical Implementation of the Biomarker miRNA Networks in the CVD Cluster of Lipid Metabolism Disorders
MiRNAs were reported as critical regulators of cholesterol metabolism, and genetic variations in miRNA loci were associated with alterations in human cholesterol and triglyceride levels. It is noteworthy that miRNAs have a two-way relationship with HDL cholesterol because they regulate several pathways of its metabolism, while at the same time HDL molecules provide a vehicle for circulating miRNAs [173]. Recent studies underline the potential utility of miRNA mimics and inhibitors in the treatment of lipid metabolism disorders. The association of miR-33 and miR-122 with the control of HDL cholesterol metabolism and other cellular functions associated with CVD has been demonstrated well in many studies [174]. The experimental inhibition of miR-33 and miR-122 in dyslipidemic mice by antisense oligonucleotides resulted in a marked increase in HDL levels and a significant decrease in VLDL levels within three months by amplifying cholesterol export and fatty acid β-oxidation [175,176]. However, some studies of the genetic ablation or chronic antagonism of these miRNAs in conjunction with the Western diet have reported adverse effects, including obesity, increased circulating triglyceride, hepatic steatosis, and hepatocellular carcinoma [177]. Further studies are also warranted to determine whether the silencing of miR-128-1 and miR-148a could alleviate dyslipidemia, obesity and insulin resistance [174,178].
On the other hand, high levels of miR-146a and miR-30c seem to have a positive effect on lipid metabolism by down-regulating lipid synthesis and lipoprotein secretion. Thus, their overexpression might be an attractive approach for the treatment of homozygous hypercholesterolemia by attenuating the intracellular lipid accumulation [179,180]. However, the inability to predict the exact mechanisms by which miRNAs exert their phenotypic effects raises some concerns about the clinical implementation of miRNA-based anti-hyperlipidemic treatments. Therefore, further experiments are necessary to elucidate the effects of individual miRNA targets on specific phenotypes, thereby facilitating the outcome evaluation of miRNA-based clinical trials for dyslipidemia [174].
11. Discussion
The practical clinical utility needed upon the translation of molecular information is stressfully evident upon the analysis of the application of pharmacogenomics (PGx) knowledge and biomarkers in the development of innovative therapeutics for CVDs. Our methodological bioinformatic approach and the data derived from this analysis contribute to uncover pharmacogenomics-guided therapeutic decisions in cardiovascular precision medicine, and to dissect miRNA-gene networks by mapping clinical utility roads for biomarkers’ implementation in diagnosis, treatment, and research. The latter is crucial because the new FDA drug approval with PGx labeling within the period of 2000–2020 in the era of cardiology was only 4.5%, compared to those for other therapeutic areas, i.e., oncology, with 49.4%; neurology, with 9.0%; infectious diseases, with 7.9%; psychiatry, with 5.6%; and inborn errors of metabolism, with 5.1% [181]. A similar demand is observed upon applying methodologies which are capable of exploiting genomic biomarkers in designed and executed clinical trials in the era of CVDs [182]. Furthermore, it was emphatically shown that the successful broad implementation of the concepts of precision cardiovascular medicine in the clinical setting presupposes that the pleiotropic molecular associations underlying biological pathways must be efficiently solved and mapped before the application of biomarkers for specific pathophysiological conditions [9]. Moreover, this direction must be seen in parallel with the practice-changing breakthroughs which have already taken place in cardiovascular medicine within the last couple of decades, but also with those advances envisioning machine learning technology, wearable devices and e-mobile data that pave the way for the achievement of the goal of the individualization of precision medicine [183]. To this end, the data presented in this article attempt to uncover clinical knowledge of practical utility in CVDs through the application of a pipeline bioinformatic analysis to map clinically-relevant and druggable miRNA-gene networks, along with the genomic signatures resulting from SNPs.
It is known that microRNAs affect cardiac cell development and heart-tissue homeostasis [184]. On the other hand, miRNA biogenesis presents dynamic nature in terms of the molecular pathways involved and the gene-target mechanisms underlying the miRNA-mediated regulation. Moreover, the maturation, secretion, transfer, uptake, and function of extracellular miRNAs in disease pathophysiology, such as CVD conditions, is still elusive in research and the clinical practice [185]. Differences in miRNA biology may also count in the case of acute and chronic pathophysiological CVD conditions, sex differences, and existing comorbidities [186]. This existing knowledge gap in miRNA biology clearly hampers the effective clinical experimentation and subsequent exploitation of miRNAs as reliable and concise biomarkers in the clinical setting of CVDs. In addition, the synthesis of miRNAs from tissues other than the cardiovascular system along with their subsequent release into plasma as extracellular vehicles (e.g., exosomes), adds further barriers towards the exploitation of miRNAs as circulating biomarkers in CVDs. To overcome such issues and rigorously validate reliable miRNA biomarkers for CVDs, it is urgent need the development of novel experimental in silico, mathematical and artificial intelligence methodologies to be applied in clinical trial design, research, and healthcare. To this end, it is interesting to note the recent development of an algorithm capable to trace microRNA organismal origin from sequencing data [187]. Also, the creation and application of physiologically-based pharmacokinetic (PBPK) models for the development of innovative genomics and nanotechnology therapeutics, along with their integration with bioinformatics tools, present promise for the successful clinical exploitation of the molecular knowledge, including miRNAs, in the years to come [3].
Many parameters were reported to alter the expression of miRNAs, and should therefore be considered before the interpretation of the results. First of all, it is argued that the quantification of miRNAs might be affected by the baseline characteristics of concomitant medication, such as statin, heparin, aspirin, and angiotensin-converting enzyme (ACE) inhibitor prescriptions [43,188]. Specifically, statins seem to decrease circulating miR-122 levels, antiplatelet drugs seem to alleviate the amount of freely circulating thrombocyte-derived miRNAs, and heparin seems to influence the polymerase chain reaction during the quantification process [189]. Moreover, renal function may significantly modify the circulating levels of miRNAs [190,191].
The major limitations of the use of miRNAs as novel biomarkers in everyday clinical practice are their laborious isolation, complex detection procedures, questionable cost-effectiveness, and non-standardized normalization methods [192], while there is still no consensus as to whether plasma or serum is a more reliable substrate for their measurement [116]. The integration of the use of miRNAs in everyday clinical practice will require the development of accurate, rapid, and inexpensive techniques. Furthermore, a substantial number of studies were either based on animal models or conducted on a small sample of human participants. Many of those studies have used different protocols, and often yielded contradictory conclusions about specific miRNA expression. Hence, larger-scale trials are warranted to assess the potential utility of miRNAs either as biomarkers or therapeutic molecules. Although most of the miRNAs studied are rarely superior to traditional biomarkers in terms of diagnostic accuracy, they can be used effectively as supplementary, rather than independent, diagnostic tests. In the near future, however, they may evolve into primary biomarkers which are used in the early stages of acute coronary syndrome management, when the enzyme levels in the bloodstream are still low and undetectable [116].
The development and execution of well-designed clinical trials to implement the molecular knowledge of multiple validated biomarkers per patient is required, and especially in CVDs, due to the various contributing risk factors and the heterogeneity observed in their pathophysiology. It is noteworthy to mention that only a very limited prospective use of genomic biomarkers in clinical trials related to new drug development as CVD therapeutics has been shown to exist, although there is genomic evidence for the investigated drug targets [179]. It has also been shown that the biomarker application in clinical trials of cardiovascular new drug development is much smaller than in other medical specialties such as oncology. Moreover, the inconsistences identified upon the use of biomarkers in clinical trials of CVDs have recently sparked discussions about the creation of international guidance on quality assurance in the selection and reliability of biomarkers, sample type, collection times, analytical methods, and storage for future research [193]. Complementary to this, lack of supportive cost-effectiveness of pharmacogenomics implementation in the everyday care of CVDs has been identified, thus calling for further improvement of clinical trial environment [194]. This shortcoming clearly highlights the gap between the design and execution of clinical trials, and the exploitation of genetic knowledge for the establishment of pharmacogenomics-guided decisions in the therapy of CVDs and the advancement of precision medicine. Moreover, the combinatorial nature of the factors modulating the genome function in physiology also seemingly contributes to CVDs’ pathophysiology. To this end, we recently published the design and execution of a prospective clinical study lying within the previously discussed concept of pharmacogenomics and precision medicine [52]. In particular, the design of this trial (GESS trial; ClinicalTrials.gov Identifier: NCT03150680), in addition to clinical, epidemiological and laboratory variables, was to include in each enrolled patient a targeted genomic analysis that covers 228 SNP biomarkers in a 117-gene network of pathophysiological and pharmacogenomic relevance. The severity of CAD in a real-world setting of patients undergoing coronary angiography was the primary rationale of the study, confirming the impact of the patients’ genomic profile in the susceptibility of CAD and the response to clopidogrel and statin therapy [52].
Nowadays, the availability of approaches for big health data analysis and the challenge of artificial intelligence methodologies offer hope for the effective treatment of complex classification, clustering, and predictive modeling tasks in cardiovascular research. Consequently, the handling and monitoring of CVD patients has been greatly benefited from such algorithms and practices based on artificial intelligence [195,196,197]. These efforts are parallel to the current healthcare environment, where the power in computerized systems allows the clinical implementation of data-driven machine learning platforms to guide therapeutic decisions in the clinical setting. Recently, by utilizing data from the GESS trial, we have developed a risk-stratification machine learning framework for the prediction of coronary artery disease severity. This data-driven predictive model, through the additional use of pharmacogenomics information, could additionally contribute to a more personalized therapy management and handling of CVD patients [198]. Overall, the use of machine learning platforms and the continuous development of relevant algorithms which are applied to predictive modeling obviously help practitioners to improve their practice and advance the progression of precision cardiovascular medicine.
