Abstract
The COVID-19 pandemic is worsening loneliness for many older people through the challenges it poses in engaging with their social worlds. Digital technology has been offered as a potential aid, however, many popular digital tools have not been designed to address the needs of older adults during times of limited contact. We propose that the Social Identity Model of Identity Change (SIMIC) could be a foundation for digital loneliness interventions. While SIMIC is a well-established approach for maintaining wellbeing during life transitions, it has not been rigorously applied to digital interventions. There are known challenges to integrating psychological theory in the design of digital technology to enable efficacy, technology acceptance, and continued use. The interdisciplinary field of Human Computer Interaction has a history of drawing on models originating from psychology to improve the design of digital technology and to design technologies in an appropriate manner. Drawing on key lessons from this literature, we consolidate research and design guidelines for multidisciplinary research applying psychological theory such as SIMIC to digital social interventions for loneliness.
Keywords: Wellbeing, Loneliness, Digital connections, User-centred design, Social cure, Social identity, Multidisciplinary
The World Health Organization declared COVID-19 a pandemic in March 2020 (WHO, 2020). Over the course of the pandemic, governments have applied differing containment strategies, often enforcing social restrictions – including quarantines, self-isolation, lockdowns, travel bans, closure of public services and third sector provisions, and social or physical distancing rules. These restrictions have been met with concerns about the health and wellbeing impacts of isolation, including increased loneliness (Brooks et al., 2020; Galea, Merchant, & Lurie, 2020; Klein, 2020), which already imposes a large public health burden (Banerjee & Rai, 2020; Holt-Lunstad, Smith, Baker, Harris, & Stephenson, 2015; Lim, Eres, & Vasan, 2020). Even when the immediate health risks of COVID-19 have passed, there may not be a return to ‘normal’ for some people due to permanent changes to social networks, support services demand, and health detriments such as functional decline (De Biase, Cook, Skelton, Witham, & ten Hove, 2020; Lorito et al., 2020; Talbot & Briggs, 2021). Considered together, the economic and social toll of the pandemic will likely require collective efforts from social, behavioural, and technology sciences for years to come.
In this review we focus on older people who are subject to a series of pandemic-related vulnerabilities such as serious health risks from COVID-19 (WHO, 2019), age-related social restrictions (Previtali, Allen, & Varlamova, 2020), the health impacts of chronic loneliness (Cacioppo, Grippo, London, Goossens, & Cacioppo, 2015; Luo, Hawkley, Waite, & Cacioppo, 2012), and restricted adoption of digital technology. Whilst technology has emerged as a vital lifeline during the pandemic there can be functional and technological barriers to adoption amongst older populations (Ehni & Wahl, 2020; Hebblethwaite, Young, & Martin Rubio, 2020; Jetten, Reicher, Haslam, & Cruwys, 2020; Shah, Nogueras, Woerden, & Kiparoglou, 2020).
In section 1, we outline psychological theories of loneliness and how loneliness interacts with ageing related challenges that might be exacerbated during the pandemic. We then advocate for the Social Identity Approach to Health (Haslam, Jetten, Cruwys, Dingle, & Haslam, 2018; Jetten, Haslam, & Haslam, 2012), and the Social Identity Model of Identity Change (SIMIC, Haslam, Steffens, et al., 2019; Jetten. et al., 2012), as a theoretical foundation for understanding loneliness as a lack of social group-belonging, and for identifying how people can maintain resilience during crises. We identify an opportunity for technology-supported, digital interventions for loneliness based on this SIMIC model.
In section 2, we review relevant work on digital interventions from the Human-Computer Interaction (HCI) literature and methods of designing useable and effective digital products that meet user needs, and are therefore more likely to achieve long-term adoption. Section 3 outlines our argument for bringing together the psychology of loneliness and social identity theory and HCI design research to build digital interventions that enable older people and their social networks to socially engage in ways that are meaningful to them, thus addressing loneliness created by social isolation. We conclude by providing some design guidelines that employ Social Identity principles to suggest ways in which digital interventions can be developed to address the social needs of older adults.
Loneliness theory and the legacy impacts of the pandemic for older people
In this section, we define loneliness and theories of loneliness, review evidence on the impacts of epidemics/pandemics on loneliness and identify why the pandemic has created a need for distanced, technology-supported communication and support to help mitigate loneliness. We then advance a particular approach to identifying and intervening in loneliness.
Understanding loneliness
Loneliness is the distressing feeling experienced during perceived social isolation, akin to thirst or hunger pangs (Hawkley & Cacioppo, 2010). Loneliness varies in intensity, duration, and frequency (Barreto et al., 2021) and is usually distinguished between either a perceived lack in close relationships and feelings of emptiness (emotional loneliness), or a perceived lack of belonging to larger networks/groups/communities (social loneliness) (Russell, Cutrona, Rose, & Yurko, 1984; Weiss, 1973, pp. xxii–236).
Loneliness results in a number of cognitive effects resulting in hypervigilance for social threats (such as hostility) and negative cognitive biases about social relationships (Hawkley & Cacioppo, 2010). This results in difficulty generating satisfactory social connections (Cacioppo et al., 2015; Heinrich & Gullone, 2006), and a reduced ability to understand emotions, engage in emotion regulation, and other self-control behaviours (Hawkley & Cacioppo, 2010; Lim et al., 2020). Qualitative research suggests loneliness is a profoundly subjective experience (Cohen-Mansfield, 2020), lonely individuals often report feeling unhopeful that they will get better (Taube, Jakobsson, Midlöv, & Kristensson, 2016), and feel trapped and disconnected from the outside world (Barke, 2017; Hauge & Kirkevold, 2012). In turn, this can reduce feelings of self-worth, power, and initiative. That is not to say that loneliness is a fixed state, rather it is fluid and changes over time (Victor, Sullivan, Woodbridge, & Thomas, 2015). Therefore, interventions hold great potential to reduce loneliness by targeting this complex set of cognitive, emotional, and social factors.
While social isolation is by itself associated with poorer health outcomes, the psychological experience of loneliness makes an additional, unique contribution to illness and mortality, comparable to that of smoking and greater than that of obesity (Holt-Lunstad et al., 2015). Loneliness predicts specific declines in physical, cognitive, and emotion regulation capabilities (Cacioppo & Hawkley, 2009). With an ageing global population, loneliness in older people increases health care costs as it is a risk factor for cognitive decline, cardiovascular disease, reduced immunity, and other physical health problems (Cacioppo et al., 2015). The resultant individual and multiple complex health needs place a burden on healthcare systems and, combined with social vulnerability during COVID-19, loneliness in older people is a now a burgeoning public health issue (Banerjee & Rai, 2020; Robb et al., 2020).
Evidence of older people's loneliness during the pandemic
There is a need for solid evidence to determine if loneliness is indeed increasing as was expected early in the pandemic (e.g. Klein, 2020). On one hand, evidence from prior epidemics suggests that loneliness can be increased by periods of involuntary social isolation (Cava & Et al., 2005; Digiovanni & Et al., 2004; Maunder, 2004; Pan, Chang, & Yu, 2005; Pellecchia, Crestani, Decroo, Van den Bergh, & Al-Kourdi, 2015). On the other hand, initial studies in the early weeks of the pandemic showed mixed results (El-Zoghby, Soltan, & Salama, 2020; Luchetti et al., 2020; Shrestha, Thapa, & Katuwal, 2020; Weinstein & Nguyen, 2020; Zhang & Ma, 2020). Later explorations have shown a general increase in loneliness during the pandemic (Dahlberg, 2021), although the pattern varies from country to country (Lieberoth et al., 2021). For example, in the UK, double the number of people reported depressive symptoms compared to 2019, and a majority of people with depressive symptoms reported feeling lonely often or always (Office for National Statistics, 2020). Further cross-cohort analyses found that people most at risk of loneliness were already socially vulnerable (Bu, Steptoe, & Fancourt, 2020).
While there was an initial expectation that older adults would experience a high degree of loneliness as a result of the pandemic, the evidence has been unclear. Population studies such as those of the ONS suggests no specific age-related effect, while others such as that by Dahlberg (2021) does suggest some specific effects on older adults. The lack of clarity is likely due to the complexity of age-related loneliness and the challenges in accurately capturing its effect. There is a need for a nuanced understanding of the ways in which ageing exposes people to certain vulnerabilities relating to isolation and how this impacts on loneliness over time. For example, it may be that older adults who had previously adapted well to living alone fared well under the COVID restrictions while those older people who were already lonely, unwell, or living with other restrictions on their freedom may be more vulnerable to intensification of loneliness (Hanna et al., 2021; Talbot & Briggs, 2021). More recent longitudinal evidence suggests that COVID-related restrictions among older adults do indeed predict loneliness and negative mental health effects in the longer-term (Mayerl, Stolz, & Freidl, 2021). However, much loneliness research has been cross-sectional, short-term, or atheoretical (Lim et al., 2020), meaning that the causes and effects of loneliness occasioned by epidemics or pandemics remains unclear (Dahlberg, 2021). Further, there are concerns that studies have underrepresented the oldest old, those not experiencing good health, and those not independently using the internet (Dahlberg, 2021).
How can the pandemic impact on loneliness?
Given the limitations of current evidence, we need theory on how the pandemic might create loneliness for some older people. Following Lim et al.‘s conceptual model of loneliness (2020), in Table 1 we set out what we expect are the main COVID-19 specific 1) triggers, 2) risk factors and correlates for loneliness, 3) how they combine to increase loneliness, and 4) the types of solutions that can be adapted to the pandemic - including digital technology.
Table 1.
The expected triggers, risk factors, and solutions for loneliness during the pandemic.
| Lim et al., 2020 map of loneliness aspects | Potential application to older people during COVID-19 pandemic |
|---|---|
| 1) Known triggers of loneliness (situation, environment) |
|
| 2) Risk factors and correlates that predispose people to loneliness or exacerbate it |
|
| 3) How triggers + risk factors (above) create/increase loneliness for older people |
|
| 4) Potential solutions for loneliness | Primary strategies older people tend to use (Kharicha, Manthorpe, Iliffe, Davies, & Walters, 2018):
|
As displayed in Table 1, the pandemic has several situational and correlational factors that will likely both cause increases in loneliness and complicate loneliness interventions. For many older people, mitigating loneliness is already challenged by the often-irreplaceable nature of lost social contacts in later stages of life (e.g., death of a spouse), feeling trapped at home alone if chronically ill (Bennet & Victor, 2012), and the effects of being left behind by digital technology (Coelho & Duarte, 2016; Lim et al., 2020). Combined with COVID-19 restrictions limiting older people's ability to engage in typical social activities, visit locations that alleviate loneliness (Schellekens & Lee, 2020), or access social services (Giebel et al., 2021), many established coping strategies are untenable. However, that is not to say that older adults are a homogenous group, there is considerable variation in people's cognitive, physical, and social health (Stone, Lin, Dannefer, & Kelley-Moore, 2017), and the ways in which older adults engage with digital technologies is equally varied (Hänninen, Taipale, & Luostari, 2021; Taipale & Hänninen, 2018). Instead, there are a range of risk factors in later life that may predispose some older adults to loneliness or exacerbate it. By facilitating social connection and providing access to meaningful activities, digital technologies hold potential to combat loneliness. While this may be true for the general population, older adults face unique barriers when accessing and using technologies. Below, we discuss these barriers and the opportunities of technologies for older people.
