Abstract
Heat kills more Australians than any other natural disaster. Previous Australian research has identified increases in Emergency Department presentations in capital cities; however, little research has examined the effects of heat in rural/regional locations. This retrospective cohort study aimed to determine if Emergency Department (ED) presentations across the south-west region of Victoria, Australia, increased on high-heat days (1 February 2017 to 31 January 2020) using the Rural Acute Hospital Data Register (RAHDaR). The study also explored differences in presentations between farming towns and non-farming towns. High-heat days were defined as days over the 95th temperature percentile. International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM) codes associated with heat-related illness were identified from previous studies. As the region has a large agricultural sector, a framework was developed to identify towns estimated to have 70% or more of the population involved in farming. Overall, there were 61,631 presentations from individuals residing in the nine Local Government Areas. Of these presentations, 3064 (5.0%) were on days of high-heat, and 58,567 (95.0%) were of days of non-high-heat. Unlike previous metropolitan studies, ED presentations in rural south-west Victoria decrease on high-heat days. This decrease was more prominent in the farming cohort; a potential explanation for this may be behavioural adaption.
Keywords: occupational health, farmers, extreme heat, heat-related illness, high-heat climate change, injury, heat exposure
1. Introduction
The climate is changing, and it is predicted that extreme weather will be more frequent and intense [1]. Globally, the most recent five years have been the warmest on record. Internationally, research has shown an increase in illness, hospitalisations, and deaths during extreme weather events/days [2,3,4]. In Australia, 2019 was both the warmest and driest year on record [5].
Heat kills more Australians than any other natural disaster; between 1900 and 2011, extreme heat accounted for 55% (4555 deaths) of the total number of deaths due to natural hazards [6]. Heat-related illness occurs from combined environmental exposure, metabolic demands, and restricted cooling mechanisms, consequently causing the body to be unable to disperse heat adequately, resulting in thermoregulatory dysfunction [7]. According to Gauer and Meyers [7], an increase of approximately two degrees in core body temperature leads to heat-related illness which can vary in nature, from mild illness such as heat-rash, cramps, and heat exhaustion, through to heatstroke and death [7]. Strenuous exercise, poor physical fitness, exposure to high temperatures and humidity, lack of acclimatisation, dehydration, chronic disease, excessive clothing, and wearing protective equipment are all identified risk factors [8].
Research conducted in metropolitan areas of Australia have investigated the effects of exposure to high-heat days and high-heat events on human health. Similarly to international studies, reports showed increased ambulance call-outs and subsequent hospital admissions for heat-related conditions, including kidney disease, deterioration in mental health, heat-related injuries (such as sunburn and heat exhaustion), asthma, and heart disease [9,10,11,12,13]. Toloo, Yu, Aitken, FitzGerald, and Tong [12] concluded that as heat increased, the likelihood of attendance to Emergency Departments by all genders and age groups increased, with those presenting being more unwell. In Victoria, Australia, the 2009 heatwave saw a 12% increase in overall Emergency Department presentations, and 374 more deaths than expected for that time of the year [14].
The working environment has been identified as a key determinant in contributing to heat-related illness [4,12,15]. By exploring heat-related mortality and morbidity in outdoor workers in Los Angeles County, researchers from the Labour Occupational Safety and Health Program [4] concluded there was a strong association between the proportion of residents working in outdoor industries and rates of Emergency Department presentations during heat events. Additionally, there have been recent calls for the United States Occupational Safety and Health Association (OSHA) to issue federal heat standards that include water, shade, and rest breaks for farm workers [16]. In Victoria, Australia, there is no maximum temperature set under the Occupational Health and Safety Act 2004 or Occupational Health and Safety Regulations 2017 for a worker to stop working. Although, some workplace agreements cite 35 °C, where employers are required to consult with the union to minimise heat risks, and decide whether workers can continue to work safely [17]. Similarly, Bi, Williams, Loughnan, Lloyd, Hansen, Kjellstrom, Dear, and Saniotis [15] investigated the effects of extreme heat on health in Australia, and highlighted occupational heat stroke (heat stroke due to work) as an area for concern.
Globally, agricultural workers have been identified as a high-risk group for suffering heat-related illness, and climate change will further increase this vulnerability [18]. Despite some coroner cases reporting deaths of agricultural workers (17 cases between 2000–2015), and data from Safe Work Australia [19] reporting 1174 (2009/10 to 2018/19) workers’ compensation claims from working in the heat, this has not been fully investigated in Australia.
Additionally, Australian heat-related illness research has largely focused on metropolitan populations [15], despite mining, agriculture, construction, and emergency services, largely non-metropolitan occupations, having been identified as high-risk occupations for heat strain. There is also limited female data available for Australian occupational heat stress settings. This may in part be due to the industry (agriculture, mining, and construction) being male-dominated; however, according to Jay and Brotherhood [20], this disparity between male and female data far exceeds the ratio of males to females in these sectors.
Therefore, the aim of this study was to determine and understand the prevalence and characteristics of heat-related illness in rural south-west Victoria (an agriculturally-based region) using the Rural Acute Hospital Data Registers (RAHDaR) from 1 February 2017 to 31 January 2020 between the warmer months of November and March, inclusive. It also aims to compare frequencies of Emergency Department presentations of individuals from farming towns and non-farming towns in rural south-west Victoria. The results from this study will assist in understanding the effects of high-heat days on the volume and types of Emergency Department attendances in rural/regional Australia. It also supports the importance of developing localised public health responses to high-heat days/events, whether in regional/rural Australia or internationally.
2. Materials and Methods
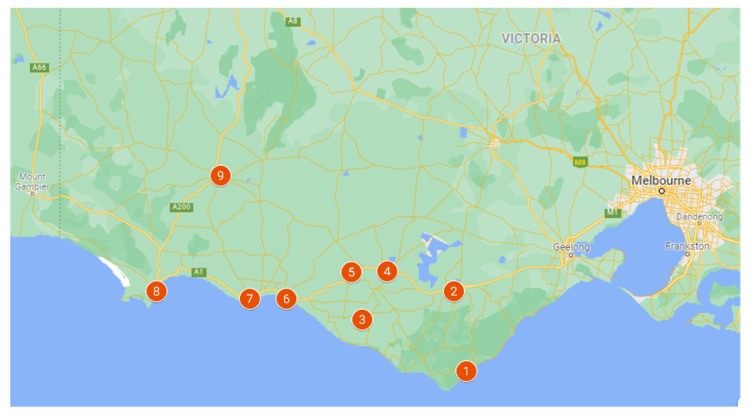
This was a cohort retrospective study utilising the Rural Acute Hospital Data Register (RAHDaR). The RAHDaR database collates detailed data on all presentations to the Emergency Department from every emergency care facility in south-west Victoria [21] (Figure 1); this is inclusive of very small rural facilities which run Urgent Care Centres (UCC). UCCs provide first-line emergency care; they can perform emergency resuscitation, stabilisation, and preparation of patient transfers to facilities that provide higher levels of care [22,23,24]. Though the Victorian Emergency Minimum Dataset (VEMD) includes mandatory-reported emergency presentations from larger Emergency Departments, RAHDaR also captures presentations at the lower-resourced south-west Victorian sites, such as the UCCs, and highlights as much as a 35% deficit in the data currently available via the government-reported dataset [25,26]. All data utilised in RAHDaR is Victorian Emergency Minimum Dataset (VEMD) and VEMD-equivalent data, and uses the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM) [27]. The data are collected for epidemiological purposes, health service planning and coordination, policy assessment and formulation, clinical research and quality improvement, and patient management [21].
