Summary
Background
Prevalence and exposures of adverse birth outcomes is well studied in low-and-middle-income countries but not well-established for the Pacific Island region. Our study mapped the available evidence on low birth weight (LBW), preterm birth, and small for gestational age (SGA)’s prevalence and their corresponding risks in the region.
Methods
We followed the five-staged Arksey and O'Malley's framework with clinicians’ consultation in the region. Five scholarly databases and non-indexed studies were searched and extracted data were analysed as numerical and thematic summaries mapping the outcomes and exposures.
Findings
We included 20 studies representing 11 Pacific Island countries with the following mean prevalence and associations at 95% confidence interval. Estimated mean prevalence for LBW and preterm births were 12% and 13%, respectively. LBW were associated with malaria in pregnancy [aOR 3.3 (1.00, 10.60)], and betel nut and tobacco [aOR 2.4 (1.00, 6.00)]. Preterm births were associated with malaria in pregnancy [aOR 6.6 (2.46, 17.62)] and maternal obesity [aOR 1.5 (1.00, 2.30)]. SGA were associated with short stature [aOR 1.7 (1.22, 2.41)] and no antenatal bookings [aOR 4.0 (2.12, 7.57)]
Interpretation
Several significant factors identified were malaria infection, obesity, betel nut and tobacco and no antenatal care, also validated by clinicians consulted.
Funding
Australia National Health and Medical Research Council.
Keywords: Adverse birth outcomes, Low birth weight, Preterm birth, Risk factors, Pacific Island countries, Pacific Islands region
Research in context.
Evidence before this study
Adverse birth outcomes such as low birth weight, preterm birth and fetal growth restriction are the primary cause of infant and child mortality and morbidity in low-and middle-income countries, including the Pacific Island region. At the outset, we conducted a literature review and initial searches on scholarly databases and online using Google and Google scholar search engines to survey the current literature on the topic using key concept terms such as adverse “birth outcomes”, “pregnancy risk factors”, and the “Pacific Island region.” We found no systematic or narrative, or scoping reviews conducted in the Pacific region on this topic. We also found a minimal number of primary studies that reported on the prevalence and measures of association of exposures and adverse birth outcomes in the region.
Added value of this study
To our knowledge, this is the first comprehensive scoping review exploring the prevalence and factors of adverse birth outcomes in the Pacific Island regions. There is limited number of research in the region on the prevalence and risk of adverse birth outcomes. Of the few studies conducted, which we reviewed in the current study, malaria in pregnancy, betel nut and tobacco use during pregnancy, obesity in pregnancy, and no and low antenatal care were notable exposures associated with adverse birth outcomes. The findings were also validated by 18 clinicians consulted working in maternal and neonatal health care from 4 countries in the region.
Implications of all the available evidence
Despite limited studies in the Pacific region, we found several important risk factors such as malaria infection, obesity, betel nut and tobacco and no antenatal care during pregnancy to be associated with the adverse birth outcomes, which are essential to inform the literature and evidence for clinical practice. Also, further study is needed to investigate the burden of adverse birth outcomes in the region.
Alt-text: Unlabelled box
Introduction
Adverse birth outcomes contribute to poorer childhood outcomes and are the primary cause of child mortality and morbidity in low-and middle-income countries (LMICs). Adverse birth outcomes, including preterm birth, small for gestational age (SGA), low birth weight (LBW), stillbirths and miscarriage, are associated with a range of social, biological, and environmental risk factors.1, 2, 3, 4
Early birth, most commonly defined as preterm birth or birth before 37 weeks of gestation, is a major determinant for neonatal mortality and morbidity.5 Preterm birth often necessitates therapy, and its prevention requires treatment, both of which are less accessible in LMICs, and can contribute to excess morbidity burden.6,7 Growth restriction while in utero can contribute to morbidity with preterm birth. SGA, a retrospective proxy for fetal growth restriction, occurs when the birth weight falls below a cut-point in the gestational age and sex-specific birth weight distribution. This cut-point is commonly the lowest 10th centile or a multiple of standard deviations below the mean weight.8 In LMICs, retrospective proxies fetal growth restriction such as SGA is determined at birth due to the lack of fetal monitoring systems during pregnancy, no routine recording of gestational dates and start of the last menstrual period, and limited availability of ultrasound dating.6 The most common proxy for both preterm birth and fetal growth restriction in LMICs is LBW, which is defined as birth weight less than 2500 g. Term LBW, defined as low birth weights from 37 weeks of completed gestation, and SGA are the preferred indicators for fetal growth restriction as newborn weight is also a consequence of time spent in utero.9 It is well established that infants that are preterm, term LBW and SGA are at elevated risk of early childhood mortality.10,11
Most of the deaths attributable to fetal growth restriction and preterm birth occur as miscarriages before the gestational age of viability or stillbirths, occurring from viability to delivery. Although there is no global consensus on when a fetus is viable, the most well adopted gestational age cut-off to discern miscarriages from stillbirths in LMICs is 28 weeks of gestation.12 According to the global burden of disease study, the prevalence of stillbirths in LMICs has been reported to be as high as 20 per 1000 live births, with Papua New Guinea (PNG) reporting 16.3 per 1000 live births.10
The Pacific Island region comprises countries with developing economies with potentially high infant and child mortality rates resulting from poor pregnancy and birth outcomes. The region consists of 22 Melanesian, Polynesian, and Micronesian countries with 12 independent sovereignties and 10 dependent or unincorporated territories either by the United States, France or New Zealand.13 It is a diverse territory in terms of socioeconomic development, culture, population and geography, with a myriad of risk factors relevant to perinatal health and early childhood mortality.14 Most Pacific Island countries are under-resourced with inadequate health facilities that affect maternal and infant health to various extents across the region, signified in several health indicators.15 For example, infant mortality has been reported to be higher in the PNG region of Melanesia (70/1000 live births) compared to the Cook Islands of Polynesia (10/1000 live births).16,17 Antenatal care coverage and skilled birth attendance in Tonga and Samoa are over 95%,18, 19, 20 compared to 49% in PNG.21 Geographical challenges across land and sea magnified by infrastructure limitations in PNG and countries of Melanesia are some of the barriers contributing to low antenatal attendance and skilled birth.14,22 Trends in morbidity and mortality due to communicable and non-communicable diseases (NCD) varies across the different subregions.14 Obesity-related NCD morbidities and mortalities in Polynesian countries of Tonga and Samoa have significantly increased.18 While, in the Melanesian region, PNG and Solomon Islands have seen a two-fold increase in the burden of NCD and communicable diseases such as diabetes and malaria across adult populations,23 and severe malnutrition among women and children.24
Maternal health in the Pacific Islands is challenged by geographical disparities and dynamics in the various parts of the region. Most Pacific Island communities are isolated by sea or land, which limits access to health services, which is added to a background of already elevated risk from socioeconomic disadvantage.14,22 The low lying islands of Polynesia and Micronesia and elsewhere in the region are continually faced with the health challenges associated with global warming.25 The wider Pacific island countries are frequently affected by natural hazards such as cyclones, floods and coastal erosion, earthquakes, and tsunamis affecting the people's livelihood and overstretching the limited health resources.22,26 Vector-borne disease such as malaria and dengue is prevalent due to the climate, recurrent heavy rains and tropical cyclones.27,28 Women and children are often vulnerable to malnutrition due to food shortages and diarrhoeal diseases in the aftermath of natural disasters.14,25
Cultural and social practices also precipitate various health risks. Betel nut use is practised in PNG, Solomon Islands, Palau and the Marshall Islands.29 Studies have reported that betel nut use is associated with oral cancers in the region and elsewhere.29,30 Studies in LMIC countries outside the Pacific Island region (South East Asia) have also shown betel nut use to be adversely associated with adverse birth outcomes.29 Kava, a traditional drink made from Piper methysticum, is another unique exposure to many Pacific Islanders, including those from Fiji, Vanuatu and Samoa.31 There is a dearth of studies on kava use and its impact on birth outcomes,32 and to date, there has been no systematic assessment of the burden of, and risk factors for adverse birth outcomes in the Pacific Island region. This scoping review aimed to map the available literature on the prevalence of adverse birth outcomes and associated risk factors in the Pacific Island countries and gain additional insights and recommendations from the perspective of health professionals.
