Summary
Background
In 2014, Indonesia launched a single payer national health insurance scheme with the aim of covering the entire population by 2024. The objective of this paper is to assess the equity with which contributions to the health financing system were distributed in Indonesia over 2015 – 2019.
Methods
This study is a secondary analysis of nationally representative data from the National Socioeconomic Survey of Indonesia (2015 – 2019). The relative progressivity of each health financing source and overall health financing was determined using a summary score, the Kakwani index.
Findings
Around a third of health financing was sourced from out-of-pocket (OOP) payments each year, with direct taxes, indirect taxes and social health insurance (SHI) each taking up 15 – 20%. Direct taxes and OOP payments were progressive sources of health financing, and indirect tax payments regressive, for all of 2015 – 2019. SHI contributions were regressive except in 2017 and 2018. The overall health financing system was progressive from 2015 to 2018, but this declined year by year and became mildly regressive in 2019.
Interpretation
The declining progressivity of the overall health financing system between 2015 – 2019 suggests that Indonesia still has a way to go in developing a fair and equitable health financing system that ensures the poor are financially protected.
Funding
This study is supported through the Health Systems Research Initiative in the UK, and is jointly funded by the Department of International Development, the Economic and Social Research Council, the Medical Research Council and the Wellcome Trust.
Research in context.
Evidence before this study
The only study to have assessed equity in health financing in Indonesia was published in 2008. This study was identified through Google Scholar and PubMed using search terms (Indonesia) AND (financing incidence OR financing incidence analysis OR progressiv* OR regressiv* OR proportio*) AND (health OR health care OR health system financ*). This study, now 13 years old, reported that the overall financing of health care in Indonesia was progressive in 2001, a time when social health insurance (SHI) in the country covered only formal sector employees and over half of the total health expenditure was sourced from out-of-pocket (OOP) payments. Due to limited data, only the four largest sources of health financing (i.e. direct taxes, indirect taxes, SHI and OOP payments) were included in the analysis. No study has assessed the changing health financing structure in Indonesia, after the launch of its National Health Insurance scheme (Jaminan Kesehatan Nasional, JKN) in 2014.
Added value of this study
To our knowledge, this is the first multi-year study to investigate the equity of health financing in Indonesia after implementation of the JKN. The 5-year (2015 – 2019) analysis provides vital information on how the burden of health funding has shifted among socio-economic groups in Indonesia. We assessed six separate health financing sources including direct taxes, indirect taxes, SHI, company health coverage (CHC), private health insurance (PHI) and OOP payments. Prior to this study, there was no evidence on the progressivity of CHC and PHI in Indonesia.
Implications of all the available evidence
As countries like Indonesia focus on reaching universal health coverage, increased attention must be paid to improving equity in health financing. While the observed progressivity of OOP payments is consistent with findings from the 2008 study, further research is needed to determine the extent to which this simply reflects the poor forgoing necessary health care. Monitoring unmet need for health care in the population is highly recommended.
