Abstract
The new coronavirus disease 2019 (COVID-19) could be associated with elevated inflammatory cytokine levels, suggesting the involvement of cytokine release syndrome. This syndrome is characterized by release of interleukin 6 correlated with COVID-19 severity and mortality. Targeting IL-6 with Tocilizumab treatment could be a potential therapeutic option for old patients. We report the case of an 88-year-old man with COVID-19 disease who presented at the admission with anemia, fever, oxygen desaturation (92%), and inflammatory syndrome (C-reactive protein (CRP) at 182.5 mg/L; reference range <5.0 mg/L). After remaining CRP level increase (206.6 mg/L), Tocilizumab administration led to rapid clinical outcome and resolution of his inflammatory syndrome. This case report represents a supplementary data confirming the efficacy and safety of Tocilizumab for COVID-19 in elderly patients.
Keywords: COVID-19, Tocilizumab, case report, elderly, inflammatory syndrome
1. Introduction
The new coronavirus pneumonia, first identified in the province of Hubei (China) and designated by the World Health Organization (WHO) as coronavirus disease 2019 (COVID-19), induced a viral infection by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that affected several organs involving the respiratory, renal, cardiovascular, central nervous, and gastrointestinal systems [1,2]. This multi organ dysfunction syndrome could be explained by the immune dysregulation caused by the SARS-CoV-2, resulting in hyperinflammation on the immune systems and cytokine release syndrome (cytokine storm) [3,4]. In this context, elderly patients are more likely to experience a more severe course of disease due to alterations in both the innate and adaptative immune systems [5]. In advanced age, it has been reported that an increase in the levels of circulating pro-inflammatory cytokines such as interleukins, growth factors, and proteases [6,7]. These elements could contribute to develop severe disease in elderly adults over 65 years old that represent 80% of the hospitalizations with a higher risk of death than those under 65 [5]. Older adults with severe COVID-19 could rapidly progress into a cytokine storm that involves hyperactivation of the immune system and hypercoagulation in the small blood vessels [8].
Because COVID-19 severity and mortality are correlated with the high levels of interleukin-6 (IL-6), administration of Tocilizumab, a recombinant monoclonal antibody which binds specifically to IL-6 receptors, was used with a decrease in fever, lower oxygen requirements, and a reduction in mortality [9,10,11,12]. However, few data exist on the effectiveness and safety of the drug treatment in elderly patients [13,14].
In this case, we describe the successful treatment by single Tocilizumab administration of an 88-year-old patient with severe COVID-19.
2. Case
An 88-year-old man was admitted in our geriatric rehabilitation unit after a blood transfusion for anemia at 5 g/L. The past medical history of the patient included epilepsy, ischemic heart failure treated, arterial hypertension, dyslipidemia, and obesity. At baseline, he had partial deafness and was brought to medical attention due to loss of autonomy for personal hygiene and dressing. After the admission, asymptomatic SARS-CoV-2 infection was confirmed by reverse transcription polymerase chain reaction (RT-PCR) test and the patient was transferred to our COVID-19 unit. He had sustained fever (38 °C), heart rate at 100/min, blood pressure at 142/65 mmHg, and the peripheral capillary oxygen saturation (SpO2) rose to 92% by 2 L/min oxygen. At the same time, blood sample analysis found elevated levels of C-reactive-protein (CRP 182.5 mg/L) a high marker of inflammation, an anemia (hemoglobin 10.8 g/dL), hyponatremia (132 mmol/L), hyperkalemia (4.53 mmol/L), and hyperuricemia (11.8 mmol/L). The patient received paracetamol (3 g/day), ramipril (5 mg/day), and lansoprazole (15 mg/day). Table 1 shows the main laboratory values made to date.
Table 1.