Methods
Study design and protocol
The systematic scoping review was registered with the Joanna Briggs Institute,33 and a detailed description of the methods was published as a protocol.34 Our review followed the Joanna Briggs Institute Reviewers Manual35 derived from Arksey and O'Malley's five-staged methodological framework.36 We also included a consultation exercise, interviewing health professionals from four countries in the region.
Research question
Our review was guided by the following research questions: (i) what is the prevalence of the adverse birth outcomes in the Pacific Island region? And (ii) what are the risk factors for adverse birth outcomes in the Pacific Island region?
Study selection and inclusion
We selected studies that corresponded to the population, concept, and context (PCC) criteria. In the review, ‘population’ includes women and births from the pacific countries, ‘concept’ includes the various social, health and behavioural risk factors associated with adverse birth outcomes. The ‘context’ included 22 sovereign island states and territories of the region, namely: American Samoa, Cook Islands, Easter Islands, Federated States of Micronesia, Fiji, Guam, Kiribati, Commonwealth of the Northern Mariana Islands (CNMI), Marshall Islands, Nauru, New Caledonia, Niue, Palau, PNG, Samoa, Solomon Islands, Tahiti, Tokelau, Tonga, Tuvalu, Vanuatu, and Wallis and Futuna.37 We considered studies published between 1 January 2000 and 28 February 2021. Studies with populations from high-income countries located in the Pacific region (e.g., Australia, New Zealand, the United States) were excluded.
Literature search
The authors consulted the Curtin University Health Science librarian to design the search strategy. Prior to the search, a preliminary literature review was undertaken to understand the extent of literature on the subject in the context. The literature search was carried out in three-stages as outlined by the Joanna Briggs Institute.38,39 In stage one, key concept terms were selected from CINAHL to identify Medical Subject Headings (MeSH) or text terms contained within the titles and abstracts of articles. Key concept terms used were adverse “birth outcomes”, “pregnancy risk factors” and the “Pacific Island region.” In stage two, all MeSH terms, key concept terms, and their synonyms were combined with Boolean operators, truncations, and wildcards to develop search strings and applied across the selected databases such as CINAHL, Medline, ProQuest, SpringerLink and Scopus. In this stage, search strings were either general or specific with their corresponding key concept terms and synonyms combined with MeSH terms identified before applying them to the database. Stage three involved searching using Google and Google Scholar for non-indexed studies on regional websites of the World Health Organisation (WHO), the Secretariat of Pacific Community and United Nation International Children Emergency Fund and hand searching reference lists of studies initially retrieved. A table of full search strategies is outlined in Supplementary File 1.
Data charting process
Once all retrieved records that matched the PCC criteria were exported to Endnote 9, we conducted data extraction based on a priori data extraction tool developed by LSKK and discussed with the co-authors (Supplementary File 2). During the data extraction, all results were entered into Excel spreadsheets alongside standard bibliographic information that included author(s), year of publication, country where the study were conducted, aims and purpose, study population, intervention type, intervention duration, outcomes, and details of key findings, including prevalence on the outcomes identified in the study and associated risk factors. LSKK conducted the data extraction and later reviewed and discussed by GAT, JJ, and GP. All arising questions and uncertainty during the process was discussed with the research team to reach an agreement.
Summarising and reporting the results
The findings, presented as tables, were obtained by mapping the data extracted from the selected articles and guided by Arksey and O'Malley.36 Information on the prevalence of LBW, preterm birth and SGA were presented in a table (Supplementary File 3). We also summarised and presented the risk factors associated with adverse birth outcomes from the included studies. We presented our findings following the preferred reporting items for scoping review and meta-analysis (PRISMA-ScR,40 Supplementary File 4).
Health professionals’ consultation
The consultation stage was conducted via one-on-one face to face or telephone interviews. Consultants were required to be health professionals (nurses, midwives, and obstetricians) from Pacific Island countries working in antenatal care, births, and neonatal units. Recruitment was purposeful and incorporated snowball sampling, with 18 consultants originally recruited from hospitals and health clinics. The interview schedule was informed by the literature review preliminary findings and the research team, experienced in qualitative research and the topic area. The interview questions asked about risk factors, adverse birth outcomes and recommendations to improve birth outcomes in Pacific Island countries.
After informed consent was obtained, interviews were conducted in English, Solomon Island Pidgin English, PNG Tok Pisin or Vanuatu Bislama, as the principal investigator was fluent in all languages and Creoles. Collected data were both quantitative (counts of nominated risk factors and adverse outcomes) and qualitative data (health professionals’ perspectives on issues). Recorded data were translated from the Creoles to English. NVIVO version 20 was used to manage the interview data and undertake the content and thematic analysis, which involved data familiarisation, formulation of codes, and development of themes.41,42 Content and thematic analysis were deemed appropriate for this study43 as this approach enabled the identification and quantifying of nominated adverse birth outcomes and risk factors and supported the generations of themes. Narrative summaries and quotes were used to illuminate the meaning of the themes.41,42 Demographic data (age, qualification, profession, country) were collected. Ethical approval was obtained from Curtin University.
Ethics approval
The part of the study which involved consultation of clinicians was approved by Curtin University human research committee with approval number: HRE2020-0530.
Role of the funding source
Funding sources was not involved in the study design; collection, analysis or interpretation of the data; and in writing of the manuscript or in the decision to submit the manuscript for publication.
