Abstract
Chronic constipation is a common gastrointestinal disorder in older adults, and it is very important to manage chronic constipation. However, evaluating these subjective symptoms is extremely difficult in cases where patients are unable to express their symptoms because of a cognitive or physical impairment. Hence, it is necessary to observe the patient’s colonic faecal retention using objective methods. Ultrasonography observation for colonic faecal retention is useful for diagnosing constipation and evaluating the effectiveness of treatment. Since there was no standard protocol for interpreting rectal ultrasonography findings, we developed an observation protocol through an expert consensus. We convened a group of experts in the diagnosis and evaluation of chronic constipation and ultrasonography to discuss and review the current literature on this matter. Together, they composed a succinct, evidence-based observation protocol for rectal faecal retention using ultrasonography. We created an observation protocol to enhance the quality and accuracy of diagnosis of chronic constipation, especially rectal constipation. This consensus statement is intended to serve as a guide for physicians, laboratory technicians and nurses who do not specialise in ultrasound or the diagnosis of chronic constipation.
Keywords: constipation, faecal retention, rectum, ultrasonography
1. Introduction
Chronic constipation is a common gastrointestinal disorder in older adults. Chronic constipation occurs in 16% of adults, with higher rates in older patients [1]. About one-third of adults aged 60 years or older report at least occasional constipation [1], and the prevalence is 50% or more in nursing home residents [2]. Moreover, chronic constipation is more commonly observed in women and those with lower socioeconomic status [3,4]. Recently, it has been shown that the prognosis of constipated patients is significantly worse than that of patients without constipation [5]. Constipated patients have an increased risk of cardiovascular events, possibly due in part to cardiovascular stress caused by anger during defaecation. Epidemiological studies in Japan have reported a significant increase in cardiovascular events, as the frequency of defaecation decreases [6]. Therefore, the management of chronic constipation is very important.
The Rome IV criteria categorise disorders of chronic constipation into four subtypes: (a) functional constipation; (b) irritable bowel syndrome with constipation; (c) opioid-induced constipation; and (d) functional defaecation disorders, including inadequate defaecatory propulsion and dyssynergic defaecation [7]. Functional constipation is the most common type of chronic constipation and is generally diagnosed based on symptoms according to the Rome IV diagnostic criteria [1]. To define functional constipation, ≥2 of the following symptoms should be present: straining at stool, lumpy or hard stool, sensation of incomplete evacuation, sensation of anorectal obstruction or blockage, need for manual manoeuvres and <3 bowel movements per week. However, three of the six Rome IV items require subjective evaluation, which is extremely difficult if patients are unable to communicate their symptoms because of a cognitive or physical impairment. Hence, it is necessary to observe patients’ colonic faecal retention using objective methods.
Diagnostic tests are typically recommended for constipation to evaluate the rectum and colon include plain abdominal X-ray (radiography), barium enema, colonoscopy, defaecography, abdominal computed tomography and magnetic resonance imaging [8,9,10]. However, these procedures involve disadvantages such as being invasive with radiation exposure, requiring long examination times or potentially providing inadequate information; moreover, they are unsuitable for follow-up testing, are expensive and lack standardisation. X-rays are a test that can be performed in many hospitals, but the cost is moderate, and the information is often unclear. Conversely, conventional ultrasonography (US) can be broadly applied in clinical practice due to its advantages of low cost, high safety, high speeds and use of non-invasive, nonionising radiation [11,12]. Recently, there has been a dramatic increase in the use of point-of-care ultrasound (POCUS) using a handheld ultrasound device by physicians or nurses who do not specialise in USs. Such handheld devices enable physicians or nurses to observe the subject at the bedside and make on-the-spot decisions for care. Ideally, POCUS can be used by anyone in a multidisciplinary team to observe faecal retention for the evaluation of constipation.
The US observation of colonic faecal retention is useful for diagnosing constipation and evaluating the effectiveness of treatment. Manabe et al. [13,14] reported that the responsiveness of patients with chronic constipation to medical treatment may be reflected in two parameters (the constipation index and the left/right distribution ratio) used to evaluate patients’ stool and/or gas distribution, which are calculated by the US observation of the colon. Thus, to properly assess constipation, the entire colon should be evaluated with US; however, not everyone in a multidisciplinary team has the high level of skill required for this type of assessment. The literature has asserted the importance of observing the presence or absence of rectal faecal retention when assessing constipation in older adults [15]; additionally, educational programmes have been developed for nurses [16], and the effectiveness of rectal US-based defaecation care in a home-care setting has been verified [17]. To build on this prior work, we decided to focus on the use of rectal US to confirm faecal retention.
