Abstract
Introduction
This study aimed to determine the additional time needed to perform an endometriosis transvaginal ultrasound (eTVUS) compared to routine transvaginal ultrasound (rTVUS).
Methods
A retrospective case–control study was performed. The study group included 199 eTVUS performed between September 2019 and September 2020. The control group comprised 105 consecutive rTVUS studies performed in the same time period. The time stamps on the ultrasound images of all cases in both groups were reviewed to determine the time taken to perform each study. Mean, median, minimum and maximum scan times for both groups were calculated as was percentage difference between scan times. A two‐tailed, unpaired t‐test of the normalised data and a Mann–Whitney U test assessing time difference of scans between two groups were performed with P value <0.05 considered statistically significant.
Results
Performing eTVUS took significantly longer than rTVUS with increases in the mean (8.4 vs 13.8 min, 64%), median (7 vs 12 min, 71%), minimum (4 vs 7 min, 75%) and maximum (19 vs 42 min, 121%) scan times. The Mann–Whitney U test indicated a statistically significant difference in the median scan times (5.0, CI 4.0–6.0), P < 0.001. An independent t‐test of the normalised data revealed a significantly larger mean scan time for eTVUS than rTVUS, Mean = 9.05 95%CI [13.17–4.94], t(302) = 4.327, P < 0.001. R 2 = 0.583.
Conclusion
Endometriosis transvaginal ultrasound added an average 5.4 min to rTVUS, which is statistically significant. For ultrasound departments wanting to offer this technique, doubling the scan time allocated to perform a transvaginal ultrasound (TVUS) is suggested.
Keywords: transvaginal ultrasound, gynaecology, endometriosis, sonographer, allotted time
Introduction
Ultrasound is the front‐line imaging modality in the assessment of all gynaecological conditions, with transvaginal ultrasound (TVUS) being the imaging modality of choice. 1 Endometriosis is one such gynaecological condition, affecting 1 in 9 women and female‐born people, 2 with the ovaries, posterior cul‐de‐sac and uterosacral ligaments the most commonly affected sites. 3 Typical symptoms of endometriosis include pelvic pain, abnormal uterine bleeding and subfertility. 3 As such, many people with endometriosis will present for ultrasound scans to assess for the cause of these symptoms. Despite the frequency of endometriosis, an assessment of the anterior and posterior compartments is not a routine inclusion in Australasian or American gynaecological ultrasound guidelines, 1 , 4 even with many studies to date showing good diagnostic accuracy for this technique. 5 , 6 , 7 , 8 , 9 , 10 Skill of the sonographer and sonologist/radiologist, 11 , 12 , 13 clinical knowledge, 13 scan time availability and lack of adequate Medicare reimbursement 14 are all factors which can pose a barrier for the performance of a comprehensive examination for endometriosis, including an assessment of the anterior and posterior compartments, as part of a routine pelvic ultrasound. As many ultrasound departments experience very high patient loads, finding the additional time needed to extend scans can be challenging. However, with clinical and consumer awareness of endometriosis growing, 2 there is momentum from both professionals and consumers alike to have an assessment for endometriosis during TVUS performed when indicated or even routinely. 15 This study aims to determine the additional time needed for a sonographer to perform a TVUS including an assessment for deep endometriosis in comparison with routine transvaginal ultrasound (rTVUS) within a specialised women's imaging practice.
Methods
Study design
A retrospective case–control study was performed. The study group included patients who underwent endometriosis transvaginal ultrasound (eTVUS), performed by one of three experienced sonographers (AD, CP or AC), at a private women's imaging clinic in Adelaide, South Australia. The control group was comprised of cases who underwent a rTVUS at the same practice by the same three sonographers in the same time period. The three sonographers had between 10 and 25 years of experience performing gynaecological ultrasound and had each performed >1000 eTVUS examinations previously.
Transvaginal ultrasound protocol
All cases were scanned according to the standardised protocols of the practice, based on current guidelines. 1 , 16 The scanning protocols employed for both the rTVUS and eTVUS are outlined in Table 1.
Table 1.
