Abstract
Introduction
Black, Hispanic, and Indigenous groups have carried the burden of COVID-19 disease in comparison to non-marginalized groups within the United States. It is important to examine the factors that have led to the observed disparities in COVID-19 risk, morbidity, and mortality. We described primary health care access within large US metropolitan cities in relation to COVID-19 rate, race/ethnicity, and income level and hypothesized that observed racial/ethnic disparities in COVID-19 rates are associated with health care provider number.
Methods
We accessed public city health department records for reported COVID-19 cases within 10 major metropolitan cities in the United States and also obtained publicly available racial/ethnic demographic median income and primary health care provider counts within individual zip codes. We made comparisons of COVID-19 case numbers within zip codes based on racial/ethnic and income makeup in relation to primary health care counts.
Results
Median COVID-19 rates differed by race/ethnicity and income. There was an inverse relationship between median income and COVID-19 rate within zip codes (rho: -0.515; p<0.001). However, this relationship was strongest within racially/ethnically non-marginalized zip codes relative to those composed mainly of racially/ethnically marginalized populations (rho: -0.427 vs. rho: -0.175 respectively). Health care provider number within zip codes was inversely associated with the COVID-19 rate. (rho: -0.157; p<0.001) However, when evaluated by stratified groups by race the association was only significant within racially/ethnically marginalized zip codes(rho: -0.229; p<0.001).
Discussion
COVID-19 case rates were associated with racial/ethnic makeup and income status within zip codes across the United States and likewise, primary care provider access also differed by these factors. However, our study reveals that structural and systemic barriers and inequities have led to disproportionate access to health care along with other factors that require identification.
Conclusion
: These results pose a concern in terms of pandemic progression into the next year and how these structural inequities have impacted and will impact vaccine distribution.
Keywords: COVID-19, Structural racism, Health disparities, Minorities, Public health
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causing the highly contagious respiratory disease Coronavirus disease 2019 (COVID-19) emerged in early 2019 and rapidly spread to pandemic levels.1 The SARS-Cov2 virus demonstrates unique characteristics leading to pervasive spread and difficulty in management as there is considerable variability in associated symptomatology which spans from asymptomatic to fatal infections.2 The United States has reported over 30 million COVID-19 cases since the first case was identified in December of 2019, and there have been over 135 million cases identified worldwide. Of those infected, over half a million people have died from COVID-19 in the United States and over three million have died worldwide.3 Most recent reports in the United States demonstrate that since peaking in January 2021, COVID-19 case rates appeared to be on the decline but have started to increase again with new variants. The decline in cases was achieved through mitigation interventions recommended by the Centers for Disease Control such as social distancing, masking, and hand hygiene. The first COVID-19 vaccine was approved for emergency use in the United States on December 11, 2020, and at the time of preparation of this manuscript over 50% of United States residents had received a COVID-19 vaccination.4
Disparities in COVID-19 disease risk, morbidity, and mortality in relation to race/ethnicity and socioeconomic barriers have been well described in the recent literature.5 An early observation within the pandemic was the disparity related to those who worked front-line jobs which did not provide the opportunity for remote work and at the same time were lower-salaried and more likely to face a furlough.6 These groups of workers, who are largely made up of those from Black, Hispanic, and overall non-white identities, were among those most impacted by COVID-19 in the United States in regard to infection risk and poorer outcomes.7 These findings demonstrate a known inequity within the United States where those who have been made most vulnerable as a result of structural inequity related to race/ethnicity (i.e. structural racism) are persistently at elevated risk during times of crisis. This harkens to past experiences on a local level such as the disproportionate impact of Hurricane Katrina in the city of New Orleans, LA in 2005 where Black residents who were already at a systemic disadvantage experienced the brunt of loss of housing and life.8 Unfortunately, the lessons from the Hurricane Katrina experience were not acted upon in addressing compounded vulnerabilities within systematically oppressed and disenfranchised populations. The novel coronavirus impact among Black and brown communities within the United States follows a continued pattern of those least protected and least able to respond as the most affected.