Results
Selection process and characteristics of studies
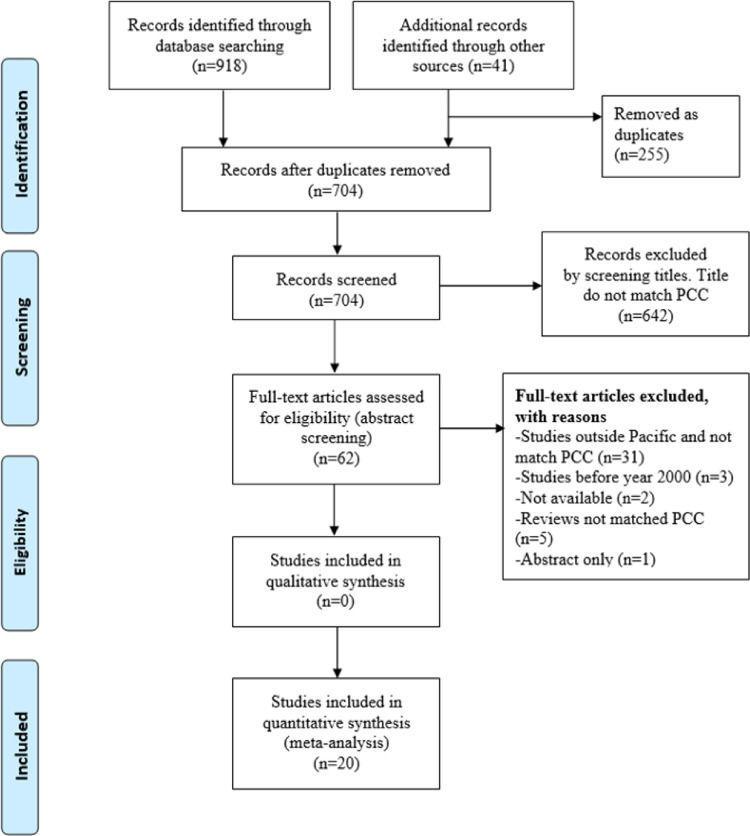
A total of 959 records were identified in the initial search of which 918 were retrieved from scholarly databases and 41 from additional website searches. After excluding 255 duplicates, 704 remained for titles and abstract screening, of which 62 was retrieved for full-text screening. Next, we excluded studies that did not meet the PCC criteria (n = 36), those conducted before 2000 (n = 3), not able to be accessed (n = 2) and abstract articles (n = 1). After all exclusions, 20 studies remained for the final review (Figure 1 illustrates the selection process using PRISMA flow diagram).
Figure 1.
PRISMA flow diagram
From: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. doi:10.1371/journal.pmed1000097.
We identified 20 studies, 11 peer-reviewed articles44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54 and nine demographic health survey reports20,21,55, 56, 57, 58, 59, 60, 61 conducted in 11 countries in the Pacific Island region, with a total population of 38,148 singleton births. Of the reported studies, seven were cohort studies,44,46,47,49,52, 53, 54 and 11 were cross sectional studies,20,21,45,51,55, 56, 57, 58, 59, 60, 61one case control study50 and one randomised clinical trial.48 Nine of the studies were conducted in PNG,21,47, 48, 49, 50, 51, 52, 53, 54 and others were conducted in other sub-regions: CNMI (n = 1),46 Kiribati (n = 1),60 Marshall Islands (n = 1),58 Nauru (n = 1),55 Palau (n = 1),44 Samoa (n = 1),56 Solomon Islands (n = 2),45,61 Tonga (n = 1),20 Tuvalu (n = 1),57 and Vanuatu (n = 1)59 (Table 1).
Table 1.
Summary of studies included in the review.
|
(i) Eleven journal articles | |||||||
|---|---|---|---|---|---|---|---|
| Author(s) | Year | Study context | Study aims | Study design | Population (Mother and infants, Births) | Adverse birth outcomes | Risk factors investigated |
| Journal | |||||||
| Unger et al.54 | 2019 | PNG Madang Province | To evaluates the associations between malaria infection and hemoglobin in PNG women. | Prospective cohort study | 1976 | LBW, preterm birth, small for gestational age (SGA) | Plasmodium Falciparum malaria infection. (microscopic submicroscopic) and plasmodium vivax malaria infection |
| Cruz et al.46 | 2018 | CNMI | To explore the racial/ethnic disparities that exist among Pacific Islander women residing in the CNMI and newborns. | Retrospective cohort study | 8918 | preterm birth, LBW | Race of CNMI, Filipino, Chinese, other Pacific Islander, maternal age and number of antenatal number of visits |
| Fowkes et al.47 | 2018 | PNG Madang Province | To determine the association between iron deficiency and birth outcomes, and malaria | Longitudinal cohort study | 279 | preterm birth, LBW | Iron deficiency anaemia, iron deficiency (Hb < 11 g/dL), moderate anemia, severe anaemia (Hb < 7 g/dL*), plasmodium falciparum malaria (peripheral blood) |
| Lufele et al.48 | 2017 | PNG Madang Province | To investigate the prevalence of Plasmodium malaria its risk factors, maternal anaemia and birth outcomes associated with women receiving at least one dose of Intermittent preventive treatment in pregnancy (IPTp). | Randomised clinical trial | 1451 | LBW, preterm birth | Plasmodium malaria infection, active placenta malaria, acute malaria infection, chronic malaria infection, past plasmodium malaria infection and anaemia |
| Berger et al.44 | 2015 | Palau | To determine the effects of betel nut with tobacco use on pre-pregnancy obesity and adverse birth outcomes. | Retrospective cohort | 1,171 | preterm birth, LBW, Preterm LBW, Term LBW, Preterm normal weight | Betel nut chewing, tobacco use, combined use of tobacco and betel nut, and obesity in pregnancy-Body Mass Index (BMI) >30) |
| Cafaro et al.45 | 2015 | Kirakira Solomon Islands Solomon Islands | To calculate the incidence of LBW and prematurity and proportion of women receiving antenatal care. | Retrospective audit and cross-sectional study | 1295 | LBW, preterm birth | Betel nut use, tobacco use and urinary tract infection in pregnancy |
| Ome-Kaius et al.49 | 2015 | PNG Madang Province | To access the effects of areca nut chewing on pregnancy outcomes, birth weight, anaemia in a large cohort of pregnant women. | Longitudinal cohort | 1769 | LBW, Stillbirth, preterm birth | Betel nut, smoking, alcohol use, low mid upper arm circumference (MUAC), maternal height, malaria prophylaxis, primigravida and fewer antenatal visits |
| Stanisic et al.52 | 2015 | PNG | |||||
| Madang | |||||||
| Province | To identify risk factors for LBW, anaemia, and preterm in pregnant women of PNG. | Prospective cohort study | 328 | LBW, preterm birth | Malaria infection, parasitemia, severe anaemia, multigravida, tobacco smoke, education and MUAC | ||
| Unger et al.53 | 2015 | PNG Madang Province | To evaluate factors with FGR among pregnant woman enrolled in randomised control trial evaluating IPTp malaria prophylaxis in pregnancy. | Cohort study with clinical trial | 671 | LBW, SGA, preterm birth low weight gain | Low MAUC (<22 cm), short stature (<150 cm), low BMI, anaemia (<90 g/l)⁎⁎, malaria infections, plasmodium falciparum malaria, plasmodium vivax malaria (peripheral or Sub-microscopic infections) |
| Senn et al.51 | 2009 | PNG Madang Province | To investigates the habits of betel nut chewing and possible impact on pregnancy. | Cross-sectional study | 310 | Reduced mean birth weight | Primigravity, betel nut, smoke, alcohol, and low BMI |
| Peters et al.50 | 2001 | PNG | To identify risk factors associated with LBW in the Western highland Province of PNG. | Prospective case-control | 299 | LBW | Maternal age, birth interval, no antenatal bookings, low antenatal attendance, fever during Pregnancy, pre-eclampsia, antepartum haemorrhage, maternal smoking, short stature, Low BMI, low haemoglobin, low education |
| (ii)Nine grey literatures | |||||||
| National Statistics Office PNG21 | 2019 | PNG | To provide information indicators of fertility, fertility preferences, family planning practices, childhood mortality, maternal and child health, knowledge, and awareness of human immunodeficiency virus- acquired immunodeficiency syndrome (HIV/AIDS), domestic violence, and other related health issues. | Demographic health survey | 4672 | LBW, Smaller than average babies | Not applicable⁎⁎⁎ |
| National Statistic Office SI61 | 2015 | Solomon Islands | To provide current and reliable data on fertility and family planning behavior, child mortality, adult and maternal mortality, children's nutritional status, the use of maternal and child healthcare services, knowledge of HIV and AIDS, and other health-related issues. | Demographic health survey | 3535 | LBW, Smaller than average baby, very small baby | Not applicable |