The scanning protocols used for both rTVUS and eTVUS.
| Protocol inclusion | rTVUS | eTVUS |
|---|---|---|
| Uterus + volume measurement | ✓ | ✓ |
| Cervix | ✓ | ✓ |
| Colour Doppler assessment of cervix | ✓ | ✓ |
| Endometrium + thickness measurement | ✓ | ✓ |
| Colour Doppler assessment of endometrium | ✓ | ✓ |
| 3D volume of uterine cavity | ✓ | ✓ |
| Ovaries +volume measurement | ✓ | ✓ |
| Ovarian mobility | ✓ | ✓ |
| Ovarian site‐specific tenderness | ✓ | ✓ |
| Uterine sliding sign | ✓ | ✓ |
| Pouch of Douglas | Assessed for fluid only | Assessed for fluid and nodules of endometriosis |
| Vaginal wall/posterior vaginal fornix | ✗ | ✓ |
| Uterosacral ligaments/torus uterinus + measurement | ✗ | ✓ |
| Rectosigmoid colon | ✗ | ✓ |
| Rectovaginal septum | ✗ | ✓ |
| Bladder | ✗ | ✓ |
| Ureters | ✗ | ✓ |
| Vesicouterine space | ✗ | ✓ |
| Bladder mobility | ✗ | ✓ |
rTVUS, routine transvaginal ultrasound; eTVUS, endometriosis transvaginal ultrasound.
The rTVUS was performed in line with the guidelines of the Australasian Society of Ultrasound in Medicine (ASUM) 1 with TVUS only being performed unless the patient did not consent to TVUS or the entirety of the uterus and ovaries could not be assessed via TVUS (e.g. when large fibroids were present). 1 Scans were routinely performed with an empty bladder to optimise both patient comfort and improve visualisation of the uterus and ovaries. For rTVUS, the uterus, endometrium and ovaries were measured and assessed for signs of pathology. A three‐dimensional volume of the uterine cavity was obtained. Mobility of the ovaries was tested with probe pressure and site‐specific tenderness (SST) noted. Status of the ‘sliding sign’ 17 was investigated, and the pouch of Douglas (POD) was assessed for the presence of fluid only.
eTVUS was performed in line with the International Deep Endometriosis Assessment (IDEA) group consensus. 16 eTVUS studies were acquired as per the rTVUS, with the addition of a dedicated assessment of the anterior compartment (bladder, ureters and vesicouterine space) and the posterior compartment (rectovaginal septum, rectosigmoid colon, uterosacral ligaments/torus uterinus and posterior vaginal fornix) (Table 1). The POD was assessed for both the presence of fluid and endometriotic nodules during the eTVUS protocol. No bowel preparation was used for the assessment of the rectosigmoid colon.
Scans were performed using a Philips Epiq Elite ultrasound system with a C10‐3MHz 2D transvaginal transducer or a C8‐5 MHz 3D transvaginal transducer (Philips Medical Systems, Andover, MA, USA), a Philips IU22 ultrasound system with a C10‐3 transvaginal transducer (Philips Medical Systems) or a GE Voluson E10 with a 5‐8 MHz transducer (GE Healthcare, Chicago, IL, USA).
Case identification and data collection
A sample size calculation was performed prior to data collection using G‐power software, 18 which found for a power of 0.95 and an effect size of 0.5, and a minimum sample size of 105 was needed for each group.
Data were retrospectively collected from the practice picture archiving computer system (PACS) and Contrast ONE (Contrast Imaging solutions, Brisbane, Australia). The study group (eTVUS) was comprised of 201 consecutive cases who presented for TVUS with a clinical suspicion of endometriosis between September 2019 and September 2020 inclusive. The cases in the control group were identified by performing a filtered search of reports for pelvic ultrasounds within the same data range, where the reports did not contain the word ‘endometriosis’, which excluded any cases who underwent eTVUS. Consecutive records of 127 cases were reviewed until 105 cases had been identified to form the control group. Two cases were excluded from the eTVUS group, resulting in the scan times from 199 cases being included (Table 2).
Table 2.
Reasons for exclusion of cases.
| Excluded cases | ||
|---|---|---|
| Reason | rTVUS group | eTVUS group |
| TA only | 5 | |
| Incomplete TVUS | 7 | |
| No time stamps | 1 | 1 |
| Different sonographer | 6 | |
| Endometriosis scan | 1 | |
| Early pregnancy scan | 2 | |
| Scan performed over two episodes | 1 | |
| Total | 22 | 2 |
TA, transabdominal ultrasound; TVUS, transvaginal ultrasound; rTVUS, routine transvaginal ultrasound; eTVUS, endometriosis transvaginal ultrasound.
The time stamps on the ultrasound images of all cases in both groups were reviewed. The start time was defined as the earliest time stamp on stored images. The end time is defined as the latest time stamp on stored images. Scan times were recorded in whole minutes only. If images in addition to TVUS were performed (e.g. pelvic floor, kidneys, transabdominal imaging), only the time taken for the TVUS segment was included. Data were double entered for quality assurance. Cases were excluded if: time stamps were not visible, studies were only performed transabdominally, TVUS was incomplete, or scans took place over two episodes. The reasons for exclusion from the final analysis can be seen in Table 2.