Figure 1.
Map of the nine south-west Victorian hospitals (1. Otway Health; 2. Colac Area Health; 3. Timboon and District Healthcare Service; 4. South West Healthcare Camperdown; 5. Terang and Mortlake Health Service; 6. South West Healthcare Warrnambool; 7. Moyne Health Service; 8. Portland District Health; 9. Western District Health Service).
As this study aimed to investigate the prevalence and characteristics of heat-related illness, only the warmer months during the study period (1 February 2017 to 31 January 2020) were utilised.
Ethics approval was sought from the South West Healthcare Human Research Ethics Committee (Ref: 2019 31) and Deakin University Human Research Ethics Committee (Ref: 2020-004).
2.1. Weather Data—Identification of Days of High-Heat
There are no Australian or internationally agreed upon definitions of a high-heat day. Previous literature was explored to determine the best method to be used in this study. Days over the 95th and 99th temperature percentiles were identified. During data analysis, it was determined there were not enough days/presentations on days over the 99th percentile for it to be significant. Therefore, all days over the 95th temperature percentile were identified as days of high-heat, and in line with other research [12,28,29].
The weather stations closest to each of the nine acute hospitals were identified. Maximum daily temperature (highest temperature (°C) recorded in the 24 h to 9 a.m.) data were downloaded into Microsoft Excel (Microsoft, Washington, DC, USA) [30] from each weather station using the Bureau of Meteorology’s ‘Weather Station Directory’ [31]. All irrelevant data (colder months) were removed, with the months of interest remaining. The temperature percentiles were calculated using the days of the study period (November to March). Due to the varying climates between hospital locations and potential acclimitisation, the 95th temperature percentiles were calculated for each hospital. Table 1 shows the temperature cut-off points for each hospital. Days above these temperature cut-offs were classified as high-heat days, and the remaining days were categorised as days of non-high-heat.
Table 1.
Hospital 95th percentile temperature cut-off points (°C).
| Victorian Bureau of Meteorology Weather Station | Acute Hospital | Temperature Cut-off Point (95th Temperature Percentile) |
|---|---|---|
| Cape Otway Lighthouse | Otway Health | 33.2 °C |
| Mortlake Racecourse | Timboon and District Health Service Terang and Mortlake Health Service South West Healthcare—Camperdown |
36.5 °C |
| Warrnambool Airport | South West Healthcare—Warrnambool | 34.1 °C |
| Mount Gellibrand | Colac Area Health | 36.7 °C |
| Portland Cashmore Airport | Portland District Health | 33.0 °C |
| Hamilton Airport | Western District Health Service—Hamilton | 36.8 °C |
| Port Fairy | Moyne Health Service | 34.4 °C |
2.2. ICD-10-AM Codes
Although there are specific ICD-10-AM heat-related codes (T67.0 heatstroke and sunstroke, and T67.1 heat syncope), previous literature has highlighted that heat precipitates a large number of other conditions, resulting in heat-related codes rarely being used [27]. Diagnosis coding used in previous literature examining heat-related illness was reviewed. Many of these studies utilised diagnostic blocks (code groups) rather than specific diagnoses to identify heat-related illness; however, this may result in the over-identification of conditions included as heat-related [3,4,9,10,11,12,32,33,34]. In order to increase the accuracy, ICD-10-AM codes from within previously identified diagnostic blocks [3,4,9,10,11,12,32,33,34] were rated independently for relevance by two investigators, both experienced clinicians. These clinicians work within different areas of the rural healthcare system, and have different clinical backgrounds, minimising the potential for study bias in their code selection. All codes identified were compared, and any discrepancies were discussed (Table 2).
Table 2.
Number of ICD-10-AM codes included under each Major Diagnostic Block.
| Major Diagnostic Block | Number of Included Diagnoses |
|---|---|
| Injury, single site, major | 186 |
| Circulatory system illness | 46 |
| Alcohol/drug abuse and alcohol-/drug-induced mental disorders | 36 |
| Poisoning | 30 |
| Respiratory system illness | 28 |
| Injury, single site, minor | 28 |
| Psychiatric illness | 26 |
| Urological system illness | 19 |
| Illness of the ear, nose, and throat | 19 |
| Neurological system illness | 17 |
| Endocrine, nutritional, and metabolic system illness | 14 |
| Other presentation (not listed elsewhere) | 11 |
| Injury, multiple sites | 11 |
| Allergy | 9 |
| System infection/parasites | 4 |
| Blood/immune system illness | 3 |
| Illness of skin, subcutaneous tissue, breast | 2 |
| Musculoskeletal/connective tissue system illness | 2 |
| Hepatobiliary system illness | 2 |
| Digestive system illness | 1 |
| Grand Total | 494 |
In broad terms, the identified ICD-10-AM codes belonged to the following Major Diagnostic Blocks (code groups):
Any presentation with a diagnosis recorded as one of the 494 identified as heat-related were included in the study.
2.3. Farming and Non-Farming Town
The south-west region of Victoria is located in the south-west corner of the state, and adjoins the South Australian border (see Figure 1). The region comprises the six local government areas of Colac Otway, Corangamite, Glenelg, Moyne, Southern Grampians, and Warrnambool, part of Surf Coast; and the centres of Colac, Hamilton, and Warrnambool. The region covers a total area of around 26,380 square kilometres or 11.6 per cent of Victoria’s total area [35,36]. Australian Bureau of Statistics (ABS) data indicate that in 2018–2019, there were 3554 farms in the Warrnambool and the south-west region, made up of dairy, beef and sheep grazing, and cropping. Agriculture, forestry, and fishing was the largest employment sector with 18,000 people, representing 28% of the region’s workforce.
