Abstract
Background
The COVID-19 pandemic led to early restrictions on access to oral health care and social distancing requirements. The authors examined the early effects of the COVID-19 pandemic on children’s oral health and access to oral health care in the United States.
Methods
Using nationally representative data from the National Survey of Children’s Health, the authors compared several measures of children’s oral health and oral health care use early during the pandemic in 2020 with 1 year earlier. Logistic (multinomial or binary) regression models were estimated, adjusting for several child and household covariates and state fixed effects. Similar comparisons were estimated for 2019 relative to 2018 to evaluate prepandemic trends.
Results
Children in 2020 were 16% (relative risk ratio, 0.84; 95% CI, 0.75 to 0.93) less likely to have excellent dental health as perceived by parents and 75% (relative risk ratio, 1.75; 95% CI, 1.14 to 2.67) more likely to have poor dental health than in 2019. In addition, children in 2020 had higher risk of bleeding gingivae (odds ratio, 1.46; 95% CI, 1.16 to 1.85). The likelihood of having a dental visit in the past 12 months was 27% (odds ratio, 0.73; 95% CI, 0.65 to 0.82) lower in 2020, including lower likelihood for preventive visits. The differences between 2020 and 2019 were observed across demographic and socioeconomic subgroups. There were no such differences between 2019 and 2018.
Conclusions
There was a widespread decline in children’s oral health status and access to oral health care early during the COVID-19 pandemic.
Practical Implications
Prompt policies and oral health campaigns are needed to counter the pandemic effects and increase timely access to dental services.
Key Words: Severe acute respiratory syndrome coronavirus 2, child dental health, access to oral health care, health policy
Abbreviation Key: NSCH, National Survey of Children's Health
The COVID-19 pandemic has posed considerable challenges to children’s health.1, 2, 3 Several COVID-19 mitigation policies were declared in the United States beginning in March and April 2020, including lockdowns and closures of schools and businesses.4 One consequence of these closures and social distancing measures was disrupting children’s access to health care services.5 , 6 Children’s oral health status was likely one of the more adversely affected domains of children’s health due to early imposed restrictions on access to dental services.7, 8, 9 However, there is little empirical evidence on the magnitude of changes in children’s oral health status and use of dental services during the COVID-19 pandemic. Our aim was to provide evidence on this matter.
In March 2020, the Centers for Diseases Control and Prevention and the American Dental Association recommended that dental offices postpone elective procedures and provide emergency care only10 , 11 due to concerns about COVID-19 exposure during treatment.12, 13, 14 Most states also imposed their own restrictions on services at dental offices in the first few months of the pandemic.15 These restrictions, along with social distancing measures, likely resulted in many parents having to postpone oral health care for their children during the pandemic, particularly for preventive care and nonemergency treatments. Although most dental clinics have reopened since June 2020, more than 60% reported lower patient volume than usual or closed by the end of 2020, and nearly 40% reported lower volume or closed by October 2021.16
The rise in unemployment early in the pandemic might have also reduced access to oral health care due to loss of income and employer-sponsored insurance coverage for 6.9 million dependents by June 2020.17 Children were more likely to experience unmet oral health care than medical care during the pandemic, especially in families with pandemic-related job or income losses.9 Among privately insured children, the use of oral health care also rebounded at a slower rate than among insured adults after the reopening.18 Limited access to, and delayed, oral health care are critical risk factors for worsened children’s oral health.19, 20, 21, 22
School closures during the pandemic likely also had adverse effects on children’s oral health. In 2020, most schools closed or changed to remote instruction. School closures disrupted children’s access to the school-based oral health care programs offered in some schools. In 2021, there were nearly 2,000 school-based health centers, approximately 16% of which provide onsite dental services to thousands of students annually.23 Moreover, school closures have disrupted children’s access to school-based breakfast and lunch meals. For some children, at-home meals might be less nutritious with more added sugar, a major risk factor for caries in children.24 , 25 Meanwhile, the social restrictions and increased time at home might have also changed children’s lifestyles and health behaviors. Some studies reported that during the pandemic children had decreased frequency of toothbrushing,26 poor oral hygiene,27 and increased consumption of sugar-sweetened beverages and snacks,26 , 28, 29, 30 which might increase risk of caries and periodontal disease.
We examined the early effects of the COVID-19 pandemic on children’s oral health and access to oral health care in the United States. Specifically, we compared several indicators of children’s oral health and use of oral health care early during the pandemic in 2020 with the same indicators 1 year before the pandemic using nationally representative data. In addition, we evaluated whether the pandemic’s effects on these outcomes differed across demographic and socioeconomic subgroups.
Methods
Study data and sample
Data were from the 2018 through 2020 waves of the National Survey of Children’s Health (NSCH), sponsored by the Maternal and Child Health Bureau and conducted by the US Census Bureau. The NSCH is a nationally representative, cross-sectional survey using both web- and paper-based questionnaires to obtain information about several aspects of children’s health and health care use. Questionnaires were completed by parents (91% of respondents) or other caregivers (9%). The NSCH randomly selects households with at least 1 child from all 50 states and the District of Columbia. In total, 125,443 households with children were selected from 2018 through 2020, and 102,740 of them completed the survey questionnaire (an interview completion rate of 82%).
The 2018 interviews were completed from June 2018 through January 2019. The 2019 interviews were completed from June 2019 through January 2020. The 2020 interviews were completed from July 2020 through January 2021. Of particular relevance to our study was that all interviews were completed at least 4 months after the COVID-19 pandemic started in the United States and after the initial widespread lockdowns and business and school closures in the United States from late March through May 2020. During the period of the 2020 NSCH wave interviews (July 27, 2020-January 22, 2021), there were more than 20 million new cases of COVID-19, with a daily average of 115,000 new cases. The main analytical sample ranged from 91,626 through 92,428 children (depending on outcome) aged 1 through 17 years with complete data on outcomes and explanatory model variables (described below). Infants aged 0 years were excluded from the main sample, as most (65%) had no teeth, but were added back to the sample in sensitivity analyses. Descriptive statistics for the main sample are presented in eTable 1 (available online at the end of this article).
Outcomes
Outcomes were measures of the child’s oral health or oral health care use. The first outcome was dental health, as perceived by parents (or other responding primary caregivers) on a Likert scale (that is, excellent, very good, good, fair, or poor). The second outcome was based on a question about whether the child had frequent or chronic difficulty with oral health problems during the past 12 months, including toothaches, bleeding gingivae, or caries. We coded a binary (0 or 1) indicator for reporting any of these problems and separate binary indicators for each of these problems. Use of dental services was measured by means of 2 variables on the basis of the survey questions: 1 was a binary indicator for whether the child had any dental visits in the past 12 months and 2 was a 3-category variable for whether the child had none, 1, or 2 or more preventive dental visits in the past 12 months. The questionnaire defined a preventive dental visit as one involving any of the following services: dental examination, dental prophylaxis, dental sealant, or fluoride treatment.