The need for technology-facilitated social connections
As identified in Table 1, the strategies used by older people to manage loneliness are a combination of: engaging with the social and physical world, cognitive coping strategies, and private strategies that they do not disclose to anyone (Kharicha et al., 2018). The pandemic has made the first strategy especially challenging. Some people have turned to the possibilities of the internet, and video technology in particular, to bridge social distances during the pandemic (Banskota, Healy, & Goldberg, 2020; Galea et al., 2020). However, there has been some discussion that video calls and other digital technologies have not been a panacea for pandemic-related loneliness because digital interventions are frequently considered to be ill-suited for older adults due to decreased internet access and lack of digital communication skills (Coelho & Duarte, 2016; Office for National Statistics, 2020). Moreover, while there is some evidence that older adults may have increased their usage of communicative technology, this may be linked to increased rather than decreased loneliness (Choi, Hammaker, DiNitto, & Marti, 2022; Holaday et al., 2021).
Some research on older people's experiences of using technology for social connections has found that they primarily use technology to maintain in-person relationships – for example, using messaging to make plans to meet, or video calls to check in on family who live far away (Liddle et al., 2021). Digital technology is reportedly less often used by older people to make new connections (Liddle et al., 2021). While online contact is generally not considered by older people to be a good replacement for face-to-face contact, it can enhance social connections by keeping people feeling connected even when they are apart, and potentially preserving connections and non-technology based ways of connection (Liddle et al., 2021), through providing ways of getting information or planning use of safer ways of gathering, including open spaces within neighbourhoods (Dahlberg, 2021). However, lonely people may be less likely to seek out contact – online or in person (Lim, Rodebaugh, Zyphur, & Gleeson, 2016; van Breen et al., 2020). Furthermore, there is mixed evidence as to whether online behaviour is caused by, or causes loneliness (Boursier, Gioia, Musetti, & Schimmenti, 2020; Lim et al., 2020; Morahan-Martin & Schumacher, 2003; Song et al., 2014; Çikrıkci, 2016). This means that digital loneliness interventions could potentially introduce risks to wellbeing. Gardiner, Geldenhuys, and Gott (2018) noted that many loneliness interventions have been implemented atheoretically (without deriving or testing formal hypotheses), and as a result have had mixed success, and could even cause detriments to wellbeing.
In this paper, we seek to advance a specific type of theoretical and evidence-based approach to designing digital loneliness interventions. We suggest a type of social facilitation intervention, in which the primary purpose is to facilitate social interactions in order to reduce loneliness, in distinction from, for example therapy, social, or technical skill development (Gardiner et al., 2018). Social facilitation is suited to the present crisis because older adults and their wider social networks and communities have had their social contacts and social capital diminished, thereby requiring collective intervention.
There are prior success cases in both introducing and training older adults in the use of digital social interventions (Blažun, Saranto, & Rissanen, 2012; Ibarra, Baez, Cernuzzi, & Casati, 2020). For example, Morton et al. (2018) trained older adults in technology use for social purposes, and found improved cognitive capacities in the trainees, supported by maintenance of self, improved self-competence, and increased social engagement. In part, the efficacy of the intervention derived from its ability to address the needs and vulnerabilities inherent in the ‘social identity’ of older adults. It sought to understand how the experiences of older adults were informed by their understandings of what it is to be a member of this social category. This and other studies which take the identity of older adult as its focus allow us to consider how loneliness may be understood and addressed as an identity-related phenomenon.
A social identity approach to loneliness intervention methodology
Several prominent theoretical approaches can apply to loneliness and social facilitation interventions. For instance, social network research enables the understanding of the role of network typologies and network structures in social capital and health and wellbeing outcomes including loneliness (Wenger, 1997). The strength of ties between network members, the long-standing-ness of the relationship, and pre-existing norms of support exchange between network members facilitates the transition of some members of a social network, into a support network for older adults (Keating, Otfinowski, Wenger, Fast, & Derksen, 2003; Peek & Lin, 1999). Interventions premised in social network theory are designed to bring together people with similar backgrounds, demographics, and localities (e.g. through befriending, support groups) (Lester, Mead, Graham, Gask, & Reilly, 2012; South et al., 2017).
In this paper we adopt a complementary theory for the purposes of designing a digital loneliness intervention - the Social Identity Approach to Health (SIAH, also referred to as “the social cure”, Haslam, Jetten, et al., 2018; Jetten et al., 2012, Jetten et al., 2020). SIAH is a socio-cognitive psychological theory that focusses on the internalisation of social identities associated with social network/group memberships, and the role these identities play in health and wellbeing, via feelings of resilience, meaning, and belonging.
A social identity is a way of defining ourselves that we share with others - for example, if my neighbour and I define ourselves as members of our local community, then we share a social identity and form part of a psychological group. A social interaction involving people who share a social identity will usually be experienced as more positive and meaningful compared to an interaction with an outgroup member (e.g., someone from another community), or member of a group you only weakly identify with (e.g., a community you live in but want to leave). The SIAH approach thus emphasises people's internal identities rather than their external social categories or shared characteristics that may not always be meaningful or desired (see Stuart, Stevenson, Koschate, Cohen, & Levine, 2022). Interventions premised on the SIAH target social cognitions and emotions and the role they play in loneliness, potentially enabling more positive social cognitions and social contact seeking behaviours (Haslam, Cruwys, et al., 2019).
Social identities are key to addressing a lack of social group-based belonging (social loneliness, Cacioppo et al., 2015). Group memberships provide individuals with a range of social and psychological resources that help them deal with the challenges they face in everyday life (Haslam, Jetten, & Waghorn, 2009). These include shared materials that enable them to readily gain access to required advice and support, which provides reassurance, reduces stress, and enhances feelings of being able to cope (Haslam, O’Brien, Jetten, Vormedal, & Penna, 2005). Sharing an identity also promotes openness, trust, giving support, and receiving support in the spirit in which it is given (Haslam, Reicher, & Levine, 2012). Groups also provide a shared worldview and imbue the social world with meaning. Together, the feelings of support, communication, and shared purpose typically contribute to an overall sense of belonging within the group.
In effect, the psychological resources provided by groups include (Haslam, Jetten, et al., 2018):
-
1.
Meaning - people who share an identity (inter)act more frequently and work towards outcomes together, imbuing meaning to what they do.
-
2.
Connection - psychological closeness to other people, such that they form part of our self or identity.
-
3.
Support - people who share an identity are more likely to help each other and perceive that support positively.
-
4.
Agency (control) - people who share an identity develop collective and personal agency in their lives.
According to the SIAH, the key to reducing/mitigating loneliness is to help people find and sustain the group memberships that provide these psychological resources of meaning, connection, support, and agency.
Moreover, it is better to belong to multiple groups, as this creates resilience, via an increased chance of positive effects from groups and less impact from the loss of one group membership (Haslam, Cruwys, Haslam, Dingle, & Chang, 2016; Iyer, Jetten, Tsivrikos, Postmes, & Haslam, 2009). For example, one longitudinal study found that the number of group memberships people possessed exerted a positive effect on quality of life over 4 months (and was sustained at 6–9 months), via a pathway from community belonging, to feeling socially supported, and in turn experiencing less loneliness (Wakefield et al., 2020).
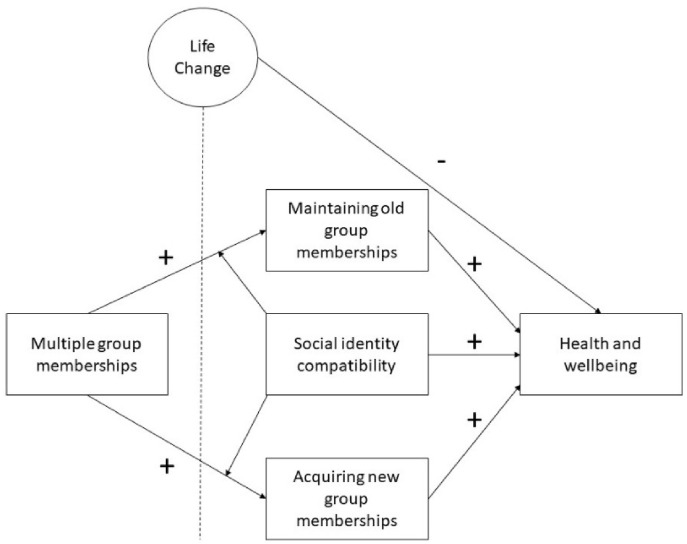
Having multiple group memberships to identify with can imbue wellbeing and reduce loneliness during life changes or traumatic events (such as this pandemic), as illustrated in the Social Identity Model of Identity Change, represented in Fig. 1 below (adapted from Haslam, Jetten, et al., 2018). Health and wellbeing (including reductions in loneliness) can be facilitated through multiple group memberships if those memberships are maintained through an otherwise aversive life change, or if people can use their existing group memberships to scaffold new group memberships (Haslam, Haslam, & Cruwys, 2019).
Fig. 1.
The Social Identity Model of Identity Change (SIMIC), adapted from Haslam, Jetten, et al., 2018.
For example, retirement is a life stage that can be detrimental to health and wellbeing for older adults as it involves the loss of a shared workplace identity (Haslam, Lam, et al., 2018; Haslam, Steffens, et al., 2019). However, health and wellbeing can be maintained if retired people either gain new group memberships (e.g. become a volunteer, take up a new social hobby), and/or continue to maintain other, existing group memberships (e.g. connections with family, friends, or social groups) (Haslam, Steffens, et al., 2019; Iyer et al., 2009; Steffens, Jetten, Haslam, Cruwys, & Haslam, 2016).
The current pandemic with its disruptions to normal daily routine and restrictions on social interactions appears analogous to life transition or crisis. Therefore, the SIAH provides a likely evidenced theoretical model for loneliness interventions during the pandemic. A key characteristic of this crisis, however, is that it is not just an individual life transition, it is simultaneously affecting older people's broader social networks, and resulting in social restrictions that impact upon people's ability to maintain or gain social identities. We will now elaborate on the wellbeing role of specific groups in an older individual's social network and establish the vulnerabilities to groups resulting from the pandemic.
Family. Family is arguably the most fundamental psychological group for the health and well-being of its members. Family identification is associated with lower depression, lower perceived stress and higher life satisfaction (Miller, Wakefield, & Sani, 2015; Sani, Herrera, Wakefield, Boroch, & Gulyas, 2012), and lower paranoid ideation (Sani, Wakefield, Herrera, & Zeybek, 2017). The ability of families to provide stress-reducing resources is especially pronounced in more family-oriented cultures (Acero, Cano-Prous, Castellanos, Martín-Lanas, & Canga-Armayor, 2017). The way in which families protect their members adheres closely to the “social cure” model: families can enhance well-being through participation and belonging. As Hanke, van Egmond, Crespo, and Boer (2016) demonstrate, family identity impacted well-being via increasing family belonging, which was in turn fostered by participation in family celebrations. In a qualitative meta-synthesis, Acero et al. (2017) show that, across a range of different social and cultural contexts, an individual family member falling ill promotes family solidarity, because the illness is experienced collectively by the whole family.
Friends. Friendships are important across the lifecycle in providing a source of companionship and support. The loneliness occasioned by a lack of friendship intimacy can be severe. However, from a “social cure” perspective, friendships are typically collective in nature, such that the basis on which they occur (age, gender, mutual interests, shared activities) often have a group dimension. Understanding this ‘peer’ dimension is key to ascertaining how friendships arise, how they give rise to group memberships and how they come to provide collective support and guide behaviour. For example, Weisz and Wood (2005) showed that perceptions that a new friend supported one's own identifications with social groups predicted the longevity and intimacy of friendships among college students. Networks comprised of voluntary friendships are associated with greater wellbeing than solely family-based support networks (Fiori, Antonucci, & Cortina, 2006, pp. P25–P32), and are enjoyable because they are based on similar interests and the quality of the relationships (Allan, 1986; Barker, 2002; Himes & Reidy, 2000; Lubben & Gironda, 2003).