Inequity in access to adequate healthcare has long been described in the medical literature.9 Across the United States, zip code “hot spots'' for COVID-19 have been described. These zip codes are most often populated by Black and brown populations and are significantly impacted by known socioeconomic barriers as a result of the legacy of structural racism within the United States.10 Due to structural barriers these areas are often called a “health care desert,” which leads to not only more difficulty in accessing acute care but also the inability to address and prevent chronic disease putting these populations at further risk.
While substantial racial/ethnic disparities in COVID-19 cases have been shown to exist, it has also been described that impacted racial/ethnic groups are not inherently at increased risk due to biological makeup. Therefore, it is important to point out structural inequities that may be targeted in the future for mitigation of disproportionate risk and the overall impact of catastrophes like COVID-19 within the United States. We aimed to describe the availability of health care within large metropolitan cities within the United States and hypothesized that observed racial and ethnic disparities in COVID-19 infection and COVID-19 within the United States are associated with the social determinants of health care providers.
Methodology
Data sources
We identified the top ten populated cities in the United States based on US census data (New York City, Chicago, Houston, Phoenix, Philadelphia, San Antonio, San Diego, Dallas, San Jose, and Los Angeles)11 and collected public data to describe demographics, primary health care provider (Internal Medicine, Family Medicine, and Pediatrics) access, and COVID19 case rate data from each zip code within each city to include the following: racial/ethnic demographics, median household income, number of primary care providers, and COVID-19 infection rates. Los Angeles was replaced with Austin, the 11th most populated city in the US, in our study due to the lack of publicly available COVID-19 case data on Los Angeles. Race and ethnicity data by zip code were abstracted from https://www.zipdatamaps.com.12 Median income by zip code data was obtained from https://www.incomebyzipcode.com.13 Quantitative counts of primary care providers per zip code were obtained from https://www.healthgrades.com.14 Primary Health care providers within a five-mile radius of an individual zip code were used. COVID-19 cases per zip code were obtained from publicly available data from the state or city health department. Data were collected between December 25th, 2020, and January 4th, 2021.
Measures
The proportion of racial/ethnic groups identified as Non-Hispanic White, Hispanic/Latino, African American/Black, and Asian were calculated for each zip code; the most prevalent race/ethnicity was identified for each zip code. We categorized individual zip codes as “racially/ethnically advantaged” if they were predominantly White or Asian or “racially/ethnically disadvantaged” if they were predominantly Hispanic/Latino or African American/Black. These classifications were made based on known economic and social advantage statistics associated with these racial/ethnic groups.15
Zip codes were categorized as “financially disadvantaged” or “financially advantaged” based on median income (<$69,000 and $69,000+, respectively) which was based on 2019 U.S. Government Census information on Income and Poverty in the United States indicating an overall median household income of $68,703 within the United States.16 These categorizations of race and income were determined based on economic, health status, and educational opportunities for different ethnic groups.
Finally, the number of primary healthcare providers (Family Practice, Internal Medicine, Pediatrics) per COVID-19 cases was converted into standardized rates by divided counts by the patient population and multiplied by 100,000.
Statistical Analysis Approach
Given the inherent skewness of the COVID-19 rates, median household income, and provider rates, we present non-parametric summary distributions (i.e., medians and interquartile ranges [IQRs]). Spearman's rank correlation was calculated when examining the unadjusted correlations between COVID-19 rates, median income, and provider rates. A categorical version of the provider rate was generated based on the underlying quartile distribution. The Mann-Whitney U test was used to compare the distribution of COVID-19 cases and provider rates between advantaged and disadvantaged zip codes. Multivariable, multi-level Poisson models were run examining the relationship between standardized COVID-19 rates with our 2 binary advantaged/disadvantaged indicators (i.e., racial/ethnic distribution and median household income) and the quartile-version of provider rates; the city was treated as a random effect with an assumed compound-symmetry covariance matrix. All analyses were completed using SAS. (version 9.4; Cary, NC.)