Statistical analysis
Oral health and oral health care use outcomes were compared between 2020 and 2019 using a regression model. Specifically, each outcome was regressed on a binary indicator (1 if 2020 survey wave and 0 if 2019 survey wave), adjusting for several conceptually relevant child, family, and state-level covariates.31 The child’s covariates were age (year-by-year binary indicators), sex, and race or ethnicity. The household covariates were the highest education of caregivers, number of children, marital status, any employment, and income as a percentage of the federal poverty threshold. The regression also adjusted for state fixed effects (binary indicators for states). To examine whether outcomes were changing before the pandemic (that is, if there were time trends), which would bias the comparison as capturing the pandemic effect, another regression model was estimated comparing the outcomes in survey wave 2019 through 2018 using the same set of covariates.
For the 2 multicategory ordered outcomes, dental health as perceived by parents (from excellent to poor) and the number of preventive dental visits, an ordered logistic regression was first considered. However, the proportional odds assumption was rejected on the basis of the Brant test.32 Therefore, the model for these 2 outcomes was estimated using multinominal logistic regression (which drops the proportional odds assumption). For binary outcomes (any dental problem, any dental visit), a binary logistic regression was used. Regression models were estimated using the survey sampling weights to obtain nationally representative estimates.
The model was estimated first for the total sample. Additional models were estimated for demographic and socioeconomic subgroups to evaluate potential differences. In those analyses, the regression models were estimated according to child’s age (1-5 years, 6-11 years, 12-17 years), sex, race or ethnicity (non-Hispanic White versus Hispanic or non-White), family income (< 200%, 200%-399%, and ≥ 400% of federal poverty threshold) and insurance status (publicly insured versus not).
Results
Oral health
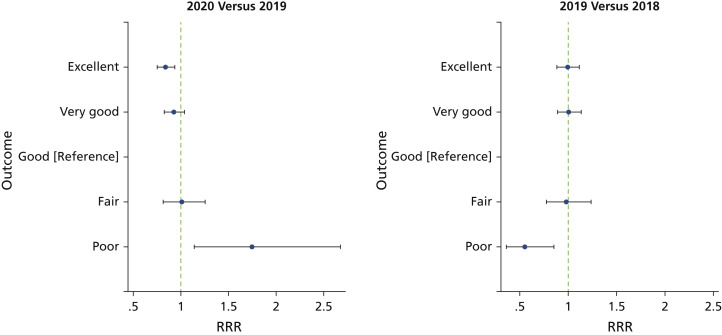
Figure 1 presents the relative risk ratios (RRRs) and their 95% confidence intervals (CIs) from the multinomial logistic regression for the child’s dental health as perceived by parents (5 categories ranging from excellent to poor, with good as the reference category) comparing 2020 with 2019. Children in 2020 were 16% (RRR, 0.84; 95% CI, 0.75 to 0.93) less likely to have excellent (versus good) dental health as perceived by parents than children in 2019. Moreover, children in 2020 were 75% (RRR, 1.75; 95% CI, 1.14 to 2.67) more likely to have a poor dental health as perceived by parents than 2019. Also, there was a statistically nonsignificant decrease in the likelihood of very good dental health as perceived by parents (RRR, 0.92; 95% CI, 0.82 to 1.04). These differences were not observed when comparing children in 2019 with children in 2018; there were similar proportions with excellent or very good dental health as perceived by parents between those years. There was an opposite difference in poor dental health as perceived by parents, in that children in 2019 were less likely to have poor teeth than in 2018. The only exception was that children were approximately 45% (RRR, 0.55; 95% CI, 0.36 to 0.85) less likely to be rated at poor dental health relative to rating them at good dental health. Therefore, time trends (based on the comparison of 2019 with 2018) do not appear to explain the difference between 2019 and 2020. Results were similar when adding infants aged 0 years.
Figure 1.
Differences (relative risk ratios [RRRs] with 95% CIs) in children’s dental health as perceived by parents between 2020 and 2019 and between 2019 and 2018. The sample included children aged 1 through 17 years. The RRRs (dots) and 95% CIs (bars) were obtained from multinomial logistic regression estimates for the child’s dental health as perceived by parents (5 categories ranging from excellent to poor, with good as the reference category) with separate regressions for comparing 2020 with 2019 and comparing 2019 with 2018. The model used data from the 2018 through 2020 waves of the National Survey of Children's Health and adjusted for age, sex, race or ethnicity, highest education of parents, number of children, marital status, any employment, income as a percentage of the federal poverty threshold, and state fixed effects. The model was weighted using the National Survey of Children's Health sampling weights to yield nationally representative estimates.
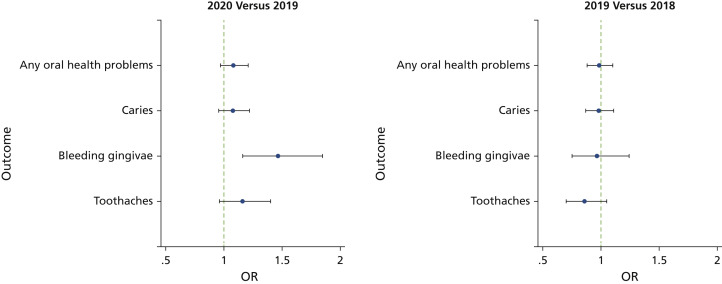
Figure 2 shows the odds ratios (ORs) from the logistic regression for oral health problems (toothaches, bleeding gingivae, caries) and for each problem separately. Children had a slightly elevated risk of any problem in 2020 compared with 2019, although the difference was not statistically significant (OR, 1.08; 95% CI, 0.97 to 1.20). When examining each problem separately, all 3 problems had elevated risks in 2020 but the difference between 2019 and 2020 was largest and statistically significant for bleeding gingivae only (OR, 1.46; 95% CI, 1.16 to 1.85). Differences between 2019 and 2018 were small and statistically nonsignificant, indicating no prepandemic time trends that would bias the observed differences between 2020 and 2019. Similar results were observed when adding infants aged 0 years.
Figure 2.
Differences (odds ratios [ORs] and 95% CIs) in children’s oral health problems between 2020 and 2019 and between 2019 and 2018. The sample included children aged 1 through 17 years. The ORs (dots) and 95% CIs (bars) were obtained from logistic regression for oral health problems (toothaches, bleeding gingivae, caries) and for each problem separately, comparing 2020 with 2019 and comparing 2019 with 2018. All models used data from the 2018 through 2020 waves of the National Survey of Children's Health and adjusted for age, sex, race or ethnicity, highest education of parents, number of children, marital status, any employment, income as a percentage of the federal poverty threshold, and state fixed effects. The model was weighted using the National Survey of Children's Health sampling weights to yield nationally representative estimates.
