Abstract
Background:
Organized athletics are undergoing a gradual resumption after a prolonged hiatus in 2020 because of the coronavirus disease 2019 (COVID-19) pandemic.
Purpose/Hypothesis:
The purpose of this study was to evaluate the effect of the 2020 COVID-19 period on emergency department (ED) visits for sports-related injuries in the United States. It was hypothesized that such visits decreased in response to the pandemic conditions.
Study Design:
Descriptive epidemiology study.
Methods:
A selection of sports (baseball, basketball, softball, soccer, American football, weightlifting, track and field, martial arts, boxing, golf, personal fitness, cycling, tennis, and ice hockey) were classified as being an organized team, organized individual, or nonorganized sport. The National Electronic Injury Surveillance System database was then queried for ED visits for sports-related injuries between January 1, 2018, and December 31, 2020, and we compared weighted national injury estimates and injury characteristics from athletes presenting to EDs in 2018 and 2019 versus those from the 2020 COVID-19 pandemic period and between March 1 and May 31, 2020 (government-imposed lockdown period). Bivariate comparisons between variables were conducted using chi-square analysis, with strength of association assessed using odds ratios.
Results:
The 164,151 unweighted cases obtained from the query resulted in a weighted national estimate of 5,664,795 sports-related injuries during the study period. Overall, there was a 34.6% decrease in sports-related ED visits in 2020 compared with the yearly average between 2018 and 2019 (baseline). The number of ED visits in 2020 decreased by 53.9% versus baseline for injuries incurred by participation in an organized team sport and by 34.9% for injuries incurred by participation in an organized individual sport. The number of ED visits during the 2020 lockdown period decreased by 76.9% versus baseline for injuries incurred by participation in an organized team sport and by 65.8% for injuries incurred by participation in an organized individual sport. Injuries sustained while participating in a nonorganized sport remained relatively unaffected and decreased by only 8.1% in 2020.
Conclusion:
ED visits in the United States for injuries sustained while participating in an organized team or individual sport underwent a decrease after the beginning of the COVID-19 pandemic in 2020, especially during the lockdown period.
Keywords: baseball, basketball, boxing, cycling, football, golf, hockey, soccer, softball, tennis
Sports-related injuries have always undergone yearly and seasonal variation 44 ; however, the effect of coronavirus disease 2019 (COVID-19)—related government lockdowns on sports injury patterns is unclear. In March 2020, several governing bodies for professional sports leagues, including the National Collegiate Athletic Association (NCAA), National Football League (NFL), National Basketball Association (NBA), and the Summer Olympics, began suspending play because of players and fans testing positive for COVID-19. 3,10,23,45 Not long after this, state governors in the United States issued lockdown orders that recommended canceling school activities, including high school and youth sports. Stay-at-home orders that lasted for months affected emergency department (ED) visits for pediatric trauma, brain injuries, and fractures. 2,11,16,32 Although these injuries and overall ED visits decreased during this time, pediatric penetrating and burn injuries increased. 32 We believe that the propensity for COVID-19 to alter the proportion of sports-related injuries is high, owing to the suspension of team athletics as well as the increase in nonorganized individual sports.
A change in injury patterns presents many challenges to the care of professional and recreational athletes. These issues include determining the appropriate level of maintenance training and the approach to returning athletes to play safely. 33,43 An athletic suspension of this scale has not been seen since World War II; however, there have been previous small instances of forced sports cessation, such as the NFL lockout in 2011 and the Major League Baseball strike in 1981. While injuries decreased during these periods, they underwent a rebound effect with a subsequent increase due to deconditioning and accelerated training regimens. 1,22,38
A thorough understanding of current injury trends in athletes is crucial for public health officials when considering the implementation of stay-at-home orders and for physicians when predicting injury risk and determining return to sports recommendations. Therefore, the purpose of our study was to evaluate the effect of the COVID-19 lockdowns on ED visits for sports-related injuries in the United States. We hypothesized that such visits decreased in response to the COVID-19 lockdowns.
Methods
This study was exempt from ethics committee approval because we used deidentified, publicly available data from an online website. We retrospectively identified cases of sports-related injuries in the US Consumer Product Safety Commission (CPSC) National Electronic Injury Surveillance System (NEISS). The database is publicly available, deidentified, and published annually on a freely accessible governmental website. It is a nationally representative probability sample of 100 designated hospital EDs stratified by hospital size and geographic location, from which weighted national estimates for queried injuries may be derived. The term “estimated” used throughout the text refers to weighted national estimates derived from the NEISS national consumer database. This sample includes large inner-city hospitals with trauma centers, as well as urban, suburban, rural, and pediatric hospitals. A wide variety of reliable, reproducible epidemiology studies on injury-related ED visits have been published using the NEISS database. 13,24,30 Specific data collection methodologies and quality control precautions are available on the CPSC website (https://www.cpsc.gov/Research--Statistics/NEISS-Injury-Data).
The NEISS database was queried between January 1, 2018, and December 31, 2020, for injuries classified as associated with the following sports (product codes in parentheses): baseball (5041), softball (5034), basketball (1205), road or commuter bicycles and accessories (5040), mountain or all-terrain bicycles and accessories (5033), boxing (1207), exercise (3299), exercise equipment (3277), weightlifting (3265), American football (1211), golf (1212), ice hockey (1279), martial arts (3257), tennis (3284), soccer (1267), and track and field (5030).
These sports were chosen based on their popularity in the United States and their characterization within the NEISS database, as well as our perceived relevance of the expected effect of the pandemic on each sport. 40 Injuries sustained while cycling were consolidated into a single category. This query yielded a total of 164,264 unweighted cases during the search period. There were 91 patients who sustained fatal injuries and 22 patients with missing data who were identified and excluded. All weighted US sports-related ED visit counts in this study are estimates unless otherwise specified.
Information regarding patient age (years), sex, body part injured, injury diagnosis, disposition (hospital admission vs discharge), injury date, and sport were extracted for analysis. Patients who were treated and transferred or were treated and admitted/hospitalized were categorized as being hospitalized, while patients who were treated/examined and released, were held for observation, or left without being seen were considered not hospitalized. Patient age was classified as being pre-high school (2-13 years), high school (14-18 years), college (19-22 years), early adulthood (23-44 years), middle adulthood (45-64 years), and late adulthood (≥65 years). Body part injured was categorized as follows: head and neck (head, neck, face, mouth, ears, and eyes), upper extremities (shoulder, upper arm, elbow, lower arm, wrist, hand, and finger), wrist and hand (wrist, hand, and finger), lower extremities (upper leg, knee, lower leg, ankle, foot, and toe), foot and ankle (foot, toe, and ankle), and other (internal, trunk, pubic region, and all other body parts). Injury diagnosis included fractures, lacerations (lacerations and punctures), strains and/or sprains, contusions and/or abrasions, dislocations, concussions, hemorrhage and/or hematoma, internal injury, and other (burns, dental, nerve, crush, foreign body, avulsion, and all other categories of injury).