Results and Discussion
The data from this study of 627 zip codes within the most highly populated cities in the United States demonstrated that overall COVID-19 rates are associated with primary care access, racial/ethnic advantage/disadvantage, and financial advantage/disadvantage within zip codes.
Difference in COVID-19 Cases Between Racially/Ethnically Advantaged and Disadvantaged Zip Codes
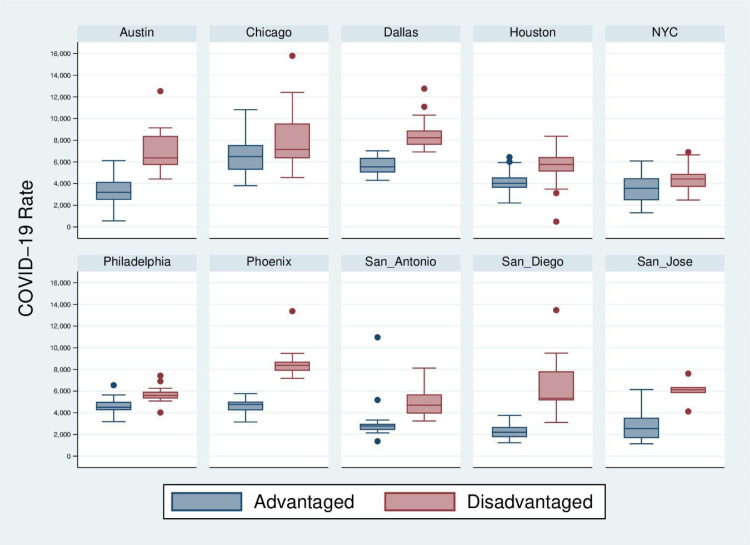
We identified 297 racially/ethnically advantaged and 330 racially/ethnically disadvantaged zip codes. Overall, the median COVID-19 rate (per 100,000 population) differed significantly between disadvantaged (5,669; IQR: 4,607-7,145) and advantaged (4,015; IQR: 2,734-5,034; p<0.001) zip codes. The higher COVID-19 rate among racially/ethnically disadvantaged zip codes was consistent for each of the 10 cities (Figure 1 ). After adjusting for financial advantage/disadvantage, the racially/ethnically disadvantaged zip codes had a significantly higher COVID-19 incidence rate (incidence rate ratio [IRR]: 1.31; 95% confidence interval [CI]: 1.30, 1.31; p<0.001)when compared to zip codes categorized as racially/ethnically advantaged.
Figure 1.
COVID-19 Case Rate Comparisons between Racially and Ethnically Advantaged vs. Disadvantaged Zip Codes
Median Income Impact on COVID-19
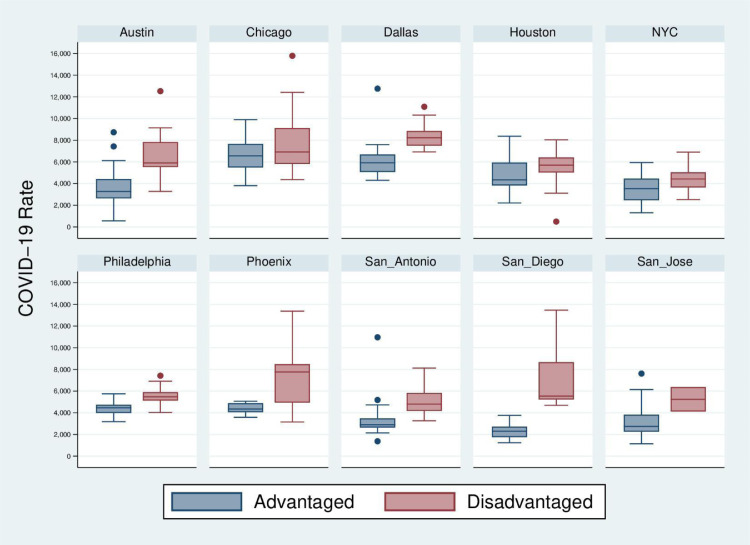
We identified 280 financially advantaged and 347 financially disadvantaged zip codes. Overall, the median COVID-19 rate (per 100,000 population) differed significantly between disadvantaged (5,525; IQR: 4,521-6,887) and advantaged (3,842; IQR: 2,659-5,013; p<0.001) zip codes. Economically disadvantaged zip codes frequently reported significantly higher COVID-19 cases than disadvantaged zip codes across cities (Figure 2 ).