A hyperechoic area shaped like a half-moon on a US reflects faecal retention in the rectum. Furthermore, an acoustic shadow on the crescent-shaped hyperechoic area in the US reflects hard stool retention. Tanaka et al. reported that 100% of older adult patients with a half-moon shape in the rectal hyperechoic area had a decreased frequency of defaecation and 92.9% of older adult patients with an acoustic shadow on the crescent-shaped hyperechoic area had hard stools. Several previous studies in children also support the use of rectal US in diagnosing constipation [18,19,20]. However, until now, there has not been a standard protocol for observing constipation via rectal US; therefore, we sought to develop an observation protocol through expert consensus.
2. Methods
Our aim was to create an observation protocol to enhance the quality and accuracy of diagnoses of chronic constipation, especially rectal constipation. This consensus statement is intended to serve as a guide for physicians, laboratory technicians and nurses who do not specialise in US or the diagnosis of chronic constipation. For a narrative review of the current literature in this area, we convened a group of gastroenterologists, sonographers, nurses and a wound, ostomy and continence nurse (WOCN) with expertise in the diagnosis and evaluation of chronic constipation and US. The criteria for the selection of the members were as follows: (1) research achievements on the evaluation of constipation via US in Japan; or (2) being the president of an academic society with high expertise in the diagnosis, assessment, treatment and defaecation care of constipation. From July to October 2020, online working group meetings were conducted once a month (a total of four meetings) to create the content of the consensus. Subsequently, another meeting was conducted for the entire membership to reach a consensus. Following discussion and agreement, they composed a succinct, evidence-based observation protocol for rectal faecal retention using US. The content of this consensus document was presented at the 22th meeting of the Japanese Society of Neurogastroenterology in Tokyo, Japan, on 20 November 2020, and a final version was developed after further discussion and agreement.
3. Protocol for the Observation of Rectal Faecal Impaction Using US
3.1. Subjects
The target population for this US observational protocol is individuals with suspected constipation. Subjects who can be interviewed are evaluated for suspected constipation according to the Rome IV diagnostic criteria [7]. For subjects who cannot be interviewed, it is necessary to obtain other objective information. For example, the Bristol Stool Form Score should be used to assess faecal characteristics, and constipation should be suspected when 1–2 hard stools are observed [21]. Constipation should also be suspected, when the stool volume is clearly low in relation to food intake.
3.2. Timing of the Observation
It is preferable to perform US observation, when there is urine retention in the bladder (since the bladder can be used as an acoustic window), when the patient does not eat immediately prior to the exam (since there is no effect of small bowel contents or gas) and when there is no gas retention in the abdomen.
3.3. Observation Procedure
3.3.1. Position/Posture
The patient should be supine and should be comfortable. The head should be propped at about 10 degrees, with a bath towel or cushion placed under the neck to relieve tension in the abdomen, and the knee joints should be gently flexed.
3.3.2. US Devices
A convex probe should be selected for the US, preferably with a bandwidth of 2–5 MHz in frequency. The required resolution is based on the following two conditions: (a) the bladder can be depicted as an anechoic area with a few multiple reflections; and (b) the boundaries and edges of the tissue can be depicted uniformly (i.e., the boundaries between the rectal contents and the intestinal tract and the bladder wall can be clearly depicted).
In addition to the US device, the procedure requires echo jelly, hand towels and tissue paper for wiping off the jelly and the blanket.
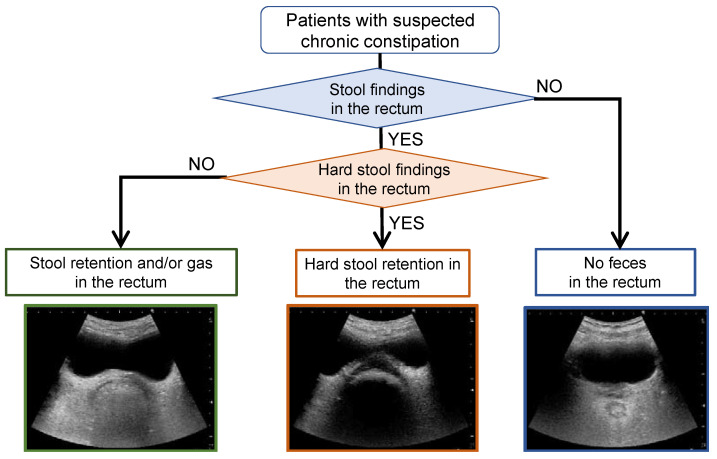
3.3.3. Flowchart of the Rectal US Observation
Figure 1 presents a flowchart of the rectal US observation to evaluate faecal retention. This flowchart is intended for use in individuals with suspected constipation, where US is used to confirm the presence, properties, location and volume of rectal faecal retention and to select treatment and care. In this flowchart, transverse US images confirm the presence and nature of rectal faecal retention, and longitudinal US images confirm the location and amount of rectal faecal retention. Here, rectal gas was classified in the same group as rectal faecal retention, because it is sometimes difficult to distinguish rectal gas from faecal retention on US images and because the diagnosis is not significantly affected even when faecal retention cannot be distinguished from rectal gas.
