Abstract
During a pandemic, it is important to know whether social capital can mitigate the risk of mental disorders, given the restrictions on social interactions. However, evidence using longitudinal data is scarce. This study examined the association between pre-pandemic social capital and depressive symptoms during COVID-19 among older adults. We used longitudinal data from the Japan Gerontological Evaluation Study (JAGES), including 8291 participants aged 65 or older who were physically and cognitively independent and not depressed at baseline. We conducted baseline and follow-up mail surveys in ten municipalities in Japan from November 2019 to January 2020 (pre-pandemic period) and from November 2020 to February 2021 (pandemic period), respectively. We measured depressive symptoms using the 15-item Geriatric Depression Scale. Social capital was measured with three validated subscales, namely, civic participation, social cohesion, and reciprocity. We performed a multilevel logistic regression analysis to examine the association. A total of 1089 (13.1%) participants newly developed depressive symptoms during the pandemic. The logistic regression showed that pre-pandemic individual-level social cohesion (odds ratio = 0.79, 95% confidence interval: 0.73 to 0.86) and reciprocity (0.89, 0.82 to 0.96) and community-level reciprocity (0.93, 0.88 to 0.98) were negatively associated with the odds of depressive symptoms. Even after adjusting for declines in social capital during the pandemic, the observed associations of pre-pandemic social capital remained. Fostering social cohesion and reciprocity may increase resilience to mental disorders during a pandemic of infectious disease.
Keywords: COVID-19, Depressive symptoms, Social cohesion, Reciprocity, Japanese older adults
1. Introduction
The COVID-19 pandemic affected people's mental health, as shown by previous longitudinal studies (Prati and Mancini, 2021). The fear of infection directly induced anxiety, and stay-at-home orders and physical distancing measures had unintended consequences for mental health (Marroquín et al., 2020; Niedzwiedz et al., 2021; Sato et al., 2021). The occurrence of mental disorders was heterogeneous, and we observed the following risk factors for such diseases: female gender, motherhood, adolescence, low socioeconomic status, unemployment, and preexisting mental and physical illness (Iob et al., 2020; Pierce et al., 2020; Racine et al., 2021; Xiong et al., 2020). Older adults are among the groups most vulnerable to mental disorders during the pandemic because they are likely to have chronic diseases and are, therefore, at high risk of developing severe complications from COVID-19 (ECDC Public Health Emergency Team et al., 2020; Petrilli et al., 2020). Family members who live apart from their older parents avoided visiting them for fear of infecting them. Older adults refrained from interacting with their relatives and friends, which led to social isolation and loneliness (Wu, 2020). A previous longitudinal study in England showed that older adults with physical impairments had a higher risk of depression, anxiety, and loneliness than those without physical impairment (Steptoe and Di Gessa, 2021). However, evidence on the general older population is lacking, and the ways of increasing resilience to mental disorders during the current pandemic are still unclear.
One of the potential preparations for difficult times is building social capital, defined as “resources that are accessed by individuals as a result of their membership of a network or a group” (Kawachi and Berkman, 2014). An ecological study found that bonding (in-group) and linking (vertical) social capital were negatively associated with excess death rates from COVID-19 across the United States counties (Fraser et al., 2021). In terms of mental health, high levels of pre-disaster cognitive social capital (i.e., trust in community, a sense of mutual support, and community attachment) were associated with decreased risk of posttraumatic stress disorder and depressive symptoms after two major earthquakes in Japan (Hikichi et al., 2016; Sato et al., 2020). Nonetheless, whether social capital can prevent mental disorders even during a pandemic of infectious disease is understudied. Stay-at-home orders and physical distancing measures limit people's social interactions and can inhibit benefits from social capital on mental health. Indeed, it was observed that the frequency of real-time contact reduced during the pandemic in England (Steptoe and Di Gessa, 2021) and that social capital measured at the individual and community levels decreased during the city lockdown in China (Luo et al., 2021). A recent study suggested that perceived neighborhood cohesion was negatively associated with depressive symptoms (Robinette et al., 2021). However, it failed to consider the time-varying effects of social capital owing to the cross-sectional study design; those with mental disorders during the pandemic may have less access to social resources than those without disorders. Thus, a longitudinal study examining the association between social capital and mental health during the pandemic is needed.
Using data from a longitudinal study of Japanese older adults, this study explored the association between pre-pandemic social capital and depressive symptoms during the COVID-19 pandemic. We also investigated whether the association of pre-pandemic social capital would remain after adjusting for its declines during the pandemic. Following a previous study (Saito et al., 2016), we assessed social capital using three subscales (i.e., civic participation, social cohesion, and reciprocity). Then, we evaluated how they were differently associated with the risk of depressive symptoms.