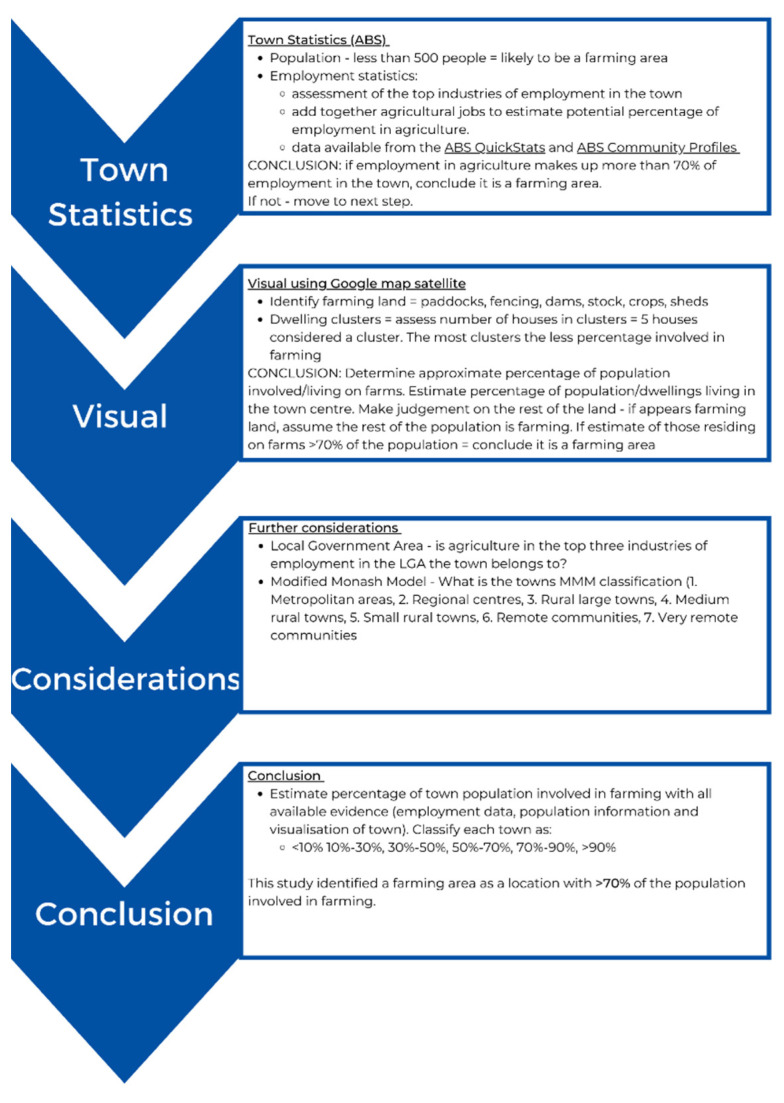
As RAHDaR does not collect employment details, it was determined that the most appropriate method to identify farmers was through town of residence. No previous work has identified towns with a high population percentage involved in agriculture. The Modified Monash Model is used to define a location as a city, rural, remote, or very remote in relation to their access to healthcare services [37]. Rural towns are identified as having a Modified Monash Model classification of MM3 or above. The classifications in this model are determined by a town’s population and distance to services, for example, a location is described as a MM3 if it is within 15 km road distance of a town with a population between 15,000 and 50,000 [37]. However, this model does not accurately identify whether a location is likely to have a large proportion of farming residents. For example, Apollo Bay is identified as MM5; however, agriculture is not identified in the top five industries of employed persons, with the top five industries making up 40% of those employed in Apollo Bay. Therefore, it cannot be assumed that towns identified as ‘rural towns’ by the Modified Monash Model are associated with agriculture.
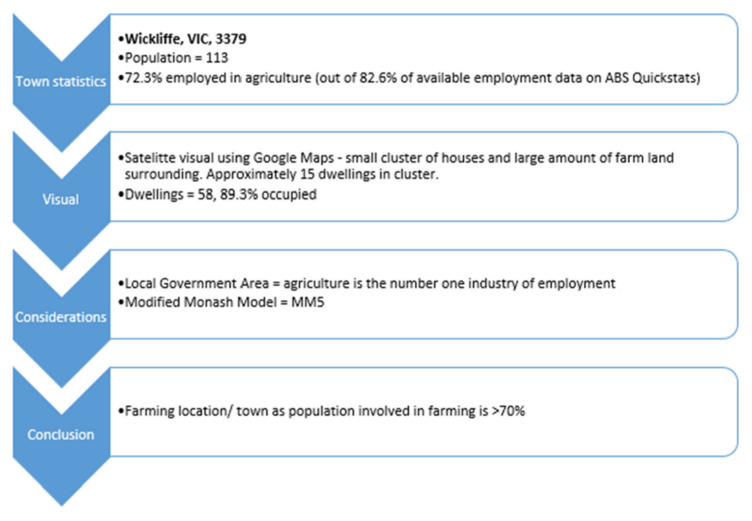
Consequently, a framework was developed to assist in identifying towns with the majority of the population involved in agriculture (Appendix A). It takes into consideration multiple factors when estimating the percentage of involvement in agriculture of a town’s population, including town population and main industries of employment as reported by the Australian Bureau of Statistics [38], and digital visualisation of the town to assess the presence of typical farming characteristics (and the assessment of clusters of houses) by researchers [39]. The Local Government Area top industries of employment and a town’s Modified Monash Model classification were also considered [36,38]. In this study, an area/town was classified as ‘farming’ if it was estimated that over 70% of the population were involved in agriculture.
The framework to identify farming towns underwent inter-rater reliability testing [40]. Three independent researchers estimated the percentage of those involved in farming in a sample of 110 towns using the framework as a guideline. Their estimations were compared to the original town classifications, and the calculated agreement was over 90%. This ensured reliability of the procedure. See Figure 2 as an example of using the decision framework.
Figure 2.
Example of using the farming framework for the location of Wickliffe to classify farming/non-farming locations [36,37,39,41].
2.4. Data Extraction and Analysis
After identification of all the high-heat days during the study period, ICD-10 AM codes (related to heat-related illness) and farming towns were identified, and the relevant data were extracted from the RAHDaR database into a Microsoft Excel file. The Statistical Package for the Social Sciences (SPSS) version 27 (IBM, New York, NY, USA) was then used for data analysis [42]. Descriptive statistics (frequencies, percentages) were calculated to identify differences in presentations in extreme heat days and non-extreme heat days, as well as between the farming and non-farming populations. A logistic regression was computed using weighted data adjusting for age, gender, Modified Monash Model, and the Index of Socio-economic Advantage and Disadvantage to test statistical significance. Weighting was applied according to each LGA’s sex, age, and employment in agriculture statistics to ensure results were representative of the cohorts’ demographics. The rate of presentations per day was calculated using the average number of high-heat days (n = 23.8) and non-high-heat days (n = 429.4 days), and dividing it by total numbers of presentations.
A logistic regression of the binary response variable of hospital presentations due to injury on the binary high-heat days independent variable with a sample size of 15,776 presentations achieves 90% power at a 0.05 significance level to detect a minimum odds ratio of 1.45.
3. Results
Overall, there were 76,457 presentations to the nine Emergency Departments (ED) and Urgent Care Centres in south-west Victoria during the 453 study days. A total of 3844 (5%) presented on days over the 95th temperature percentiles (as outlined in the Section 2), and 72,613 (95%) on days not classified as high-heat. A total of 19.4% (14,826) of the presentations belonged to individuals not residing in the nine Local Government Areas of south-west Victoria, and were removed from further analysis; therefore, the total number of presentations analysed was 61,631.
Total populations for the farming and non-farming cohorts were calculated. The total population of the farming town cohort (of towns with approximately over 70% of the population involved in farming) was estimated to be 15,890 people, whereas the non-farming town population was 171,180 [38], resulting in a total target population for the study of 187,070.
Table 3 shows the top six Major Diagnostic Blocks presenting to the Emergency Department during the study period. Injuries were the most common type of presentation in all groups. However, on high-heat days, there was a drop in the rate per day of injury. Though injuries decreased in both the farming and non-farming groups, the percentage difference was substantially greater in the farming population (41% vs. 25%). Additionally, musculoskeletal/connective tissue system illness also decreased in farmers on high-heat days (−40%). The results suggest that the rate of farmers presenting to the Emergency Department on high-heat days was lower for injuries (−41%), digestive system illness (−6%), musculoskeletal/connective tissue system illness (−40%), neurological system illness (−28%), and ‘other’ presentations (−16%) when compared to non-high-heat days. Conversely, circulatory system illness (+5%) and respiratory system illness (+12%) increased on days of high-heat in the farming cohort. In the non-farming group, the rate of presentations also increased for circulatory system illness (+8%) and ‘other’ presentations, which include alcohol and drug abuse (+2%), on high-heat days. Overall, total farmer presentations decreased by 21%, and non-farmers by 6.5%.