Nonetheless, novel individualized treatments should be developed based on the existing knowledge of miRNAs. The manipulation of miRNAs and thus gene expression provides a revolutionary chance to block or even reverse the progression of atherosclerosis. However, a continuing restriction of miRNA-based therapies is the difficulty in achieving the steady, targeted delivery of pharmacological compounds to miRNA targets. Although the emergence of miRNA therapeutics has not yet been translated into FDA-approved candidates for medical intervention, candidate drugs are in clinical development, or in phase 1 and phase 2 clinical trials [199]. Hopefully, the merging of miRNA and nanomedicine technology will help in the translation of both of these powerful therapeutic tools, and will facilitate their integration into the daily clinical routine. In any case, however, by building infrastructures in the clinical setting of CVDs which are capable, in real-time, of implementing molecular knowledge, of contributing to interdisciplinary translational research efforts, of providing suitable registries and clinical databases, and of encouraging and facilitating the education of practitioners with synergies, the scientific society is expected to lead to rigorous and significant advancements in cardiovascular precision medicine and pharmacogenomics in the years to come.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cells11040607/s1. Table S1: multiMiR_CAD_miRNAs_results.xlsx; Table S2: DOSE_terms_enrichment_results.xlsx; Table S3: Reactome_pathways_enrichment_results.xlsx; Table S4: List of selected validated target genes (VTGs) with their interacting miRs.
Author Contributions
Conceptualization of the study, I.S.V., F.C.; methodology, K.A.K., I.S.V., F.C.; data curation, K.A.K., F.C.; writing—original draft preparation, F.C., K.A.K., I.S.V., C.I.P., E.G., A.S.P., E.K.; writing—review and editing, F.C., K.A.K., I.S.V., C.I.P., E.G., N.M., N.F.T., A.S.P., E.K., M.C., A.P., G.S., L.A., D.C.; supervision, I.S.V.; project administration, I.S.V., D.C., G.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was co-financed through the call for Proposals for the Action “Competitiveness, entrepreneurship & innovation” in the framework of the Operational Programme “Research, Create, Innovate” (Project Code: T1EDK-02354) of the Partnership Agreement for the Development Programme 2014–2020 by the European Social Fund (ESF) and Greek National funds.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Benjamin E.J., Muntner P., Alonso A., Bittencourt M.S., Callaway C.W., Carson A.P., Chamberlain A.M., Chang A.R., Cheng S., Das S.R., et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Vizirianakis I.S. Nanomedicine and personalized medicine toward the application of pharmacotyping in clinical practice to improve drug-delivery outcomes. Nanomed.-Nanotechnol. Biol. Med. 2011;7:11–17. doi: 10.1016/j.nano.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Vizirianakis I.S., Miliotou A.N., Mystridis G.A., Andriotis E.G., Andreadis I.I., Papadopoulou L.C., Fatouros D.G. Tackling pharmacological response heterogeneity by PBPK modeling to advance precision medicine productivity of nanotechnology and genomics therapeutics. Expert Rev. Precis. Med. Drug Dev. 2019;4:139–151. doi: 10.1080/23808993.2019.1605828. [DOI] [Google Scholar]
- 4.Vizirianakis I.S., Fatouros D.G. Personalized nanomedicine: Paving the way to the practical clinical utility of genomics and nanotechnology advancements. Adv. Drug Deliv. Rev. 2012;64:1359–1362. doi: 10.1016/j.addr.2012.09.034. [DOI] [PubMed] [Google Scholar]
- 5.Leopold J.A., Loscalzo J. Emerging Role of Precision Medicine in Cardiovascular Disease. Circ. Res. 2018;122:1302–1315. doi: 10.1161/CIRCRESAHA.117.310782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaiou M., El Amri H. Cardiovascular pharmacogenetics: A promise for genomically-guided therapy and personalized medicine. Clin. Genet. 2017;91:355–370. doi: 10.1111/cge.12881. [DOI] [PubMed] [Google Scholar]
- 7.Holmes M.V., Richardson T.G., Ference B.A., Davies N.M., Smith G.D. Integrating genomics with biomarkers and therapeutic targets to invigorate cardiovascular drug development. Nat. Rev. Cardiol. 2021;18:435–453. doi: 10.1038/s41569-020-00493-1. [DOI] [PubMed] [Google Scholar]
- 8.Morton S.U., Quiat D., Seidman J.G., Seidman C.E. Genomic frontiers in congenital heart disease. Nat. Rev. Cardiol. 2022;19:26–42. doi: 10.1038/s41569-021-00587-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Padmanabhan S., Dominiczak A.F. Genomics of hypertension: The road to precision medicine. Nat. Rev. Cardiol. 2021;18:235–250. doi: 10.1038/s41569-020-00466-4. [DOI] [PubMed] [Google Scholar]
- 10.Zhou S.S., Jin J.P., Wang J.Q., Zhang Z.G., Freedman J.H., Zheng Y., Cai L. MiRNAs in cardiovascular diseases: Potential biomarkers, therapeutic targets and challenges review-article. Acta Pharmacol. Sin. 2018;39:1073–1084. doi: 10.1038/aps.2018.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siasos G., Bletsa E., Stampouloglou P.K., Oikonomou E., Tsigkou V., Paschou S.A., Vlasis K., Marinos G., Vavuranakis M., Stefanadis C., et al. MicroRNAs in cardiovascular disease. Hell. J. Cardiol. HJC Hell. Kardiol. Ep. 2020;61:165–173. doi: 10.1016/j.hjc.2020.03.003. [DOI] [PubMed] [Google Scholar]
- 12.Akodad M., Mericskay M., Roubille F. Micro-RNAs as promising biomarkers in cardiac diseases. Ann. Transl. Med. 2016;4:551. doi: 10.21037/atm.2016.12.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghafouri-Fard S., Gholipour M., Taheri M. Role of microRNAs in the pathogenesis of coronary artery disease. Front. Cardiovasc. Med. 2021;8:632392. doi: 10.3389/fcvm.2021.632392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krammer T.L., Mayr M., Hackl M. microRNAs as promising biomarkers of platelet activity in antiplatelet therapy monitoring. Int. J. Mol. Sci. 2020;21:3477. doi: 10.3390/ijms21103477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schulte C., Karakas M., Zeller T. microRNAs in cardiovascular disease—Clinical application. Clin. Chem. Lab. Med. 2017;55:687–704. doi: 10.1515/cclm-2016-0576. [DOI] [PubMed] [Google Scholar]
- 16.Felekkis K., Papaneophytou C. Challenges in Using Circulating Micro-RNAs as Biomarkers for Cardiovascular Diseases. Int. J. Mol. Sci. 2020;21:561. doi: 10.3390/ijms21020561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Giassafaki L.P.N., Siqueira S., Panteris E., Psatha K., Chatzopoulou F., Aivaliotis M., Tzimagiorgis G., Mullertz A., Fatouros D.G., Vizirianakis I.S. Towards analyzing the potential of exosomes to deliver microRNA therapeutics. J. Cell. Physiol. 2021;236:1529–1544. doi: 10.1002/jcp.29991. [DOI] [PubMed] [Google Scholar]
- 18.Kaneto C.M., Nascimento J.S., Prado M., Mendonca L.S.O. Circulating miRNAs as biomarkers in cardiovascular diseases. Eur. Rev. Med. Pharmacol. Sci. 2019;23:2234–2243. doi: 10.26355/eurrev_201903_17271. [DOI] [PubMed] [Google Scholar]
- 19.Zamani P., Fereydouni N., Butler A.E., Navashenaq J.G., Sahebkar A. The therapeutic and diagnostic role of exosomes in cardiovascular diseases. Trends Cardiovasc. Med. 2019;29:313–323. doi: 10.1016/j.tcm.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Verduci L., Tarcitano E., Strano S., Yarden Y., Blandino G. CircRNAs: Role in human diseases and potential use as biomarkers. Cell Death Dis. 2021;12:468. doi: 10.1038/s41419-021-03743-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang L., Zhang Y., Wang Y., Zhao Y., Ding H., Li P. Circular RNAs: Functions and Clinical Significance in Cardiovascular Disease. Front. Cell Dev. Biol. 2020;8:584051. doi: 10.3389/fcell.2020.584051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Correia C.C.M., Rodrigues L.F., de Avila Pelozin B.R., Oliveira E.M., Fernandes T. Long Non-Coding RNAs in Cardiovascular Diseases: Potential Function as Biomarkers and Therapeutic Targets of Exercise Training. Non-Coding RNA. 2021;7:65. doi: 10.3390/ncrna7040065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yeh C.F., Chang Y.E., Lu C.Y., Hsuan C.F., Chang W.T., Yang K.C. Expedition to the missing link: Long noncoding RNAs in cardiovascular diseases. J. Biomed. Sci. 2020;27:48. doi: 10.1186/s12929-020-00647-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beermann J., Piccoli M.T., Viereck J., Thum T. Non-coding rnas in development and disease: Background, mechanisms, and therapeutic approaches. Physiol. Rev. 2016;96:1297–1325. doi: 10.1152/physrev.00041.2015. [DOI] [PubMed] [Google Scholar]