Figure 2.
COVID-19 Rate and Zipcode Median Income Advantage vs. Disadvantage Classification by City
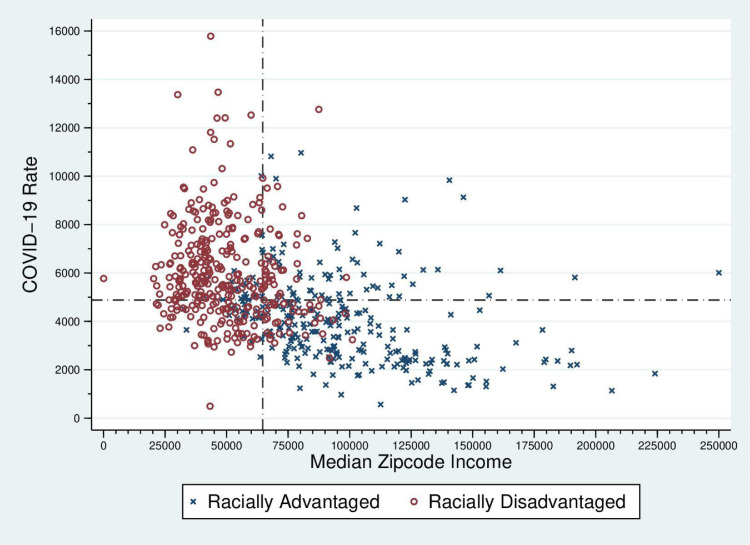
We further observed that in zip codes defined as racially/ethnically advantaged the median income was $91,138 in comparison to a median income of $46,965 in racially/ethnically disadvantaged zip codes (p <0.001). We observed a negative correlation between median income and COVID-19 rates (rho: -0.515; p<0.001). However, when stratifying the analysis by racially/ethnically advantaged in comparison to disadvantaged, the correlation was greater within racially/ethnically advantaged zip codes (rho: -0.427; p<0.001) compared to racially disadvantaged zip codes (rho: -0.175; p<0.001) (Figure 3 ).
Figure 3.
Relationship between Median Income and COVID-19 Rates by Racially and Ethnically Advantaged vs. Disadvantaged Status
After adjusting for racial/ethnic advantage/disadvantage, financially disadvantaged zip codes had significantly higher COVID-19 rates (IRR:1.15; 95% CI: 1.14, 1.15; p<0.001) compared to financially advantaged zip codes. Financially disadvantaged zip codes continued to have significantly higher COVID-19 rates even after stratifying by racially/ethnically advantaged (IRR: 1.12; 95% CI: 1.11, 1.13; p<0.001) and racially/ethnically disadvantaged (IRR: 1.08: 95% CI: 1.07, 1.09; p<0.001).