Figure 1.
Flowchart for the observation of rectal faecal retention with ultrasonography.
3.3.4. Probe Scanning and Typical Images
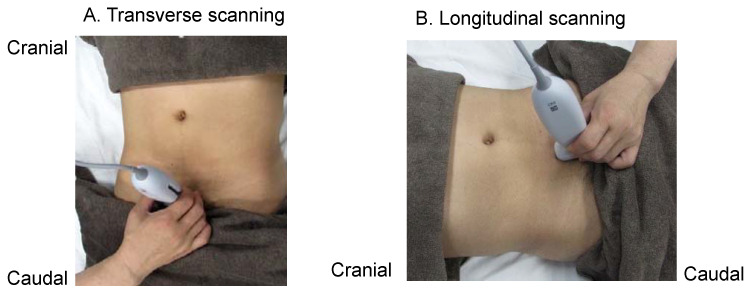
In both transverse and longitudinal scans, the US probe is placed at the superior border of the pubic bone, and the US beam is tilted caudally 10–30 degrees to visualise the bladder (Figure 2). The bladder is used as an acoustic window, and the rectum visualisation is deeper than that of the bladder.
Figure 2.
How to apply the ultrasound probe. The probe is placed at the superior margin of the pubis for both transverse scanning (A) and longitudinal scanning (B). In both techniques, the ultrasound beam is tilted caudally by 10–30 degrees to visualise the bladder. The bladder is used as an acoustic window, with the rectum being visualised deeper than the bladder.
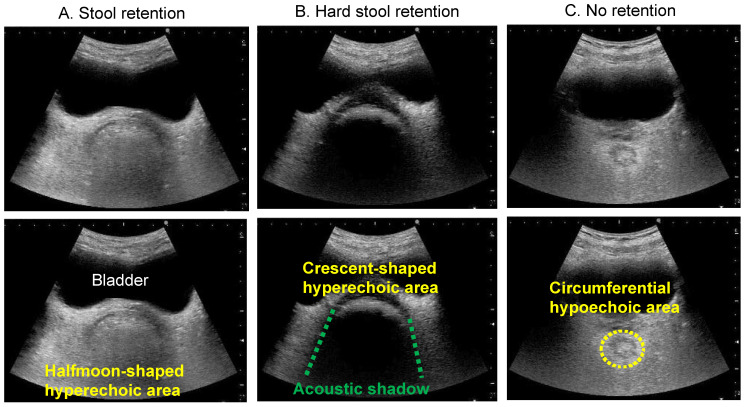
When there are contents (faecal retention) in the rectal lumen, US waves are reflected from the surface of the contents at a depth deeper than the bladder (anechoic area) and a hyperechoic area with a half-moon shape is depicted in the transverse US image (Figure 3A). In addition, when there is hard stool accumulation, an acoustic shadow is depicted in the transverse US image of the crescent-shaped hyperechoic area (Figure 3B). In contrast, if there is no faecal retention or gas in the rectal lumen, no obvious hyperechoic area is depicted. In the transverse US image, a circumferential hypoechoic area may be observed as an empty intestine (Figure 3C) [22].
Figure 3.
Transverse rectal ultrasound images showing the presence of stool and hard stool. The top three images are the original ultrasound images, and the bottom three images illustrate the ultrasound findings. (A) Stool retention. A halfmoon-shaped hyperechoic area is observed in the lower part of the bladder. (B) Hard stool retention. A crescent-shaped hyperechoic area with an acoustic shadow is observed in the lower part of the bladder. (C) No retention. No hyperechoic area is observed, because there is no faecal retention. A circumferential hypoechoic area is observed in the lower part of the bladder.
