Abstract
A lack of vitamin D seems to be related to autoimmune diseases including autoimmune thyroiditis (AIT). This study intends to determine the correlation between improvement of 25-hydroxyvitamin D [25(OH)D] levels and AIT in patients from an outpatient endocrine clinic in Frankfurt, Germany. This study included 933 patients with thyroid peroxidase antibodies (anti-TPO-Ab) ≥34 kIU/l, including most patients with clear AIT due to a concurrent sonographic evidence of reduced echogenicity. We performed clinical evaluation and laboratory analysis at five points in time within two years retrospectively. Due to a high dropout rate within the observation period, we excluded the last two time points from analysis. Data from 933 AIT patients revealed 89% having vitamin D deficiency or insufficiency [25(OH)D <75 nmol/l] with a median 25(OH)D level of 39.7 nmol/l. At baseline, a weak inverse correlation between 25(OH)D and anti-TPO-Ab was observed during winter (r s =–0.09, p=0.048*), but not during summer time (p>0.2). We discovered 58 patients having initially a 25(OH)D level < 75 nmol/l (median: 40.2 nmol/l), which improved over time to a 25(OH)D level ≥ 75 nmol/l (median: 83.2 nmol/l, p<0.0005***). Simultaneously, the median anti-TPO-Ab level showed a significant decrease of 25% from 245.8 to 181.3 kIU/l (p=0.036*). A significant reduction of the median anti-TPO-Ab level of 9% was also observed in the control group, which consisted of patients having constantly a 25(OH)D level <75 nmol/l. The result may suggest that in particular patients with 25(OH)D levels < 75 nmol/l benefit from an increase of 25(OH)D levels ≥ 75 nmol/l. Further prospective randomized controlled clinical trials are needed to finally evaluate if vitamin D has immunmodulatory effects in AIT.
Key words: autoimmune thyroid disease, vitamin D deficiency, 25(OH)D
Introduction
Autoimmune thyroiditis (AIT) is not only one of the most prevalent human autoimmune diseases, but also the most frequent cause of primary hypothyroidism. It is characterized by lymphocytic infiltration of the thyroid gland with subsequent gradual destruction and fibrous replacement of thyroid tissue. A German epidemiological study, the “Study of Health in Pomerania” (SHIP), showed the prevalence of thyroid peroxidase antibody (anti-TPO-Ab) positivity to be 7%; 4.1% having a anti-TPO-Ab level > 200 IU/ml 1 . 1.2% of the subjects had a positive anti-TPO-Ab titer and showed the sonographic features of AIT 1 .
The pathogenesis of AIT includes the cellular and humoral immunity. Initial infiltration of the thyroid gland contains antigen-presenting cells (APCs), in particular dendritic cells (DCs) 2 . APCs present thyroid-specific autoantigens to CD4-positive T lymphocytes, which may induce AIT in case of disturbed immune tolerance. The pathogenesis includes different subpopulations of T-lymphocytes e. g., CD4-positive T lymphocytes (T H 1, T H 2, T H 17, T reg ) and CD8-positive T lymphocytes. Autoantibodies are produced by B-cell-derived plasma cells.
The diagnosis of AIT is based on the presence of antibodies against thyroid specific antigens, primarily anti-TPO-Ab and on a sonographically proven reduced echogenicity of the thyroid parenchyma. In regard of thyroid specific autoantibodies, the proof of anti-TPO-Ab is considered the most sensitive diagnostic marker for AIT 3 .
Vitamin D is essential for calcium homeostasis, phosphate metabolism as well as bone health. In recent decades, however, it has been recognized that the vitamin D receptor (VDR) and vitamin D activating enzymes are expressed in far more tissues, suggesting that the functions of vitamin D go beyond the skeletal effects 4 5 6 . The active metabolite of Vitamin D, 1,25-dihydroxyvitamin D [1,25(OH) 2 D 3 ], is considered a potent immune modulator with influence on the innate and adaptive immune responses ( Fig. 1 ).
Fig. 1.