| Bureau of Statistics56 | 2014 | Samoa | To provide information for policymakers, planners, researchers, and program managers, for use in planning, implementing, monitoring, and evaluating population and health programs within the country. | Demographic health survey | 3192 | LBW, Smaller than average baby, very small baby | Not applicable |
| Ministry of Health VNSO59 | 2013 | Vanuatu | To furnish policymakers and planners with detailed information on fertility, family planning, infant and child mortality, maternal and child health and nutrition, and knowledge of HIV and AIDS and other sexually transmitted infections. | Demographic health survey | 1562 | LBW | Not applicable |
| Ministry of Health TDoS20 | 2012 | Tonga | To ensure better understanding and use of these data and widely dissemination of results at different planning levels. | Demographic health survey | 1703 | LBW, Smaller than average baby, very small baby | Not applicable |
| National Statistic Office KaSotPC60 | 2009 | Kiribati | To provide information for policymakers, planners, researchers, and program managers, for use in planning, implementing, monitoring, and evaluating population and health programs in the country. | Demographic health survey | 1099 | LBW, very small baby | Not applicable |
| Bureau of Statistics NatSotPC55 | 2007 | Nauru | To provide information for policymakers, planners, researchers, and program managers, for use in planning, implementing, monitoring, and evaluating population and health programs in the country. | Demographic health survey | 322 | LBW, very small baby | Not applicable |
| Central Statistics Division57 | 2007 | Tuvalu | To provide information for policymakers, planners, researchers, and program managers, for use in planning, implementing, monitoring, and evaluating population and health programs in the country. | Demographic health survey | 447 | LBW, Smaller than average baby, very small baby | Not applicable |
| Economic Policy58 | 2007 | Marshall Islands | To provide information for policymakers, planners, researchers, and program managers for use planning, implementation, monitoring and evaluation of population and health programs in the country. | Demographic health survey | 1173 | LBW, Smaller than average baby, very small baby | Not applicable |
Notes:
grams per decilitre.
grams per litre.
Not applicable; these surveys did not present measure of associations between the independent and dependent variables.
Prevalence of adverse birth outcomes
Prevalence of the various adverse birth outcomes was reported for 11 countries in the region (Supplementary File 3). Nineteen studies20,21,44, 45, 46, 47, 48, 49, 50,52, 53, 54, 55, 56, 57, 58, 59, 60, 61 representing 11 countries reported the prevalence of LBW which ranged from 3% in CNMI46 to 27% in Nauru with a mean of 12%.55 The Polynesian and Micronesian countries such as CNMI,46 Palau,44 Samoa,56 Tonga20 and Tuvalu57 reported LBW prevalence of less than 10%. Six studies44, 45, 46, 47,52,54 reported the prevalence of preterm births which ranged from 7% in CNMI46 to 24% in the Solomon Islands with estimated mean of 13%.45 The Palau study reported a prevalence for preterm LBW of 5%, term LBW of 4% and a prevalence for preterm normal weight of 4%.44
Risk factors for adverse birth outcomes
Low birth weight
Six studies, five from PNG48,50, 51, 52,54 and one from Palau,44 reported the risk factors for LBW. LBW was associated with malaria infection in pregnancy.48,52,54 These studies investigated acute and chronic, and microscopic and sub-microscopic malaria infections, which were all associated with an increased risk of LBW.48,52,54 Southeast Asian ovalocytosis infection in pregnancy was associated with LBW,52 as was betel nut and tobacco use in pregnancy.44,50 Low maternal mid-upper arm circumference (<23 cm) and short stature (<150 cm)49 were also associated with LBW. Young and advanced maternal ages (< 22 years and > 35 years)50 were associated with LBW. Other risk factors associated with LBW were birth intervals less than 2 years, no antenatal booking, fever during pregnancy,50 and female infant and primigravida (Supplementary file 5).49
Preterm birth
Six studies reported risk factors for preterm births from PNG,47,49,52,54 CNMI,46 and Palau.44
Three studies reported that malaria infections during pregnancy were associated with preterm birth.48,52,54 Two of the studies showed that acute and chronic placental malaria were associated with preterm birth, with chronic infection showing a stronger association.48,52 Microscopic malaria infections were also associated with preterm birth.54 Three studies reported preterm birth were associated with demographic, health risk factors such as maternal obesity,44 maternal age (age <20 years and ≥ than 35 years) and insufficient antenatal care (1–8 visits) in the CNMIs.46 Pacific Islands, Filipino women and CNMI women living in CNMI were associated with higher risk of preterm birth than women in CNMI of Chinese descent (Supplementary file 6).46
Small for gestational age
Only one study showed the risk factors associated with SGA. This study reported that low maternal haemoglobin level (Hb<9 mg/L) during pregnancy, maternal upper arm circumference (<22 cm), short maternal stature (<150 cm) and primigravida were associated with SGA (Supplementary File 7).53
Changes in mean birth weight
Six studies47, 48, 49,51, 52, 53 reported associations with mean birth weight. Acute placental malaria during pregnancy was associated with reductions in mean birth weight.48 Primigravity and tobacco smoking during pregnancy were also reported as factors that were associated with reductions in mean birth weight (Supplementary File 8).52
Stillbirth and miscarriage
Only one study investigated associations with stillbirth and miscarriage.49 In this study, there was marginal evidence for an association between heavy betel nut use and stillbirth and miscarriage (Supplementary file 7).49
Health professionals
Demographic profile
We interviewed 18 health professionals from the Pacific Island countries of the Solomon Islands (n = 11), PNG (n = 3), Fiji (n = 2) and Vanuatu (n = 2). They were midwives (n = 7), neonatal care nurses (n = 5), obstetricians (n = 3), registered nurses (n = 2), and a paediatrician (n = 1) practising in major tertiary hospitals (n = 15) and rural community practice (n = 3). Eleven health professionals had qualifications equivalent to a master's degree, post-graduate or above, while seven had an undergraduate degree or diploma. The health professional mean age was 42 years, and their average work experience was 17 years. The data provided by the health professionals were quantified and categorised and presented under the following themes: (a) adverse birth outcomes and risk factors; (b) mitigating risk factors during pre-pregnancy; and (c) mitigating risk factors during pregnancy.
