Abstract
Inadvertent tracheal tube misplacement and particularly endobronchial intubation are well-known complications of emergency endotracheal intubation (ETI) in pediatric trauma patients, which require repositioning of the tube to avoid impairment of gas exchange. The main aim of study was to identify the frequency of tube misplacement and associated factors of pediatric trauma patients who received ETI either by prehospital physician-staffed emergency medical service (EMS), or at emergency department (ED) admission to a single level-1 trauma center. Sixty-five patients (median age 14 years and median injury severity score 29) were included. Of these, 30 underwent helicopter EMS ETI, 29 ground EMS ETI, and 6 ED ETI. Seventeen cases (26%) of tracheal tube misplacement were recognized. After multivariable analysis, tracheal tube misplacement was independently negatively associated with body weight (OR 0.86; 95% CI, 0.76–0.99; p = 0.032) and helicopter EMS ETI (OR 0.20; 95% CI, 0.04–0.97; p = 0.036). Two of nineteen patients received tube thoracostomy due to endobronchial intubation. Mortality and length of stay were comparable in patients with misplaced tubes and correctly placed tubes. The results suggest that particularly small children require attention to avoid tracheal tube misplacement, which emphasizes the need for special training. Helicopter EMS physicians’ expertise might be beneficial in prehospital pediatric trauma patients requiring advanced airway management.
Keywords: pediatric trauma, tracheal intubation, airway management, helicopter emergency medical service
1. Introduction
Advanced airway management in pediatric patients is a challenge for emergency medical service (EMS) providers because of the considerable physiological and anatomical differences and a much lower frequency compared to adults [1,2,3]. In the United States, the estimated pediatric out-of-hospital tracheal intubation rate is 6.7 per 1000 cases [1]. According to a recent meta-analysis, the risk of intubation failure is 3.54-fold higher in pediatric patients than in adults [4]. Success rates vary considerably depending on the EMS system, whereas physician-staffed providers, particularly physician-staffed helicopter EMS, may have higher expertise than paramedic-based systems [5,6,7,8,9].
Unrecognized esophageal intubation accounts for the most fatal mechanical complication, ultimately leading to hypoxia and death. Tracheal intubation into one mainstem bronchus may cause impairment of gas exchange and lung atelectasis [10]. Furthermore, unrecognized endobronchial intubation may also lead to avoidable chest tube placement at the unventilated chest side due to absent breath sounds mimicking pneumothorax [11,12]. Although there is previous evidence that children are prone to endobronchial intubation, studies identifying associated factors are scarce [12,13,14,15,16,17,18,19,20,21].
Thus, the aim of this study was, first, to analyze the frequency of tracheal tube misplacement in a study cohort of pediatric trauma patients that had intubation performed by either prehospital EMS or in the emergency department of a tertiary care hospital, and second, to identify associated factors and clinical consequences of this complication.
2. Materials and Methods
2.1. Study Design
Data from pediatric trauma patients who underwent prehospital or emergency department intubation were retrospectively analyzed regarding the need for tracheal tube replacement due to misplacement and particularly endobronchial intubation (the raw data can be found in Table S1). The analysis of associated factors with tube misplacement included demographic data, management characteristics, and outcomes of patients, comparing cases with correctly placed tubes and cases with misplaced tubes. Furthermore, we investigated all patients who underwent tube thoracostomy, particularly those with tracheal tube misplacement. This study was approved by the Ethics Committee of the Medical Faculty of Leipzig, Germany (No. 441/15-ek), which waived the need for informed consent. The study was retrospectively registered at the German Clinical Trials Register under DRKS-ID: DRKS00028045.
2.2. Patient Enrollment
The local trauma registry of the University Hospital Leipzig was retrospectively reviewed for pediatric trauma patients admitted from January 2008 to December 2019. The inclusion criteria were age < 18 years, admission directly from the scene of the accident, and emergency tracheal intubation in the prehospital setting at the scene of the accident or during management in the emergency department. Patients with supraglottic airway devices were excluded. Tracheal tube malposition requiring replacement was defined as unrecognized esophageal intubation, endobronchial intubation (detected on CT scans, plane chest radiography, and by auscultation), and tube dislocations or critical tube-to-carina distances with tube positions less than two centimeters above the carina (identified on either CT scans or plane chest radiography). Data were obtained from medical records, the radiological information system, and the picture archiving and communication system (MEDOS RIS version 9.3.3008, Nexus MagicWeb Version VA60C_0115, Visage Imaging, PACS: syngo.plaza, Siemens Healthcare, Erlangen, Germany).
2.3. General Management
Prehospital care of pediatric major trauma patients was performed by emergency response physicians until hospital admission. In the City of Leipzig and the greater Leipzig area, there were 19 physician-staffed ground EMS bases and 4 helicopter EMS bases. One ground EMS base was stationed at the study hospital and was exclusively run by their physicians. These physicians mainly worked in departments of anesthesiology, trauma surgery, or emergency department and attended 2–4 shifts per month at the EMS base. Two helicopter EMS of the Leipzig region were staffed with physicians from the study center and two other tertiary care hospitals. Airway management equipment of all prehospital EMS providers contained direct laryngoscopy devices (Macintosh blades), supraglottic airway devices (laryngeal tubes or laryngeal masks), and surgical airway devices (percutaneous devices using the Seldinger technique, or open cricothyroidotomy). Video laryngoscopy devices (including Macintosh-style blades and hyper-angulated blades) were available on two physician-staffed EMS helicopters in the greater Leipzig area, whereas most ground-based EMS providers had also introduced them in their physician-staffed rapid response units. Airway management equipment of the emergency department was comparable to EMS devices and additionally included fiberoptic bronchoscopes for awake fiberoptic intubation.