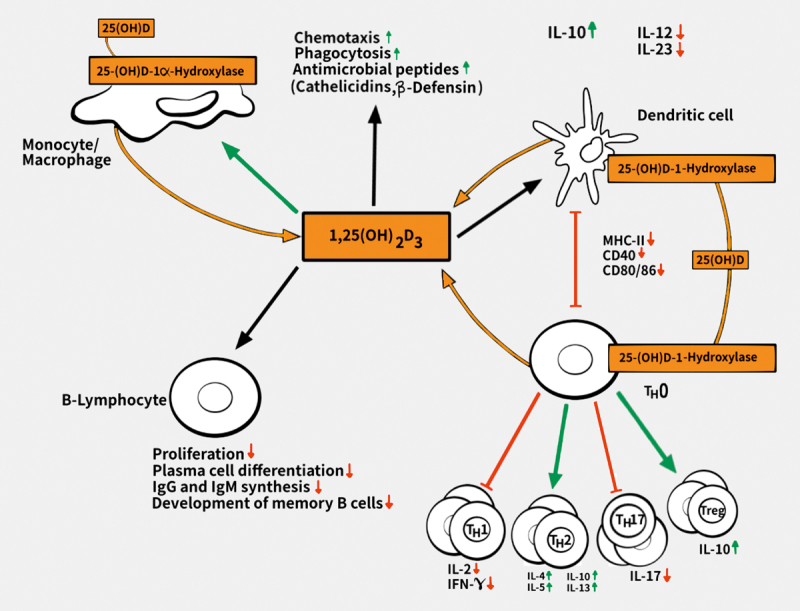
Overview of the effects of vitamin D on the immune system [adapted from 36 . Immune cells are able to convert 25(OH)D to active 1,25(OH) 2 D 3 and subsequent respond to 1,25(OH) 2 D 3 due to vitamin D receptor expression. Vitamin D can modulate the innate and adaptive immune response. Modulation of innate immune response includes monocyte stimulation and therefore, an increased chemotaxis, phagocytosis and production of antimicrobial peptides. Effects of 1,25(OH) 2 D 3 on T lymphocytes include the limitation of inflammatory T H 1- and T H 17-response, shift towards anti-inflammatory T H 2-phenotype and induction of regulatory T lymphocytes (T reg ). 1,25(OH) 2 D 3 affects maturation and activity of dendritic cells: 1,25(OH) 2 D 3 induces tolerogenic dendritic cells due to decreased expression of MHC-II, the co-stimulatory molecules CD40, CD80, CD86, a reduced IL-12-secretion, and an increase of the anti-inflammatory cytokine IL-10. 1,25(OH) 2 D 3 comprises also direct effects on B lymphocytes: it is capable to limit the proliferation of activated B lymphocytes, induce their apoptosis, and inhibit plasma cell differentiation, and therefore also the synthesis of the antibodies IgG, IgM, and memory B cells.
The first indications for the influence of vitamin D on the immune system derive from the 1980s, in which the presence of the VDR in activated human immune cells was detected 5 . Nowadays, it is well known that the VDR is present in various subpopulations of immune cells, for example, in activated CD4- and CD8 positive T lymphocytes and APCs such as macrophages and DCs 5 7 .
Different studies showed that Vitamin D deficiency is associated with the occurrence and progression of autoimmune diseases 8 9 10 . The connection between vitamin D and autoimmune disease was derived from studies that have found a link between the prevalence of certain autoimmune diseases and sun exposure. Whether this effect is due to the moderate ultraviolet (UV) radiation itself, the subsequent increased 1,25(OH) 2 D 3 synthesis or a combination of both is unclarified 11 .
There is an association between increasing incidence and prevalence and higher latitude for autoimmune diseases, including type 1 diabetes mellitus, multiple sclerosis and rheumatoid arthritis 8 9 10 .
Considering recent studies, the association between vitamin D levels and AIT is still conflicting. While some studies detected a significant negative correlation between serum 25(OH)D and anti-TPO-Ab levels 12 13 14 , others did not reveal this correlation 15 16 17 . Most current evidence suggests a higher rate of vitamin D deficiency in patients with AIT compared with controls 12 13 14 15 18 19 20 .
In view of this controversial results, this study is planned to evaluate the vitamin D status in patients with AIT from an outpatientʼs endocrine clinic in Frankfurt, Germany.
Subjects and Methods
Our study population included 933 patients (856 females and 77 males; mean age 43.4±14.4 years) who presented at our outpatient endocrine clinic between 2003 and 2013. The diagnosis of AIT was based on elevated anti-TPO-Ab≥34 kIU/l and sonographic pattern suggestive for AIT. All 933 patients had elevated anti-TPO-Ab, most patients had a clear AIT due to a concurrent sonographic pattern suggestive for AIT. We performed clinical evaluation including daily medicine intake [vitamin D and levothyroxine (LT4) dosage] and laboratory analysis such as measurement of anti-TPO-Ab titers and 25(OH)D levels as well as parathyroid hormone (PTH) levels, thyrotropin (TSH) levels, and free thyroid hormones levels at five points in time within two years retrospectively. Due to a high dropout rate within the observation period of 97.5%, we excluded the last two time points from analysis.