2. Methods
2.1. The spread of COVID-19 infection in Japan and the government's response
The first case of COVID-19 in Japan was reported on January 16, 2020. On January 30, 2020, the World Health Organization declared that the outbreak of COVID-19 constitutes a Public Health Emergency of International Concern. The infection rapidly spread in Japan from March 2020. In our study sites, the monthly average of new cases rose from 10.6 (April–October 2020) to 55.3 per 100,000 people (November 2020–February 2021; the period of a follow-up survey in this study) (see Supplementary Table S1 for details). The government declared a state of emergency twice during the study period (the first period: April 7, 2020–May 25, 2020; the second period: January 8, 2021–March 21, 2021). These declarations did not entail any legally enforceable stipulations, and the government requested people to refrain from going out unnecessarily during the two periods. The population complied with the requirement, and there was a 60%–80% reduction in the number of people in major cities going out during the first period of the declaration (Agoop Corp, 2020). In the present study, we followed up with the study participants before and after the first period of the declaration.
2.2. Participants
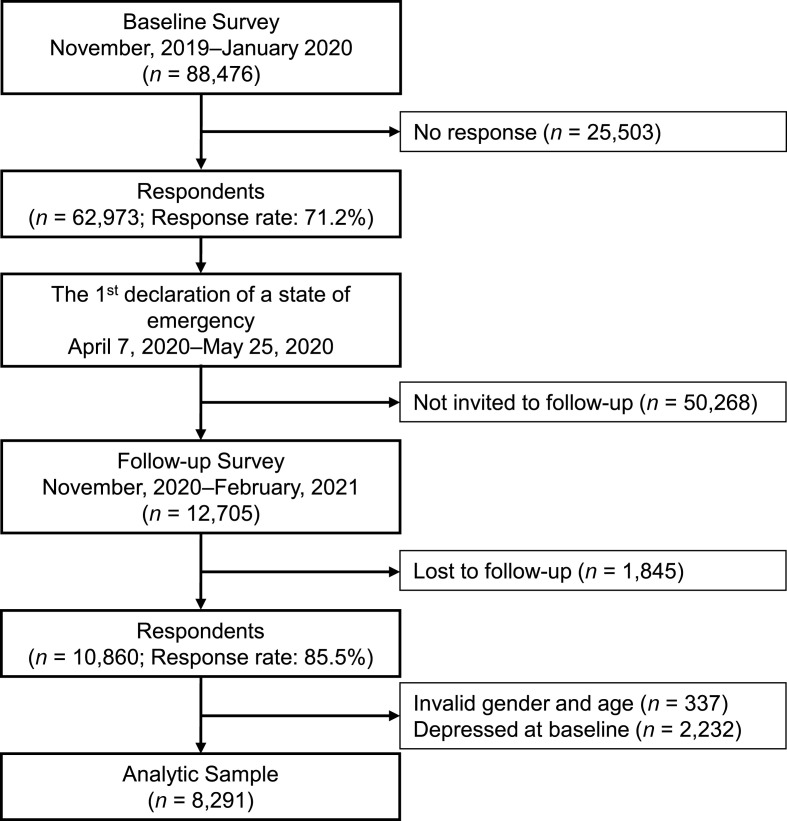
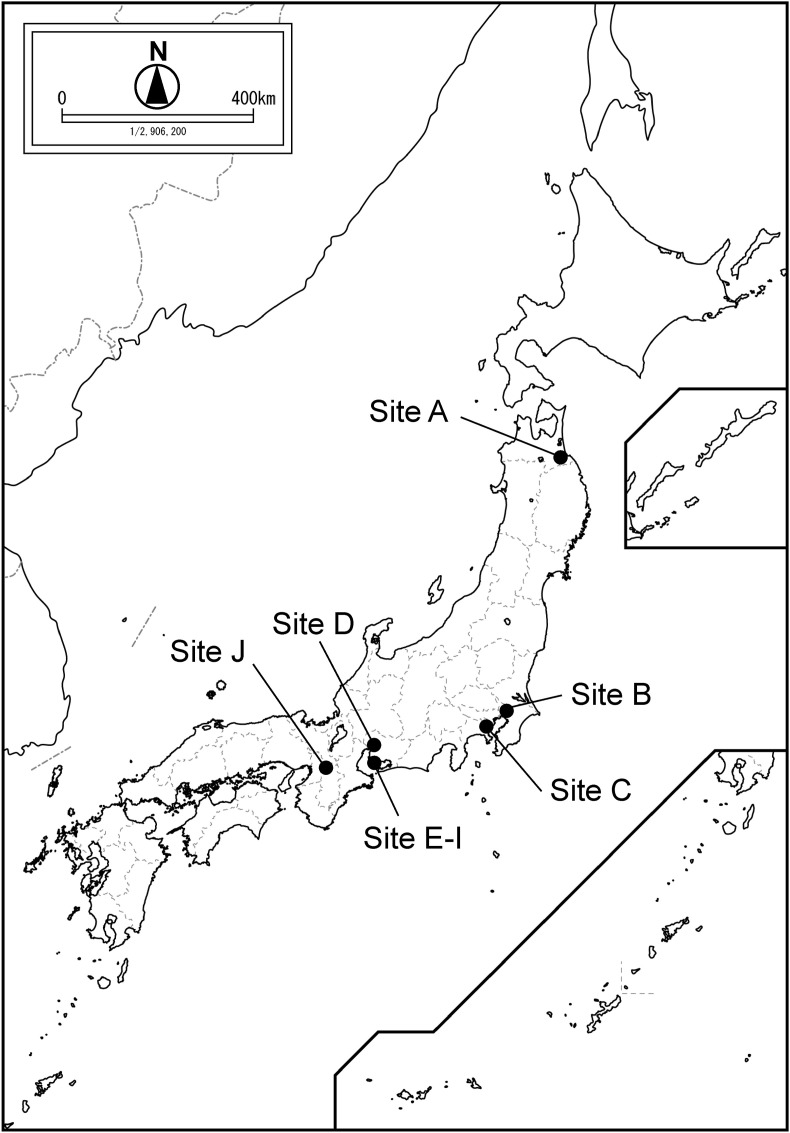
Our data were collected as a part of the Japan Gerontological Evaluation Study. This is an ongoing nationwide longitudinal study of people aged 65 or older who are physically and cognitively independent (i.e., not certified as needing assistance from public long-term care insurance) in Japan. Fig. 1 depicts a flow chart of our sample. At baseline survey, we mailed self-report questionnaires to eligible residents using random sampling methods in ten municipalities whose officials agreed to participate, from November 2019 to January 2020. Fig. 2 illustrates the locations of the study sites, and Supplementary Table S1 shows their characteristics. Of 88,476 residents invited, 62,973 returned the questionnaires, corresponding to a response rate of 71.2%. A follow-up survey was conducted from November 2020 to February 2021. We randomly selected 12,705 residents who responded to the baseline survey and mailed questionnaires to them. Out of the invited residents, 10,860 returned the questionnaires to the follow-up survey, corresponding to a follow-up rate of 85.5%. We excluded 337 respondents whose gender and age could not be confirmed or were reported in error. In addition, 2232 respondents who reported depressive symptoms at baseline (i.e., their score on the 15-item Geriatric Depression Scale (Burke et al., 1991; Wada et al., 2003) was five or higher) were also excluded from the analysis. Thus, we studied the average sample of 8291 participants who were at risk of depressive symptoms during the study period (we imputed missing values of depressive symptoms at baseline using multiple imputations, and samples varied in size between 8277 and 8317 across imputations; the average sample size was 8291).
Fig. 1.
A flow-chart of the analytic sample.
Fig. 2.
Study sites in Japan.
2.3. Depressive symptoms
