Abstract
Background: Lanthanum carbonate is a phosphate binder used in advanced kidney disease. Its radiopaque appearance has been described in many case studies and case series. Misinterpretation of this phenomenon leads to unnecessary diagnostic tests and procedures. The objectives of this study were to summarize the literature on lanthanum carbonate opacities and present a visual overview. Methods: A systematic search was conducted using MEDLINE, Embase, and Web of Science. We included all types of studies, including case reports/studies, describing radiological findings of lanthanum carbonate opacities in patients with chronic kidney disease. No filter for time was set. Results: A total of 36 articles were eligible for data extraction, and 33 articles were included in the narrative synthesis. Lanthanum carbonate opacities were most commonly reported in the intestines (26 studies, 73%), stomach (8 studies, 21%), and the aerodigestive tract (2 studies, 6%). The opacities in the intestine were most frequently described as multiple, scattered radiopaque densities, compared with the aerodigestive tract, where the opacities were described as a single, round foreign body. Suspicion of contrast medium or foreign bodies was the most common differential diagnosis. LC opacities in patients with CKD are commonly misinterpreted as foreign bodies or suspect contrast media. Conclusions: CKD patients treated with LC may have opacities throughout the digestive tract that can vary in appearance. Stopping LC treatment or changing to an alternative phosphate binder prior to planned image studies can avoid diagnostic confusion. If this is not an option, knowledge of the presentation of LC opacities is important.
Keywords: lanthanum carbonate, image studies, CKD
1. Introduction
Phosphate retention exacerbates renal osteodystrophy and increases the risk of soft tissue and vascular calcification and death [1]. Therefore, medical treatment includes phosphate binders [2]. Phosphate binders are used to control hyperphosphatemia [3]. They can be divided into calcium-containing phosphate binders such as calcium carbonate and calcium acetate. In cases of increased calcium levels, calcium-free phosphate binders, including the most widely used calcium-free phosphate binders sevelamer and lanthanum carbonate (LC), are used.
LC Lanthanum carbonate was introduced in 2005 in the United States, and in 2009 in Japan, under the brand name Fosrenol™ [4,5]. LC is available as a chewable tablet or oral powder [6]. It disassociates in the upper gastrointestinal tract to lanthanum ions (La3+), forming insoluble lanthanum phosphate complexes that pass through the GI tract almost unabsorbed [6,7]. The absorbed part is excreted in bile [7]. The appearance of LC-associated opacities’ was first described in 2006, suggesting that the opacities were related to calcium-phosphate accumulation [8]. However, it has since become clear that LC is responsible for the opacities [9]. The atomic number in LC is relatively high, at 57, and therewith close to barium at 56, which could explain the similarity to contrast signals. Other studies have described how the opacities in various anatomical regions with different image procedures can cause confusion with differential diagnosis. In worst cases, misinterpretation leads to unnecessary follow-up, delayed operations or procedures, and even surgical interventions [10,11,12,13].
This study was designed to identify the most common differential diagnosis and pitfalls when LC opacities are misinterpreted. In addition, we provide a visual overview of the varying appearances of LC in the digestive tract. Our systematic review is the first to assess LC opacities’ locations and appearances on different image modalities. Finally, we discuss directions for future research.
2. Materials and Methods
A systematic review was performed in accordance with the PRISMA statement [14]. The review was registered in advance at Prospero with the registration number CRD42020204971.
2.1. Eligibility
We included peer-reviewed studies of the radiological findings of chronic kidney disease patients treated with lanthanum carbonate opacities and published in English. We excluded posters, reviews or abstracts, or papers published in a language other than English.
2.2. Search Strategy and Study Selection
A database search in MEDLINE, Embase, and Web of Science was conducted on 23 September 2020. The search consisted of two blocks—one for chronic kidney disease (CKD) and one for LC. The two blocks were combined with the Boolean operator AND and modified accordingly for each database. The full search strategy can be found in Supplementary Materials. There were no filters used in relation to time. The OVID™ filter was used to locate articles published in English to identify human studies only.
Articles were uploaded to Covidence™, and duplicates were removed. All studies were screened by title and abstract and, if eligible, for full text, by two independent investigators (J.K. and N.P.H.). A.N.Ø.S. was consulted as a referee in case of disagreement.
2.3. Data Extraction and Analysis
The following data regarding study characteristics were included in the extraction tables: publication year, country, study type, number of patients and image modality, opacity characteristics, location of opacity and differential diagnosis, type of exposure, and duration. The data were extracted using an Excel prespecified data abstraction form and piloted and evaluated after the first couple of studies had been extracted. Data extraction was performed independently (J.K. and N.P.H.), and in case of disagreement, A.N.Ø.S. was consulted.
Data analysis was conducted using narrative synthesis according to the guidelines for Synthesis without Meta-analysis in Systematic Reviews [15]. Studies were grouped according to exposure time, type of image modality and location of the opacity, and the characteristics of the opacity. Results of the analysis are described in absolute numbers or in percentages.
2.4. Quality Assessment
The quality of the studies was assessed by J.K. and N.P.H. using the “Methodological quality and synthesis of case series and case reports” chart [16]. The chart validated quality using eight questions.
Publications that did not ascertain the outcome (question 2), did not rule out alternative causes (question 4), and did not describe the case in full detail (question 8) were excluded.
The use of the chart for quality assessment of the cohort studies was discussed by J.K. and N.P.H. and found suitable. The aim of this study was to assess the most common differential diagnosis and pitfalls with LC opacities, for which the quality of the studies would be sufficient if they fulfilled the criteria listed in the chart. Hence, the chart was used for all included studies.