Emergency department and trauma room management were organized according to the recommendations of the German Society of Pediatric Surgery (DGKCH) and the German Society of Trauma Surgery (DGU) [22,23]. The trauma room activation was performed by the EMS teams at the scene or by a dispatcher of the Leipzig Fire Control Center. After standardized clinical assessment and under consideration of individual condition, emergency sonography and an initial whole-body CT were performed, whereas critically unstable children were transferred directly to the operating room or underwent only head CT. In children who underwent chest CT or plane chest radiography (CXR), tracheal tube positions were classified according to tube-to-carina distances (TCDs), where available. TCD was measured using the RIS/PACS.
2.4. Statistical Analysis
The data are reported as the mean (standard deviation (SD)) for normally distributed data, as the median (interquartile range (IQR)) for non-normally distributed data, and as numbers (percentages). Patient characteristics were compared by applying Fisher’s exact test and the Mann–Whitney U test or Student’s t-test for non-normally and normally distributed variables, respectively. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated in the framework of logistic regression analysis, comparing correctly placed tubes and tubes requiring replacement. The investigated associations for tubes requiring replacement were age, sex, height, weight, body mass index (BMI), injury severity score (ISS), admission systolic blood pressure (SBP) values, Glasgow coma scale (GCS) scores, SpO2 values, American Society of Anesthesiologists (ASA) classification, chest CT or plain chest radiography (CXR) data, and performances of emergency surgery and cardiopulmonary resuscitation (CPR). Age groups were infants (<1 year), pre-school children (1–5 years), schoolchildren (6–11 years), and adolescents (12–17 years). The investigated outcome factors were length of stay in the pediatric intensive care unit (PICU), ventilator days, 24 h mortality, and 30-day mortality. Data on procedure details (intubation situs and complications) and qualification levels of providers were primarily collected. In case the number of missing data on these variables was high, no further analysis was performed. The alpha level of significance was set at 0.05 without correction for multiple testing as we followed an exploratory approach. All tests were two-tailed. Multivariable analysis was performed on parameters found to be statistically significant in univariable analysis (p ≤ 0.05) to assess independent associations applying stepwise logistic regression based on Akaike’s information criterion, as implemented in the stepAIC function of the R addon package MASS 7.3.54. All analyses were performed in the framework of R 4.1.1.
3. Results
3.1. Baseline Characteristics
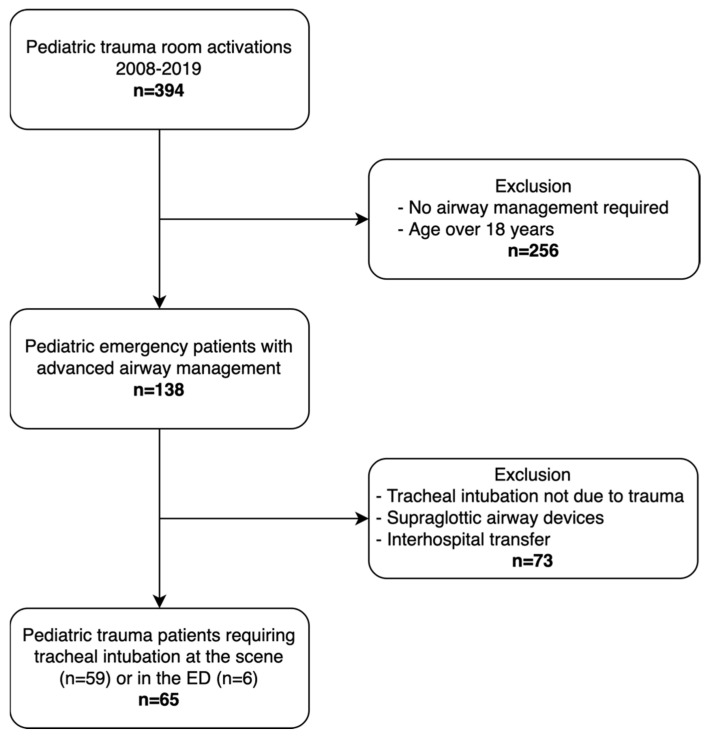
Sixty-five children met the inclusion criteria and were analyzed (Figure 1). The baseline characteristics are displayed in Table 1. Median patient age was 14 years (IQR 8.5). Patients’ ages were distributed as follows: infants under one year: none (0.0%), preschool children (1 to 5 years): 12 (18.5%), schoolchildren (6–11 years): 14 (21.5%), and adolescents (12–18 years): 39 (60.0%). The blunt trauma mechanism was exclusively recorded (61.5% road traffic accidents, 23.1% falls from height, and 15.4% blunt trauma of other causes). The median ISS was 29 (IQR 21). Tracheal intubation was attempted in the prehospital setting in 59 patients (90.8%; 30 by helicopter EMS and 29 by ground EMS) and in the emergency department in 6 patients (9.2%). After intubation, all patients received capnography monitoring to confirm the tracheal tube position.
Figure 1.
Study flowchart.
Table 1.