- 25.Mendell J.T., Olson E.N. MicroRNAs in stress signaling and human disease. Cell. 2012;148:1172–1187. doi: 10.1016/j.cell.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carthew R.W., Sontheimer E.J. Origins and Mechanisms of miRNAs and siRNAs. Cell. 2009;136:642–655. doi: 10.1016/j.cell.2009.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ishizu H., Siomi H., Siomi M.C. Biology of Piwi-interacting RNAs: New insights into biogenesis and function inside and outside of germlines. Genes Dev. 2012;26:2361–2373. doi: 10.1101/gad.203786.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schimmel P. RNA Processing and Modifications: The emerging complexity of the tRNA world: Mammalian tRNAs beyond protein synthesis. Nat. Rev. Mol. Cell Biol. 2018;19:45–58. doi: 10.1038/nrm.2017.77. [DOI] [PubMed] [Google Scholar]
- 29.Cordes K.R., Srivastava D. MicroRNA regulation of cardiovascular development. Circ. Res. 2009;104:724–732. doi: 10.1161/CIRCRESAHA.108.192872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Quiat D., Olson E.N. MicroRNAs in cardiovascular disease: From pathogenesis to prevention and treatment. J. Clin. Investig. 2013;123:11–18. doi: 10.1172/JCI62876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Rosa S., Curcio A., Indolfi C. Emerging role of micrornas in cardiovascular diseases. Circ. J. 2014;78:567–575. doi: 10.1253/circj.CJ-14-0086. [DOI] [PubMed] [Google Scholar]
- 32.Das S., Abdel-Mageed A.B., Adamidi C., Adelson P.D., Akat K.M., Alsop E., Ansel K.M., Arango J., Aronin N., Avsaroglu S.K., et al. The Extracellular RNA Communication Consortium: Establishing Foundational Knowledge and Technologies for Extracellular RNA Research. Cell. 2019;177:231–242. doi: 10.1016/j.cell.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Van Rooij E., Sutherland L.B., Liu N., Williams A.H., McAnally J., Gerard R.D., Richardson J.A., Olson E.N. A signature pattern of stress-responsive microRNAs that can evoke cardiac hypertrophy and heart failure. Proc. Natl. Acad. Sci. USA. 2006;103:18255–18260. doi: 10.1073/pnas.0608791103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wronska A., Kurkowska-Jastrzebska I., Santulli G. Application of microRNAs in diagnosis and treatment of cardiovascular disease. Acta Physiol. 2015;213:60–83. doi: 10.1111/apha.12416. [DOI] [PubMed] [Google Scholar]
- 35.Condorelli G., Latronico M.V.G., Cavarretta E. MicroRNAs in cardiovascular diseases: Current knowledge and the road ahead. J. Am. Coll. Cardiol. 2014;63:2177–2187. doi: 10.1016/j.jacc.2014.01.050. [DOI] [PubMed] [Google Scholar]
- 36.Keller T., Boeckel J.N., Groß S., Klotsche J., Palapies L., Leistner D., Pieper L., Stalla G.K., Lehnert H., Silber S., et al. Improved risk stratification in prevention by use of a panel of selected circulating microRNAs. Sci. Rep. 2017;7:4511. doi: 10.1038/s41598-017-04040-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Papageorgiou N., Tousoulis D., Androulakis E., Siasos G., Briasoulis A., Vogiatzi G., Kampoli A.M., Tsiamis E., Tentolouris C., Stefanadis C. The Role of microRNAs in Cardiovascular Disease. Curr. Med. Chem. 2012;19:2605–2610. doi: 10.2174/092986712800493048. [DOI] [PubMed] [Google Scholar]
- 38.Feinberg M.W., Moore K.J. MicroRNA Regulation of Atherosclerosis. Circ. Res. 2016;118:703–720. doi: 10.1161/CIRCRESAHA.115.306300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hosen M.R., Goody P.R., Zietzer A., Nickenig G., Jansen F. MicroRNAs as Master Regulators of Atherosclerosis: From Pathogenesis to Novel Therapeutic Options. Antioxid. Redox Signal. 2020;33:621–644. doi: 10.1089/ars.2020.8107. [DOI] [PubMed] [Google Scholar]
- 40.MacRae C.A., Vasan R.S. The future of genetics and genomics. Circulation. 2016;133:2634–2639. doi: 10.1161/CIRCULATIONAHA.116.022547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lin Y., Qian F., Shen L., Chen F., Chen J., Shen B. Computer-aided biomarker discovery for precision medicine: Data resources, models and applications. Brief. Bioinform. 2019;20:952–975. doi: 10.1093/bib/bbx158. [DOI] [PubMed] [Google Scholar]
- 42.Shi R., Ge L., Zhou X., Ji W.J., Lu R.Y., Zhang Y.Y., Zeng S., Liu X., Zhao J.H., Zhang W.C., et al. Decreased platelet miR-223 expression is associated with high on-clopidogrel platelet reactivity. Thromb. Res. 2013;131:508–513. doi: 10.1016/j.thromres.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 43.Willeit P., Zampetaki A., Dudek K., Kaudewitz D., King A., Kirkby N.S., Crosby-Nwaobi R., Prokopi M., Drozdov I., Langley S.R., et al. Circulating MicroRNAs as novel biomarkers for platelet activation. Circ. Res. 2013;112:595–600. doi: 10.1161/CIRCRESAHA.111.300539. [DOI] [PubMed] [Google Scholar]
- 44.Zhang Y.Y., Zhou X., Ji W.J., Shi R., Lu R.Y., Li J.L., Yang G.H., Luo T., Zhang J.Q., Zhao J.H., et al. Decreased circulating microRNA-223 level predicts high on-treatment platelet reactivity in patients with troponin-negative non-ST elevation acute coronary syndrome. J. Thromb. Thrombolysis. 2014;38:65–72. doi: 10.1007/s11239-013-1022-9. [DOI] [PubMed] [Google Scholar]
- 45.Peng L., Liu J., Qin L., Liu J., Xi S., Lu C., Yin T. Interaction between platelet-derived microRNAs and CYP2C19*2 genotype on clopidogrel antiplatelet responsiveness in patients with ACS. Thromb. Res. 2017;157:97–102. doi: 10.1016/j.thromres.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 46.Jiang Q.H., Wang Y.D., Hao Y.Y., Juan L.R., Teng M.X., Zhang X.J., Li M.M., Wang G.H., Liu Y.L. miR2Disease: A manually curated database for microRNA deregulation in human disease. Nucleic Acids Res. 2009;37:D98–D104. doi: 10.1093/nar/gkn714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ruepp A., Kowarsch A., Schmidl D., Buggenthin F., Brauner B., Dunger I., Fobo G., Frishman G., Montrone C., Theis F.J. PhenomiR: A knowledgebase for microRNA expression in diseases and biological processes. Genome Biol. 2010;11:R6. doi: 10.1186/gb-2010-11-1-r6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ru Y.B., Kechris K.J., Tabakoff B., Hoffman P., Radcliffe R.A., Bowler R., Mahaffey S., Rossi S., Calin G.A., Bemis L., et al. The multiMiR R package and database: Integration of microRNA-target interactions along with their disease and drug associations. Nucleic Acids Res. 2014;42:e133. doi: 10.1093/nar/gku631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hsu S.D., Lin F.M., Wu W.Y., Liang C., Huang W.C., Chan W.L., Tsai W.T., Chen G.Z., Lee C.J., Chiu C.M., et al. miRTarBase: A database curates experimentally validated microRNA-target interactions. Nucleic Acids Res. 2011;39:D163–D169. doi: 10.1093/nar/gkq1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Xiao F.F., Zuo Z.X., Cai G.S., Kang S.L., Gao X.L., Li T.B. miRecords: An integrated resource for microRNA-target interactions. Nucleic Acids Res. 2009;37:D105–D110. doi: 10.1093/nar/gkn851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li P.P.D., Fu Y.X., Ru J.L., Huang C., Du J.F., Zheng C.L., Chen X.T., Li P.P.D., Lu A.P., Yang L., et al. Insights from systems pharmacology into cardiovascular drug discovery and therapy. BMC Syst. Biol. 2014;8:s12918–s13014. doi: 10.1186/s12918-014-0141-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Vizirianakis I.S., Chatzopoulou F., Papazoglou A.S., Karagiannidis E., Sofdis G., Stalikas N., Stefopoulos C., Kyritsis K.A., Mittas N., Theodoroula N.F., et al. The GEnetic Syntax Score: A genetic risk assessment implementation tool grading the complexity of coronary artery disease-rationale and design of the GESS study. BMC Cardiovasc. Disord. 2021;21:284. doi: 10.1186/s12872-021-02122-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Yu G.C., Wang L.G., Yan G.R., He Q.Y. DOSE: An R/Bioconductor package for disease ontology semantic and enrichment analysis. Bioinformatics. 2015;31:608–609. doi: 10.1093/bioinformatics/btu684. [DOI] [PubMed] [Google Scholar]
- 54.Yu G.C., He Q.Y. ReactomePA: An R/Bioconductor package for reactome pathway analysis and visualization. Mol. Biosyst. 2016;12:477–479. doi: 10.1039/C5MB00663E. [DOI] [PubMed] [Google Scholar]