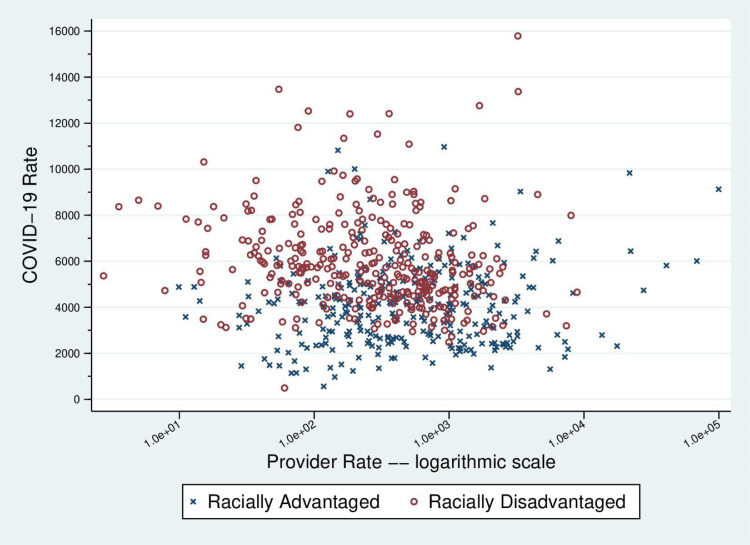
Health Care Provider Access Across Racial/Ethnic Groups
Overall, the health care provider number per zip code was associated with the COVID-19 rates (rho: -0.157; p<0.001). We further observed that those residing in racially/ethnically advantaged zip codes had, on average, 108 more primary care health providers available than those in disadvantaged neighborhoods (p <0.001). When further evaluating racial/ethnic advantage and disadvantage we observed that our initial finding of an association between health care provider number and COVID-19 rate was only significant for racially/ethnically disadvantaged zip codes (rho: -0.229; p<0.001) while non-significant for racially/ethnically advantaged (rho: 0.053; p=0.365) (Figure 4 ).
Figure 4.
Relationship between Provider Rates and COVID-19 Rates by Racially and Ethnically Advantaged vs. Disadvantaged Status
As we further explored the impact of primary healthcare provider number on COVID-19 risk, we observed that when primary healthcare provider number quantified as quartiles decreased, the COVID-19 incidence rate ratio increased. (Table 1 )
Table 1.
Quartile Comparisons of Primary Health Care Provider Numbers and Related Incidence Rate Ratios of COVID-19.
| COVID-19 Incidence Rate Ratio | P-value | 95% Confidence Interval | ||
|---|---|---|---|---|
| Provider Rate | ||||
| Quartile 1 | 1.14 | <0.0001 | 1.13-1.15 | |
| Quartile 2 | 1.08 | <0.0001 | 1.07-1.08 | |
| Quartile 3 | 1.05 | <0.0001 | 1.04-1.05 | |
| Quartile 4 | -ref- | <0.0001 | — |
The Impact of the Results
We observed that racial/ethnic disadvantage and income were associated with increased COVID-19 rates in large metropolitan cities across the United States which have previously been demonstrated within the recent literature. As we aimed to identify structural inequities that have contributed to the observed disparities in COVID-19 risk and outcomes, we analyzed provider number as a primary variable related to community/neighborhood inequities. We observed that primary healthcare provider access varied within these cities in relation to both racial and economic advantages which were associated with COVID-19 infection. These findings are important in revealing the root causes of observed health disparities and provide a signal of structural drivers that impact entire communities putting them at increased risk of poor health outcomes in the United States.
In further detail, we observed that COVID-19 cases were higher in racially/ethnically disadvantaged neighborhoods (i.e. neighborhoods that are predominantly non-white) consistently with average case numbers being 1000 cases higher in comparison to racially/ethnically advantaged zip codes. Throughout the COVID-19 pandemic there has been increased recognition of the impact of structural racism within the United States and within institutions (e.g. medicine/healthcare) overall as a cause of higher observed case rates and mortality among both adults and children from marginalized racial/ethnic groups. Within discussions about observed COVID-19 health disparities many have cited that those who belong to highly impacted racial/ethnic groups are more “at-risk” due to the nature of their living conditions (e.g. multi-family households), job duties (e.g. more often doing jobs that require direct human contact and less opportunity to work from home), and baseline increased risk due to higher prevalence of chronic disease.17,18 However, structural and institutional inequities which lead to such risk factors must also be examined for eradication.