Baseline characteristics of the study cohort.
| Overall | Tracheal Tube Position Correct | Tracheal Tube Misplacement | p | |
|---|---|---|---|---|
| n (%) | 65 (100) | 48 (73.8) | 17 (26.2) | |
| Age (years) | 14.0 (8.5) | 16 (4) | 9 (7.5) | <0.001 |
| Male, n (%) | 40 (62) | 31 (65) | 9 (53) | 0.404 |
| Height (cm) | 165 (48) | 170 (22) | 127 (42) | <0.001 |
| Weight (kg) | 51.2 (25.1) | 59.2 (23.5) | 28.7 (13.1) | <0.001 |
| BMI | 20.4 (4.7) | 21.5 (4.8) | 17.7 (2) | <0.001 |
| GCS | 8 (8) | 8 (10.5) | 4 (7) | 0.317 |
| SBP (mmHg) | 100 (85.5) | 100 (78.5) | 90 (110) | 0.208 |
| HR (min−1) | 100 (37.5) | 102.5 (44.5) | 98 (77) | 0.153 |
| SpO2 (%) | 95 (18) | 93 (17.3) | 97 (52) | 0.116 |
| ISS | 29 (21) | 26 (19.5) | 29 (27) | 0.373 |
| RTA, n (%) | 40 (61.5) | 30 (62.5) | 10 (58.8) | 0.781 |
| Fall from height, n (%) | 15 (23.1) | 11 (22.9) | 4 (23.5) | 1 |
| Other cause n (%) | 10 (15.4) | 7 (14.6) | 3 (17.6) | 0.713 |
| Helicopter EMS ETI, n (%) | 30 (46.2) | 26 (54.2) | 4 (23.5) | 0.046 |
| Ground EMS ETI, n (%) | 29 (44.6) | 18 (37.5) | 11 (64.7) | 0.087 |
| ED ETI, n (%) | 6 (9.2) | 4 (8.3) | 2 (11.8) | 0.648 |
| CPR prior ED, n (%) | 19 (29) | 13 (27) | 6 (35) | 0.546 |
| WBCT, n (%) | 43 (66.2) | 33 (68.8) | 10 (58.8) | 0.554 |
| CCT only | 10 (15.3) | 6 (12.5) | 4 (23.5) | 0.434 |
| No CT | 12 (18.5) | 8 (16.7) | 4 (23.5) | 0.713 |
| Emergency surgery, n (%) | 46 (70.8) | 37 (66.7) | 9 (52.9) | 0.071 |
| Ventilator (days) | 1.0 (5) | 1.0 (5) | 1 (6) | 0.596 |
| PICU (days) | 5.0 (11.5) | 5.0 (11.5) | 6 (12) | 0.611 |
| 24 h mortality, n (%) | 8 (12.3) | 5 (10.4) | 3 (17.6) | 0.421 |
| 30-day mortality, n (%) | 18 (27.7) | 12 (25.0) | 6 (35.3) | 0.529 |
BMI, body mass index; GCS, Glasgow coma scale; SBP, systolic blood pressure; HR, heart rate; SpO2, peripheral oxygen saturation; ISS, injury severity score; RTA, road traffic accident; EMS, emergency medical service; ETI, endotracheal intubation; ED, emergency department; CPR, cardiopulmonary resuscitation; WBCT, whole-body computed tomography; CCT, cranial computed tomography; CT, computed tomography; PICU, pediatric intensive care unit. Squared brackets indicate interquartile ranges (IQR) preceded by medians, while round brackets of continuous traits indicate standard deviations, preceded by means.
3.2. Tracheal Intubation
Seventeen cases (26.2%) of tracheal tube misplacement were recognized within the first hour of acute trauma resuscitation, of which eight were endobronchial intubations (five detected on CT scans and three by auscultation). Nine cases were tube dislocations or critical tube-to-carina distances with tube positions less than 2 cm above the carina, including one case of esophageal intubation that was immediately recognized and corrected in the prehospital setting and presented with a tube position of 0.5 cm above the carina on CT. Cases of unrecognized esophageal intubation were not observed.
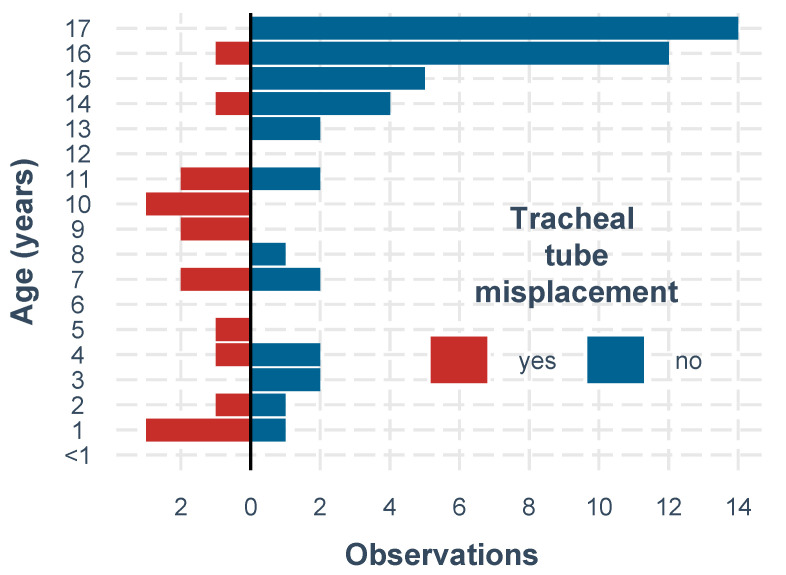
ISS, sex, and vital parameters were similarly distributed in both study groups, whereas age, height, weight, BMI, and helicopter EMS ETI provided significant differences of tracheal tube misplacements (Figure 2). Regarding the method of intubation, patients requiring CPR at the scene underwent crash ETI without the use of drugs, whereas all other patients received rapid sequence induction ETI. Patients with and without CPR presented with comparable ETI misplacement rates.
Figure 2.
Tracheal tube misplacement and age.