- 55.Wu T., Hu E., Xu S., Chen M., Guo P., Dai Z., Feng T., Zhou L., Tang W., Zhan L., et al. ClusterProfiler 4.0: A universal enrichment tool for interpreting omics data. Innovation. 2021;2:100141. doi: 10.1016/j.xinn.2021.100141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yu G.C., Wang L.G., Han Y.Y., He Q.Y. ClusterProfiler: An R Package for Comparing Biological Themes among Gene Clusters. Omics-A J. Integr. Biol. 2012;16:284–287. doi: 10.1089/omi.2011.0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wang J.Z., Du Z.D., Payattakool R., Yu P.S., Chen C.F. A new method to measure the semantic similarity of GO terms. Bioinformatics. 2007;23:1274–1281. doi: 10.1093/bioinformatics/btm087. [DOI] [PubMed] [Google Scholar]
- 58.Gu Z.G., Eils R., Schlesner M. Complex heatmaps reveal patterns and correlations in multidimensional genomic data. Bioinformatics. 2016;32:2847–2849. doi: 10.1093/bioinformatics/btw313. [DOI] [PubMed] [Google Scholar]
- 59.Shannon P., Markiel A., Ozier O., Baliga N.S., Wang J.T., Ramage D., Amin N., Schwikowski B., Ideker T. Cytoscape: A software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–2504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Moreau P.R., Bosch V.T., Bouvy-Liivrand M., Ounap K., Ord T., Pulkkinen H.H., Polonen P., Heinaniemi M., Yla-Herttuala S., Laakkonen J.P., et al. Profiling of Primary and Mature miRNA Expression in Atherosclerosis-Associated Cell Types. Arterioscler. Thromb. Vasc. Biol. 2021;41:2149–2167. doi: 10.1161/ATVBAHA.121.315579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Conrad T., Marsico A., Gehre M., Orom U.A. Microprocessor Activity Controls Differential miRNA Biogenesis In Vivo. Cell Rep. 2014;9:542–554. doi: 10.1016/j.celrep.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 62.Xiong X.D., Cho M., Cai X.P., Cheng J., Jing X., Cen J.M., Liu X., Yang X.L., Suh Y. A common variant in pre-miR-146 is associated with coronary artery disease risk and its mature miRNA expression. Mutat. Res.-Fundam. Mol. Mech. Mutagenesis. 2014;761:15–20. doi: 10.1016/j.mrfmmm.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 63.Quan X., Ji Y., Zhang C., Guo X., Zhang Y., Jia S., Ma W., Fan Y., Wang C. Circulating MiR-146a May be a Potential Biomarker of Coronary Heart Disease in Patients with Subclinical Hypothyroidism. Cell. Physiol. Biochem. 2018;45:226–236. doi: 10.1159/000486769. [DOI] [PubMed] [Google Scholar]
- 64.Dang L.T.H., Lawson N.D., Fish J.E. MicroRNA Control of Vascular Endothelial Growth Factor Signaling Output during Vascular Development. Arterioscler. Thromb. Vasc. Biol. 2013;33:193–200. doi: 10.1161/ATVBAHA.112.300142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Carmeliet P. Manipulating angiogenesis in medicine. J. Intern. Med. 2004;255:538–561. doi: 10.1111/j.1365-2796.2003.01297.x. [DOI] [PubMed] [Google Scholar]
- 66.Olsson A.K., Dimberg A., Kreuger J., Claesson-Welsh L. VEGF receptor signalling—In control of vascular function. Nat. Rev. Mol. Cell Biol. 2006;7:359–371. doi: 10.1038/nrm1911. [DOI] [PubMed] [Google Scholar]
- 67.Wang X., Sundquist K., Svensson P.J., Rastkhani H., Palmer K., Memon A.A., Sundquist J., Zoller B. Association of recurrent venous thromboembolism and circulating microRNAs. Clin. Epigenet. 2019;11:28. doi: 10.1186/s13148-019-0627-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhao Y.J., Yuan Y.Q., Qiu C.G. Underexpression of CACNA1C Caused by Overexpression of microRNA-29a Underlies the Pathogenesis of Atrial Fibrillation. Med. Sci. Monit. 2016;22:2175–2181. doi: 10.12659/MSM.896191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nickenig G., Harrison D.G. The AT1-type angiotensin receptor in oxidative stress and atherogenesis. Part II: AT1 receptor regulation. Circulation. 2002;105:530–536. doi: 10.1161/hc0402.102619. [DOI] [PubMed] [Google Scholar]
- 70.Zhu N., Zhang D., Chen S., Liu X., Lin L., Huang X., Guo Z., Liu J., Wang Y., Yuan W., et al. Endothelial enriched microRNAs regulate angiotensin II-induced endothelial inflammation and migration. Atherosclerosis. 2011;215:286–293. doi: 10.1016/j.atherosclerosis.2010.12.024. [DOI] [PubMed] [Google Scholar]
- 71.Zheng L., Xu C.C., Chen W.D., Shen W.L., Ruan C.C., Zhu L.M., Zhu D.L., Gao P.J. MicroRNA-155 regulates angiotensin II type 1 receptor expression and phenotypic differentiation in vascular adventitial fibroblasts. Biochem. Biophys. Res. Commun. 2010;400:483–488. doi: 10.1016/j.bbrc.2010.08.067. [DOI] [PubMed] [Google Scholar]
- 72.Haas U., Sczakiel G., Laufer S.D. MicroRNA-mediated regulation of gene expression is affected by disease-associated SNPs within the 3′-UTR via altered RNA structure. RNA Biol. 2012;9:924–937. doi: 10.4161/rna.20497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ceolotto G., Papparella I., Bortoluzzi A., Strapazzon G., Ragazzo F., Bratti P., Fabricio A.S.C., Squarcina E., Gion M., Palatini P., et al. Interplay between miR-155, AT1R A1166C polymorphism, and AT1R expression in young untreated hypertensives. Am. J. Hypertens. 2011;24:241–246. doi: 10.1038/ajh.2010.211. [DOI] [PubMed] [Google Scholar]
- 74.Stanković A., Kolaković A., Živković M., Djurić T., Bundalo M., Končar I., Davidović L., Alavantić D. Angiotensin receptor type 1 polymorphism A1166C is associated with altered AT1R and miR-155 expression in carotid plaque tissue and development of hypoechoic carotid plaques. Atherosclerosis. 2016;248:132–139. doi: 10.1016/j.atherosclerosis.2016.02.032. [DOI] [PubMed] [Google Scholar]
- 75.Goldstein J.L., Brown M.S. A century of cholesterol and coronaries: From plaques to genes to statins. Cell. 2015;161:161–172. doi: 10.1016/j.cell.2015.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kurtz C.L., Fannin E.E., Toth C.L., Pearson D.S., Vickers K.C., Sethupathy P. Inhibition of miR-29 has a significant lipid-lowering benefit through suppression of lipogenic programs in liver. Sci. Rep. 2015;5:12911. doi: 10.1038/srep12911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Liu M.X., Gao M., Li C.Z., Yu C.Z., Yan H., Peng C., Li Y., Li C.G., Ma Z.L., Zhao Y., et al. Dicer1/miR-29/HMGCR axis contributes to hepatic free cholesterol accumulation in mouse non-alcoholic steatohepatitis. Acta Pharmacol. Sin. 2017;38:660–671. doi: 10.1038/aps.2016.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Selitsky S.R., Dinh T.A., Toth C.L., Kurtz C.L., Honda M., Struck B.R., Kaneko S., Vickers K.C., Lemon S.M., Sethupathy P. Transcriptomic analysis of chronic hepatitis b and c and liver cancer reveals microrna-mediated control of cholesterol synthesis programs. mBio. 2015;6:e01500-15. doi: 10.1128/mBio.01500-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kirac D., Bayam E., Dagdelen M., Gezmis H., Sarikaya S., Pala S., Altunok E.C., Genc E. HMGCR and ApoE mutations may cause different responses to lipid lowering statin therapy. Cell. Mol. Biol. 2017;6:43–48. doi: 10.14715/cmb/2017.63.10.6. [DOI] [PubMed] [Google Scholar]
- 80.Bentzon J.F., Otsuka F., Virmani R., Falk E. Mechanisms of plaque formation and rupture. Circ. Res. 2014;114:1852–1866. doi: 10.1161/CIRCRESAHA.114.302721. [DOI] [PubMed] [Google Scholar]
- 81.Kolodgie F.D., Burke A.P., Farb A., Gold H.K., Yuan J., Narula J., Finn A.V., Virmani R. The thin-cap fibroatheroma: A type of vulnerable plaque the major precursor lesion to acute coronary syndromes. Curr. Opin. Cardiol. 2001;16:285–292. doi: 10.1097/00001573-200109000-00006. [DOI] [PubMed] [Google Scholar]
- 82.Misra A., Feng Z., Chandran R.R., Kabir I., Rotllan N., Aryal B., Sheikh A.Q., Ding L., Qin L., Fernández-Hernando C., et al. Integrin beta3 regulates clonality and fate of smooth muscle-derived atherosclerotic plaque cells. Nat. Commun. 2018;9:2073. doi: 10.1038/s41467-018-04447-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Motovska Z., Kvasnicka J., Widimsky P., Petr R., Hajkova J., Bobcikova P., Osmancik P., Odvodyova D., Katina S. Platelet glycoprotein GP VI 13254C allele is an independent risk factor of premature myocardial infarction. Thromb. Res. 2010;125:e61–e64. doi: 10.1016/j.thromres.2009.09.002. [DOI] [PubMed] [Google Scholar]
- 84.Weiss E.J., Bray P.F., Tayback M., Schulman S.P., Kickler T.S., Becker L.C., Weiss J.L., Gerstenblith G., Goldschmidt-Clermont P.J. A Polymorphism of a Platelet Glycoprotein Receptor as an Inherited Risk Factor for Coronary Thrombosis. N. Engl. J. Med. 1996;334:1090–1094. doi: 10.1056/NEJM199604253341703. [DOI] [PubMed] [Google Scholar]