Neighbours/communities. Much pandemic related media has focused on mobilising community groups and neighbourhoods (Galea et al., 2020; Marston, Renedo, & Miles, 2020; Wu, 2020). Neighbourhoods form another fundamentally meaningful group, providing both a social environment and a proximal cohort which shapes the everyday lives of residents (McNamara, Stevenson, & Muldoon, 2013). Neighbourhoods have been found to be important groups for coping with economic and social challenges (Elahi et al., 2018; Fong, Cruwys, Haslam, & Haslam, 2019; McNamara et al., 2013) as well as reducing loneliness (Kellezi et al., 2019; McNamara et al., 2021).
Professional supporters. The relationship between individuals and support services is also social identity-based depending on the degree to which the services are seen to form part of the ingroup or outgroup (Stevenson, McNamara, & Muldoon, 2014). Inequalities in healthcare access among vulnerable groups are often directly attributable to feelings of ‘stigmatisation’ whereby the clientele perceive that their group is perceived negatively by service providers. Stigma has been found to deter service use among excluded groups including those from ethnic minority communities (Campbell & McLean, 2002; Mclean, Campbell, & Cornish, 2003) and socially disadvantaged backgrounds (Fong, Wright, & Wimer, 2016; Warr, Davern, Mann, & Gunn, 2017). The stigma associated with mental illness has been found to deter people suffering from mental health complaints from seeking assistance (Ben-Zeev, Corrigan, Britt, & Langford, 2012, p.; Clement et al., 2015), specifically to avoid being labelled as mentally ill (Corrigan, 2004; Vogel, Wade, & Hackler, 2007). Similarly, the stigma associated with loneliness has also been found to deter service uptake.
Stigma has its effects on service use though corroding confidence, undermining the willingness of individuals to engage and resulting in mistrust, miscommunication and negative intergroup encounters (Andelic, Stevenson, & Feeney, 2019; Ekström, Lindström, & Karlsson, 2013). Conversely sharing a common social identity between service provider and user can reverse these effects and foster positive therapeutic relationships. Viewing staff as behaving in the interests of clients fosters openness, trust and adherence to advice (Stevenson et al., 2014).
The impacts on groups during the pandemic. To tackle loneliness and the social impacts of the pandemic in a systematic and reproducible manner we need to understand how the above groups have been impacted during the pandemic and employ theory-based technological design that can address the gaps and vulnerabilities that have been exposed. Most obviously, the strain placed on health services means that the availability of professional supporters and their ability to provide quality care has been markedly reduced (Hanna et al., 2021). Likewise, the ability of families and friends to maintain regular face-to-face contact has been diminished, especially in relation to cross-generational contact with non-cohabiting older relatives; the legacy of this reduced contact on loneliness is yet unclear (Dahlberg, 2021), but may have fractured relationships and resulted in chronic loneliness fears and cognitions (Harkin et al., unpublished). Neighbourhoods which may once have been the sites of social activities and frequent casual contact encounters have also largely been stripped of these functions. While some communities have strengthened local connections and engaged in cooperative behaviour, such as voluntary work, donations of food, and offering emotional support (Bowe et al., 2020; Wolf, Haddock, Manstead, & Maio, 2020), not all communities had the resources to do so (Jetten et al., 2020). Whilst some groups moved activities online during the pandemic, many ceased meeting and have not been able to resume activities. Impoverished communities facing structural inequality and discrimination have been left some neighbourhoods to fend for themselves (Templeton et al., 2020). Of note is the socio-economic status of neighbourhood which is associated with both lack of local amenities and stigmatisation of residents (as outlined in section 1, Table 1).
Therefore, the pandemic has diminished the ability of individuals to access the social and psychological resources afforded by their group memberships and many have been prevented from actively maintaining or gaining the group memberships necessary to cope with this fundamental social change. Through enhancing and enabling older people's connections with these different types of social groups (and potentially others not mentioned), digital interventions could counteract some of the negative impacts created by the shutdown of social activities and increased social isolation that has occurred and facilitate the capacity of groups to deliver psychological resources including connectedness, social support, meaning, and agency. We will next expand on what is needed in digital interventions.
Digital approaches for addressing loneliness
We have considered the serious impact of large-scale periods of isolation, as imposed during the pandemic, on loneliness. We proposed a theoretical approach to address the wellbeing of adversely affected older adults and their social groups. We now review digital technologies as loneliness interventions, design characteristics for effective digital interventions, and identify research challenges (including understanding and predicting loneliness trends, building for system adoption and continued use, and integrating theory and user centred design). This review allows us to locate relevant approaches for applying theory to digital loneliness interventions. In the final section of the paper, we will consolidate this work along with design guidelines – thereby building bridges between social/behavioural theory and HCI/information systems (Hekler, Klasnja, Froehlich, & Buman, 2013).
Digital technologies as loneliness interventions
Technology-supported loneliness intervention studies have utilised diverse technology-oriented approaches (Khosravi, Rezvani, & Wiewiora, 2016), from training older adults to use the internet, to interacting in forums and video calls (Neves, Franz, Munteanu, & Baecker, 2018), social networks (Pauly et al., 2019), online virtual classes (Isaacson, Cohen, & Shpigelman, 2019; Tomasino et al., 2017), and messaging (Ibarra et al., 2020). Most of the reported intervention studies used off-the-shelf solutions e.g., Facebook (Cotten, Ford, Ford, & Hale, 2014; Larsson, Padyab, Larsson-Lund, & Nilsson, 2016), Skype (Banbury et al., 2017), or WhatsApp (Jarvis, Chipps, & Padmanabhanunni, 2019).
Evidence for the efficacy of some digital loneliness interventions remains inconclusive particularly amongst older adults living in the community (Vines, Pritchard, Wright, Olivier, & Brittain, 2015; Waycott et al., 2014). Waycott has led several studies looking at social networking (e.g., Facebook) amongst lonely older adults, arguing that the results indicate success even amongst the oldest adults (albeit based on very low participation numbers) (Waycott et al., 2013). However, they also note that feelings loneliness can be exacerbated by unmet expectations about the social platform (Waycott, Wadley, Schutt, Stabolidis, & Lederman, 2015), with a conclusion that the technology itself has got to be a mechanism for connecting people to people, rather than as a solution or replacement for face to face contact (see also Liddle et al., 2021).
This reliance on off-the-shelf technical solutions could limit effectiveness as general technical solutions can be challenging to use for older people (Ibarra et al., 2020), and were not built for the right domain specific purpose - such as addressing loneliness or facilitating social support. Solutions that do not consider the unique needs and requirements of older people may even be detrimental for wellbeing, especially if they have complex or insufficient privacy controls and are not transparent in their processes (Coelho & Duarte, 2016; Shrewsbury, 2002).
In addition to studies trialling off-the-shelf solutions for loneliness, many custom-designed wellbeing digital platforms have been developed. Yet, there is also a lack of evidence regarding their effectiveness in improving mental health (Goodday et al., 2020). What the evidence does show to date is that a key criterion of effective technology-supported interventions is that they are designed with users, to facilitate ongoing participation in the intervention platform (Gulliksen et al., 2003; Shaw, Ellis, & Ziegler, 2018).
Design characteristics for effective digital interventions
While the evidence we have outlined is somewhat limited, some lessons have been learnt about designing apps to improve mental health. Chandrashekar (2018) has reviewed meta-studies of the use of apps for people with depression, anxiety and schizophrenia; the key design characteristics of effective apps include the importance of a simple user interface and the helpfulness of providing a small number of regular usage reminders. In an 8-week randomized trial of a suite of 13 mental health apps (Zhang et al., 2019) found that participants who engaged in self-tracking experienced reduced depression symptoms. In reviewing the behaviour of users, Zhang et al. found that there was not a direct relationship between amount/frequency of engagement and reductions in depression, highlighting that the digital platform or device does not need to repeatedly harass users to enter data; as long as they engage with the system, they will receive some form of benefit.
This principle is also evidenced in one of the most widely used apps in the area in the UK - True Colours; a digital tool for monitoring mood disorders. Used by over 36,000 individuals, it has formed part of 21 unique research and clinical service settings in the United Kingdom (Goodday et al., 2020). Reflecting on their experiences with the app, the authors note that the ability to prompt for input is an advantage that apps have over hard copy symptom monitoring diaries, but that this facility needs to be used with care. These design insights align with other work in the personal informatics domain (Choe, Lee, Kay, Pratt, & Kientz, 2015; Ferrario et al., 2017) which have argued for minimal user interactions with tracking systems to reduce the potentially high burden of manual tracking, which can lead to high attrition rates (Lazar, Koehler, Tanenbaum, & Nguyen, 2015).
In short, the design implications for digital loneliness interventions are to balance users’ needs against the burden that using a digital technology poses. Attrition from digital technologies including apps is often very high (Lazar et al., 2015). The challenge of technology adoption and continued use is one of the key challenges we discuss next.
Identified research challenges for digital loneliness interventions
Based on our review above of digital interventions for loneliness and mental health, we have identified some key challenges requiring further research and applied practice. These considerations would need to be addressed in future research applying our suggested Social Identity Approach to a digital loneliness intervention.
Understanding and predicting loneliness trends
In section one we noted that loneliness can fluctuate in intensity, duration, and frequency of episodes (Barreto et al., 2021). Detecting loneliness and predicting when loneliness is about to increase or decrease, could enable digital platforms – and their human users – to recognise meaningful trends, identify risk factors/correlates of loneliness, allocate resources where most needed, and optimize interventions. There has been some technical headway made in detecting loneliness, and changes in loneliness intensity, by employing machine learning techniques to detect loneliness through classification of collected naturally occurring data. Data have included user entered, and raw data from phones, including GPS data, screen time, call data, and message data (Doryab et al., 2019; Gao, Li, Zhu, Liu, & Liu, 2016), information about social media app usage (Pulekar & Agu, 2016), more detailed information about the type of calls and a limited number of daily activities (Sanchez, Martinez, Campos, Estrada, & Pelechano, 2015), or raw data collected by phones and smartwatches to capture daily activity patterns related to loneliness (Doryab, Frost, Faurholt-Jepsen, Kessing, & Bardram, 2015). Alternate approaches have employed machine learning to detect loneliness using questionnaire data, such as demographic information and health related information (Yang & Bath, 2018), or audio data, to analyse speech and recognise sentiment (Badal et al., 2020).
These previous studies in machine learning have not yet captured the progression of loneliness over time, or the comprehensive set of variables involved. Research is needed that addresses these variables over time to understand the progression of loneliness during and beyond the pandemic (Luchetti et al., 2020).
Given the need to overcome such design challenges it is crucial to have a methodological approach translating psychological theory into systems that adequately meet both system needs and the needs of the user. The next section discusses User Centred Design, an iterative approach for working with stakeholders to design useful, useable, and effective products.
Building for adoption and continued use
As we have argued, there are key design criteria that will help make a system engaging over the long-term. This includes designing such that people are willing to record their information, and that information is meaningfully used, with any results interpretable back to users. If users are not willing to adopt a system (particularly when they are not forced to use it), then the system cannot achieve efficacy. While engaging systems can lack efficacy, a system must be engaging enough to be used to be effective.
The technology acceptance and adoption literature emphasises many factors associated with technology adoption and continued use, including ease of use, technology attributes, agency/control, individual differences, and technology extraction and subtraction (Shaw et al., 2018). The latter is particularly novel because it centres on the relationship between humans and technology, and whether technology can help extend the person's self-identity or detriment it.
While initial adoption is essential, with systems designed to impact long-term conditions, such as loneliness, adoption is likely to be needed over months or potentially years to be effective. This requires people to see the technology as an extension of their self and fitting to their needs (Shaw et al., 2018). To make platforms engaging over the longer term requires public involvement, including the needs and requirements of a broad range of stakeholders (Coelho & Duarte, 2016; Mitton, Smith, Peacock, Evoy, & Abelson, 2009) – not only the older adult, but also their support network such as family, friends, healthcare workers, and other groups as described in section one.