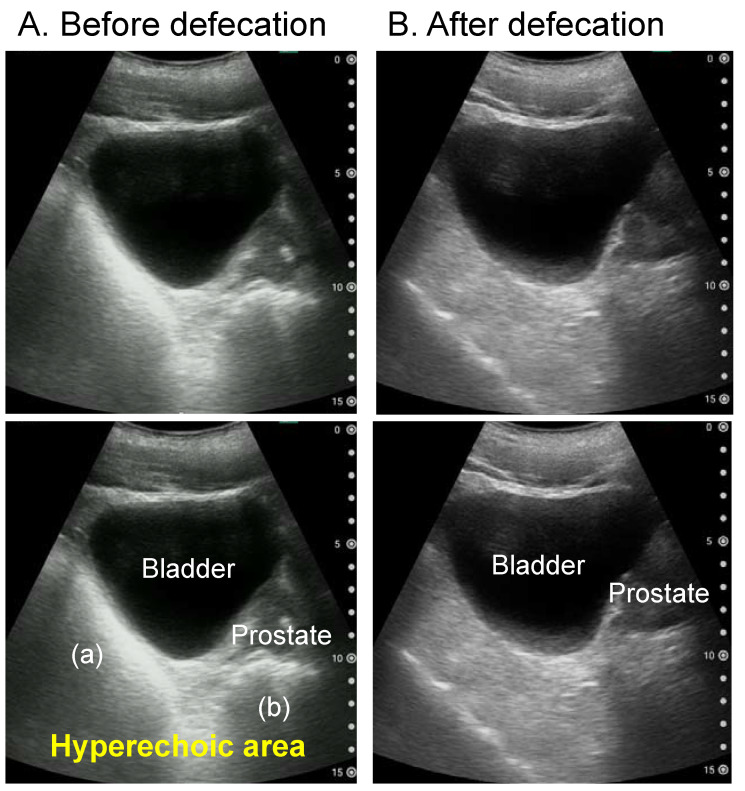
The longitudinal US image can show the location and amount of rectal faecal retention. For example, the longitudinal image can be used to determine whether the faecal retention is in the upper or lower rectum. Figure 4 shows the longitudinal rectal US images of a healthy adult before and after defaecation. There is faecal retention in both the upper and lower rectums before defaecation, whereas there is no faecal retention in either rectum after defaecation.
Figure 4.
Longitudinal rectal ultrasound images of a healthy male in his 30s before (A) and after (B) defaecation. The top two images are the original ultrasound images, whereas the respective bottom images describe the findings. Before defaecation, there was faecal retention in both the upper (a) and lower (b) rectum. There is no faecal retention in rectum.
3.4. Findings That Need to Be Differentiated: Paradoxical Diarrhoea
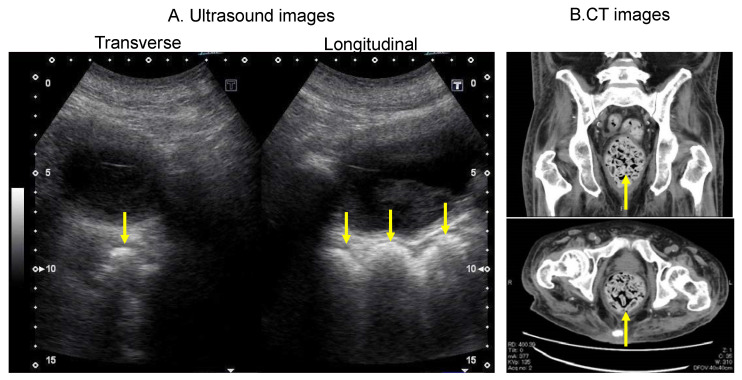
Paradoxical diarrhoea needs to be differentiated in US findings [23,24]. Faecal impaction is defined as a large amount of compressed faecal retention at the level of the bowel that cannot be expelled spontaneously, causes rectal distention and results in continuous contact between the faeces and the wall, which may cause mucous membrane irritation and a resulting increase in mucous secretion [25]. In addition, faecal impaction can cause the prolonged relaxation of the internal anal sphincter; in combination with the neuropathy component of the pudendal nerve [26], this prolonged relaxation can cause watery stools to seep out around the hard mass of faeces [27]. Paradoxical diarrhoea may not be diagnosed as constipation, because watery stools are expelled gradually. Figure 5 shows a clinical image of a patient who had frequent episodes of diarrhoea, but the computed tomography image shows intense faecal impaction in the rectum. In patients with paradoxical diarrhoea, a crescent-shaped hyperechoic area with acoustic shadows can be observed.
Figure 5.
Ultrasound images of a patient who had frequent episodes of diarrhoea with intense faecal impaction in the rectum on CT imaging. (A) Rectal ultrasound images showing a hyperechoic area indicating faecal retention (arrows). (B) CT image showing faecal retention in the rectum (arrows). The upper image shows a longitudinal section, and the lower image shows a transverse section. CT, computed tomography.