Statistical analysis
Mean, median, minimum and maximum scan times for both groups were calculated as was percentage difference between scan times for the two groups. Data were checked for normalcy. The non‐normally distributed raw data were analysed using a two‐tailed unpaired non‐parametric test (Mann–Whitney U test) assessing time difference of scans between the two groups (rTVUS vs eTVUS), with a P value <0.05 considered statistically significant. The data were also transformed, and the normalised data analysed using a two‐tailed, unpaired parametric t‐test. Statistical analysis was performed using GraphPad Prism version 8.0.0 for Windows (GraphPad Software, San Diego, CA USA).
Ethical approval
This project was approved by the University of South Australia Human Research Ethics Committee (project number 204082).
Results
The distribution of scan times for both groups can be seen in Figures 1 and 2. Performing eTVUS took significantly longer than performing rTVUS with increases in the mean (8.4 vs 13.8 min, 64%), median (7 vs 12 min, 71%), minimum (4 vs 7 min, 75%) and maximum (19 vs 42 min, 121%) scan times as outlined in Table 3. The data did not follow a Gaussian distribution (Figure 2). The Mann–Whitney U test indicated that there was a statistically significant difference in the median scan times of 5.0 min (CI 4.0 = 6.0), U (NRTVS = 105, NETVS = 199) = 3243, P < 0.001.
Figure 1.
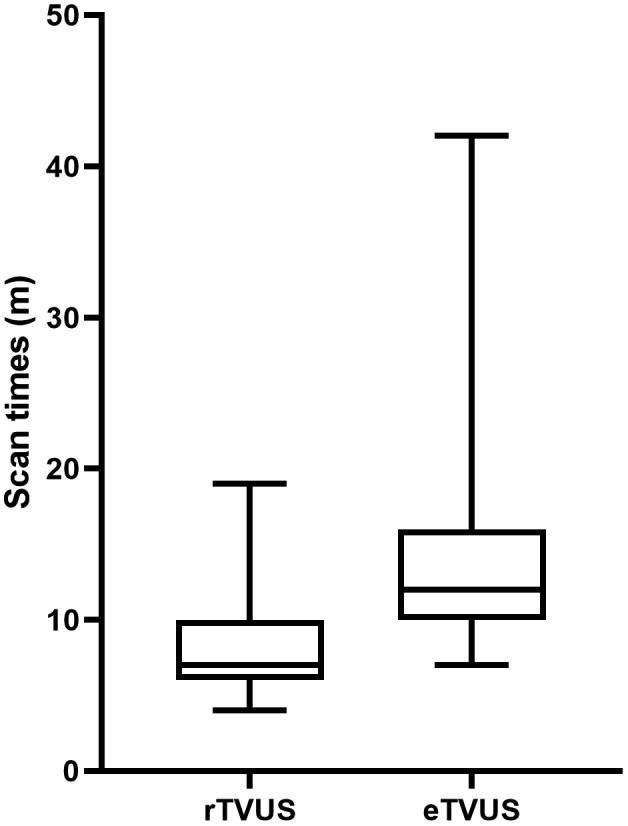
F A box and whisker plot of the distribution of scan times for both the rTVUS and eTVUS group.
Figure 2.
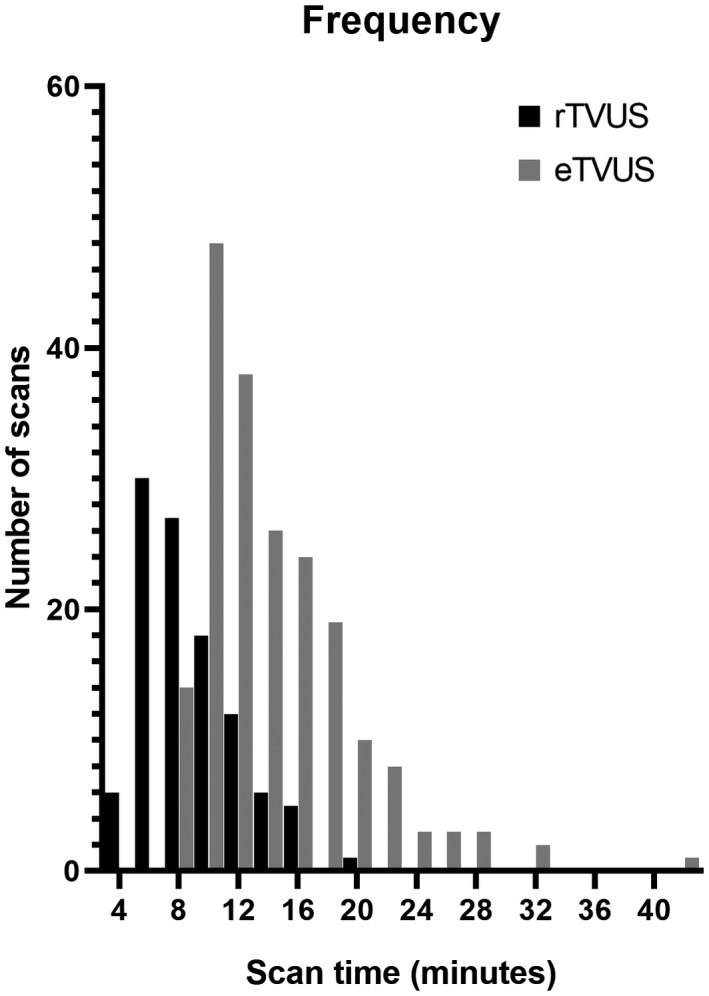
A histogram of the frequency distribution of scan times for both the rTVUS and eTVUS group. The data do not follow a Gaussian distribution.