- 85.Kucharska-Newton A.M., Monda K.L., Campbell S., Bradshaw P.T., Wagenknecht L.E., Boerwinkle E., Wasserman B.A., Heiss G. Association of the platelet GPIIb/IIIa polymorphism with atherosclerotic plaque morphology: The Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis. 2011;216:151–156. doi: 10.1016/j.atherosclerosis.2011.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Evans R.M., Barish G.D., Wang Y.X. PPARs and the complex journey to obesity. Nat. Med. 2004;10:355–361. doi: 10.1038/nm1025. [DOI] [PubMed] [Google Scholar]
- 87.Torra I.P., Chinetti G., Duval C., Fruchart J.C., Staels B. Peroxisome proliferator-activated receptors: From transcriptional control to clinical practice. Curr. Opin. Lipidol. 2001;12:245–254. doi: 10.1097/00041433-200106000-00002. [DOI] [PubMed] [Google Scholar]
- 88.Tyagi S., Gupta P., Saini A., Kaushal C., Sharma S. The peroxisome proliferator-activated receptor: A family of nuclear receptors role in various diseases. J. Adv. Pharm. Technol. Res. 2011;2:236–240. doi: 10.4103/2231-4040.90879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Chandra M., Miriyala S., Panchatcharam M. PPAR γ and Its Role in Cardiovascular Diseases. PPAR Res. 2017;2017:6404638. doi: 10.1155/2017/6404638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lee E.K., Lee M.J., Abdelmohsen K., Kim W., Kim M.M., Srikantan S., Martindale J.L., Hutchison E.R., Kim H.H., Marasa B.S., et al. miR-130 Suppresses Adipogenesis by Inhibiting Peroxisome Proliferator-Activated Receptor Expression. Mol. Cell. Biol. 2011;31:626–638. doi: 10.1128/MCB.00894-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Motawi T.K., Shaker O.G., Ismail M.F., Sayed N.H. Peroxisome Proliferator-Activated Receptor Gamma in Obesity and Colorectal Cancer: The Role of Epigenetics. Sci. Rep. 2017;7:10714. doi: 10.1038/s41598-017-11180-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lin Q., Gao Z., Alarcon R.M., Ye J., Yun Z. A role of miR-27 in the regulation of adipogenesis. FEBS J. 2009;276:2348–2358. doi: 10.1111/j.1742-4658.2009.06967.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhang J.F., Fu W.M., He M.L., Xie W.D., Lv Q., Wan G., Li G., Wang H., Lu G., Hu X., et al. MiRNA-20a promotes osteogenic differentiation of human mesenchymal stem cells by co-regulating BMP signaling. RNA Biol. 2011;8:829–838. doi: 10.4161/rna.8.5.16043. [DOI] [PubMed] [Google Scholar]
- 94.Oladi M., Nohtani M., Avan A., Mirhafez S.R., Tajbakhsh A., Ghasemi F., Asadi A., Elahdadi Salmani M., Mohammadi A., Hoseinzadeh L., et al. Impact of the C1431T polymorphism of the peroxisome proliferator activated receptor-gamma (PPAR-γ) gene on fasted serum lipid levels in patients with coronary artery disease. Ann. Nutr. Metab. 2015;66:149–154. doi: 10.1159/000381358. [DOI] [PubMed] [Google Scholar]
- 95.Lagou V., Scott R.A., Manios Y., Chen T.L.J., Wang G., Grammatikaki E., Kortsalioudaki C., Liarigkovinos T., Moschonis G., Roma-Giannikou E., et al. Impact of peroxisome proliferator-activated receptors γ and δ on adiposity in toddlers and preschoolers in the GENESIS study. Obesity. 2008;16:913–918. doi: 10.1038/oby.2008.1. [DOI] [PubMed] [Google Scholar]
- 96.Ding S., Liu L., Zhuge Q.C., Yu Z., Zhang X., Xie J., Hong W., Wang S., Yang Y., Chen B. The meta-analysis of the association of PPARG P12A, C161T polymorphism and coronary heart disease. Wien. Klin. Wochenschr. 2012;124:671–677. doi: 10.1007/s00508-012-0223-0. [DOI] [PubMed] [Google Scholar]
- 97.Wang P., Wang Q., Yin Y., Yang Z., Li W., Liang D., Zhou P. Association between peroxisome proliferator-activated receptor gamma gene polymorphisms and atherosclerotic diseases: A meta-analysis of case-control studies. J. Atheroscler. Thromb. 2015;22:912–925. doi: 10.5551/jat.26138. [DOI] [PubMed] [Google Scholar]
- 98.Li M., Chen X., Chen L., Chen K., Zhou J., Song J. MiR-1-3p that correlates with left ventricular function of HCM can serve as a potential target and differentiate HCM from DCM. J. Transl. Med. 2018;16:161. doi: 10.1186/s12967-018-1534-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhang J., Xing Q., Zhou X., Li J., Li Y., Zhang L., Zhou Q., Tang B. Circulating miRNA-21 is a promising biomarker for heart failure. Mol. Med. Rep. 2017;16:7766–7774. doi: 10.3892/mmr.2017.7575. [DOI] [PubMed] [Google Scholar]
- 100.Ranade K., Jorgenson E., Sheu W.H.-H., Pei D., Hsiung C.A., Chiang F.T., Chen Y.D.I., Pratt R., Olshen R.A., Curb D., et al. A polymorphism in the α1 adrenergic receptor is associated with resting heart rate. Am. J. Hum. Genet. 2002;70:935–942. doi: 10.1086/339621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Börjesson M., Magnusson Y., Hjalmarson Å., Andersson B. A novel polymorphism in the gene coding for the beta1-adrenergic receptor associated with survival in patients with heart failure. Eur. Heart J. 2000;21:1853–1858. doi: 10.1053/euhj.1999.1994. [DOI] [PubMed] [Google Scholar]
- 102.Mak T.W., Hauck L., Grothe D., Billia F. p53 regulates the cardiac transcriptome. Proc. Natl. Acad. Sci. USA. 2017;114:2331–2336. doi: 10.1073/pnas.1621436114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Nomura S., Satoh M., Fujita T., Higo T., Sumida T., Ko T., Yamaguchi T., Tobita T., Naito A.T., Ito M., et al. Cardiomyocyte gene programs encoding morphological and functional signatures in cardiac hypertrophy and failure. Nat. Commun. 2018;9:4435. doi: 10.1038/s41467-018-06639-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rokavec M., Li H., Jiang L., Hermeking H. The p53/miR-34 axis in development and disease. J. Mol. Cell Biol. 2014;6:214–230. doi: 10.1093/jmcb/mju003. [DOI] [PubMed] [Google Scholar]
- 105.Lee R.C., Feinbaum R.L., Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. doi: 10.1016/0092-8674(93)90529-Y. [DOI] [PubMed] [Google Scholar]
- 106.Chen C.Y., Lee D.S., Choong O.K., Chang S.K., Hsu T., Nicholson M.W., Liu L.W., Lin P.J., Ruan S.C., Lin S.W., et al. Cardiac-specific microRNA-125b deficiency induces perinatal death and cardiac hypertrophy. Sci. Rep. 2021;11:2377. doi: 10.1038/s41598-021-81700-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhou H., Sen L.I.N., Youdong H.U., Dianxuan G.U.O., Wang Y., Xia L.I. miR-125a-5p and miR-7 inhibits the proliferation, migration and invasion of vascular smooth muscle cell by targeting EGFR. Mol. Med. Rep. 2021;24:708. doi: 10.3892/mmr.2021.12347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Prasad S.V.N., Gupta M.K., Duan Z.H., Surampudi V.S.K., Liu C.G., Kotwal A., Moravec C.S., Starling R.C., Perez D.M., Sen S., et al. A unique microRNA profile in end-stage heart failure indicates alterations in specific cardiovascular signaling networks. PLoS ONE. 2017;12:e0170456. doi: 10.1371/journal.pone.0170456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ritter C.A., Arteaga C.L. The epidermal growth factor receptor-tyrosine kinase: A promising therapeutic target in solid tumors. Semin. Oncol. 2003;30:3–11. doi: 10.1053/sonc.2003.50027. [DOI] [PubMed] [Google Scholar]
- 110.Dyck J.R.B., Lopaschuk G.D. Malonyl CoA Control of Fatty Acid Oxidation in the Ischemic Heart. J. Mol. Cell. Cardiol. 2002;34:1099–1109. doi: 10.1006/jmcc.2002.2060. [DOI] [PubMed] [Google Scholar]
- 111.Gimbrone M.A., García-Cardeña G. Endothelial Cell Dysfunction and the Pathobiology of Atherosclerosis. Circ. Res. 2016;118:620–636. doi: 10.1161/CIRCRESAHA.115.306301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Libby P., Ridker P.M., Hansson G.K. Progress and challenges in translating the biology of atherosclerosis. Nature. 2011;473:317–325. doi: 10.1038/nature10146. [DOI] [PubMed] [Google Scholar]
- 113.Lu Y., Thavarajah T., Gu W.D., Cai J.J., Xu Q.B. Impact of miRNA in Atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2018;38:E159–E170. doi: 10.1161/ATVBAHA.118.310227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Pereira-da-Silva T., Cruz M.C., Carrusca C., Ferreira R.C., Napoleao P., Carmo M.M. Circulating microRNA profiles in different arterial territories of stable atherosclerotic disease: A systematic review. Am. J. Cardiovasc. Dis. 2018;8:1–13. [PMC free article] [PubMed] [Google Scholar]