Organized team sports were defined as sports that must be performed predominantly in a team setting both when training and competing and included soccer, American football, baseball, softball, basketball, tennis, and ice hockey. Organized individual sports were defined as sports that can be trained for individually but usually require in-person officiating, the presence of an opponent, or access to a shared facility in order to participate. These sports included track and field, golf, boxing, martial arts, and weightlifting. Nonorganized sports were defined as sports that are performed primarily in an individual setting and included cycling (mountain and road) and personal fitness. The time period for each injury was classified as being either within or outside of the approximate state-instituted lockdown period. In many US states, and for the purpose of this study, the lockdown time period was considered the time between March 1 and May 31, 2020.
Data regarding the 2020 monthly incidence of confirmed cases of COVID-19 in the United States was sourced from the Johns Hopkins University Coronavirus Resource Center, which in turn aggregates data from a multitude of institutional sources, including the World Health Organization, the European Centre for Disease Prevention and Control, the US Centers for Disease Control and Prevention, and many others. These data are publicly available, reliable, and have been used in previous studies. 7,15
Statistical Analysis
Weighted national estimates were calculated using IBM SPSS Statistics for Windows (Version 27.0; IBM Corp). Figures were designed using GraphPad Prism (GraphPad Software). Bivariate comparisons between variables were conducted using chi-square analysis with strength of association assessed using odds ratios (ORs) with 95% CIs. In cases where there are >2 categories, all ORs constitute a comparison between the group of interest and all other categories consolidated into a single group. P values < .05 (2-sided) were considered statistically significant.
Results
Table 1 demonstrates the number of ED visits in the United States between 2018 and 2020 for sports-related injuries, stratified by patient characteristics. The 164,151 unweighted cases resulted in a weighted estimate of 5,664,795 sports-related injuries in the United States between 2018 and 2020. In 2020 overall, there was a 34.6% decrease in sports-related ED visits compared with the yearly average between 2018 and 2019 (baseline). During the 2020 lockdown period, there was a 76.9% decrease in injuries incurred by participation in an organized team sport and a 65.8% decrease in injuries incurred by participation in an organized individual sport, while injuries incurred by participation in nonorganized sports decreased by 16.6%. Most sports-related ED visits occurred in patients aged <22 years (55.7%). Patients aged ≤13 years or less (OR, 0.793; 95% CI, 0.789-0.797; P < .001) and patients aged 14 to 18 years (OR, 0.723; 95% CI, 0.720-0.727; P < .001) accounted for a smaller proportion of sports-related ED visits in 2020 compared with baseline, while patients aged 23 to 44 years (OR, 1.349; 95% CI, 1.342-1.356; P < .001), 45 to 64 years (OR, 1.343; 95% CI, 1.335-1.352; P < .001), and ≥65 years (OR, 1.542; 95% CI, 1.531-1.553; P < .001) all accounted for larger proportions.
TABLE 1.
Estimated Number of US ED Visits for Nonfatal Sports-Related Injuries, 2018-2020, Classified by Patient Characteristics a
| Total Cases, n | Estimated Injuries, n (% of Total) | Baseline Yearly Injuries, n | Estimated Injuries in 2020, n (% of Baseline) | 2020 Overall vs Baseline | Lockdown b vs Baseline | |||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |||||
| Sample size | 164,151 | 5,664,795 | 2,134,444 | 1,395,903 (65.4) | — | — | ||
| Age group, y | ||||||||
| ≤13 | 51,885 | 1,381,272 (24.4) | 542,242 | 296,786 (54.7) | 0.793 (0.789-0.797) | <.001 | 0.639 (0.633-0.646) | <.001 |
| 14-18 | 42,965 | 1,355,377 (23.9) | 540,272 | 274,833 (50.9) | 0.723 (0.720-0.727) | <.001 | 0.500 (0.493-0.506) | <.001 |
| 19-22 | 10,536 | 418,732 (7.4) | 156,907 | 104,917 (66.9) | 1.024 (1.016-1.033) | <.001 | 0.818 (0.803-0.833) | <.001 |
| 23-44 | 32,129 | 1,306,011 (23.1) | 478,926 | 348,178 (72.7) | 1.349 (1.342-1.356) | <.001 | 1.181 (1.168-1.193) | <.001 |
| 45-64 | 17,007 | 727,396 (12.8) | 255,781 | 215,833 (84.4) | 1.343 (1.335-1.352) | <.001 | 1.753 (1.730-1.775) | <.001 |
| ≥65 | 9628 | 475,986 (8.4) | 160,316 | 155,354 (96.9) | 1.542 (1.531-1.553) | <.001 | 1.977 (1.948-2.006) | <.001 |
| Sex | ||||||||
| Male | 120,349 | 4,074,092 (71.9) | 1,545,395 | 983,301 (63.6) | 0.908 (0.904-0.913) | <.001 | 0.923 (0.913-0.933) | <.001 |
| Female | 43,801 | 1,590,683 (28.1) | 589,041 | 412,601 (70.0) | 1.101 (1.096-1.106) | <.001 | 1.083 (1.072-1.094) | <.001 |
a The baseline yearly number of injuries was calculated from the average of the yearly number of injuries observed in 2018 and 2019. The term “estimated” refers to weighted national estimates derived from the NEISS national consumer database described in the study methodology. Percentages may not add to 100% due to rounding error. Dashes indicate no coherent corresponding value; ED, emergency department; NEISS, National Electronic Injury Surveillance System; OR, odds ratio.
b Between March 1, 2020, and May 31, 2020.