Table 3.
Scan times for both groups with simple statistics (mean, median, minimum and maximum) plus absolute and percentage differences between the groups.
| Scanning times (min) | |||
|---|---|---|---|
| rTVUS | eTVUS | Difference (%) | |
| All sonographers | |||
| n | 105 | 199 | – |
| Mean (±SD) | 8.4 (±3.2) | 13.8 (±5.2) | 5.4 (64%) |
| Median | 7 | 12 | 5.0 (71%) |
| Minimum | 4 | 7 | 3.0 (75%) |
| Maximum | 19 | 42 | 23.0 (121%) |
| IQR (25%, 75%) | 6.0–10.0 | 10.0–16.0 | – |
| Sonographer A | |||
| n | 50 | 36 | – |
| Mean (±SD) | 8.9 (±3.5) | 16.4 (±6.4) | 7.5 (84%) |
| Median | 8 | 16 | 8.0 (100%) |
| Minimum | 4 | 7 | 3.0 (75%) |
| Maximum | 19 | 32 | 13.0 (68%) |
| IQR (25%, 75%) | 6.0–11.3 | 11.3–20.8 | – |
| Sonographer B | |||
| n | 29 | 122 | – |
| Mean (±SD) | 6.9 (±2.4) | 13.6(±5.2) | 6.7 (97%) |
| Median | 6 | 12 | 6.0 (100%) |
| Minimum | 4 | 8 | 4.0 (100%) |
| Maximum | 15 | 42 | 27.0 (180%) |
| IQR (25%, 75%) | 5.0–7.5 | 10.0–16.0 | – |
| Sonographer C | |||
| n | 26 | 41 | – |
| Mean (±SD) | 8.6 (±2.9) | 12.3 (±3.5) | 3.7 (43%) |
| Median | 8.5 | 12 | 3.5 (41%) |
| Minimum | 4 | 7 | 3.0 (75%) |
| Maximum | 15 | 21 | 6.0 (40%) |
| IQR (25%, 75%) | 6.0–10.3 | 10.0–14.3 | – |
An independent t test of the normalised data revealed that eTVUS took significantly longer than rTVUS, Mean = 9.05 95%CI [13.17–4.94], t(302) = 4.327, P < 0.001. R 2 = 0.583. Overall, the mean eTVUS time was 5.4 min longer than the mean time of rTVUS.
When broken down by the performance of the individual sonographers, similar trends were noted as outlined in Table 3.
Discussion
This study has shown that performing eTVUS adds a statistically significant amount of time to rTVUS with a 71% increase in the median scan times and 64% increase in the mean scan times. To the best of our knowledge, this is the first paper published to date assessing the additional time burden of performing eTVUS in comparison with rTVUS. When broken down between individual sonographers as outlined in Table 3, there was a discrepancy between the percentage differences seen between sonographer B and sonographer C (mean 97% vs 43%, median 100% vs 41%, minimum 100% vs 75% and maximum 180% vs 40%). As scan times typically were relatively quick (rTVUS mean 8.4 min vs eTVUS mean 13.8 min), these differences were not as stark when comparing the minute values.
