Abstract
Alcohol consumption is a known, modifiable risk factor for incident atrial fibrillation (AF). However, it remains unclear whether the protective effect of moderate alcohol consumption-that has been reported for various cardiovascular diseases also applies to the risk for new-onset AF. The purpose of this meta-analysis was to evaluate the role of different drinking patterns (low: <14 grams/week; moderate: <168 grams/week; and heavy: >168 grams/week) on the risk for incident AF. Major electronic databases were searched for observational cohorts examining the role of different drinking behaviors on the risk for incident AF. We analyzed 16 studies (13,044,007 patients). Incident AF rate was 2.3%. Moderate alcohol consumption significantly reduced the risk for new-onset AF when compared to both abstainers (logOR: −0.20; 95%CI: −0.28–−0.12; I2: 96.71%) and heavy drinkers (logOR: −0.28; 95%CI: −0.37–−0.18; I2: 95.18%). Heavy-drinking pattern compared to low also increased the risk for incident AF (logOR: 0.14; 95%CI: 0.01–0.2; I2: 98.13%). Substantial heterogeneity was noted, with more homogeneous results documented in cohorts with follow-up shorter than five years. Our findings suggest a J-shaped relationship between alcohol consumption and incident AF. Up to 14 drinks per week seem to decrease the risk for developing AF. Because of the substantial heterogeneity observed, no robust conclusion can be drawn. In any case, our results suggest that the association between alcohol consumption and incident AF is far from being a straightforward dose-response effect.
Keywords: atrial fibrillation, incidence, alcohol, risk factor, drinking, lifestyle
1. Introduction
Atrial fibrillation (AF) is the most common arrhythmia in adults [1], with an estimated prevalence between 2% and 4% [2]. The complexity of its pathogenesis requires a holistic and multidisciplinary approach to the management of AF patients, and the potential impact of multiple comorbidities on AF risk underscores the importance of controlling modifiable risk factors.
Modifiable risk factors are potent contributors to AF development and progression [3]. The Atrial Fibrillation Better Care (ABC) pathway provides an integrated model of care of AF patients as compared to usual care [4,5]. The “C” part of the ABC pathway involves, among other interventions, investigation and management of unhealthy lifestyle factors, such as smoking, alcohol consumption, and physical inactivity [6]. Specifically, both acute and chronic alcohol consumption are modifiable risk factors for incident AF [7,8]. Moreover, a recent RCT reported that alcohol abstinence reduced AF recurrence in regular drinkers with AF [9]. Nevertheless, whether there is a kind of protective alcohol consumption, as it has been reported for a variety of cardiovascular diseases [10], as well as the amount of alcohol that may be clinically relevant [11] remain unclear.
In this systematic review and meta-analysis, we aimed to explore the impact of different drinking patterns on the risk for developing AF.
2. Materials and Methods
This systematic review and meta-analysis was performed according to the PRISMA guidelines [12]. The predefined protocol was registered in PROSPERO database (ID: 303961).
Medline (via PubMed) and Scopus were searched using a strategy based on the following combination of keywords (((“alcohol consumption”) OR (“alcohol drinking”) OR (“binge drinking”) OR (“alcohol intake”)) AND (“atrial fibrillation”)) from inception up to December 2021. Additional hand-search was also performed using the references of the articles that were identified as relevant (snowball strategy).
After deduplication, two independent reviewers (M.K. and I.A.) screened all articles at title and abstract level. Potentially eligible studies were further reviewed based on the full text. In the final analysis, we included observational cohorts examining the association between alcohol consumption and incident AF, if they had a follow-up period of at least 1year, and they reported raw incidence numbers (cases/controls) for at least 3 categories of drinking behavior (i.e., abstainers/low consumption, moderate consumption, and heavy consumption). Articles not available in English were excluded. Any disagreements were resolved by consultation with an expert (G.G.).
Data regarding studies and patient characteristics as well as the outcome of interest were extracted in a predesigned Microsoft Office Excel 2007 by two independent reviewers (M.K. and I.A.). Subsequently, they were crosschecked for any disagreements, which were resolved by a senior (G.G.). Alcohol consumption categories are summarized as grams of alcohol per week (gr/w). When categories were expressed as grams per day, they were transformed to gr/w by multiplying with 7. If they were expressed as standard drinks or units, we assumed that each standard drink contains 12 g of alcohol, and every unit equals 8 g of pure ethanol, according to the definitions mostly used in the included studies. When more than 3 categories were available, we tried to combine them into meaningful groups. We defined abstainers/low consumption as 0–14 gr/w, moderate consumption <168 gr/w (or <84 gr/w for women), and heavy consumption as >168 gr/w (or >84 gr/w for women).
Risk of bias within studies was assessed in duplicate with the National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [13]. Disagreements were resolved by consensus. Studies with an overall score ≥80% were deemed as high quality. Publication bias was evaluated both visually, using contour-enhanced funnel plots (with the level of statistical significance set at 1%, 5%, and 10%) and with Egger’s test [14].