Also excluded from this study were pregnant patients including the first 12 weeks after delivery. Immunological changes occurring within this period can be responsible for a drop in autoantibody levels 21 22 23 . Written informed consent was obtained from all participants. Approval of ethics committee was granted in September 2006.
Laboratory tests
Serum concentration of 25(OH)D was measured using electrochemiluminescent immunoassay (ECLIA) kit from Roche Diagnostics, Germany. In regard to Holick et al. 25(OH)D levels <50 nmol/l were classified as vitamin D deficiency, levels between 50 and 74.9 nmol/l as insufficient and a 25(OH)D concentration ≥75 nmol/l was considered sufficient 24 . Anti-TPO-Ab level was assessed by ECLIA kit (Roche Diagnostics, Germany). Patients with anti-TPO-Ab ≥34 kIU/l were considered positive for anti-TPO-Ab. Levels of free triiodothyronine (fT3), free thyroxine (fT4) and TSH were measured using ECLIA kits (Roche Diagnostics, Germany).
Statistical analysis
All parameters are presented as mean±standard deviation as well as median, 25 th and 75 th percentiles (lower quartile/upper quartile). The statistical program SPSS 23 (SPSS, Chicago, IL, USA) and R (R Core Team 2019). R Foundation for Statistical Computing, Vienna, Austria) were used for all analysis. Normality of the distribution was evaluated using Kolmogorov–Smirnov–Lillierfors test. Since the tests indicated that variables did not follow normal distribution, nonparametric tests were used. Spearmanʼs correlation coefficient was used to analyze the correlations among the variables. To detect differences between two or more than two groupsʼ of medians, Mann–Whitney, van Elteren [in order to stratify for season (May–Oct., Nov.–Apr.)] or Kruskal–Wallis tests were applied. Differences between time points were determined by Friedman and Wilcoxon tests, the influence of relevant covariables as season was analyzed using conditional inference trees 25 . Binary data was evaluated by chi-square test and McNemarʼs test. Bonferroni correction was used of adjusting p-value for multiple testing. All tests were two-sided and p-values ≤0.05 were considered statistically significant.
Results
At first visit, data from 933 patients (100%) were considered. The following visits within the observation period of 24 months contained data from 355 (38%), 194 (20.8%), and 80 (8.6%) patients respectively.
The mean time interval between the first and the second visit was 8.5±6.7 months and between the second and the third visit 6.3±6.2 months.
The baseline characteristics of the 933 AIT patients of the study participants are presented in Table 1 . The vast majority of patients enrolled in our study were women (91.7%). The mean age of disease onset was 35.5±13.8 years and the mean disease duration at study enrollment was 4.9±5.5 years.
Table 1 Baseline characteristics of our study population.
| Study population at first visit | 933 (100%) |
|---|---|
| Age (years) | 43.4±14.4 |
| Gender | ♀ 856/933 (91.7%) |
| ♂ 77/933 (8.3%) | |
| BMI (kg/m 2 ) | 25.9±5.7 |
| Age of disease onset (years) | 35.5±13.8 |
| Disease duration (years) | 4.9±5.5 |
| Patients with immigration background | 268/933 (28.7%) |
BMI: Body mass index.
The most frequent concomitant autoimmune disease were rheumatoid arthritis, vitiligo, and psoriasis vulgaris.
Table 2 reveals the laboratory characteristics at three points in time. Amongst cases, the mean TSH was 2.9±7.6 mIU/l (reference interval: 0.27–4.2 mIU/l), fT3 was 2.3±0.6 pg/ml (reference interval: 2–4.4 pg/ml), and fT4 was 13.3±3 ng/l (reference interval: 9.3–17 ng/l). 80% of the patients received LT4 treatment at first visit. Mean anti-TPO-Ab level was 293.4±259.3 kIU/l (reference interval: <34 kIU/l).
Table 2 Laboratory characteristics of our study population.