Table 3.
Major Diagnostic Blocks presenting to the Emergency Department on high/non-high-heat days in farming and non-farming areas.
| Major Diagnostic Blocks | Overall Presentations | Farming Areas | Non-Farming Areas | ||||||
|---|---|---|---|---|---|---|---|---|---|
| High-Heat Days n (Rate per Day) |
Non-High-Heat Days n (Rate per Day) |
Difference per Day | % Difference on High-Heat Days (Rounded) | High-Heat Days n (Rate per Day) |
Non-High-Heat Days n (Rate per Day) | Difference per Day | % Difference on High-Heat Days (Rounded) |
||
| Injury (multiple sites, single site major, single site minor) | 15,776 | 41 (1.72) | 1251 (2.91) | −1.2 | −41% | 579 (24.33) | 13,905 (32.38) | −8.05 | −25% |
| Digestive system illness |
6630 | 24 (1.01) | 459 (1.07) | −0.06 | −6% | 305 (12.82) | 5842 (13.61) | −0.79 | −6% |
| Circulatory system illness | 5051 | 16 (0.67) | 274 (0.64) | 0.03 | 5% | 268 (11.26) | 4493 (10.46) | 0.80 | 8% |
| Respiratory system illness | 3877 | 17 (0.71) | 274 (0.64) | 0.08 | 12% | 187 (7.86) | 3399 (7.92) | −0.06 | −1% |
| Musculoskeletal/connective tissue system illness | 3215 | 7 (0.29) | 212 (0.49) | −0.20 | −40% | 150 (6.30) | 2846 (6.63) | −0.33 | −5% |
| Neurological system illness | 3089 | 8 (0.34) | 201 (0.47) | −0.13 | −28% | 149 (6.26) | 2731 (6.36) | −0.10 | −2% |
| Other (alcohol/drug abuse and alcohol-/drug-induced mental disorders; allergy; blood/immune system illness; endocrine, nutritional, and metabolic system illness; gynaecological illness; hepatobiliary system illness; illness of other and unknown symptoms; illness of the eyes; injury, multiple sites; male reproductive system illness; newborn/neonate illness; obstetric illness; poisoning; psychiatric illness; social problem; other presentation *) | 20,780 | 71 (2.98) | 1528 (3.56) | −0.58 | −16% | 1024 (43.03) | 18,157 (42.28) | 0.74 | 2% |
| Total | 58,418 | 184 (7.73) | 4199 (9.78) | −2.05 | −21% | 2662 (111.85) | 51,373 (119.64) | −7.79 | −7% |
* Other presentations, n = 5708; missing cases, n = 3213. The rate per day was calculated using the average number of days of high-heat (n = 23.8 days) and non-high-heat days (n = 429.4 days).
Table 4 demonstrates the characteristics of presentations to the south-west Victorian EDs on high and non-high-heat days between farmers and non-farmers. The average age of presentations was 42.3 years (±26.6). The farming cohort was slightly younger than the individuals presenting from non-farming areas. This difference in attendance was statistically significant on both days of high-heat (p = 0.025) and non-high-heat (p < 0.001). Overall, more females (n = 31,618, 51.3%) presented to ED than males (n = 30,013, 48.7%). However, there were more males (n = 2370, 52.2%) from farming areas presenting to ED than females from farming areas (n = 2170, 47.8%). On days of non-high-heat, there was a statistically significant difference (p < 0.001) between farmers and non-farmers and the gender presenting to ED. Farming males had higher presentations on days of high-heat (55.3%), whereas presentations of farming females were higher on non-high-heat days (47.9%). There was a statistically significant difference between MMM rankings between farmers and non-farmers on both high-heat (p < 0.001) and non-high-heat days (p < 0.001). Farming areas had a lower proportion of presentations from Modified Monash Model (MMM) 4 on high-heat and non-high-heat days, with the large majority of presentations from farming areas classified as MMM5. Similarly, the difference between farmers and non-farmers on high (p < 0.001) and non-high-heat days (p < 0.001) in the Index of Relative Socio-economic Advantage and Disadvantage (ISRAD) was significant. Presentations from non-farming areas were more likely to be associated with lower deciles of the ISRAD index, meaning higher socio-economic disadvantage, whereas farming presentations were mainly from middle ISRAD deciles.
Table 4.
Characteristics of presentations to the Emergency Departments across the south-west.
| Characteristics of ED Presentations | Overall | Days of Extreme Heat | Days of Non-Extreme Heat | ||||||
|---|---|---|---|---|---|---|---|---|---|
| N (%) | Farming Areas n (%) |
Non-Farming Areas n (%) |
DF | Sig (p-Value) |
Farming Areas n (%) |
Non-Farming Areas n (%) |
DF | Sig (p-Value) |
|
| Age | |||||||||
| Mean (years) | 42.3 | 39.4 | 43.7 | 1 | 0.025 | 38.6 | 42.6 | 1 | <0.001 |
| Gender | |||||||||
| Male | 30,013 (48.7%) | 110 (55.3%) | 1399 (48.8%) | 1 | 0.79 | 2260 (52.1%) | 26,244 (48.4%) | 1 | <0.001 |
| Female | 31,618 (51.3%) | 89 (44.7%) | 1466 (51.2%) | 2081 (47.9%) | 27,982 (51.6%) | ||||
| Arrival Transport Mode * | 1 | 0.020 | 1 | <0.001 | |||||
| Ambulance Service (Air Ambulance, Ambulance Service, Helicopter, Road Ambulance, police vehicle) | 10,543 (17.1%) | 24 (12.3%) | 540 (19.1%) | 536 (12.4%) | 9443 (17.5%) | ||||
| Other (Private car, community/public transport/voluntary drivers) | 50,792 (82.4%) | 171 (87.7%) | 2293 (80.9%) | 3372 (87.6%) | 44,556 (82.5%) | ||||
| Triage Category ** | 3 | 0.033 | 3 | <0.001 | |||||
| Resuscitation and Emergency | 5681 (9.2%) | 20 (10.0%) | 283 (9.9%) | 374 (8.6%) | 5004 (9.2%) | ||||
| Urgent | 19,689 (31.9%) | 61 (30.8%) | 1008 (35.2%) | 1244 (28.7%) | 17,376 (32.1%) | ||||
| Semi Urgent | 27,651 (44.9%) | 79 (39.9%) | 1224 (42.8%) | 1966 (45.3%) | 24,382 (45.0%) | ||||
| Non-Urgent | 8589 (13.9%) | 38 (19.2%) | 345 (12.1%) | 756 (17.4%) | 7450 (13.7%) | ||||
| Departure Status *** | 2 | 0.661 | 2 | <0.001 | |||||
| Admitted | 15,754 (25.7%) | 58 (29.9%) | 759 (26.9%) | 1052 (24.4%) | 13,885 (25.7%) | ||||
| Discharged home | 41,487 (67.7%) | 120 (61.9%) | 1818 (64.3%) | 3059 (71.0%) | 36,490 (67.6%) | ||||
| Left at own risk/after clinical advice | 3981 (6.5%) | 16 (8.2%) | 245 (8.7%) | 192 (4.5%) | 3528 (6.5%) | ||||
| Modified Monash Model | 1 | <0.001 | 1 | <0.001 | |||||
| MMM4 or less | 40,412 (65.6%) | 13 (6.5%) | 2037 (71.1%) | 222 (5.1%) | 38,140 (70.3%) | ||||
| MMM5 | 21,219 (34.4%) | 186 (93.5%) | 828 (28.9%) | 4119 (94.9%) | 16,086 (29.7%) | ||||
| Index of Relative Socio-economic Advantage and Disadvantage (ISRAD) | 1 | <0.001 | 1 | <0.001 | |||||
| 2–4 | 46,864 (76.0%) | 64 (32.2%) | 2306 (80.5%) | 1329 (30.6%) | 43,165 (79.6%) | ||||
| 5–7 | 12,730 (20.7%) | 124 (62.3%) | 468 (16.3%) | 2693 (62.0%) | 9445 (17.4%) | ||||
| 8–10 | 2037 (3.3%) | 11 (5.5%) | 91 (3.2%) | 319 (7.3%) | 1616 (3.0%) | ||||
* ‘Undertaker’ (n = 3) presentations removed. ‘Police vehicle’ (n = 252) in ambulance service, as these are typically mental health or intoxicated patients. Missing cases, n = 293; ** Missing cases, n = 21; *** Correctional/custodial facility (n = 45), dead on arrival (n = 8), and died within ED (n = 17) removed as numbers too low.