Oral health care use
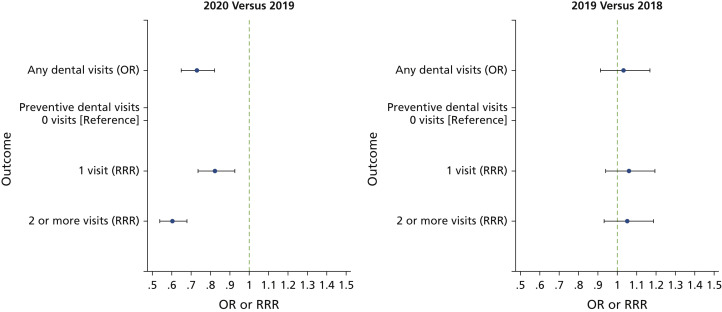
Figure 3 reports the estimates for oral health care use measures. The likelihood of having a dental visit in the past 12 months was 27% (OR, 0.73; 95% CI, 0.65 to 0.82) lower in 2020 than in 2019. Similarly, children were 18% (RRR, 0.82; 95% CI, 0.74 to 0.93) less likely to have had 1 preventive dental visit in the past 2 months and 40% (RRR, 0.60; 95% CI, 0.54 to 0.68) less likely to have had 2 or more preventive dental visits in 2020. All estimates comparing 2019 with 2018 were small and statistically nonsignificant, suggesting no bias from prepandemic trends. Results were similar when adding infants aged 0 years.
Figure 3.
Differences (odds ratios [ORs] or relative risk ratios [RRRs] and 95% CIs) in children’s use of dental visits between 2020 and 2019 and between 2019 and 2018. The sample included children aged 1 through 17 years. The ORs (dots) and 95% CIs (bars) were obtained from logistic regression for any dental visits comparing 2020 with 2019 and comparing 2019 with 2018. The RRRs (dots) and 95% CIs (bars) were obtained from multinomial logistic regression estimates for number of preventive dental visits (3 categories of none, 1, or 2 or more visits, with no visit as reference group) comparing 2020 with 2019 and comparing 2019 with 2018. All models used data from the 2018 through 2020 waves of the National Survey of Children's Health and adjusted for age, sex, race or ethnicity, highest education of parents, number of children, marital status, any employment, income as a percentage of the federal poverty threshold, and state fixed effects. The model was weighted using the National Survey of Children's Health sampling weights to yield nationally representative estimates.
Subgroup analyses
Table 1, Table 2, and 3 report the regression results for children’s dental health as perceived by parents, oral health problems, and oral health care use, respectively, according to age, race or ethnicity, sex, income, and public health insurance status. Most estimates were generally similar across subgroups. The increased likelihood of poor dental health in 2020 was most pronounced among Hispanic or non-White children, those with household income from 200% through 399% of the federal poverty threshold, and those without public insurance coverage (Table 1). The increase in bleeding gingivae likelihood was largest among children aged 1 through 5 years (Table 2), also largest when adding infants aged 0 years (eTable 2; available online at the end of this article). All subgroups had statistically significant declines in oral health care use in 2020 (Table 3).
Table 1.
Differences (RRRs∗ with 95% CIs†) in children’s‡ dental health as perceived by parents between 2020 and 2019 and between 2019 and 2018.
| CHILDREN’S DENTAL HEALTH AS PERCEIVED BY PARENTS |
|||||
|---|---|---|---|---|---|
| VARIABLE | No. | Excellent, RRR (95% CI) | Very Good, RRR (95% CI) | Fair, RRR (95% CI) | Poor, RRR (95% CI) |
| 2020 Versus 2019 | |||||
| Aged 1-5 y | 16,756 | 0.73§ (0.565 to 0.932) | 0.80¶ (0.610 to 1.039) | 0.64 (0.377 to 1.090) | 1.88 (0.790 to 4.468) |
| Aged 6-11 y | 20,442 | 0.90 (0.753 to 1.072) | 0.98 (0.827 to 1.173) | 1.01 (0.740 to 1.367) | 1.85¶ (0.889 to 3.844) |
| Aged 12-17 y | 27,488 | 0.84§ (0.707 to 0.996) | 0.92 (0.771 to 1.107) | 1.23 (0.876 to 1.730) | 1.39 (0.812 to 2.393) |
| Non-Hispanic White | 44,497 | 0.88§ (0.782 to 0.984) | 0.91 (0.803 to 1.022) | 0.98 (0.792 to 1.223) | 1.21 (0.721 to 2.046) |
| Hispanic or non-White | 20,189 | 0.80§ (0.669 to 0.962) | 0.96 (0.799 to 1.155) | 1.04 (0.756 to 1.436) | 2.49# (1.368 to 4.515) |
| < 200% federal poverty threshold | 16,898 | 0.82§ (0.680 to 0.989) | 0.92 (0.764 to 1.116) | 0.92 (0.677 to 1.261) | 1.12 (0.660 to 1.912) |
| 200%-399% federal poverty threshold | 20,543 | 0.86 (0.719 to 1.033) | 0.90 (0.748 to 1.083) | 1.16 (0.834 to 1.613) | 3.12# (1.465 to 6.637) |
| ≥ 400% federal poverty threshold | 27,245 | 0.86 (0.717 to 1.033) | 0.98 (0.811 to 1.190) | 1.08 (0.752 to 1.564) | 1.31 (0.547 to 3.121) |
| Publicly insured | 14,316 | 0.78§ (0.638 to 0.958) | 0.87 (0.711 to 1.054) | 1.06 (0.760 to 1.491) | 1.06 (0.591 to 1.887) |
| Not publicly insured | 49,151 | 0.89¶ (0.785 to 1.013) | 1.01 (0.883 to 1.151) | 1.36¶ (1.043 to 1.762) | 2.15# (1.205 to 3.851) |
| 2019 Versus 2018 | |||||
| Aged 1-5 y | 13,916 | 1.17 (0.906 to 1.522) | 1.12 (0.850 to 1.463) | 1.03 (0.580 to 1.839) | 1.00 (0.465 to 2.147) |
| Aged 6-11 y | 17,206 | 1.02 (0.850 to 1.235) | 1.02 (0.847 to 1.220) | 1.11 (0.786 to 1.554) | 0.48§ (0.262 to 0.891) |
| Aged 12-17 y | 23,087 | 0.88 (0.738 to 1.049) | 0.96 (0.798 to 1.157) | 0.84 (0.578 to 1.207) | 0.54¶ (0.267 to 1.079) |
| Non-Hispanic White | 38,149 | 1.04 (0.926 to 1.170) | 1.10 (0.971 to 1.241) | 0.98 (0.789 to 1.226) | 0.95 (0.535 to 1.671) |
| Hispanic or non-White | 16,060 | 0.96 (0.793 to 1.169) | 0.92 (0.759 to 1.121) | 0.97 (0.676 to 1.385) | 0.35# (0.192 to 0.647) |
| < 200% federal poverty threshold | 13,898 | 0.95 (0.777 to 1.164) | 0.96 (0.787 to 1.170) | 1.07 (0.769 to 1.503) | 0.55§ (0.318 to 0.954) |
| 200%-399% federal poverty threshold | 17,269 | 1.03 (0.861 to 1.231) | 1.08 (0.898 to 1.298) | 0.83 (0.572 to 1.199) | 0.80 (0.375 to 1.704) |
| ≥ 400% federal poverty threshold | 23,042 | 1.02 (0.842 to 1.229) | 1.01 (0.826 to 1.231) | 0.88 (0.589 to 1.307) | 0.42§ (0.179 to 0.980) |
| Publicly insured | 11,781 | 0.94 (0.756 to 1.170) | 0.99 (0.808 to 1.219) | 0.93 (0.661 to 1.318) | 0.71 (0.419 to 1.194) |
| Not publicly insured | 41,304 | 1.01 (0.886 to 1.156) | 1.01 (0.877 to 1.157) | 0.93 (0.697 to 1.241) | 0.47§ (0.250 to 0.881) |
RRR: Relative risk ratio.