| Study population at three points in time | 933 (100%) | 355 (38%) | 194/933 (20.8%) | Reference interval |
|---|---|---|---|---|
| TSH (mIU/l) | 2.9 (±7.6) | 1.95 (±3.1) | 2.3 (±5) | 0.27–4.2 |
| fT3 (pg/ml) | 2.3 (±0.6) | 2.9 (±0.5) | 2.9 (±0.85) | 2.0–4.4 |
| fT4 (ng/l) | 13.3 (±3.05) | 13.5 (±2.6) | 13.2 (±2.5) | 9.3–17 |
| Anti-TPO-Ab (kIU/l) | 293.45 (±259.3) | 269.9 (±241) | 251.9 (±244.05) | <34 |
| TRAK (IU/l) | 3.5 (±4) | 4.1 (±17.6) | 5.9 (±39.1) | <1.8 |
| Received LT4 | 747/933 (80%) | 325/355 (91.5%) | 180/195 (92.3%) | |
| LT4 (μg/day) | 96.2 (±41.9) | 94.3 (±45.8) | 94.3 (±38.1) | |
| 25(OH)D (nmol/l) | 43.3 (±23.5) | 48.45 (±26) | 48.4 (±23.5) | ≥ 75 |
| PTH (pmol/l) | 4.9 (±2.6) | 4.8 (±2.2) | 4.8 (±2.3) | 1.6–6.9 |
| Received vitamin D3 | 73/933 (7.8%) | 82/355 (23.1%) | 54/195 (27.7%) | |
| Vitamin D3 (IE/day) | 1998.8 (±3118.6) | 1732.8 (±2367) | 1437.4 (±1149.8) |
TSH: Thyroid-stimulating hormone; fT3: Triiodothyronine; fT4: Free thyroxine; Anti-TPO-Ab: Thyroid perioxidase antibodies; TRAK: Anti-TSH receptor antibodies; LT4: Levothyroxine; 25(OH)D: 25-Hydroxyvitamin D; PTH: Parathyroid hormone.
At first visit 834/933 (89.4%) patients had a 25(OH)D level < 75 nmol/l, with a mean level of 43.3±23.5 nmol/l. Mean PTH level was in the reference interval of 1.6–6.9 pmol/l.
Seasonality of 25(OH)D level with significant winter-summer fluctuations was observed. Lowest levels of 25(OH)D were found in March [median: 26.4 nmol/l (18.1; 45.35)], highest levels in August [median: 51.3 nmol/l (34; 70)] ( Fig. 2 ). Anti-TPO-Ab levels revealed no opposite rhythmic patterns of the seasonality.
Fig. 2.
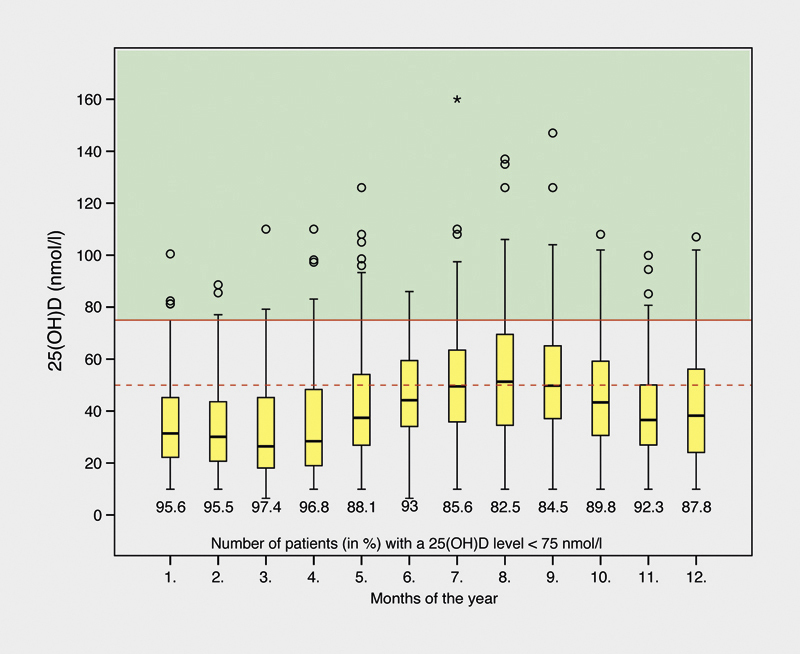
Seasonality of 25(OH)D level.
At baseline, a weak inverse correlation between 25(OH)D levels and anti-TPO-Ab levels was observed during winter ( r s = –0.09, p=0.048), but not during summer time (p >0.2).
For the whole cohort, a significant increase of 25(OH)D levels were shown between the first and the second visit (43.3±23.5 nmol/l to 48.5±26 nmol/l, p <0.0005***), however not during subsequent measurements.
Via regression tree modeling we identified five subgroups for change in 25(OH)D levels between the first and the second measurement, dependent on the season of the first and second measurement (Nov.–Apr., May–Oct.) and vitamin D intake during the time of the second measurement. Vitamin D intake during the time of the first measurement had no significant influence. If vitamin D intake during the time of the second measuring was present, a significant increase in 25(OH)D levels was observed independently of seasons (p <0.0001***, median change 27.9 (interquartile range: 9.7; 43.2). If both measurements took place in summer or both in winter, no significant change in 25(OH)D levels was observed (p=0.16 and p=0.08, respectively). If the first measurement took place in winter, the second measurement in summer 25(OH)D levels rose significantly [p ≤0.0001***, median change 10.8 (IQR: 2.2; 27.5)], if the opposite was true, the levels decreased significantly [p ≤ 0.0001***, median change –15.8 (IQR: –27.7; 3.9)].