Depressive symptoms were measured using the 15-item Geriatric Depression Scale and considered participants with a score of five or higher as presenting depressive symptoms (the area under the curve = 0.98, sensitivity = 0.97, and specificity = 0.95), based on a previous validation study (Nyunt et al., 2009).
2.4. Social capital
We measured social capital at the individual and community levels in three scales, as validated by a previous study: civic participation, social cohesion, and reciprocity (Saito et al., 2016). Civic participation was represented as the number of groups (sports groups, hobby groups, study or cultural groups, volunteer groups, and skills teaching groups) that participated more than once a month. Social cohesion was represented as the number of the following items for which participants answered “moderately agree” or “strongly agree” on a five-point Likert scale: “Do you think people living in your community can be trusted in general?”, “Do you think people living in your community try to help others in most situations?” and “How attached are you to the community you live in?” Reciprocity was represented as the number of affirmative responses to the following items: “Do you have someone who listens to your concerns and complaints?”, “Do you listen to someone's concerns or complaints?” and “Do you have someone who looks after you when you are sick and confined to a bed for a few days?” The Likert scale of each of the three scales ranged from 0 to 3 (those who participated in three or more groups were assigned the value of 3).
We used the average score of individual responses within an elementary school district as community-level social capital (Saito et al., 2016). The board of education in each municipality establishes the boundary of an elementary school district. It often coincides with the socio-geographic area of a former village where residents helped each other with farm work, shared common facilities such as shrines, temples, and community centers, and enjoyed local festivals and other cultural events (Aida et al., 2009). We included 455 districts within the ten municipalities; each district had 18.2 participants on average. The scores of the individual- and community-level social capital were standardized to z-scores.
2.5. Other covariates
We adjusted for potential confounders measured at baseline: gender; age; educational attainment (low: ≤ 9 years, middle: 10–12 years, high: ≥ 13 years); annual equivalized household income (low: < 2.0, middle: 2.0–4.0, high: ≥ 4.0 [million Japanese Yen]); married or other; living alone or not; employed or not; having a preexisting illness or not; instrumental activities of daily living measured using the Tokyo Metropolitan Institute of Gerontology Index of Competence (independent: 5 points, dependent: ≤ 4 points) (Koyano et al., 1991). We also included municipality-level variables: population density obtained from the Statistical Observations of Municipalities in 2019 compiled by Ministry of Internal Affairs and Communications; the monthly average of new cases of COVID-19 from November 2020 to February 2021 per 100,000 people obtained from the websites of municipalities or prefectures (accessed on December 3, 2021).