3. Results
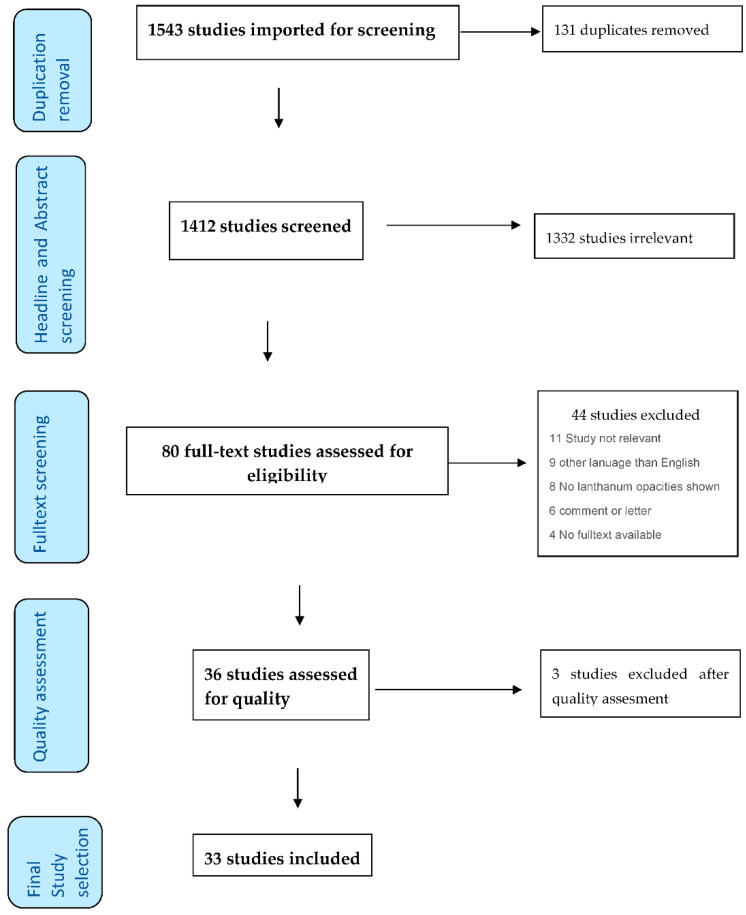
A database search identified 1412 studies after the removal of duplicates. The full-text screening was conducted for 80 studies, of which 36 were included for data extraction. After quality extraction, 3 papers were excluded, resulting in 33 studies for the narrative synthesis (see Figure 1).
Figure 1.
Flowchart on the included studies and the screening process according to PRISMA.
The narrative synthesis consisted of 30 [8,9,10,11,12,13,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40] single case reports, 1 case series [4], and 2 cohort studies [41,42]. The case series included 9 patients, and the cohort studies included 126 and 169 patients.
Therefore, the review consists of reports from a total of 334 patients. The studies were from 14 different countries, with Japan being the most common [4,24,28,31,32,41].
Among the included papers, 13 studies reported dispensing LC in tablet form, but the remaining articles did not specify the dispensation form. The duration of LC treatment ranged from days [12] to 6 years [31]; 19 articles did not specify duration treatment.
Characteristics of included studies can be found in Table 1.
Table 1.
Study and patient characteristics of the included studies.
| Author | Year | Country | Studie Design | Number of Included Patients | Age | Sex | Dialyses Modality | LC Dosis/Day | LC Dispensation Form | Duration of LC Treatment |
|---|---|---|---|---|---|---|---|---|---|---|
| Cerny et al. | 2006 | Germany | Case report | 1 | 82 | M | HD | 4500 mg | NR | 6 mo |
| David et al. | 2007 | Germany | Case report | 1 | 46 | F | HD | 2250 mg | NR | NR |
| C-L Chuang et al. | 2007 | Taiwan | Case report | 1 | 30 | F | PD | 750 mg | NR | 3 mo |
| Singanamala et al. | 2008 | USA | Case report | 1 | 75 | F | (acute) HD | NR | Tablets | NR (added during hospital stay) |
| Pafcugová et al. | 2008 | Czech Republic | Case report | 1 | 77 | M | HD | NR | Tablets | NR |
| Wu et al. | 2008 | Taiwan | Case report | 1 | 56 | F | PD | 2250 mg | Tablets | 6 mo |
| Badre et al. | 2008 | USA | Case report | 1 | 54 | M | HD | 3000 mg | Tablets | 3 mo |
| Kato et al. | 2009 | Japan | Case series | 9 | 41–60 (53 ± 2) | 7 M, 2 F | HD | NR | Tablets | 5–112 days |
| Muller et al. | 2009 | France | Case report | 1 | 75 | F | HD | 1500 mg | Tablets | NR |
| Connor et al. | 2009 | UK | Case report | 1 | 50 | M | HD | NR | NR | NR |
| Turkmen et al. | 2009 | Turkey | Case report | 1 | 56 | F | HD | 3000 mg | NR | NR |
| Huijisoon et al. | 2009 | Netherlands | Case report | 1 | 25 | M | HD | 2250 mg | Tablets | NR |
| Hayashi et al. | 2010 | Japan | Case report | 1 | 68 | M | HD | 750 mg increased to 1500 mg after 4 days | Tablets | 8 days |
| Chacko et al. | 2010 | Australia | Case report | 1 | 66 | F | PD | 2250 mg | NR | NR |
| Hofmann et al. | 2010 | Germany | Case report | 1 | 66 | F | PD | NR | NR | NR |
| Schmitt et al. | 2010 | Germany | Case report | 1 | 54 | F | HD | NR | NR | NR |
| Fürstenberg et al. | 2010 | UK | Cohort study | 169 → 24 prescribed LC (the rest other phosphate binders) | mean age 57 ± 16 (35.5 ± 3.6 in LC group) | 46% M (37.5% in LC group) | 125 PD and 44 HD (PD 66.7% in LC group) | Mean 2250 mg | NR | 10.0 ± 1.3 mo |
| Crush et al. | 2010 | Ireland | Case report | 1 | 62 | M | HD | 3000 mg | NR | 12 mo |
| Walsh et al. | 2011 | USA | Case report | 1 | 64 | M | NR | 3000 mg | NR | NR |
| Vila-Navarro et al. | 2012 | Spain | Case report | 1 | 73 | M | HD | NR | NR | NR |
| Muller et al. | 2012 | France | Case report | 1 | 77 | NR | PD | 3000 mg | Tablets | NR |
| Kuroiwa et al. | 2015 | Japan | Case report | 1 | 66 | M | HD | NR | NR | NR |
| Salerno et al. | 2015 | Belgium | Case report | 1 | 65 | M | HD | 1000 mg | NR | A couple of days |
| Ruiz-Pardo et al. | 2016 | Spain | Case report | 1 | 84 | F | HD | 1500 mg | Tablets | 1 mo |
| Sahbudin et al. | 2016 | UK | Case report | 1 | 66 | M | NR | NR | NR | NR |
| Nishikawa et al. | 2017 | Japan | Case report | 1 | 64 | F | PD | 750–1500 mg | NR | 6 y |
| Harris et al. | 2017 | UK | Case report | 1 | 84 | M | HD | 1000 mg | NR | NR |
| Paranji et al. | 2017 | USA | Case report | 1 | 75 | M | NR | NR | Tablets | NR |
| Shitomi et al. | 2017 | Japan | Cohort study | 23 (14 had CT examinations) | 34–82 | 16 M, 7 F | 3 PD and 20 HD | 750 mg for all, but some had the dose reduced to 500 mg for a period. | NR | 3–67 mo |
| Chang et al. | 2018 | Taiwan | Case report | 1 | 82 | F | HD | 1000 mg | NR | 5 mo |
| Fischer et al. | 2019 | Israel | Case report | 1 | 69 | M | NR | NR | Tablets | NR (added during hospital stay) |
| Shiratori et al. | 2019 | Japan | Case report | 1 | 74 | M | HD | NR | NR | 62 mo |
| Galo et al. | 2019 | USA | Case report | 1 | 21 | M | Acute onset of chronic renal failure. Not started on dialysis at the time of the imaging study. | 3000 mg | Tablets | NR |
3.1. Quality of Included Studies
All but three articles passed the quality assessment. Both of the cohort studies were included and the case series article as well. The quality assessment is displayed in Table 2.