A strength of this study was its large sample size in both the study and control groups. This large sample size suggests our reported means are likely quite accurate and allowed us to include the outliers, highlighting that in cases of severe endometriosis (e.g. multiple nodules and extensive adhesions), extremely long scan times can be required, much more so than seen in rTVUS. One eTVUS took 42 min to perform which was significantly longer than most other eTVUS cases. This case involved extensive deep endometriosis with multiple nodules in multiple anatomical locations (Figure 3) and extensive adhesions (Videos 4, 5) causing distortion to the normal pelvic anatomy. It should also be noted that this was 180% longer than the longest rTVUS (19 min). It must therefore be considered that although infrequently occurring, cases of severe endometriosis encountered during eTVUS can result in excessively long scan times being required.
Figure 3.
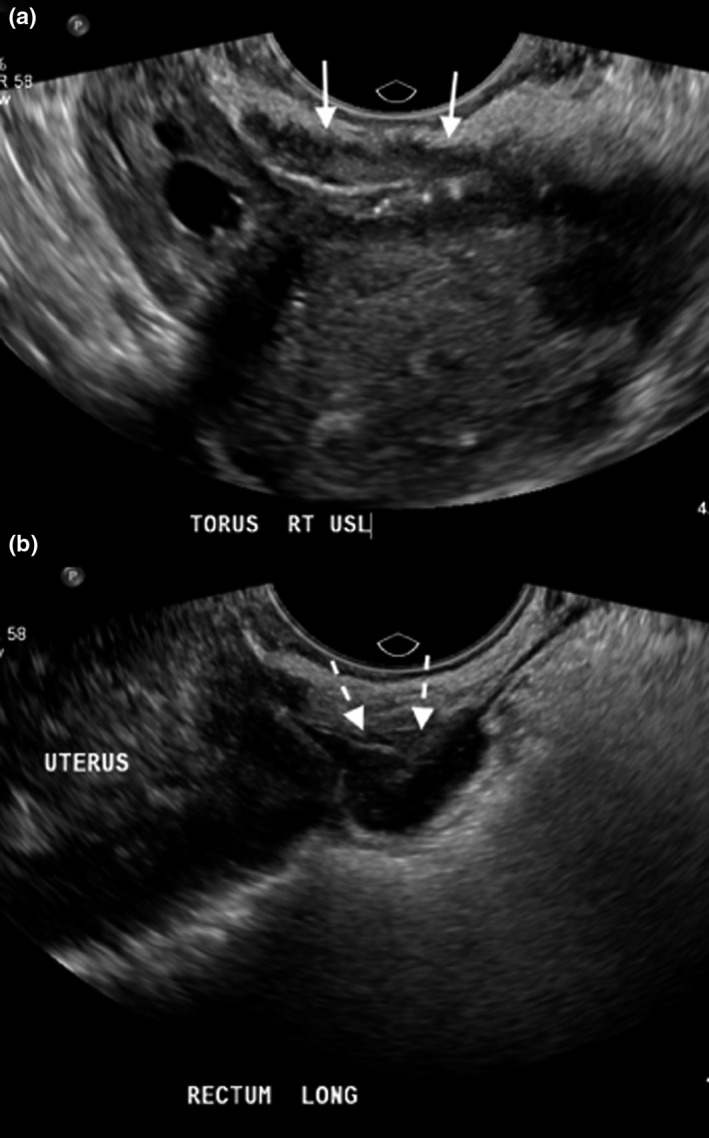
Two nodules of endometriosis seen within the pelvis of the case which took 42 minutes. A large nodule of endometriosis is seen within the right uterosacral ligament, extending into the torus uterinus as shown by the white solid arrows (a). A nodule of endometriosis was also seen within the rectal wall (b) as depicted by the dashed arrows. Also present in this case were extensive pelvic adhesions, including obliteration of the pouch of Douglas and a left ovarian cyst (not pictured).
Figure 4.

Gentle pressure is being applied to the right ovary and uterus with the transvaginal transducer. The right ovary and uterus can be seen to move together, along with the right uterosacral ligament and the large nodule within. This is due to dense adhesions in this region.
Figure 5.

The uterine ‘sliding sign’ manoeuvre is being performed by applying gentle pressure with the transvaginal transducer to the posterior vaginal fornix. The posterior wall of this retroverted uterus and the adjacent anterior rectal wall are not seen to move apart freely suggesting obliteration of the pouch of Douglas.