2.6. Statistical analysis
We conducted a multilevel logistic regression analysis with random intercepts to examine the association between pre-pandemic social capital and depressive symptoms during the pandemic. The data had a three-level hierarchical structure; individuals at level 1 were nested within communities at level 2, nested within municipalities at level 3. In Model 1, we adjusted for the three scales of the individual- and community-level social capital measured at baseline. In Model 2, we additionally adjusted for changes in the social capital scores (i.e., the social capital score at baseline minus the score at follow-up) to investigate whether pre-pandemic social capital was independently associated with depressive symptoms even when social capital levels decreased during the pandemic.
We were unable to follow up with some participants; thus, stabilized inverse probability of attrition weighting was adopted to address the potential attribution bias. The participants who were successfully followed up were weighted by fractions with the numerator as the percentage of participants who could be followed up and the denominator as the probability of followed for that individual estimated by logistic regression using all the covariates and fixed effects of municipalities. Compared to those who were lost to follow up, those who were followed up were more likely to be men, married, with high levels of education, household income, individual- and community-level civic participation, individual-level social cohesion, and less likely to be living alone and depressed at baseline. After weighting, these observed characteristics were well balanced between the two groups (Supplementary Table S2).
Missing values were imputed using multiple imputation by chained equations with ten imputed datasets, assuming that the data were missing at random (i.e., a missing mechanism is related to other observed variables). The percentage of missing values for each variable ranged from 0.0% to 18.5% (see Supplementary Table S3 for details). We calculated robust standard errors. All analyses were performed with STATA, version 16.1 (Stata Corp, College Station, TX).
3. Results
Table 1 describes the participants’ characteristics. The score of civic participation decreased during the pandemic, whereas social cohesion increased at the individual level. The score of individual reciprocity did not change markedly. We found similar tendencies at the community-level social capital. Among the participants, 1089 (13.1%) newly developed depressive symptoms.
Table 1.
Characteristics of participants.
| N | % | Mean | SD | |
|---|---|---|---|---|
| Individual-level variables (N = 8291)a | ||||
| Gender (men) | 4131 | 49.8 | ||
| Age, years | 74.9 | 5.91 | ||
| Education | ||||
| Low | 1574 | 19.0 | ||
| Middle | 3422 | 41.3 | ||
| High | 3295 | 39.7 | ||
| Household income | ||||
| Low | 3204 | 38.6 | ||
| Middle | 3707 | 44.7 | ||
| High | 1380 | 16.6 | ||
| Married | 6209 | 74.9 | ||
| Living alone | 1244 | 15.0 | ||
| Employed | 2390 | 28.8 | ||
| Having preexisting illness | 1764 | 21.3 | ||
| Independence of IADL | 7791 | 94.0 | ||
| Social capital, pointsb | ||||
| Civic participation (baseline) | 1.03 | 1.09 | ||
| Civic participation (follow-up) | 0.87 | 1.03 | ||
| Social cohesion (baseline) | 2.17 | 1.00 | ||
| Social cohesion (follow-up) | 2.22 | 0.97 | ||
| Reciprocity (baseline) | 2.88 | 0.45 | ||
| Reciprocity (follow-up) | 2.87 | 0.45 | ||
| Depressive symptoms (follow-up) | 1089 | 13.1 | ||
| Community-level variables (N = 455) | ||||
| Number of participants within a district | 18.2 | 19.4 | ||
| Social capital, pointsc | ||||
| Civic participation (baseline) | 0.93 | 0.31 | ||
| Civic participation (follow-up) | 0.76 | 0.28 | ||
| Social cohesion (baseline) | 1.97 | 0.32 | ||
| Social cohesion (follow-up) | 2.01 | 0.31 | ||
| Reciprocity (baseline) | 2.80 | 0.16 | ||
| Reciprocity (follow-up) | 2.79 | 0.16 | ||
| Municipality-level variables (N = 10) | ||||
| Population density, person/km2 | 3944.2 | 2936.9 | ||
| Monthly average number of new cases d | ||||
| Before the follow-up | 10.6 | 5.7 | ||
| Follow-up period | 55.3 | 29.6 | ||
Abbreviations: SD, standard deviation; IADL, instrumental activities of daily living.
Imputed data were used. Participants who were not depressed at baseline varied between 8277 and 8317 across imputations. The average sample size was 8,291.
P-values for paired t-test between the baseline and the follow-up of individual-level civic participation, social cohesion, and reciprocity were <0.001, 0.001, and 0.22, respectively.
P-values for paired t-test between the baseline and the follow-up of community-level civic participation, social cohesion, and reciprocity were <0.001, 0.052, and 0.23, respectively.
Per 100,000 people. The period before the follow-up was from April to October 2020, whereas the follow-up period was from November 2020 to February 2021.