Table 2.
Overview quality assessment on all studies.
| Yes | No | Unclear | |
|---|---|---|---|
| Does the case/the case series mirror the whole experience of the investigator? | 3 | 0 | 33 |
| Was the exposure adequately ascertained? | 20 | 16 | 0 |
| Was the outcome adequately ascertained | 35 | 0 | 1 |
| Were alternative causes ruled out? | 14 | 12 | 10 |
| Was the case/case series described with sufficient details? | 33 | 0 | 3 |
3.2. Type of Image Modality
The most frequent image modality was X-ray, reported in 73% of the papers [8,9,10,11,13,17,18,19,20,21,22,23,25,26,27,29,33,34,35,36,37,38], and CT, reported in 49% of the papers [4,8,9,11,18,19,21,24,26,28,31,32,33,37,41]. Two or more types of radiological imaging were reported in 33% of the papers [8,9,11,18,19,21,26,28,29,33,37].
Location, characteristics of opacity, and differential diagnosis
LC opacities were most commonly reported in the intestines (26 studies, 73%) [4,8,10,11,12,13,17,18,19,21,23,24,25,26,27,28,29,30,33,34,35,36,38,39,40,41,42], with 24% of all of the studied papers specifying the colon [13,23,25,30,34,36,37,39]. LCs were also reported in the stomach, by 21% of all studies [9,19,21,31,32,40,41], or the aerodigestive tract, by 6% of the papers [20,22].
The most frequently reported characteristics of LC in the intestines were multiple, scattered radiopaque densities [4,8,10,11,13,17,18,21,23,25,26,27,29,30,33,34,35,36,37,38,39,40,42], compared with LC opacities in the aerodigestive tract, where LC was reported as a single, round foreign body, with one of the papers describing it as coin shaped [20,22]. Three publications described the LC opacities as multiple, hyperdense elements with sharp edges and beam hardening [9,12,24]. In addition, there was a single case whereby the whole tablet was seen in the terminal ileum together with digested residues in the colon diverticulum [4], and another case in which the opacity is described as a radiopaque puddle with dilation and fecal impaction [19]. All LC opacities from the colon were described as multiple, scattered radiopaque densities [13,23,25,30,34,36,37,39].
Nine (38%) of the papers reporting LC opacities in the intestines also reported suspicion for contrast medium as a differential diagnosis [25,27,30,34,35,36,37,38,39]. All of these cases described multiple, scattered radiopaque densities. For detailed descriptions of varying radiological findings of LC opacities in the stomach [9,19,21,31,32,40,41], see Table 3, and for a visual overview, see Figure 2, Figure 3 and Figure 4.
Table 3.
practical overview including radiological study, finding, location, take-home message, and link to the article.
| Author | Year | Image Study Modality (CT, X-ray, etc.) | Characteristic of Opacity | Location of Opacities | Differential Diagnosis | Take-Home Message | Link to the Article for Further Reference |
|---|---|---|---|---|---|---|---|
| Cerny et al. | 2006 | X-ray | Multiple, scattered radiopaque densities | Colon | Contrast medium (ruled out) | NR | Radiographic Appearance of Lanthanum|NEJM |
| David et al. | 2007 | X-ray + CT | Multiple, scattered radiopaque densities. | Intestines | NR | Lanthanum should temporarily be discontinued prior to image studies. Suggest that radiologic examinations could be used to monitor compliance in patients taking LC. | Heavy metal—rely on gut feelings: novel diagnostic approach to test drug compliance in patients with lanthanum intake|Nephrology Dialysis Transplantation|Oxford Academic (oup.com) |
| C-L Chuang et al. | 2007 | X-ray | Multiple, scattered radiopaque densities. | Intestines | Contrast medium (ruled out) | The phenomenon should be brought to the radiologist’s attention. | The Case∣A peritoneal dialysis patient with an unusual abdominal Film—ScienceDirect |
| Singanamala et al. | 2008 | X-ray | Single, round foreign body. | Aerodigestive tract | Foreign object | NR | Images in Dialysis Series Editors: Ursula C. Brewster and Mark A. Perazella: An Unexpected Finding on Chest Roentgenogram Following Hemodialysis Catheter Placement—Singanamala—2008—Seminars in Dialysis—Wiley Online Library |
| Pafcugová et al. | 2008 | X-ray + CT | Hyperdense elements with sharp edges + beam hardening. | Stomach | NR | Switch patients from lanthanum carbonate to a different phosphate binder prior to radiological examinations. | Radio-opaque appearance of lanthanum carbonate in a patient with chronic renal failure|Nephrology Dialysis Transplantation|Oxford Academic (oup.com) |
| Wu et al. | 2008 | X-ray | Multiple, scattered radiopaque densities. | Intestines | NR | Educating physicians can prevent misinterpretation. | A 56-year-old woman with starry radiopacities|Annals of Saudi Medicine (annsaudimed.net) |
| Badre et al. | 2008 | X-ray | Multiple, scattered radiopaque densities. | Upper left quadrant of abdomen→stomach. | NR | Tablets should be chewed completely prior to swallowing. | Unusual Abdominal Radio-opaque Densities in an ESRD Patient—Badre—2014—Seminars in Dialysis—Wiley Online Library |