3.3. Risk Factors Associated with Tracheal Tube Misplacement
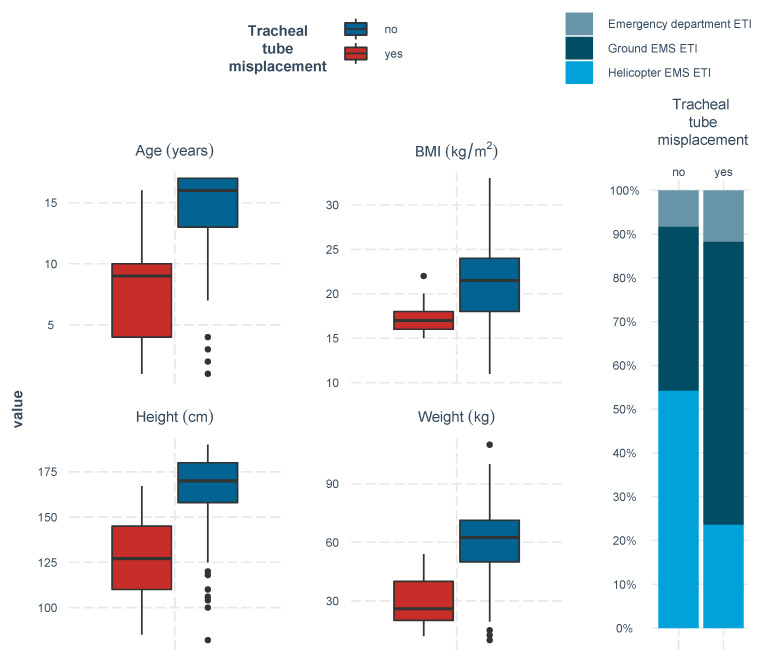
Univariable risk factors (negatively) associated with tracheal tube misplacement were age, body height, body weight, body mass index, and helicopter EMS ETI (Table 2, Figure 3). After adjustment using multivariable stepwise logistic regression analysis removing age and body mass index (as being part of the variables of height and weight), tracheal tube misplacement remained independently negatively associated with body weight (OR 0.86; 95% CI, 0.76–0.99; p = 0.032) and helicopter EMS ETI (OR 0.20; 95% CI, 0.04–0.97; p = 0.036) (Table 3).
Table 2.
Significant univariable risk factors associated with tracheal tube misplacement.
| Predictor | Univariable OR (95% CI) | p |
|---|---|---|
| Age | 0.81 (0.71–0.90) | <0.001 |
| Height | 0.96 (0.94–0.98) | <0.001 |
| Weight | 0.94 (0.90–0.97) | <0.001 |
| BMI | 0.75 (0.61–0.89) | 0.003 |
| Helicopter EMS ETI | 0.26 (0.06–0.85) | 0.035 |
BMI, body mass index; EMS, emergency medical service; ETI, endotracheal intubation.
Figure 3.
Univariable associations with tracheal tube misplacement.
Table 3.
Significant adjusted predictors identified in a stepwise logistic multivariable regression model of associated factors with tracheal tube misplacement.
| Predictor | Multivariable OR (95% CI) | p |
|---|---|---|
| Weight | 0.86 (0.76–0.99) | 0.032 |
| Helicopter EMS ETI | 0.20 (0.04–0.97) | 0.036 |
EMS, emergency medical service; ETI, endotracheal intubation.
3.4. Characteristics of Helicopter EMS and Ground EMS
A detailed analysis of prehospital EMS characteristics confirmed significantly higher misplacement rates (p = 0.039) and further revealed significantly lower Glasgow coma scale scores (p = 0.043), higher injury severity scores (p = 0.034), and most significantly, lower systolic blood pressure values (p = 0.003) in patients intubated by ground EMS rather than by helicopter EMS. Although the rate of cardiopulmonary resuscitation prior to ED admission and 24 h mortality did not reach significant levels in the ground EMS ETI group, a significantly higher 30-day mortality rate was observed (p = 0.047) (Table 4).
Table 4.
Comparison of helicopter EMS vs. ground EMS characteristics of the study cohort.
| Helicopter EMS ETI | Ground EMS ETI | p | |
|---|---|---|---|
| n (%) | 30 (56.2) | 29 (44.6) | |
| Age (years) | 14.5 (6) | 16 (8) | 0.681 |
| Male, n (%) | 19 (63.3) | 19 (65.5) | 1 |
| Height (cm) | 155.7 (27.2) | 152.8 (31.3) | 0.968 |
| Weight (kg) | 52.6 (21.8) | 54.6 (27.7) | 0.652 |
| BMI | 20 (5) | 21 (8) | 0.575 |
| GCS | 8 (11) | 5 (7) | 0.043 |
| ISS | 25 (18) | 34 (20) | 0.034 |
| SBP (mmHg) | 111 (52) | 80 (110) | 0.003 |
| HR (min−1) | 108.5 (35) | 98 (59) | 0.067 |
| SpO2 (%) | 94.5 (10) | 94 (77) | 0.435 |
| ETI misplacement, n (%) | 4 (13.3) | 11 (37.9) | 0.039 |
| CPR prior ED, n (%) | 6 (20) | 11 (37.9) | 0.158 |
| 24 h mortality, n (%) | 2 (6.7) | 5 (17.2) | 0.254 |
| 30-day mortality, n (%) | 5 (16.7) | 12 (41.4) | 0.047 |
EMS, emergency medical service; ETI, endotracheal intubation; BMI, body mass index; GCS, Glasgow coma scale; ISS, injury severity score; SBP, systolic blood pressure; HR, heart rate; SpO2, peripheral oxygen saturation; CPR, cardiopulmonary resuscitation; ED, emergency department; WBCT, whole-body computed tomography. Squared brackets indicate interquartile ranges (IQR) preceded by medians, while round brackets of continuous traits indicate standard deviations, preceded by means.