Alt-text: Unlabelled box
Introduction
Moving towards Universal Health Coverage (UHC) requires a sustainable and equitable health financing system. Health financing should not only seek to raise sufficient funds and use them efficiently but do so in an equitable manner.1 There is a consensus among policymakers and health financing experts that payment for health care should be based on ability to pay (ATP) rather than utilization of health care.2,3 The relationship between health care payments and ATP, or progressivity of health financing, is a common measure of the performance of a health system in terms of equity and financial protection.4,5 In a progressive health system, the proportion of income contributed to financing health care increases with income. A regressive health system is considered to be inequitable, as people with lower income contribute a higher proportion of their income than those with higher income.6
Given the importance of equitable health financing in achieving the goal of UHC, it is critical that financing incidence is monitored frequently to ensure that the poor do not bear a disproportionate burden of financing the health system, and that progress is being made in reducing any excessive burden. Financing incidence analysis (FIA), sometimes referred to as progressivity analysis, is one of the tools for assessing the fairness of health financing systems. FIA assesses the distribution of the burden of financing the health system across socioeconomic groups relative to income.6
Health systems in low- and middle- income countries (LMICs) rely on many different sources of revenue for health financing, the most common ones being taxation (direct and indirect) and out-of-pocket (OOP) payments.7 Other major sources include social health insurance (SHI) contributions, private health insurance (PHI) premiums, community-based health insurance and donations. Several FIA studies have been conducted in LMICs and provide data on progress towards UHC and equity in health financing.8, 9, 10, 11, 12 In LMICs where compulsory SHI schemes are implemented, most have reported SHI as a progressive source of health financing.8
Indonesia is a middle-income country with the largest economy in Southeast Asia. It has a population of over 270 million, making it the world's fourth most populous nation. The overall health of Indonesians has improved significantly over the past three decades. Life expectancy in Indonesia has increased from 62.3 to 71.5 years between 1990 and 2018.13 Morbidity and mortality due to communicable, maternal, neonatal and nutritional causes have also decreased significantly.14 However, the state of health and access to health services vary throughout the country.15,16 For example, the World Health Organization (WHO) has reported large inequalities across provinces in access to maternal and child healthcare and availability of healthcare infrastructure.17
Indonesia is also moving towards UHC with its National Health Insurance scheme (Jaminan Kesehatan Nasional, JKN). Indonesia launched the JKN in 2014 with a target of covering 98% of its population by 2024.18 The scheme collects contributions from formal/informal/non-salaried workers and pays full or partial premiums for low-income members. By the end of 2019, about 84% of Indonesia's population was covered by the JKN.19 Apart from SHI, Indonesia's health system includes other government schemes financed through taxes and non-public schemes such as company health coverage (CHC), PHI and OOP payments. In 2019, the government's spending on health amounted to 113·6 trillion rupiah (7·9 billion USD) which was almost double the amount in 2015.20,21 The reliance on OOP payments has decreased in recent years, but about one third of health expenditure still comes from OOP payments. According to Indonesia's National Health Accounts (NHA) data in 2019, OOP payments were the largest contributor to total health expenditure, accounting for 32·1% (Table 1).22 This is followed by various government schemes and the JKN, which represented 29·1% and 23·1% of total health expenditure respectively. Health expenditure through PHI is low with a share of only 3·5%.
Table 1.
Health sector funding sources as a proportion of total health expenditure 2015–2019.
| 2015 | 2016 | 2017 | 2018 | 2019 | |
|---|---|---|---|---|---|
| Social health insurance | 17·6% | 19·3% | 22·2% | 22·8% | 23·1% |
| Other public schemes | 25·5% | 29·5% | 28·2% | 29·0% | 29·1% |
| Private health insurance | 2·8% | 3·1% | 3·2% | 3·1% | 3·5% |
| Company health coverage | 13·0% | 11·3% | 11·6% | 11·0% | 11·1% |
| Household out-of-pocket | 40·2% | 35·8% | 33·7% | 33·0% | 32·1% |
| Non-Profit schemes | 0·9% | 1·1% | 1·1% | 1·1% | 1·0% |
Source: National Health Accounts Indonesia 2019.
While one study has explored progressivity of financing in Indonesia in 2001,23 no further FIA studies have been undertaken to assess the equity of the health financing system subsequent to the introduction of the JKN. Such analysis is valuable to policymakers in understanding the impact of recent reforms on progressing towards UHC.6 Thus, this paper aims to assess how the equity of health financing in Indonesia has changed over a five-year period from 2015 to 2019 and to provide evidence for future health policies.
Methods
Data sources
The sources of health financing analysed in this study included direct taxes, indirect taxes, SHI, CHC, PHI and OOP payments. Our study drew on three key national datasets: the National Socioeconomic Survey (SUSENAS) for the years 2015 to 2019; the Indonesian Family Life Survey (IFLS) 2014; and the Indonesian National Health Accounts 2019.