Table 2 presents the results of a multilevel logistic regression examining the association between depressive symptoms and social capital. In Model 1, individual-level pre-pandemic social cohesion (odds ratio = 0.79, 95% confidence interval: 0.73 to 0.86) and reciprocity (0.89, 0.82 to 0.96) were negatively associated with the odds for depressive symptoms. Community-level pre-pandemic reciprocity was also associated with a reduced risk of depressive symptoms (0.93, 0.88 to 0.98). After adjusting for changes in the scores of social capital during the pandemic in Model 2, individual-level pre-pandemic social capital was independently associated with decreased odds for depressive symptoms in the three scales (civic participation: 0.85, 0.75 to 0.97; social cohesion: 0.66, 0.61 to 0.72; reciprocity: 0.82, 0.75 to 0.89). During the pandemic, declines in the scores of social capital at the individual level were associated with an increased risk of depressive symptoms (civic participation: 1.23, 1.16 to 1.31; social cohesion: 1.47, 1.35 to 1.60; reciprocity: 1.20, 1.12 to 1.29). At the community level, we found an independent association between pre-pandemic reciprocity and reduced risk of depressive symptoms (0.92, 0.87 to 0.97).
Table 2.
Multilevel logistic regression for depressive symptoms during the pandemic.
| Model 1 |
Model 2 |
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Individual-level social capital | ||||||
| Pre-pandemic civic participation | 0.92 | 0.83 | 1.03 | 0.85 | 0.75 | 0.97 |
| Pre-pandemic social cohesion | 0.79 | 0.73 | 0.86 | 0.66 | 0.61 | 0.72 |
| Pre-pandemic reciprocity | 0.89 | 0.82 | 0.96 | 0.82 | 0.75 | 0.89 |
| Changes in civic participation | 1.23 | 1.16 | 1.31 | |||
| Changes in social cohesion | 1.47 | 1.35 | 1.60 | |||
| Changes in reciprocity | 1.20 | 1.12 | 1.29 | |||
| Community-level social capital | ||||||
| Pre-pandemic civic participation | 0.99 | 0.93 | 1.06 | 0.97 | 0.90 | 1.04 |
| Pre-pandemic social cohesion | 1.00 | 0.94 | 1.06 | 1.04 | 0.97 | 1.11 |
| Pre-pandemic reciprocity | 0.93 | 0.88 | 0.98 | 0.92 | 0.87 | 0.97 |
| Changes in civic participation | 1.05 | 0.95 | 1.16 | |||
| Changes in social cohesion | 0.97 | 0.91 | 1.03 | |||
| Changes in reciprocity | 1.03 | 0.99 | 1.08 | |||
All models included the following covariates: gender, age, educational attainment, annual equivalized household income, marital status, living alone, employment status, preexisting illness, instrumental activities of daily living, population density, and the monthly average of new cases of COVID-19 during the follow-up; changes in social capital were calculated as the score of social capital at baseline minus the score at follow-up. We used stabilized inverse probability of attrition weighting.
Abbreviations: OR, odds ratio; CI, confidence interval.
To check the robustness of the results, we performed the same analyses, including the data of those who were depressed at baseline (n = 10,523), adjusting the baseline depressive symptoms categorized into three states using the 15-item Geriatric Depression Scale (0–4: not depressed; 5–9: moderately depressed; 10 or higher: severely depressed (Shin et al., 2019)). We found more conservative point estimates for the individual-level social capital and similar results for the community-level social capital (Supplementary Table S4). We also performed complete case analyses (i.e., using data from participants without missing values [n = 4470]) and obtained similar results (Supplementary Table S5).
4. Discussion
This study explored whether pre-pandemic social capital was protective against the risk of depressive symptoms during the COVID-19 pandemic using longitudinal data of Japanese older adults. We found that individual-level social cohesion and reciprocity and community-level reciprocity were negatively associated with the odds for depressive symptoms.
This study adopted a validated scale of social capital that conceptualized it with three subscales: civic participation, social cohesion, and reciprocity (Saito et al., 2016). The unadjusted results of the study indicated that the mean score of individual-level civic participation decreased during the pandemic, whereas the social cohesion score increased and the reciprocity score did not change. We interpret these findings as indicating that stay-at-home orders and physical distancing measures significantly impacted civic participation, but the other two aspects of social capital had been sustained or had somewhat improved through cooperative actions such as preventive behaviors and information exchanges during this difficult time. In theory, the concept of social capital can be divided into a structural dimension and a cognitive dimension (Harpham et al., 2002; Islam et al., 2006; McKenzie et al., 2002). The scale of civic participation we used represents a structural dimension that refers to the extent and intensity of engagement in community activities, while the scale of social cohesion represents a cognitive dimension that reflects subjective trust, mutual support, and community attachment, all of which foster cooperative behaviors. The subscale named “reciprocity” consists of receiving and providing emotional support and receiving instrumental support. It can be categorized as a structural component because it measures externally observable aspects of network connections (Islam et al., 2006; Saito et al., 2016), while it can also be categorized as a cognitive component because the concept of reciprocity and social supports are considered subjective matters in another definition (Harpham et al., 2002). In the present study, we found that individual-level social cohesion and reciprocity were more clearly associated with a decreased risk of depressive symptoms than civic participation. Our findings are in line with previous reviews that found consistent negative associations of cognitive social capital and mixed evidence on the effect of structural social capital on mental health (De Silva et al., 2005; Ehsan and De Silva, 2015). In addition, this study showed that the preferable associations of pre-pandemic individual-level social cohesion and reciprocity remained after adjusting for changes in social capital during the pandemic. Thus, fostering social cohesion and reciprocity in peace times may be beneficial in increasing resilience to mental health problems during pandemics of infectious disease.