Digital interventions also need to adapt to older users' needs over time to compensate for age related declines (Coelho & Duarte, 2016; Wagner, Hassanein, & Head, 2010), whilst gaining their involvement as active citizens in managing their health and wellbeing (Godfrey & Johnson, 2009Godfrey & Johnson, 2009). Older adults are frequently excluded in the design process and as a result not using health and wellbeing technology (Harrington, Wilcox, Connelly, Rogers, & Sanford, 2018).
User-Centred Design (UCD) is a useful methodology that emphasises key variables associated with technology adoption including ease of use, technology attributes such as simplicity, transparency of state, and clarity of purpose (Norman, 2013; Shaw et al., 2018). UCD provides a promising conceptual framework for the aforementioned digital design requirements. UCD asserts that users should be integrated into development, not just for their observations, but also as contributors of design ideas and solutions as user participation can help realize products that more accurately respond to user needs (Gulliksen et al., 2003). Furthermore, since new technologies can impact vital rights such as privacy and autonomy (Wright, 2011), it is critical that such issues be addressed during the development process to avoid harm to the user (Wright & Friedewald, 2013). UCD relies on iterative cycles of design, assessment, and improvement (Gulliksen et al., 2003), meaning that UCD tends to result in systems which users will more willingly engage (McCurdie et al., 2012). The challenge is how to integrate psychological theory with UCD.
Integration of theory into interface and interaction design
A theory driven approach helps understand how technology influences people's experiences and how users interpret the role of the technology in behaviour change processes (Hekler, Klasnja, Froehlich, & Buman, 2013). As described earlier, the Social Cure and the Social Identity Model of Identity Change (Haslam, Jetten, et al., 2018; Jetten et al., 2012) approach asserts the necessity of helping older people to adapt to life transitions and crises by engaging them in an active role of connecting with and adding to their social group memberships over time.
We have outlined the case for using user-centred design methods as key to the successful adoption, continued use, and efficacy of a digital loneliness intervention. But given that user-centred design methods work directly with users to gather their requirements, it is not clear how to integrate this work with psychological theory. The work of Hekler and colleagues (Hekler et al., 2013; Hekler, Klasnja, et al., 2016; Hekler, Michie, et al., 2016) suggests roadmaps for such integrative work.
In particular, Hekler, Michie, et al. (2016) suggest adopting an ‘agile’ approach to science, where small modular tests of hypotheses are executed through minimally viable software products that can be rapidly user tested and shared through open science outlets. Once support is obtained for these minimal viable products, they can be extended to consider variables ensuring continued use, so as to develop the longitudinal data needed in data analysis and prediction. Taking up this challenge offers many opportunities but also challenges, requiring knowledge of how to do ‘transdisciplinarity-in-the-small’ and relinquishing some of our disciplinary allegiances (Nuseibeh, 2022).
Conclusion, future research and design guidelines
In this paper, we reviewed evidence and theory on how a crisis such as the COVID-19 pandemic and individual factors might make some older people susceptible to loneliness, and furthermore, how typical methods of addressing loneliness are difficult under circumstances where face-to-face social interaction is limited or where support networks and services have been severely diminished. There are opportunities and challenges in understanding how digital interventions can supplement and empower people to enhance their social group memberships. We put forward an evidence-based theoretical model – the Social Identity Model of Identity Change - that illustrates how people can maintain wellbeing, and reduce/protect against loneliness, through maintaining or gaining multiple, important social group memberships during times of stressful change (Haslam, Jetten, et al., 2018). This approach is especially relevant to changes associated with ageing, which can be associated with loss of identity, and impoverished and fragile social connections (Jetten & Pachana, 2012; Victor & Bowling, 2012). We argued that the social identity approach should be integrated into a digital platform to design a social facilitation type of intervention for loneliness (Gardiner et al., 2018), which can empower older people and their social groups/networks to engage in maintaining or gaining multiple group memberships.
In the second section, we reviewed selected research on digital platforms and highlighted gaps in the suitability of existing platforms (either off the shelf or bespoke) for detecting and intervening in loneliness. These were, primarily: that current systems do not combine both detection and intervention in loneliness; there is a lack of longitudinal analysis of loneliness in all fields we reviewed; and that publicly available solutions (including social media platforms) are not domain specific or private, nor trustworthy. Our review of the HCI literature also raised pertinent design issues: ensuring that older people and their support networks are properly engaged in the design process, that an intervention is easy to use and not burdensome, and tested for efficacy in the domain intended (and not harmful). For this, user-centred design (UCD) methodologies are vital for understanding and accommodating older adults needs and the needs of their social groups/networks.
Psychological and behavioural science can be integrated with computer science disciplines to inform how to implement theory effectively, to develop design guidelines for similar technologies, and to drive further empirical research (Hekler et al., 2013; Waycott, Vetere, & Ozanne, 2019; Waycott & Vines, 2019). The next steps we suggest are in the form of both empirical research questions and design guidelines. While some of what we suggest is applicable to many types of digital social facilitation interventions, there are also some unique and yet to be explored possibilities based on the Social Identity Approach to Health and the Social Identity Model of Identity Change.
Future research suggestions
A social identity approach to a social facilitation style of digital intervention needs to facilitate personal reflection and the development of social goals or strategies through a group-level lens. Online ‘social identity mapping’ exercises can help people raise their awareness of their existing group-based social networks and resources as well as to set social goals and goals for joining or sustaining their group memberships (Bentley et al., 2020, in press). These digital interventions have not yet developed a consideration of the user-design principles needed to sustain adoption among users, including iterative design and testing of user interfaces. This is particularly pertinent for the older adult user group for whom technology usage is often experienced as an age-related threat and have been excluded from technology design (Harrington et al., 2018). Moreover, online identity mapping tools have been developed without a consideration of the benefits and challenges of making multiple groups simultaneously salient to the user – something known to increase psychological resilience, but also highlight tensions and incompatibility between groups (Iyer et al., 2009).
Methods for detecting or accommodating identity change or changes in loneliness, through data science/machine learning, could more fully realize the Social Identity Model of Identity Change (SIMIC) as a tool for digital intervention. Longitudinal machine learning techniques are currently insufficient for longitudinal detection or prediction of loneliness over time. The innovative development of such techniques could be used in adaptive software engineering to deliver micro-interventions for loneliness (Klasnja et al., 2015). For example, interventions for acute loneliness may need to be different to when loneliness is becoming chronic due to identity change or identity losses that are permanent. Such detection systems would require continued use by older adults and their social networks in longitudinal self-report, thus needing to provide value for use, such as self-reflective data (Isaacs et al., 2013; Pennebaker, 1997) or the ability for sharing self-report data with others in their support network, in a controlled and meaningful way (Kanis, Robben, & Kröse, 2015; Riva et al., 2016).
Further research is needed to explore how to balance individual agency, personal control, and empowerment of individuals (see Greenaway, Cruwys, Haslam, & Jetten, 2016; Haslam et al., 2016; Shaw et al., 2018), with sharing and connecting mechanisms. In particular, older people who are lonely (or who require greater solitude) need to feel empowered and in control of their social engagements (Stuart et al., 2022), including being able to keep some of their group memberships separate across multiple social domains (Stuart, Bandara, & Levine, 2019; Stuart & Levine, 2017). This would allow people to enact their different identities and roles within their group memberships, varying the levels of support they both give and receive from others as we have described - such as from family, friends, or professional healthcare relationships.
Additionally, the types of support that people pre-pandemic usually received from face-to-face groups can be partially replicated through online experiences, with some synchronous aspects, to maintain continuity to group membership during disruptions and to support with transitions between face to face and online experiences. Further research is required on how to make these online experiences sufficient and acceptable to users. We suggest iterative user-centred design methods combined with psychological theory could explore how to balance these needs. Commercial platforms have not typically provided accessible support and inclusive experiences – and in fact their reason for existing may be opaque and unacceptable to users.
Finally, we raise some points specific to addressing the societal inequalities that can give rise to loneliness in some older adults (e.g. discrimination, stigma, and lack of representation of cultural diversity, see Table 1). Inequality is a risk factor for loneliness and therefore something that needs to be more closely considered in a loneliness digital intervention. We also mentioned ageism during COVID-19, in that messages about health vulnerability were sometimes extended to include discriminatory age-based stereotypes (Previtali et al., 2020), which have the potential to undermine older adults self-worth and contribute to poorer wellbeing (Haslam, Cruwys, & Haslam, 2014). There are several ideas that could be carried forward in future research around applying the SIAH and SIMIC to address inequality and discrimination issues in the design of digital loneliness interventions. One idea is to create opportunities for older people to use digital technology to organise their own groups and engage in activism and awareness raising for social good. Another consideration is to promote agency for maintaining positive social identities. Technology that does not draw on the skills of older adults has a potential to reduce perceived agency and frame older adulthood within a negative aging stereotype (Barrie, La Rose, Detlor, Julien, & Serenko, 2021). Finally, groups of older adults with existing marginalised identities e.g. people living with chronic illness, may have a greater need for loneliness interventions as these characteristics can be loneliness risk factors. However, they can also have challenging barriers to interacting with digital interfaces, for example if they have mobility or motor control issues. Digital interventions for older adults need to be cognisant and design to adapt to these needs, in order to be suitable.
Design guidelines
Based on our review, we suggest these guidelines for a social facilitation digital intervention for loneliness reduction among older adults based on the Social Identity Approach to Health and multidisciplinary methods of research and design.
-
•
Design should be grounded in facilitating awareness of social groups, social goals, and strategies to enhancing collective or group activities.
-
•
Design needs to allow maintenance of multiple existing groups, ideally making multiple group memberships salient to the users.
-
•
Enable older adults to join/add new group memberships over time, to strengthen their social networks and provide resilience to social disruption or threats.
-
•
Enable self-report, active engagement with reporting and reflecting on identity, loneliness, and wellbeing.
-
•
Enable mutual social support mechanisms where they are desired (including both the giving and receiving of support) to enhance a feeling of reciprocity and self-worth.
-
•
Facilitate agency, by giving people control over their engagement and use of digital interventions. This also means giving people the option to separate groups from each other.
-
•
Help reduce the heightened social threat and anxiety accompanying chronic loneliness by supporting and scaffolding social interactions and enabling users to gradually build a positive sense of shared identity with new contacts.
-
•
Ensure that the intervention is non-stigmatising, and non-detrimental to wellbeing by heeding human rights principles in the development and deployment of the intervention, including consideration of accountability, equality, non-discrimination, accessibility and availability (Australian Rights Commission, 2021).
-
•
Create opportunities for older people to use digital technology to organise their own groups and engage in activism and awareness raising for social good, which could enhance agency and work towards reducing stigma (Liddle et al., 2021) and rebuilding communities after COVID-19.
-
•
Design must manage the burden of use that can be created by technology by using an interface suitable to older adults, and nudging reminders that suit the schedule and levels of technology use of older people.
Conclusion
We have argued that there is a need for theoretically driven methods for tackling COVID-19 related loneliness with digital interventions; this need will extend beyond the pandemic, due the social and economic ramifications resulting. We have suggested the Social Identity Approach to Health because of the need to target cognitive and emotional effects of loneliness and the detriments caused to community and social groups during the pandemic. The Social Identity Model of Identity Change (SIMIC) offers both explanation of older adults' experiences of loss and loneliness, as well as insight into intervention for older adults experiencing these stressful life transitions. By employing multidisciplinary methodologies, researchers can combine psychology/behavioural theory, machine learning methods for advanced data analysis, and user-centred technology for designing a useable, engaging, and effective digital loneliness intervention. Testing such digital interventions requires engaging with factors predicting technology adoption and continued use so as to collect the longitudinal data necessary to complete a feedback loop to theory verification and generalisation (see Hekler et al., 2013). Filling in this theory-application loop would ensure that the vulnerabilities in older people's social networks that have been exposed by the pandemic can be holistically addressed, and that the true opportunities of digital interventions for reducing social isolation and loneliness can be realised.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
This work was funded by: UK Engineering and Physical Sciences Research Council (EP/V027263/1, EP/R013144/1), Science Foundation Ireland (SFI 13/RC/2094, 16/SP/3804, 20/COV/0133), Australian Research Council, Centre of Excellence for the Dynamics of Language (CE140100041).