Patients treated with LT4 had a significant lower anti-TPO-Ab level in comparison to those not treated [median: 205.6 kIU/l (70.65; 416.2) vs. 314.2 kIU/l (140.1; 511.5), p <0.0005***]. The anti-TPO-Ab level decreased from 293.5±259.3 kIU/l to 269.9±241 kIU/l (p=0.0005***). Although LT4 therapy correlates with anti-TPO-Ab levels at baseline, we did not find any correlation for the second measurement and LT4 nor vitamin D intake and change in anti-TPO-levels (p >0.2): Via regression tree modeling we observe that neither LT4 and vitamin D intake nor change in 25(OH)D levels seem to influence change in anti-TPO-Ab levels significantly. As expected, there was a negative correlation between the 25(OH)D level and the PTH level (winter: r s =–0.29, p <0.0001***, summer: r s =–0.25, p <0.0001***) as well as the 25(OH)D level and the body mass index (kg/m 2 ) (winter: r s =–0.17, p=0.0004*** summer: r s =–0.28, p <0.0001***). There was no significant negative correlation between TSH and 25(OH)D levels (winter: p >0.2, summer: r s =–0.08, p=0.07).
We discovered 58 patients having initially an inadequate level of 25(OH)D <75 nmol/l (median: 40.2 nmol/l), which improved until the second visit to a sufficient level of 25(OH)D ≥75 nmol/l (+107.2%, median: 83.2 nmol/l, p <0.0005***) due to self-supplementation of vitamin D or intake prescribed by physicians or due the influence of seasons. Simultaneously, the median anti-TPO-Ab level had a decrease of 24.6% from 245.8 kIU/l to 181.3 kIU/l (p=0.036*) ( Fig. 3 ). The control group consisted of patients which had constantly a 25(OH)D level <75 nmol/l (at first and second presentation), but nevertheless the 25(OH)D level showed an increase of 39.7% between this two points in time. A statistically significant reduction of the median anti-TPO-Ab level of almost 9% was also observed in the control group. The difference in reduction of anti-TPO-Ab levels between both groups was not statistically significant (p >0.2).
Fig. 3.
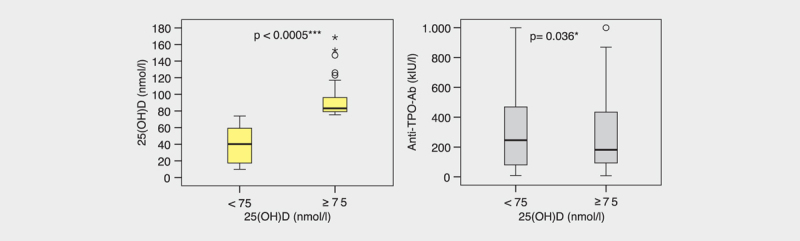
Subgroup with improvement of 25(OH)D ≥ 75 nmol/l. a Significant difference in 25(OH)D levels (Wilcoxon test). b Significant difference in anti-TPO-Ab levels (Wilcoxon test).
Discussion and Conclusions
Many recent studies address the relationship between the serum 25(OH)D level and autoimmune disorders like AIT. The present state of studies is still controversial. While some studies have found a significant negative correlation between serum 25(OH)D and anti-TPO-Ab levels 12 13 14 , others did not detect this correlation 15 16 17 . Many studies revealed a significant higher rate of vitamin D deficiency among patients with AIT compared with controls 12 13 14 15 18 19 20 .
The main focus of our analysis was the association between the vitamin D status and AIT. Vitamin D status was assessed by serum concentrations of 25(OH)D; autoimmune activity of AIT by measurement of serum anti-TPO-Ab levels.
At baseline, we observed a weak inverse correlation between 25(OH)D and anti-TPO-Ab level during winter, but not during summer time. Further points in time revealed no significant correlation. A significant increase of 25(OH)D levels was observed between the first and the second visit. Simultaneously, the anti-TPO-Ab concentration decreased significantly. After the time of 8.5±203.2 months, no further increase in 25(OH)D levels was detected. This limitation may be due to retrospective study design. Therefore, association beyond this period cannot be evaluated. Another limitation is, that there was a nonsignificant trend toward higher LT4 intake at the second point in time, which may also lower anti-TPO-Ab levels. A number of studies revealed the same effect of treatment with LT4 on anti-TPO-Ab levels 26 27 28 . Chiovato et al. showed that expression of thyroid microsomal autoantigen on differentiated rat thyroid cells (FRTL-5) is dependent on TSH in cell culture 29 . Indirect immunofluorescence revealed no cell surface expression of thyroid antigen after TSH elimination 29 . Thus, LT4 intake leads to a decrease in TSH-levels, may lower expression of thyroid antigen followed by a reduction in anti-TPO-Ab levels 30 .