Table 2 depicts the number of sports-related ED visits between 2018 and 2020, stratified by sport and category of sport. Compared with baseline, the number of visits in 2020 decreased by 53.9% for injuries incurred during participation in an organized team sport and by 34.9% for injuries incurred during participation in an organized individual sport. Injuries sustained while participating in a nonorganized sport remained relatively unaffected and decreased by only 8.1% in 2020. Track and field had the greatest decrease (66.1%), while cycling was the only sport to undergo an overall increase (1.2%) in the number of ED visits in 2020. Organized team sports comprised a much smaller proportion of all sports-related ED visits from 2020 compared with the 2018 and 2019 baseline (OR, 0.535; 95% CI, 0.532-0.537; P < .001), while the proportion of organized individual sports-related ED visits did not undergo a significant change in 2020 compared with baseline (OR, 0.995; 95% CI, 0.988-1.002; P < .001). Nonorganized sports underwent an increase in the proportion of sports-related ED visits in 2020 compared with baseline (OR, 1.868; 95% CI, 1.860-1.876; P < .001), which was even more pronounced in the approximate COVID-19 US lockdown period (OR, 3.317; 95% CI, 3.285-3.350; P < .001).
TABLE 2.
Estimated Number of US ED Visits for Nonfatal Sports-Related Injuries, 2018-2020, Categorized by Sport a
| Total Cases, n | Estimated Injuries, n (% of Total) | Baseline Yearly Injuries, n | Estimated Injuries in 2020, n (% of Baseline) | 2020 Overall vs Baseline | Lockdown b vs Baseline | |||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) c | P | OR (95% CI) c | P | |||||
| Organized team sports | 87,123 | 2,732,918 (48.2) | 1,110,369 | 512,179 (46.1) | 0.535 (0.532-0.537) | <.001 | 0.321 (0.318-0.325) | <.001 |
| Soccer | 16,568 | 468,860 (8.3) | 193,704 | 81,452 (42.0) | 0.621 (0.616-0.626) | <.001 | 0.356 (0.348-0.363) | <.001 |
| American football | 23,047 | 711,426 (12.6) | 294,623 | 122,181 (41.5) | 0.599 (0.595-0.603) | <.001 | 0.563 (0.551-0.575) | <.001 |
| Baseball | 6986 | 234,334 (4.1) | 96,154 | 42,027 (43.7) | 0.658 (0.650-0.666) | <.001 | 0.340 (0.331-0.349) | <.001 |
| Softball | 4112 | 28,282 (0.5) | 66,870 | 28,282 (42.3) | 0.639 (0.631-0.648) | <.001 | 0.231 (0.223-0.240) | <.001 |
| Basketball | 33,613 | 1,054,184 (18.6) | 419,708 | 214,768 (51.2) | 0.743 (0.739-0.747) | <.001 | 0.558 (0.550-0.565) | <.001 |
| Tennis | 1302 | 53,709 (0.9) | 20,045 | 13,619 (67.9) | 1.039 (1.017-1.062) | <.001 | 1.114 (1.063-1.167) | <.001 |
| Ice hockey | 1495 | 48,383 (0.9) | 19,267 | 9850 (51.5) | 0.780 (0.761-0.800) | <.001 | 0.119 (0.101-0.139) | <.001 |
| Organized individual sports | 14,493 | 568,749 (10.0) | 214,556 | 139,637 (65.1) | 0.995 (0.988-1.002) | .135 | 0.706 (0.694-0.717) | <.001 |
| Track and field | 2158 | 69,526 (1.2) | 29,728 | 10,071 (33.9) | 0.515 (0.503-0.526) | <.001 | 0.281 (0.269-0.294) | <.001 |
| Golf | 2138 | 111,347 (2.0) | 39,229 | 32,890 (83.8) | 1.289 (1.270-1.308) | <.001 | 1.244 (1.204-1.284) | <.001 |
| Martial arts | 1972 | 70,367 (1.2) | 27,302 | 15,764 (57.7) | 0.882 (0.864-0.899) | <.001 | 0.480 (0.454-0.507) | <.001 |
| Boxing | 1228 | 43,931 (0.8) | 15,650 | 12,632 (80.7) | 1.236 (1.208-1.266) | <.001 | 0.834 (0.788-0.883) | <.001 |
| Weightlifting | 6997 | 273,578 (4.8) | 102,649 | 68,281 (66.5) | 1.018 (1.008-1.028) | <.001 | 0.831 (0.812-0.850) | <.001 |
| Nonorganized sports | 62,534 | 2,363,108 (41.7) | 809,510 | 744,088 (91.9) | 1.868 (1.860-1.876) | <.001 | 3.317 (3.285-3.350) | <.001 |
| Cycling | 35,764 | 1,266,597 (22.4) | 420,552 | 425,492 (101.2) | 1.787 (1.778-1.796) | <.001 | 2.944 (2.914-2.974) | <.001 |
| Personal fitness | 26,770 | 1,096,511 (19.4) | 388,958 | 318,595 (81.9) | 1.327 (1.320-1.334) | <.001 | 1.536 (1.519-1.553) | <.001 |
a The baseline yearly number of injuries was calculated from the average of the yearly number of injuries observed in 2018 and 2019. The term “estimated” refers to weighted national estimates derived from the NEISS national consumer database described in the study methodology. Percentages may not add to 100% due to rounding error. ED, emergency department; NEISS, National Electronic Injury Surveillance System; OR, odds ratio.
b Between March 1, 2020, and May 31, 2020.
c ORs with a P value ≥ .05 are considered not significant and are marked in bold.
Table 3 depicts the number of ED visits between 2018 and 2020 for sports-related injuries, stratified by body part injured, injury diagnosis, and hospitalization status. The overall most commonly injured body part between 2018 and 2020 was the lower extremity (31.0%), which accounted for a lower proportion of body parts injured in 2020 compared with the 2018 and 2019 baseline (OR, 0.881; 95% CI, 0.876-0.885; P < .001), especially during the lockdown time period (OR, 0.739; 95% CI, 0.732-0.747; P < .001). Strains and sprains accounted for 23.2% of the number of ED visits for sports-related injuries between 2018 and 2020 but accounted for a significantly lower proportion of sports-related ED visits in 2020 (OR, 0.787; 95% CI, 0.783-0.791; P < .001) and during the COVID-19 lockdown time period (OR, 0.620; 95% CI, 0.613-0.628; P < .001) than at baseline. Concussions also accounted for a lower proportion of sports-related ED visits in 2020 (OR, 0.762; 95% CI, 0.753-0.772; P < .001) and during the lockdown period (OR, 0.634; 95% CI, 0.615-0.654; P < .001) than at the 2018 and 2019 baseline. Finally, the majority (93.0%) of all patients who visited the ED for sports-related injuries between 2018 and 2020 were not hospitalized. Patients who were not hospitalized after their sports-related ED visit accounted for a larger proportion of injuries in 2020 (OR, 1.420; 95% CI, 1.408-1.431; P < .001) and during the lockdown period (OR, 1.863; 95% CI, 1.833-1.893; P < .001) than at the 2018 and 2019 baseline.