- 115.Zernecke A., Bidzhekov K., Noels H., Shagdarsuren E., Gan L., Denecke B., Hristov M., Koppel T., Jahantigh M.N., Lutgens E., et al. Delivery of MicroRNA-126 by Apoptotic Bodies Induces CXCL12-Dependent Vascular Protection. Sci. Signal. 2009;2:ra81. doi: 10.1126/scisignal.2000610. [DOI] [PubMed] [Google Scholar]
- 116.Economou E.K., Oikonomou E., Siasos G., Papageorgiou N., Tsalamandris S., Mourouzis K., Papaioanou S., Tousoulis D. The role of microRNAs in coronary artery disease: From pathophysiology to diagnosis and treatment. Atherosclerosis. 2015;241:624–633. doi: 10.1016/j.atherosclerosis.2015.06.037. [DOI] [PubMed] [Google Scholar]
- 117.Jansen F., Yang X., Proebsting S., Hoelscher M., Przybilla D., Baumann K., Schmitz T., Dolf A., Endl E., Franklin B.S., et al. MicroRNA expression in circulating microvesicles predicts cardiovascular events in patients with coronary artery disease. J. Am. Heart Assoc. 2014;3:e001249. doi: 10.1161/JAHA.114.001249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Fichtlscherer S., De Rosa S., Fox H., Schwietz T., Fischer A., Liebetrau C., Weber M., Hamm C.W., Roxe T., Muller-Ardogan M., et al. Circulating MicroRNAs in Patients With Coronary Artery Disease. Circ. Res. 2010;107:677–684. doi: 10.1161/CIRCRESAHA.109.215566. [DOI] [PubMed] [Google Scholar]
- 119.Santulli G. microRNAs Distinctively Regulate Vascular Smooth Muscle and Endothelial Cells: Functional Implications in Angiogenesis, Atherosclerosis, and In-Stent Restenosis. Microrna Basic Sci. Mol. Biol. Clin. Pract. 2015;887:53–77. doi: 10.1007/978-3-319-22380-3_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wei Y.Y., Nazari-Jahantigh M., Neth P., Weber C., Schober A. MicroRNA-126,-145, and -155 A Therapeutic Triad in Atherosclerosis? Arterioscler. Thromb. Vasc. Biol. 2013;33:449–454. doi: 10.1161/ATVBAHA.112.300279. [DOI] [PubMed] [Google Scholar]
- 121.Fang Q., Tian M., Wang F., Zhang Z.H., Du T.Y., Wang W., Yang Y., Li X.Q., Chen G.Z., Xiao L., et al. Amlodipine induces vasodilation via Akt2/Sp1-activated miR-21 in smooth muscle cells. Br. J. Pharmacol. 2019;176:2306–2320. doi: 10.1111/bph.14679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Takahashi Y., Satoh M., Minami Y., Tabuchi T., Itoh T., Nakamura M. Expression of miR-I 46a/b is associated with the Toll-like receptor 4 signal in coronary artery disease: Effect of renin-angiotensin system blockade and statins on miRNA-I 46a/b and Toll-like receptor 4 levels. Clin. Sci. 2010;119:395–405. doi: 10.1042/CS20100003. [DOI] [PubMed] [Google Scholar]
- 123.Zhang Y.J., Liu D.Q., Chen X., Li J., Li L.M., Bian Z., Sun F., Lu J.W., Yin Y.A., Cai X., et al. Secreted Monocytic miR-150 Enhances Targeted Endothelial Cell Migration. Mol. Cell. 2010;39:133–144. doi: 10.1016/j.molcel.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 124.Zhou J.Q., Shao G.F., Chen X.L., Yang X., Huang X.Y., Peng P., Ba Y.N., Zhang L., Jehangir T., Bu S.Z., et al. miRNA 206 and miRNA 574-5p are highly expression in coronary artery disease. Biosci. Rep. 2016;36:e00295. doi: 10.1042/BSR20150206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Li H.Y., Zhao X., Liu Y.Z., Meng Z., Wang D., Yang F., Shi Q.W. Plasma MicroRNA-126-5p is Associated with the Complexity and Severity of Coronary Artery Disease in Patients with Stable Angina Pectoris. Cell. Physiol. Biochem. 2016;39:837–846. doi: 10.1159/000447794. [DOI] [PubMed] [Google Scholar]
- 126.Tang Y., Zhang Y.C., Chen Y., Xiang Y., Shen C.X., Li Y.G. The role of miR-19b in the inhibition of endothelial cell apoptosis and its relationship with coronary artery disease. Sci. Rep. 2015;5:15132. doi: 10.1038/srep15132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Wang H.W., Huang T.S., Lo H.H., Huang P.H., Lin C.C., Chang S.J., Liao K.H., Tsai C.H., Chan C.H., Tsai C.F., et al. Deficiency of the MicroRNA-31-MicroRNA-720 Pathway in the Plasma and Endothelial Progenitor Cells from Patients With Coronary Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2014;34:857–869. doi: 10.1161/ATVBAHA.113.303001. [DOI] [PubMed] [Google Scholar]
- 128.Sayed A.S.M., Xia K., Li F., Deng X., Salma U., Li T.B., Deng H., Yang D.F., Zhou H.Y., Yang T.L., et al. The diagnostic value of circulating microRNAs for middle-aged (40-60-year-old) coronary artery disease patients. Clinics. 2015;70:257–263. doi: 10.6061/clinics/2015(04)07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Dong J., Liang Y.Z., Zhang J., Wu L.J., Wang S., Hua Q., Yan Y.X. Potential Role of Lipometabolism-Related MicroRNAs in Peripheral Blood Mononuclear Cells as Biomarkers for Coronary Artery Disease. J. Atheroscler. Thromb. 2017;24:430–441. doi: 10.5551/jat.35923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Vindis C., Faccini J., Ruidavets J.B., Cordelier P., Martins F., Maoret J.J., Ferrieres J., Elbaz M., Bongard V., Ferrieres J., et al. Circulating miR-155, miR-145 and let-7c as diagnostic biomarkers of the coronary artery disease. Atherosclerosis. 2017;263:E277. doi: 10.1016/j.atherosclerosis.2017.06.892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zeller T., Keller T., Ojeda F., Reichlin T., Twerenbold R., Tzikas S., Wild P.S., Reiter M., Czyz E., Lackner K.J., et al. Assessment of microRNAs in patients with unstable angina pectoris. Eur. Heart J. 2014;35:2106–2114. doi: 10.1093/eurheartj/ehu151. [DOI] [PubMed] [Google Scholar]
- 132.D’Alessandra Y., Devanna P., Limana F., Straino S., Di Carlo A., Brambilla P.G., Rubino M., Carena M.C., Spazzafumo L., De Simone M., et al. Circulating microRNAs are new and sensitive biomarkers of myocardial infarction. Eur. Heart J. 2010;31:2765–2773. doi: 10.1093/eurheartj/ehq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Thygesen K., Alpert J.S., Jaffe A.S., Simoons M.L., Chaitman B.R., White H.D., Katus H.A., Apple F.S., Lindahl B., Morrow D.A., et al. Third Universal Definition of Myocardial Infarction. Circulation. 2012;126:2020–2035. doi: 10.1161/CIR.0b013e31826e1058. [DOI] [PubMed] [Google Scholar]
- 134.Wang R.R., Li N., Zhang Y.H., Ran Y.Q., Pu J.L. Circulating MicroRNAs are Promising Novel Biomarkers of Acute Myocardial Infarction. Intern. Med. 2011;50:1789–1795. doi: 10.2169/internalmedicine.50.5129. [DOI] [PubMed] [Google Scholar]
- 135.Ward J.A., Esa N., Pidikiti R., Freedman J.E., Keaney J.F., Tanriverdi K., Vitseva O., Ambros V., Lee R., McManus D.D. Circulating Cell and Plasma microRNA Profiles Differ between Non-ST-Segment and ST-Segment-Elevation Myocardial Infarction. Fam. Med. Med. Sci. Res. 2013;2:108. doi: 10.4172/2327-4972.1000108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu S.D., Guo X.M., Zhong W., Weng R.Q., Liu J., Gu X.D., Zhong Z.X. Circulating MicroRNA Expression Profiles in Patients with Stable and Unstable Angina. Clinics. 2020;75:e1546. doi: 10.6061/clinics/2020/e1546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Gao H., Guddeti R.R., Matsuzawa Y., Liu L.P., Su L.X., Guo D., Nie S.P., Du J., Zhang M. Plasma Levels of microRNA-145 Are Associated with Severity of Coronary Artery Disease. PLoS ONE. 2015;10:e0123477. doi: 10.1371/journal.pone.0123477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Guo J.F., Zhang Y., Zheng Q.X., Zhang Y., Zhou H.H., Cui L.M. Association between elevated plasma microRNA-223 content and severity of coronary heart disease. Scand. J. Clin. Lab. Investig. 2018;78:373–378. doi: 10.1080/00365513.2018.1480059. [DOI] [PubMed] [Google Scholar]
- 139.Lu H.Q., Liang C., He Z.Q., Fan M., Wu Z.G. Circulating miR-214 is associated with the severity of coronary artery disease. J. Geriatr. Cardiol. 2013;10:34–38. doi: 10.3724/Sp.J.1263.2013.01011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Qiu X.K., Ma J. Alteration in microRNA-155 level correspond to severity of coronary heart disease. Scand. J. Clin. Lab. Investig. 2018;78:219–223. doi: 10.1080/00365513.2018.1435904. [DOI] [PubMed] [Google Scholar]