The RRRs and 95% CIs were obtained from multinomial logistic regression estimates for the child’s dental health as perceived by parents (5 categories ranging from excellent to poor, with good as the reference category) with separate regressions for comparing 2020 with 2019 and comparing 2019 with 2018. The model used data from the 2018-2020 waves of the National Survey of Children's Health and adjusted for age, sex, race or ethnicity, highest education of parents, number of children, marital status, any employment, income as a percentage of the federal poverty threshold, and state fixed effects. The model was weighted by the National Survey of Children's Health sampling weights to yield nationally representative estimates.
The sample included children aged 1-17 years.
P < .05.
P < .1.
P < .01.
Table 2.
Differences (ORs∗ and 95% CIs†) in children’s‡ oral health problems between 2020 and 2019 and between 2019 and 2018.
| 2020 VERSUS 2019 |
2019 VERSUS 2018 |
|||||
|---|---|---|---|---|---|---|
| VARIABLE | No. | OR | 95% CI | No. | OR | 95% CI |
| Any Oral Health Problems | ||||||
| Aged 1-5 y | 16,723 | 1.19 | 0.916 to 1.549 | 13,843 | 0.98 | 0.758 to 1.269 |
| Aged 6-11 y | 20,319 | 1.03 | 0.883 to 1.212 | 17,066 | 1.01 | 0.856 to 1.186 |
| Aged 12-17 y | 27,304 | 1.08 | 0.907 to 1.297 | 22,884 | 0.99 | 0.821 to 1.195 |
| Non-Hispanic White | 44,289 | 1.04 | 0.924 to 1.166 | 37,867 | 0.97 | 0.860 to 1.084 |
| Hispanic or non-White | 20,057 | 1.11 | 0.934 to 1.324 | 15,926 | 1.01 | 0.838 to 1.207 |
| < 200% federal poverty threshold | 16,813 | 1.06 | 0.879 to 1.267 | 13,819 | 0.98 | 0.813 to 1.179 |
| 200%-399% federal poverty threshold | 20,441 | 1.11 | 0.923 to 1.325 | 17,139 | 0.99 | 0.826 to 1.177 |
| ≥ 400% federal poverty threshold | 27,092 | 1.09 | 0.918 to 1.285 | 22,835 | 0.96 | 0.806 to 1.149 |
| Publicly insured | 14,248 | 1.00 | 0.825 to 1.216 | 11,722 | 1.19§ | 0.983 to 1.451 |
| Not publicly insured | 48,891 | 1.09 | 0.970 to 1.231 | 40,967 | 0.91 | 0.804 to 1.032 |
| Caries | ||||||
| Aged 1-5 y | 16,825 | 1.10 | 0.808 to 1.501 | 13,967 | 0.95 | 0.700 to 1.286 |
| Aged 6-11 y | 20,432 | 1.04 | 0.879 to 1.234 | 17,179 | 1.03 | 0.865 to 1.225 |
| Aged 12-17 y | 27,467 | 1.12 | 0.917 to 1.378 | 23,032 | 0.95 | 0.776 to 1.172 |
| Non-Hispanic White | 44,541 | 1.04 | 0.913 to 1.173 | 38,137 | 0.92 | 0.814 to 1.046 |
| Hispanic or non-White | 20,183 | 1.11 | 0.914 to 1.350 | 16,041 | 1.03 | 0.844 to 1.263 |
| < 200% federal poverty threshold | 16,902 | 1.09 | 0.892 to 1.337 | 13,901 | 1.00 | 0.819 to 1.231 |
| 200%-399% federal poverty threshold | 20,555 | 1.11 | 0.907 to 1.347 | 17,262 | 0.93 | 0.765 to 1.120 |
| ≥ 400% federal poverty threshold | 27,267 | 1.00 | 0.830 to 1.209 | 23,015 | 0.97 | 0.794 to 1.180 |
| Publicly insured | 14,324 | 0.99 | 0.800 to 1.228 | 11,791 | 1.24¶ | 1.004 to 1.534 |
| Not publicly insured | 49,187 | 1.07 | 0.942 to 1.221 | 41,269 | 0.87¶ | 0.757 to 0.994 |
| Bleeding Gingivae | ||||||
| Aged 1-5 y | 14,999 | 3.44# | 1.849 to 6.395 | 9,745 | 1.36 | 0.682 to 2.716 |
| Aged 6-11 y | 20,365 | 1.39§ | 0.977 to 1.991 | 17,123 | 1.06 | 0.741 to 1.517 |
| Aged 12-17 y | 27,383 | 1.30 | 0.927 to 1.823 | 22,973 | 0.87 | 0.599 to 1.251 |
| Non-Hispanic White | 44,430 | 1.24 | 0.943 to 1.634 | 38,034 | 1.08 | 0.810 to 1.441 |
| Hispanic or non-White | 20,104 | 1.69# | 1.195 to 2.378 | 15,654 | 0.89 | 0.619 to 1.286 |
| < 200% federal poverty threshold | 16,857 | 1.31 | 0.912 to 1.873 | 13,862 | 0.94 | 0.651 to 1.353 |
| 200%-399% federal poverty threshold | 20,484 | 1.69# | 1.141 to 2.493 | 16,949 | 1.09 | 0.696 to 1.719 |
| ≥ 400% federal poverty threshold | 27,141 | 1.37 | 0.924 to 2.025 | 22,948 | 0.84 | 0.555 to 1.265 |
| Publicly insured | 14,171 | 1.41§ | 0.951 to 2.076 | 11,755 | 0.97 | 0.651 to 1.440 |
| Not publicly insured | 49,051 | 1.61# | 1.216 to 2.139 | 41,148 | 1.11 | 0.826 to 1.485 |
| Toothaches | ||||||
| Aged 1-5 y | 16,788 | 1.19 | 0.778 to 1.816 | 13,947 | 1.21 | 0.774 to 1.893 |
| Aged 6-11 y | 20,377 | 1.09 | 0.836 to 1.430 | 17,163 | 0.74¶ | 0.562 to 0.964 |
| Aged 12-17 y | 27,411 | 1.21 | 0.883 to 1.646 | 23,030 | 0.90 | 0.642 to 1.272 |
| Non-Hispanic White | 44,438 | 1.05 | 0.840 to 1.310 | 38,116 | 1.05 | 0.840 to 1.308 |
| Hispanic or non-White | 20,138 | 1.23 | 0.930 to 1.635 | 16,024 | 0.75§ | 0.559 to 1.014 |
| < 200% federal poverty threshold | 16,856 | 0.98 | 0.744 to 1.278 | 13,879 | 0.86 | 0.644 to 1.148 |
| 200%-399% federal poverty threshold | 20,526 | 1.31 | 0.922 to 1.847 | 17,251 | 0.91 | 0.652 to 1.274 |
| ≥ 400% federal poverty threshold | 27,194 | 1.54# | 1.120 to 2.108 | 23,010 | 0.80 | 0.568 to 1.114 |
| Publicly insured | 14,292 | 1.15 | 0.850 to 1.550 | 11,777 | 0.94 | 0.693 to 1.269 |
| Not publicly insured | 49,081 | 1.24§ | 0.984 to 1.570 | 41,251 | 0.86 | 0.673 to 1.089 |
OR: Odds ratio.