TABLE 3.
Estimated Number of US ED Visits for Nonfatal Sports-Related Injuries, 2018-2020, by Disposition, Body Part, and Diagnosis a
| Total Cases, n | Estimated Injuries, n (% of Total) | Baseline Yearly Injuries, n | Estimated Injuries in 2020, n (% of Baseline) | 2020 Overall vs Baseline | Lockdown b vs Baseline | |||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P | OR (95% CI) | P | |||||
| Body part | ||||||||
| Upper extremity | 47,459 | 1,574,048 (27.8) | 592,040 | 389,967 (65.9) | 1.010 (1.005-1.015) | <.001 | 1.038 (1.027-1.048) | <.001 |
| Shoulder | 10,191 | 379,448 (6.7) | 139,867 | 99,713 (71.3) | 1.097 (1.088-1.106) | <.001 | 1.184 (1.163-1.207) | <.001 |
| Elbow | 4278 | 144,163 (2.5) | 52,787 | 38,588 (73.1) | 1.121 (1.106-1.136) | <.001 | 1.103 (1.072-1.135) | <.001 |
| Hand and wrist | 24,865 | 816,668 (14.4) | 316,195 | 184,278 (58.3) | 0.875 (0.869-0.880) | <.001 | 0.826 (0.815-0.837) | <.001 |
| Lower extremity | 50,553 | 1,754,403 (31.0) | 675,166 | 404,070 (59.9) | 0.881 (0.876-0.885) | <.001 | 0.739 (0.732-0.747) | <.001 |
| Knee | 15,325 | 541,846 (9.6) | 209,643 | 122,560 (58.5) | 0.884 (0.877-0.890) | <.001 | 0.755 (0.742-0.768) | <.001 |
| Foot and ankle | 24,940 | 859,153 (15.2) | 334,223 | 190,707 (57.1) | 0.852 (0.847-0.858) | <.001 | 0.646 (0.637-0.654) | <.001 |
| Head and neck | 37,915 | 1,237,197 (21.8) | 465,332 | 306,534 (65.9) | 1.009 (1.004-1.015) | <.001 | 1.087 (1.075-1.099) | <.001 |
| Other | 27,302 | 1,066,248 (18.8) | 389,272 | 287,701 (73.9) | 1.164 (1.158-1.170) | <.001 | 1.311 (1.296-1.326) | <.001 |
| Not stated | 921 | 32,880 (0.6) | 12,625 | 7629 (60.4) | 0.923 (0.898-0.950) | <.001 | 0.788 (0.738-0.841) | <.001 |
| Diagnosis | ||||||||
| Concussion | 6734 | 187,607 (3.3) | 74,958 | 37,690 (50.3) | 0.762 (0.753-0.772) | <.001 | 0.634 (0.615-0.654) | <.001 |
| Contusion/abrasion | 19,693 | 703,766 (12.4) | 273,314 | 157,138 (57.5) | 0.864 (0.858-0.870) | <.001 | 0.837 (0.825-0.849) | <.001 |
| Dislocation | 3948 | 143,332 (2.5) | 52,381 | 38,571 (73.6) | 1.130 (1.115-1.145) | <.001 | 1.171 (1.137-1.206) | <.001 |
| Fracture | 31,209 | 957,053 (16.9) | 346,998 | 263,057 (75.8) | 1.196 (1.189-1.203) | <.001 | 1.408 (1.391-1.424) | <.001 |
| Hemorrhage/hematoma | 1442 | 49,402 (0.9) | 18,077 | 13,247 (73.28) | 1.122 (1.097-1.147) | <.001 | 1.402 (1.339-1.468) | <.001 |
| Laceration/puncture | 13,029 | 446,968 (7.9) | 158,718 | 129,532 (81.6) | 1.273 (1.264-1.283) | <.001 | 1.677 (1.651-1.703) | <.001 |
| Internal injury | 10,979 | 372,805 (6.6) | 137,777 | 97,251 (70.6) | 1.085 (1.076-1.095) | <.001 | 1.222 (1.201-1.244) | <.001 |
| Strain/sprain | 36,102 | 1,314,095 (23.2) | 516,783 | 280,529 (54.3) | 0.787 (0.783-0.791) | <.001 | 0.620 (0.613-0.628) | <.001 |
| Other | 41,014 | 1,489,747 (26.3) | 555,429 | 378,889 (68.2) | 1.059 (1.054-1.064) | <.001 | 0.970 (0.960-0.980) | <.001 |
| Disposition | ||||||||
| Not hospitalized | 153,223 | 5,268,889 (93.0) | 136,314 | 123,259 (90.4) | 1.420 (1.408-1.431) | <.001 | 1.863 (1.833-1.893) | <.001 |
| Hospitalized | 10,927 | 395,887 (7.0) | 1,998,122 | 1,272,645 (63.7) | 0.704 (0.699-0.710) | <.001 | 0.537 (0.528-0.546) | <.001 |
a The baseline yearly number of injuries was calculated from the average of the yearly number of injuries observed in 2018 and 2019. The term “estimated” refers to weighted national estimates derived from the NEISS national consumer database described in the study methodology. Percentages may not add to 100% due to rounding error. ED, emergency department; NEISS, National Electronic Injury Surveillance System; OR, odds ratio.
b Between March 1, 2020, and May 31, 2020.