Adverse birth outcomes and risk factors. The most frequent adverse birth outcomes reported by the health professionals were preterm birth (n = 14), followed by LBW (n = 12) and small for gestational age (n = 11). The most frequently nominated risk factors for adverse birth outcomes were physical and emotional stress (n = 13), teenage pregnancy (n = 11) malaria (n = 11), and poverty (n =11) (Supplementary file 9).
Mitigating of risk factors during pre-pregnancy
Most health professionals (n = 13) reported the risk of adverse birth outcomes could be reduced during pre-pregnancy. They believed that actions to reduce the risk of adverse birth outcomes could be developing pre-pregnancy health care policy, providing holistic health care, effective health education for women and girls, and incorporating sexual and reproductive health into the school curriculum. Health education orientated to informing women of the importance of, family planning, antenatal care, good nutrition, substance use avoidance, and raising awareness on sexually transmitted infections (STIs) would be beneficial.
“Educate young women and girls on good care before pregnancy… collaborate and implement program on sexual and reproductive health on safe sex practice… establish community participation with churches and social organisations” (Midwife, PNG).
“Health education is essential for mothers before pregnancy, on good nutrition, danger signs, early antenatal care, personal hygiene, prophylaxis and delivery at the health facilities” (Midwife, Vanuatu)
Health professionals also suggested that the current health system should focus on health promotion. This was reflected when a midwife from Solomon Islands said:
“The health system should also focus on public health and care for women during pre-pregnancy… pre-pregnancy health care is the public health profession's role and should be integrated with clinical care” (Midwife, Solomon Islands)
“We should have a special clinic for women to seek advice if they [women] planning to get pregnant” (Neonatal care nurse, Solomon Islands)
Mitigating risk factors during pregnancy
Health providers reflected on how risk factors leading to adverse birth outcomes could be mitigated at the time of pregnancy. Most health professionals (n = 13) called for comprehensive and ethical antenatal care involving health assessments, physical examinations, provisions of screening for STIs and malaria and provision of malaria prophylaxis and drug supplements (e.g., iron tablets and folic acid).
“We must monitor vital signs such as blood pressure, fetal heart rate, glucose, and protein to detect any underlying health condition… we monitor mothers’ weight, no weight gain would mean growth restriction [to the fetus], if the weight increases abnormally, it could mean gestational diabetes” (Midwife, Vanuatu)
“Screen all antenatal mothers for syphilis, malaria and anaemia and treat them early” (Midwife, Solomon Islands)
“….provide malaria prophylaxis, ferrous sulphate with folic acid, albendazole and tetanus vaccine to prevent illness during pregnancy (neonatal nurse, Solomon Island)
Health professionals also suggested the need to improve antenatal health services in rural areas, improve health professionals’ practices, and the need for the provision of health education during antenatal care in local dialects as a means of reducing exposure to risk factors and adverse birth outcomes.
“….problems with birth outcomes occur mostly in rural area… therefore the government should focus on rural health” (Midwife, PNG)
“Trained midwives should see the pregnant woman not as a task but as a whole person” (Midwife, Solomon Islands)
“Use brochures, posters, and pamphlets in local dialects… where lacking in staff, use of pre-recorded speech and videos in antenatal education” (Neonatal care nurse, Vanuatu).
Discussion
Summary of findings from this scoping review
To our knowledge, this scoping review is the first to examine the available evidence on the burden of adverse birth outcomes and their risk factors in the Pacific Island region. Our review of 22 countries and territories located in the region found a dearth of published peer reviewed studies (n = 11) and grey literature (n = 9) that met our inclusion criteria. Studies that did not follow standard reporting guidelines were excluded. Nonetheless, the included studies were informative in (i) identifying the adverse birth outcomes most and least well-studied; (ii) providing an indication of the expected burden of adverse birth outcomes; and (iii) identifying the range of risk factors that have been investigated in the Pacific Island region. In summary, we identified that (i) LBW and preterm birth were the most well-studied outcomes but there were relatively few studies conducted on mortality endpoints; (ii) the prevalence of the adverse birth outcomes varied considerably both within and between regions, and very high for some locations such as the Solomon Islands; and that (iii) although health, obstetric, social and behavioural risk factors have been investigated, several, such as betel nut chewing, are relatively unique to the region and require further investigation. Outside PNG few studies have been conducted.
Prevalence of adverse birth outcomes in the Pacific Island region
There are several plausible explanations for the wide range for prevalence of LBW. Firstly, relatively lower prevalence of LBW and preterm birth in the Polynesia and Micronesia may reflect better maternal health, higher antenatal coverage and greater likelihood of presence of a skilled birth attendant.18, 19, 20 The estimated mean LBW prevalence (12%) in the Pacific island countries is comparable to those11 from LMICs of Africa and Asia.62 The mean estimated prevalence for preterm birth was 13% is comparable to WHO estimates of 14% for Pacific region,63 which is also similar to estimated prevalence for preterm birth (10–15%) in LMIC by WHO.63 The true prevalence of preterm birth and LBW were hampered by lack of routine accurate records of pregnancy dates, underreporting of stillbirths, lack of availability of measurement instruments and small sample sizes. These two adverse birth outcomes were both the most investigated and identified by the health professionals as those most frequently occurring of concern in the region.
Risk factors for adverse birth outcomes in the Pacific Island region
Malaria
Malaria infections reported in PNG showed significant associations with LBW, preterm births, and changes in mean birth weights.48,52,54 Malaria infection was also reported as a major cause of preterm birth, LBW, miscarriage, and stillbirth by the consulted health professionals. Malaria is endemic in all coastal areas of the three Melanesian countries of PNG, Solomon Islands and Vanuatu64, 65, 66, 67 with PNG as the epicentre of malaria infection in the Western Pacific region.65,68 Malaria is also endemic in Vanuatu but infection fluctuates across the different seasons,59 while most countries of Polynesia and Micronesia have been declared as malaria-free by WHO.69 Successful provision of malaria prophylaxis to pregnant women in the region has been a challenge due to drug shortages and poor access to woman in isolated rural areas.65,68 We conclude that malaria is a risk factor in pregnancy and adverse birth outcomes in the malaria-endemic areas of the Pacific Island region, although the magnitude of the association remains unclear.
Anaemia and worm infestation
Health professionals interviewed nominated anaemia and worm infestation to be associated with the adverse birth outcomes of which both conditions were prevalent in the region.47,70 Oral iron supplements and albendazole stat doses during pregnancy are part of the antenatal care protocol in most Pacific Island countries.47 However, accessing these medications can be challenging due to consistent drug shortages, poor access to women in rural and isolated areas, and low antenatal care attendance resulting in a significant portion of pregnant women not taking these medications.22 The health professionals called for improved antenatal care and health education on prophylaxis and supplements during pre-pregnancy and pregnancy, at all levels, including public health and social organisations, and churches as an innovative mitigation strategy.
Substance use
Betel nut and tobacco use in PNG and Palau were associated with LBW,50,44 birth weight reduction,52 stillbirth and miscarriage.49 Studies from Southeast Asia have also reported betel nut chewing during pregnancy as having an impact on birth weight, fetal length and preterm birth.15,29,68 The magnitude of the effects of betel nut chewing on birth outcomes remains unclear. Reductions in birth weight from betel nut use appear to be at least as large as those reported for smoking during pregnancy. The health professionals that we consulted also perceived betel nut, tobacco and kava use as having a negative impact on pregnancy and birth outcomes. Although the impact of kava use has been rarely studied in the peer-reviewed literature, health professionals reported its detrimental effects on pregnancy outcomes. Given the increase in kava use in the region,31 there is a need for future investigation on its impact on births and pregnancies.