ORs and 95% CIs were obtained from logistic regression for oral health problems (toothaches, bleeding gingivae, caries) and for each problem separately, comparing 2020 with 2019 and comparing 2019 with 2018. All models used data from the 2018-2020 waves of the National Survey of Children's Health and adjusted for age, sex, race or ethnicity, highest education of parents, number of children, marital status, any employment, income as a percentage of the federal poverty threshold, and state fixed effects. The model was weighted by the National Survey of Children's Health sampling weights to yield nationally representative estimates.
The sample included children aged 1-17 years.
P < .1.
P < .05.
P < .01.
Table 3.
Differences (ORs∗ or RRRs† and 95% CIs‡) in children’s§ use of dental visits between 2020 and 2019 and between 2019 and 2018.
| NO. OF PREVENTIVE DENTAL VISITS (MULTINOMINAL LOGISTIC REGRESSION) |
||||||||
|---|---|---|---|---|---|---|---|---|
| ANY DENTAL VISITS |
1 Preventive Visit |
≥ 2 Preventive Visits |
||||||
| VARIABLE | No. | OR | 95% CI | No. | RRR | 95% CI | RRR | 95% CI |
| 2020 Versus 2019 | ||||||||
| Aged 1-5 y | 16,857 | 0.67¶ | 0.572 to 0.795 | 16,836 | 0.73¶ | 0.612 to 0.865 | 0.57¶ | 0.471 to 0.701 |
| Aged 6-12 y | 20,458 | 0.78# | 0.620 to 0.991 | 20,398 | 0.93 | 0.744 to 1.158 | 0.57¶ | 0.463 to 0.714 |
| Aged 12-17 y | 27,480 | 0.76# | 0.621 to 0.941 | 27,428 | 0.84∗∗ | 0.691 to 1.021 | 0.69¶ | 0.570 to 0.831 |
| Non-Hispanic White | 44,587 | 0.78¶ | 0.685 to 0.884 | 44,500 | 0.85# | 0.754 to 0.964 | 0.62¶ | 0.549 to 0.703 |
| Hispanic or non-White | 20,208 | 0.67¶ | 0.563 to 0.808 | 20,162 | 0.78¶ | 0.654 to 0.935 | 0.57¶ | 0.477 to 0.687 |
| < 200% federal poverty threshold | 16,927 | 0.80# | 0.673 to 0.960 | 16,876 | 0.85∗∗ | 0.711 to 1.018 | 0.68¶ | 0.564 to 0.825 |
| 200%-399% federal poverty threshold | 20,579 | 0.66¶ | 0.535 to 0.803 | 20,555 | 0.76¶ | 0.620 to 0.922 | 0.59¶ | 0.486 to 0.722 |
| ≥ 400% federal poverty threshold | 27,289 | 0.68¶ | 0.557 to 0.822 | 27,231 | 0.80# | 0.663 to 0.960 | 0.50¶ | 0.420 to 0.606 |
| Publicly insured | 14,344 | 0.62¶ | 0.506 to 0.752 | 14,317 | 0.69¶ | 0.569 to 0.844 | 0.51¶ | 0.413 to 0.629 |
| Not publicly insured | 49,245 | 0.76¶ | 0.653 to 0.885 | 49,150 | 0.86# | 0.743 to 0.993 | 0.61¶ | 0.531 to 0.707 |
| 2019 Versus 2018 | ||||||||
| Aged 1-5 y | 14,002 | 1.01 | 0.863 to 1.194 | 13,981 | 1.09 | 0.922 to 1.293 | 0.95 | 0.772 to 1.160 |
| Aged 6-12 y | 17,223 | 0.94 | 0.718 to 1.223 | 17,179 | 0.91 | 0.710 to 1.168 | 1.06 | 0.835 to 1.345 |
| Aged 12-17 y | 23,114 | 1.14 | 0.904 to 1.432 | 23,037 | 1.19 | 0.961 to 1.473 | 1.08 | 0.883 to 1.331 |
| Non-Hispanic White | 38,249 | 0.99 | 0.873 to 1.123 | 38,156 | 1.05 | 0.928 to 1.188 | 1.05 | 0.928 to 1.184 |
| Hispanic or non-White | 16,090 | 1.08 | 0.887 to 1.309 | 16,041 | 1.08 | 0.893 to 1.309 | 1.07 | 0.880 to 1.297 |
| < 200% federal poverty threshold | 13,934 | 0.98 | 0.807 to 1.189 | 13,896 | 0.98 | 0.807 to 1.191 | 0.92 | 0.755 to 1.128 |
| 200%-399% federal poverty threshold | 17,314 | 1.21∗∗ | 0.997 to 1.472 | 17,279 | 1.24# | 1.020 to 1.499 | 1.24# | 1.021 to 1.502 |
| ≥ 400% federal poverty threshold | 23,091 | 0.96 | 0.786 to 1.175 | 23,022 | 1.05 | 0.869 to 1.279 | 1.10 | 0.907 to 1.343 |
| Publicly insured | 11,813 | 1.09 | 0.883 to 1.352 | 11,787 | 1.05 | 0.851 to 1.297 | 1.09 | 0.872 to 1.356 |
| Not publicly insured | 41,418 | 1.10 | 0.938 to 1.280 | 41,314 | 1.13 | 0.975 to 1.311 | 1.12 | 0.965 to 1.291 |
OR: Odds ratio.
RRR: Relative risk ratio.
The ORs and 95% CIs were obtained from logistic regression for any dental visits comparing 2020 with 2019 and comparing 2019 with 2018. The RRRs and 95% CIs were obtained from multinomial logistic regression estimates for number of preventive dental visits (3 categories of none, 1, or 2 or more visits, with no visit as reference group) comparing 2020 with 2019 and comparing 2019 with 2018. All models used data from the 2018-2020 waves of the National Survey of Children's Health and adjusted for age, sex, race or ethnicity, highest education of parents, number of children, marital status, any employment, income as a percentage of the federal poverty threshold, and state fixed effects. The model was weighted by the National Survey of Children's Health sampling weights to yield nationally representative estimates.
The sample included children aged 1-17 years.
P < .01.
P < .05.
P < .1.