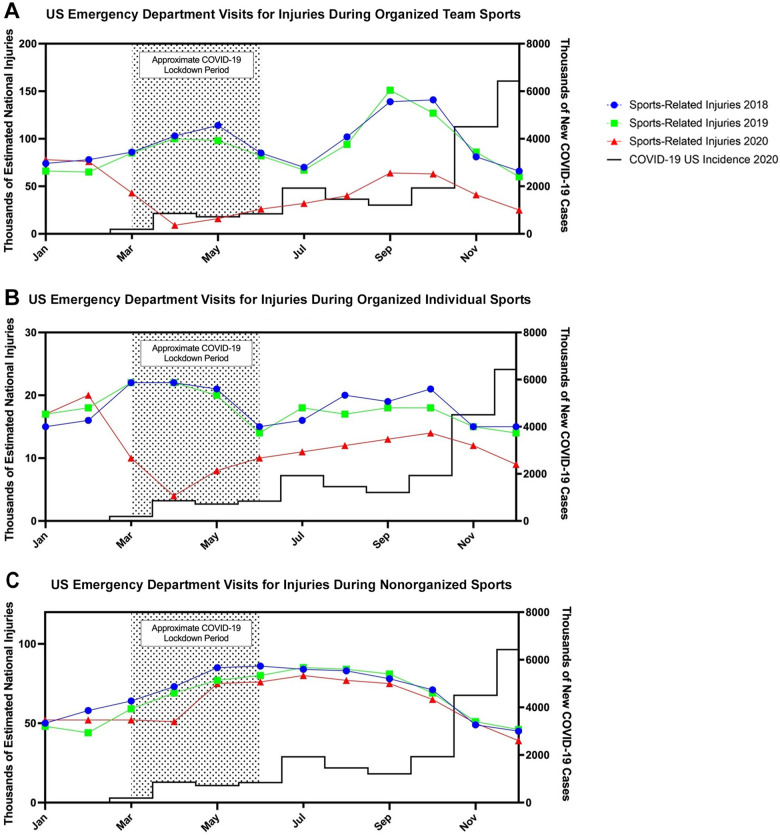
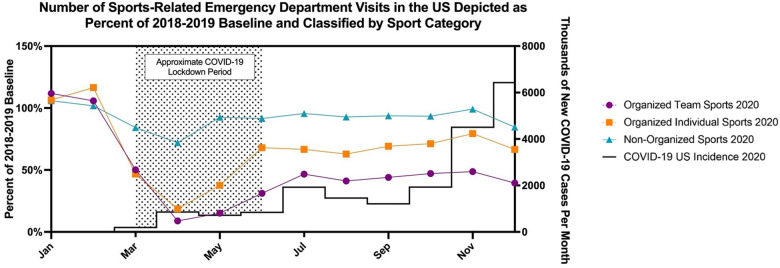
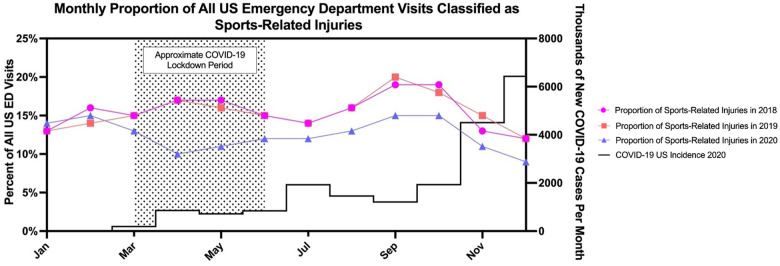
Figure 1 demonstrates the monthly number of sports-related ED visits in 2018, 2019, and 2020 for organized team sports, organized individual sports, and nonorganized sports, superimposed over the monthly incidence of positive COVID-19 tests, respectively. Figure 2 depicts the number of sports-related ED visits as a percentage of the 2018 and 2019 baselines, which demonstrates the relative effect of COVID-19 on organized team, organized individual, and nonorganized sport-related ED visits. April 2020 underwent the greatest drop in sports-related injuries, with organized team sports-related ED visits dropping by 91.1%, organized individual sports-related ED visits dropping by 81.6%, and nonorganized sports-related ED visits dropping by only 27.9% of the 2018 and 2019 April baseline. Figure 3 demonstrates the proportion of all US ED injuries that were sports related. Between March and December 2020, sports-related injuries comprised a smaller percentage of ED visits than in 2018 or 2019.
Figure 1.
Monthly incidence of positive COVID-19 tests in 2020 (black line) with estimated monthly number of sports-related emergency department visits in the United States in 2018 (blue line), 2019 (green line), and 2020 (red line) for (A) organized team sports, (B) organized individual sports, and (C) nonorganized sports. The shaded area represents the 2020 COVID lockdown period.
Figure 2.
Monthly incidence of positive COVID-19 tests in 2020 (black line) with the estimated monthly number of sports-related emergency department visits in the United States in 2020 expressed as a percentage of the 2018 and 2019 baseline for organized team sports (purple line), organized individual sports (orange line), and nonorganized sports (cyan line). The shaded area represents the 2020 COVID lockdown period.
Figure 3.
Monthly incidence of positive COVID-19 tests in 2020 (black line) with the estimated monthly number of sports-related emergency department (ED) visits in the United States expressed as a percentage of all US ED visits in 2018 (pink line), 2019 (orange line), and 2020 (purple line). The shaded area represents the 2020 COVID lockdown period.
Discussion
In the present study, we found that the United States observed a 34.6% decrease in the overall number of sports-related ED visits in 2020. A similar decrease in ED volume has been established by previous studies within various patient populations 4,19 and is attributed to institutional recommendations to treat minor injuries at home and the general fear of contracting COVID-19 during a hospital visit. Organized team sports underwent an overall 53.9% decrease in the number of ED visits; organized individual sports underwent a 34.9% decrease in the number of ED visits; and nonorganized sports remained near the 2018 and 2019 baseline, with only an 8.9% decrease in the number of ED visits. For sports that require access to specialized shared facilities, a decrease in sports-related ED visits was expected secondary to lower injury rates due to decreased sports participation.
Sports-related injuries are a common occurrence in the United States, affecting up to 8.6 million athletes per year. 36 Among elite adolescent athletes, the 1-year injury prevalence is reportedly as high as 91.6% and costs patients millions of dollars in health care expenditures. 17,42 While many sports-related injuries are not serious enough to warrant a trip to the ED, those that are account for approximately 2.7 million annual US ED visits for sports-related injuries in children and young adults. 29 Under the duress of the COVID-19 pandemic, many sporting disciplines have endured varying levels of obstruction. Elite athletics encountered an increased injury rate throughout 2020 due to physical and behavioral factors secondary to quarantining: namely, a multifactorial constellation of deconditioning, depression, and the miscalculation of readiness to return to sports after a prolonged hiatus. 25,35 In the past, the severe acute respiratory syndrome pandemic led to a decrease in ED visits and health care costs associated with injuries in both pediatric and adult populations. 14,16 We expected to observe a similar effect during the COVID-19 pandemic, wherein reduced participation in in-person officiated team sports and reluctance to risk viral exposure would lead to a decrease in the utilization of ED resources for sports-related injuries.