| Kato et al. | 2009 | CT | Multiple, scattered radiopaque densities in intestines, and one case of a whole tablet seen in the terminal ileum together with digested residues in colon diverticulum. | Intestines | NR | LC should be used with caution in patients with diverticular flare-ups + in patients who are unable to chew tablets. | Accumulation of lanthanum carbonate in the digestive tracts|SpringerLink |
| Muller et al. | 2009 | X-ray + CT | Multiple, scattered radiopaque densities. | Intestines, especially in the rectosigmoid region. | NR | LC should be used with caution in patients with diverticular flare-ups + in patients who are unable to chew tablets. | confusional state associated with use of lanthanum carbonate in a dialysis patient: a case report|Nephrology Dialysis Transplantation | Oxford Academic (oup.com) |
| Connor et al. | 2009 | X-ray | Multiple, scattered radiopaque densities. | Colon | NR | Clinicians of all backgrounds should be aware of the distinctive radiological appearances seen in patients taking lanthanum carbonate. When possible, alternative phosphate binders should be temporarily employed before radiological examinations. | An unusual abdominal radiograph Postgraduate Medical Journal (bmj.com) |
| Turkmen et al. | 2009 | X-ray | Multiple, scattered radiopaque densities. | Throughout the ascending and transverse colon segments | NR | NR | An unusual hurdle to renal transplantation: speckled abdominal opacities induced by lanthanum carbonate—Turkmen—2010—Internal Medicine Journal—Wiley Online Library |
| Huijisoon et al. | 2009 | X-ray | Multiple, scattered radiopaque densities. | Intestines | Contrast medium (ruled out) | Patients should chew the tablets sufficiently. | Dustri Online Services |
| Hayashi et al. | 2010 | CT | Multiple, hyperdense elements with sharp edges + beam hardening. | Intestines | Foreign bodies | Radiologists should be familiar with the appearance of LC. Temporarily switch to a different phosphate binder before the radiological examination. If CT or X-ray is necessary, perform before administration of LC. | Beam-hardening artifacts on computed tomography images caused by lanthanum carbonate hydrate in a patient on dialysis SpringerLink |
| Chacko et al. | 2010 | X-ray | Multiple, scattered radiopaque densities. | Intestines | Sclerosing peritonitis, tuberculosis, and lead ingestion | Awareness of LCs radiopaque features will prevent unnecessary investigations. | Christmas lights in the gastrointestinal tract The Medical Journal of Australia (mja.com.au) |
| Hofmann et al. | 2010 | X-ray | Multiple, scattered radiopaque densities. | Colon | Oral or rectal contrast medium | NR | Colonic Opacification in a Patient with End-Stage Kidney Disease—Gastroenterology (gastrojournal.org) |
| Schmitt et al. | 2010 | X-ray + CT | Multiple, scattered radiopaque densities. | Intestines | NR | Proposes that Lanthanum should temporarily be discontinued prior to image studies | Layout 1 (nih.gov) |
| Fürstenberg et al. | 2010 | DEXA | Multiple, scattered radiopaque densities. | Intestines | NR | LC opacities in the GI tract can lead to erroneous overestimation of bone mineral content. | Overestimation of Lumbar Spine Calcium with Dual Energy X-Ray Absorptiometry Scanning due to the Prescription of Lanthanum Carbonate in Patients with Chronic Kidney Disease—Abstract—American Journal of Nephrology 2010, Vol. 32, No. 5—Karger Publishers |
| Crush et al. | 2010 | X-ray | Multiple, scattered radiopaque densities. | Colon | Contrast medium (ruled out) | Physicians should be informed about the phenomenon. | Perplexing plain abdominal X-ray Gut (bmj.com) |
| Walsh et al. | 2011 | DEXA | Multiple, scattered radiopaque densities. | Colon | Contrast medium | Lanthanum in the colon falsely increases BMD measurement. Suggests temporarily switching to a different phosphate binder before DXA scan if possible. | ClinicalKey |
| Vila-Navarro et al. | 2012 | X-ray | Multiple, scattered radiopaque densities. | Colon and appendix | Contrast medium (ruled out) | NR | 07_IPD_2384-Vila.ing_Maquetación 1 (grupoaran.com) |
| Muller et al. | 2012 | X-ray + CT | Radiopaque puddle with dilation and fecal impaction. | Stomach | NR | Chewing the tablet is essential. Caution is required if the patient suffers from constipation as he is at risk of developing a fecaloma or encephalopathy if the lanthanum serum content increases and crosses the brain blood barrier. | Radio-opaque fecal impaction and pseudo-occlusion in a dialyzed patient taking lanthanum carbonate—Muller—2012—Hemodialysis International—Wiley Online Library |
| Kuroiwa et al. | 2015 | UL + CT | Hyperecchoic signal in the intestines. | Intestines | NR | Anesthesiologists who perform transesophageal echocardiography and the abdominal US need to be familiar with the characteristics of LCH. | Lanthanum carbonate hydrate causes artifacts on ultrasound (nih.gov) |