The majority of presentations arrived at Emergency Departments via a transport mode classified as ‘other’ (82.4%, n = 50,792), which includes private car or community/public transport/voluntary drivers, whereas 17.1% (n = 10,543) arrived in an ambulance service. There was a statistically significant difference between the arrival transport mode of farmers and non-farmers on both days of high-heat (p = 0.020) and non-high-heat days (p < 0.001), with the large majority of farmers arriving using ‘other’ transport modes. Most presentations were classified as ‘urgent’ (n = 19,689, 31.9%) and ‘semi urgent’ (n = 27,651, 44.9%). There was a statistically significant difference on both days of high- (p = 0.033) and non-high-heat (p < 0.001) between farmers and non-farmers and triage category. ‘Urgent’ presentations (Australian Triage Category 1–3) were higher in the non-farming areas on days of high-heat and non-high-heat, whereas ‘non-urgent’ presentations (Australian Triage Category 4–5) were higher in the farming group on both days of high- and non-high-heat [43]. The majority of cases were discharged home from ED (67.7%, n = 41,487). There was a statistically significant difference between the departure status of farmers and non-farmers on days on non-high-heat (p < 0.001). The results suggest that on high-heat days, more farmers were admitted to hospital (29.9%), and less were discharged home (61.9%) compared to days of non-high-heat (24.4% and 71.0%, respectively).
Table 5 shows the results of logistic regression models comparing the prevalence of presentations to the Emergency Department and UCCs on heat and non-heat days between farmers and non-farmers after employing frequency weights on age, gender, and employment in agriculture at the LGA level. There was a significant difference in both the unadjusted and adjusted regressions. After adjusting for age, gender, Modified Monash Model (MMM), and the Index of Socio-economic Advantage and Disadvantage (ISRAD), farmers were 17% (95% CI: 0.73–0.95; p = 0.005) less likely to present to the Emergency Department on high-heat days compared to those from non-farming areas.
Table 5.
Logistic regression comparing prevalence of presentations to the Emergency Department on heat/non-heat days with farming status.
| Model | Chi-Square | Degrees of Freedom | p-Value | Odds Ratio | 95% Confidence Intervals | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Unadjusted | 18.43 | 1 | <0.001 | 0.79 | 0.71 | 0.88 |
| Adjusted Gender and Age * | 17.65 | 1 | <0.001 | 0.80 | 0.72 | 0.89 |
| Confounder Adjusted ** | 7.78 | 1 | 0.005 | 0.83 | 0.73 | 0.95 |
* Adjusted for age and gender; ** Adjusted for age, gender, Modified Monash Model (MMM), and Index of Relative Socio-economic Advantage and Disadvantage (ISRAD).
4. Discussion
Globally, research has identified increased mortality and morbidity on high-heat days [44]. Similarly, previous Australian literature has recognised increases in ill health due to high-heat [9,12,45]. On the contrary, the results of this study have demonstrated that there is a general decrease in presentations to ED on days of high-heat in rural south-west Victoria. This was particularly the case in the farming population, as the results suggested farmers were 17% less likely to present to ED on high-heat days when compared to those from non-farming areas. This contrasts with Williams et al. [46], whom explored effects of heatwaves on morbidity and mortality across South Australia, and identified significantly increased presentations to ED during heatwaves in the city of Adelaide; however, the differences did vary in regional locations, which included mining, agricultural, and coastal areas. Unsurprisingly, as our study was completed in a rural area, the most common Major Diagnostic Block presenting to ED on both high and non-high-heat days was injury [47], with injury more common in rural and regional areas. However, on high-heat days, there was a marked decrease in injuries in both farmers and non-farmers, which is contradictory to other findings which typically see an increase in injuries on days of high-heat [9,48,49]. In accordance with previous research, circulatory system illness increased in both cohorts on days of high-heat [11,13]. Furthermore, respiratory system illness increased in the farming population on high-heat days. Research undertaken in Finland identified that health-related cardiorespiratory symptoms increased in people with pre-existing lung conditions, agricultural workers, pensioners, and the unemployed [50]. Khalaj, Lloyd, Sheppeard, and Dear [9] investigated the impacts on health of heat waves in five regions in the state of New South Wales, and identified the most common primary diagnoses for hospital admission were injury, circulatory system illness, and respiratory system illness.
The results of this study suggest farmers are less likely overall to present to EDs than non-farmers. This finding was unexpected and contradictory to a Los Angeles County study exploring whether heat-related health outcomes are more prevalent in communities with higher proportions of construction, agricultural, and other outdoor industry workers—concluding that with each percentage increase in residents working in agriculture, a 10.9% increase in heat-related ED visits was reported [4]. Further, as the Australian farming population has been identified as an ageing workforce, and the risk of heat-related illness is higher for older people, it was anticipated that the farmers in this study population would be at even greater risk of heat-related illness due to the combination of older age and outdoor physical work [51]. Therefore, the results of this study suggest this farming population may be aware of the risks of working on high-heat days, and adapt their behaviours accordingly. Additionally, although not specifically developed for agriculture, Worksafe Victoria [52] and Safe Work Australia [53] provide guidance on working in heat. The Australian Centre for Agricultural Health and Safety [54] utilised the hierarchy of control to suggest methods of preventing heat-related illness while working on the farm. Furthermore, regional total fire ban days ban or severely restrict the use of vehicles, machinery, and mobile equipment, which may then contribute in reducing farm-related injuries [55]. However, it is hard to surmise if the reduction in the use of machinery and vehicles then lends itself to more physically challenging tasks, which could exacerbate and, thus, explain the increased cardiovascular and respiratory illnesses.