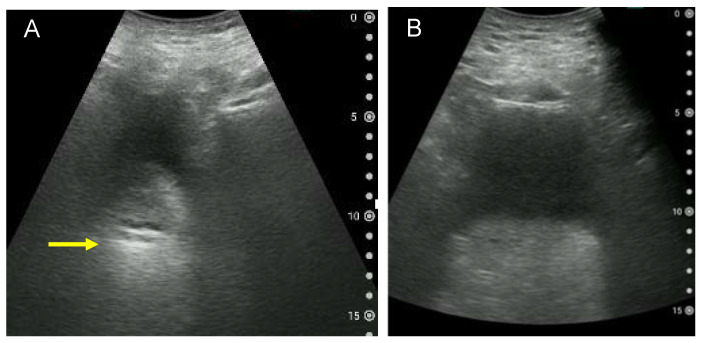
3.5. Cases That Are Difficult to Observe
Obesity, the lack of urine in the bladder and gastrointestinal gas are factors that make US observation difficult. It is believed that the increased thickness of the abdominal wall due to obesity causes attenuation and scattering of the US beam, affecting the image quality when viewing the bladder and deep tissue [28]. Figure 6 shows examples of a blurred US image of the bladder and rectum. Blurred US images also occur, when there is little urine in the bladder. Therefore, whenever possible, US should be performed with at least 100 mL of urine stored. In addition, it has been reported that abdominal gas increases after eating [29]. Since gas can affect the quality of US images, it is necessary to avoid examinations just after eating or to avoid gas entering the US screen by having patients lie on their left side.
Figure 6.
Examples of a blurred ultrasound image of the bladder and rectum. (A) Blurred transverse ultrasound image of the rectum due to little urine in the bladder and intestinal gas. A hyperechoic area is observed, possibly indicating faecal retention (arrow). (B) Transverse ultrasound image of the rectum in an adult male with a body mass index of 28.6 kg/m2. Due to the thickness of the abdominal wall, the bladder and rectum cannot be clearly observed. The volume of urine voided immediately after imaging is approximately 180 mL.
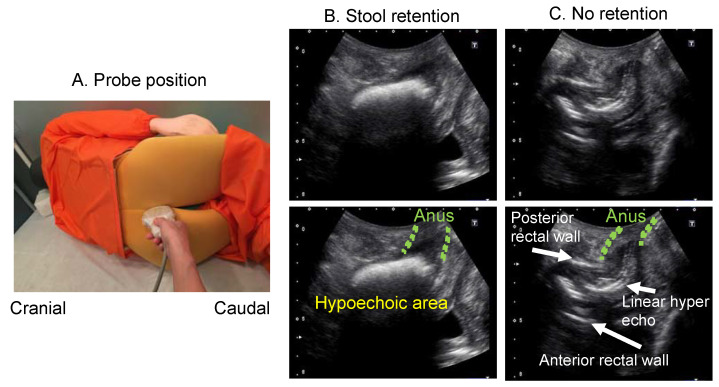
When observing rectal faecal retention by transabdominal US is difficult due to any of the above reasons, the intergluteal cleft approach is effective [30]. Patients should lie on their left side, with bent knees, and the medical provider should place the US probe between the patient’s tailbone and anus to confirm faecal retention in the lower rectum (Figure 7).
Figure 7.
Probe position and rectal ultrasound images in intergluteal cleft scanning method. (A) Probe position. By placing the subject in a side-lying position and flexing the knees, a space is created between the coccyx and the anus. The probe is applied to this area with a longitudinal scan. (B) US image when there is stool retention. The stool in the lower rectum is observed as a hyperechoic area. (C) Ultrasound image when there is no stool retention. When stool is not accumulated, a hyperechoic line is observed, and even the anterior rectal wall is observed.
4. Future Challenges
There are several issues we need to address in the future. The first is image quality adjustment for US devices. The images presented in this article are from both portable and high-end devices, and there is no consensus on how image quality should be adjusted. The second issue is gas discrimination. As in previous studies [13,14], gas in the rectum and faecal retention were not distinguished in this study. The third issue is the development of an educational programme for US observation. It is expected that physicians and nurses who have not used US in the past will observe the rectum for diagnostic or POCUS purposes. Currently, POCUS educational programmes for nurses are being developed [16], but standardised educational materials will be necessary in the future so that multiple professions can acquire rectal US observation skills in a short time. Lastly, a system should be developed to support skills in reading US images. Reading skills are very important in the acquisition and evaluation of rectal US images. However, since reading skills are affected by differences in experience, a system that can support reading is required. A classification of rectal faecal retention findings based on deep learning has already been developed [31], and the development of US devices equipped with such a system will be necessary in the future.