The SUSENAS is a multi-purpose household survey covering a nationally representative sample of at least 200,000 households.24 In SUSENAS 2015 – 2019, samples were drawn from all 34 provinces in Indonesia. The core questionnaire collects basic socioeconomic information for all household members. Since the SUSENAS surveys in 2015 – 2019 did not collect income data, we used income data from the fifth wave of the IFLS (IFLS5) and mapped it to the SUSEANS surveys. The IFLS is a longitudinal socioeconomic and health survey which collects individual, household and community level data using multistage stratified sampling. The sampling frame is based on households from 13 Indonesian provinces, representative of about 83% of the population.25 Within each of the 13 provinces, enumeration areas (EAs) were randomly chosen from a sample frame used in the 1993 SUSENAS survey. IFLS5 was conducted in 2014 and included over 30 modules. It was completed by 50,148 individuals (51% women) of all ages from 16,204 households located in both urban and rural areas.25
Data analysis
Ability to pay (ATP)
ATP was measured using non-food consumption (including alcohol and tobacco) in the SUSENAS and IFLS5 datasets. Monthly home rental cost (actual or estimated) was also included. Where no home rental was paid (e.g. household owned their home), the householder was asked to estimate the rent they would have had to pay if they rented it. Survey weights were used for analysis of the SUSENAS and IFLS5 datasets to account for over- or under-representation of population strata in the sample.3
Health financing sources
In this study, direct tax payments included personal income tax and corporate income tax. To estimate personal income tax, we first calculated the ratios of household expenditure to personal income in the IFLS5. These ratios were then mapped to the SUSENAS datasets using ATP rankings (50 quantiles), so households with the same ATP ranking would have the same expenditure-personal income ratio. Household personal income in the SUSENAS datasets (2015 – 2019) was predicted using expenditure data from the SUSENAS datasets and the ratios of expenditure to personal income from the IFLS5. The information on marginal tax rates obtained from the Ministry of Finance was used to estimate the amount of personal income tax paid by households.26 In this analysis, we only included expenditure-personal income ratios smaller than one. For corporate income tax, we first calculated the average gross business income and net profit in IFLS5 by taxable personal income categories. We then mapped the average business income and net profit from the IFLS5 to the SUSENAS based on personal income categories. Whether the households received any business credit was used as an indicator for owning a business in the SUSENAS datasets.
Indirect tax payments by households in the SUSENAS datasets (value-added tax, sales tax on luxury goods, excise tax and import duties) were calculated using the expenditure data and tax rates sourced from Indonesian law and regulatory documents.27, 28, 29 The SHI contributions in the SUSENAS datasets were calculated based on the predicted income and the SHI premium rates defined by the National Health Insurance Agency (Badan Penyelenggara Jaminan Sosial Kesehatan, BPJS).30 After comparing health expenditure on the JKN using the NHA reports with the revenue collected from JKN members using the BPJS annual financial reports, we found that the JKN was in deficit throughout 2015 – 2019. We have assumed that the Indonesian government was paying the deficit through taxation (indirect and direct taxes). For CHC, regulations require that contributions are made by both employers (4% of monthly salaries) and employees (1% of monthly salaries). As the 4% would have been part of the employees’ benefit package, we assumed that 5% of predicted household income would be contributed to CHC by relevant households in the SUSENAS datasets. The ownership of SHI and CHC was informed by respondents’ answers to survey questions in the SUSENAS. Both PHI and OOP payments were directly derived from SUSENAS survey responses.
Financing incidence analysis
The assessment of health financing incidence involved, first, assessing the progressivity of each financing source, and second, assessing the progressivity of the health financing system as a whole. We used the Kakwani index (KI) to assess the relative progressivity of various financing schemes - taxation (direct and indirect taxes), SHI, PHI, CHC and OOP payments - from 2015 to 2019.31 The KI is a summary measure of progressivity and ranges from −2 to 1; a positive value indicates a progressive financing source and a negative value the opposite.32 The calculation of KI is based on two underlying indices, the Gini index and the concentration index (details in Table 2). The Gini index is derived from the Lorenz curve which shows the distribution of income across households, ranked in ascending order. The concentration index is derived from the concentration curve that plots the cumulative percentage share of health care payments for each household in the same ascending order as the Lorenz curve.3 Households with missing data on consumption (food and non-food) were excluded from the analysis. If the household reported consumption but no data was available on certain variables such as PHI payment, the household would still be included in the calculation of the Gini Index, but would not be included in the calculation of the concentration index and the KI for PHI. In this study, missing data constituted less than 1% of the data. Dominance tests were conducted to examine the consistency of progressivity along the distribution of ATP.3 If the Lorenz curve dominates (lies above the concentration curve), it means those with a lower income contribute a smaller proportion of their income to health care payments than those with higher income, and is progressive across all income levels (and vice versa).