Statistical analysis: Continuous variables were summarized as mean (standard deviation). For pooling the outcomes of interest, we first calculated odds ratios (OR) along with their corresponding 95% confidence intervals (CI); subsequently, we transformed logarithmically the calculated OR and 95%CI to perform the final analysis. To allow for expected effect size dispersion between studies, a random effects (DerSimonian–Laird) model was adopted. Heterogeneity was assessed using I2, with values more than 50% representing substantial heterogeneity [15]. To investigate the heterogeneity observed, we performed subgroup analysis based on the duration of follow up and the region that each study was conducted and sensitivity analysis, including only high-quality studies. Furthermore, meta-regression analysis was used to investigate the confounding effect of mean age, mean body mass index, number of males, smokers, and hypertensive and diabetic patients. Finally, we evaluated the linearity between weekly alcohol consumption and the risk for AF. A restricted cubic spline model, with three knots at 25%, 50%, and 75% of the distribution, was crated (using the original subcategories of alcohol intake per week). Linearity was assessed by comparing the slopes of the regression line using the Wald test, with p-values < 0.05 indicating nonlinearrelationship [16]. All analyses were performed using STATA/MP version 16.0, Texas, USA, and R (R Foundation, version 3.6.3) softwares.
3. Results
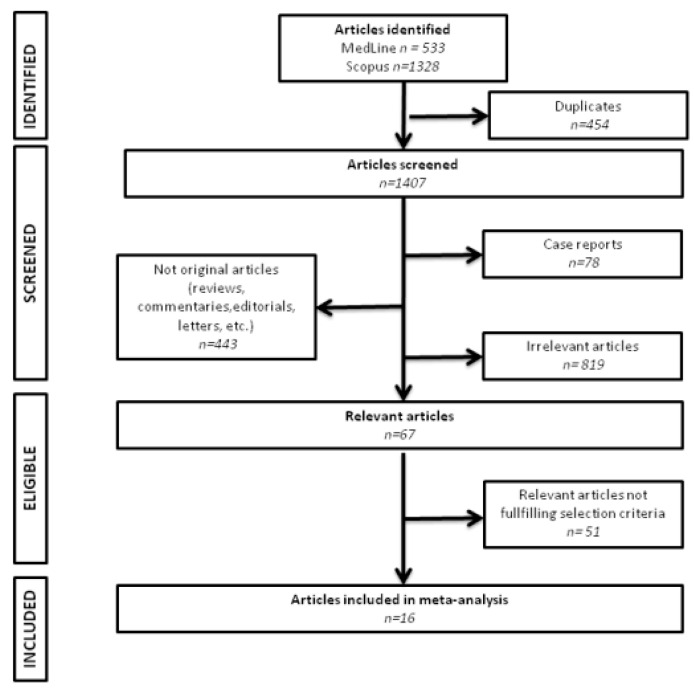
We identified 19 eligible studies. Three of them were excluded due to patient overlapping; thus, we analyzed 16 cohorts [8,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31]. The flow of study selection is summarized in Figure 1. In total, 13,044,007 patients were analyzed, and 305,433 (2.3%) cases of incident AF were documented. Most of the studies were conducted in Europe, and the overall follow-up ranged from 2.7 to up to 50 years. AF was mostly ascertained using medical records and the International Classification of Diseases (ICD) system. Five studies used periodic electrocardiograms to identify patients with newly diagnosed AF. Data regarding the incidence of AF in the low-consumption category were available in all studies, while 15 and 14 of them provided meaningful information for the moderate and heavy-consumption categories, respectively. Study characteristics are summarized in Table 1. Transformations used to estimate weekly alcohol consumption in each study are depicted in Supplementary Table S1.
Figure 1.
Flow of study selection.
Table 1.
Characteristics of the included studies.
| Study | Region | Follow-Up (Years) |
Method of AF Diagnosis | N | Males (%) | Age | BMI | HT (%) |
DM (%) |
Sm (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Djoussé L et al., 2004 | US | >50 | ECG | 5727 | 51 | 45.8 8.04 |
NA | NA | 12 | NA |
| Ruigómez A et al., 2005 | UK | 2.7 | ICD | 5525 | 47.2 | NA | NA | 19.1 | 4.2 | 29.7 |
| Conen D et al., 2008 | U.S. | 12.4 | ECG. medical records | 34.715 | 0 | 53.1 7.1 |
24.9 4.5 |
25.3 | 2.4 | 48.5 |
| Liang Y et al., 2012 | Multi-center | 4.6 | ECG | 30.433 | 70 | 66.4 7.2 |
NA | 70 | 37.2 | 62.3 |