This consensus document has some limitations. First, its content was not compiled through a systematic review. Just as previous studies have validated the efficacy of surgery for chronic constipation [32,33], future systematic reviews should also validate the efficacy of US assessment for constipation. Second, our consensus does not quantify the percentage of consensus among the experts, unlike what was performed in a previous study [34]. Nevertheless, this expert consensus document can help physicians, nurses and other professionals unfamiliar with US to practice POCUS for constipation, especially in the assessment of rectal feacal retention. Alongside physical examination and rectal examination, the use of US to observe faecal retention in the colon can be included in the management algorithm for identifying chronic constipation [35].
5. Conclusions
An expert consensus has been reached on the use of US by multidisciplinary teams to observe rectal faecal retention, evaluate constipation and select appropriate treatment and care. This consensus statement outlined a standard procedure for using US to observe the presence, properties, location and volume of rectal faecal retention.
Acknowledgments
The authors would like to thank Fujifilm Medical Corporation for sponsoring this consensus meeting held on 20 November 2020. The authors also would like to thank Tokatsu Clinic Hospital for providing us with the ultrasound images.
Author Contributions
Conceptualization, M.M., N.M. (Noboru Misawa), M.T. and N.M. (Noriaki Manabe); Project administration, A.K., K.H., H.S. and A.N.; Supervision, A.K., J.S., H.T., M.K. and K.H.; Visualization, M.M. and N.M. (Noboru Misawa); Writing—original draft, M.M. and N.M. (Noboru Misawa); Writing—review & editing, M.T., N.M. (Noriaki Manabe), T.K. and N.T. All the authors were involved in the planning of the expert consensus meeting; M.M., N.M. (Noboru Misawa), M.T., N.M. (Noriaki Manabe), A.K., H.T., J.S., M.K., K.H., H.S. and A.N. participated as panellists at the expert consensus meeting at the 22th meeting of the Japanese Society of Neurogastroenterology in Tokyo, Japan, on 20 November 2020. T.K. and N.T. participated in online working group meetings and the expert consensus meeting. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Written informed consent has been obtained from the patients to publish this paper, with the approval from each institution.
Conflicts of Interest
M.M. belonged to a social collaboration department that receives funding from Fujifilm Corporation (Tokyo, Japan) N.T. belongs to a social collaboration department that receives funding from Fujifilm Corporation. M.K. has served in speaking and teaching commitments for Takeda Pharmaceutical Co., Ltd. (Tokyo, Japan), and Otsuka Pharmaceutical Co. (Tokyo, Japan). and has received scholarship grants from Fujifilm Co., Ltd. (Tokyo, Japan) and EA farm Co., Ltd. (Tokyo, Japan).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bharucha A.E., Pemberton J.H., Locke G.R., 3rd American Gastroenterological Association technical review on constipation. Gastroenterology. 2013;144:218–238. doi: 10.1053/j.gastro.2012.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bouras E.P., Tangalos E.G. Chronic constipation in the elderly. Gastroenterol. Clin. N. Am. 2009;38:463–480. doi: 10.1016/j.gtc.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 3.Camilleri M., Ford A.C., Mawe G.M., Dinning P.G., Rao S.S., Chey W.D. Chronic constipation. Nat. Rev. Dis. Primers. 2017;3:17095. doi: 10.1038/nrdp.2017.95. [DOI] [PubMed] [Google Scholar]
- 4.Suares N.C., Ford A.C. Prevalence of, and risk factors for, chronic idiopathic constipation in the community: Systematic review and meta-analysis. Am. J. Gastroenterol. 2011;106:1582–1591. doi: 10.1038/ajg.2011.164. [DOI] [PubMed] [Google Scholar]