Our data show that there is a significant positive correlation between anti-TPO-Ab and TSH-levels. This relationship confirms the progressive thyroid cell damage due to autoantibodies and subsequent elevation of TSH-levels. A negative correlation was also found between TSH-levels and 25(OH)D-levels, which is in accordance to the case-control study from Mansournia et al. 15 . This relationship may be an indicator of changes in thyroid function due to vitamin D and its influence on autoimmunity. In the end, it is not only important if vitamin D lowers anti-TPO-Ab levels but also if it has an influence on thyroid function and necessity of thyroid hormone substitution.
The main focus of our study was the association between the vitamin D status and anti-TPO-Ab levels. We discovered 58 patients having initially an inadequate level of 25(OH)D which improved over time to a sufficient level (+107%, p <0.0005***). This improvement took place after 11.4±6.6 months. Simultaneously, the median anti-TPO-Ab concentration had a decrease of 24.6% (p=0.036*). There was no significant difference in LT4 intake and TSH levels (p=0.154 and p=0.061, respectively). Hence, we assume that LT4 intake did not influence the reduction of anti-TPO-Ab levels. A statistically significant reduction of the median anti-TPO-Ab level of almost 9% was also observed in the control group. Here it has to be taken into account, that the 25(OH)D level also had a significant increase.
The result of the present subgroup analysis may suggests that in particular patients with deficient or insufficient 25(OH)D levels benefit from an increase of 25(OH)D levels (≥75 nmol/l), although the difference between the subgroups did not reach statistical significance. These results are in accordance with three prospective studies from Greece 13 , India 31 , and Poland 32 , which addresses the effect of vitamin D3 substitution on anti-TPO-Ab levels. Mazokopakis et al. found a significant decrease of anti-TPO-Ab levels in the 186 AIT patients after 4 months substitution of vitamin D3 1200–4000 international units (IU) 13 . The randomized, controlled trial with 102 AIT patients from Chaudary et al. revealed a significant reduction of anti-TPO-Ab titers in the intervention group (vitamin D3 60.000 IU weekly and calcium 500 mg/day for 8 weeks) with TSH-levels ≤10 mIU/l in comparison to control group 31 . A very recent study with 34 affected women receiving LT4 for at least 6 months and normal vitamin D status [25(OH)D above 30 ng/ml ≅ above 75 nmol/l] showed that intake of vitamin D3 2000 IU/day reduced titers of thyroid antibodies after 6 months 32 .
Not only reduced exposure to UV-B radiation, but also VDR, vitamin D binding protein (DBP), and 1α-hydroxylase (CYP27B1) gene polymorphisms can lead to impaired immunomodulatory properties of vitamin D 33 34 35 .
Whether vitamin D deficiency is a causal factor in the pathogenesis of AIT or if vitamin D deficiency is a consequence of AIT with subsequent hypothyroidism is not clear. Our data cannot provide evidence of causality. Therefore, further prospective randomized controlled clinical trials are needed to finally evaluate if vitamin D has immunmodulatory effects in AIT and to determine the optimal serum 25(OH)D levels in patients with autoimmune disorders.