| Sano F et al., 2014 | Japan | 6.4 | ECG. medical records | 8284 | 35.7 | 56 | NA | 30.2 | NA | 18.6 |
| Larsson SC et al., 2015 | Sweden | 12 | ICD. ECG | 75.276 | 58.2 | 60.5 | 25.4 | 22.3 | 7 | 23.9 |
| Martín-Pérez M et al., 2016 | UK | 2.7 | medical records | 4489 | 55 | NA | NA | NA | NA | 58.7 |
| Tolstrup JS et al., 2016 | Denmark | 6.1 | ICD | 88.782 | 45.1 | 57.4 14.5 |
25.4 4.1 |
18.1 | 3.7 | 22.3 |
| Gémes K et al., 2017 | Norway | 8 | ECG | 47.002 | 44.9 | 52.3 15.7 |
27.1 4.4 |
NA | NA | 55.9 |
| Di Castelnuovo A et al., 2017 | Italy | 8.2 | medical records | 22.065 | 48.6 | 55.3 11.9 |
28 4.6 |
55.7 | 9.2 | 23.6 |
| Garg PK et al., 2018 | U.S. | 9.4 | ECG. self-reports | 9576 | 42.6 | 63.3 8.1 |
29 6 |
NA | NA | 12.6 |
| Ariansen I et al., 2020 (males) | Norway | 9 | hospital discharge diagnosis | 234.392 | 48.4 | 43.5 10 |
25.6 3.8 |
NA | 1.2 | 63.4 |
| Kim YG et al., 2020 | Korea | NA | ICD | 9.776.956 | 54.7 | 47 14.1 |
23.7 3.2 |
25.4 | 8.6 | 40.4 |
| Lee SR et al., 2020 | Korea | 5 | ICD | 1.719.401 | 46 | 66 0 |
24.3 3 |
53 | 20.5 | 30.6 |
| Park CS et al., 2021 | Korea | 7.1 | ICD | 2.551.036 | 59.9 | 57.7 11.9 |
NA | 56.8 | 100 | 44.1 |
| Choi YJ et al., 2021 | Korea | 4 | ICD | 112.984 | 35 | 63.3 10.6 |
25.1 3.3 |
21.7 | 100 | 23.8 |
AF, atrial fibrillation; N, number of patients; BMI, body mass index; HT, hypertension; DM, diabetes mellitus; Sm, smokers; NA, not available; U.S., United States of America; UK, United Kingdom; ECG, electrocardiogram; ICD, International Classification of Diseases. Continuous variables are summarized as mean (SD).
The risk of bias assessment is summarized in Supplementary Table S2. Nine studies were deemed as moderate quality (score between 70 and 80%), mainly due to the absence of both power analysis description and exposure reassessment. Only four cohorts presented low risk of bias. No significant publication bias was revealed except the analysis regarding moderate versus low consumption. (Supplementary Figures S1–S3). The corresponding Egger’s test p-values were 0.08 for heavy versus low consumption, <0.001 for moderate versus low consumption, and 0.9 for heavy versus moderate consumption.
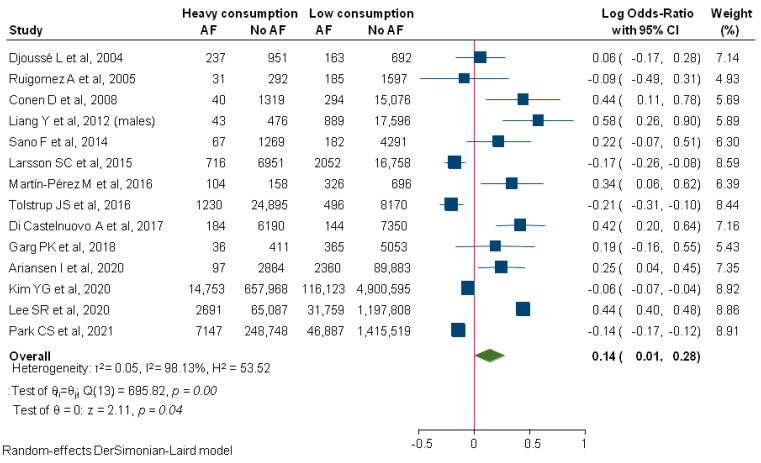
Compared to low consumption, heavy alcohol consumption significantly increased the risk for new-onset AF (logOR: 0.14; 95%CI: 0.01–0.2; I2: 98.13%; Figure 2). In subgroup analysis, significantly lower heterogeneity was documented for studies with an overall follow up of less than 5 years (logOR: 0.37; 95%CI: 0.17–0.56; I2: 62.23%), while the effect size was non-significant for studies that followed patients for a longer time period (logOR: 0.07; 95%CI: −0.06–0.19; I2: 87.27%).
Figure 2.
Comparison between heavy and low alcohol consumption regarding incident AF. AF, Atrial Fibrillation.
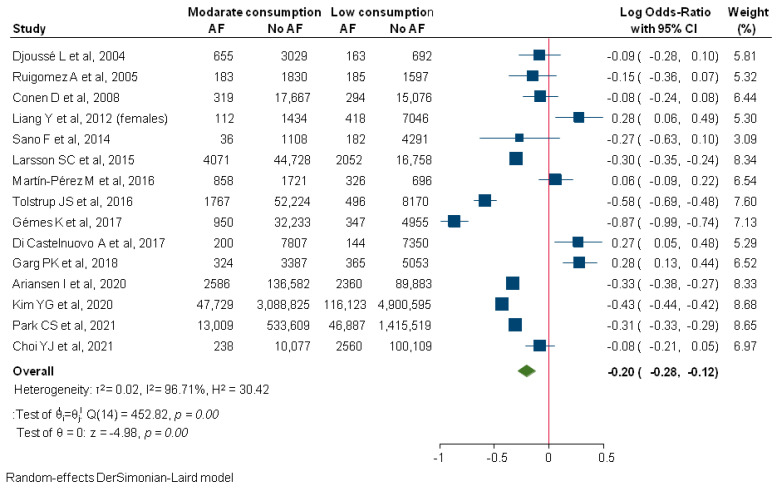
Patients following a moderate consumption pattern were at significantly lower risk for new-onset AF compared to abstainers (logOR: −0.20; 95%CI: −0.28–−0.12; I2: 96.71%; Figure 3). An increasing number of hypertensive patients (p = 0.04) significantly augmented the effect size estimation in meta-regression analysis, explaining almost 10% of the initial heterogeneity.