| Salerno et al. | 2015 | CT | Multiple, hyperdense elements with sharp edges + beam hardening. | Intestines | Foreign bodies, intestinal bleeding. | One should pay more attention to the patient’s food habits as well as the drugs he is receiving to avoid misinterpretations of the radiological imaging studies. | The Risk of Mistaking Intestinal Lanthanum Carbonate for Intestinal Bleeding on CT (nih.gov) |
| Ruiz-Pardo et al. | 2016 | X-ray | Multiple scattered radiopaque densities. | Intestines | Contrast medium | NR | 10_IPD_3822_Ruiz.Ing.indd (reed.es) |
| Sahbudin et al. | 2016 | DEXA + X-ray | Multiple scattered radiopaque densities. | Intestines | NR | Alternative phosphate binders should be used. | Lanthanum carbonate in chronic renal failure|The BMJ |
| Nishikawa et al. | 2017 | CT | High-density layer around the entire circumference of the stomach wall. | Stomach wall | NR | Clinicians should be aware of this clinical condition as a possible cause of nausea | Lanthanum deposition in the gastric mucosa in a patient undergoing hemodialysis|QJM: An International Journal of Medicine|Oxford Academic (oup.com) |
| Harris et al. | 2017 | X-ray + CT | Multiple, scattered radiopaque densities (X-ray) + attenuation in the bowel wall and scattered opacities in the stomach and intestines (CT). | Intestines | Plebosclerotic colitis, hemorrhage | In Plebosclerotic colitis, it is unusual for the whole colon to be involved. | A case of lanthanum carbonate ingestion thought to be Plebosclerotic colitis on CT imaging and abdominal radiograph—ScienceDirect |
| Paranji et al. | 2017 | X-ray | A radiopaque coin-shaped foreign body. | aerodigestive tract | Foreign object | Tablets should be crushed/chewed sufficiently before swallowing due to the risk of aspiration. | All that glitters is not gold: A case of lanthanum carbonate aspiration—Suchitra Paranji, Neethi Paranji, Adam S Weltz, 2017 (sagepub.com) |
| Shitomi et al. | 2017 | CT | High-attenuating lines in the stomach wall. | Stomach | Non—proven to be lanthanum with biopsies | Coined lanthanum carbonate accumulation in the gastric mucosa “gastric lanthanosis”. The clinical implication is unknown. | Gastric lanthanosis (lanthanum deposition) in dialysis patients treated with lanthanum carbonate—Shitomi—2017—Pathology International—Wiley Online Library |
| Chang et al. | 2018 | X-ray + CT | Multiple, scattered radiopaque densities. | Colon | Barium contrast | Clinicians may take its radiopaque characteristic as an advantage to assess the patient’s drug adherence. | Starry-sky bowels|SpringerLink |
| Fischer et al. | 2019 | X-ray + CT | Multiple, scattered radiopaque densities. | Stomach, small intestines, and rectum. | Foreign bodies | Familiarity with the unique appearance of lanthanum carbonate on imaging can prevent misinterpretation of imaging modalities. | Page loading—ClinicalKey |
| Shiratori et al. | 2019 | CT | Hyperdensity areas in the stomach wall. | Stomach | NR | Esophagogastroduodenoscopy was performed showing white regional lesions due to Lanthanum carbonate deposition. | Lanthanum deposition in the gastric mucosa in a patient treated with hemodialysis BMJ Case Reports |
| Galo et al. | 2019 | UL + X-ray + CT | Multiple, scattered radiopaque densities. | Intestines | Foreign bodies and other drugs that typically cause radiopaque appearance. | The chewable tablets should be fully chewed or crushed prior to ingestion. One should first rule out abdominal diseases before prescribing lanthanum carbonate. Recognition of lanthanum carbonate artifacts can avoid extensive and costly use of medical resources for this benign condition. | Lanthanum-Induced Radiopaque Intestinal Precipitates: A Potential Cause of Intestinal Foreign Bodies (nih.gov) |
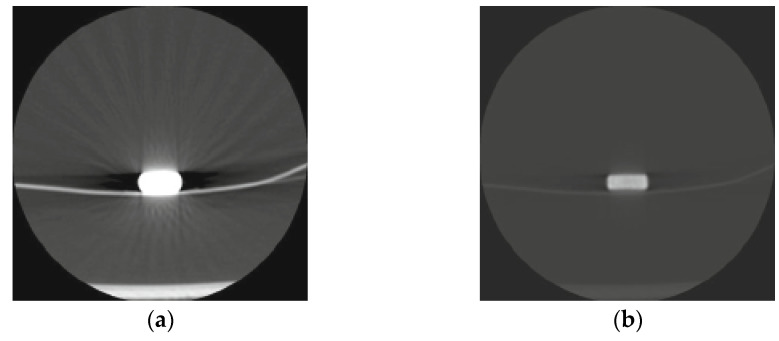
Figure 2.
(a) Visual overview of lanthanum carbonate opacities. Axial CT images of lanthanum carbonate hydrate (Fosrenol chewable tablet) (window level 1500, window width −500) are shown, with a strong artifact due to a beam-hardening effect on the left, and on the right, with a window level of 15,000 and window width of 4000. (b) Beam-hardening artifacts on computed tomography images are also presented, caused by lanthanum carbonate hydrate in a patient on dialysis. Reprinted with permission from ref. [24]. Copyright 2010. Japanese Journal of Radiology.
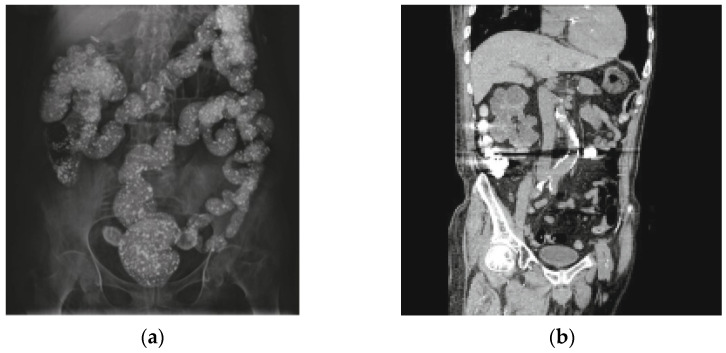
Figure 3.
Plain abdominal radiography in which lanthanum carbonate opacities are observed in the totality of the colonic frame (a). (b) a coronal multiplanar reconstruction computed tomography (CT) image with strong artifacts caused by tablets in the ascending and transverse colon is observed. Lanthanum carbonate has a radiopaque appearance on the plain abdominal radiography. Reprinted with permission from ref. [27]. Copyright 2016 Revista Española Enfermedades.
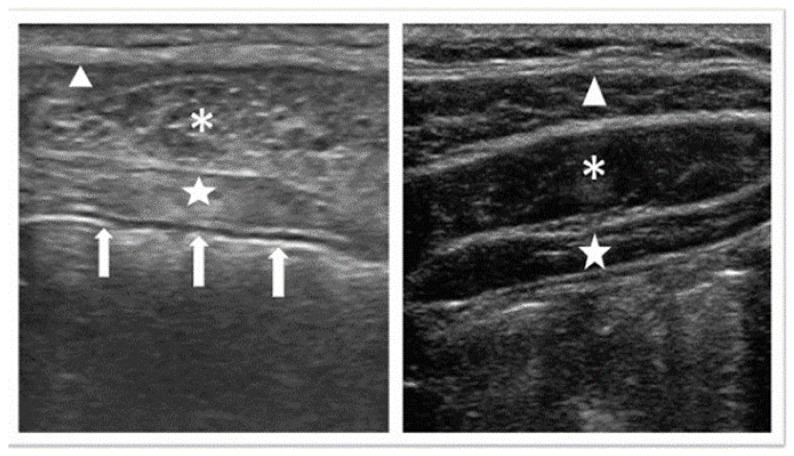
Figure 4.