3.5. Clinical Consequences of Tracheal Tube Misplacement
Nineteen patients received tube thoracostomy, of which two had confirmed endobronchial intubation and no radiological confirmation of thoracic injury. In these two patients, tube thoracostomy was performed due to absent breathing sounds, which were erroneously considered as pneumothorax. Mortality rates after 24 h and 30 days, length of stay in the PICU, ventilator days, emergency surgery, and CPR frequencies were comparable in patients with and without ETI misplacement.
4. Discussion
The observed frequency of tracheal tube misplacement of 26.0% and particularly 12.3% endobronchial intubation in our study is in line with the results of previous pediatric studies. In the last two decades, various frequencies of endobronchial tube misplacements, ranging from 0% [8], over 2.4% [3], 3.6% [14], 6.2% [19], 6.4% [18], 8% [17] 12.8% [16], 13.2% [21], to 21.0%, have been reported [12]. Furthermore, some studies assessing pediatric tube positions found that the tube tips were generally placed too deep in even larger proportions (24.5% [16], 38.3% [20], 38.9% [15], 50.0% [12], and 69% [24], respectively).
Univariable analysis of our data revealed the patient-dependent variables of young age, short body height, low body weight, and low body mass index as being associated with tracheal tube misplacement. After the adjustment for multivariable testing, a significant association between low body weight and tracheal tube misplacement remained evident. Low body weight as a risk factor for tracheal tube misplacement in pediatric trauma patients is a new finding that has to be confirmed in further studies. These studies should provide relevant sample sizes across all age categories to rule out whether our findings are center-specific or may be generalizable.
There are some anatomical factors that may contribute to tracheal tube misplacement. First, the quality of the tube’s fixation may contribute to its dislocation. Second, the documentation of the insertion depth itself, measured by the reading of the tube at the fixation at the incisors or the mouth’s angle, is crucial to assess the risk of tube malposition. In children in whom tracheal tube displacement was only recognized after arrival in the emergency department, it cannot be determined whether the tube was originally placed incorrectly or if it dislocated during transport [25].
Numerous studies investigated the impact of head movement after intubation on the TCD and on the tube tip-to-vocal cords distance, respectively. Neck flexion results in moving the tracheal tube towards the carina, while neck extension leads to a displacement in the opposite direction. The rotation of the head to the side can withdraw the tube tip from the trachea towards the tube fixation or away from the tube fixation, respectively [26,27,28,29]. Considering these findings, it seems reasonable that once correctly placed ETTs can easily displace, particularly in smaller children.
An improved tube insertion depth may be achieved by assessing various anatomical distances (e.g., the upper incisor to manubriosternal joint length) prior to intubation [30,31,32]. Formula approaches on bedside prediction of adequate tube insertion depth use body weight, body height, tube diameter (e.g., 3× tube size), and the age in years for calculations [33,34,35]. However, in an emergency situation, the actual height and weight of the patients are often not available and have to be roughly estimated. Thus, only capnography and the visual placement of the tube marking between the vocal cords may be reliably associated with a correct tracheal positioning of the tube tip [36]. The individual anatomy (e.g., a short neck) always needs to be considered for the prevention of deep tube misplacements.
Regarding the frequency of tube misplacement comparing helicopter EMS and ground EMS, we observed a beneficial effect of helicopter EMS that remained after adjustment with other significant patient-related variables. Although both EMS systems were physician-staffed, helicopter EMS usually provide more experienced doctors than ground EMS. For instance, at the two helicopter EMS bases mainly responsible for the catchment area of the study, physicians needed to have a board certification (anesthetists in most cases) and a professional experience of more than five years in ground EMS. However, patients intubated by ground EMS were significantly more severely injured than helicopter EMS patients. This may impair the comparability and interpretation of the results and should be noted. In ground EMS intubation, the CPR rate until ED admission was almost twice as high as in helicopter EMS intubation. Since intubation under CPR is usually performed as crash intubation, emergency circumstances may have also contributed to a higher tube misplacement rate in this group. We considered chest compression-associated movements under CPR as a possible contributing factor for tube misplacement, but it did not reach statistical significance.
In the literature, recent studies involving greater sample sizes of pediatric patients found high rates for overall and first-pass intubation success, and even survival benefits in helicopter EMS [5,6,7,13,14,37,38,39,40,41]. One study found no difference in mortality comparing helicopter EMS and ground EMS, although helicopter EMS patients had a higher injury severity [42]. Furthermore, there is a controversy in the literature regarding air transport vs. ground transport in children with minor vs. major injuries [41]. In summary, our results support previous studies in that, whenever available, helicopter EMS should be dispatched simultaneously with ground EMS to achieve the best possible intubation performances in pediatric trauma patients requiring advanced airway management [4,5,6].
Our results suggest that pediatric trauma patients experiencing tracheal tube misplacement are not associated with adverse outcomes compared with patients with correctly placed tubes. Mortality rates at 24 h and at 30 days were similar in all groups. This is in line with results from 26 of 616 intubated adult trauma patients of our center [11]. However, we observed two cases of possibly unnecessary tube thoracostomy due to unrecognized endobronchial intubation [12]. Thus, we recommend routine use of point-of-care ultrasound (POCUS) to exclude pneumothorax in prehospital and emergency department trauma management [43].
After emergency intubation of a severely injured child, we recommend the thorough fixation of the tube after auscultation and capnography, inspection of the chest for breathing symmetry, and POCUS assessment, if available. The insertion depth of the tube (in cm) should be written at the fixation material and documented in the charts. In case of massive facial or oral bleeding, pharyngeal tamponade may be applied. The head should be fixed (e.g., head blocks, cervical spine immobilization) and the tracheal tube and ventilation hose should be positioned without any tension to prevent dislocation due to pull-forces during EMS transport and handover maneuvers. During transport, frequent inspection of the tube insertion site and, if possible, repeated auscultation of the chest should be performed. If the respiratory and/or circulatory condition deteriorates, kinking of the ventilator hose or tracheal tube should be checked and correct tube connection should be confirmed [44]. Possible pneumothorax should be anticipated early and ultimately be decompressed.