- 5.Sumida K., Molnar M.Z., Potukuchi P.K., Thomas F., Lu J.L., Yamagata K. Constipation and risk of death and cardiovascular events. Atherosclerosis. 2019;281:114–120. doi: 10.1016/j.atherosclerosis.2018.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Honkura K., Tomata Y., Sugiyama K., Kaiho Y., Watanabe T., Zhang S. Defecation frequency and cardiovascular disease mortality in Japan: The Ohsaki cohort study. Atherosclerosis. 2016;246:251–256. doi: 10.1016/j.atherosclerosis.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 7.Aziz I., Whitehead W.E., Palsson O.S., Törnblom H., Simrén M. An approach to the diagnosis and management of Rome IV functional disorders of chronic constipation. Expert Rev. Gastroenterol. Hepatol. 2020;14:39–46. doi: 10.1080/17474124.2020.1708718. [DOI] [PubMed] [Google Scholar]
- 8.Seltzer R. Evaluation and diagnosis of constipation. Gastroenterol. Nurs. 2012;35:343–348. doi: 10.1097/SGA.0b013e31826b16a1. [DOI] [PubMed] [Google Scholar]
- 9.Remes-Troche J.M., Rao S.S. Diagnostic testing in patients with chronic constipation. Curr. Gastroenterol. Rep. 2006;8:416–424. doi: 10.1007/s11894-006-0028-2. [DOI] [PubMed] [Google Scholar]
- 10.Rao S.S., Ozturk R., Laine L. Clinical utility of diagnostic tests for constipation in adults: A systematic review. Am. J. Gastroenterol. 2005;100:1605–1615. doi: 10.1111/j.1572-0241.2005.41845.x. [DOI] [PubMed] [Google Scholar]
- 11.Berger M.Y., Tabbers M.M., Kurver M.J., Boluyt N., Benninga M.A. Value of abdominal radiography, colonic transit time, and rectal ultrasound scanning in the diagnosis of idiopathic constipation in children: A systematic review. J. Pediatr. 2012;161:e1–e2. doi: 10.1016/j.jpeds.2011.12.045. [DOI] [PubMed] [Google Scholar]
- 12.Perniola G., Shek C., Chong C.C., Chew S., Cartmill J., Dietz H.P. Defecation proctography and translabial ultrasound in the investigation of defecatory disorders. Ultrasound Obs. Gynecol. 2008;31:567–571. doi: 10.1002/uog.5337. [DOI] [PubMed] [Google Scholar]
- 13.Manabe N., Kamada T., Hata J., Haruma K. New ultrasonographic evaluation of stool and/or gas distribution for treatment of chronic constipation. Int. J. Colorectal Dis. 2018;33:345–348. doi: 10.1007/s00384-018-2964-3. [DOI] [PubMed] [Google Scholar]
- 14.Manabe N., Kamada T., Kusunoki H., Hata J., Haruma K. Usefulness of ultrasonographic evaluation of stool and/or gas distribution for the treatment strategy of chronic constipation. JGH Open. 2019;3:310–315. doi: 10.1002/jgh3.12162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tanaka S., Yabunaka K., Matsumoto M., Tamai N., Noguchi H., Yoshida M. Fecal Distribution Changes Using Colorectal Ultrasonography in Older People with Physical and Cognitive Impairment Living in Long-Term Care Facilities: A Longitudinal Observational Study. Healthcare. 2018;6:55. doi: 10.3390/healthcare6020055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsumoto M., Yoshida M., Miura Y., Sato N., Okawa Y., Yamada M. Feasibility of the constipation point-of-care ultrasound educational program in observing fecal retention in the colorectum: A descriptive study. Jpn. J. Nurs. Sci. 2021;18:e12385. doi: 10.1111/jjns.12385. [DOI] [PubMed] [Google Scholar]
- 17.Matsumoto M., Yoshida M., Yabunaka K., Nakagami G., Miura Y., Fujimaki S. Safety and efficacy of a defecation care algorithm based on ultrasonographic bowel observation in Japanese home-care settings: A single-case, multiple-baseline study. Geriatr. Gerontol. Int. 2020;20:187–194. doi: 10.1111/ggi.13858. [DOI] [PubMed] [Google Scholar]
- 18.Di Pace M.R., Catalano P., Caruso A.M., Bommarito D., Casuccio A., Cimador M. Is rectal disimpact always necessary in children with chronic constipation? Evaluation with pelvic ultrasound. Pediatr. Surg. Int. 2010;26:601–606. doi: 10.1007/s00383-010-2602-9. [DOI] [PubMed] [Google Scholar]
- 19.Karaman A., Ramadan S.U., Karaman I., Gokharman D., Erdogan D., Kacar M. Diagnosis and follow-up in constipated children: Should we use ultrasound? J. Pediatr. Surg. 2010;45:1849–1855. doi: 10.1016/j.jpedsurg.2010.05.006. [DOI] [PubMed] [Google Scholar]