A comparison of an abdominal ultrasonogram from a patient treated with lanthanum carbonate and that of a healthy man in his 30s is presented. The portion observed as a white line below the transversus abdominis (white arrows) is the wall of the gastrointestinal tract. ∆: External oblique muscle; *: Internal oblique muscle; ☆: Transversus abdominis muscle; Lanthanum carbonate hydrate causes artifacts on ultrasound reprinted with permission from ref [28] under the Creative Commons Attribution 4.0 International License. Copyright Journal of Anesthesia 2015.
Beam-hardening artifacts on computed tomography images are shown, which were caused by lanthanum carbonate hydrate in a patient on dialysis. Reprinted with permission from ref. [24]. Copyright Japanese Journal of Radiology 2010.
4. Discussion
Our review highlights that LC opacities can be seen throughout the gastrointestinal (GI) tract and even in the upper airways. In general X-ray, ultrasound and CT can be affected by LC opacities, but also other image modalities such as dual-emission X-ray absorptiometry (DEXA) scanning [29,30,42] and transesophageal echocardiography [28]. The heterogeneous differential diagnoses can lead to many misinterpretations (Table 4).
Table 4.
Differential diagnosis of lanthanum carbonate opacities.
We did not find any examples of in vivo MRI studies regarding the effect of LC. However, one magnetic resonance imaging (MRI) study performed an in vitro trial with LC in plastic bottles filled with distilled water or edible agar. The study determined that ground LC tablets had no contrast enhancement effect on T1-weighted images; on T2-weighted images, it did not affect the signal intensity of the solvent. However, unground LC tablets may be visualized as filling defects on MRIs [43].
4.1. Fosrenol Administration
Some case reports described the cause of the LC opacities as whole tablets contributing to hoarseness, dysphagia, and fecaloma [4,20,22].
Furthermore, a differential diagnosis of foreign bodies results in suspicion of perforation, obstruction, intussusception, fistula formation, abdominal abscess formation, and death, and therefore, is a medically urgent situation [44]. Patients with chronic kidney disease must be encouraged to chew or crush the LC tablets, switch to Fosrenol powder, or use an alternative phosphate binder. A few studies suggest that LC should be used with caution in diverticulitis patients, as diverticulitis flare-ups may occur if the tablets are not appropriately chewed [4,18]. In particular, 1000 mg LC tablets may cause a problem for the older population, as they are 2.2 cm in diameter [20].
Radio-opacity is not exclusively linked to LC. Other drugs such as chloral hydrate, heavy metals, iodides, phenothiazines, enteric-coated pills, and solvents could also be considered if radiographic opacities are seen in imaging [45].
4.2. Could LC Opacities Have a Hidden Consequence?
Other studies have described the LC deposition in the gastric mucosa during endoscopy examinations as whitish lesions [46]. Shitomi et al. named the phenomenon “gastric lanthanosis” and described the pathology as reflective bright white spots by gastroscopy and eosinophilic histiocytes [41]. Another study described a high-density layer around the entire circumference of the stomach wall. These authors reported reddish-brown deposits phagocytized by macrophages histologically, and X-ray spectroscopy confirmed the presence of lanthanum in the specimen. Iwamuro et al. argued that lanthanum deposition might cause gastric erosions, ulcers, and epigastric discomfort [47]. However, a recent review described the progression and outcome of gastric lanthanosis as unknown [46]. the authors of this review propose an investigation of the clinical importance of gastric lanthanosis as a potential future research field.
The strength of this study lies in the fact that, to our knowledge, this is the first systematic review regarding LC opacities in image studies of chronic kidney disease patients. Our review gives a good overview of the consequences of differential diagnosis of LC opacities.
Nevertheless, our study also has weaknesses. Our review consists almost exclusively of case studies. Due to this feature, we were unable to determine the extent of the problem with LC opacities among patients taking LC. However, producing a visual overview of LC opacities does not require studies with a specific design. Future research might focus on the frequency of LC opacities and the most common locations, as well as the long-term effects of gastric lanthanosis.
5. Conclusions
Our review shows that LC opacities can vary in appearance and have been observed throughout the digestive tract of patients with chronic kidney disease. Unfortunately, the misinterpretation of these radiological opacities results in many different differential diagnoses. Therefore, we recommend that patients treated with LC should switch to an alternative phosphate binder several days prior to image testing, to avoid misinterpretation. In addition, radiologists and clinicians ordering imaging should be familiar with the effect of LC treatment on imaging, to avoid unnecessary diagnostic tests. Other tasks include making sure patients receiving LC are able to chew the tablets and, alternatively, considering a change to LC powder or an alternative phosphate binder. Further studies regarding the long-term effects of gastric lanthanosis could yield important insights.
Acknowledgments
The authors would like to thank Caroline Margaret Moos for proofreading and helping with the literature research.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/diagnostics12020464/s1, Search Strategy.
Author Contributions
Conceptualization, J.K., N.P.H. and A.N.Ø.S.; methodology, J.K., N.P.H. and A.N.Ø.S.; validation, J.K., N.P.H. and A.N.Ø.S.; writing—original draft preparation, A.N.Ø.S., F.B., A.H.B. and J.K.; writing—review and editing, A.N.Ø.S., F.B., A.H.B. and J.K.; supervision, J.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Since this study was a systematic review, no ethical approval was required.
Informed Consent Statement
Not applicable.