Main laboratory values made to date.
| Parameters (Laboratory Reference) | Admission | Day 2 | Day 8 | Day 13 |
|---|---|---|---|---|
| CRP (<5.0 mg/L) | 182.5 | 176.8 | 206.6 | 23.3 |
| Hemoglobin (12.9–16.7 g/dL) | 10.8 | 10.7 | 9.9 | 10.0 |
| Natremia (136–145 mmol/L) | 132 | 135 | 137 | 139 |
| Kalemia (3.40–4.50 mmol/L) | 4.53 | 4.56 | 4.38 | 3.75 |
| Lymphocytes (1.070–4.100 g/L), | 1.470 | 1.010 | 0.690 | 0.48 |
| Blood creatinine (62.0–106.0 µmol/L) | 99.9 | 103.3 | 78.4 | 88.1 |
| Blood urea (2.86–8.21 mmol/L) | 11.8 | 12.9 | 8.2 | 7.1 |
| MDRD 1 (>90) | 62 | 60 | 82 | 72 |
| NT-proBNP 2 (50.0–125.0 pg/mL) | - | 9118.0 | 3819.0 |
1 MDRD: modification of diet in renal disease 2 NT-proBNP: pro-brain natriuretic peptide.
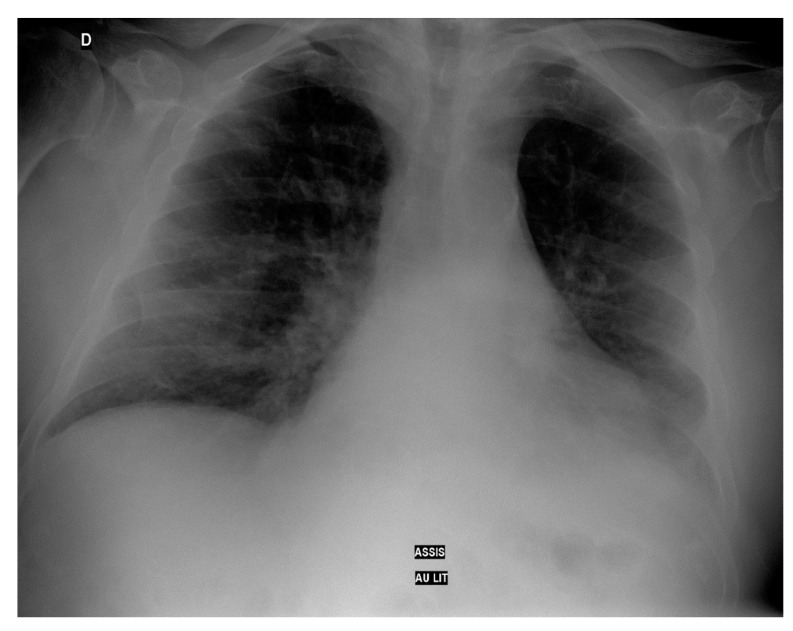
On day 2, he presented a sudden oxygen desaturation (SpO2 90%) stabilized with the administration of oxygen at high flow (4 L/min). The thoracic radiography showed an alveolar and interstitial diffuse damage and a left basal outpouring (Figure 1).
Figure 1.
Thoracic radiography at day 2.
At this time, the patient received dexamethasone (6 mg daily for 10 days), enoxaparin (4000 UI daily for 30 days), and combination of amoxicillin and clavulanic acid (1 g/200 mg × 3/day for 2 days) as the recommendations for the therapeutic management of COVID patients from the Paris University Hospitals (AP-HP) and the European Respiratory Society guideline. On day 3, a computed tomography angiogram of the chest was ordered and revealed left segmental pulmonary emboli without sign of pulmonary arterial hypertension (Figure 2).
Figure 2.
Computed tomography angiogram of the chest at day 3. (arrow shows the emblism).
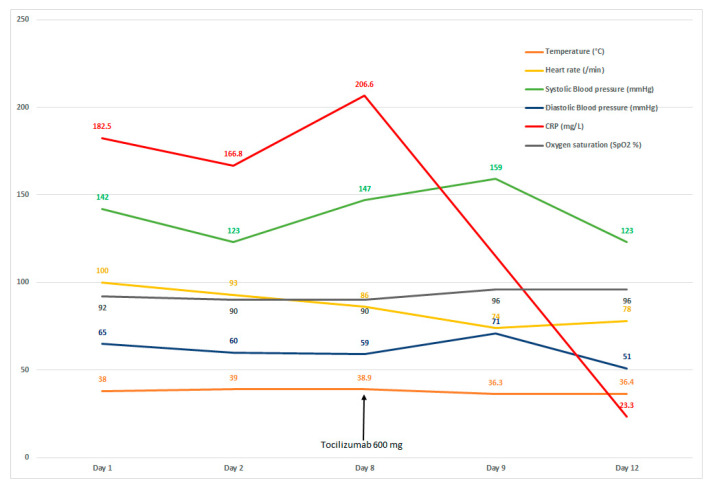
On day 4, spiramicin (3 MUI × 3/day) was added and ceftriaxone 1 g daily to treat a urinary tract infection to Morganella morgana. The combination of amoxicillin and clavulanic acid was stopped without impact on the fever. By hospital day 8, its clinical state was judged to be critical with persistent high fever (38.9 °C), blood pressure at 147/59 mmHg, heart rate 86/min, oxygen saturation 90% with 5 L/min, and high level of CRP 206.6 mg/L. Figure 3 summarizes major clinical parameters and CRP levels obtained during the hospital course.