Research has shown that exposure to hot environments reduces worker productivity, and increases the likelihood of work-related injuries (WRIs). However, these studies have been largely focused on metropolitan areas [15]. Behavioural adaptions to hot weather in farming/agriculture may include self-pacing, increased rest periods, performing more strenuous activities in the cooler parts of the day, working under shade or ventilated sheds, increased water consumption, avoiding dark surfaces, appropriate clothing/personal protective equipment, modifying tools or equipment to reduce physical demands, and monitoring environmental conditions [56,57,58]. Spector, Krenz, Rauser, and Bonauto [33] investigated agricultural workers’ heat-related illness claims in Washington State, identifying that the majority of claims were due to a lack of worker training and a lack of a heat safety plan. This may not be as prevalent in the Australian farming context, as 99% of farms in Australia are family owned and operated, and as a result, farmers may be able to adapt their behaviours to avoid outdoor/physical work in extreme heat [59] In the USA, workers carried out, on average, one hour less work per day when temperatures exceeded 37 °C (compared with days in which the temperature was below 30 °C), as workers self-paced to maintain thermal comfort [60]. Heat-related health risks increase when work is ‘externally paced’, such as through production quotas, peer pressure, and remuneration by output, factors found in fruit picking and sheep shearing occupations [61]. The European Agency for Safety and Health at Work [58] suggested that modern technology could further assist in preventing heat-related illness in farmers, such as using smart watches or similar devices to monitor vital signs (e.g., heart beat and blood pressure), which could prevent serious illness, particularly circulatory system illness. Family farming, by its very nature, does allow for self-pacing, and this may help to explain the reductions in ED presentations on high-heat days from farmers, and should be promoted in outdoor working industries globally.
The results of this study highlight the importance of considering context in regard to heat-related illness, as local factors, including climate, demographics, and acclimatisation/adaptive capacity can play a large role; it is not a one size fits all [62]. It has been suggested that the impacts of heatwaves in metropolitan areas are more severe, as the built environment retains more heat [63,64]. Conversely, characteristics commonly present in regional/rural populations, including occupational (higher proportions of outdoor workers) and socio-demographic (e.g., lower socio-economic status, ageing population) factors, present increased risks for heat-related illness [3,46]. Sun, Weinberger, Nori-Sarma, Sprangler, Sun, Dominici, and Wellenius [62] emphasised the importance of local public health preparedness for specific locally defined temperature thresholds, as communities are acclimatised to different climates. This may include identifying local at-risk populations, increasing public awareness of heat-related health risks, heat illness prevention education, identification of local hazards and potential exposures, and the communities’ and local healthcare facilities’ adaptive capacity for potential increases in demand [28,62]. On a local level, the Victorian Government, Australia, currently issues heath alerts to organisations and the public for days over 30 °C [65]. More contextual public health service messages (e.g., to agricultural workers [58]) could be released through local organisations and social media to remind people of the increased risk of illness on high-heat days, specifically, cardiovascular and respiratory illness in this study population, as well as suggestions for reducing the risk, and acting quickly if unwell. Health care workers can also provide relevant information on preventing heat-related illness (e.g., the exacerbation of cardiovascular disease and respiratory illnesses, particularly to farming populations).
As the climate is changing, and high-heat days are likely to become more frequent and intense, it is important to understand protective factors for heat-related illness [66]. Currently, the farming/agriculture industry experiences high rates of injury and workplace fatalities [67]; however, as the results of this study demonstrate, on high-heat days, there is a large reduction of farmers presenting to ED and UCCs with injury. This is the first study to utilise the farming decision framework. The study was strengthened by the recruitment of all presentations (of south-west Victorian LGA residents) to the Emergency Departments during the study period to avoid selection bias. As the RAHDaR database does not collect occupation status, this decision framework allows for the identification of these two cohorts (farming and non-farming) to allow for a closer comparison of the behaviours and use of services. The authors acknowledge that the decision framework may miss some farm workers who reside in non-farming areas and regional towns or cities, and this is identified as a limitation of the decision framework. However, this study does highlight the value of collecting occupation data at both Emergency Departments and UCCs, as this is currently not collected [68]. It also calls attention to the importance of understanding local context before initiating a public health heat response.
5. Conclusions
This is the first study to examine presentations to ED and UCCs in a rural Australian setting, and explore farming populations’ use of these services. This study confirms that unlike previous metropolitan studies, there is an overall decrease in presentations to ED on high-heat days in rural Victoria. Farmers are less likely than non-farmers to present on high-heat days overall, and with a significant reduction of injuries and musculoskeletal/connective tissue system illness in comparison to non-farmers. This suggests farmers in this cohort are aware of the risks of working/engaging in high-intensity activities on high-heat days, and adjust their behaviours accordingly. Those from farming towns that do attend, however, are more likely to be admitted for cardiovascular and respiratory type illness. The model used in this study could be replicated in other regions to address gaps in rural data, and better understand the patterns of presentations to Emergency Departments. This would enable better preparation, and possibly prevent the predicted presentations on high-heat days in rural and agricultural communities. Further investigation is needed into the effects of consecutive high-heat days, and the day following a high-heat day.
Acknowledgments
The authors wish to acknowledge the substantial contribution of David Rendell in the development of the farming area framework and data analysis.
Appendix A
Figure A1.
Framework for determining farming populations.
Author Contributions
J.A., S.B., T.B. and K.K. were responsible for study conceptualisation and methodology design; K.K., data curation/gathering; J.A. and M.M., data analysis; J.A., S.B., T.B. and M.M., data/result interpretation; J.A. and S.B., original draft preparation; and all authors contributed to the draft review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
The National Centre for Farmer Health is funded by the Victorian Government.
Institutional Review Board Statement
Ethics approval was gained from the South West Healthcare Human Research Ethics Committee (Ref: 2019 31), and Deakin University Human Research Ethics Committee (Ref: 2020-004).
Informed Consent Statement
Patient consent was waived due to this being a retrospective study of a de-identified database. Consent was gained from each of the participating hospital CEOs.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.CSIRO . State of the Climate 2018. Bureau of Meterology & CSIRO; Canberra, Australia: 2018. [Google Scholar]
- 2.Wald A. Emergency Department Visits and Costs for Heat-Related Illness Due to Extreme Heat or Heat Waves in the United States: An Integrated Review. Nurs. Econ. 2019;37:1. [Google Scholar]
- 3.Hess J., Saha S., Luber G. Summertime Acute Heat Illness in U.S. Emergency Departments from 2006 through 2010: Analysis of Nationaly Representative Sample. Environ. Health Perspect. 2014;122:11. doi: 10.1289/ehp.1306796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riley K., Wilhalme H., Delp L., Eisenman D. Mortality and Morbidity during Extreme Heat Events and Prevalence of Outdoor Work: An Analysis of Community-Level Data from Los Angeles County, California. Int. J. Environ. Res. Public Policy. 2018;15:4. doi: 10.3390/ijerph15040580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bureau of Meterology Annual Climate Statement. [(accessed on 29 October 2021)];2019 Available online: http://www.bom.gov.au/climate/current/annual/aus/#:~:text=2019%20was%20Australia’s%20warmest%20year%20on%20record%2C%20with%20the%20annual,1.33%20%C2%B0C%20in%202013.