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Volzke H, Ludemann J, Robinson D M et al. The prevalence of undiagnosed thyroid disorders in a previously iodine-deficient area. Thyroid. 2003;13:803–810. doi: 10.1089/105072503768499680. [DOI] [PubMed] [Google Scholar]
- 2.Voorby H A, Kabel P J, de Haan M et al. Dendritic cells and class II MHC expression on thyrocytes during the autoimmune thyroid disease of the BB rat. Clin Immunol Immunopathol. 1990;55:9–22. doi: 10.1016/0090-1229(90)90065-x. [DOI] [PubMed] [Google Scholar]
- 3.Mariotti S, Caturegli P, Piccolo P et al. Antithyroid peroxidase autoantibodies in thyroid diseases. J Clin Endocrinol Metab. 1990;71:661–669. doi: 10.1210/jcem-71-3-661. [DOI] [PubMed] [Google Scholar]
- 4.OʼConnell T D, Simpson R U. Immunochemical identification of the 1,25-dihydroxyvitamin D3 receptor protein in human heart. Cell Biol Int. 1996;20:621–624. doi: 10.1006/cbir.1996.0081. [DOI] [PubMed] [Google Scholar]
- 5.Provvedini D M, Tsoukas C D, Deftos L J et al. 1,25-dihydroxyvitamin D3 receptors in human leukocytes. Science. 1983;221:1181–1183. doi: 10.1126/science.6310748. [DOI] [PubMed] [Google Scholar]
- 6.Howitz J, Brodthagen H, Schwartz M et al. Prevalence of vitiligo. Epidemiological survey on the Isle of Bornholm, Denmark. Arch Dermatol. 1977;113:47–52. doi: 10.1001/archderm.113.1.47. [DOI] [PubMed] [Google Scholar]
- 7.Veldman C M, Cantorna M T, DeLuca H F. Expression of 1,25-dihydroxyvitamin D(3) receptor in the immune system. Arch Biochem Biophys. 2000;374:334–338. doi: 10.1006/abbi.1999.1605. [DOI] [PubMed] [Google Scholar]
- 8.Mohr S B, Garland C F, Gorham E D et al. The association between ultraviolet B irradiance, vitamin D status and incidence rates of type 1 diabetes in 51 regions worldwide. Diabetologia. 2008;51:1391–1398. doi: 10.1007/s00125-008-1061-5. [DOI] [PubMed] [Google Scholar]
- 9.Simpson S, Jr., Blizzard L, Otahal P et al. Latitude is significantly associated with the prevalence of multiple sclerosis: a meta-analysis. J Neurol Neurosurg Psychiatry. 2011;82:1132–1141. doi: 10.1136/jnnp.2011.240432. [DOI] [PubMed] [Google Scholar]
- 10.Vieira V M, Hart J E, Webster T F et al. Association between residences in U.S. northern latitudes and rheumatoid arthritis: A spatial analysis of the Nursesʼ Health Study. Environ Health Perspect. 2010;118:957–961. doi: 10.1289/ehp.0901861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Juzeniene A, Moan J. Beneficial effects of UV radiation other than via vitamin D production. Dermatoendocrinol. 2012;4:109–117. doi: 10.4161/derm.20013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bozkurt N C, Karbek B, Ucan B et al. The association between severity of vitamin D deficiency and Hashimotoʼs thyroiditis. Endocr Pract. 2013;19:479–484. doi: 10.4158/EP12376.OR. [DOI] [PubMed] [Google Scholar]
- 13.Mazokopakis E E, Papadomanolaki M G, Tsekouras K C et al. Is vitamin D related to pathogenesis and treatment of Hashimotoʼs thyroiditis? Hell J Nucl Med. 2015;18:222–227. [PubMed] [Google Scholar]
- 14.Shin D Y, Kim K J, Kim D et al. Low serum vitamin D is associated with anti-thyroid peroxidase antibody in autoimmune thyroiditis. Yonsei Med J. 2014;55:476–481. doi: 10.3349/ymj.2014.55.2.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mansournia N, Mansournia M A, Saeedi S et al. The association between serum 25OHD levels and hypothyroid Hashimotoʼs thyroiditis. J Endocrinol Invest. 2014;37:473–476. doi: 10.1007/s40618-014-0064-y. [DOI] [PubMed] [Google Scholar]
- 16.Goswami R, Marwaha R K, Gupta N et al. Prevalence of vitamin D deficiency and its relationship with thyroid autoimmunity in Asian Indians: A community-based survey. Br J Nutr. 2009;102:382–386. doi: 10.1017/S0007114509220824. [DOI] [PubMed] [Google Scholar]
- 17.Yasmeh J, Farpour F, Rizzo V et al. Hashimotoʼs Thyroiditis not associated with Vitamin-D Deficiency. Endocr Pract. 2016;22:809–813. doi: 10.4158/EP15934.OR. [DOI] [PubMed] [Google Scholar]
- 18.Kivity S, Agmon-Levin N, Zisappl M et al. Vitamin D and autoimmune thyroid diseases. Cell Mol Immunol. 2011;8:243–247. doi: 10.1038/cmi.2010.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tamer G, Arik S, Tamer I et al. Relative vitamin D insufficiency in Hashimotoʼs thyroiditis. Thyroid. 2011;21:891–896. doi: 10.1089/thy.2009.0200. [DOI] [PubMed] [Google Scholar]