Despite evidence in favour of eTVUS first appearing within the literature nearly two decades ago, 19 eTVUS is still predominantly only available in specialised gynaecological imaging centres throughout Australia, with rTVUS typically performed as the norm in general imaging settings, even when patients present with a clinical suspicion of endometriosis. 15 Several proponents of eTVUS have advocated for the incorporation of eTVUS into all rTVUS, regardless of the scan indication, 15 , 20 whilst others have pushed for a minimum of quality ultrasound assessment, which includes assessment of the anterior and posterior compartments for people with suspected endometriosis prior to surgical intervention. 21 There is a paucity within the literature explaining why the uptake of eTVUS within routine sonographic practice has been slow. Skill of the sonographer and sonologist/radiologist 11 , 12 , 13 and clinical knowledge 13 have been alluded to within published works as such barriers. Additionally, the need to perform dynamic assessments (when the sonographer performing these is not the clinician reporting the findings), lack of adequate remuneration and scan time limitations have also been anecdotally reported in our professional encounters and conversations as barriers to the uptake of this technique. This study has shown that performing eTVUS adds an average of 5.4 min to rTVUS, which, whilst not excessive, is a significant additional time requirement, which needs to be considered when formulating scanning protocols. In Australia, as there is currently no additional remuneration from Medicare for extending an rTVUS to include eTVUS, 14 this additional time allocation may be cost prohibitive in some centres.
Endometriosis is a very common condition and currently carries a diagnostic delay of approximately 6.4 years. 22 As people presenting for gynaecological ultrasound do not represent the general population, but rather those with a high likelihood of various gynaecological conditions, the prevalence of endometriosis amongst patients presenting for gynaecological ultrasound is likely far higher. Leonardi et al. 23 reported that approximately 28% of patients presenting for TVUS in a gynaecology‐focused ultrasound practice had a high clinical suspicion of endometriosis. The addition of an assessment of the anterior and posterior compartments would therefore be a high value inclusion to many rTVUS examinations and could aid in reducing the diagnostic delay, especially in cases of deep endometriosis. 24 Although the additional time required to perform eTVUS may be undesirable for patients, especially if experiencing pelvic pain, within their review, Deed et al. 25 found TVUS to typically be well accepted by patients, especially if adequately informed of the need for such imaging. As such, it is likely that with sufficient informed consent, the additional time burden required to complete an eTVUS would likely result in an improved patient experience; however, studies exploring this hypothesis are needed. Given the potential for improved outcomes for patients, inclusion of eTVUS into both local departmental scanning protocols and future national guideline updates should be considered. If the additional time requirement presented is prohibitive, reallocation of time from other aspects of gynaecological ultrasound protocols with lower clinical value, such as extensive TAS or routine kidney imaging, 26 could be contemplated.
We were unable to locate any published works to date which can aid clinicians in planning for adequate time allocation for eTVUS. Whilst several guidelines exist to aid departments in the design of scanning protocols for gynaecological ultrasound, 1 , 4 , 16 there is no guidance for what constitutes an appropriate scan time. We hope that this work can be well utilised by ultrasound departments in the formation of protocols for the inclusion of eTVUS when indicated.
There are several limitations within this study that must be considered if doing this. Firstly, the times reported in this study were obtained retrospectively from the review of time stamps to judge transvaginal scan times. As these only represent when images were taken, and sonographers may spend time before the acquisition of the first image or after the acquisition of the last image assessing structures in real time, this may have resulted in an under reporting of the true time taken to perform both rTVUS and eTVUS.
Additionally, any extension images required (such as transabdominal views or kidney images) were excluded from our analysis. The reported times also do not take into account the time sonographers spend communicating with patients, gaining consent, having patients prepare for examination (e.g. emptying bladder and undressing) and performing post exam duties (e.g. having patients redress, cleaning and disinfecting transvaginal probes and writing worksheets). As such, the reported times do not represent the appointment times required to complete the examination. The sonographers involved in this study also report that completing the required sonographers report or worksheet for complex eTVUS cases is significantly more time‐consuming than for rTVUS. Measurement of this was beyond the scope of this study.
This study was completed within a specialised women’s imaging centre. The sonographers involved in this study were all very experienced and specialised in obstetric and gynaecological ultrasound. As such, these findings may not translate to less experienced or more generalised sonographers. Although the mean additional time needed for eTVUS was 5.4 min, a less experienced or non‐specialised sonographer would likely need longer to complete both rTVUS and eTVUS. Median scan times of eTVUS were double that of rTVUS for one of our participating sonographers, despite extensive experience. We would therefore suggest that, if looking to incorporate an assessment for endometriosis into rTVUS appointments, practices consider doubling the time allocated to performing a TVUS. In‐house time audits could be performed to assess how this would translate to examination times within a specific department. Future prospective studies assessing time allocation for eTVUS would be beneficial, as would studies from general imaging settings to further support the development of robust, thorough and achievable scanning protocols.