- 6.Coates L., Haynes K., O’Brien J., McAveney J., Dimer de Oliveira F. Exploring 167 years of vulnerability: An examination of extreme heat events in Australia 1844–2010. Environ. Sci. Policy. 2014;42:33–44. doi: 10.1016/j.envsci.2014.05.003. [DOI] [Google Scholar]
- 7.Gauer R., Meyers B.K. Heat-Related Illnesses. Am. Fam. Physician. 2019;99:482–489. [PubMed] [Google Scholar]
- 8.Victorian Government Department of Health and Human Services . Extreme Heat. Department of Health and Human Services; Melbourne, Australia: 2015. [Google Scholar]
- 9.Khalaj B., Lloyd G., Sheppeard V., Dear K. The health impacts of heat waves in five regions of New South Wales, Australia: A case-only analysis. Int. Arch. Occup. Environ. Health. 2010;83:833–842. doi: 10.1007/s00420-010-0534-2. [DOI] [PubMed] [Google Scholar]
- 10.Nitschke M., Tucker G.R., Bi P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med. J. Aust. 2007;187:662–665. doi: 10.5694/j.1326-5377.2007.tb01466.x. [DOI] [PubMed] [Google Scholar]
- 11.Nitschke M., Tucker G.R., Hansen A.L., Williams S., Zhang Y., Bi P. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: A case-series analysis. J. Environ. Health. 2011;10:42. doi: 10.1186/1476-069X-10-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Toloo G.S., Yu W., Aitken P., FitzGerald G., Tong S. The impact of heatwaves on emergency department visits in Brisbane, Australia: A time series study. J. Crit. Care. 2014;18:R69. doi: 10.1186/cc13826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lindstrom S.J., Nagalingam V., Newnham H.H. Impact of the 2009 Melbourne heatwave on a major public hospital. Intern. Med. J. 2013;43:1246–1250. doi: 10.1111/imj.12275. [DOI] [PubMed] [Google Scholar]
- 14.Victorian Government . January 2009 Heatwave in Victoria: An Assessment of Health Impacts. Department of Health; Melbourne, Australia: 2009. [Google Scholar]
- 15.Bi P., Williams S., Loughnan M., Lloyd G., Hansen A., Kjellstrom T., Dear K., Saniotis A. The Effects of Extreme Heat on Human Mortality and Morbidity in Australia: Implications for Public Health. Asia Pac. J. 2011;23:27S–36S. doi: 10.1177/1010539510391644. [DOI] [PubMed] [Google Scholar]
- 16.Sainato M. ‘We’re not Animals, We’re Human Beings’: US Farm Workers Labor in Deadly Heat with Few Protections. [(accessed on 31 November 2021)]. Available online: https://www.theguardian.com/environment/2021/jul/16/farmworkers-labor-deadly-heat-few-protections.
- 17.Electrical Trades Union When Is It Too Hot to Keep Working? [(accessed on 19 October 2021)]. Available online: https://www.etuvic.com.au/ETUV/Your_Union/News/When_s_it_too_hot_to_keep_working_.aspx.
- 18.Tigchelaar M. Work adaptions insufficient to address growing heat risk for U.S. agricultural workers. Environ. Res. Lett. 2020;15:094035. doi: 10.1088/1748-9326/ab86f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Safe Work Australia This Summer, Ensure that You Know the Hazard of Working in Heat and in Air Pollution 2020. [(accessed on 19 October 2021)]; Available online: https://www.safeworkaustralia.gov.au/media-centre/news/summer-ensure-you-know-hazards-working-heat-and-air-pollution.
- 20.Jay O., Brotherhood J.R. Occupational heat stress in Australian workplaces. Temperature. 2016;3:394–411. doi: 10.1080/23328940.2016.1216256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kloot K., Baker T.R. Building a research-ready database of rural emergency presentations: The RAHDaR pilot study. Emerg. Med. Australas. 2019;31:126–128. doi: 10.1111/1742-6723.13156. [DOI] [PubMed] [Google Scholar]
- 22.Kloot K. Initial destination hospital of paediatric prehospital patients in rural Victoria. Emerg. Med. Australas. 2016;28:205–210. doi: 10.1111/1742-6723.12558. [DOI] [PubMed] [Google Scholar]
- 23.Independent Hospital Pricing Authority . Definition of Emergency Services for ABF Purposes. ABS; Canberra, Australia: 2016. [Google Scholar]
- 24.Victorian Department of Health and Human Services . Victorian Emergency Minimum Dataset (VEMD) User Manual. DHHA; Melbourne, Australia: 2017. [Google Scholar]
- 25.Peck B., Terry D.R., Kloot K. Understanding childhood injuries in rural areas: Using Rural Acute Hospital Data Register to address previous data deficiencies. Emerg. Med. Australas. 2020;32:646–649. doi: 10.1111/1742-6723.13565. [DOI] [PubMed] [Google Scholar]
- 26.Terry D.R., Peck B., Kloot K. The data deficit for asthma emergency presentations might surprise you: How RAHDaR addresses the data chasm. Rural Remote Health. 2020;20:5776. doi: 10.22605/RRH5776. [DOI] [PubMed] [Google Scholar]
- 27.Australian Consortium for Classification Development . The International Statistical Classification of Diseases and Related Health Problems. 10th ed. Independent Hospital Pricing Authority; Sydney, Australia: 2017. Australia Modification (ICD-10-AM/ACHI/ACS) [Google Scholar]
- 28.Pogacar T., SZnidarsic Z., Kajfez Bogataj L., Flouris A.D.K.P., Crepinsek Z. Heat Waves Occurence and Outdoor Workers’ Self-assessment of Heat Stress in Slovenia and Greece. Int. J. Environ. Res. Public Health. 2019;16:597. doi: 10.3390/ijerph16040597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Linares C., Diaz J. Impact of high temperatures on hospital admissions: Comparative analysis with previous studies about mortality (Madrid) Eur. J. Public Health. 2007;18:317–322. doi: 10.1093/eurpub/ckm108. [DOI] [PubMed] [Google Scholar]
- 30.Microsoft Microsoft Excel. [(accessed on 30 November 2021)]. Available online: https://www.microsoft.com/en-au/microsoft-365/excel.
- 31.Bureau of Meterology Weather Station Directory. [(accessed on 20 March 2020)]; Available online: http://www.bom.gov.au/climate/data/stations/
- 32.Campbell S.M., Remenyi T.A., Williamson G.J., White C.J., Johnston F.H. The Value of Local Heatwave Impact Assessment: A Case-Crossover Analysis of Hospital Emergency Department Presentations in Tasmania, Australia. Int. J. Environ. Res. Public Health. 2019;16:3715. doi: 10.3390/ijerph16193715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Spector J.T., Krenz J., Rauser E., Bonauto D.K. Heat-Related Illness in Washington State Agriculture and Forestry Sectors. Am. J. Ind. Med. 2014;57:881–895. doi: 10.1002/ajim.22357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kovats R.S., Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. J. Occup. Environ. 2004;61:893–898. doi: 10.1136/oem.2003.012047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Australian Bureau of Statistics Regional Population by Age and Sex. [(accessed on 19 October 2021)]; Available online: https://www.abs.gov.au/statistics/people/population/regional-population-age-and-sex/latest-release.
- 36.Australian Bureau of Statistics Community Profiles. [(accessed on 20 October 2021)]; Available online: https://www.abs.gov.au/websitedbs/D3310114.nsf/Home/2016%20Census%20Community%20Profiles.