Discussion
Using nationally representative data, we examined the early effects of the COVID-19 pandemic on oral health and oral health care use for children in the United States by means of comparing these outcomes between 2020 (the first year of the COVID-19 pandemic) and 2019 (1 year before the pandemic). There was a decline in children’s dental health as perceived by parents as excellent and an increase in rating as poor in 2020. In addition, there was greater reporting of bleeding gingivae. Consistent with these differences in oral health, there was also a decline in the likelihood of dental visits, including preventive care visits. These differences between 2020 and 2019 were observed across a range of demographic and socioeconomic subgroups. Overall, there was no evidence of prepandemic trends based on comparisons between 2019 and 2018 that would explain the observed differences between 2020 and 2019. These results suggest that the COVID-19 pandemic had widespread adverse effects on children’s oral health and oral health care use in its first year. These results are consistent with those of other studies in the United Kingdom, Israel, and Brazil, which also showed that the COVID-19 pandemic was significantly associated with reduced access to oral health care and poorer oral health status among children.26 , 33, 34, 35
Improving children’s oral health and access to oral health care has long been a desired policy and public health objective in the United States, even before the COVID-19 pandemic. Preventable dental problems often lead to chronic oral health conditions among children. According to the Centers for Disease Control and Prevention, in 2011 through 2016, nearly one-half of children had caries.36 The prevalence of untreated caries was high, ranging between 5% and 17% depending on age, including 10% among toddlers and 17% among adolescents.36 At the same time, oral health care remains one of the greatest unmet health care needs among children, with multiple barriers to access, including unaffordable financial cost, lack of dental insurance coverage, difficulty finding a dental provider accepting Medicaid, and transportation costs.37, 38, 39, 40 The pandemic likely magnified 1 or more of these barriers to oral health care for most families, particularly with the widespread closures of dental practices early on, social distancing measures, and employment and income loss for some families. The decline in oral health status and oral health care use may result in more untreated oral health problems among children, which can adversely affect their overall health and development in several ways. Poor oral health can result in pain, infection, sepsis, sleep disruption, decreased appetite, and other health complications and is associated with lower psychosocial well-being and academic performance.41, 42, 43, 44
The findings highlight the importance of addressing unmet oral health care needs among children, including their increase during the pandemic, through effective policy interventions that address barriers, including the availability of providers and reducing patient out-of-pocket direct and indirect costs. Continuing to monitor children’s oral health and access to dental services during the ongoing pandemic should also be a public health and policy priority. Real-time data collection and analysis, including through survey and administrative data analyses (such as Medicaid and private insurance claims data) are optimal for monitoring and prompt targeting of unmet needs. However, these data resources lag behind in time, as do most national health surveys, indicating the need for new surveys of families to monitor these trends across the population. These surveys can identify household-level factors that are promoting or worsening oral health and access to care during the pandemic. As such, they can inform the need for household and community-level interventions to mitigate the pandemic’s effects on children’s oral health, including promoting low-sugar diets, water fluoridation, and educating parents and children about dental hygiene practices. In a 2021 national survey, one-quarter of parents reported that their children improved in 1 or more oral health practices during the pandemic, including more frequent toothbrushing, flossing, use of fluoride mouthrinse, or consuming fewer sugar-containing beverages.45 Although this represents only a small proportion of children with improved dental habits during the pandemic, there is both great potential and need to promote healthier behaviors.
Our study has some data limitations. Because all measures of children’s oral health and access to oral health care in the NSCH are reported via parents (or for a small proportion via other caregivers), there is the possibility for measurement error. However, it is unlikely that any measurement error is different before and after the COVID-19 pandemic. Therefore, any measurement error is unlikely to bias the magnitude of differences between survey years, but can inflate the variance of estimates (that is, wider 95% CIs and higher P values). Another issue was that all outcomes, except for dental health as perceived by parents, covered the past 12 months. Therefore, it is possible that some of the responses to these questions in 2020 captured the prepandemic period. However, because the NSCH data were collected from July 2020 through January 2021 (at least 4 months after the pandemic was declared in March and after the early lockdowns and business, including dental practice, closures), these questions are likely to capture changes introduced during the COVID-19 pandemic. If anything, questions about the past 12 months might underestimate the pandemic’s effects on these outcomes. Finally, it is possible that the pandemic’s effects on children’s oral health differ across areas according to availability of dentists or other related contextual factors. We leave this question for future research.
Conclusions
Our study provided evidence of widespread decline in oral health status and access to oral health care among children in the United States early during the COVID-19 pandemic. These findings highlight the need to monitor these trends through timely data collection and to counter the pandemic effects through prompt policies and oral health campaigns that increase awareness about household prevention activities, water fluoridation where needed, and timely access to dental services.
Biographies
Dr. Lyu is an assistant professor, Division of Health Systems Management and Policy, University of Memphis, Memphis, TN.
Dr. Wehby is a professor and the John W. Colloton Chair, Departments of Health Management and Policy, Economics, and Preventive and Community Dentistry, and Public Policy Center, Director of Graduate Studies, Department of Health Management and Policy, University of Iowa, Iowa City, IA, and a research associate, National Bureau of Economic Research, Cambridge, MA.
Footnotes
Disclosure. Drs. Lyu and Wehby did not report any disclosures.
Dr. Wehby acknowledges funding from grant 1R03DE026224 from the National Institute of Dental and Craniofacial Research, National Institutes of Health.
Supplemental data related to this article can be found at: https://doi.org/10.1016/j.adaj.2022.02.008.
Supplemental Data
eTable 1.
Descriptive statistics∗ according to year for children aged 1 through 17 years using data from the 2018-2020 National Survey of Children’s Health.
| VARIABLE | 2018 | 2019 | 2020 |
|---|---|---|---|
| Rated Oral Health (%) | |||
| Poor | 1.0 | 0.6 | 1.0 |
| Fair | 4.3 | 4.2 | 4.4 |
| Good | 14.9 | 14.9 | 16.0 |
| Very good | 30.8 | 31.5 | 32.1 |
| Excellent | 48.9 | 48.9 | 46.6 |
| Any Oral Health Problems (%) | 13.8 | 13.7 | 14.1 |
| Caries | 11.5 | 11.3 | 11.6 |
| Bleeding gingivae | 1.9 | 1.8 | 2.5 |
| Toothaches | 4.4 | 3.7 | 4.0 |
| Any dental visits | 82.2 | 82.8 | 79.4 |
| No. of Preventive Dental Visits (%) | |||
| No preventive dental visit | 20.5 | 19.6 | 23.7 |
| 1 preventive dental visit | 34.3 | 34.9 | 38.1 |
| 2 or more preventive dental visits | 45.2 | 45.5 | 38.2 |
| Age (%) | |||
| 1-5 y | 28.7 | 28.3 | 28.9 |
| 6-11 y | 35.6 | 35.9 | 34.8 |
| 12-17 y | 35.7 | 35.9 | 36.3 |
| Sex (%) | |||
| Male | 51.2 | 51.2 | 51.0 |
| Female | 48.8 | 48.8 | 49.0 |
| Race and Ethnicity (%) | |||
| Non-Hispanic White | 52.0 | 51.9 | 52.7 |
| Non-Hispanic Black | 11.9 | 12.0 | 11.6 |
| Non-Hispanic others | 10.7 | 10.9 | 11.1 |
| Hispanic | 25.5 | 25.2 | 24.7 |
| Education (%) | |||
| < High school | 8.6 | 8.4 | 7.9 |
| High school | 17.8 | 17.8 | 18.0 |
| Some college | 22.0 | 21.4 | 20.5 |
| ≥ College | 51.6 | 52.4 | 53.7 |
| No. of Children (%) | |||
| 1 | 24.7 | 25.3 | 24.4 |
| 2 | 39.4 | 39.2 | 40.4 |
| 3 | 23.3 | 23.6 | 23.2 |
| ≥ 4 | 12.6 | 11.9 | 12.0 |
| Income as Percentage of Federal Poverty Threshold (%) | |||
| < 100% federal poverty threshold | 16.8 | 15.8 | 14.3 |
| 100-200% federal poverty threshold | 21.9 | 21.4 | 21.3 |
| 200-300% federal poverty threshold | 15.7 | 17.4 | 18.0 |
| 300-399% federal poverty threshold | 12.4 | 12.5 | 13.3 |
| ≥ 400% federal poverty threshold | 33.2 | 32.8 | 33.1 |
| Marital Status (%) | 82.3 | 82.7 | 83.0 |
| Employment Status (%) | 94.8 | 95.3 | 97.6 |
| No. | 27,050 | 26,316 | 37,548 |
The descriptive statistics are all weighted using the sampling weights.
eTable 2.