This study considered not only individual-level social capital but also community-level social capital and found that pre-pandemic reciprocity at the community level was independently associated with decreased odds for depressive symptoms, regardless of individual socioeconomic condition and individual perceptions of community social capital. The concept of reciprocity as social capital was demonstrated to be similar to the concept of social support when it was measured at the individual level (Kawachi and Berkman, 2014; Saito et al., 2016). At the individual level, reciprocity represents an ego-centric network that provides support via close and strong ties. However, such individualistic views cannot fully explain variations in mental health outcomes between communities (Hikichi et al., 2016; Lowe et al., 2015; Sato et al., 2020; Wind and Komproe, 2012). In contrast to individualistic reciprocity, the measure at the community level reflects a contextual effect derived from belongingness to a community embracing weak ties; in other words, social capital has positive externalities (spillover effects) (Kawachi and Berkman, 2014). The sense of security that one can rely on neighbors in case of emergency can induce a protective effect on mental health during a pandemic, even for individuals who have limited access to social support. Compared to community-level reciprocity, community-level social cohesion did not correlate with depressive symptoms. As for social cohesion, the individual-level variable appeared to explain most of the variation in depressive symptoms. In a contingency situation, such as an infectious disease outbreak, the aspect of social capital that promotes exchanging tangible supports within the community (i.e., reciprocity) may explain better the regional variation in the incidence of depression than social cohesion.
This study has several limitations. First, the study findings may lack generalizability because we studied a Japanese population. Japanese measures for COVID-19 were less stringent than other countries that implemented city lockdowns. However, our findings are still informative for other countries because most of the population followed the government's stay-at-home requirement, which was without legal enforcement (Agoop Corp, 2020). Second, we could not obtain information on those who did not respond to the baseline survey; thus, there could be a selection bias. However, the response rate of over 70% for the baseline survey was higher than response rates in similar studies of older adults (Santos-Eggimann et al., 2009). In addition, we addressed an attrition bias at the follow-up survey by adopting inverse probability of attrition weighting and successfully balanced observable characteristics of participants between those who could be followed up and those who were lost to follow up. Third, we measured outcomes and exposures using self-reported questionnaires, and thus reporting errors could have occurred. Nonetheless, the measures we used have been well-validated and widely used in studies of older populations (Burke et al., 1991; Saito et al., 2016; Wada et al., 2003).
Despite these limitations, our study has significant strengths. First, we could assess levels of social capital and the status of mental health at the pre-pandemic period. The longitudinal data enabled us to obtain results without recall bias and confounding with mental health status during the pandemic. Second, we could conduct nationwide mail surveys using rigorous random sampling methods, collaborating with the participating municipalities. Unlike early findings of COVID-19 using the Internet survey, our results provide representative inferences within the study sites, including older adults who cannot use the Internet. Third, the questionnaires of the Japan Gerontological Evaluation Study were developed to harmonize with other studies, such as the English Longitudinal Study of Ageing (Aida et al., 2018; Noguchi et al., 2021). We expect that further international comparative studies will confirm the generalizability of our findings to other countries, including England, which introduced stricter measures for physical distancing than Japan.
In conclusion, our findings showed that individual-level social cohesion and reciprocity and community-level reciprocity were associated with decreased odds of depressive symptoms. The associations were robust even after considering changes in social capital during the COVID-19 pandemic. Policies and interventions fostering social cohesion and reciprocity may be more beneficial in preventing depression than civic participation given the restricted social interactions during pandemics of infectious diseases. For example, establishing relationships where neighbors can support older adults when they need help would mitigate anxiety and loneliness during a pandemic. Moreover, equipping the older population with devices and skills to use information and communication technologies will enable them to maintain social connections with their relatives and friends and receive professional assistance such as counseling and information provision. Our findings provide valuable insights on how to prepare for pandemics of unknown infectious diseases that will potentially occur in the future.
Ethical statement
This study was reviewed and approved by the ethics committees of Kyoto University (R3153), the National Center for Geriatrics and Gerontology (1274-2), and Chiba University (3442). The study was conducted in accordance with the principles of the Declaration of Helsinki and its later amendments. All participants provided written informed consent when they returned a questionnaire.
CRediT author statement
Koryu Sato: Conceptualization, Methodology, Software, Formal analysis, Investigation, Writing – Original Draft, Funding Acquisition.: Naoki Kondo: Writing – Review & Editing, Supervision.: Katsunori Kondo: Investigation, Writing – Review & Editing, Project Administration, Funding Acquisition.