- 37.Australian Government Department of Health Modified Monash Model. [(accessed on 19 October 2021)]; Available online: https://www.health.gov.au/health-topics/health-workforce/health-workforce-classifications/modified-monash-model.
- 38.Australian Bureau of Statistics QuickStats Canberra. [(accessed on 20 October 2021)]; Available online: https://www.abs.gov.au/websitedbs/D3310114.nsf/Home/2016%20QuickStats.
- 39.Google Google Maps. [(accessed on 20 October 2021)]. Available online: https://www.google.com/maps/
- 40.Burns M.K. How to establish interrater relability. Nursing. 2014;44:56–58. doi: 10.1097/01.NURSE.0000453705.41413.c6. [DOI] [PubMed] [Google Scholar]
- 41.Australian Government Department of Health Health Workforce Locator. [(accessed on 26 October 2021)]; Available online: https://www.health.gov.au/resources/apps-and-tools/health-workforce-locator/health-workforce-locator.
- 42.IBM Downloading IBM SPSS Statistics 27. [(accessed on 19 October 2021)]. Available online: https://www.ibm.com/support/pages/downloading-ibm-spss-statistics-27.
- 43.Australasian College for Emergency Medicine . Guidelines on the Implementation of the Australasian Triage Scale in Emergency Departments. Australasian College for Emergency Medicine; Melbourne, Australia: 2016. [Google Scholar]
- 44.Basu R. High ambient temperature and mortality: A review of epidemiologic studies from 2001 to 2008. Environ. Health. 2009;8:40. doi: 10.1186/1476-069X-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams S., Nitschke M., Sullivan T., Tucker G.R., Weinstein P., Pisaniello D.L., Parton K.A., Bi P. Health and health in Adelaide, South Australia: Assessment of heat threshlds and temperature relationships. Sci. Total Environ. 2012;414:126–133. doi: 10.1016/j.scitotenv.2011.11.038. [DOI] [PubMed] [Google Scholar]
- 46.Williams S., Venugopal K., Nitschke M., Nairn J., Fawcett R., Beattie C., Wynwood G., Bi P. Regional morbidity and mortality during heatwaves in South Australia. Int. J. Biometeorol. 2018;62:1911–1926. doi: 10.1007/s00484-018-1593-4. [DOI] [PubMed] [Google Scholar]
- 47.Australian Institute of Health and Welfare Rural and Remote Health Canberra. [(accessed on 12 October 2021)]; Available online: https://www.aihw.gov.au/reports/australias-health/rural-and-remote-health.
- 48.Xiang J., Bi P., Pisaniello D., Hansen A., Sullivan T. Association between high temperature and work-related injuries in Adelaide, South Australia, 2001–2010. Occup. Environ. Med. 2013;71:246–252. doi: 10.1136/oemed-2013-101584. [DOI] [PubMed] [Google Scholar]
- 49.Xiang J., Bi P., Pisaniello D., Hansen A. The impact of heatwaves on workers’ health and safety in Adelaide, South Australia. Environ. Res. 2014;133:90–95. doi: 10.1016/j.envres.2014.04.042. [DOI] [PubMed] [Google Scholar]
- 50.Näyhä S., Rintamäki H., Donaldson G., Hassi J., Jousilahti P., Laatikainen T., Jaakkola J.J., Ikäheimo T.M. The prevalence of heat-related cardiorespiratory symptoms: The vulnerable groups identified from the National FINRISK 2007 Study. Int. J. Biometeorol. 2016;61:657–668. doi: 10.1007/s00484-016-1243-7. [DOI] [PubMed] [Google Scholar]
- 51.Horton G., Hanna L., Kelly B. Drought, drying and climate change: Emerging health issues for ageing Australians in rural areas. Australas. J. Ageing. 2010;29:2–7. doi: 10.1111/j.1741-6612.2010.00424.x. [DOI] [PubMed] [Google Scholar]
- 52.Worksafe Victoria Working in Heat. [(accessed on 12 October 2021)]; Available online: https://www.worksafe.vic.gov.au/resources/working-heat.
- 53.Safe Work Australia Working in Heat. [(accessed on 12 October 2021)]; Available online: https://www.safeworkaustralia.gov.au/topic/working-heat.
- 54.Heat Stress on the Farm. [(accessed on 30 November 2021)]. Available online: https://aghealth.sydney.edu.au/wp-content/uploads/2019/05/19.-Heat-Stress.pdf.
- 55.Country Fire Authority Can I or Can’t I? [(accessed on 16 January 2022)]; Available online: https://www.cfa.vic.gov.au/warnings-restrictions/total-fire-bans-and-ratings/can-i-or-cant-i.
- 56.Jackson L.L., Rosenberg H.R. Preventing Heat-Related Illness Among Agricultural Workers. J. Agromed. 2010;15:200–215. doi: 10.1080/1059924X.2010.487021. [DOI] [PubMed] [Google Scholar]
- 57.Victorian Farmers Federation . Victorian Farmers Federation, Annual Report 2019/20. Victorian Farmers Federation; Melbourne, Victoria: 2020. [Google Scholar]
- 58.European Agency for Safety and Health at Work . Review of the Future of Agriculture and Occupational Safety and Health (OSH) Publications Office of the European Union; Luxembourg: 2020. [Google Scholar]
- 59.National Farmers Federation Farm Facts. [(accessed on 16 January 2022)]. Available online: https://nff.org.au/media-centre/farm-facts/
- 60.Zivin J.G., Neidell M.J. Temperature and the Allocation of Time: Implications for Climate Change. National Bureau of Economic Research; Cambridge, MA, USA: 2010. [Google Scholar]
- 61.Hanna E.G., Kjellstron T., Bennett C., Dear K. Climate change and rising heat: Population health implications for working people in Australia. Asia Pac. J. 2011;23:14S–26S. doi: 10.1177/1010539510391457. [DOI] [PubMed] [Google Scholar]
- 62.Sun S., Weinberger K.R., Nori-Sarma A., Spangler K.R., Sun Y., Dominici F., Wellenius G.A. Ambient heat and risks of emergency department visits among adults in the United States: Time stratified case crossover study. BMJ. 2021;375:e065653. doi: 10.1136/bmj-2021-065653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McGeehin M.A., Mirabelli M. The Potential Impacts of Climate Variability and Change on Temperature-Related Morbidity and Mortality in the United States. Environ. Health Perspect. 2001;109:185–199. doi: 10.1289/ehp.109-1240665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hibbard K.A., Hoffman F.M., Huntzinger D., West T.O. Changes in Land Cover and Terrestrial Biogeochemistry. U.S. Global Change Research Program; Washington, DC, USA: 2017. [Google Scholar]
- 65.Victorian Department of Health . Heat Health Alerts. Department of Health; Melbourne, Australia: 2021. [Google Scholar]
- 66.Climate Council of Australia . On The Frontline: Climate Change & Rural Communities. Climate Council of Australia Ltd.; Sydney, Australia: 2016. [Google Scholar]
- 67.Safe Work Australia . Work-Related Traumatic Injury Fatalities, Australia. Safe Work Australia; Canberra, Australia: 2019. [Google Scholar]
- 68.Victorian Government Department of Health . VEMD User Manual 2020–21 Sections 1 to 6. Department of Health; Melbourne, Australia: 2020. [Google Scholar]