Differences (RRRs∗ or ORs† with 95% CIs‡) in children’s oral health and use of dental visits between 2020 and 2019 and between 2019 and 2018 in children aged 0 through 5 years.
| 2020 VERSUS 2019 |
2019 VERSUS 2018 |
|||||
|---|---|---|---|---|---|---|
| VARIABLE | No. | RRR/OR | 95% CI | No. | RRR/OR | 95% CI |
| Dental Health as Perceived by Parents (Multinominal Logistic Regression, RRR) | 17,501 | 14,556 | ||||
| Excellent | — | 0.78§ | 0.605 to 0.995 | — | 1.12 | 0.867 to 1.452 |
| Very good | — | 0.82 | 0.631 to 1.071 | — | 1.09 | 0.831 to 1.430 |
| Fair | — | 0.67 | 0.396 to 1.141 | — | 0.97 | 0.546 to 1.718 |
| Poor | — | 1.98 | 0.833 to 4.710 | — | 0.92 | 0.426 to 1.966 |
| Any Oral Health Problems | 18,867 | 1.17 | 0.911 to 1.512 | 15,602 | 0.92 | 0.707 to 1.191 |
| Caries | 18,981 | 1.11 | 0.819 to 1.517 | 15,737 | 0.94 | 0.698 to 1.277 |
| Bleeding gingivae | 17,245 | 2.60¶ | 1.322 to 5.123 | 11,765 | 1.51 | 0.819 to 2.800 |
| Toothaches | 18,940 | 1.11 | 0.746 to 1.640 | 15,719 | 0.98 | 0.644 to 1.495 |
| Any dental visits | 19,016 | 0.66¶ | 0.560 to 0.775 | 15,781 | 1.06 | 0.899 to 1.246 |
| No. of Preventive Dental Visits (Multinominal Logistic Regression, RRR) | ||||||
| 1 preventive visit | Not applicable | 0.71¶ | 0.598 to 0.843 | Not applicable | 1.13 | 0.956 to 1.342 |
| ≥ 2 preventive visits | 18,997 | 0.55¶ | 0.450 to 0.670 | 15,760 | 1.00 | 0.813 to 1.229 |
RRR: Relative risk ratio.
OR: Odds ratio.
The RRRs and 95% CIs were obtained from multinomial logistic regression estimates for the child’s dental health as perceived by parents (5 categories ranging from excellent to poor, with good as the reference category) and number of preventive dental visits (3 categories of none, 1, or 2 or more visits, with no visit as reference group) with separate regressions for comparing 2020 with 2019 and comparing 2019 with 2018. The ORs and 95% CIs were obtained from logistic regression for oral health problems (toothaches, bleeding gingivae, caries) and for each problem separately and any dental visits comparing 2020 with 2019 and comparing 2019 with 2018. All models used data from the 2018-2020 waves of the National Survey of Children's Health and adjusted for age, sex, race or ethnicity, highest education of parents, number of children, marital status, any employment, income as a percentage of the federal poverty threshold, and state fixed effects. The model was weighted by the National Survey of Children's Health sampling weights to yield nationally representative estimates.
P < .05.
P < .01.
References
- 1.Fry-Bowers E.K. Children are at risk from COVID-19. J Pediatr Nurs. 2020;53:A10. doi: 10.1016/j.pedn.2020.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irwin M., Lazarevic B., Soled D., Adesman A. The COVID-19 pandemic and its potential enduring impact on children. Curr Opin Pediatr. 2022;34(1):107–115. doi: 10.1097/MOP.0000000000001097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rajmil L., Hjern A., Boran P., Gunnlaugsson G., de Camargo O.K., Raman S. Impact of lockdown and school closure on children’s health and well-being during the first wave of COVID-19: a narrative review. BMJ Paediatr Open. 2021;5(1) doi: 10.1136/bmjpo-2021-001043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raifman J., Nocka K., Jones D., et al. COVID-19 US state policy database. www.tinyurl.com/statepolicies
- 5.Whaley C.M., Pera M.F., Cantor J., et al. Changes in health services use among commercially insured US populations during the COVID-19 pandemic. JAMA Netw Open. 2020;3(11) doi: 10.1001/jamanetworkopen.2020.24984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Callison K., Ward J. Associations between individual demographic characteristics and involuntary health care delays as a result of COVID-19: study examines associations between individual demographic characteristics and involuntary health care delays as a result of COVID-19. Health Aff (Millwood) 2021;40(5):837–843. doi: 10.1377/hlthaff.2021.00101. [DOI] [PubMed] [Google Scholar]
- 7.Meyer B.D., Danesh D.O. The impact of COVID-19 on preventive oral health care during wave one. Front Dent Med. 2021;2:636766. [Google Scholar]
- 8.Maupome G, Scully AC, Yepes JF, Eckert GJ, Downey T. Trends in dental insurance claims in the United States before and during the SARS-CoV-2 pandemic in 2020. J Public Health Dent. Published online January 9, 2022. https://doi.org/10.1111/jphd.12491 [DOI] [PubMed]
- 9.Burgette J.M., Weyant R.J., Ettinger A.K., Miller E., Ray K.N. What is the association between income loss during the COVID-19 pandemic and children’s dental care? JADA. 2021;152(5):369–376. doi: 10.1016/j.adaj.2021.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burger D. ADA recommending dentists postpone elective procedures. ADA News. March 16, 2020. https://www.ada.org/publications/ada-news/2020/march/ada-recommending-dentists-postpone-elective-procedures
- 11.Interim infection prevention and control guidance for dental settings during the coronavirus disease 2019 (COVID-19) pandemic. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
- 12.Brian Z., Weintraub J.A. Oral health and COVID-19: increasing the need for prevention and access. Prev Chronic Dis. 2020;17:E82. doi: 10.5888/pcd17.200266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ge Z.-Y., Yang L.-M., Xia J.-J., Fu X.-H., Zhang Y.-Z. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B. 2020;21(5):361–368. doi: 10.1631/jzus.B2010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meng L., Hua F., Bian Z. Coronavirus disease 2019 (COVID-19): emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99(5):481–487. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Versaci M.B. COVID-19 state mandates and recommendations. ADA News. April 13, 2020. https://www.ada.org/publications/ada-news/2020/april/find-covid-19-dental-regulations-by-state-with-ada-interactive-map
- 16.Economic impact of COVID-19 on dental practices. American Dental Association. https://www.ada.org/resources/research/health-policy-institute/impact-of-covid-19/private-practice-results
- 17.Fronstin P., Woodbury S.A. How many Americans have lost jobs with employer health coverage during the pandemic? The Commonwealth Fund. October 7, 2020. https://www.commonwealthfund.org/publications/issue-briefs/2020/oct/how-many-lost-jobs-employer-coverage-pandemic