Conclusion
Endometriosis transvaginal ultrasound took an average of 5.4 min longer to perform than rTVUS, which resulted in significantly longer mean (64%) and median (71%) scan times. As there is currently no additional Medicare rebate offered for performing eTVUS rather than rTVUS, an assessment for endometriosis could be cost prohibitive in some Australian centres. As such, future reviews of the Medicare Benefit Scheme must take this into account to ensure patient access to eTVUS is not impeded and diagnosis is not avoidably delayed.
To the authors’ knowledge, this is the first published study looking at time allotment for eTVUS. As this study was performed within a specialised women’s imaging practice, these findings may not translate to less experienced or more generalised sonographers. Therefore, future prospective studies assessing time provision for eTVUS would be beneficial as would studies from general imaging settings.
Author Contributions
Alison Deslandes: Conceptualization (lead); Data curation (equal); Formal analysis (lead); Investigation (lead); Methodology (lead); Project administration (lead); Writing‐original draft (lead); Writing‐review & editing (equal). Nayana Parange: Conceptualization (supporting); Formal analysis (supporting); Investigation (supporting); Methodology (supporting); Supervision (supporting); Writing‐review & editing (equal). Jessie Childs: Conceptualization (supporting); Formal analysis (supporting); Investigation (supporting); Methodology (supporting); Supervision (supporting); Writing‐review & editing (equal). Brooke Osborne: Conceptualization (supporting); Formal analysis (supporting); Investigation (supporting); Methodology (supporting); Supervision (supporting); Writing‐review & editing (equal). Catrina Pannucio: Data curation (equal); Writing‐review & editing (equal). Anthea Croft: Data curation (equal); Writing‐review & editing (equal). Eva Bezak: Conceptualization (supporting); Formal analysis (supporting); Investigation (supporting); Methodology (supporting); Project administration (supporting); Supervision (lead); Writing‐review & editing (equal).
Funding
No funding information is provided.
Conflict of Interest
Alison Deslandes is a director of ASUM. Catrina Panuccio is the managing director of Specialist Imaging Partners.
References
- 1. Australasian Society of Ultrasound in Medicine (ASUM) . Guidelines on the Performance of a Gynaecological Ultrasound Examination; 2020. Available from http://www.asum.com.au/files/public/SoP/curver/Obs‐Gynae/Gynaecological‐GL‐2020.pdf. Accessed 01 July 2021.
- 2. Rowlands I, Abbott J, Montgomery G, Hockey R, Rogers P, Mishra G. Prevalence and incidence of endometriosis in Australian women: a data linkage cohort study. BJOG 2021; 128(4): 657–65. [DOI] [PubMed] [Google Scholar]
- 3. Sengupta J, Anupa G, Bhat MA, Ghosh D. Molecular biology of endometriosis. Hum Reprod 2017; 71–141. [Google Scholar]
- 4. American Institute of Ultrasound in Medicine (AIUM) . AIUM practice guideline for the performance of ultrasound of the female pelvis. J Ultrasound Med 2014;33(6):1122. [DOI] [PubMed] [Google Scholar]
- 5. Deslandes A, Parange N, Childs JT, Osborne B, Bezak E. Current status of transvaginal ultrasound accuracy in the diagnosis of deep infiltrating endometriosis before surgery. J Ultrasound Med 2020; 39(8): 1477–149. [DOI] [PubMed] [Google Scholar]
- 6. Gerges B, Li W, Leonardi M, Mol B, Condous G. Meta‐analysis and systematic review to determine the optimal imaging modality for the detection of rectosigmoid deep endometriosis. Ultrasound Obstet Gynecol 2020; 58: 190–200. [DOI] [PubMed] [Google Scholar]
- 7. Gerges B, Li W, Leonardi M, Mol B, Condous G. Meta‐analysis and systematic review to determine the optimal imaging modality for the detection of bladder deep endometriosis. Eur J Obstet Gynecol Reprod Biol 2021; 261: 124–33. [DOI] [PubMed] [Google Scholar]
- 8. Guerriero S, Ajossa S, Minguez JA, Jurado M, Mais V, Melis GB, et al. Accuracy of transvaginal ultrasound for diagnosis of deep endometriosis in uterosacral ligaments, rectovaginal septum, vagina and bladder: systematic review and meta‐analysis. Ultrasound Obstet Gynecol 2015; 46(5): 534–45. [DOI] [PubMed] [Google Scholar]