Our findings are of chief concern for the sports medicine physician since they likely reveal a prolonged period of systematically undertreated or ignored sports-related injuries. While participation in organized sports continues to make a slow recovery, our findings demonstrated that, as of December 31, 2020, sports-related patient volume for US EDs has yet to return to baseline. The relative decrease in the proportion of school-aged children and increase in the proportion of adults aged ≥23 years who comprise sports-related ED visits in the United States in 2020 can be attributed to state-mandated school closures that occurred during the lockdown period that were later followed by a shift toward a predominantly virtual classroom setting. Surprisingly, college-aged adults comprised a larger proportion of sports-related ED visits in 2020 than the 2018 and 2019 baseline, despite university closures and the widespread adoption of virtual classrooms. This finding may be explained by college-aged adult participation in unofficial sports leagues and independent fitness training, which might not be as readily available for school-aged children as for college-aged adults. The higher proportion of male ED visits (71.9%) in the current study may be explained by a significantly higher incidence of sports-related injuries in male athletes than in female athletes 27,31 and overall higher rates of male sports participation as demonstrated by previous studies. 9,28
Restrictions brought on by the US lockdown limited both in-person gatherings and access to gymnasiums, fitness centers, and schools, thereby severely affecting team and individual sports requiring in-person officiating, coaching, or gymnasium access. The present study found that, during the lockdown, athletes were less likely to present to an ED with an injury sustained while participating in an organized sport compared with the 2018 and 2019 baseline. On the other hand, ED visits for injuries sustained while participating in nonorganized sports (sports that do not require gatherings or access to a shared facility) decreased by only 8.1% and were responsible for a much higher proportion of sports-related ED visits throughout 2020 than for the 2018 and 2019 baseline. While nonorganized sports still endured a decrease in ED visits, these were likely somewhat offset by increased participation in “COVID-19 safe” individual sports, like running and cycling. In fact, a number of cities worldwide underwent changes to transportation infrastructure leading to the development of “pop-up” bicycle lanes, at an average of 11.4 km per city over the course of 4 months. 18 Several urban centers experienced a surge in outdoor activities during the lockdown, especially in cycling volume. 8,34 The increased demand for outdoor activities and equipment explains the isolated rise in cycling injuries observed during the pandemic, with untrained “at-risk” individuals suddenly taking up the sport. However, despite efforts to promote exercise during the pandemic, many people continued to struggle with a prolonged reduction in physical activity. 5
The proportion of patients reporting to EDs for sports-related concussions during the COVID-19 pandemic was less than that observed during the 2018 and 2019 baseline. One explanation may be related to the relative frequency of concussions in organized versus nonorganized sports. While concussions are a major concern in some nonorganized sports such as cycling, 12 the elevated risk of concussions in contact sports such as ice hockey, boxing, American football, martial arts, and soccer is very well established in the literature, especially during match play. 26,41 Therefore, a decrease in ED visits for sports-related concussions during the lockdown time period wherein organized contact sports went on hiatus was expected. Often, athletes deliberately avoid reporting concussion symptoms for fear of being unable to play. 6,20,21 If a concussion is likely to be perceived as a lower acuity injury, the decrease in ED visits may not constitute a true decrease in concussions but rather general patient unwillingness to go to the ED for a concussion during a pandemic. The same unwillingness to visit the ED may hold true for perceived lower acuity injuries such as strains and sprains, contusions, and abrasions, as well as injuries to body parts including hands, knees, and feet, all of which accounted for a lower proportion of sports-related ED visits in 2020 than during the 2018 and 2019 baseline.
The underreporting of sports-related injuries may have long-term ramifications, especially regarding avoidance of ED resources for insidious injuries such as concussions, which often involve subtle symptoms (dizziness, nausea, headache, etc) that may appear trivial at first glance to nonmedical personnel. 39 Long-term consequences of unreported repeat concussions include various neuropsychiatric deficits including impaired attention; memory; cognition; and, in some cases, depression, suicidality, poor impulse control, aggression, Parkinsonism, and dementia. 37 Physicians may use the present data to anticipate the underreporting of sports-related injuries and should consequently adopt a high threshold for recommending time off from play in players for whom a concussion diagnosis is not entirely clear.
It is important to discuss the injury counts for sports-related ED visits in relation to the month and the number of COVID-19 cases in the United States. There was a clear bimodal distribution for organized sports in both 2018 and 2019, reflective of their seasonality under normal conditions (Figures 1A and 1B). Under the pandemic conditions of 2020, there was almost no evidence of a bimodal distribution: the effect of COVID-19 effectively negated seasonal injury trends in organized sports. Nevertheless, there was almost no effect on sports-related ED visits for nonorganized sports under pandemic conditions, both within and outside of the lockdown period (Figure 1C). Interestingly, after the lockdown period and as the incidence of COVID-19 continued to rise, ED visits for sports-related injuries remained stable (Figure 2). We did not observe an expected spike in sports-related ED visits as detrained athletes returned to sports in the postlockdown period. This differed from the literature findings in professional athletes, wherein elite athletes returning to sports after the COVID-19 pandemic experienced a greater likelihood of sustaining an injury. 35 Nevertheless, because of continued ED avoidance for fear of contracting COVID-19, our results may not constitute an accurate depiction of the frequency of sports-related injuries sustained in the postlockdown period, especially given the incremental rise in incidence of COVID-19 in the latter months of 2020. In fact, Figure 3 demonstrates that, through the end of 2020, sports-related injuries continued to comprise a lower proportion of all ED visits than in previous years. In addition, nonprofessional athletes, who constituted the majority of those incurring these injuries, may not perceive the same pressure to return to sports since their livelihood does not depend on it and therefore may not be exposed to the same elevated risk of injury secondary to deconditioning. Future investigation is warranted after data from the next few years become available, especially after the widespread implementation of COVID-19 vaccination as well as the sense of security this may impart.