Figure 3.
Comparison between moderate and low alcohol consumption regarding incident AF. AF, Atrial Fibrillation.
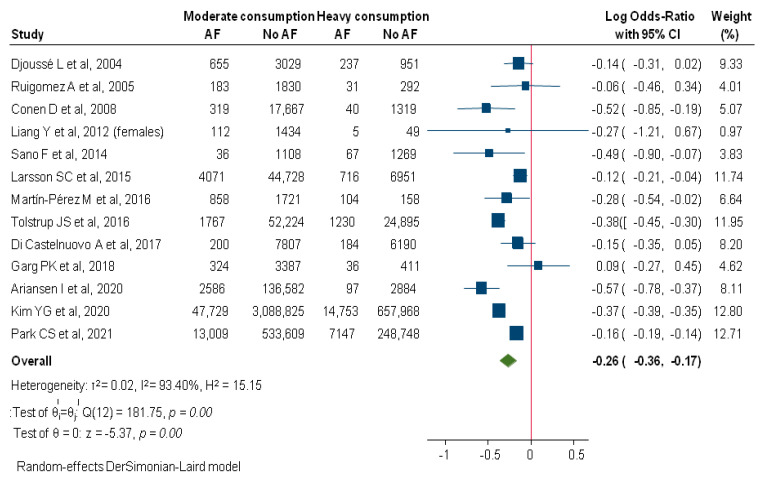
When compared to the heavy-drinking pattern, moderate alcohol consumption was also associated with decreased incidence of AF (logOR: −0.26; 95%CI: −0.36–−0.17; I2: 93.4%; Figure 4). Higher mean age of the included subjects significantly decreased this protective effect (p = 0.03), explaining 43% of the initial heterogeneity. Moreover, analysis of the subgroup of studies with shorter follow up (<5 years) revealed a highly homogeneous estimation (logOR: −0.22; 95%CI: −0.43–−0.003; I2: 0%), while decreased but substantial heterogeneity was found for studies with longer follow up (logOR: −0.25; 95%CI: −0.36–−0.15; I2: 84.61%).
Figure 4.
Comparison between moderate and heavy alcohol consumption regarding incident AF. AF, Atrial Fibrillation.
Sensitivity analysis based on four high-quality cohorts did not change the above-mentioned results (Supplementary Figures S4–S6).
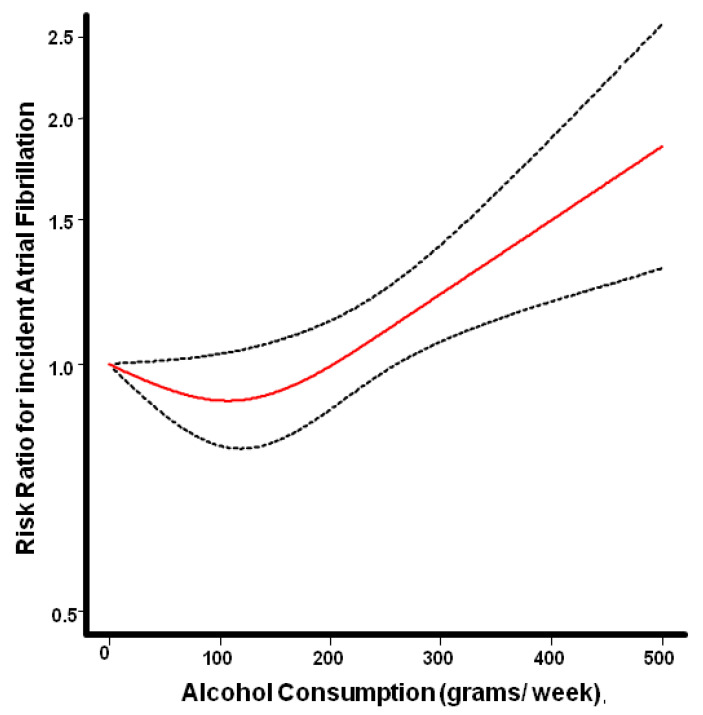
Regression analysis, using the restricted cubic spline model, demonstrated a J-shaped association between alcohol consumption and the risk for AF, without evidence of linearity (p = 0.0017), Figure 5.
Figure 5.
Pooled dose response relationship between weekly alcohol consumption and risk for incident atrial fibrillation seems to follow a J shaped pattern. Abstinence served as the reference category. The red line depicts the estimated risk ratio, while the dotted lines represent the corresponding 95% confidence intervals.
4. Discussion
In this systematic review and meta-analysis, we assessed the potential association between alcohol consumption and incident AF. After categorizing weekly drinking behavior into low, moderate, and heavy drinking, we demonstrated that moderate alcohol consumption pattern may yield a kind of protective effect against new-onset AF. Subjects consuming up to two drinks per day were in significantly lower risk compared to heavy drinkers, especially hypertensive ones. Moreover, this attenuated risk of mild drinking pattern was maintained in the comparison with the abstainers although it seems to be more evident in younger subjects. The heavy-drinking pattern was found to be the most harmful, as it also significantly increased the risk for incident AF when compared to the low pattern. These results should be interpreted with great caution because of the substantial heterogeneity that was noted in all analyses. Comparisons involving the heavy-drinking pattern, in particular, seem to be more homogeneous in the subgroup of studies with shorter mean follow up, which might reflect changing drinking behavior over the time.