There are known and well-described inequities within our institutions and systems in the United States which include housing, education, criminal justice, finance, and health care.19 Legislative and policy-driven racism have harmed Black and brown communities within the United States for centuries. The policy practice of redlining is one example whereby racism and inequity were incorporated within the very fabric of communities throughout the United States. The practice of redlining involves designating specific communities populated by predominantly Black residents as undesirable for investment by financial institutions and for mortgage lending. These intentional discriminatory practices have led to neighborhoods and communities today, which are populated by Black and brown residents, lacking investment to support basic needs for healthy living such as grocery and general stores, adequately funded public schools, green space, and homeownership opportunities to build wealth.20 These conditions put communities at a disadvantage and increased risk during significant events like natural disasters and health epidemics. The results of our study exemplify the current state impact of historical redlining practices whereby we observed that predominantly Black and brown communities were not only more affected by COVID-19 incidence but higher case rates aligned with lack of primary healthcare access uniquely within these same communities. We observed an overall lower healthcare provider rate in racially/ethnically disadvantaged neighborhoods and our additional analysis demonstrated that provider availability within zip codes led to lower COVID-19 incidence rate ratios. The lasting effects of redlining in communities leading to disinvestment by banks, lack of government-funded development, and basic infrastructures that would drive economic growth, likely lessen attraction for health care organizations and providers resulting in health care deserts. Intentional investment and development within communities are needed to close health disparity gaps. An additional and movable barrier to improving primary care provider availability within predominantly non-white zip codes is to increase the racial and ethnic diversity of physicians with the goal of matching the demographics of the community and the United States overall.
Black and Hispanic physicians combined only make 10.8% of total physicians in the United States despite census projection indicating that these groups comprise over 30% of the United States population.21,22 Diversifying the physician and overall healthcare workforce is critical to closing the currently observed health care disparity gaps that exist between marginalized communities of color and non-marginalized primarily white communities. Bias, discrimination, and racism within the medical environment are also known to lead to suboptimal care, valid distrust, and overall ineffective medical practice.23,24 Increasing the diversity of health care providers congruent with the general population can serve to mitigate such biases and discrimination within medical environments. Research demonstrates that healthcare provider trust and medication/recommendation uptake are improved with racial/ethnic concordance between patient and health care provider. In addition, diversity within medical teams improves the overall effectiveness of care. Finally, it is demonstrated that Black, Hispanic, and Indigenous physicians are more likely to practice in areas populated by these groups as well as to practice in overall underserved areas.25 , 26 Increasing the racial/ethnic diversity to address gaps in under-representation within the medical workforce is an additional strategy to address the observed disparities pointed out in our study.
Our study also highlights the overall impact of income equality and health risk as well as how this aligns with race within our society. Not surprisingly, we observed that zip codes with lower median incomes had higher COVID-19 rates and these zip codes also had lower primary health care providers. Black and brown communities disproportionately comprised financially disadvantaged zip codes while white communities were disproportionately represented within financially advantaged zip codes. Research has shown that people with higher incomes overall report being in good health. A study by the Monthly Labor Review showed that average life expectancy in income groups close to the poverty line is decreasing, while those with middle to higher income were headed towards a longer life expectancy. Surveys taken of these individuals showed that people from higher families “overwhelmingly” reported being in good health with those in the group being “twice as likely” to report being in excellent health in comparison to those in the bottom group. COVID-19 had many repercussions outside of the direct effects of the illness itself as over 50% of households reported losing income due to the pandemic since March of 2020. While this income loss was widespread across the country, “it was disproportionately reported among households that were already on the lower end of income scales in 2019.”27 As previously mentioned, lower-wage workers were also more likely to be in riskier occupational environments for COVID-19 infection.
A striking observation within our study was that even within lower-income zip codes that were predominantly white, COVID-19 rates still tended to be lower than predominantly Black and brown zip codes. We also found that while higher income within racially advantaged neighborhoods seemed to be protective against higher COVID-19 rates, this correlation was not as strong within racially disadvantaged zip codes. These findings suggest that “income” per se for Black and brown communities is not singularly protective in disease and overall health risk, as the long-term consequences of lack of wealth within such communities are likely most impactful. This research is further emphasized by the consistency of results across top populated cities in the United States indicating a national crisis.