Table 2.
Indices for assessing equity in health financing.
| Index type | Description |
|---|---|
| Gini index | The Gini index is derived from the Lorenz curve which shows the distribution of income across households, ranked in ascending order. The Gini ranges from 0 to 1, with 0 representing perfect equality in the distribution of ATP and 1 representing perfect inequality.6 |
| Concentration index | The concentration index is derived from the concentration curve that plots the cumulative percentage share of health care payments for each household in the same ascending order as the Lorenz curve.3 The concentration index ranges from -1 (all health care payments are made by the poorest households) to 1 (all health care payments are made by the richest households).31,52 |
| Kakwani index | The Kakwani index is obtained as the difference between the concentration and the Gini index. |
The progressivity of the whole health financing system was estimated by taking the weighted sum of the KI of each financing source. National Health Accounts data from the Ministry of Health,22 JKN contributions from the Social Security Agency for Health,33,34 and government revenue reports from the Ministry of Finance20,21 were used to derive the proportional contributions or weightings for each source of health financing for years 2015 – 2019 (Appendix Table A2).
Adjustment for household members
To account for household size and age of household members, all key variables were adjusted using an adult equivalent (AE) scale based on the following formula: AE = (A + αK)θ where A is the number of adults in the household, K is the number of children, α is the cost of a child relative to that of an adult, and θ the degree of economies of scale.3,35 Children are defined as those under 15 years old.36 The values of α and θ were assumed to be 0·5 and 0·75 respectively in the base case analysis.35,37 In the analysis, we first calculated the direct taxes, indirect taxes, SHI, PHI, CHC and OOP payments at the household level. We then divided the total household payments by the AE scale to obtain individual-level estimates.
Sensitivity analysis
Sensitivity analyses were conducted to assess the impact of using different AE scales and different measures of ATP. The alternative AE scales used were AE = A + 0.3K and AE = (A + K)0.5. Total consumption (food and non-food) was used as the alternative measure for ATP. We also conducted sensitivity analysis around the proportional contributions of individual health financing sources towards overall health financing. The proportional contributions of direct taxes were increased by 10%, 25% and 50%. The weightings of indirect taxes were reduced accordingly, and the proportions of other financing sources remain unchanged. In the baseline analysis, we only included expenditure-income ratios smaller than one from the IFLS5 when we predicted personal income in the SUSENAS datasets. In the sensitivity analysis, we relaxed this constraint by including all ratios. All analyses were conducted using STATA 15.1.38
Role of the funding source
The funding source had no role in the design of this study, analyses of the data, interpretation of the data, writing of the report or decision to submit the results.
Results
Baseline analysis
Table 3 presents the Gini indices (non-food consumption), concentration indices and KIs for each source of financing and the health system as a whole. The Gini indices ranged between 0·470 and 0·509, indicating an unequal distribution of wealth among the whole population. We found that the poorest 20% of all households held a share of non-food consumption that was less than 5%, while the richest 20% of households held a share that exceeded 50% (Appendix Table A3). The concentration indices for health care payments through various funding schemes were all positive, indicating that health care payments were also concentrated in the wealthy population.
Table 3.