These results are in line with previous analyses reporting that high levels of alcohol intake increase the risk for new-onset AF [32,33,34]. Gallagher et al. [32] examined the impact of moderate drinking behavior. They reported that consuming up to 6–7 standard drinks per week is not associated with higher incidence of AF. The current analysis suggests that consuming up to 14 drinks per week is probably associated with a kind of “protective” effect against AF even when compared to an abstinence pattern (up to 1–2 drinks per week). This contradicts the conclusions of Larsson et al. [21], which suggested that even moderate alcohol consumption is a risk factor for atrial fibrillation. Their meta-analysis, however, differs significantly in terms of methodology and study selection.
Beneficial cardiovascular effects of moderate alcohol consumption have been previously described. Ding et al. recently reported that a reduction in both cardiovascular events and cardiovascular mortality was observed in patients with a weekly intake of 42–56 g of alcohol [10], while Yoon et al., despite almost similar results, questioned these protective effects in younger people and in patients with multiple comorbidities [35]. Moreover, various researchers have reported that light to moderate consumption either reduces or does not affect the incidence of various classic risk factors for AF development. Attenuated risk for type 2 diabetes [36], heart failure [37] and coronary heart disease [10,38] has also been described. Similar results have been documented for chronic kidney disease [39], chronic obstructive pulmonary disease [40], and mental health [41]. Finally, the role of alcohol consumption regarding incident hypertension remains controversial [42,43]. Conceptually, the notion that a factor, namely low-to-moderate alcohol consumption, which appears to have a largely beneficial effect on cardiovascular disease risk and even on overall mortality (25% lower mortality [6]), is straightforwardly detrimental in terms of incident AF borders on the paradoxical.
On the other hand, alcohol consumption seems to yield an unfavorable effect on atrial structure and function. Voskoboinik et al., after performing high-density mapping in patients undergoing AF ablation, reported lower bipolar voltages and more frequent complex potentials in drinkers compared to non-drinkers [44]. In addition, impaired left atrium mechanics [45] and increased levels of atrial natriuretic peptides [46] and left atrial size [47,48] have been documented in patients consuming alcohol regularly, irrespective of the amount.
This study has several limitations. A major one is the substantial heterogeneity that was found across all comparisons and limits the applicability of our findings. Furthermore, information about alcohol consumption was provided by the subjects, which may be a source of recall bias. It is also possible that a substantial number of patients might have changed their drinking behavior throughout the follow up. Moreover, baseline comorbidities, which could account for at least a part of the observed heterogeneity, were inadequately reported by most studies. Finally, the beverage-specific effects on incident AF may have influenced our analysis.
5. Conclusions
In this systematic review and meta-analysis, we demonstrate that the association between alcohol consumption and the risk for AF may follow a J-shaped curve; meta-regression analysis did not show that this pattern could be attributed to potential confounders. Based on current literature, this risk reduction might be attributed to the protective effect of moderate drinking regarding various known risk factors for AF development. These results should be interpreted with caution because of the substantial heterogeneity that was revealed, and no clear clinical implications can be suggested. Further studies emphasizing on the role of moderate consumption are needed to clarify this relationship and evolve our understanding regarding the underlying pathophysiology. In any case, our results suggest that the association between alcohol consumption and incident AF is far from being a straightforward dose-response effect.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics12020479/s1, Table S1: Transformation of the original alcohol consumption categories for the final analysis. Table S2: Quality assessment, Figure S1: Contour enhanced funnel plot for the comparison between heavy and low alcohol consumption. Figure S2: Contour enhanced funnel plot for the comparison between moderate and heavy alcohol consumption. Figure S3: Contour enhanced funnel plot for the comparison between moderate and low alcohol consumption. Figure S4: Comparison between heavy and low alcohol consumption regarding incident AF. Sensitivity analysis. Figure S5: Comparison between moderate and heavy alcohol consumption regarding incident AF. Sensitivity analysis. Figure S6: Comparison between moderate and low alcohol consumption regarding incident AF. Sensitivity analysis.