Funding
This study used data from the Japan Gerontological Evaluation Study, which was supported by the Japan Society for the Promotion of Sciences (15H01972, 20K18931, 21K10323), the Japanese Ministry of Health, Labour and Welfare (H28-Choju-Ippan-002), the Japan Agency for Medical Research and Development (JP18dk0110027, JP18ls0110002, JP18le0110009, JP19dk0110034, JP20dk0110034), and the National Center for Geriatrics and Gerontology (29–42). Surveys in some municipalities were partially funded by the municipal resources. The funders played no role in the design and conduct of the study; the management, analysis, and interpretation of the data; the preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Declaration of competing interest
There are no conflicts of interest to declare.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.healthplace.2022.102772.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Aida J., Hanibuchi T., Nakade M., Hirai H., Osaka K., Kondo K. The different effects of vertical social capital and horizontal social capital on dental status: a multilevel analysis. Soc. Sci. Med. 2009;69(4):512–518. doi: 10.1016/j.socscimed.2009.06.003. 1982. [DOI] [PubMed] [Google Scholar]
- Aida J., Cable N., Zaninotto P., Tsuboya T., Tsakos G., Matsuyama Y., Ito K., Osaka K., Kondo K., Marmot M.G., Watt R.G. Social and behavioural determinants of the difference in survival among older adults in Japan and England. Gerontology. 2018;64(3):266–277. doi: 10.1159/000485797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke W.J., Roccaforte W.H., Wengel S.P. The short form of the geriatric depression scale: a comparison with the 30-item form. J. Geriatr. Psychiatr. Neurol. 1991;4(3):173–178. doi: 10.1177/089198879100400310. [DOI] [PubMed] [Google Scholar]
- Corp Agoop. 2020. Analysis of Human Flow Changes in the Spread of a Novel Coronavirus.https://corporate-web.agoop.net/pdf/covid-19/agoop_analysis_coronavirus.pdf [Google Scholar]
- De Silva M.J., McKenzie K., Harpham T., Huttly S.R.A. Social capital and mental illness: a systematic review. J. Epidemiol. Commun. Health. 2005;59(8):619–627. doi: 10.1136/jech.2004.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ECDC Public Health Emergency Team, Danis K., Fonteneau L., Georges S., Daniau C., Bernard-Stoecklin S., Domegan L., O'Donnell J., Hauge S.H., Dequeker S., Vandael E., Van der Heyden J., Renard F., Sierra N.B., Ricchizzi E., Schweickert B., Schmidt N., Abu Sin M., Eckmanns T., Schneider E. High impact of COVID-19 in long-term care facilities, suggestion for monitoring in the EU/EEA. Euro Surveill.: Bulletin Europeen Sur Les Maladies Transmissibles = Eur. Commun. Dis. Bull. 2020;25(22) doi: 10.2807/1560-7917.ES.2020.25.22.2000956. May 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehsan A.M., De Silva M.J. Social capital and common mental disorder: a systematic review. J. Epidemiol. Commun. Health. 2015;69(10):1021–1028. doi: 10.1136/jech-2015-205868. [DOI] [PubMed] [Google Scholar]
- Fraser T., Aldrich D.P., Page-Tan C. Bowling alone or distancing together? The role of social capital in excess death rates from COVID19. Soc. Sci. Med. 2021;284:114241. doi: 10.1016/j.socscimed.2021.114241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harpham T., Grant E., Thomas E. Measuring social capital within health surveys: key issues. Health Pol. Plann. 2002;17(1):106–111. doi: 10.1093/heapol/17.1.106. [DOI] [PubMed] [Google Scholar]
- Hikichi H., Aida J., Tsuboya T., Kondo K., Kawachi I. Can community social cohesion prevent posttraumatic stress disorder in the aftermath of a disaster? A natural experiment from the 2011 tohoku earthquake and tsunami. Am. J. Epidemiol. 2016;183(10):902–910. doi: 10.1093/aje/kwv335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iob E., Frank P., Steptoe A., Fancourt D. Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Netw. Open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.26064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.K., Merlo J., Kawachi I., Lindström M., Gerdtham U.-G. Social capital and health: does egalitarianism matter? A literature review. Int. J. Equity Health. 2006;5:3. doi: 10.1186/1475-9276-5-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Berkman L.F. In: Social Epidemiology. second ed. Berkman L.F., Kawachi I., Glymour M.M., editors. Oxford University Press; 2014. Social capital, social cohesion, and health; pp. 290–319. [Google Scholar]
- Koyano W., Shibata H., Nakazato K., Haga H., Suyama Y. Measurement of competence: reliability and validity of the TMIG Index of competence. Arch. Gerontol. Geriatr. 1991;13(2):103–116. doi: 10.1016/0167-4943(91)90053-S. [DOI] [PubMed] [Google Scholar]
- Lowe S.R., Joshi S., Pietrzak R.H., Galea S., Cerdá M. Mental health and general wellness in the aftermath of Hurricane Ike. Soc. Sci. Med. 2015;124:162–170. doi: 10.1016/j.socscimed.2014.11.032. 1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo M., Zhang D., Shen P., Yin Y., Yang S., Jia P. COVID-19 lockdown and social capital changes among youths in China. Int. J. Health Pol. Manag. 2021 doi: 10.34172/ijhpm.2021.17. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marroquín B., Vine V., Morgan R. Mental health during the COVID-19 pandemic: effects of stay-at-home policies, social distancing behavior, and social resources. Psychiatr. Res. 2020;293:113419. doi: 10.1016/j.psychres.2020.113419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie K., Whitley R., Weich S. Social capital and mental health. Br. J. Psychiatr.: J. Ment. Sci. 2002;181:280–283. doi: 10.1192/bjp.181.4.280. [DOI] [PubMed] [Google Scholar]