Limitations
We are aware of several limitations of the study, including the retrospective design. The relatively small sample size and the single center design lower the significance of our results. Not all of our patients underwent CT scans following tracheal intubation and patients who died at the scene or were declared dead on arrival were not included and might have presented with other characteristics. A detailed analysis of the airway management (e.g., intubation situs, number of attempts or complications, training level of intubating physician) was not possible due to inconsistent documentation or missing data. Another limitation is that we did not document tube insertion depth on admission to the emergency department. Furthermore, our data analysis followed an explanatory approach. Hence, our findings require replication in independent datasets.
5. Conclusions
The results of this study cohort suggest that particularly small children require attention to avoid tracheal tube misplacement, which emphasizes the need for special training. Helicopter EMS physicians´ expertise might be beneficial in prehospital pediatric trauma patients requiring advanced airway management, which has to be confirmed in further prospective studies with higher sample sizes.
Acknowledgments
We acknowledge support from the German Research Foundation (DFG) and University of Leipzig within the program of Open Access Publishing.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/children9020289/s1, Table S1: Raw data file.
Author Contributions
Conceptualization, M.F.S.; methodology, F.R., B.D. and M.F.S.; software, H.K.; validation, F.R. and M.F.S.; formal analysis, F.R., H.K. and M.F.S.; data curation, M.F.S.; writing—original draft preparation, M.F.S. and F.R.; writing—review and editing, B.D., P.Z., T.S., M.S., D.G., S.E., C.K. and M.L.; visualization, H.K.; supervision, M.F.S.; project administration, M.F.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the Medical Faculty of the University of Leipzig (protocol code, No. 441/15-ek; date of approval, 14 September 2020).
Informed Consent Statement
Not applicable.
Data Availability Statement
Data supporting the reported results can be found in Table S1: Raw data file.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Carlson J.N., Gannon E., Mann N.C., Jacobson K.E., Dai M., Colleran C., Wang H.E. Pediatric Out-of-Hospital Critical Procedures in the United States. Pediatr. Crit. Care Med. 2015;16:e260–e267. doi: 10.1097/PCC.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 2.Hansen M., Lambert W., Guise J.M., Warden C.R., Mann N.C., Wang H. Out-of-hospital pediatric airway management in the United States. Resuscitation. 2015;90:104–110. doi: 10.1016/j.resuscitation.2015.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eich C., Roessler M., Nemeth M., Russo S.G., Heuer J.F., Timmermann A. Characteristics and outcome of prehospital paediatric tracheal intubation attended by anaesthesia-trained emergency physicians. Resuscitation. 2009;80:1371–1377. doi: 10.1016/j.resuscitation.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Rodríguez J.J., Higuita-Gutiérrez L.F., Carrillo Garcia E.A., Castaño Betancur E., Luna Londoño M., Restrepo Vargas S. Meta-Analysis of Failure of Prehospital Endotracheal Intubation in Pediatric Patients. Emerg. Med. Int. 2020;2020:7012508. doi: 10.1155/2020/7012508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Garner A.A., Bennett N., Weatherall A., Lee A. Success and complications by team composition for prehospital paediatric intubation: A systematic review and meta-analysis. Crit. Care. 2020;24:149. doi: 10.1186/s13054-020-02865-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garner A.A., Bennett N., Weatherall A., Lee A. Physician-staffed helicopter emergency medical services augment ground ambulance paediatric airway management in urban areas: A retrospective cohort study. Emerg. Med. J. 2019;36:678–683. doi: 10.1136/emermed-2019-208421. [DOI] [PubMed] [Google Scholar]