Author Contributions
Formal analysis, resources, data curation, writing—original draft preparation, I.A., M.K., S.V., G.G.; writing—review and editing, S.D., V.V., G.G.; supervision, V.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Conen D., Chae C.U., Glynn R.J., Tedrow U.B., Everett B.M., Buring J.E., Albert C.M. Risk of death and cardiovascular events in initially healthy women with new-onset atrial fibrillation. JAMA. 2011;305:2080–2087. doi: 10.1001/jama.2011.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benjamin E.J., Muntner P., Alonso A., Bittencourt M.S., Callaway C.W., Carson A.P., Chamberlain A.M., Chang A.R., Cheng S., Das S.R., et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 3.Huxley R.R., Lopez F.L., Folsom A.R., Agarwal S.K., Loehr L.R., Soliman E.Z., Maclehose R., Konety S., Alonso A. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: The Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2011;123:1501–1508. doi: 10.1161/CIRCULATIONAHA.110.009035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lip G.Y.H. The ABC pathway: An integrated approach to improve AF management. Nat. Rev. Cardiol. 2017;14:627–628. doi: 10.1038/nrcardio.2017.153. [DOI] [PubMed] [Google Scholar]
- 5.Guo Y., Lane D.A., Wang L., Zhang H., Wang H., Zhang W., Wen J., Xing Y., Wu F., Xia Y., et al. Mobile Health Technology to Improve Care for Patients With Atrial Fibrillation. J. Am. Coll. Cardiol. 2020;75:1523–1534. doi: 10.1016/j.jacc.2020.01.052. [DOI] [PubMed] [Google Scholar]
- 6.Rienstra M., Hobbelt A.H., Alings M., Tijssen J.G.P., Smit M.D., Brügemann J., Geelhoed B., Tieleman R.G., Hillege H.L., Tukkie R., et al. Targeted therapy of underlying conditions improves sinus rhythm maintenance in patients with persistent atrial fibrillation: Results of the RACE 3 trial. Eur. Heart J. 2018;39:2987–2996. doi: 10.1093/eurheartj/ehx739. [DOI] [PubMed] [Google Scholar]
- 7.Voskoboinik A., Prabhu S., Ling L.H., Kalman J.M., Kistler P.M. Alcohol and Atrial Fibrillation: A Sobering Review. J. Am. Coll. Cardiol. 2016;68:2567–2576. doi: 10.1016/j.jacc.2016.08.074. [DOI] [PubMed] [Google Scholar]
- 8.Conen D., Tedrow U.B., Cook N.R., Moorthy M.V., Buring J.E., Albert C.M. Alcohol consumption and risk of incident atrial fibrillation in women. JAMA. 2008;300:2489–2496. doi: 10.1001/jama.2008.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Voskoboinik A., Kalman J.M., De Silva A., Nicholls T., Costello B., Nanayakkara S., Prabhu S., Stub D., Azzopardi S., Vizi D., et al. Alcohol Abstinence in Drinkers with Atrial Fibrillation. N. Engl. J. Med. 2020;382:20–28. doi: 10.1056/NEJMoa1817591. [DOI] [PubMed] [Google Scholar]
- 10.Ding C., O’Neill D., Bell S., Stamatakis E., Britton A. Association of alcohol consumption with morbidity and mortality in patients with cardiovascular disease: Original data and meta-analysis of 48,423 men and women. BMC Med. 2021;19:167. doi: 10.1186/s12916-021-02040-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marcus G.M., Vittinghoff E., Whitman I.R., Joyce S., Yang V., Nah G., Gerstenfeld E.P., Moss J.D., Lee R.J., Lee B.K., et al. Acute Consumption of Alcohol and Discrete Atrial Fibrillation Events. Ann. Intern. Med. 2021;174:1503–1509. doi: 10.7326/M21-0228. [DOI] [PubMed] [Google Scholar]
- 12.Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009;62:e1–e34. doi: 10.1016/j.jclinepi.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 13.National Institutes of Health Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. [(accessed on 19 December 2021)];2014 Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
- 14.Egger M., Smith G.D., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. Br. Med. J. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryan R., Cochrane Consumers and Communication Review Group Heterogeneity and subgroup analyses in Cochrane Consumers and Communication Group Reviews: Planning the Analysis at Protocol Stage. [(accessed on 19 December 2021)]. Available online: https://cccrg.cochrane.org/sites/cccrg.cochrane.org/files/public/uploads/heterogeneity_subgroup_analyses_revising_december_1st_2016.pdf.
- 16.Harrell F.E., Jr., Lee K.L., Pollock B.G. Regression models in clinical studies: Determining relationships between predictors and response. J. Natl. Cancer Inst. 1988;80:1198–1202. doi: 10.1093/jnci/80.15.1198. [DOI] [PubMed] [Google Scholar]