- 20.Camurdan O M, Doger E, Bideci A et al. Vitamin D status in children with Hashimoto thyroiditis. J Pediatr Endocrinol Metab. 2012;25:467–470. [PubMed] [Google Scholar]
- 21.Smyth P P, Wijeyaratne C N, Kaluarachi W N et al. Sequential studies on thyroid antibodies during pregnancy. Thyroid. 2005;15:474–477. doi: 10.1089/thy.2005.15.474. [DOI] [PubMed] [Google Scholar]
- 22.Kuijpens J L, Pop V J, Vader H L et al. Prediction of post partum thyroid dysfunction: can it be improved? Eur J Endocrinol. 1998;139:36–43. doi: 10.1530/eje.0.1390036. [DOI] [PubMed] [Google Scholar]
- 23.Kampe O, Jansson R, Karlsson F A. Effects of L-thyroxine and iodide on the development of autoimmune postpartum thyroiditis. J Clin Endocrinol Metab. 1990;70:1014–1018. doi: 10.1210/jcem-70-4-1014. [DOI] [PubMed] [Google Scholar]
- 24.Holick M F, Binkley N C, Bischoff-Ferrari H A et al. Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96:1911–1930. doi: 10.1210/jc.2011-0385. [DOI] [PubMed] [Google Scholar]
- 25.Hothorn T, Hornik K, Zeileis A. Unbiased recursive partitioning: A conditional inference framework. J Comput Graph Statistics. 2006;15:651–674. [Google Scholar]
- 26.Schmidt M, Voell M, Rahlff I et al. Long-term follow-up of antithyroid peroxidase antibodies in patients with chronic autoimmune thyroiditis (Hashimotoʼs thyroiditis) treated with levothyroxine. Thyroid. 2008;18:755–760. doi: 10.1089/thy.2008.0008. [DOI] [PubMed] [Google Scholar]
- 27.Padberg S, Heller K, Usadel K H et al. One-year prophylactic treatment of euthyroid Hashimotoʼs thyroiditis patients with levothyroxine: Is there a benefit? Thyroid. 2001;11:249–255. doi: 10.1089/105072501750159651. [DOI] [PubMed] [Google Scholar]
- 28.Romaldini J H, Biancalana M M, Figueiredo D I et al. Effect of L-thyroxine administration on antithyroid antibody levels, lipid profile, and thyroid volume in patients with Hashimotoʼs thyroiditis. Thyroid. 1996;6:183–188. doi: 10.1089/thy.1996.6.183. [DOI] [PubMed] [Google Scholar]
- 29.Chiovato L, Vitti P, Lombardi A et al. Expression of the microsomal antigen on the surface of continuously cultured rat thyroid cells is modulated by thyrotropin. J Clin Endocrinol Metab. 1985;61:12–16. doi: 10.1210/jcem-61-1-12. [DOI] [PubMed] [Google Scholar]
- 30.Rieu M, Richard A, Rosilio M et al. Effects of thyroid status on thyroid autoimmunity expression in euthyroid and hypothyroid patients with Hashimotoʼs thyroiditis. Clin Endocrinol (Oxf) 1994;40:529–535. doi: 10.1111/j.1365-2265.1994.tb02494.x. [DOI] [PubMed] [Google Scholar]
- 31.Chaudhary S, Dutta D, Kumar M et al. Vitamin D supplementation reduces thyroid peroxidase antibody levels in patients with autoimmune thyroid disease: An open-labeled randomized controlled trial. Indian J Endocrinol Metab. 2016;20:391–398. doi: 10.4103/2230-8210.179997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krysiak R, Szkrobka W, Okopien B. The effect of vitamin D on thyroid autoimmunity in levothyroxine-treated women with hashimotoʼs thyroiditis and normal vitamin D status. Exp Clin Endocrinol Diabetes. 2017;125:229–233. doi: 10.1055/s-0042-123038. [DOI] [PubMed] [Google Scholar]
- 33.Pani M A, Regulla K, Segni M et al. Vitamin D 1alpha-hydroxylase (CYP1alpha) polymorphism in Gravesʼ disease, Hashimotoʼs thyroiditis and type 1 diabetes mellitus. Eur J Endocrinol. 2002;146:777–781. doi: 10.1530/eje.0.1460777. [DOI] [PubMed] [Google Scholar]
- 34.Kurylowicz A, Ramos-Lopez E, Bednarczuk T et al. Vitamin D-binding protein (DBP) gene polymorphism is associated with Gravesʼ disease and the vitamin D status in a Polish population study. Exp Clin Endocrinol Diabetes. 2006;114:329–335. doi: 10.1055/s-2006-924256. [DOI] [PubMed] [Google Scholar]
- 35.Yazici D, Yavuz D, Tarcin O et al. Vitamin D receptor gene ApaI, TaqI, FokI and BsmI polymorphisms in a group of Turkish patients with Hashimotoʼs thyroiditis. Minerva Endocrinol. 2013;38:195–201. [PubMed] [Google Scholar]
- 36.Mathieu C. Vitamin D and the immune system: Getting it right. IBMS BoneKEy. 2011;8:178–186. [Google Scholar]