References
- Acero Á.R., Cano‐Prous A., Castellanos G., Martín‐Lanas R., Canga‐Armayor A. Family identity and severe mental illness: A thematic synthesis of qualitative studies. European Journal of Social Psychology. 2017;47(5):611–627. doi: 10.1002/ejsp.2240. [DOI] [Google Scholar]
- Allan G. Friendship and care for elderly people. Ageing and Society. 1986;6(1):1–12. [Google Scholar]
- Andelic N., Stevenson C., Feeney A. Managing a moral identity in debt advice conversations. British Journal of Social Psychology. 2019;58(3):630–648. doi: 10.1111/bjso.12303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badal V.D., Graham S.A., Depp C.A., Shinkawa K., Yamada Y., Palinkas L.A., et al. Prediction of loneliness in older adults using natural language processing: Exploring sex differences in speech. American Journal of Geriatric Psychiatry. 2020 doi: 10.1016/j.jagp.2020.09.009. S1064748120304796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banbury A., Chamberlain D., Nancarrow S., Dart J., Gray L., Parkinson L. Can videoconferencing affect older people's engagement and perception of their social support in long-term conditions management: A social network analysis from the telehealth literacy project. Health and Social Care in the Community. 2017;25(3):938–950. doi: 10.1111/hsc.12382. [DOI] [PubMed] [Google Scholar]
- Banerjee D., Rai M. Social isolation in Covid-19: The impact of loneliness. International Journal of Social Psychiatry. 2020 doi: 10.1177/0020764020922269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banskota S., Healy M., Goldberg E. 15 smartphone apps for older adults to use while in isolation during the COVID-19 pandemic. Western Journal of Emergency Medicine. 2020;21(3) doi: 10.5811/westjem.2020.4.47372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barke J. Community-based research and approaches to loneliness prevention. Working with Older People. 2017;21(2):115–123. doi: 10.1108/WWOP-10-2016-0032. [DOI] [Google Scholar]
- Barker J.C. Neighbors, friends, and other nonkin caregivers of community-living dependent elders. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2002;57(3):S158–S167. doi: 10.1093/geronb/57.3.s158. [DOI] [PubMed] [Google Scholar]
- Barreto M., Victor C., Hammond C., Eccles A., Richins M.T., Qualter P. Loneliness around the world: Age, gender, and cultural differences in loneliness. Personality and Individual Differences. 2021;169 doi: 10.1016/j.paid.2020.110066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrie H., La Rose T., Detlor B., Julien H., Serenko A. Because I'm old”: The role of ageism in older adults' experiences of digital literacy training in public libraries. Journal of Technology in Human Services. 2021;39(4):379–404. [Google Scholar]
- Ben-Zeev D., Corrigan P.W., Britt T.W., Langford L. Stigma of mental illness and service use in the military. Journal of Mental Health. 2012;21(3):264–273. doi: 10.3109/09638237.2011.621468. [DOI] [PubMed] [Google Scholar]
- Bennet K.M., Victor C. ’He wasn't in that chair’: What loneliness means to widowed older people. International Journal of Ageing and Later Life. 2012;7(1):33–52. doi: 10.3384/ijal.1652-8670.127133. [DOI] [Google Scholar]
- Bentley S.V., Greenaway K.H., Haslam S.A., Cruwys T., Steffens N.K., Haslam C., et al. Social identity mapping online. Journal of Personality and Social Psychology. 2020;118(2):213–241. doi: 10.1037/pspa0000174. [DOI] [PubMed] [Google Scholar]
- Bentley S.V., Haslam C., Haslam S.A., Jetten J., Larwood J., La Rue C.J. Groups 2 connect: An online activity to maintain social connection and well-being during COVID-19. Applied Psychology: Health and Well-Being. (in press) [DOI] [PubMed]
- Blažun H., Saranto K., Rissanen S. Impact of computer training courses on reduction of loneliness of older people in Finland and Slovenia. Computers in Human Behavior. 2012;28(4):1202–1212. doi: 10.1016/j.chb.2012.02.004. [DOI] [Google Scholar]
- Boursier V., Gioia F., Musetti A., Schimmenti A. Facing loneliness and anxiety during the COVID-19 isolation: The role of excessive social media use in a sample of Italian adults. Frontiers in Psychiatry. 2020;11:586222. doi: 10.3389/fpsyt.2020.586222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowe M., Gray D., Stevenson C., McNamara N., Wakefield J.R.H., Kellezi B., et al. A social cure in the community: A mixed-method exploration of the role of social identity in the experiences and well-being of community volunteers. European Journal of Social Psychology. 2020;50(7):1523–1539. doi: 10.1002/ejsp.2706. [DOI] [Google Scholar]
- van Breen J., Kutlaca M., Koc Y., Jeronimus B., Reitsema A.M., Jovanović V., et al. 2020. Lockdown lives: A longitudinal study of inter-relationships amongst feelings of loneliness, social contacts and solidarity during the COVID-19 lockdown in early 2020. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu F., Steptoe A., Fancourt D. Who is lonely in lockdown? Cross-cohort analyses of predictors of loneliness before and during the COVID-19 pandemic. Public Health. 2020;186:31. doi: 10.1016/j.puhe.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo S., Grippo A.J., London S., Goossens L., Cacioppo J.T. Loneliness: Clinical import and interventions. Perspectives on Psychological Science. 2015;10(2):238–249. doi: 10.1177/1745691615570616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo J.T., Hawkley L.C. Perceived social isolation and cognition. Trends in Cognitive Sciences. 2009;13(10):447–454. doi: 10.1016/j.tics.2009.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell C., McLean C. Ethnic identities, social capital and health inequalities: Factors shaping African-Caribbean participation in local community networks in the UK. Social Science & Medicine. 2002;55(4):643–657. doi: 10.1016/S0277-9536(01)00193-9. [DOI] [PubMed] [Google Scholar]
- Cava M.A., et al. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nursing. 2005;22(5):398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [DOI] [PubMed] [Google Scholar]
- Chandrashekar P. Do mental health mobile apps work: Evidence and recommendations for designing high-efficacy mental health mobile apps. mHealth. 2018;4 doi: 10.21037/mhealth.2018.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang E.C., Sanna L.J., Hirsch J.K., Jeglic E.L. Loneliness and negative life events as predictors of hopelessness and suicidal behaviors in hispanics: Evidence for a diathesis-stress model. Journal of Clinical Psychology. 2010;66(12):1242–1253. doi: 10.1002/jclp.20721. [DOI] [PubMed] [Google Scholar]
- Choe E.K., Lee B., Kay M., Pratt W., Kientz J.A. Proceedings of the 2015 ACM international joint conference on pervasive and ubiquitous computing. 2015. SleepTight: Low-burden, self-monitoring technology for capturing and reflecting on sleep behaviors; pp. 121–132. [DOI] [Google Scholar]
- Choi N.G., Hammaker S., DiNitto D.M., Marti C.N. COVID-19 and loneliness among older adults: Associations with mode of family/friend contacts and social participation. Clinical Gerontologist. 2022:1–13. doi: 10.1080/07317115.2021.2013383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Çikrıkci Ö. The effect of internet use on well-being: Meta-analysis. Computers in Human Behavior. 2016;65:560–566. doi: 10.1016/j.chb.2016.09.021. [DOI] [Google Scholar]
- Clement S., Schauman O., Graham T., Maggioni F., Evans-Lacko S., Bezborodovs N., et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychological Medicine. 2015;45(1):11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- Coelho J., Duarte C. A literature survey on older adults' use of social network services and social applications. Computers in Human Behavior. 2016;58:187–205. doi: 10.1016/j.chb.2015.12.053. [DOI] [Google Scholar]
- Cohen-Mansfield J. COVID-19 and older adults in Israel—common challenges and recommendations. Quality in Ageing and Older Adults. 2020;21(4, SI):209–216. doi: 10.1108/QAOA-09-2020-0043. [DOI] [Google Scholar]
- Corrigan P. How stigma interferes with mental health care. American Psychologist. 2004;59(7):614–625. doi: 10.1037/0003-066X.59.7.614. [DOI] [PubMed] [Google Scholar]
- Cotten S.R., Ford G., Ford S., Hale T.M. Internet use and depression among retired older adults in the United States: A longitudinal analysis. Journal of Gerontology: Serie Bibliographique. 2014;69(5):763–771. doi: 10.1093/geronb/gbu018. [DOI] [PubMed] [Google Scholar]
- Dahlberg L. Loneliness during the COVID-19 pandemic. Aging & Mental Health. 2021;25(7):1161–1164. doi: 10.1080/13607863.2021.1875195. [DOI] [PubMed] [Google Scholar]
- De Biase S., Cook L., Skelton D.A., Witham M., ten Hove R. The COVID-19 rehabilitation pandemic. Age and Ageing. 2020;49(5):696–700. doi: 10.1093/ageing/afaa118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Digiovanni C., et al. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science. 2004;3(4):265–272. doi: 10.1089/bsp.2004.2.26510.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- Doryab A., Frost M., Faurholt-Jepsen M., Kessing L.V., Bardram J.E. Impact factor analysis: Combining prediction with parameter ranking to reveal the impact of behavior on health outcome. Personal and Ubiquitous Computing. 2015;11 [Google Scholar]
- Doryab A., Villalba D.K., Chikersal P., Dutcher J.M., Tumminia M., Liu X., et al. Identifying behavioral phenotypes of loneliness and social isolation with passive sensing: Statistical analysis, data mining and machine learning of smartphone and fitbit data. JMIR MHealth and UHealth. 2019;7(7) doi: 10.2196/13209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eden P., Shannon S., Thomas M. MinterEllison; 2020. COVID-19 in aged care: A human rights approach.https://www.minterellison.com/articles/covid-19-in-aged-care-a-human-rights-approach [Google Scholar]
- Ehni H.-J., Wahl H.-W. Six propositions against ageism in the COVID-19 pandemic. Journal of Aging & Social Policy. 2020:1–11. doi: 10.1080/08959420.2020.1770032. [DOI] [PubMed] [Google Scholar]
- Ekström M., Lindström A., Karlsson S. Managing troubles-talk in the renegotiation of a loan contract. Discourse Studies. 2013;15(4):371–394. doi: 10.1177/1461445613483038. [DOI] [Google Scholar]
- El-Zoghby S.M., Soltan E.M., Salama H.M. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. Journal of Community Health. 2020;45(4):689–695. doi: 10.1007/s10900-020-00853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elahi A., McIntyre J.C., Hampson C., Bodycote H.J., Sitko K., White R.G., et al. Home is where you hang your hat: Host town identity, but not hometown identity, protects against mental health symptoms associated with financial stress. Journal of Social and Clinical Psychology. 2018;37(3):159–181. doi: 10.1521/jscp.2018.37.3.159. [DOI] [Google Scholar]
- Ferrario M.A., Simm W., Gradinar A., Forshaw S., Smith M.T., Lee T., et al. Computing and mental health: Intentionality and reflection at the click of a button. Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare. 2017:1–10. doi: 10.1145/3154862.3154877. [DOI] [Google Scholar]
- Fiori K.L., Antonucci T.C., Cortina K.S. Social network typologies and mental health among older adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2006;61(1):P25–P32. doi: 10.1093/geronb/61.1.p25. [DOI] [PubMed] [Google Scholar]
- Fokkema T., De Jong Gierveld J., Dykstra P.A. Cross-national differences in older adult loneliness. Journal of Psychology. 2012;146(1–2):201–228. doi: 10.1080/00223980.2011.631612. [DOI] [PubMed] [Google Scholar]