- 17.Djoussé L., Levy D., Benjamin E.J., Blease S.J., Russ A., Larson M.G., Massaro J.M., D’Agostino R.B., Wolf P.A., Ellison R.C. Long-term alcohol consumption and the risk of atrial fibrillation in the Framingham Study. Am. J. Cardiol. 2004;93:710–713. doi: 10.1016/j.amjcard.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 18.Ruigómez A., Johansson S., Wallander M.A., García Rodríguez L.A. Predictors and prognosis of paroxysmal atrial fibrillation in general practice in the UK. BMC Cardiovasc. Disord. 2005;5:20. doi: 10.1186/1471-2261-5-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang Y., Mente A., Yusuf S., Gao P., Sleight P., Zhu J., Fagard R., Lonn E., Teo K.K., ONTARGET and TRANSCEND Investigators Alcohol consumption and the risk of incident atrial fibrillation among people with cardiovascular disease. CMAJ. 2012;184:E857–E866. doi: 10.1503/cmaj.120412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sano F., Ohira T., Kitamura A., Imano H., Cui R., Kiyama M., Okada T., Yamagishi K., Sankai T., Tanigawa T., et al. Heavy alcohol consumption and risk of atrial fibrillation. The Circulatory Risk in Communities Study (CIRCS) Circ. J. 2014;78:955–961. doi: 10.1253/circj.CJ-13-1387. [DOI] [PubMed] [Google Scholar]
- 21.Larsson S.C., Drca N., Wolk A. Alcohol consumption and risk of atrial fibrillation: A prospective study and dose-response meta-analysis. J. Am. Coll. Cardiol. 2014;64:281–289. doi: 10.1016/j.jacc.2014.03.048. [DOI] [PubMed] [Google Scholar]
- 22.Martín-Pérez M., Ruigómez A., Michel A., García Rodríguez L.A. Incidence and risk factors for atrial fibrillation in patients with newly diagnosed heart failure. J. Cardiovasc. Med. (Hagerstown) 2016;17:608–615. doi: 10.2459/JCM.0000000000000403. [DOI] [PubMed] [Google Scholar]
- 23.Tolstrup J.S., Wium-Andersen M.K., Ørsted D.D., Nordestgaard B.G. Alcohol consumption and risk of atrial fibrillation: Observational and genetic estimates of association. Eur. J. Prev. Cardiol. 2016;23:1514–1523. doi: 10.1177/2047487316641804. [DOI] [PubMed] [Google Scholar]
- 24.Gémes K., Malmo V., Laugsand L.E., Loennechen J.P., Ellekjaer H., László K.D., Ahnve S., Vatten L.J., Mukamal K.J., Janszky I. Does Moderate Drinking Increase the Risk of Atrial Fibrillation? The Norwegian HUNT (Nord-Trøndelag Health) Study. J. Am. Heart Assoc. 2017;6:e007094. doi: 10.1161/JAHA.117.007094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Di Castelnuovo A., Costanzo S., Bonaccio M., Rago L., De Curtis A., Persichillo M., Bracone F., Olivieri M., Cerletti C., Donati M.B., et al. Moderate Alcohol Consumption Is Associated with Lower Risk for Heart Failure But Not Atrial Fibrillation. JACC Heart Fail. 2017;5:837–844. doi: 10.1016/j.jchf.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 26.Garg P.K., O’Neal W.T., Ogunsua A., Thacker E.L., Howard G., Soliman E.Z., Cushman M. Usefulness of the American Heart Association’s Life Simple 7 to Predict the Risk of Atrial Fibrillation (from the REasons for Geographic And Racial Differences in Stroke [REGARDS] Study) Am. J. Cardiol. 2018;121:199–204. doi: 10.1016/j.amjcard.2017.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ariansen I., Degerud E., Gjesdal K., Tell G.S., Næss Ø. Examining the lower range of the association between alcohol intake and risk of incident hospitalization with atrial fibrillation. Int. J. Cardiol. Heart Vasc. 2020;31:100679. doi: 10.1016/j.ijcha.2020.100679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kim Y.G., Han K.D., Choi J.I., Boo K.Y., Kim D.Y., Lee K.N., Shim J., Kim J.S., Kim Y.H. Frequent drinking is a more important risk factor for new-onset atrial fibrillation than binge drinking: A nationwide population-based study. Europace. 2020;22:216–224. doi: 10.1093/europace/euz256. [DOI] [PubMed] [Google Scholar]
- 29.Lee S.R., Choi E.K., Ahn H.J., Han K.D., Oh S., Lip G.Y.H. Association between clustering of unhealthy lifestyle factors and risk of new-onset atrial fibrillation: A nationwide population-based study. Sci. Rep. 2020;10:19224. doi: 10.1038/s41598-020-75822-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Park C.S., Han K.D., Choi E.K., Kim D.H., Lee H.J., Lee S.R., Oh S. Lifestyle is associated with atrial fibrillation development in patients with type 2 diabetes mellitus. Sci. Rep. 2021;11:4676. doi: 10.1038/s41598-021-84307-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choi Y.J., Han K.D., Choi E.K., Jung J.H., Lee S.R., Oh S., Lip G.Y.H. Alcohol Abstinence and the Risk of Atrial Fibrillation in Patients With Newly Diagnosed Type 2 Diabetes Mellitus: A Nationwide Population-Based Study. Diabetes Care. 2021;44:1393–1401. doi: 10.2337/dc20-2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gallagher C., Hendriks J.M.L., Elliott A.D., Wong C.X., Rangnekar G., Middeldorp M.E., Mahajan R., Lau D.H., Sanders P. Alcohol and incident atrial fibrillation—A systematic review and meta-analysis. Int. J.Cardiol. 2017;246:46–52. doi: 10.1016/j.ijcard.2017.05.133. [DOI] [PubMed] [Google Scholar]
- 33.Kodama S., Saito K., Tanaka S., Horikawa C., Saito A., Heianza Y., Anasako Y., Nishigaki Y., Yachi Y., Iida K.T., et al. Alcohol consumption and risk of atrial fibrillation: A meta-analysis. J. Am. Coll. Cardiol. 2011;57:427–436. doi: 10.1016/j.jacc.2010.08.641. [DOI] [PubMed] [Google Scholar]