Limitations
A recognized limitation of our study is that data were obtained from publicly available databases between December 2020 and January 2021; as such, COVID-19 case numbers have had dynamic changes during this time. However, this study provides a retrospective view of observed pandemic-related disparities. Additional limitations include that data were obtained from single sources for COVID-19 case numbers, income, and racial/ethnic demographic data therefore reliability of data may vary between different sources. However, an effort was made to check the reliability of data across more than one source, and when available government-sourced data was utilized. Barriers were also encountered within data sources from government agencies. For example, accessed data for the city of Los Angeles did not include information on COVID-19 rates per zip code, so this city was not able to be included in our analysis. We also recognize that race and ethnicity are social constructs, and those who identify within a certain racial/ethnic identity make up a heterogeneous group with inherent differences in “advantage” and “disadvantage.” However, given the legacy of land and cultural pillage, slavery, discrimination, and racism within the United States, one can argue that the impact of these practices leads to an overall disadvantage for all who identify from such groups.
Implications and conclusion
The COVID-19 pandemic continues to affect the lives of millions of people daily with likely irreversible damage having been done over the past year. Our study demonstrates that income and racial/ethnic disadvantage are associated with primary health care provider access and COVID-19 case rates. We believe that these findings are a maker of disinvestment within marginalized communities as a result of structural and systemic racism within the United States leading to a lack of opportunity for wealth building and healthy living is an important undercurrent of the observed COVID-19 health disparities. These results pose concerns when considering how the pandemic will progress within the next year and how these structural inequities have impacted and will impact vaccine distribution. Reducing these structural inequities requires national leadership and coordination with, state, and local government to implement legislation and funding to correct intentional disinvestments within communities and to correct other institutional harms. Working towards economic development that promotes equity and growth within communities as well as addressing the lack of opportunity for wealth within marginalized populations can help lead to the goal of health equity within the United States.
Footnotes
Declarations of Competing Interest: None.
References
- 1.Chowell G., Mizumoto K. The COVID-19 pandemic in the USA: what might we expect? Lancet. 2020;395(10230):1093–1094. doi: 10.1016/S0140-6736(20)30743-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Menni C., Valdes A.M., Freidin M.B., et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med. 2020;26(7):1037–1040. doi: 10.1038/s41591-020-0916-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention; 2020. Characteristics of Health Care Personnel with COVID-19 - United States. February 12–April 9. [Google Scholar]
- 4.Anderson KA. and M. States ranked by percentage of population vaccinated: April 10. Becker's Hospital Review. https://www.beckershospitalreview.com/public-health/states-ranked-by-percentage-of-population-vaccinated-march-15.html. Accessed April 12, 2021.
- 5.Figueroa J.F., Wadhera R.K., Lee D., Yeh R.W., Sommers BD. Community-Level Factors Associated With Racial And Ethnic Disparities In COVID-19 Rates In Massachusetts. Health Aff (Millwood) 2020;39(11):1984–1992. doi: 10.1377/hlthaff.2020.01040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Memmott T., Carley S., Graff M., et al. Sociodemographic disparities in energy insecurity among low-income households before and during the COVID-19 pandemic. Nat Energy. 2021;6:186–193. doi: 10.1038/s41560-020-00763-9. [DOI] [Google Scholar]
- 7.Oronce C.I.A., Scannell C.A., Kawachi I., Tsugawa Y. Association Between State-Level Income Inequality and COVID-19 Cases and Mortality in the USA. J Gen Intern Med. 2020;35(9):2791–2793. doi: 10.1007/s11606-020-05971-3. Accessed April 12, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nixon R., Wick J., Sze J., Gilman N., Walsh K.T., Lee B. Aftermath of Katrina: A Time of Environmental Racism. arcgis.com. https://www.arcgis.com/apps/Cascade/index.html?appid=2106693b39454f0eb0abc5c2ddf9ce40. Accessed April 21, 2021.