- 18.Choi S.E., Simon L., Basu S., Barrow J.R. Changes in dental care use patterns due to COVID-19 among insured patients in the United States. JADA. 2021;152(12):1033–1043.e3. doi: 10.1016/j.adaj.2021.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crall J.J., Vujicic M. Children’s oral health: progress, policy development, and priorities for continued improvement. Health Aff (Millwood) 2020;39(10):1762–1769. doi: 10.1377/hlthaff.2020.00799. [DOI] [PubMed] [Google Scholar]
- 20.Drummond B., Meldrum A., Boyd D. Influence of dental care on children's oral health and wellbeing. Br Dent J. 2013;214(11):E27. doi: 10.1038/sj.bdj.2013.533. [DOI] [PubMed] [Google Scholar]
- 21.Fisher-Owens S.A., Gansky S.A., Platt L.J., et al. Influences on children's oral health: a conceptual model. Pediatrics. 2007;120(3):e510–e520. doi: 10.1542/peds.2006-3084. [DOI] [PubMed] [Google Scholar]
- 22.Kelly S.E., Binkley C.J., Neace W.P., Gale B.S. Barriers to care-seeking for children’s oral health among low-income caregivers. Am J Public Health. 2005;95(8):1345–1351. doi: 10.2105/AJPH.2004.045286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chazin S. Engaging schools to support better oral health for low-income children. Center for Health Care Strategies. August 2015. https://www.chcs.org/resource/engaging-schools-support-better-oral-health-low-income-children
- 24.Kalash D.A. How COVID-19 deepens child oral health inequities. JADA. 2020;151(9):643–645. doi: 10.1016/j.adaj.2020.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Touger-Decker R., van Loveren C. Sugars and dental caries. Am J Clin Nutr. 2003;78(4):881s–892s. doi: 10.1093/ajcn/78.4.881S. [DOI] [PubMed] [Google Scholar]
- 26.Gotler M., Oren L., Spierer S., Yarom N., Ashkenazi M. The impact of COVID-19 lockdown on maintenance of children's dental health: a questionnaire-based survey. JADA. 2022;153(5):440–449. doi: 10.1016/j.adaj.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baptista A.S., Prado I.M., Perazzo M.F., et al. Can children’s oral hygiene and sleep routines be compromised during the COVID-19 pandemic? Int J Paediatr Dent. 2021;31(1):12–19. doi: 10.1111/ipd.12732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jansen E., Thapaliya G., Aghababian A., Sadler J., Smith K., Carnell S. Parental stress, food parenting practices and child snack intake during the COVID-19 pandemic. Appetite. 2021;161:105119. doi: 10.1016/j.appet.2021.105119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Munasinghe S., Sperandei S., Freebairn L., et al. The impact of physical distancing policies during the COVID-19 pandemic on health and well-being among Australian adolescents. J Adolesc Health. 2020;67(5):653–661. doi: 10.1016/j.jadohealth.2020.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ruiz-Roso M.B., de Carvalho Padilha P., Mantilla-Escalante D.C., et al. Covid-19 confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020;12(6):1807. doi: 10.3390/nu12061807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guarnizo-Herreño C.C., Wehby G.L. Explaining racial/ethnic disparities in children’s dental health: a decomposition analysis. Am J Public Health. 2012;102(5):859–866. doi: 10.2105/AJPH.2011.300548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brant R. Assessing proportionality in the proportional odds model for ordinal logistic regression. Biometrics. 1990;46(4):1171–1178. [PubMed] [Google Scholar]
- 33.Fux-Noy A., Mattar L., Shmueli A., Halperson E., Ram D., Moskovitz M. Oral health care delivery for children during COVID-19 pandemic: a retrospective study. Front Public Health. 2021;9(504) doi: 10.3389/fpubh.2021.637351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Knorst J.K., Brondani B., Tomazoni F., et al. COVID-19 pandemic reduces the negative perception of oral health-related quality of life in adolescents. Qual Life Res. 2021;30(6):1685–1691. doi: 10.1007/s11136-021-02757-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel N., Viswanathan A., Lee J., et al. Paediatric dental A&E service during the COVID-19 pandemic in the Greater London area. Eur Arch Paediatr Dent. 2021;22(3):507–513. doi: 10.1007/s40368-020-00589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention . Centers for Disease Control and Prevention, US Department of Health and Human Services; 2019. Oral Health Surveillance Report: Trends in Dental Caries and Sealants, Tooth Retention, and Edentulism, United States, 1999–2004 to 2011–2016. [Google Scholar]
- 37.Badri P., Saltaji H., Flores-Mir C., Amin M. Factors affecting children's adherence to regular dental attendance: a systematic review. JADA. 2014;145(8):817–828. doi: 10.14219/jada.2014.49. [DOI] [PubMed] [Google Scholar]
- 38.Zhou J.Y., Elyasi M., Amin M. Associations among dental insurance, dental visits, and unmet needs of US children. JADA. 2017;148(2):92–99. doi: 10.1016/j.adaj.2016.11.013. [DOI] [PubMed] [Google Scholar]
- 39.Decker S.L. Medicaid payment levels to dentists and access to dental care among children and adolescents. JAMA. 2011;306(2):187–193. doi: 10.1001/jama.2011.956. [DOI] [PubMed] [Google Scholar]
- 40.Mofidi M., Rozier R.G., King R.S. Problems with access to dental care for Medicaid-insured children: what caregivers think. Am J Public Health. 2002;92(1):53–58. doi: 10.2105/ajph.92.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Guarnizo-Herreño C.C., Lyu W., Wehby G.L. Children's oral health and academic performance: evidence of a persisting relationship over the last decade in the United States. J Pediatr. 2019;209:183–189.e182. doi: 10.1016/j.jpeds.2019.01.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Guarnizo-Herreño C.C., Wehby G.L. Children's dental health, school performance, and psychosocial well-being. J Pediatr. 2012;161(6):1153–1159. doi: 10.1016/j.jpeds.2012.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sheiham A. Dental caries affects body weight, growth and quality of life in pre-school children. Br Dent J. 2006;201(10):625–626. doi: 10.1038/sj.bdj.4814259. [DOI] [PubMed] [Google Scholar]
- 44.Watt R.G., Mathur M.R., Aida J., Bonecker M., Venturelli R., Gansky S.A. Oral health disparities in children: a canary in the coalmine? Pediatr Clin North Am. 2018;65(5):965–979. doi: 10.1016/j.pcl.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 45.Clark S.J., Freed G.L., Singer D.C., Gebremariam A., Schultz D.S.L. Pandemic-posed challenges to children's oral health. Mott Poll Report. 2021;38(1) [Google Scholar]