- 34.Samokhvalov A.V., Irving H.M., Rehm J. Alcohol consumption as a risk factor for atrial fibrillation: A systematic review and meta-analysis. Eur. J. Cardiovasc. Prev. Rehabil. 2010;17:706–712. doi: 10.1097/HJR.0b013e32833a1947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yoon S.J., Jung J.G., Lee S., Kim J.S., Ahn S.K., Shin E.S., Jang J.E., Lim S.H. The protective effect of alcohol consumption on the incidence of cardiovascular diseases: Is it real? A systematic review and meta-analysis of studies conducted in community settings. BMC Public Health. 2020;20:90. doi: 10.1186/s12889-019-7820-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li X.H., Yu F.F., Zhou Y.H., He J. Association between alcohol consumption and the risk of incident type 2 diabetes: A systematic review and dose-response meta-analysis. Am. J. Clin. Nutr. 2016;103:818–829. doi: 10.3945/ajcn.115.114389. [DOI] [PubMed] [Google Scholar]
- 37.Larsson S.C., Wallin A., Wolk A. Alcohol consumption and risk of heart failure: Meta-analysis of 13 prospective studies. Clin. Nutr. 2018;37:1247–1251. doi: 10.1016/j.clnu.2017.05.007. [DOI] [PubMed] [Google Scholar]
- 38.Ronksley P.E., Brien S.E., Turner B.J., Mukamal K.J., Ghali W.A. Association of alcohol consumption with selected cardiovascular disease outcomes: A systematic review and meta-analysis. BMJ. 2011;342:d671. doi: 10.1136/bmj.d671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yuan H.C., Yu Q.T., Bai H., Xu H.Z., Gu P., Chen L.Y. Alcohol intake and the risk of chronic kidney disease: Results from a systematic review and dose-response meta-analysis. Eur. J. Clin. Nutr. 2021;75:1555–1567. doi: 10.1038/s41430-021-00873-x. [DOI] [PubMed] [Google Scholar]
- 40.Kaluza J., Harris H.R., Linden A., Wolk A. Alcohol Consumption and Risk of Chronic Obstructive Pulmonary Disease: A Prospective Cohort Study of Men. Am. J. Epidemiol. 2019;188:907–916. doi: 10.1093/aje/kwz020. [DOI] [PubMed] [Google Scholar]
- 41.Mezue K., Abbas T., Radfar A., Zureigat H., Abohashem S., Shin L., Pitman R., Osborne M., Tawakol A. Alcohol’s Beneficial Effect on Cardiovascular Disease Is Partially Mediated through Modulation of Stress-Associated Brain Activity. J. Am. Coll. Cardiol. 2021;77((Suppl. 2)):6. doi: 10.1016/S0735-1097(21)01349-8. [DOI] [Google Scholar]
- 42.Briasoulis A., Agarwal V., Messerli F.H. Alcohol consumption and the risk of hypertension in men and women: A systematic review and meta-analysis. J. Clin. Hypertens. (Greenwich) 2012;14:792–798. doi: 10.1111/jch.12008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roerecke M., Tobe S.W., Kaczorowski J., Bacon S.L., Vafaei A., Hasan O.S.M., Krishnan R.J., Raifu A.O., Rehm J. Sex-Specific Associations Between Alcohol Consumption and Incidence of Hypertension: A Systematic Review and Meta-Analysis of Cohort Studies. J. Am. Heart Assoc. 2018;7:e008202. doi: 10.1161/JAHA.117.008202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Voskoboinik A., Wong G., Lee G., Nalliah C., Hawson J., Prabhu S., Sugumar H., Ling L.H., McLellan A., Morton J., et al. Moderate alcohol consumption is associated with atrial electrical and structural changes: Insights from high-density left atrial electroanatomic mapping. Heart Rhythm. 2019;16:251–259. doi: 10.1016/j.hrthm.2018.10.041. [DOI] [PubMed] [Google Scholar]
- 45.Hung C.L., Gonçalves A., Lai Y.J., Lai Y.H., Sung K.T., Lo C.I., Liu C.C., Kuo J.Y., Hou C.J., Chao T.F., et al. Light to Moderate Habitual Alcohol Consumption Is Associated with Subclinical Ventricular and Left Atrial Mechanical Dysfunction in an Asymptomatic Population: Dose-Response and Propensity Analysis. J. Am. Soc. Echocardiogr. 2016;29:1043–1051. doi: 10.1016/j.echo.2016.07.014. [DOI] [PubMed] [Google Scholar]
- 46.Djoussé L., Hunt S.C., Eckfeldt J.H., Arnett D.K., Province M.A., Ellison R.C. Alcohol consumption and plasma atrial natriuretic peptide (from the HyperGEN study) Am. J. Cardiol. 2006;98:628–632. doi: 10.1016/j.amjcard.2006.03.041. [DOI] [PubMed] [Google Scholar]
- 47.Voskoboinik A., Costello B.T., Kalman E., Prabhu S., Sugumar H., Wong G., Nalliah C., Ling L.H., McLellan A., Hettige T., et al. Regular Alcohol Consumption Is Associated With Impaired Atrial Mechanical Function in the Atrial Fibrillation Population: A Cross-Sectional MRI-Based Study. JACC Clin. Electrophysiol. 2018;4:1451–1459. doi: 10.1016/j.jacep.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 48.Singh K.J., Cohen B.E., Na B., Regan M., Schiller N.B., Whooley M.A. Alcohol consumption and 5-year change in left atrial volume among patients with coronary heart disease: Results from the Heart and Soul study. J. Card. Fail. 2013;19:183–189. doi: 10.1016/j.cardfail.2012.12.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.