- 141.Zhong J.F., He Y., Chen W.J., Shui X.R., Chen C., Lei W. Circulating microRNA-19a as a Potential Novel Biomarker for Diagnosis of Acute Myocardial Infarction. Int. J. Mol. Sci. 2014;15:20355–20364. doi: 10.3390/ijms151120355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Gadde S., Rayner K.J. Nanomedicine Meets microRNA: Current Advances in RNA-Based Nanotherapies for Atherosclerosis. Arterioscler. Thromb. Vasc. Biol. 2016;36:e73–e79. doi: 10.1161/ATVBAHA.116.307481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Sun C.X., Alkhoury K., Wang Y.I., Foster G.A., Radecke C.E., Tam K., Edwards C.M., Facciotti M.T., Armstrong E.J., Knowlton A.A., et al. IRF-1 and miRNA126 Modulate VCAM-1 Expression in Response to a High-Fat Meal. Circ. Res. 2012;111:1054–1064. doi: 10.1161/CIRCRESAHA.112.270314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Hergenreider E., Heydt S., Tréguer K., Boettger T., Horrevoets A.J.G., Zeiher A.M., Scheffer M.P., Frangakis A.S., Yin X., Mayr M., et al. Atheroprotective communication between endothelial cells and smooth muscle cells through miRNAs. Nat. Cell Biol. 2012;14:249–256. doi: 10.1038/ncb2441. [DOI] [PubMed] [Google Scholar]
- 145.Hu S., Huang M., Li Z., Jia F., Ghosh Z., Lijkwan M.A., Fasanaro P., Sun N., Wang X., Martelli F., et al. MicroRNA-210 as a novel therapy for treatment of ischemic heart disease. Circulation. 2010;122:S124–S131. doi: 10.1161/CIRCULATIONAHA.109.928424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Briasoulis A., Tousoulis D., Vogiatzi G., Siasos G., Papageorgiou N., Oikonomou E., Genimata V., Konsola T., Stefanadis C. MicroRNAs: Biomarkers for Cardiovascular Disease in Patients with Diabetes Mellitus. Curr. Top. Med. Chem. 2013;13:1533–1539. doi: 10.2174/15680266113139990102. [DOI] [PubMed] [Google Scholar]
- 147.Carè A., Catalucci D., Felicetti F., Bonci D., Addario A., Gallo P., Bang M.L., Segnalini P., Gu Y., Dalton N.D., et al. MicroRNA-133 controls cardiac hypertrophy. Nat. Med. 2007;13:613–618. doi: 10.1038/nm1582. [DOI] [PubMed] [Google Scholar]
- 148.Chen J.-F., Murchison E.P., Tang R., Callis T.E., Tatsuguchi M., Deng Z., Rojas M., Hammond S.M., Schneider M.D., Selzman C.H., et al. Targeted deletion of Dicer in the heart leads to dilated cardiomyopathy and heart failure. Proc. Natl. Acad. Sci. USA. 2008;105:2111–2116. doi: 10.1073/pnas.0710228105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Cheng Y., Ji R., Yue J., Yang J., Liu X., Chen H., Dean D.B., Zhang C. MicroRNAs Are Aberrantly Expressed in Hypertrophic Heart. Am. J. Pathol. 2007;170:1831–1840. doi: 10.2353/ajpath.2007.061170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Halkein J., Tabruyn S.P., Ricke-Hoch M., Haghikia A., Nguyen N.-Q.-N., Scherr M., Castermans K., Malvaux L., Lambert V., Thiry M., et al. MicroRNA-146a is a therapeutic target and biomarker for peripartum cardiomyopathy. J. Clin. Investig. 2013;123:2143–2154. doi: 10.1172/JCI64365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Ikeda S., He A., Kong S.W., Lu J., Bejar R., Bodyak N., Lee K.-H., Ma Q., Kang P.M., Golub T.R., et al. MicroRNA-1 Negatively Regulates Expression of the Hypertrophy-Associated Calmodulin and Mef2a Genes. Mol. Cell. Biol. 2009;29:2193–2204. doi: 10.1128/MCB.01222-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Jaguszewski M., Osipova J., Ghadri J.-R., Napp L.C., Widera C., Franke J., Fijalkowski M., Nowak R., Fijalkowska M., Volkmann I., et al. A signature of circulating microRNAs differentiates takotsubo cardiomyopathy from acute myocardial infarction. Eur. Heart J. 2014;35:999–1006. doi: 10.1093/eurheartj/eht392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Jakubik D., Fitas A., Eyileten C., Jarosz-Popek J., Nowak A., Czajka P., Wicik Z., Sourij H., Siller-Matula J.M., De Rosa S., et al. MicroRNAs and long non-coding RNAs in the pathophysiological processes of diabetic cardiomyopathy: Emerging biomarkers and potential therapeutics. Cardiovasc. Diabetol. 2021;20:55. doi: 10.1186/s12933-021-01245-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kuwabara Y., Ono K., Horie T., Nishi H., Nagao K., Kinoshita M., Watanabe S., Baba O., Kojima Y., Shizuta S., et al. Increased MicroRNA-1 and MicroRNA-133a Levels in Serum of Patients With Cardiovascular Disease Indicate Myocardial Damage. Circ. Cardiovasc. Genet. 2011;4:446–454. doi: 10.1161/CIRCGENETICS.110.958975. [DOI] [PubMed] [Google Scholar]
- 155.Zhao Y., Ransom J.F., Li A., Vedantham V., von Drehle M., Muth A.N., Tsuchihashi T., McManus M.T., Schwartz R.J., Srivastava D. Dysregulation of Cardiogenesis, Cardiac Conduction, and Cell Cycle in Mice Lacking miRNA-1-2. Cell. 2007;129:303–317. doi: 10.1016/j.cell.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 156.Sucharov C., Bristow M.R., Port J.D. miRNA expression in the failing human heart: Functional correlates. J. Mol. Cell. Cardiol. 2008;45:185–192. doi: 10.1016/j.yjmcc.2008.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Song X.-W., Li Q., Lin L., Wang X.-C., Li D.-F., Wang G.-K., Ren A.-J., Wang Y.-R., Qin Y.-W., Yuan W.-J., et al. MicroRNAs are dynamically regulated in hypertrophic hearts, and miR-199a is essential for the maintenance of cell size in cardiomyocytes. J. Cell. Physiol. 2010;225:437–443. doi: 10.1002/jcp.22217. [DOI] [PubMed] [Google Scholar]
- 158.Oikonomou E., Zografos T., Papamikroulis G.-A., Siasos G., Vogiatzi G., Theofilis P., Briasoulis A., Papaioannou S., Vavuranakis M., Gennimata V., et al. Biomarkers in Atrial Fibrillation and Heart Failure. Curr. Med. Chem. 2019;26:873–887. doi: 10.2174/0929867324666170830100424. [DOI] [PubMed] [Google Scholar]
- 159.Pordzik J., Jakubik D., Jarosz-Popek J., Wicik Z., Eyileten C., De Rosa S., Indolfi C., Siller-Matula J.M., Czajka P., Postula M. Significance of circulating microRNAs in diabetes mellitus type 2 and platelet reactivity: Bioinformatic analysis and review. Cardiovasc. Diabetol. 2019;18:113. doi: 10.1186/s12933-019-0918-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Klenke S., Eul S., Peters J., Neumann T., Adamzik M., Frey U.H. Circulating miR-192 is a prognostic marker in patients with ischemic cardiomyopathy. Future Cardiol. 2018;14:283–289. doi: 10.2217/fca-2017-0108. [DOI] [PubMed] [Google Scholar]
- 161.Schipper M.E.I., van Kuik J., de Jonge N., Dullens H.F.J., de Weger R.A. Changes in Regulatory MicroRNA Expression in Myocardium of Heart Failure Patients on Left Ventricular Assist Device Support. J. Heart Lung Transplant. 2008;27:1282–1285. doi: 10.1016/j.healun.2008.09.005. [DOI] [PubMed] [Google Scholar]
- 162.Calderon-Dominguez M., Belmonte T., Quezada-Feijoo M., Ramos-Sánchez M., Fernández-Armenta J., Pérez-Navarro A., Cesar S., Peña-Peña L., Vea À., Llorente-Cortés V., et al. Emerging role of microRNAs in dilated cardiomyopathy: Evidence regarding etiology. Transl. Res. 2020;215:86–101. doi: 10.1016/j.trsl.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 163.Wang Y., Li M., Xu L., Liu J., Wang D., Li Q., Wang L., Li P., Chen S., Liu T. Expression of Bcl-2 and microRNAs in cardiac tissues of patients with dilated cardiomyopathy. Mol. Med. Rep. 2017;15:359–365. doi: 10.3892/mmr.2016.5977. [DOI] [PubMed] [Google Scholar]
- 164.Fan K.-L., Zhang H.-F., Shen J., Zhang Q., Li X.-L. Circulating microRNAs levels in Chinese heart failure patients caused by dilated cardiomyopathy. Indian Heart J. 2013;65:12–16. doi: 10.1016/j.ihj.2012.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Sucharov C.C., Kao D.P., Port J.D., Karimpour-Fard A., Quaife R.A., Minobe W., Nunley K., Lowes B.D., Gilbert E.M., Bristow M.R. Myocardial microRNAs associated with reverse remodeling in human heart failure. JCI Insight. 2017;2:e89169. doi: 10.1172/jci.insight.89169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bernardo B.C., Ooi J.Y., Matsumoto A., Tham Y.K., Singla S., Kiriazis H., Patterson N.L., Sadoshima J., Obad S., Lin R.C. Sex differences in response to miRNA-34a therapy in mouse models of cardiac disease: Identification of sex-, disease- and treatment-regulated miRNAs. J. Physiol. 2016;594:5959–5974. doi: 10.1113/JP272512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Schulte C. Diagnostic and prognostic value of circulating microRNAs in heart failure with preserved and reduced ejection fraction. World J. Cardiol. 2015;7:843. doi: 10.4330/wjc.v7.i12.843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Vogel B., Keller A., Frese K.S., Leidinger P., Sedaghat-Hamedani F., Kayvanpour E., Kloos W., Backe C., Thanaraj A., Brefort T., et al. Multivariate miRNA signatures as biomarkers for non-ischaemic systolic heart failure. Eur. Heart J. 2013;34:2812–2823. doi: 10.1093/eurheartj/eht256. [DOI] [PubMed] [Google Scholar]
- 169.Nair N., Kumar S., Gongora E., Gupta S. Circulating miRNA as novel markers for diastolic dysfunction. Mol. Cell. Biochem. 2013;376:33–40. doi: 10.1007/s11010-012-1546-x. [DOI] [PubMed] [Google Scholar]