Progressivity of individual financing source and overall health financing in Indonesia 2015 – 2019 (ATP based on non-food consumption).
| 2015 |
2016 |
2017 |
2018 |
2019 |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Concentration index | Kakwani index | Concentration index | Kakwani index | Concentration index | Kakwani index | Concentration index | Kakwani index | Concentration index | Kakwani index | |
| Indirect taxes | 0·426 | -0·077 | 0·407 | -0·064 | 0·409 | -0·066 | 0·417 | -0·06 | 0·461 | -0·049 |
| Value-added tax | 0·486 | -0·017 | 0·457 | -0·014 | 0·457 | -0·019 | 0·462 | -0·015 | 0·499 | -0·01 |
| Luxury goods tax | 0·881 | 0·378 | 0·861 | 0·39 | 0·856 | 0·381 | 0·861 | 0·385 | 0·860 | 0·351 |
| Excise tax | 0·162 | -0·341 | 0·175 | -0·296 | 0·166 | -0·309 | 0·164 | -0·313 | 0·268 | -0·241 |
| Import tax | 0·616 | 0·113 | 0·569 | 0·098 | 0·579 | 0·104 | 0·605 | 0·129 | 0·623 | 0·114 |
| Others | 0·563 | 0·060 | 0·532 | 0·061 | 0·549 | 0·073 | 0·551 | 0·074 | 0·585 | 0·075 |
| Direct taxes | 0·556 | 0·053 | 0·526 | 0·055 | 0·508 | 0·033 | 0·505 | 0·028 | 0·557 | 0·048 |
| Personal income tax | 0·557 | 0·054 | 0·527 | 0·056 | 0·510 | 0·034 | 0·506 | 0·030 | 0·559 | 0·049 |
| Corporate income tax | 0·276 | -0·227 | 0·241 | -0·230 | 0·311 | -0·164 | 0·294 | -0·183 | 0·175 | -0·334 |
| Social health insurance (JKN) | 0·491 | -0·012 | 0·421 | -0·050 | 0·476 | 0·000 | 0·482 | 0·006 | 0·393 | -0·116 |
| Company health coverage | 0·791 | 0·288 | 0·786 | 0·315 | 0·637 | 0·161 | 0·635 | 0·159 | 0·402 | -0·107 |
| Private health insurance | 0·669 | 0·167 | 0·551 | 0·080 | 0·425 | -0·051 | 0·393 | -0·084 | 0·443 | -0·066 |
| Out-of-pocket | 0·562 | 0·059 | 0·538 | 0·067 | 0·531 | 0·055 | 0·526 | 0·049 | 0·543 | 0·034 |
| Overall | 0·573 | 0·070 | 0·534 | 0·063 | 0·512 | 0·037 | 0·510 | 0·034 | 0·479 | -0·030 |
| Gini | 0·503 | 0·471 | 0·476 | 0·477 | 0·509 | |||||
All indices are significant with p<0·05. The p-value is for a test where the index equals 0.
A positive Kakwani index indicates progressivity and a negative value the opposite.
A positive concentration index indicates that the rich contribute more to health care payments.
The proportional contributions of each source of health financing towards overall health financing are summarized in Appendix Table A3.
For indirect taxes, direct taxes and SHI, the proportion of payments by each quintile group were similar across the five-year period (Appendix Tables A4–A6). On the other hand, relatively few of those in the poorest 20% of households were part of CHC, but their share of CHC payments greatly increased to 6·8% in 2019 compared with 0·5% in 2015 (Appendix Table A7). Meanwhile, the proportion of CHC payments among the richest 20% of households declined. The proportion of PHI payments from lower ATP quintiles also increased since 2015 but dropped among the richer population (Appendix Table A8). In terms of OOP payments, the burden was largely borne by the higher income groups (Appendix TableA9). The share of OOP payments by the poorest 20% of households remained below 5% over the 5-year period. In contrast, there was an increase in the share of OOP payments paid by the middle quintile groups over the same period.