- Fong P., Cruwys T., Haslam C., Haslam S.A. Neighbourhood identification and mental health: How social identification moderates the relationship between socioeconomic disadvantage and health. Journal of Environmental Psychology. 2019;61:101–114. doi: 10.1016/j.jenvp.2018.12.006. [DOI] [Google Scholar]
- Fong K., Wright R.A., Wimer C. The cost of free assistance: Why low-income individuals do not access food pantries. Journal of Sociology & Social Welfare. 2016;43(1):71–94. [Google Scholar]
- Galea S., Merchant R.M., Lurie N. The mental health consequences of COVID-19 and physical distancing: The need for prevention and early intervention. JAMA Internal Medicine. 2020;180(6):817–818. doi: 10.1001/jamainternmed.2020.1562. [DOI] [PubMed] [Google Scholar]
- Gao Y., Li A., Zhu T., Liu X., Liu X. How smartphone usage correlates with social anxiety and loneliness. PeerJ. 2016;4 doi: 10.7717/peerj.2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner C., Geldenhuys G., Gott M. Interventions to reduce social isolation and loneliness among older people: An integrative review. Health and Social Care in the Community. 2018;26(2) doi: 10.1111/hsc.12367. https://onlinelibrary.wiley.com/doi/full/10.1111/hsc.12367 [DOI] [PubMed] [Google Scholar]
- Giebel C., Lord K., Cooper C., Shenton J., Cannon J., Pulford D., et al. A UK survey of COVID-19 related social support closures and their effects on older people, people with dementia, and carers. International Journal of Geriatric Psychiatry. 2021;36(3):393–402. doi: 10.1002/gps.5434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godfrey M., Johnson O. Digital circles of support: Meeting the information needs of older people. Computers in Human Behavior. 2009;25(3):633–642. [Google Scholar]
- Gonyea J.G., Curley A., Melekis K., Levine N., Lee Y. Loneliness and depression among older adults in urban subsidized housing. Journal of Aging and Health. 2018;30(3):458–474. doi: 10.1177/0898264316682908. [DOI] [PubMed] [Google Scholar]
- Goodday S.M., Atkinson L., Goodwin G., Saunders K., South M., Mackay C., et al. The true colours remote symptom monitoring system: A decade of evolution. Journal of Medical Internet Research. 2020;22(1):e15188. doi: 10.2196/15188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenaway K.H., Cruwys T., Haslam S.A., Jetten J. Social identities promote well‐being because they satisfy global psychological needs. European Journal of Social Psychology. 2016;46(3):294–307. [Google Scholar]
- Gulliksen J., Göransson B., Boivie I., Blomkvist S., Persson J., Cajander Å. Key principles for user-centred systems design. Behaviour & Information Technology. 2003;22(6):397–409. doi: 10.1080/01449290310001624329. [DOI] [Google Scholar]
- Hanke K., van Egmond M.C., Crespo C., Boer D. Blessing or burden? The role of appraisal for family rituals and flourishing among LGBT adults. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 2016;30(5):562–568. doi: 10.1037/fam0000214. [DOI] [PubMed] [Google Scholar]
- Hanna K., Giebel C., Tetlow H., Ward K., Shenton J., Cannon J., et al. Emotional and mental wellbeing following COVID-19 public health measures on people living with dementia and carers. Journal of Geriatric Psychiatry and Neurology. 2021 doi: 10.1177/0891988721996816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hänninen R., Taipale S., Luostari R. Exploring heterogeneous ICT use among older adults: The warm experts' perspective. New Media & Society. 2021;23(6):1584–1601. https://doi.org/10.1177.2F1461444820917353. [Google Scholar]
- Harkin, L., Stuart, A., Stevenson, C., Daly, R., Park, M. S.-A., Katz, D., Sanderson, L., Gooch, D., Levine, M., & Price, B. (unpublished). Being cut off from social identity resources has shaped loneliness during the COVID-19 pandemic: A longitudinal interview study with medically vulnerable older adults from the United Kingdom [Preprint]. PsyArXiv. https://doi.org/10.31234/osf.io/rhf32.
- Harrington C.N., Wilcox L., Connelly K., Rogers W., Sanford J. Proceedings of the 12th EAI international conference on pervasive computing technologies for healthcare. 2018. Designing health and fitness apps with older adults: Examining the value of experience-based Co-design; pp. 15–24. [DOI] [Google Scholar]
- Haslam C., Cruwys T., Chang M.X.-L., Bentley S.V., Haslam S.A., Dingle G.A., et al. GROUPS 4 HEALTH reduces loneliness and social anxiety in adults with psychological distress: Findings from a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2019;87(9):787. doi: 10.1037/ccp0000427. [DOI] [PubMed] [Google Scholar]
- Haslam C., Steffens N.K., Branscombe N.R., Haslam S.A., Cruwys T., Lam B.C.P., et al. The importance of social groups for retirement adjustment: Evidence, application, and policy implications of the social identity model of identity change. Social Issues and Policy Review. 2019;13(1):93–124. doi: 10.1111/sipr.12049. [DOI] [Google Scholar]
- Haslam C., Haslam S.A., Cruwys T. In: Social scaffolding: Applying the lessons of contemporary social science to health and healthcare. Williams R., Kemp V., Alexander Haslam S., Haslam C., Bhui K.S., Bailey S., editors. Cambridge University Press; 2019. Social scaffolding: Supporting the development of positive social identities and agency in communities; p. 244. [Google Scholar]
- Haslam C., Cruwys T., Haslam S.A. The we's have it”: Evidence for the distinctive benefits of group engagement in enhancing cognitive health in aging. Social Science & Medicine. 2014;120:57–66. doi: 10.1016/j.socscimed.2014.08.037. [DOI] [PubMed] [Google Scholar]
- Haslam C., Cruwys T., Haslam S.A., Dingle G., Chang M.X.-L. Groups 4 Health: Evidence that a social-identity intervention that builds and strengthens social group membership improves mental health. Journal of Affective Disorders. 2016;194:188–195. doi: 10.1016/j.jad.2016.01.010. [DOI] [PubMed] [Google Scholar]
- Haslam C., Jetten J., Cruwys T., Dingle G., Haslam S.A. Routledge; 2018. The new psychology of health: Unlocking the social cure. [Google Scholar]
- Haslam S.A., Jetten J., Waghorn C. Social identification, stress and citizenship in teams: A five-phase longitudinal study. Stress and Health. 2009;25(1):21–30. doi: 10.1002/smi.1221. [DOI] [Google Scholar]
- Haslam S.A., O'Brien A., Jetten J., Vormedal K., Penna S. Taking the strain: Social identity, social support, and the experience of stress. British Journal of Social Psychology. 2005;44(3) doi: 10.1348/014466605X37468. [DOI] [PubMed] [Google Scholar]
- Haslam S.A., Reicher S.D., Levine M. In: The social cure: Identity, health and well-being. Jetten J., Haslam C., Haslam S.A., editors. Psychology Press; 2012. When other people are heaven, when other people are hell: How social identity determines the nature and impact of social support; pp. 157–174. [Google Scholar]
- Hauge S., Kirkevold M. Variations in older persons' descriptions of the burden of loneliness. Scandinavian Journal of Caring Sciences. 2012;26:553–560. doi: 10.1111/j.1471-6712.2011.00965.x. [DOI] [PubMed] [Google Scholar]
- Hawkley L.C., Cacioppo J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Annals of Behavioral Medicine. 2010;40(2):218–227. doi: 10.1007/s12160-010-9210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hebblethwaite S., Young L., Martin Rubio T. Pandemic precarity: Aging and social engagement. Leisure Sciences. 2020:1–7. doi: 10.1080/01490400.2020.1773998. [DOI] [Google Scholar]
- Heinrich L.M., Gullone E. The clinical significance of loneliness: A literature review. Clinical Psychology Review. 2006;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Hekler E.B., Klasnja P., Froehlich J.E., Buman M.P. Mind the theoretical gap: Interpreting, using, and developing behavioral theory in HCI research. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2013:3307–3316. doi: 10.1145/2470654.2466452. [DOI] [Google Scholar]
- Hekler E.B., Klasnja P., Froehlich J.E., Buman M.P. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2013. Mind the theoretical gap: Interpreting, using, and developing behavioral theory in HCI research; pp. 3307–3316. [DOI] [Google Scholar]
- Hekler E.B., Klasnja P., Riley W.T., Buman M.P., Huberty J., Rivera D.E., et al. Agile science: Creating useful products for behavior change in the real world. Translational Behavioral Medicine. 2016;6(2):317–328. doi: 10.1007/s13142-016-0395-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hekler E.B., Michie S., Pavel M., Rivera D.E., Collins L.M., Jimison H.B., et al. Advancing models and theories for digital behavior change interventions. American Journal of Preventive Medicine. 2016;51(5):825–832. doi: 10.1016/j.amepre.2016.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himes C.L., Reidy E.B. The role of friends in caregiving. Research on Aging. 2000;22(4):315–336. doi: 10.1177/0164027500224001. [DOI] [Google Scholar]
- Holaday L.W., Oladele C.R., Miller S.M., Dueñas M.I., Roy B., Ross J.S. Loneliness, sadness, and feelings of social disconnection in older adults during the COVID‐19 pandemic. Journal of the American Geriatrics Society. 2021 doi: 10.1111/jgs.17599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: A meta-analytic review. Perspectives on Psychological Science. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Human rights and technology final report. Australian Human Rights Commission; 2021. https://humanrights.gov.au/our-work/rights-and-freedoms/publications/human-rights-and-technology-final-report-2021 [Google Scholar]
- Ibarra F., Baez M., Cernuzzi L., Casati F. A systematic review on technology-supported interventions to improve old-age social wellbeing: Loneliness, social isolation, and connectedness. Journal of Healthcare Engineering. 2020:1–14. doi: 10.1155/2020/2036842. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Isaacs E., Konrad A., Walendowski A., Lennig T., Hollis V., Whittaker S. Echoes from the past: How technology mediated reflection improves well-being. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2013:1071–1080. doi: 10.1145/2470654.2466137. [DOI] [Google Scholar]
- Isaacson M., Cohen I., Shpigelman C.N. 3rd IET international conference on technologies for active and assisted living (TechAAL 2019) 2019. Leveraging emotional wellbeing and social engagement of the oldest old by using advanced communication technologies: A pilot study using uniper-care’s technology. 5 (5 pp.)-5 (5 pp.) [DOI] [Google Scholar]
- Iyer A., Jetten J., Tsivrikos D., Postmes T., Haslam S.A. The more (and the more compatible) the merrier: Multiple group memberships and identity compatibility as predictors of adjustment after life transitions. British Journal of Social Psychology. 2009;48(4):707–733. doi: 10.1348/014466608X397628. [DOI] [PubMed] [Google Scholar]
- Jarvis M.A., Chipps J., Padmanabhanunni A. This phone saved my life”: Older persons' experiences and appraisals of an mHealth intervention aimed at addressing loneliness. Journal of Psychology in Africa. 2019;29(2):159–166. doi: 10.1080/14330237.2019.1594650. [DOI] [Google Scholar]
- Jetten J., Haslam C., Haslam S.A. Psychology Press; 2012. The social cure: Identity, health and well-being. [Google Scholar]
- Jetten J., Pachana N. The social cure: Identity, health and well-being. Psychology Press; 2012. Not wanting to grow old: A social identity model of identity change (SIMIC) analysis of driving cessation among older adults; pp. 97–113. [Google Scholar]
- Jetten J., Reicher S.D., Haslam S.A., Cruwys T. SAGE Publications Limited; 2020. Together apart: The psychology of Covid-19. [Google Scholar]