- 7.Bläsius F.M., Horst K., Brokmann J.C., Lefering R., Andruszkow H., Hildebrand F., TraumaRegister Dgu Helicopter Emergency Medical Service and Hospital Treatment Levels Affect Survival in Pediatric Trauma Patients. J. Clin. Med. 2021;10:837. doi: 10.3390/jcm10040837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nevin D.G., Green S.J., Weaver A.E., Lockey D.J. An observational study of paediatric pre-hospital intubation and anaesthesia in 1933 children attended by a physician-led, pre-hospital trauma service. Resuscitation. 2014;85:189–195. doi: 10.1016/j.resuscitation.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Gerritse B.M., Draaisma J.M., Schalkwijk A., van Grunsven P.M., Scheffer G.J. Should EMS-paramedics perform paediatric tracheal intubation in the field? Resuscitation. 2008;79:225–229. doi: 10.1016/j.resuscitation.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Lohser J., Slinger P. Lung Injury after One-Lung Ventilation: A Review of the Pathophysiologic Mechanisms Affecting the Ventilated and the Collapsed Lung. Anesth. Analg. 2015;121:302–318. doi: 10.1213/ANE.0000000000000808. [DOI] [PubMed] [Google Scholar]
- 11.Heyne G., Ewens S., Kirsten H., Fakler J.K.M., Özkurtul O., Hempel G., Krämer S., Struck M.F. Risk factors and outcomes of unrecognised endobronchial intubation in major trauma patients. Emerg. Med. J. 2021 doi: 10.1136/emermed-2021-211786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Simons T., Söderlund T., Handolin L. Radiological evaluation of tube depth and complications of prehospital endotracheal intubation in pediatric trauma: A descriptive study. Eur. J. Trauma Emerg. Surg. 2017;43:797–804. doi: 10.1007/s00068-016-0758-2. [DOI] [PubMed] [Google Scholar]
- 13.Tarpgaard M., Hansen T.M., Rognås L. Anaesthetist-provided pre-hospital advanced airway management in children: A descriptive study. Scand. J. Trauma Resusc. Emerg. Med. 2015;23:61. doi: 10.1186/s13049-015-0140-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Burns B.J., Watterson J.B., Ware S., Regan L., Reid C. Analysis of Out-of-Hospital Pediatric Intubation by an Australian Helicopter Emergency Medical Service. Ann. Emerg. Med. 2017;70:773–782.e4. doi: 10.1016/j.annemergmed.2017.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt A.R., Ulrich L., Seifert B., Albrecht R., Spahn D.R., Stein P. Ease and difficulty of pre-hospital airway management in 425 paediatric patients treated by a helicopter emergency medical service: A retrospective analysis. Scand. J. Trauma Resusc. Emerg. Med. 2016;24:22. doi: 10.1186/s13049-016-0212-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.To Y.H., Ong Y.G., Chong S.L., Ang P.H., Bte Zakaria N.D., Lee K.P., Pek J.H. Differences in intubation outcomes for pediatric patients between pediatric and general Emergency Departments. Paediatr. Anaesth. 2021;31:713–719. doi: 10.1111/pan.14185. [DOI] [PubMed] [Google Scholar]
- 17.Easley R.B., Segeleon J.E., Haun S.E., Tobias J.D. Prospective study of airway management of children requiring endotracheal intubation before admission to a pediatric intensive care unit. Crit. Care Med. 2000;28:2058–2063. doi: 10.1097/00003246-200006000-00065. [DOI] [PubMed] [Google Scholar]
- 18.Sagarin M.J., Chiang V., Sakles J.C., Barton E.D., Wolfe R.E., Vissers R.J., Walls R.M., National Emergency Airway Registry (NEAR) investigators Rapid sequence intubation for pediatric emergency airway management. Pediatr. Emerg. Care. 2002;18:417–423. doi: 10.1097/00006565-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Matettore A., Ramnarayan P., Jones A., Randle E., Lutman D., O’Connor M., Chigaru L. Adverse Tracheal Intubation-Associated Events in Pediatric Patients at Nonspecialist Centers: A Multicenter Prospective Observational Study. Pediatr. Crit. Care Med. 2019;20:518–526. doi: 10.1097/PCC.0000000000001923. [DOI] [PubMed] [Google Scholar]
- 20.Miller K.A., Kimia A., Monuteaux M.C., Nagler J. Factors Associated with Misplaced Endotracheal Tubes during Intubation in Pediatric Patients. J. Emerg. Med. 2016;51:9–18. doi: 10.1016/j.jemermed.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Bai W., Golmirzaie K., Burke C., Van Veen T., Christensen R., Voepel-Lewis T., Malviya S. Evaluation of emergency pediatric tracheal intubation by pediatric anesthesiologists on inpatient units and the emergency department. Paediatr. Anaesth. 2016;26:384–391. doi: 10.1111/pan.12839. [DOI] [PubMed] [Google Scholar]
- 22.Deutsche Deutsche Gesellschaft für Kinderchirurgie e.V. (DGKCH). Polytraumaversorgung im Kindesalter. AWMF-Register-Nr. 006-120, Klasse S2k. 2020. [(accessed on 19 January 2022)]. Available online: https://www.awmf.org/uploads/tx_szleitlinien/006-120k_S2k_Polytraumaversorgung-im-Kindesalter_2020-12.pdf.
- 23.Deutsche Gesellschaft für Unfallchirurgie e.V. (DGU). Polytrauma/Schwerverletzten-Behandlung. AWMF-Register Nr. 012/019, Klasse: S3. 2016. [(accessed on 19 January 2022)]. Available online: http://www.awmf.org/uploads/tx_szleitlinien/012-019l_S3_Polytrauma_Schwerverletzten-Behandlung_2016-09.pdf.