- 170.Watson C.J., Gupta S.K., O’Connell E., Thum S., Glezeva N., Fendrich J., Gallagher J., Ledwidge M., Grote-Levi L., McDonald K., et al. MicroRNA signatures differentiate preserved from reduced ejection fraction heart failure. Eur. J. Heart Fail. 2015;17:405–415. doi: 10.1002/ejhf.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Wong L.L., Armugam A., Sepramaniam S., Karolina D.S., Lim K.Y., Lim J.Y., Chong J.P.C., Ng J.Y.X., Chen Y.-T., Chan M.M.Y., et al. Circulating microRNAs in heart failure with reduced and preserved left ventricular ejection fraction. Eur. J. Heart Fail. 2015;17:393–404. doi: 10.1002/ejhf.223. [DOI] [PubMed] [Google Scholar]
- 172.Peterlin A., Počivavšek K., Petrovič D., Peterlin B. The Role of microRNAs in Heart Failure: A Systematic Review. Front. Cardiovasc. Med. 2020;7:161. doi: 10.3389/fcvm.2020.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Vickers K.C., Palmisano B.T., Shoucri B.M., Shamburek R.D., Remaley A.T. MicroRNAs are transported in plasma and delivered to recipient cells by high-density lipoproteins. Nat. Cell Biol. 2011;17:104. doi: 10.1038/ncb3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Aryal B., Singh A.K., Rotllan N., Price N., Fernandez-Hernando C. MicroRNAs and lipid metabolism. Curr. Opin. Lipidol. 2017;28:273–280. doi: 10.1097/MOL.0000000000000420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Rayner K.J., Esau C.C., Hussain F.N., McDaniel A.L., Marshall S.M., van Gils J.M., Ray T.D., Sheedy F.J., Goedeke L., Liu X.Q., et al. Inhibition of miR-33a/b in non-human primates raises plasma HDL and lowers VLDL triglycerides. Nature. 2011;478:404–407. doi: 10.1038/nature10486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Wagschal A., Najafi-Shoushtari S.H., Wang L., Goedeke L., Sinha S., deLemos A.S., Black J.C., Ramírez C.M., Li Y., Tewhey R., et al. Genome-wide identification of microRNAs regulating cholesterol and triglyceride homeostasis. Nat. Med. 2015;21:1290–1297. doi: 10.1038/nm.3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Horie T., Nishino T., Baba O., Kuwabara Y., Nakao T., Nishiga M., Usami S., Izuhara M., Sowa N., Yahagi N., et al. MicroRNA-33 regulates sterol regulatory element-binding protein 1 expression in mice. Nat. Commun. 2013;4:2883. doi: 10.1038/ncomms3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Esau C., Davis S., Murray S.F., Yu X.X., Pandey S.K., Pear M., Watts L., Booten S.L., Graham M., McKay R., et al. miR-122 regulation of lipid metabolism revealed by in vivo antisense targeting. Cell Metab. 2006;3:87–98. doi: 10.1016/j.cmet.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 179.Soh J., Iqbal J., Queiroz J., Fernandez-Hernando C., Hussain M.M. MicroRNA-30c reduces hyperlipidemia and atherosclerosis in mice by decreasing lipid synthesis and lipoprotein secretion. Nat. Med. 2013;19:892–900. doi: 10.1038/nm.3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Yang K., He Y.S., Wang X.Q., Lu L., Chen Q.J., Liu J., Sun Z., Shen W.F. MiR-146a inhibits oxidized low-density lipoprotein-induced lipid accumulation and inflammatory response via targeting toll-like receptor 4. FEBS Lett. 2011;585:854–860. doi: 10.1016/j.febslet.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 181.Kim J.A., Ceccarelli R., Lu C.Y. Pharmacogenomic Biomarkers in US FDA-Approved Drug Labels (2000–2020) J. Pers. Med. 2021;11:179. doi: 10.3390/jpm11030179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Adeniyi O., Ramamoorthy A., Schuck R., Sun J., Wilson J., Zineh I., Pacanowski M. An Overview of Genomic Biomarker Use in Cardiovascular Disease Clinical Trials. Clin. Pharmacol. Ther. 2019;106:841–846. doi: 10.1002/cpt.1473. [DOI] [PubMed] [Google Scholar]
- 183.Kalman J.M., Lavandero S., Mahfoud F., Nahrendorf M., Yacoub M.H., Zhao D. Looking back and thinking forwards—15 years of cardiology and cardiovascular research. Nat. Reviews. Cardiol. 2019;16:651–660. doi: 10.1038/s41569-019-0261-7. [DOI] [PubMed] [Google Scholar]
- 184.Colpaert R.M.W., Calore M. Epigenetics and microRNAs in cardiovascular diseases. Genomics. 2021;113:540–551. doi: 10.1016/j.ygeno.2020.12.042. [DOI] [PubMed] [Google Scholar]
- 185.O’Brien J., Hayder H., Zayed Y., Peng C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018;9:402. doi: 10.3389/fendo.2018.00402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Mannon E.C., Ray S.C., Ryan M.J. Does sex matter? An update on the implementation of sex as a biological variable in research. Am. J. Physiol.-Ren. Physiol. 2020;318:F329–F331. doi: 10.1152/ajprenal.00575.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Kang W., Eldfjell Y., Fromm B., Estivill X., Biryukova I., Friedländer M.R. miRTrace reveals the organismal origins of microRNA sequencing data. Genome Biol. 2018;19:213. doi: 10.1186/s13059-018-1588-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Weber M., Baker M.B., Patel R.S., Quyyumi A.A., Bao G., Searles C.D. MicroRNA Expression Profile in CAD Patients and the Impact of ACEI/ARB. Cardiol. Res. Pract. 2011;2011:532915. doi: 10.4061/2011/532915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Kaudewitz D., Zampetaki A., Mayr M. MicroRNA Biomarkers for Coronary Artery Disease? Curr. Atheroscler. Rep. 2015;17:70. doi: 10.1007/s11883-015-0548-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Gidlöf O., Andersson P., van der Pals J., Götberg M., Erlinge D. Cardiospecific microRNA Plasma Levels Correlate with Troponin and Cardiac Function in Patients with ST Elevation Myocardial Infarction, Are Selectively Dependent on Renal Elimination, and Can Be Detected in Urine Samples. Cardiology. 2011;118:217–226. doi: 10.1159/000328869. [DOI] [PubMed] [Google Scholar]
- 191.Singh N., Heggermont W., Fieuws S., Vanhaecke J., Van Cleemput J., De Geest B. Endothelium-enriched microRNAs as diagnostic biomarkers for cardiac allograft vasculopathy. J. Heart Lung Transplant. 2015;34:1376–1384. doi: 10.1016/j.healun.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 192.Sato F., Tsuchiya S., Terasawa K., Tsujimoto G. Intra-Platform Repeatability and Inter-Platform Comparability of MicroRNA Microarray Technology. PLoS ONE. 2009;4:e5540. doi: 10.1371/journal.pone.0005540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Januzzi J.L., Jr., Canty J.M., Das S., DeFilippi C.R., Gintant G.A., Gutstein D.E., Jaffe A., Kaushik E.P., Leptak C., Mehta C., et al. Gaining Efficiency in Clinical Trials With Cardiac Biomarkers: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2021;77:1922–1933. doi: 10.1016/j.jacc.2021.02.040. [DOI] [PubMed] [Google Scholar]
- 194.Zhu Y., Swanson K.M., Rojas R.L., Wang Z., St Sauver J.L., Visscher S.L., Prokop L.J., Bielinski S.J., Wang L., Weinshilboum R., et al. Systematic review of the evidence on the cost-effectiveness of pharmacogenomics-guided treatment for cardiovascular diseases. Genet. Med. 2020;22:475–486. doi: 10.1038/s41436-019-0667-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Silverio A., Cavallo P., De Rosa R., Galasso G. Big Health Data and Cardiovascular Diseases: A Challenge for Research, an Opportunity for Clinical Care. Front. Med. 2019;6:36. doi: 10.3389/fmed.2019.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Seetharam K., Brito D., Farjo P.D., Sengupta P.P. The Role of Artificial Intelligence in Cardiovascular Imaging: State of the Art Review. Front. Cardiovasc. Med. 2020;7:618849. doi: 10.3389/fcvm.2020.618849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Judd R.M. Machine Learning in Medical Imaging: All Journeys Begin With a Single Step. JACC Cardiovasc. Imaging. 2020;13:696–698. doi: 10.1016/j.jcmg.2019.08.028. [DOI] [PubMed] [Google Scholar]
- 198.Mittas N., Chatzopoulou F., Kyritsis K.A., Papagiannopoulos C.I., Theodoroula N.F., Papazoglou A.S., Karagiannidis E., Sofidis G., Moysidis D.V., Stalikas N., et al. A Risk-Stratification Machine Learning Framework for the Prediction of Coronary Artery Disease Severity: Insights from the GESS Trial. Front. Cardiovasc. Med. 2022;8:812182. doi: 10.3389/fcvm.2021.812182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Hanna J., Hossain G.S., Kocerha J. The Potential for microRNA Therapeutics and Clinical Research. Front. Genet. 2019;10:478. doi: 10.3389/fgene.2019.00478. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.