- 9. Guerriero S, Ajossa S, Orozco R, Perniciano M, Jurado M, Melis GB, et al. Accuracy of transvaginal ultrasound for diagnosis of deep endometriosis in the rectosigmoid: systematic review and meta‐analysis. Ultrasound Obstet Gynecol 2016; 47(3): 281–9. [DOI] [PubMed] [Google Scholar]
- 10. Nisenblat V, Bossuyt PM, Farquhar C, Johnson N, Hull ML. Imaging modalities for the non‐invasive diagnosis of endometriosis. Cochrane Database Syst Rev 2016;2(2):CD009591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Agarwal SK, Chapron C, Giudice LC, Laufer MR, Leyland N, Missmer SA, et al. Clinical diagnosis of endometriosis: a call to action. Am J Obstet Gynecol 2019; 220(4): 354 e1–354 e12. [DOI] [PubMed] [Google Scholar]
- 12. As‐Sanie S, Black R, Giudice LC, Gray Valbrun T, Gupta J, Jones B, et al. Assessing research gaps and unmet needs in endometriosis. Am J Obstet Gynecol 2019; 221(2): 86–94. [DOI] [PubMed] [Google Scholar]
- 13. Menakaya UA. Capacity building in endometriosis ultrasound: are we there yet? Australas J Ultrasound Med 2015; 18(4): 129–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Australian Government, Department of Health . Medicare benefits schedule (MBS) online. Canberra: Australian Govt. Pub. Service; 2021. Available from http://www.mbsonline.gov.au/internet/mbsonline/publishing.nsf/Content/Home. Accessed 01 August 2021. [Google Scholar]
- 15. Piessens S. Is it time to include assessment of the most common gynaecological condition in the routine ultrasound evaluation of the pelvis? Australas J Ultrasound Med 2019; 22(2): 83–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guerriero S, Condous G, van den Bosch T, Valentin L, Leone FPG, Van Schoubroeck D, et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, definitions and measurements: a consensus opinion from the International Deep Endometriosis Analysis (IDEA) group. Ultrasound Obstet Gynecol 2016; 48(3): 318–32. [DOI] [PubMed] [Google Scholar]
- 17. Reid S, Lu C, Casikar I, Reid G, Abbott J, Cario G, et al. Prediction of pouch of Douglas obliteration in women with suspected endometriosis using a new real‐time dynamic transvaginal ultrasound technique: the sliding sign. Ultrasound Obstet Gynecol 2013; 41(6): 685–91. [DOI] [PubMed] [Google Scholar]
- 18. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: A flexible statistical analysis program for the social, behavioral and biomedical sciences. Behav Res Methods 2007; 39: 175–91. [DOI] [PubMed] [Google Scholar]
- 19. Bazot M, Thomassin I, Hourani R, Cortez A, Darai E. Diagnostic accuracy of transvaginal sonography for deep pelvic endometriosis. Ultrasound Obstet Gynecol 2004; 24(2): 180–5. [DOI] [PubMed] [Google Scholar]
- 20. Piessens S, Edwards A. Sonographic evaluation for endometriosis in routine pelvic ultrasound. J Minim Invasive Gynecol 2020; 27(2): 265–6. [DOI] [PubMed] [Google Scholar]
- 21. Reid S, Winder S, Condous G. Sonovaginography: redefining the concept of a “normal pelvis” on transvaginal ultrasound pre‐laparoscopic intervention for suspected endometriosis. Australas J Ultrasound Med 2011; 14(2): 21–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. O’Hara R, Rowe H, Fisher J. Managing endometriosis: a cross‐sectional survey of women in Australia. J Psychosom Obstet Gynaecol 2020; 1–8. [DOI] [PubMed] [Google Scholar]
- 23. Leonardi M, Martins WP, Espada M, Georgousopoulou E, Condous G. Prevalence of negative sliding sign representing pouch of Douglas obliteration during pelvic transvaginal ultrasound for any indication. Ultrasound Obstet Gynecol 2020; 56(6): 928–33. [DOI] [PubMed] [Google Scholar]
- 24. Hudelist G, Fritzer N, Thomas A, Niehues C, Oppelt P, Haas D, et al. Diagnostic delay for endometriosis in Austria and Germany: causes and possible consequences. Hum Reprod 2012; 27(12): 3412–6. [DOI] [PubMed] [Google Scholar]
- 25. Deed K, Childs J, Thoirs K. What are the perceptions of women towards transvaginal sonographic examinations? Sonography 2014; 1(2): 33–8. [Google Scholar]
- 26. Brennan O, Oh S, Necas M. The value of surveying the kidneys during pelvic ultrasound examinations. Australas J Ultrasound Med 2019; 22(2): 118–28. [DOI] [PMC free article] [PubMed] [Google Scholar]