Data Availability Statement
Links to the different studies included in the review are listed in Table 3.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Block G.A., Hulbert-Shearon T.E., Levin N.W., Port F.K. Association of serum phosphorus and calcium x phosphate product with mortality risk in chronic hemodialysis patients: A national study. Am. J. Kidney Dis. 1998;31:607–617. doi: 10.1053/ajkd.1998.v31.pm9531176. [DOI] [PubMed] [Google Scholar]
- 2.Ruospo M., Palmer S.C., Natale P., Craig J.C., Vecchio M., Elder G.J., Strippoli G.F. Phosphate binders for preventing and treating chronic kidney disease-mineral and bone disorder (CKD-MBD) Cochrane Database Syst. Rev. 2018;8:CD006023. doi: 10.1002/14651858.CD006023.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tonelli M., Pannu N., Manns B. Oral phosphate binders in patients with kidney failure. N. Engl. J. Med. 2010;362:1312–1324. doi: 10.1056/NEJMra0912522. [DOI] [PubMed] [Google Scholar]
- 4.Kato A., Takita T., Furuhashi M. Accumulation of lanthanum carbonate in the digestive tracts. Clin. Exp. Nephrol. 2010;14:100–101. doi: 10.1007/s10157-009-0240-0. [DOI] [PubMed] [Google Scholar]
- 5.Albaaj F., Hutchison A.J. Lanthanum carbonate (Fosrenol): A novel agent for the treatment of hyperphosphataemia in renal failure and dialysis patients. Int. J. Clin. Pract. 2005;59:1091–1096. doi: 10.1111/j.1368-5031.2005.00592.x. [DOI] [PubMed] [Google Scholar]
- 6.Fosrenol (Lanthanum) [Prescribing Information] Takeda Pharmaceuticals America, Inc.; Lexington, MA, USA: 2020. [Google Scholar]
- 7.Savica V., Calo L.A., Monardo P., Santoro D., Bellinghieri G. Phosphate binders and management of hyperphosphataemia in end-stage renal disease. Nephrol. Dial. Transplant. 2006;21:2065–2068. doi: 10.1093/ndt/gfl289. [DOI] [PubMed] [Google Scholar]
- 8.David S., Kirchhoff T., Haller H., Meier M. Heavy metal–rely on gut feelings: Novel diagnostic approach to test drug compliance in patients with lanthanum intake. Nephrol. Dial. Transplant. 2007;22:2091–2092. doi: 10.1093/ndt/gfm208. [DOI] [PubMed] [Google Scholar]
- 9.Pafcugova J., Horackova M., Hraskova M., Forejt J., Szabo M., Padr R. Radio-opaque appearance of lanthanum carbonate in a patient with chronic renal failure. Nephrol. Dial. Transplant. 2008;23:1776–1777. doi: 10.1093/ndt/gfn015. [DOI] [PubMed] [Google Scholar]
- 10.Chacko Y., Clark C.J. Christmas lights in the gastrointestinal tract. Med. J. Aust. 2010;193:56. doi: 10.5694/j.1326-5377.2010.tb03744.x. [DOI] [PubMed] [Google Scholar]
- 11.Harris K., Balcam S. A case of lanthanum carbonate ingestion thought to be phlebosclerotic colitis on CT imaging and abdominal radiograph. Radiography. 2017;23:e23–e26. doi: 10.1016/j.radi.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Salerno D., Colin P.E., Ernotte C., Dubois B., Meunier P. The Risk of Mistaking Intestinal Lanthanum Carbonate for Intestinal Bleeding on CT. J. Belg. Soc. Radiol. 2015;99:87–88. doi: 10.5334/jbr-btr.852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Turkmen K., Solak Y., Anil M., Polat H., Tonbul H.Z. An unusual hurdle to renal transplantation: Speckled abdominal opacities induced by lanthanum carbonate. Intern. Med. J. 2010;40:e1–e2. doi: 10.1111/j.1445-5994.2010.02369.x. [DOI] [PubMed] [Google Scholar]
- 14.Page M.J., McKenzie J.E., Bossuyt P.M., Boutron I., Hoffmann T.C., Mulrow C.D., Shamseer L., Tetzlaff J.M., Akl E.A., Brennan S.E., et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021;88:105906. doi: 10.1016/j.ijsu.2021.105906. [DOI] [PubMed] [Google Scholar]
- 15.Campbell M., McKenzie J.E., Sowden A., Katikireddi S.V., Brennan S.E., Ellis S., Hartmann-Boyce J., Ryan R., Shepperd S., Thomas J., et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ. 2020;368:l6890. doi: 10.1136/bmj.l6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murad M.H., Sultan S., Haffar S., Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid. Based Med. 2018;23:60–63. doi: 10.1136/bmjebm-2017-110853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu H.C., Lin S.H. A 56-year-old woman with starry radiopacities. Ann. Saudi. Med. 2008;28:469. doi: 10.5144/0256-4947.2008.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muller C., Chantrel F., Faller B. A confusional state associated with use of lanthanum carbonate in a dialysis patient: A case report. Nephrol. Dial. Transplant. 2009;24:3245–3247. doi: 10.1093/ndt/gfp340. [DOI] [PubMed] [Google Scholar]
- 19.Muller C., Muller S., Sissoko A., Klein A., Faller B., Chantrel F. Radio-opaque fecal impaction and pseudo-occlusion in a dialyzed patient taking lanthanum carbonate. Hemodial. Int. 2012;16:556–558. doi: 10.1111/j.1542-4758.2011.00647.x. [DOI] [PubMed] [Google Scholar]
- 20.Paranji S., Paranji N., Weltz A.S. All that glitters is not gold: A case of lanthanum carbonate aspiration. SAGE Open Med. Case Rep. 2017;5:2050313X17712642. doi: 10.1177/2050313X17712642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fischer M., Shavit M.M., Gork I. An incidental finding of metallic objects in a patient with chronic renal failure. Eur. J. Intern. Med. 2019;65:e3–e4. doi: 10.1016/j.ejim.2019.03.007. [DOI] [PubMed] [Google Scholar]
- 22.Singanamala S., Roer D.A., Perazella M.A. An unexpected finding on chest roentgenogram following hemodialysis catheter placement. Semin Dial. 2008;21:293–294. doi: 10.1111/j.1525-139X.2007.00395.x. [DOI] [PubMed] [Google Scholar]
- 23.Connor A., Taylor J.E. An unusual abdominal radiograph. Postgrad Med. J. 2009;85:68. doi: 10.1136/pgmj.2008.073890. [DOI] [PubMed] [Google Scholar]