- 9.Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. 2012;123:167–174. [PMC free article] [PubMed] [Google Scholar]
- 10.Benitez J., Courtemanche C., Yelowitz A. Racial and Ethnic Disparities in COVID-19: Evidence from Six Large Cities. J Econ Race Policy. 2020;3:243–261. doi: 10.1007/s41996-020-00068-9. Accessed April 21, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Largest cities in the United States by population. Ballotpedia. https://ballotpedia.org/Largest_cities_in_the_United_States_by_population. Accessed March 29, 2021.
- 12.Zipdatamaps - Interactive ZIP Code Maps and Data. zdm. https://www.zipdatamaps.com/. Accessed April 1, 2021.
- 13.INCOME BY ZIP CODE. US Income Statistics - Current Census Data for Zip Codes. https://www.incomebyzipcode.com/. Accessed April 1, 2021.
- 14.Find a Doctor - Doctor Reviews - Online Doctor Appointments; 2021 Healthgrades https://www.healthgrades.com/. Accessed April 1,
- 15.Ethnic and Racial Minorities & Socioeconomic Status. American Psychological Association: 2021 https://www.apa.org/pi/ses/resources/publications/minorities Accessed March 29.
- 16.Bureau USC. Income and Poverty in the United States: 2019. The United States Census Bureau. https://www.census.gov/library/publications/2020/demo/p60-270.html. Published September 15, 2020. Accessed March 29, 2021.
- 17.Hyde S. Income and Health Outcomes. Monthly Labor Review. 2021 https://www.bls.gov/opub/mlr/2017/beyond-bls/pdf/income-and-health-outcomes.pdf Published February 2017. Accessed March 30. [Google Scholar]
- 18.COVID-19 Pandemic's Impact on Household Employment and Income. https://crsreports.congress.gov/product/pdf/IN/IN11457. Published November 9, 2020. Accessed March 30, 2021.
- 19.Health Equity Considerations and Racial and Ethnic Minority Groups. Centers for Disease Control and Prevention. 2021 https://www.cdc.gov/coronavirus/2019-ncov/community/health-equity/race-ethnicity.html Published February 12, 2021. Accessed April 2. [Google Scholar]
- 20.White GB. The Data Are Damning: How Race Influences School Funding. The Atlantic. 2021 https://www.theatlantic.com/business/archive/2015/09/public-school-funding-and-the-role-of-race/408085/ Published September 30, 2015. Accessed March 29. [Google Scholar]
- 21.Riley WJ. Health disparities: gaps in access, quality and affordability of medical care. Trans Am Clin Climatol Assoc. 2012;123:167–174. [PMC free article] [PubMed] [Google Scholar]
- 22.Census US. QuickFacts United States. QuickFacts United States. https://www.census.gov/quickfacts/fact/table/US/PST045219. Accessed June 17, 2021.
- 23.Egede LE. Race, ethnicity, culture, and disparities in health care. J Gen Intern Med. 2006;21(6):667–669. doi: 10.1111/j.1525-1497.2006.0512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Minority Health. National Institute of Allergy and Infectious Diseases. https://www.niaid.nih.gov/research/minority-health. Accessed March 29, 2021.
- 25.Smedley B.D., Stith A.Y., Colburn L., et al. Increasing Racial and Ethnic Diversity Among Physicians: An Intervention to Address Health Disparities? National Academies Press (US); Washington (DC): 2001. Institute of Medicine (US). The Right Thing to Do, The Smart Thing to Do: Enhancing Diversity in the Health Professions: Summary of the Symposium on Diversity in Health Professions in Honor of Herbert W. Nickens, M.D. [PubMed] [Google Scholar]
- 26.Komaromy M., Grumbach K., Drake M., Vranizan K., Lurie N., Keane D., Bindman AB. The role of black and Hispanic physicians in providing health care for underserved populations. N Engl J Med. 1996 May 16;334(20):1305–1310. doi: 10.1056/NEJM199605163342006. PMID: 8609949. [DOI] [PubMed] [Google Scholar]
- 27.COVID-19 Pandemic's Impact on Household Employment and Income. https://crsreports.congress.gov/product/pdf/IN/IN11457. Published November 9, 2020. Accessed March 30, 2021.