Limitations
Many of the limitations of this study are inherent to the NEISS database. First, the database only records injuries that warrant a visit to the ED and not those that were fatal prior to hospitalization. Therefore, the NEISS database does not effectively capture very low or high acuity injuries. Since fatal injuries are less likely to occur in sports than are mild injuries, 46 high acuity injuries and sports with higher acuity injury profiles are likely overrepresented in this analysis. In addition, the NEISS database does not consistently record granular injury information such as severity, subtype, imaging, laboratory values, or detailed patient histories. In order to ensure that there were enough unweighted counts to produce reliable national estimates, we chose only the most popular and clinically relevant sports to represent all sports-related injuries. Since some sports such as volleyball, lacrosse, and field hockey were not included in this analysis, these national estimates likely constitute an underrepresentation of the true count of all sports-related ED visits. In addition, many athletic organizations and institutions likely had medical staff who continued to function throughout the lockdown period, thereby providing a safer and therefore more appealing option for treatment of sports-related injuries during the pandemic. Since the NEISS database does not document national sports participation rates, this study did not evaluate the effect of the COVID-19 pandemic on injury rates. Hourly or individual injury rates would be useful for future investigations since they would facilitate evaluation of the effect of the COVID-19 pandemic on the per hour or per participant risk of injury.
Conclusion
In the United States, ED visits for injuries sustained while participating in an organized sport underwent a decrease after the beginning of the COVID-19 pandemic, especially during the months that best correspond to the governmental lockdowns. ED visits for injuries sustained while participating in a nonorganized sport remained stable throughout 2020.
Footnotes
Final revision submitted September 19, 2021; accepted November 8, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: B.M.G. has received consulting fees from Medical Device Business Services and Zimmer Biomet. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Binney ZO, Hammond KE, Klein M, Goodman M, Janssens A. NFL injuries before and after the 2011 collective bargaining agreement (CBA). arXiv. Preprint posted online May 3, 2018. https://arxiv.org/abs/1805.01271
- 2. Bram JT, Johnson MA, Magee LC, et al. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. J Pediatr Orthop. 2020;40(8):373–379. doi:10.1097/BPO.0000000000001600 [DOI] [PubMed] [Google Scholar]
- 3. Chappell B, Welna D. Tokyo Olympics postponed for a year. Accessed August 28, 2021. https://www.npr.org/2020/03/24/820593807/tokyo-olympics-postponed-due-to-coronavirus-pandemic?t=1641911227970
- 4. Ciacchini B, Tonioli F, Marciano C, et al. Reluctance to seek pediatric care during the COVID-19 pandemic and the risks of delayed diagnosis. Ital J Pediatr. 2020;46:87. doi:10.1186/s13052-020-00849-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Constandt B, Thibaut E, De Bosscher V, Scheerder J, Ricour M, Willem A. Exercising in times of lockdown: an analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int J Environ Res Public Health. 2020;17(11):4144. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7312512/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Conway F, Domingues M, Monaco R, et al. Concussion symptom underreporting among incoming NCAA Division I college athletes. Clin J Sport Med. 2020;30(3):203–209. doi:10.1097/JSM.0000000000000557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi:10.1016/S1473-3099(20)30120-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Doubleday A, Choe Y, Isaksen TB, Miles S, Errett NA. How did outdoor biking and walking change during COVID-19?: a case study of three U.S. cities. PLoS One. 2021;16(1):e0245514. doi:10.1371/journal.pone.0245514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Eime RM, Harvey JT, Charity MJ, Payne WR. Population levels of sport participation: implications for sport policy. BMC Public Health. 2016;16(1):752. doi:10.1186/s12889-016-3463-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. ESPN News Services. NBA suspends season until further notice after player tests positive for the coronavirus. Published 2020. Accessed August 28, 2021. https://www.espn.com/nba/story/_/id/28887560/nba-suspends-season-further-notice-player-tests-positive-coronavirus
- 11. Fahy S, Moore J, Kelly M, Flannery O, Kenny P. Analysing the variation in volume and nature of trauma presentations during COVID-19 lockdown in Ireland. Bone Joint Open. 2020;1(6):261–266. doi:10.1302/2633-1462.16.bjo-2020-0040.r1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Helmich I, von Gotz D, Emsermann C, et al. Not just contact sports: significant numbers of sports-related concussions in cycling. J Sports Med Phys Fit. 2019;59(3):496–501. doi:10.23736/S0022-4707.18.08329-9 [DOI] [PubMed] [Google Scholar]
- 13. Hoge C, Sabbagh R, Morgan M, Grawe BM. Epidemiology of youth and high school American football-related injuries presenting to United States emergency departments: 2010-2019. Published online May 31, 2021. Phys Sportsmed. doi:10.1080/00913847.2021.1931980 [DOI] [PubMed] [Google Scholar]
- 14. Huang HH, Yen DHT, Kao WF, Wang LM, Huang CI, Lee CH. Declining emergency department visits and costs during the severe acute respiratory syndrome (SARS) outbreak. J Formos Med Assoc. 2006;105(1):31–37. doi:10.1016/S0929-6646(09)60106-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kamel Boulos MN, Geraghty EM. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr. 2020;19(1):8. doi:10.1186/s12942-020-00202-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keays G, Friedman D, Gagnon I. Pediatric injuries in the time of covid-19. Health Promot Chronic Dis Prev Canada. 2020;40(11-12):336–341. doi:10.24095/hpcdp.40.11/12.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Knowles SB, Marshall SW, Miller T, et al. Cost of injuries from a prospective cohort study of North Carolina high school athletes. Inj Prev. 2007;13(6):416–421. doi:10.1136/ip.2006.014720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kraus S, Koch N. Provisional COVID-19 infrastructure induces large, rapid increases in cycling. Proc Natl Acad Sci U S A. 2021;118(15):e2024399118. doi:10.1073/pnas.2024399118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kuitunen I, Ponkilainen VT, Launonen AP, et al. The effect of national lockdown due to COVID-19 on emergency department visits. Scand J Trauma Resusc Emerg Med. 2020;28(1):114. doi:10.1186/s13049-020-00810-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McDonald T, Burghart MA, Nazir N. Underreporting of concussions and concussion-like symptoms in female high school athletes. J Trauma Nurs. 2016;23(5):241–246. doi:10.1097/JTN.0000000000000227 [DOI] [PubMed] [Google Scholar]