Maternal obesity and obesity-related conditions
A study in Palau reported maternal obesity to be positively associated with preterm birth.44 This finding was also supported by the interviewed health professionals who reported obesity-related diseases such as: type 2 diabetes, gestational diabetes, hypertension, and pregnancy-induced hypertension as risk factors for adverse birth outcomes. The health professionals also reported pre-eclampsia, a hypertensive disorder of pregnancy,71 as a notable cause of LBW and preterm birth. We conclude that obesity, which occurs among 36% of women in the Pacific Island region,14,18 is likely to have a role in maternal health during pregnancy, whether or not it is a direct cause of adverse birth outcomes in the region.72
Poor antenatal care and access
Our literature review found no antenatal bookings and lower number of antenatal visits was associated with LBW50 and preterm birth.46 This was also reflected in the health professionals concerns about poor presentation for antenatal care, influenced by poor access to health facilities and health seeking behaviours. Health professionals were concerned that shortage of staff and lack of health facilities especially in rural areas have contributed to lack of quality in antenatal care. Our findings were also validated by recent studies in the region which showed poor quality maternal care in the region leads to poor outcomes in newborns.22,73
Quality of reporting and number of studies in the Pacific Island region
Our review found a dearth of studies for all countries, for all risk factors and for all birth outcomes that have been investigated to date in the Pacific Islands region. Of the all 20 studies representing the 11 Pacific Island countries (CNMI, Kiribati, Marshall Islands, Nauru, Palau, PNG, Samoa, Solomon Islands, Tonga, Tuvalu, Vanuatu), the measure of association for risk factors and adverse birth outcomes were reported in ten studies, which came from only three countries (PNG, Palau, and CNMI).44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54 Also, the association of risk factors and adverse birth outcomes was reported by nine population-based cohort studies,44,46,47,49, 50, 51, 52, 53, 54 and a randomised control trial48 of which four had small study populations.47,50, 51, 52 Two DHS reports from Nauru55 and Tuvalu57 also used small samples to produce prevalence estimates. Many studies did not report measures of uncertainty (confidence intervals or variance), control for confounding or attempt to identify potential sources of bias. This assessment stems from limited research capacity in the region,29,74 and limited resources for health administration.16 Consultation with health professionals was essential, assisting in illuminating the findings from the literature, contributing additional insights and recommendations to reduce exposure to risk factors and adverse birth outcomes in the Pacific region.
Limitations of this scoping review
We could not access health reports and grey literature that were only published in hardcopy. It is plausible that many health systems in the region do not disseminate health information online. We were also unable to obtain the views of health professionals from the Polynesian and Micronesian regions
Conclusion
Despite the limited studies, the review identified a range of risk factors and adverse birth outcomes relevant to the Pacific Island region. The prevalence of adverse birth outcomes is not well-ascertained for countries within the region, although LBW and preterm birth were relatively more frequently investigated. There were a range of risk factors for adverse birth outcomes - such as, malaria, substance use, obesity and poor antenatal care – that are either relatively prevalent or somewhat unique to the Pacific Islands region. These risk factors have not been comprehensively investigated in the region and were confirmed by health professionals as risk factors of concern.
Contributors
LSKK, GP, GT and JJ conceived and conceptualised study design. LSKK conducted searches and initial study selection. LSKK, GP, GT and JJ did the final study selection. LSKK conducted study analysis under guidance of GP and GT. LSKK and JJ designed stakeholder consultation study, LSKK conduct interviews and data analysis. LSKK wrote first draft and reviewed by GP, GAT and JJ. HB and GD read and approved the final paper.
Supplemental Material: Supplemental material for this article is available online.
Funding
GP was supported with funding from the National Health and Medical Research Council Project and Investigator Grants #1099655 and #1173991, institutional funding for the WA Health and Artificial Intelligence Consortium, and the Research Council of Norway through its Centres of Excellence funding scheme #262700. GAT was supported with funding from the National Health and Medical Research Council Investigator Grant #1195716. LSSK is recipient of scholarship from the Department of Foreign Affairs, Australia Award.
Declaration of interests
The authors declared no potential conflicts of interest.
Acknowledgment
We want to acknowledge all 18 health professionals from Fiji, PNG, Solomon Islands and Vanuatu to participate in the study. We also acknowledge the Nurse instructor (JT) of the Paediatrics and Neonatal care of the National Referral Hospital in the Solomon Islands to conduct one on one interviews.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100402.
Appendix. Supplementary materials
References
- 1.Blumenshine P., Egerter S., Barclay C.J., Cubbin C., Braveman P.A. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39(3):263–272. doi: 10.1016/j.amepre.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 2.Gedefaw G., Alemnew B., Demis A. Adverse fetal outcomes and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Pediatr. 2020;20:1–12. doi: 10.1186/s12887-020-02176-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Campbell E.E., Seabrook J.A. The influence of socioeconomic status on adverse birth outcomes. Can J Midwifery Res Pract. 2016;15(2):11–20. [Google Scholar]
- 4.Degno S., Lencha B., Aman R., et al. Adverse birth outcomes and associated factors among mothers who delivered in Bale zone hospitals, Oromia Region, Southeast Ethiopia. J Int Med Res. 2021;49 doi: 10.1177/03000605211013209. 030006052110132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vogel J.P., Chawanpaiboon S., Moller A.B., Watananirun K., Bonet M., Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:3–12. doi: 10.1016/j.bpobgyn.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Sayers S.M., Lancaster P.A.L., Whitehead C.L. In: International Encyclopedia of Public Health. 2nd ed. Quah S.R., editor. Academic Press; Oxford: 2017. Fetal growth restriction: causes and outcomes; pp. 132–142. [Google Scholar]
- 7.Tsegaye B., Kassa A. Prevalence of adverse birth outcome and associated factors among women who delivered in Hawassa town governmental health institutions, south Ethiopia, in 2017. Reprod Health. 2018;15(1):193. doi: 10.1186/s12978-018-0631-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kandasamy Y., Tanchi P.P.D., Edmonds L.K. Small for gestational age and low birth weight term admissions to a tertiary perinatal centre in Northern Queensland, Australia. J Immigr Minor Health. 2015;17(1):227–231. doi: 10.1007/s10903-013-9891-8. [DOI] [PubMed] [Google Scholar]
- 9.Ohmi HK, Hirooka A, Hata Y, Mochizuki. Low birth weight OECD health at a glance 2017. 2016 2017. http://www.oecd.org/els/health-systems/health-data.htm30.