- 20.Hatori R., Tomomasa T., Ishige T., Tatsuki M., Arakawa H. Fecal retention in childhood: Evaluation on ultrasonography. Pediatr. Int. 2017;59:462–466. doi: 10.1111/ped.13185. [DOI] [PubMed] [Google Scholar]
- 21.Chumpitazi B.P., Self M.M., Czyzewski D.I., Cejka S., Swank P.R., Shulman R.J. Bristol Stool Form Scale reliability and agreement decreases when determining Rome III stool form designations. Neurogastroenterol. Motil. 2016;28:443–448. doi: 10.1111/nmo.12738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yabunaka K., Matsumoto M., Yoshida M., Tanaka S., Miura Y., Tsutaoka T. Assessment of rectal feces storage condition by a point-of-care pocket-size ultrasound device for healthy adult subjects: A preliminary study. Drug Discov. 2018;12:42–46. doi: 10.5582/ddt.2018.01001. [DOI] [PubMed] [Google Scholar]
- 23.Cohen R.A., Pops M.A. Paradoxical diarrhea with opiates. JAMA. 1968;205:802–803. doi: 10.1001/jama.1968.03140370104032. [DOI] [PubMed] [Google Scholar]
- 24.Wilson R., Gundry C.H. Paradoxical diarrhoea in childhood. Can. Med. Assoc. J. 1955;72:362–368. [PMC free article] [PubMed] [Google Scholar]
- 25.Serrano Falcón B., Barceló López M., Mateos Muñoz B., Álvarez Sánchez A., Rey E. Fecal impaction: A systematic review of its medical complications. BMC Geriatr. 2016;16:4. doi: 10.1186/s12877-015-0162-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rao S.S. Pathophysiology of adult fecal incontinence. Gastroenterology. 2004;126((Suppl. 1)):S14–S22. doi: 10.1053/j.gastro.2003.10.013. [DOI] [PubMed] [Google Scholar]
- 27.Müller-Lissner S. General geriatrics and gastroenterology: Constipation and faecal incontinence. Best Pr. Res Clin. Gastroenterol. 2002;16:115–133. doi: 10.1053/bega.2002.0269. [DOI] [PubMed] [Google Scholar]
- 28.Dahl J.J., Sheth N.M. Reverberation clutter from subcutaneous tissue layers: Simulation and in vivo demonstrations. Ultrasound Med. Biol. 2014;40:714–726. doi: 10.1016/j.ultrasmedbio.2013.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perez F., Accarino A., Azpiroz F., Quiroga S., Malagelada J.R. Gas distribution within the human gut: Effect of meals. Am. J. Gastroenterol. 2007;102:842–849. doi: 10.1111/j.1572-0241.2007.01071.x. [DOI] [PubMed] [Google Scholar]
- 30.Sano Y., Muto M., Urata K., Akiyama K. The study of feces property assessment with the ultrasonography: Usefulness of lower rectum assessment by intergluteal cleft approach scanning method. Jpn. J. Med. Ultrasound Technol. 2020;45:168–174. [Google Scholar]
- 31.Matsumoto M., Tsutaoka T., Nakagami G., Tanaka S., Yoshida M., Miura Y. Deep learning-based classification of rectal fecal retention and analysis of fecal properties using ultrasound images in older adult patients. Jpn. J. Nurs. Sci. 2020;17:e12340. doi: 10.1111/jjns.12340. [DOI] [PubMed] [Google Scholar]
- 32.Grossi U., Horrocks E.J., Mason J., Knowles C.H., Williams A.B., NIHR CapaCiTY Working Group. Pelvic Floor Society Surgery for constipation: Systematic review and practice recommendations: Results IV: Recto-vaginal reinforcement procedures. Colorectal. Dis. 2017;3:73–91. doi: 10.1111/codi.13781. [DOI] [PubMed] [Google Scholar]
- 33.Knowles C.H., Grossi U., Chapman M., Mason J., NIHR CapaCiTY Working Group. Pelvic Floor Society Surgery for constipation: Systematic review and practice recommendations: Results I: Colonic resection. Colorectal. Dis. 2017;3:17–36. doi: 10.1111/codi.13779. [DOI] [PubMed] [Google Scholar]
- 34.Picciariello A., O’Connell P.R., Hahnloser D., Gallo G., Munoz-Duyos A., Schwandner O. Obstructed defaecation syndrome: European consensus guidelines on the surgical management. Br. J. Surg. 2021;108:1149–1153. doi: 10.1093/bjs/znab123. [DOI] [PubMed] [Google Scholar]
- 35.Corsetti M., Brown S., Chiarioni G., Dimidi E., Dudding T., Emmanuel A. Chronic constipation in adults: Contemporary perspectives and clinical challenges. 2: Conservative, behavioural, medical and surgical treatment. Neurogastroenterol. Motil. 2021;33:e14070. doi: 10.1111/nmo.14070. [DOI] [PubMed] [Google Scholar]