- 21. Meier TB, Brummel BJ, Singh R, Nerio CJ, Polanski DW, Bellgowan PSF. The underreporting of self-reported symptoms following sports-related concussion. J Sci Med Sport. 2015;18(5):507–511. doi:10.1016/j.jsams.2014.07.008 [DOI] [PubMed] [Google Scholar]
- 22. Myer GD, Faigenbaum AD, Cherny CE, Heidt RS, Hewett TE. Did the NFL lockout expose the Achilles heel of competitive sports. J Orthop Sports Phys Ther. 2011;41(10):702–705. doi:10.2519/jospt.2011.0107 [DOI] [PubMed] [Google Scholar]
- 23. National Collegiate Athletic Association. NCAA cancels remaining winter and spring championships. Published 2020. Accessed November 9, 2021. https://www.ncaa.org/about/resources/media-center/news/ncaa-cancels-remaining-winter-and-spring-championships
- 24. Nhan DT, Klyce W, Lee RJ. Epidemiological patterns of alternative racquet-sport injuries in the United States, 1997-2016. Orthop J Sports Med. 2018;6(7):2325967118786237. doi:10.1177/2325967118786237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Pillay L, Janse van Rensburg DCC, Jansen van Rensburg A, et al. Nowhere to hide: the significant impact of coronavirus disease 2019 (COVID-19) measures on elite and semi-elite South African athletes. J Sci Med Sport. 2020;23(7):670–679. doi:10.1016/j.jsams.2020.05.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Prien A, Grafe A, Rössler R, Junge A, Verhagen E. Epidemiology of head injuries focusing on concussions in team contact sports: a systematic review. Sports Med. 2018;48(4):953–969. doi:10.1007/s40279-017-0854-4 [DOI] [PubMed] [Google Scholar]
- 27. Ristolainen L, Heinonen A, Waller B, Kujala UM, Kettunen JA. Gender differences in sport injury risk and types of injuries: a retrospective twelve-month study on cross-country skiers, swimmers, long-distance runners and soccer players. J Sport Sci Med. 2009;8(3):443–451. [PMC free article] [PubMed] [Google Scholar]
- 28. The National Federation of State High School Associations. 2018-19 High School Athletics Participation Survey. Accessed April 10, 2021. https://www.nfhs.org/media/1020412/2018-19_participation_survey.pdf
- 29. Rui P, Ashman JJ, Akinseye A. Emergency department visits for injuries sustained during sports and recreational activities by patients aged 5-24 years, 2010-2016. Natl Health Stat Rep. 2019;133:1–15. [PubMed] [Google Scholar]
- 30. Sabbagh RS, Hoge C, Kanhere AP, Coscia AC, Grawe BM. The epidemiology of indoor and outdoor rock climbing injuries presenting to United States emergency departments. Published online June 16, 2021. J Sports Med Phys Fit. doi:10.23736/S0022-4707.21.12578-2 [DOI] [PubMed] [Google Scholar]
- 31. Sallis RE, Jones K, Sunshine S, Smith G, Simon L. Comparing sports injuries in men and women. Int J Sports Med. 2001;22(6):420–423. doi:10.1055/s-2001-16246 [DOI] [PubMed] [Google Scholar]
- 32. Sanford EL, Zagory J, Blackwell JM, Szmuk P, Ryan M, Ambardekar A. Changes in pediatric trauma during COVID-19 stay-at-home epoch at a tertiary pediatric hospital. J Pediatr Surg. 2021;56(5):918–922. doi:10.1016/j.jpedsurg.2021.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Santos-Ferreira D, Tomás R, Dores H. TEAM to defeat Covid-19: a management strategy plan to address return to play in sports medicine. Orthop J Sports Med. 2020;8(9):2325967120951453. doi:10.1177/2325967120951453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Schweizer A, Leiderer A, Mitterwallner V, Walentowitz A, Mathes GH, Steinbauer MJ. Outdoor cycling activity affected by COVID-19 related epidemic-control-decisions. PLoS One. 2021;16(5):e0249268. doi:10.1371/journal.pone.0249268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Seshadri DR, Thom ML, Harlow ER, Drummond CK, Voos JE. Case report: return to sport following the COVID-19 lockdown and its impact on injury rates in the German soccer league. Front Sports Act Living. 2021;3:604226. doi:10.3389/fspor.2021.604226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Sheu Y, Chen LH, Hedegaard H. Sports- and recreation-related injury episodes in the United States, 2011-2014. Natl Health Stat Rep. 2016;99:1–12. [PubMed] [Google Scholar]
- 37. Stern RA, Riley DO, Daneshvar DH, Nowinski CJ, Cantu RC, McKee AC. Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. PM R. 2011;3(10):S460–S467. doi:10.1016/j.pmrj.2011.08.008 [DOI] [PubMed] [Google Scholar]
- 38. Stokes KA, Jones B, Bennett M. Returning to play after prolonged training restrictions in professional collision sports. Int J Sports Med. 2020;41(13):895–911. doi:10.1055/a-1180-3692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Tator CH. Concussions and their consequences: current diagnosis, management and prevention. CMAJ. 2013;185(11):975–979. doi:10.1503/cmaj.120039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. The Outdoor Foundation. Outdoor Participation Report 2019. Accessed April 10, 2021. https://outdoorindustry.org/resource/2019-outdoor-participation-report/
- 41. Tommasone BA, McLeod TCV. Contact sport concussion incidence. J Athl Train. 2006;41(4):470–472. [PMC free article] [PubMed] [Google Scholar]
- 42. Von Rosen P, Heijne A, Frohm A, Friden C, Kottorp A. High injury burden in elite adolescent athletes: a 52-week prospective study. J Athl Train. 2018;53(3):262–270. doi:10.4085/1062-6050-251-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wall BT, Morton JP, van Loon LJC. Strategies to maintain skeletal muscle mass in the injured athlete: nutritional considerations and exercise mimetics. Eur J Sport Sci. 2015;15(1):53–62. doi:10.1080/17461391.2014.936326 [DOI] [PubMed] [Google Scholar]
- 44. Waltzman D, Womack LS, Thomas KE, Sarmiento K. Trends in emergency department visits for contact sports-related traumatic brain injuries among children - United States, 2001-2018. MMWR Morb Mortal Wkly Rep. 2020;69(27):870–874. doi:10.15585/mmwr.mm6927a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wilner B. Roger Goodell orders all NFL team facilities closed for 2 weeks. The Denver Post. March 25, 2020. https://www.denverpost.com/2020/03/25/roger-goodell-orders-nfl-team-facilities-closed-coronavirus/
- 46. Zemper ED. Catastrophic injuries among young athletes. Br J Sports Med. 2010;44(1):13–20. doi:10.1136/bjsm.2009.069096 [DOI] [PubMed] [Google Scholar]