- 10.Wang H., Bhutta Z.A., Coates M.M., et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet N Am Ed. 2016;388(10053):1725–1774. doi: 10.1016/S0140-6736(16)31575-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blencowe H., Krasevec J., de Onis M., et al. National, regional, and worldwide estimates of low birthweight in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2019;7(7):e849–ee60. doi: 10.1016/S2214-109X(18)30565-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blencowe H., Cousens S., Jassir F.B., et al. National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health. 2016;4(2):e98–e108. doi: 10.1016/S2214-109X(15)00275-2. [DOI] [PubMed] [Google Scholar]
- 13.Magnusson R.S., Patterson D. How can we strengthen governance of non-communicable diseases in Pacific Island countries and territories? Asia Pac Policy Stud. 2015;2(2):293–309. [Google Scholar]
- 14.Horwood P.F., Tarantola A., Goarant C., et al. Health challenges of the pacific region: insights from history, geography, social determinants, genetics, and the microbiome. Front Immunol. 2019;10(2184) doi: 10.3389/fimmu.2019.02184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.World Health Organization . World Health Organization; 2013. Country Coping Stratergy at a Glance, Pacific Island Countries World Health Organization. [Google Scholar]
- 16.Linhart C, Karen C, Renee S, Gerald H, Richard T. Trends in neonatal and infant mortality for Pacific Island states. Secretariat of the pacific community cataloguing-in-publication data, 2015.
- 17.Christine L., Karen C., Renee S., Gerald H., Richard T. Noumea Secretariat of the Pacific Community; Noumea: 2015. Trends in Neonatal and Infant Mortality for Pacific Island States. [Google Scholar]
- 18.WHO Western Pacific . WHO Western Pacific Region; 2011. Western Pacific Country Health Information Profile 2011 revision. 1211 Geneva 27. [Google Scholar]
- 19.Bureau of Statistics S. Samoa demographic and health survey 2014 by census-surveys and demography division. Samoa Bureau of Statistics Apia, Samoa: Samoa demographic and health survey 2014 /Census-Surveys and Demography Division. - Apia, Samoa: Samoa Bureau of Statistics, Government of Samoa, 2014, 2014
- 20.Ministry of Health TDoS, The Secretariat of the Pacific Community, and United Nations Population Fund. Tonga Demographic and Health Survey 2012. Secretariat of the Pacific Community Noumea, New Caledonia: Secretariat of the Pacific Community, 2012
- 21.National Statistics Office PNG. Papua Nue Guinea demographic Health Survey 2016-2018 the DHS program ICF Rockville, Maryland, USA: national statistical office Port Moresby, Papua New Guinea, 2018
- 22.Wilson A.N., Spotswood N., Hayman G.S., et al. Improving the quality of maternal and newborn care in the Pacific region: a scoping review. Lancet Reg Health West Pac. 2020;3 doi: 10.1016/j.lanwpc.2020.100028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gani A. Some aspects of communicable and non-communicable diseases in Pacific Island countries. Soc Indic Res. 2009;91(2):171–187. [Google Scholar]
- 24.Charlton K.E., Russell J., Gorman E., et al. Fish, food security and health in Pacific Island countries and territories: a systematic literature review. BMC Public Health. 2016;16(1):285. doi: 10.1186/s12889-016-2953-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Barnett J. Dangerous climate change in the Pacific Islands: food production and food security. Reg Environ Chang. 2011;11(1):229–237. [Google Scholar]
- 26.Kumar L., Jayasinghe S., Gopalakrishnan T., Nunn PD. In: Climate Change and Impacts in the Pacific. Kumar L., editor. Springer International Publishing; Cham: 2020. Climate change and the Pacific Islands; pp. 1–31. [Google Scholar]
- 27.Smith J., Lloyd T., Bobogare A., et al. Malaria early warning tool: linking inter-annual climate and malaria variability in northern Guadalcanal, Solomon Islands. Malar J. 2017;16:1. doi: 10.1186/s12936-017-2120-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan C.W., Iata H., Yaviong J., et al. Surveillance for malaria outbreak on malaria-eliminating islands in Tafea Province, Vanuatu after Tropical Cyclone Pam in 2015. Epidemiol Infect. 2017;145(1):41–45. doi: 10.1017/S0950268816002041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.De Silva M., Panisi L., Brownfoot F.C., et al. Systematic review of areca (betel nut) use and adverse pregnancy outcomes. Int J Gynaecol Obstet. 2019;147(3):292–300. doi: 10.1002/ijgo.12971. [DOI] [PubMed] [Google Scholar]
- 30.Hossain M.F., Anwar M., Akhtar S., Numan S.M. Adverse effects on health posed by consumption of Areca nut (Areca catechu L., family: Palmaceae) Int J Commun Med Public Health. 2015;2(4):357–360. [Google Scholar]
- 31.Community SotP. Fiji Kava quality manual Suva secretariate of the Pacific community?
- 32.Shimoda L.M.N., Park C., Stokes A.J., Gomes H.H., Turner H. Pacific Island 'Awa (Kava) extracts, but not isolated kavalactones, promote proinflammatory responses in model mast cells. Phytother Res. 2012;26(12):1934–1941. doi: 10.1002/ptr.4652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Institute JB. Collaborating entity the western Australian group for evidence informed healthcare practice: a JBI centre of excellence. 2020. https://jbi.global/node/2258.
- 34.Kaforau L.S.K., Tessema G.A., Jancey J., Dhamrait G.K., Bugoro H., Pereira G.F. Prevalence and risk factors of adverse birth outcomes in the Pacific Island region: a scoping review protocol. BMJ Open. 2021;11(4) doi: 10.1016/j.lanwpc.2022.100402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Aromataris E., Munn Z. Joana Briggs Institute: Joana Briggs Institute; 2020. JBI Reviewer's Manual; p. 488. [Google Scholar]
- 36.Arksey H., O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32. [Google Scholar]
- 37.Andrew N.L., Bright P., de la Rua L., Teoh S.J., Vickers M. Coastal proximity of populations in 22 Pacific Island Countries and territories. PLoS One. 2019;14(9) doi: 10.1371/journal.pone.0223249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levac D., Colquhoun H., O'Brien K.K. Scoping studies: advancing the methodology. Implement Sci. 2010;5(1):69. doi: 10.1186/1748-5908-5-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peters M., Godfrey C., Khalil H., Mcinerney P., Soares C., Parker D. 2017 Guidance for the conduct of JBI scoping reviews. Joana Briggs Inst Rev Man. 2017;13:141–146. [Google Scholar]
- 40.Tricco A.C., Lillie E., Zarin W., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 41.Erlingsson C., Brysiewicz P. A hands-on guide to doing content analysis. Afr J Emerg Med. 2017;7(3):93–99. doi: 10.1016/j.afjem.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Liamputtong P. Making sense of qualitative data: analysis process qualitative research method 2013 pp 241–63.