Figure 3.
Clinical parameters from day 1 to day 12 (Tocilizumab administration at day 8).
At this time, the choice of Tocilizumab treatment was discussed and validated in a multidisciplinary meeting with geriatricians and clinical pharmacists.
The patient received a single dose of intravenous Tocilizumab at 8 mg/kg (600 mg) with no clinical improvement. The same day, the clinical state of the patient progressed favorably with normal temperature at 36.3 °C, heart rate 74/min, and blood pressure 159/71 mmHg. The CRP level was significantly decreased to 23.3 mg/L after 5 days of drug administration and normalized at day 10 of drug administration. The oxygen saturation was increased more progressively, and the oxygen discharge was effective by day 28 after the Tocilizumab administration. Four weeks later, the patient was seen in an out-patient setting and had been doing well.
3. Discussion
We report the case of an 88-year-old man with risk factors including an older age that was treated successfully by Tocilizumab for a severe COVID-19 disease. Clinical data showed that the patient’s vital parameters improved after drug treatment. Moreover, a significant decrease in CRP and fever levels was observed just after a single infusion, suggesting the potential impact of Tocilizumab on the cytokine release syndrome. Therefore, our patient did not experience any adverse events.
Because studies in severe COVID-19 observed the association with elevated levels of IL-6 and mortality, randomized clinical trials suggested benefit of the anti-IL-6 receptor monoclonal antibody Tocilizumab with reported heterogenous results [15,16,17,18,19]. In a randomized clinical trial that included 130 patients hospitalized with COVID-19 and moderate-to-severe pneumonia, Tocilizumab did not reduce the mortality over 28 days in comparison with the usual care group [16]. These results were supported by the study by Tsai et al. on the impact of Tocilizumab administration on mortality in severe COVID-19 that recorded no statistical difference between the Tocilizumab group and the no Tocilizumab group (odds ratio, 1.0; 95% confidence interval, 0.465–2.151; p = 1.00) [20]. In a recent research article, a trial that examined survival varied with baseline CRP levels demonstrated the administration of Tocilizumab was beneficial in patients with CRP levels greater than 15.0 g/L [21]. Some studies have also evaluated the Tocilizumab treatment in patients with severe COVID-19, suggesting its efficacy on mortality [22,23,24]. The TCZ efficacy on mortality on day 14 and 28 was retrospectively evaluated in 62 patients (57.4 ± 14.3 years) who received one to two doses of TCZ (400–800 mg every 12 h) [22]. There was a significant difference in the 28-day (TCZ = 62 and control = 86) and in the 14-day (9.7% vs. 24.4%, p = 0.022) fatality rate among the TCZ-treated patients and control group. The inflammatory marker CRP decreased in the TCZ-treated patients, indicating a response to the IL-6 blocker. Moreover, a meta-analysis including 10 studies involving 1675 severe COVID-19 patients (median age >52 years) revealed a significant difference in mortality in the Tocilizumab group compared to the control group (19.5% vs. 28.3%, p < 0.00001) [24]. As in our clinical case, a Spanish cohort of elderly COVID-19 patients (mean age 85.2 years) found benefit in patients receiving Tocilizumab and corticosteroids (adjusted estimation HR 0.09, 95% CI: 0.01–0.74) [23]. Elderly patients are frequently absent from clinical trials even though we need efficacy and safety data in this population. More information is needed regarding the dose schedule of Tocilizumab treatment, eligibility criteria to select the patients, and association with other therapeutic options such as corticosteroids or antiviral drugs.