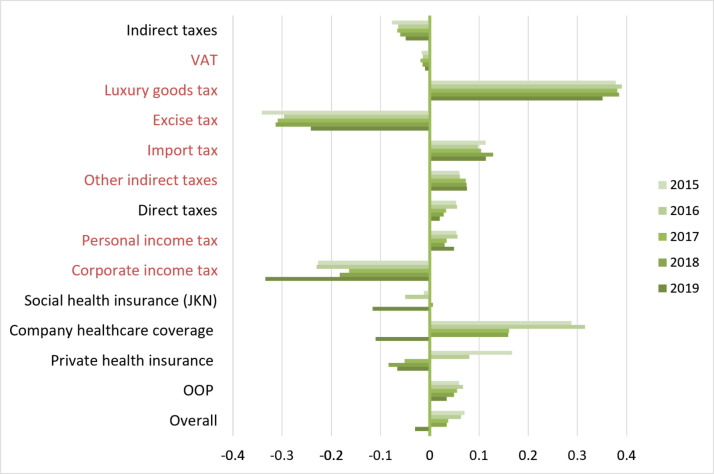
The KIs for direct taxes and OOP payments were positive throughout the 5-year period, indicating that these two sources of funding were progressive (Table 3 and Figure 1). Indirect taxes were regressive with negative KIs. SHI was regressive except in 2017 and 2018. CHC was the most progressive source of financing before 2019, but became regressive in 2019. PHI was progressive in 2015 and 2016 and regressive after that time. Overall, health financing in Indonesia was slightly progressive between 2015 and 2018, as measured by the KI. However, the level of progressivity declined year by year and became regressive in 2019.
Figure 1.
Progressivity of each health financing source (Kakwani index).
Dominance tests
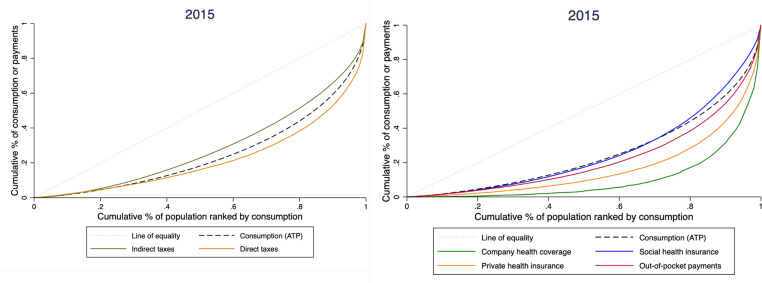
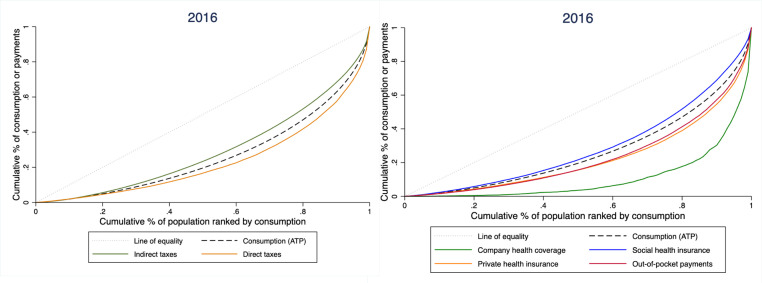
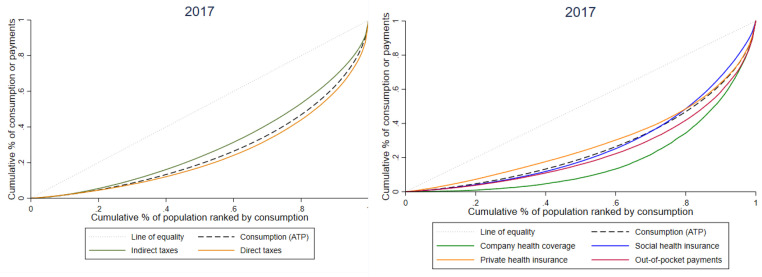
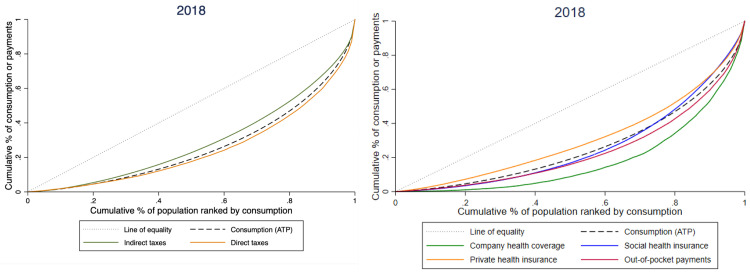
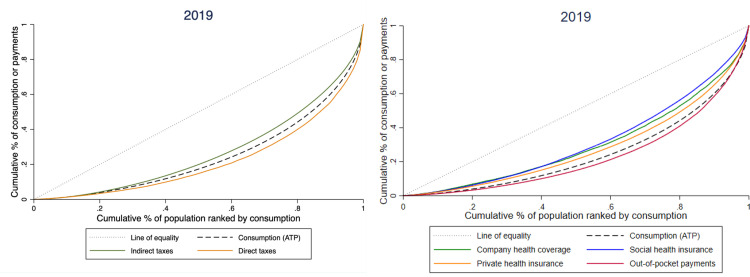
The Lorenz curve of consumption (ATP) and concentration curves for the various sources of health financing for 2015-2019 are shown in Figure 2, Figure 3, Figure 4, Figure 5, Figure 6. For each year, the concentration curves for OOP payments lay below the Lorenz curve, indicating that the progressivity of this source of health financing was consistent along the entire distribution of ATP (Table 4). With the exception of 2018, the concentration curve for indirect tax payments crossed the Lorenz curve indicating that while indirect taxes were regressive overall, they tended to be progressive at lower ATP quantile points. The concentration curve for direct tax payments also crossed the Lorenz curve at lower ATP quantile points for each year, indicating that this source of financing was regressive for poorer households despite a positive KI. The curves for SHI crossed the Lorenz curve in years 2015, 2017, and 2018, suggesting that its progressivity was not consistent along the ATP distribution. For CHC, the concentration curves were well below the Lorenz curve in years 2015 – 2018 but then moved above the Lorenz curve in 2019, which corresponds to a change from the most progressive financing source before 2019 to a regressive health financing source in 2019. The concentration curves for PHI payments were dominated by the Lorenz curve in 2015 and 2016 but after that fell below the Lorenz curve, indicating that this source of payment became regressive.
Figure 2.
Lorenz curve and concentration curves by financing source in 2015.
Figure 3.
Lorenz curve and concentration curves by financing source in 2016.
Figure 4.