- 24.Hayashi H., Machida M., Sekine T., Yamaguchi H., Kiriyama T., Kumita S. Beam-hardening artifacts on computed tomography images caused by lanthanum carbonate hydrate in a patient on dialysis. Jpn J. Radiol. 2010;28:322–324. doi: 10.1007/s11604-010-0426-0. [DOI] [PubMed] [Google Scholar]
- 25.Hofmann U., Beer M. Colonic opacification in a patient with end-stage kidney disease. Gastroenterology. 2010;139:e8–e9. doi: 10.1053/j.gastro.2009.10.066. [DOI] [PubMed] [Google Scholar]
- 26.Schmitt R., Haller H., Lotz J. Intestinal radiopacities in chronic renal failure. CMAJ. 2010;182:E856. doi: 10.1503/cmaj.091935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ruiz Pardo J., Ibanez Canovas N., Abrisqueta Carrion J., Lujan Mompean J.A., Parrilla Paricio P. Lanthanum carbonate has a radiopaque appearance on the plain abdominal radiography. Rev. Esp. Enferm. Dig. 2016;108:365–366. [PubMed] [Google Scholar]
- 28.Kuroiwa K.K., Nakazawa M., Nishizawa M. Lanthanum carbonate hydrate causes artifacts on ultrasound. J. Anesth. 2015;29:974. doi: 10.1007/s00540-015-2034-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sahbudin I. Lanthanum carbonate in chronic renal failure. BMJ. 2016;2016:352. doi: 10.1136/bmj.i158. [DOI] [Google Scholar]
- 30.Walsh J.P., Lteif A.A. Lanthanum carbonate interference with lumbar spine DXA. J. Clin. Densitom. 2011;14:499–501. doi: 10.1016/j.jocd.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 31.Shiratori Y., Oguri N. Lanthanum deposition in the gastric mucosa in a patient treated with haemodialysis. BMJ Case Rep. 2019;12 doi: 10.1136/bcr-2019-230550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nishikawa Y., Yokoi H., Sakurai T., Horimatsu T., Miyamoto S. Lanthanum deposition in the gastric mucosa in a patient undergoing hemodialysis. QJM. 2018;111:347–348. doi: 10.1093/qjmed/hcx250. [DOI] [PubMed] [Google Scholar]
- 33.Galo J., Madrid B., Kupin W. Lanthanum-Induced Radiopaque Intestinal Precipitates: A Potential Cause of Intestinal Foreign Bodies. Case Rep. Nephrol. 2019;2019:1298674. doi: 10.1155/2019/1298674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Crush L., O’Connor O.J., Plant W., Clarkson M.R., Shanahan F., Maher M.M. Perplexing plain abdominal x-ray. Radiographic opacities were due to the lanthanum. Gut. 2011;60:218–254. doi: 10.1136/gut.2010.215822. [DOI] [PubMed] [Google Scholar]
- 35.Huijssoon M., Ipema K., Franssen C.F. Pie-shaped corpora aliena in a dialysis patient. Clin. Nephrol. 2009;72:422. doi: 10.5414/CNP72422. [DOI] [PubMed] [Google Scholar]
- 36.Cerny S., Kunzendorf U. Images in clinical medicine. Radiographic appearance of lanthanum. N. Engl. J. Med. 2006;355:1160. doi: 10.1056/NEJMicm050535. [DOI] [PubMed] [Google Scholar]
- 37.Chang F.M., Tarng D.C., Yang C.Y. Starry-sky bowels. Int. J. Colorectal. Dis. 2018;33:1807–1808. doi: 10.1007/s00384-018-3173-9. [DOI] [PubMed] [Google Scholar]
- 38.Chuang C.L., Chiou S.Y., Li S.Y., Jian D.Y., Chen J.Y. The case: A peritoneal dialysis patient with an unusual abdominal film. Treatment with lanthanum carbonate. Kidney Int. 2007;72:1291–1292. doi: 10.1038/sj.ki.5002413. [DOI] [PubMed] [Google Scholar]
- 39.Vila-Navarro S., Gomila-Roy G.E., Hemfelt-Minobis A., Khorrami-Minaei S., Ginard-Vicens D. Unusual image of lanthanum carbonate in the abdominal radiograph. Rev. Esp. Enferm. Dig. 2012;104:379–380. doi: 10.4321/S1130-01082012000700007. [DOI] [PubMed] [Google Scholar]
- 40.Badre P., Raissi S. Unusual abdominal radio-opaque densities in an ESRD patient. Semin. Dial. 2014;27:E55–E56. doi: 10.1111/j.1525-139X.2008.00469.x. [DOI] [PubMed] [Google Scholar]
- 41.Shitomi Y., Nishida H., Kusaba T., Daa T., Yano S., Arakane M., Kondo Y., Nagai T., Abe T., Gamachi A., et al. Gastric lanthanosis (lanthanum deposition) in dialysis patients treated with lanthanum carbonate. Pathol. Int. 2017;67:389–397. doi: 10.1111/pin.12558. [DOI] [PubMed] [Google Scholar]
- 42.Furstenberg A., Buscombe J., Davenport A. Overestimation of lumbar spine calcium with dual energy X-ray absorptiometry scanning due to the prescription of lanthanum carbonate in patients with chronic kidney disease. Am. J. Nephrol. 2010;32:425–431. doi: 10.1159/000320481. [DOI] [PubMed] [Google Scholar]
- 43.Nakamura S., Awai K., Komi M., Morita K., Namimoto T., Yanaga Y., Utsunomiya D., Date S., Yamashita Y. Signal intensity of lanthanum carbonate on magnetic resonance images: Phantom study. Jpn J. Radiol. 2011;29:366–370. doi: 10.1007/s11604-010-0557-3. [DOI] [PubMed] [Google Scholar]
- 44.Hunter T.B., Taljanovic M.S. Foreign bodies. Radiographics. 2003;23:731–757. doi: 10.1148/rg.233025137. [DOI] [PubMed] [Google Scholar]
- 45.Spiegel S.M., Hyams B.B. Radiographic demonstration of a toxic agent. J. Can. Assoc. Radiol. 1984;35:204–205. [PubMed] [Google Scholar]
- 46.Iwamuro M., Urata H., Tanaka T., Okada H. Review of the diagnosis of gastrointestinal lanthanum deposition. World J. Gastroenterol. 2020;26:1439–1449. doi: 10.3748/wjg.v26.i13.1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iwamuro M., Urata H., Tanaka T., Ando A., Nada T., Kimura K., Yamauchi K., Kusumoto C., Otsuka F., Okada H. Lanthanum Deposition in the Stomach: Usefulness of Scanning Electron Microscopy for Its Detection. Acta Med. Okayama. 2017;71:73–78. doi: 10.18926/AMO/54828. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Links to the different studies included in the review are listed in Table 3.