4. Conclusions
In conclusion, Tocilizumab may be an optional treatment in elderly patients with severe COVID-19 associated with high CRP level. However, further research is needed to identify optimal elderly patient population for treatment with Tocilizumab, and to confirm its effectiveness and safety.
Author Contributions
C.O.O. and J.S. decided study design and concept, drafted manuscript; N.L. revised manuscript; K.T. revised manuscript; H.R. revised manuscript; J.B.H. revised manuscript; N.E.O. revised manuscript; G.Z. revised manuscript; M.M.A.Z. revised manuscript; M.A. revised manuscript; A.J. revised manuscript; J.S. decided study design and concept, provided study supervision, revised manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki. As a single case report, ethical review and approval was not applicable.
Informed Consent Statement
Informed consent was obtained from patient involved in the study.
Data Availability Statement
The data presented in this study can be requested to the corresponding author. The data are not publicly available due to confidentiality and anonymity.
Conflicts of Interest
All authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W., Si H.R., Zhu Y., Li B., Huang C.L., et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang F., Deng L., Zhang L., Cai Y., Cheung C.W., Xia Z. Review of the Clinical Characteristics of Coronavirus Disease 2019 (COVID-19) J. Gen. Intern. Med. 2020;35:1545–1549. doi: 10.1007/s11606-020-05762-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chinnadurai R., Ogedengbe O., Agarwal P., Money-Coomes S., Abdurrahman A.Z., Mohammed S., Kalra P.A., Rothwell N., Pradhan S. Older age and frailty are the chief predictors of mortality in COVID-19 patients admitted to an acute medical unit in a secondary care setting- a cohort study. BMC Geriatr. 2020;20:409. doi: 10.1186/s12877-020-01803-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franceschi C., Garagnani P., Parini P., Giuliani C., Santoro A. Inflammaging: A new immune-metabolic viewpoint for age-related diseases. Nat. Rev. Endocrinol. 2018;14:576–590. doi: 10.1038/s41574-018-0059-4. [DOI] [PubMed] [Google Scholar]
- 7.Schmeer C., Kretz A., Wengerodt D., Stojiljkovic M., Witte O.W. Dissecting Aging and Senescence-Current Concepts and Open Lessons. Cells. 2019;8:1446. doi: 10.3390/cells8111446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Terpos E., Ntanasis-Stathopoulos I., Elalamy I., Kastritis E., Sergentanis T.N., Politou M., Psaltopoulou T., Gerotziafas G., Dimopoulos M.A. Hematological findings and complications of COVID-19. Am. J. Hematol. 2020;95:834–847. doi: 10.1002/ajh.25829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li H., Liu L., Zhang D., Xu J., Dai H., Tang N., Su X., Cao B. SARS-CoV-2 and viral sepsis: Observations and hypotheses. Lancet. 2020;395:1517–1520. doi: 10.1016/S0140-6736(20)30920-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhang X., Tan Y., Ling Y., Lu G., Liu F., Yi Z., Jia X., Wu M., Shi B., Xu S., et al. Viral and host factors related to the clinical outcome of COVID-19. Nature. 2020;583:437–440. doi: 10.1038/s41586-020-2355-0. [DOI] [PubMed] [Google Scholar]
- 11.Napoli C., Benincasa G., Criscuolo C., Faenza M., Liberato C., Rusciano M. Immune reactivity during COVID-19: Implications for treatment. Immunol. Lett. 2021;231:28–34. doi: 10.1016/j.imlet.2021.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ali A., Kamjani M.H., Kesselman M.M. The Role of Tocilizumab in Cytokine Storm and Improving Outcomes in COVID-19. Recent Pat. Antiinfect. Drug Discov. 2020;15:104–112. doi: 10.2174/1574891X15666200922155712. [DOI] [PubMed] [Google Scholar]