Lorenz curve and concentration curves by financing source in 2017.
Figure 5.
Lorenz curve and concentration curves by financing source in 2018.
Figure 6.
Lorenz curve and concentration curves by financing source in 2019.
Table 4.
Dominance test results by source of health financing.
| Dominance† |
|||||
|---|---|---|---|---|---|
| 2015 | 2016 | 2017 | 2018 | 2019 | |
| Indirect tax | * | * | * | - | * |
| Direct tax | * | * | * | * | * |
| Social health insurance | * | - | * | * | - |
| Company health coverage | + | + | + | + | - |
| Private health insurance | + | + | - | - | - |
| Out-of-pocket | + | + | + | + | + |
Dominance test is based on the multiple comparison approach that tests differences at 19 evenly spaced quantiles.
+Lorenz curve dominates; - concentration curve dominates; *curves cross.
Sensitivity analysis
Concentration and Kakwani indices using alternative AE scales and total consumption (food and non-food) as a measure of ATP are presented in Appendix Tables A10–A12. Using alternative AE scales has little effect on the progressivity of individual health financing sources and the overall health financing system, as the indices are almost identical to the baseline results. When total consumption was considered as a measure of ATP, the concentration indices remained similar to the baseline concentration indices, whereas the Gini indices dropped to around 0·4 (range 0·37 – 0·43) compared to 0·5 (range 0·47 – 0·51) in the baseline analysis (using non-food consumption expenditure). As a result of the more equitable Gini index using total consumption expenditure, the progressivity of individual health financing sources and overall health financing was higher each year than when non-food consumption was used for ATP, with overall health financing becoming progressive in 2019. Increased proportional contributions of direct taxes and decreased proportions of indirect taxes would slightly improve overall progressivity (Appendix Table A13). When we used expenditure-income ratios both greater than one and smaller than one from the IFLS5 to predict personal income in the SUSENAS datasets, the progressivity of all income-related health financing sources fell (Appendix Table A14). Direct tax payments and SHI became regressive throughout 2015 – 2019. The overall health financing system also became regressive after 2015. But no matter which AE scale, measure of ATP, or set of proportional contributions was used, and how income in the SUSENAS datasets was predicted, the progressivity of overall health financing displayed a downward trend over the study period.