- Niedzwiedz C.L., Green M.J., Benzeval M., Campbell D., Craig P., Demou E., Leyland A., Pearce A., Thomson R., Whitley E., Katikireddi S.V. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J. Epidemiol. Commun. Health. 2021;75(3):224–231. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noguchi T., Saito M., Aida J., Cable N., Tsuji T., Koyama S., Ikeda T., Osaka K., Kondo K. Association between social isolation and depression onset among older adults: a cross-national longitudinal study in England and Japan. BMJ Open. 2021;11(3) doi: 10.1136/bmjopen-2020-045834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyunt M.S.Z., Fones C., Niti M., Ng T.-P. Criterion-based validity and reliability of the Geriatric Depression Screening Scale (GDS-15) in a large validation sample of community-living Asian older adults. Aging Ment. Health. 2009;13(3):376–382. doi: 10.1080/13607860902861027. [DOI] [PubMed] [Google Scholar]
- Petrilli C.M., Jones S.A., Yang J., Rajagopalan H., O'Donnell L., Chernyak Y., Tobin K.A., Cerfolio R.J., Francois F., Horwitz L.I. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. Br. Med. J. 2020;369 doi: 10.1136/bmj.m1966. m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M., Hope H., Ford T., Hatch S., Hotopf M., John A., Kontopantelis E., Webb R., Wessely S., McManus S., Abel K.M. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatr. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G., Mancini A.D. The psychological impact of COVID-19 pandemic lockdowns: a review and meta-analysis of longitudinal studies and natural experiments. Psychol. Med. 2021;51(2):201–211. doi: 10.1017/S0033291721000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine N., Hetherington E., McArthur B.A., McDonald S., Edwards S., Tough S., Madigan S. Maternal depressive and anxiety symptoms before and during the COVID-19 pandemic in Canada: a longitudinal analysis. Lancet Psychiatr. 2021;8(5):405–415. doi: 10.1016/S2215-0366(21)00074-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinette J.W., Bostean G., Glynn L.M., Douglas J.A., Jenkins B.N., Gruenewald T.L., Frederick D.A. Perceived neighborhood cohesion buffers COVID-19 impacts on mental health in a United States sample. Soc. Sci. Med. 2021;285:114269. doi: 10.1016/j.socscimed.2021.114269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito M., Kondo N., Aida J., Kawachi I., Koyama S., Ojima T., Kondo K. Development of an instrument for community-level health related social capital among Japanese older people: the JAGES Project. J. Epidemiol. 2016;27:221–227. doi: 10.1016/j.je.2016.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos-Eggimann B., Cuénoud P., Spagnoli J., Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J. Gerontol.: Series A. 2009;64A(6):675–681. doi: 10.1093/gerona/glp012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato K., Amemiya A., Haseda M., Takagi D., Kanamori M., Kondo K., Kondo N. Post-disaster changes in social capital and mental health: a natural experiment from the 2016 kumamoto earthquake. Am. J. Epidemiol. 2020 doi: 10.1093/aje/kwaa041. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato K., Sakata R., Murayama C., Yamaguchi M., Matsuoka Y., Kondo N. Changes in work and life patterns associated with depressive symptoms during the COVID-19 pandemic: an observational study of health app (CALO mama) users. Occup. Environ. Med. 2021 doi: 10.1136/oemed-2020-106945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shin C., Park M.H., Lee S.-H., Ko Y.-H., Kim Y.-K., Han K.-M., Jeong H.-G., Han C. Usefulness of the 15-item geriatric depression scale (GDS-15) for classifying minor and major depressive disorders among community-dwelling elders. J. Affect. Disord. 2019;259:370–375. doi: 10.1016/j.jad.2019.08.053. [DOI] [PubMed] [Google Scholar]
- Steptoe A., Di Gessa G. Mental health and social interactions of older people with physical disabilities in England during the COVID-19 pandemic: a longitudinal cohort study. Lancet Public Health. 2021;6(6):e365–e373. doi: 10.1016/S2468-2667(21)00069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wada T., Ishine M., Kita T., Fujisawa M., Matsubayashi K. Depression screening of elderly community‐dwelling Japanese. J. Am. Geriatr. Soc. 2003;51(9):1328–1329. doi: 10.1046/j.1532-5415.2003.514207.x. [DOI] [PubMed] [Google Scholar]
- Wind T.R., Komproe I.H. The mechanisms that associate community social capital with post-disaster mental health: a multilevel model. Soc. Sci. Med. 2012;75(9):1715–1720. doi: 10.1016/j.socscimed.2012.06.032. 1982. [DOI] [PubMed] [Google Scholar]
- Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Global Health Res. Pol. 2020;5:27. doi: 10.1186/s41256-020-00154-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.