- 13.Streicher C., Engalenc X., Gaudin M., Vignaud G., Daulange A., Abraham B. Could Tocilizumab be an Attractive Therapeutic Option for Elderly Patients with Severe COVID-19? A Case Report. Clin. Drug Investig. 2020;40:1085–1088. doi: 10.1007/s40261-020-00969-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kataoka H., Kodama F., Tomita T., Kondo M., Nagasaka A., Nishikawa S., Mukai M. Immediate Amelioration of Severe Respiratory Distress in Sjögren’s Syndrome with COVID-19 Treated with a Single Dose of Off-label Tocilizumab. Intern. Med. 2021;60:639–643. doi: 10.2169/internalmedicine.6010-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.REMAP-CAP Investigators. Gordon A.C., Mouncey P.R., Al-Beidh F., Rowan K.M., Nichol A.D., Arabi Y.M., Annane D., Beane A., van Bentum-Puijk W., et al. Interleukin-6 Receptor Antagonists in Critically Ill Patients with COVID-19. N. Engl. J. Med. 2021;384:1491–1502. doi: 10.1056/NEJMoa2100433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hermine O., Mariette X., Tharaux P.L., Resche-Rigon M., Porcher R., Ravaud P., CORIMUNO-19 Collaborative Group Effect of Tocilizumab vs. Usual Care in Adults Hospitalized with COVID-19 and Moderate or Severe Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021;181:32–40. doi: 10.1001/jamainternmed.2020.6820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stone J.H., Frigault M.J., Serling-Boyd N.J., Fernandes A.D., Harvey L., Foulkes A.S., Horick N.K., Healy B.C., Shah R., Bensaci A.M., et al. BACC Bay Tocilizumab Trial Investigators. Efficacy of Tocilizumab in Patients Hospitalized with Covid-19. N. Engl. J. Med. 2020;383:2333–2344. doi: 10.1056/NEJMoa2028836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Salvarani C., Dolci G., Massari M., Merlo D.F., Cavuto S., Savoldi L., Bruzzi P., Boni F., Braglia L., Turrà C., et al. RCT-TCZ-COVID-19 Study Group. Effect of Tocilizumab vs. Standard Care on Clinical Worsening in Patients Hospitalized with COVID-19 Pneumonia: A Randomized Clinical Trial. JAMA Intern. Med. 2021;181:24–31. doi: 10.1001/jamainternmed.2020.6615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Salama C., Han J., Yau L., Reiss W.G., Kramer B., Neidhart J.D., Criner G.J., Kaplan-Lewis E., Baden R., Pandit L., et al. Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N. Engl. J. Med. 2021;384:20–30. doi: 10.1056/NEJMoa2030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsai A., Diawara O., Nahass R.G., Brunetti L. Impact of tocilizumab administration on mortality in severe COVID-19. Sci. Rep. 2020;10:19131. doi: 10.1038/s41598-020-76187-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mariette X., Hermine O., Tharaux P.L., Resche-Rigon M., Steg P.G., Porcher R., Ravaud P. Effectiveness of Tocilizumab in Patients Hospitalized with COVID-19: A Follow-up of the CORIMUNO-TOCI-1 Randomized Clinical Trial. JAMA Intern. Med. 2021;181:1241–1243. doi: 10.1001/jamainternmed.2021.2209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-Baadani A., Eltayeb N., Alsufyani E., Albahrani S., Basheri S., Albayat H., Batubara E., Ballool S., Al Assiri A., Faqihi F., et al. Efficacy of tocilizumab in patients with severe COVID-19: Survival and clinical outcomes. J. Infect. Public. Health. 2021;14:1021–1027. doi: 10.1016/j.jiph.2021.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Duarte-Millán M.A., Mesa-Plaza N., Guerrero-Santillán M., Morales-Ortega A., Bernal-Bello D., Farfán-Sedano A.I., García de Viedma-García V., Velázquez-Ríos L., Frutos-Pérez B., De Ancos-Aracil C.L., et al. Prognostic factors and combined use of tocilizumab and corticosteroids in a Spanish cohort of elderly COVID-19 patients. J. Med. Virol. 2021 doi: 10.1002/jmv.27488. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhao J., Cui W., Tian B.P. Efficacy of tocilizumab treatment in severely ill COVID-19 patients. Crit. Care. 2020;24:524. doi: 10.1186/s13054-020-03224-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study can be requested to the corresponding author. The data are not publicly available due to confidentiality and anonymity.