- 24.Volsko T.A., McNinch N.L., Prough D.S., Bigham M.T. Adherence to Endotracheal Tube Depth Guidelines and Incidence of Malposition in Infants and Children. Respir. Care. 2018;63:1111–1117. doi: 10.4187/respcare.06024. [DOI] [PubMed] [Google Scholar]
- 25.Sunde G.A., Kottmann A., Heltne J.K., Sandberg M., Gellerfors M., Krüger A., Lockey D., Sollid S.J.M. Standardised data reporting from pre-hospital advanced airway management—A nominal group technique update of the Utstein-style airway template. Scand. J. Trauma Resusc. Emerg. Med. 2018;26:46. doi: 10.1186/s13049-018-0509-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yan S., Zhang H. Impact of changes in head position during head and neck surgery on the depth of tracheal tube intubation in anesthetized children. BMC Anesthesiol. 2020;20:124. doi: 10.1186/s12871-020-01033-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim J.T., Kim H.J., Ahn W., Kim H.S., Bahk J.H., Lee S.C., Kim C.S., Kim S.D. Head rotation, flexion, and extension alter endotracheal tube position in adults and children. Can. J. Anaesth. 2009;56:751–756. doi: 10.1007/s12630-009-9158-y. [DOI] [PubMed] [Google Scholar]
- 28.Weiss M., Knirsch W., Kretschmar O., Dullenkopf A., Tomaske M., Balmer C., Stutz K., Gerber A.C., Berger F. Tracheal tube-tip displacement in children during head-neck movement—A radiological assessment. Br. J. Anaesth. 2006;96:486–491. doi: 10.1093/bja/ael014. [DOI] [PubMed] [Google Scholar]
- 29.Herway S.T., Benumof J.L. The tracheal accordion and the position of the endotracheal tube. Anaesth. Intensive Care. 2017;45:177–188. doi: 10.1177/0310057X1704500207. [DOI] [PubMed] [Google Scholar]
- 30.Jain A., Wadhwa B., Saxena K.N. Preventing inadvertent Endobronchial intubation: Upper incisor to manubriosternal joint length as a predictor of airway length in children. Paediatr. Anaesth. 2020;30:1240–1244. doi: 10.1111/pan.14023. [DOI] [PubMed] [Google Scholar]
- 31.Lee B.J., Yi J.W., Chung J.Y., Kim D.O., Kang J.M. Bedside prediction of airway length in adults and children. Anesthesiology. 2009;111:556–560. doi: 10.1097/ALN.0b013e3181af6496. [DOI] [PubMed] [Google Scholar]
- 32.Koshy T., Misra S., Chatterjee N., Dharan B.S. Accuracy of a Chest X-Ray-Based Method for Predicting the Depth of Insertion of Endotracheal Tubes in Pediatric Patients Undergoing Cardiac Surgery. J. Cardiothorac. Vasc. Anesth. 2016;30:947–953. doi: 10.1053/j.jvca.2016.01.031. [DOI] [PubMed] [Google Scholar]
- 33.Lee S.U., Jung J.Y., Kim D.K., Kwak Y.H., Kwon H., Cho J.H., Park J.W., Choi Y.J. New decision formulas for predicting endotracheal tube depth in children: Analysis of neck CT images. Emerg. Med. J. 2018;35:303–308. doi: 10.1136/emermed-2017-206795. [DOI] [PubMed] [Google Scholar]
- 34.Phipps L.M., Thomas N.J., Gilmore R.K., Raymond J.A., Bittner T.R., Orr R.A., Robertson C.L. Prospective assessment of guidelines for determining appropriate depth of endotracheal tube placement in children. Pediatr. Crit. Care Med. 2005;6:519–522. doi: 10.1097/01.PCC.0000165802.32383.9E. [DOI] [PubMed] [Google Scholar]
- 35.Lau N., Playfor S.D., Rashid A., Dhanarass M. New formulae for predicting tracheal tube length. Paediatr. Anaesth. 2006;16:1238–1243. doi: 10.1111/j.1460-9592.2006.01982.x. [DOI] [PubMed] [Google Scholar]
- 36.Weiss M., Gerber A.C., Dullenkopf A. Appropriate placement of intubation depth marks in a new cuffed paediatric tracheal tube. Br. J. Anaesth. 2005;94:80–87. doi: 10.1093/bja/aeh294. [DOI] [PubMed] [Google Scholar]
- 37.Elonheimo L., Ljungqvist H., Harve-Rytsälä H., Jäntti H., Nurmi J. Frequency, indications and success of out-of-hospital intubations in Finnish children. Acta Anaesthesiol. Scand. 2021;66:125–131. doi: 10.1111/aas.13980. [DOI] [PubMed] [Google Scholar]
- 38.Oude Alink M.B., Moors X.R.J., Karrar S., Houmes R.J., Hartog D.D., Stolker R.J. Characteristics, management and outcome of prehospital pediatric emergencies by a Dutch HEMS. Eur. J. Trauma Emerg. Surg. 2021 doi: 10.1007/s00068-020-01579-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Brown J.B., Leeper C.M., Sperry J.L., Peitzman A.B., Billiar T.R., Gaines B.A., Gestring M.L. Helicopters and injured kids: Improved survival with scene air medical transport in the pediatric trauma population. J. Trauma Acute Care Surg. 2016;80:702–710. doi: 10.1097/TA.0000000000000971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Renberg M., Hertzberg D., Kornhall D., Günther M., Gellerfors M. Pediatric Prehospital Advanced Airway Management by Anesthesiologist and Nurse Anesthetist Staffed Critical Care Teams. Prehosp. Disaster Med. 2021;36:547–552. doi: 10.1017/S1049023X21000637. [DOI] [PubMed] [Google Scholar]
- 41.Duffens A., Grigorian A., de Virgilio C., Chin T., Kim D., Lekawa M., Schubl S.D., Nahmias J. Association of Risk of Mortality in Pediatric Patients Transferred from Scene by Helicopter with Major but Not Minor Injuries. Pediatr. Emerg. Care. 2020;38:e287–e291. doi: 10.1097/PEC.0000000000002263. [DOI] [PubMed] [Google Scholar]
- 42.Enomoto Y., Tsuchiya A., Tsutsumi Y., Ishigami K., Osone J., Togo M., Yasuda S., Inoue Y. Association between physician-staffed helicopter versus ground emergency medical services and mortality for pediatric trauma patients: A retrospective nationwide cohort study. PLoS ONE. 2020;15:e0237192. doi: 10.1371/journal.pone.0237192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramsingh D., Ghazal E., Gordon B., Ross P., Goltiao D., Alschuler M., Pugh J., Holsclaw M., Mason L. Relationship Between Evaluations of Tracheal Tube Position Using Ultrasound and Fluoroscopy in an Infant and Pediatric Population. J. Clin. Med. 2020;9:1707. doi: 10.3390/jcm9061707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Van de Voorde P., Turner N.M., Djakow J., de Lucas N., Martinez-Mejias A., Biarent D., Bingham R., Brissaud O., Hoffmann F., Johannesdottir G.B., et al. European Resuscitation Council Guidelines 2021: Paediatric Life Support. Resuscitation. 2021;161:327–387. doi: 10.1016/j.resuscitation.2021.02.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data supporting the reported results can be found in Table S1: Raw data file.