- Kanis M., Robben S., Kröse B. In: Human behavior understanding. Salah A.A., Kröse B.J.A., Cook D.J., editors. Springer International Publishing; 2015. How are you doing? Enabling older adults to enrich sensor data with subjective input; pp. 39–51. [DOI] [Google Scholar]
- Keating N., Otfinowski P., Wenger C., Fast J., Derksen L. Understanding the caring capacity of informal networks of frail seniors: A case for care networks. Ageing and Society. 2003;23(1):115–127. [Google Scholar]
- Kellezi B., Wakefield J.R.H., Stevenson C., McNamara N., Mair E., Bowe M., et al. The social cure of social prescribing: A mixed-methods study on the benefits of social connectedness on quality and effectiveness of care provision. BMJ Open. 2019;9(11) doi: 10.1136/bmjopen-2019-033137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kharicha K., Manthorpe J., Iliffe S., Davies N., Walters K. Strategies employed by older people to manage loneliness: Systematic review of qualitative studies and model development. International Psychogeriatrics. 2018;30(12):1767–1781. doi: 10.1017/S1041610218000339. [DOI] [PubMed] [Google Scholar]
- Khosravi P., Rezvani A., Wiewiora A. The impact of technology on older adults' social isolation. Computers in Human Behavior. 2016;63:594–603. doi: 10.1016/j.chb.2016.05.092. [DOI] [Google Scholar]
- Klasnja P., Hekler E.B., Shiffman S., Boruvka A., Almirall D., Tewari A., et al. Microrandomized trials: An experimental design for developing just-in-time adaptive interventions. Health Psychology. 2015;34(Suppl):1220–1228. doi: 10.1037/hea0000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein E. Vox; 2020. Coronavirus will also cause a loneliness epidemic.https://www.vox.com/2020/3/12/21173938/coronavirus-covid-19-social-distancing-elderly-epidemic-isolation-quarantine [Google Scholar]
- Kuyper L., Fokkema T. Loneliness among older lesbian, gay, and bisexual adults: The role of minority stress. Archives of Sexual Behavior. 2010;39(5):1171–1180. doi: 10.1007/s10508-009-9513-7. [DOI] [PubMed] [Google Scholar]
- Larsson E., Padyab M., Larsson-Lund M., Nilsson I. Effects of a social internet-based intervention programme for older adults: An explorative randomised crossover study. British Journal of Occupational Therapy. 2016;79(10):629–636. doi: 10.1177/0308022616641701. [DOI] [Google Scholar]
- Lazar A., Koehler C., Tanenbaum T.J., Nguyen D.H. Proceedings of the 2015 ACM international joint conference on pervasive and ubiquitous computing. 2015. Why we use and abandon smart devices; pp. 635–646. [DOI] [Google Scholar]
- Lester H., Mead N., Graham C.C., Gask L., Reilly S. An exploration of the value and mechanisms of befriending for older adults in England. Ageing and Society. 2012;32(2):307–328. doi: 10.1017/S0144686X11000353. [DOI] [Google Scholar]
- Liddle J., Stuart A., Worthy P., Levine M., Kastelle T., Wiles J., et al. Building the threads of connection that we already have”: The nature of connections via technology for older people. Clinical Gerontologist. 2021;44(4):406–417. doi: 10.1080/07317115.2020.1852638. [DOI] [PubMed] [Google Scholar]
- Lieberoth A., Lin S.-Y., Stöckli S., Han H., Kowal M., Gelpi R., et al. Stress and worry in the 2020 coronavirus pandemic: Relationships to trust and compliance with preventive measures across 48 countries in the COVIDiSTRESS global survey. Royal Society Open Science. 2021;8(2):200589. doi: 10.1098/rsos.200589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim M.H., Eres R., Vasan S. Understanding loneliness in the twenty-first century: An update on correlates, risk factors, and potential solutions. Social Psychiatry and Psychiatric Epidemiology. 2020;55(7):793–810. doi: 10.1007/s00127-020-01889-7. [DOI] [PubMed] [Google Scholar]
- Lim M.H., Rodebaugh T.L., Zyphur M.J., Gleeson J.F.M. Loneliness over time: The crucial role of social anxiety. Journal of Abnormal Psychology. 2016;125(5):620–630. doi: 10.1037/abn0000162. [DOI] [PubMed] [Google Scholar]
- Lorito C.D., Masud T., Gladman J., Godfrey M., Dunlop M., Harwood R.H. Deconditioning in people living with dementia during the COVID-19 pandemic: Findings from the promoting activity, independence and stability in early dementia (PrAISED) process evaluation. medRxiv. 2020 doi: 10.1101/2020.11.16.20231100. 2020.11.16.20231100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubben J., Gironda M. Centrality of social ties to the health and well-being of older adults. Social Work and Health Care in an Aging Society. 2003:319–350. [Google Scholar]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., et al. The trajectory of loneliness in response to COVID-19. American Psychologist. 2020;75(7):897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo Y., Hawkley L.C., Waite L.J., Cacioppo J.T. Loneliness, health, and mortality in old age: A national longitudinal study. Social Science & Medicine. 2012;74(6):907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marston C., Renedo A., Miles S. Community participation is crucial in a pandemic. The Lancet. 2020;395(10238):1676–1678. doi: 10.1016/s0140-6736(20)31054-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: Lessons learned. Philosophical Transactions of the Royal Society of London Series B Biological Sciences. 2004;359(1447):1117–1125. doi: 10.1098/rstb.2004.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayerl H., Stolz E., Freidl W. Longitudinal effects of COVID-19-related loneliness on symptoms of mental distress among older adults in Austria. Public Health. 2021;200:56–58. doi: 10.1016/j.puhe.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurdie T., Taneva S., Casselman M., Yeung M., McDaniel C., Ho W., Cafazzo J. mHealth consumer apps: The case for user-centered design. Biomedical Instrumentation & Technology. 2012;46(s2):49–56. doi: 10.2345/0899-8205-46.s2.49. [DOI] [PubMed] [Google Scholar]
- Mclean C., Campbell C., Cornish F. African-Caribbean interactions with mental health services in the UK: Experiences and expectations of exclusion as (re)productive of health inequalities. Social Science & Medicine. 2003;56(3):657–669. doi: 10.1016/S0277-9536(02)00063-1. [DOI] [PubMed] [Google Scholar]
- McNamara N., Stevenson C., Costa S., Bowe M., Wakefield J., Kellezi B., et al. Community identification, social support, and loneliness: The benefits of social identification for personal well‐being. British Journal of Social Psychology. 2021;60(4):1379–1402. doi: 10.1111/bjso.12456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNamara N., Stevenson C., Muldoon O.T. Community identity as resource and context: A mixed method investigation of coping and collective action in a disadvantaged community. European Journal of Social Psychology. 2013;43(5):393–403. doi: 10.1002/ejsp.1953. [DOI] [Google Scholar]
- Mereish E.H., Poteat V.P. A relational model of sexual minority mental and physical health: The negative effects of shame on relationships, loneliness, and health. Journal of Counseling Psychology. 2015;62(3):425–437. doi: 10.1037/cou0000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller K., Wakefield J.R.H., Sani F. Identification with social groups is associated with mental health in adolescents: Evidence from a Scottish community sample. Psychiatry Research. 2015;228(3):340–346. doi: 10.1016/j.psychres.2015.05.088. [DOI] [PubMed] [Google Scholar]
- Mitton C., Smith N., Peacock S., Evoy B., Abelson J. Public participation in health care priority setting: A scoping review. Health Policy. 2009;91(3):219–228. doi: 10.1016/j.healthpol.2009.01.005. [DOI] [PubMed] [Google Scholar]
- Morahan-Martin J., Schumacher P. Loneliness and social uses of the Internet. Computers in Human Behavior. 2003;19(6):659–671. doi: 10.1016/S0747-5632(03)00040-2. [DOI] [Google Scholar]
- Morton T.A., Wilson N., Haslam C., Birney M., Kingston R., McCloskey L.-G. Activating and guiding the engagement of seniors with online social networking: Experimental findings from the AGES 2.0 project. Journal of Aging and Health. 2018;30(1):27–51. doi: 10.1177/0898264316664440. [DOI] [PubMed] [Google Scholar]
- Neves B.B., Franz R.L., Munteanu C., Baecker R. Adoption and feasibility of a communication app to enhance social connectedness amongst frail institutionalized oldest old: An embedded case study. Information, Communication & Society. 2018;21(11):1681–1699. doi: 10.1080/1369118X.2017.1348534. [DOI] [Google Scholar]
- Norman D. 2013. The Design of Everyday Things: Revised and Expanded Edition. Basic books. [Google Scholar]
- Nuseibeh B. 2022. Trans-disciplinarity in-the-small. LinkedIn.https://www.linkedin.com/pulse/trans-disciplinarity-in-the-small-bashar-nuseibeh [Google Scholar]
- Office for National Statistics . 2020. Coronavirus and depression in adults.https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/articles/coronavirusanddepressioninadultsgreatbritain/june2020 Great Britain. [Google Scholar]
- Pan P.J.D., Chang S.-H., Yu Y.-Y. A support group for home-quarantined college students exposed to SARS: Learning from practice. Journal for Specialists in Group Work. 2005;30(4):363–374. doi: 10.1080/01933920500186951. [DOI] [Google Scholar]
- Pauly T., Lay J.C., Kozik P., Graf P., Mahmood A., Hoppmann C.A. Technology, physical activity, loneliness, and cognitive functioning in old age. GeroPsych. 2019;32(3):111–123. doi: 10.1024/1662-9647/a000208. [DOI] [Google Scholar]
- Peek M.K., Lin N. Age differences in the effects of network composition on psychological distress. Social Science & Medicine. 1999;49(5):621–636. doi: 10.1016/s0277-9536(99)00139-2. [DOI] [PubMed] [Google Scholar]
- Pellecchia U., Crestani R., Decroo T., Van den Bergh R., Al-Kourdi Y. Social consequences of Ebola containment measures in Liberia. PLoS One. 2015;10(12) doi: 10.1371/journal.pone.0143036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennebaker J.W. Writing about emotional experiences as a therapeutic process. Psychological Science. 1997;8(3):162–166. [Google Scholar]
- Previtali F., Allen L.D., Varlamova M. Not only virus spread: The diffusion of ageism during the outbreak of COVID-19. Journal of Aging & Social Policy. 2020;32(4–5):506–514. doi: 10.1080/08959420.2020.1772002. [DOI] [PubMed] [Google Scholar]
- Pulekar G., Agu E. 2016 IEEE healthcare innovation point-of-care technologies conference (HI-POCT) 2016. Autonomously sensing loneliness and its interactions with personality traits using smartphones; pp. 134–137. [DOI] [Google Scholar]
- Riva G., Villani D., Cipresso P., Repetto C., Triberti S., Di Lernia D., et al. Positive and transformative technologies for active ageing. Studies in Health Technology and Informatics. 2016;220:308–315. [PubMed] [Google Scholar]
- Robb C.E., de Jager C.A., Ahmadi-Abhari S., Giannakopoulou P., Udeh-Momoh C., McKeand J., et al. Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: A survey of older adults in london, UK. Frontiers in Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.591120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rook K.S. Research on social support, loneliness, and social isolation: Toward an integration. Review of Personality & Social Psychology. 1984;5:239–264. [Google Scholar]
- Russell D., Cutrona C.E., Rose J., Yurko K. Social and emotional loneliness: An examination of Weiss's typology of loneliness. Journal of Personality and Social Psychology. 1984;46(6):1313–1321. doi: 10.1037/0022-3514.46.6.1313. [DOI] [PubMed] [Google Scholar]
- Sanchez W., Martinez A., Campos W., Estrada H., Pelechano V. Inferring loneliness levels in older adults from smartphones. Journal of Ambient Intelligence and Smart Environments. 2015;7(1):85–98. doi: 10.3233/AIS-140297. [DOI] [Google Scholar]