- 43.White M., Marsh E. Content analysis: a flexible methodology. Libr Trends. 2006;55 [Google Scholar]
- 44.Berger K.E., Masterson J., Mascardo J., et al. The effects of chewing betel nut with tobacco and pre-pregnancy obesity on adverse birth outcomes among Palauan women. Matern Child Health J. 2016;20(8):1696–1703. doi: 10.1007/s10995-016-1972-6. [DOI] [PubMed] [Google Scholar]
- 45.Cafaro J., Randle E., Wyche P., Higgins M., Fink J., Jones PD. An assessment of current antenatal care practices and identification of modifiable risk factors for prematurity and low birth weight infants in pregnancy in Solomon Islands. Int J Rural Remote Health Res Educ Pract Policy. 2015 [PubMed] [Google Scholar]
- 46.Cruz R.D., Grant J., Heck J.E., Cash H.L. Disparities in adverse perinatal outcomes among Pacific Islanders in the commonwealth of the Northern Mariana Islands. Prev Chronic Dis. 2018;15(3) doi: 10.5888/pcd15.170385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fowkes F.J.I., Davidson E., Agius P.A., Beeson J.G. Understanding the interactions between iron supplementation, infectious disease and adverse birth outcomes is essential to guide public health recommendations. BMC Med. 2019;17(1):153. doi: 10.1186/s12916-019-1376-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lufele E., Umbers A., Ordi J., et al. Risk factors and pregnancy outcomes associated with placental malaria in a prospective cohort of Papua New Guinean women. Malar J. 2017;16(1):427. doi: 10.1186/s12936-017-2077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ome-Kaius M., Unger H.W., Singirok D., et al. Determining effects of areca (betel) nut chewing in a prospective cohort of pregnant women in Madang Province, Papua New Guinea. BMC Pregnancy Childbirth. 2015;15(1):177. doi: 10.1186/s12884-015-0615-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Peters H., Vince J., Friesen H. Low birthweight at a Papua New Guinea highlands hospital. J Trop Pediatr. 2001;47(1):17–23. doi: 10.1093/tropej/47.1.17. [DOI] [PubMed] [Google Scholar]
- 51.Senn M., Baiwog F., Winmai J., Mueller I., Rogerson S., Senn N. Betel nut chewing during pregnancy, Madang province, Papua New Guinea. Drug Alcohol Depend. 2009;105(1):126–131. doi: 10.1016/j.drugalcdep.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 52.Stanisic D.I., Moore K.A., Baiwog F., et al. Risk factors for malaria and adverse birth outcomes in a prospective cohort of pregnant women resident in a high malaria transmission area of Papua New Guinea. Trans R Soc Trop Med Hyg. 2015;109(5):313–324. doi: 10.1093/trstmh/trv019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Unger H.W., Ome-Kaius M., Karl S., et al. Factors associated with ultrasound-aided detection of suboptimal fetal growth in a malaria-endemic area in Papua New Guinea. BMC Pregnancy Childbirth. 2015;15(1):83. doi: 10.1186/s12884-015-0511-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Unger H.W., Rosanas-Urgell A., Robinson L.J., et al. Microscopic and submicroscopic Plasmodium falciparum infection, maternal anaemia and adverse pregnancy outcomes in Papua New Guinea: a cohort study. Malar J. 2019;18(1):302. doi: 10.1186/s12936-019-2931-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bureau of Statistics NatSotPC. Republic of Nauru Demographic and Health Survey 2007. Secretariat of the Pacific Community, Noumea, New Caledonia Secretariat of the Pacific Community, 2007
- 56.Bureau of Statistics S. Samoa Demographic and Health Survey 2014 by census-surveys and demography division. Samoa Bureau of Statistics Apia, Samoa: Samoa demographic and health survey 2014 /census-surveys and demography division. - Apia, Samoa: Samoa Bureau of Statistics, Government of Samoa, 2014, 2014
- 57.Central Statistics Division tSotPC, and Macro International Inc. Tuvalu Demographic and Health Survey 2007. Noumea, New Caledonia Secretariat of the Pacific Community Noumea, New Caledonia October 2009, 2007
- 58.Economic Policy PaSOM, Marshall Islands. Marshall Islands demographic and health survey 2007. Secretariat of the Pacific Community Noumea, New Caledonia, 2008: Secretariat of the Pacific Community, 2007
- 59.Ministry of Health VNSO, the Secretariat of the Pacific Community. Vanuatu Demographic and Health Survey 2013. Secretariat of the Pacific Community Noumea, New Caledonia November 2014: Secretariat of the Pacific Community Noumea, 2013
- 60.National Statistic Office KaSotPC. Kiribati Demographic and Health Survey 2009. Secretariat of the Pacific Community Noumea, New Caledonia December 2010: Secretariat of the Pacific Community, 2009
- 61.National Statistic Office SI, Seretariate of the Pacific community,. Solomon Islands Demographic and Health Survey 2015 /Solomon Islands National Statistics Office, Solomon Islands Ministry of Health and Medical Services and the Pacific Community. SPC's Noumea Headquarters B.P. D5, 98848 Noumea Cedex, New Caledonia, 2017: SPC's Noumea HeadquartersB.P. D5; 2017.
- 62.World Health Organisation . World Health Organisation; 2014. Global Nutrition Targets 2025 Low Birth Weight Policy Brief. [Google Scholar]
- 63.Howsen CP, Kinney MV, Lawn JE. The global action report on preterm, 2012.
- 64.Donald W., Pasay C., Guintran J.O., et al. The utility of malaria rapid diagnostic tests as a tool in enhanced surveillance for malaria elimination in Vanuatu. PLoS One. 2016;11(11) doi: 10.1371/journal.pone.0167136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hetzel MW, Saweri OPM, Kuadima JJ, et al. Papua New Guinea malaria indicator survey 2016-2017: malaria prevention, infection, and treatment. 2018
- 66.Wangdi K., Sarma H., Leaburi J., McBryde E., Clements A.C.A. Evaluation of the malaria reporting system supported by the district health information system 2 in Solomon Islands. Malar J. 2020;19(1):372. doi: 10.1186/s12936-020-03442-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Opeskin B. Malaria in Pacific populations: seen but not heard? J Popul Res. 2009;26(2):175–199. [Google Scholar]
- 68.World Health Organisation . Geneva World Health Organisation; 2020. World malaria report 2020: 20 years of global progress and challenges. [Google Scholar]
- 69.World Health Organisation. Countries and territories certified malaria-free by WHO. 2019. https://www.who.int/malaria/areas/elimination/malaria-free-countries/en/.
- 70.Bradbury R., Hii S., Harrington H., Speare R., Traub R. Ancylostoma ceylanicum Hookworm in the Solomon Islands. Emerg Infect Dis. 2017;23 doi: 10.3201/eid2302.160822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Uzan J., Carbonnel M., Piconne O., Asmar R., Ayoubi J. Pre-eclampsia: pathophysiology, diagnosis, and management. Vascular health and risk management. 2011;7:467–474. doi: 10.2147/VHRM.S20181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kessaram T., McKenzie J., Girin N., et al. Overweight, obesity, physical activity and sugar-sweetened beverage consumption in adolescents of Pacific islands: results from the global school-based student health survey and the youth risk behavior surveillance system. BMC Obesity. 2015;2(1):34. doi: 10.1186/s40608-015-0062-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tosif S., Nasi T., Gray A., Sadr-Azodi N., Ogaoga D., Duke T. Assessment of the quality of neonatal care in the Solomon Islands. J Paediatr Child Health. 2017;54 doi: 10.1111/jpc.13686. [DOI] [PubMed] [Google Scholar]
- 74.Redman-MacLaren M., MacLaren D., Asugeni R., et al. We can move forward": challenging historical inequity in public health research in Solomon Islands. Int J Equity Health. 2010;9:25. doi: 10.1186/1475-9276-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.