- Sani F., Herrera M., Wakefield J.R.H., Boroch O., Gulyas C. Comparing social contact and group identification as predictors of mental health. British Journal of Social Psychology. 2012;51(4):781–790. doi: 10.1111/j.2044-8309.2012.02101.x. [DOI] [PubMed] [Google Scholar]
- Sani F., Wakefield J.R.H., Herrera M., Zeybek A. On the association between greater family identification and lower paranoid ideation among non-clinical individuals: Evidence from Cypriot and Spanish students. Journal of Social and Clinical Psychology. 2017;36(5):396–418. doi: 10.1521/jscp.2017.36.5.396. [DOI] [Google Scholar]
- Schellekens M.P.J., Lee van der M.L. Loneliness and belonging: Exploring experiences with the COVID-19 pandemic in psycho-oncology. Psycho-Oncology. 2020;29(9):1399–1401. doi: 10.1002/pon.5459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S.G.S., Nogueras D., Woerden H. C. van, Kiparoglou V. The COVID-19 pandemic: A pandemic of lockdown loneliness and the role of digital technology. Journal of Medical Internet Research. 2020;22(11) doi: 10.2196/22287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw H., Ellis D.A., Ziegler F.V. The Technology Integration Model (TIM). Predicting the continued use of technology. Computers in Human Behavior. 2018;83:204–214. doi: 10.1016/j.chb.2018.02.001. [DOI] [Google Scholar]
- Shrestha D.B., Thapa B.B., Katuwal N. Psychological distress in Nepalese residents during COVID-19 pandemic: A community level survey. BMC Psychiatry. 2020;20 doi: 10.1186/s12888-020-02904-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrewsbury C.M. Information technology issues in an era of greater state responsibilities. Journal of Aging & Social Policy. 2002;14(3–4):195–209. doi: 10.1300/J031v14n03_11. [DOI] [PubMed] [Google Scholar]
- Song H., Zmyslinski-Seelig A., Kim J., Drent A., Victor A., Omori K., et al. Does Facebook make you lonely?: A meta analysis. Computers in Human Behavior. 2014;36:446–452. doi: 10.1016/j.chb.2014.04.011. [DOI] [Google Scholar]
- South J., Giuntoli G., Kinsella K., Carless D., Long J., McKenna J. Walking, connecting and befriending: A qualitative pilot study of participation in a lay-led walking group intervention. Journal of Transport & Health. 2017;5:16–26. doi: 10.1016/j.jth.2016.12.008. [DOI] [Google Scholar]
- Steffens N.K., Jetten J., Haslam C., Cruwys T., Haslam S.A. Multiple social identities enhance health post-retirement because they are a basis for giving social support. Frontiers in Psychology. 2016;7 doi: 10.3389/fpsyg.2016.01519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson C., McNamara N., Muldoon O. Stigmatised identity and service usage in disadvantaged communities: Residents', community workers' and service providers' perspectives. Journal of Community & Applied Social Psychology. 2014;24(6):453–466. doi: 10.1002/casp.2184. [DOI] [Google Scholar]
- Stone M.E., Lin J., Dannefer D., Kelley-Moore J.A. The continued eclipse of heterogeneity in gerontological research. Journal of Gerontology: Serie Bibliographique. 2017;72(1):162–167. doi: 10.1093/geronb/gbv068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart A., Bandara A.K., Levine M. The psychology of privacy in the digital age. Social and Personality Psychology Compass. 2019;13(11) [Google Scholar]
- Stuart A., Levine M. Beyond ‘nothing to hide’: When identity is key to privacy threat under surveillance: Surveillance, identity and privacy threat. European Journal of Social Psychology. 2017;47(6):694–707. doi: 10.1002/ejsp.2270. [DOI] [Google Scholar]
- Stuart A., Stevenson C., Koschate M., Cohen J., Levine M. ‘Oh no, not a group!’ the factors that lonely or isolated people report as barriers to joining groups for health and well‐being. British Journal of Health Psychology. 2022;27(1):179–193. doi: 10.1111/bjhp.12536. [DOI] [PubMed] [Google Scholar]
- Taipale S., Hänninen R. More years, more technologies: Aging in the digital era. Human Technology. 2018;14(3):258–263. doi: 10.17011/ht/urn.201811224833. [DOI] [Google Scholar]
- Talbot C.V., Briggs P. ‘Getting back to normality seems as big of a step as going into lockdown’: The Impact of the COVID-19 pandemic on people with early-middle stage dementia. Age and Ageing. 2021;50(3) doi: 10.1093/ageing/afab012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taube E., Jakobsson U., Midlöv P., Kristensson J. Being in a Bubble: The experience of loneliness among frail older people. Journal of Advanced Nursing. 2016;72(3):631–640. doi: 10.1111/jan.12853. [DOI] [PubMed] [Google Scholar]
- Templeton A., Guven S.T., Hoerst C., Vestergren S., Davidson L., Ballentyne S., et al. Inequalities and identity processes in crises: Recommendations for facilitating safe response to the COVID-19 pandemic. British Journal of Social Psychology. 2020;59(3):674–685. doi: 10.1111/bjso.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Tilburg T. Losing and gaining in old age: Changes in personal network size and social support in a four-year longitudinal study. Journal of Gerontology: Serie Bibliographique. 1998;53B(6):S313–S323. doi: 10.1093/geronb/53B.6.S313. [DOI] [PubMed] [Google Scholar]
- Tomasino K.N., Lattie E.G., Ho J., Palac H.L., Kaiser S.M., Mohr D.C. Harnessing peer support in an online intervention for older adults with depression. American Journal of Geriatric Psychiatry. 2017;25(10):1109–1119. doi: 10.1016/j.jagp.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasileiou K., Barnett J., Barreto M., Vines J., Atkinson M., Lawson S., et al. Experience of loneliness associated with being an informal caregiver: A qualitative investigation. Frontiers in Psychology. 2017;8 doi: 10.3389/fpsyg.2017.00585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor C.R., Bowling A. A longitudinal analysis of loneliness among older people in Great Britain. Journal of Psychology. 2012;146(3):313–331. doi: 10.1080/00223980.2011.609572. [DOI] [PubMed] [Google Scholar]
- Victor C., Sullivan M.P., Woodbridge R., Thomas M. Bentham Open; 2015. Dancing with loneliness in later life: A pilot study mapping seasonal variations. [Google Scholar]
- Vines J., Pritchard G., Wright P., Olivier P., Brittain K. An age-old problem: Examining the discourses of ageing in HCI and strategies for future research. ACM Transactions on Computer-Human Interaction. 2015;22(1):1–27. doi: 10.1145/2696867. [DOI] [Google Scholar]
- Vogel D.L., Wade N.G., Hackler A.H. Perceived public stigma and the willingness to seek counseling: The mediating roles of self-stigma and attitudes toward counseling. Journal of Counseling Psychology. 2007;54(1):40–50. doi: 10.1037/0022-0167.54.1.40. [DOI] [Google Scholar]
- Wagner N., Hassanein K., Head M. Computer use by older adults: A multi-disciplinary review. Computers in Human Behavior. 2010;26(5):870–882. doi: 10.1016/j.chb.2010.03.029. [DOI] [Google Scholar]
- Wakefield J.R.H., Stevenson C., McNamara N., Bowe M., Wilson I., Halder M., et al. Social prescribing as ‘social cure’: A longitudinal study of the health benefits of social connectedness within a social prescribing pathway. Journal of Health Psychology. 2020 doi: 10.1177/1359105320944991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warr D., Davern M., Mann R., Gunn L. Diversifying experiences of community and the implications for addressing place-based poverty. Urban Policy and Research. 2017;35(2):150–164. doi: 10.1080/08111146.2015.1135791. [DOI] [Google Scholar]
- Waycott J., Davis H., Vetere F., Morgans A., Gruner A., Ozanne E., et al. Captioned photographs in psychosocial aged care: Relationship building and boundary work. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2014:4167–4176. doi: 10.1145/2556288.2557290. [DOI] [Google Scholar]
- Waycott J., Vetere F., Ozanne E. In: Ageing and digital technology: Designing and evaluating emerging technologies for older adults. Neves B.B., Vetere F., editors. Springer; 2019. Building social connections: A framework for enriching older adults' social connectedness through information and communication technologies; pp. 65–82. [DOI] [Google Scholar]
- Waycott J., Vetere F., Pedell S., Kulik L., Ozanne E., Gruner A., et al. Older adults as digital content producers. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2013:39–48. doi: 10.1145/2470654.2470662. [DOI] [Google Scholar]
- Waycott J., Vines J. In: Ageing and digital technology: Designing and evaluating emerging technologies for older adults. Neves B.B., Vetere F., editors. Springer; 2019. Designing technologies with older adults: Ethical tensions and opportunities; pp. 173–187. [DOI] [Google Scholar]
- Waycott J., Wadley G., Schutt S., Stabolidis A., Lederman R. The challenge of technology research in sensitive settings: Case studies in ‘sensitive HCI. Proceedings of the Annual Meeting of the Australian Special Interest Group for Computer Human Interaction. 2015:240–249. doi: 10.1145/2838739.2838773. [DOI] [Google Scholar]
- Weinstein N., Nguyen T. Motivation and preference in isolation: A test of their different influences on responses to self-isolation during the COVID-19 outbreak. Royal Society Open Science. 2020;7(5):200458. doi: 10.1098/rsos.200458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss R.S. The MIT Press; 1973. Loneliness: The experience of emotional and social isolation; p. xxii. [Google Scholar]
- Weisz C., Wood L.F. Social identity support and friendship outcomes: A longitudinal study predicting who will be friends and best friends 4 years later. Journal of Social and Personal Relationships. 2005 doi: 10.1177/0265407505052444. [DOI] [Google Scholar]
- Wenger G.C. Social networks and the prediction of elderly people at risk. Aging & Mental Health. 1997;1(4):311–320. [Google Scholar]
- WHO . 2019. Advice for the public on COVID-19 – world health organization.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public [Google Scholar]
- Wolf L.J., Haddock G., Manstead A.S.R., Maio G.R. The importance of (shared) human values for containing the COVID-19 pandemic. British Journal of Social Psychology. 2020;59(3):618–627. doi: 10.1111/bjso.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020. [Google Scholar]
- Wright D. A framework for the ethical impact assessment of information technology. Ethics and Information Technology. 2011;13(3):199–226. doi: 10.1007/s10676-010-9242-6. [DOI] [Google Scholar]
- Wright D., Friedewald M. Integrating privacy and ethical impact assessments. Science and Public Policy. 2013;40(6):755–766. doi: 10.1093/scipol/sct083. [DOI] [Google Scholar]
- Wu B. Social isolation and loneliness among older adults in the context of COVID-19: A global challenge. Glob Health Res Policy. 2020;5:27. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang H., Bath P.A. Predictors of loneliness among older men and women in england. Journal of Epidemiology & Community Health. 2018 doi: 10.1136/jech-2018-SSMabstracts.125. [DOI] [Google Scholar]
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in liaoning province, China: A cross-sectional study. International Journal of Environmental Research and Public Health. 2020;17(7):2381. doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang R., Nicholas J., Knapp A.A., Graham A.K., Gray E., Kwasny M.J., et al. Clinically meaningful use of mental health apps and its effects on depression: Mixed methods study. Journal of Medical Internet Research. 2019;21(12) doi: 10.2196/15644. [DOI] [PMC free article] [PubMed] [Google Scholar]