Discussion
This is the first multi-year study to investigate the equity of health financing in Indonesia after implementation of the JKN. Our analysis shows that the Indonesian health financing system was progressive between 2015 and 2018, with a declining trend. In 2019, health financing in Indonesia became regressive.
Our study has shed some light on how the implementation of the JKN has impacted the equity of health financing in Indonesia. In our analysis, the SHI was mildly progressive in 2017 and 2018. The Kakwani indices for SHI in 2017 and 2018 were close to zero, which means that the poor and the rich were contributing almost the same share of their non-food expenditure towards SHI contributions. As a result, the SHI appears to have had minimal impact on the progressivity of the overall health system in Indonesia in 2017 and 2018. While the SHI was regressive in 2015 and 2016, due to the small share of SHI in total health funding (less than 18%), the overall progressivity was not affected. However, in 2019, as the share of SHI revenue increased to 23%, overall health financing in Indonesia became regressive as a result of a regressive SHI. The concentration index for SHI in 2019 would need to have been at least 0.53 (Kakwani index 0.021) to generate a positive Kakwani index for the overall health financing system. Given that SHI is designed to relieve the financial burden on the poor, the regressive nature of SHI in 2019 suggests that more needs to be done to ensure the poor are financially protected. Since the low-income population in Indonesia receive subsidies under the JKN scheme, it is not surprising to see that the population with lower ATP contributed a relatively smaller share towards SHI payments, as shown in the dominance tests for years 2015, 2017 and 2018. However, SHI still displayed an overall trend of being either regressive or proportional. This finding reflects the nature of the JKN levy. During the study period, the government charged a fixed rate for employees from both public and private sectors (5% of monthly income) with a ceiling of Rp 8 million monthly salary30 for assessed contributions, which means the burden of JKN premiums was disproportional to household ATP. Although the Indonesian government raised the monthly salary ceiling to Rp 12 million (USD 827) in 2020, the ceiling is low for high-income populations.
Another important finding of our study is that OOP payment is a progressive source of health financing in Indonesia. Although a positive KI indicates some degree of equity in health financing, the progressivity of OOP is likely to be partly driven by unmet need.39 This is because low-income households may forgo health care and avoid OOP payments simply because they cannot afford the cost; conversely those at the upper end of the income scale may choose to incur higher OOP payments for higher quality or amenity services. Our analysis also found that as Indonesia's reliance on OOP payments decreased year by year (41% of total health expenditure in 2015 to 33% in 2019), the progressivity of OOP payments also fell. Although the burden of OOP payments was still largely borne by the richest 20% of the population, their share of OOP payments dropped slightly (Appendix Table A9). In contrast, the poorest 20% of the population contributed a similar share of OOP payments across the five years. The JKN was designed to provide financial protection by reducing OOP payments for the insured. It is possible that people in higher socio-economic groups have better access to information on how the JKN operates including which services are covered, giving them an advantage over poorer groups. Limited awareness among the poor of the benefits provided by health insurance schemes has been reported in other LMIC.40, 41, 42, 43 The gap between the scheduled fee and the real cost of accessing health care may also explain why the poor are not fully financially protected under JKN. In Indonesia, BPJS provides capitation payments for primary health care and the Indonesian Case Base Groups (INA-CBG) payments for hospital care. Theoretically, JKN members do not have to pay if they attend health facilities operated under the JKN network. But there is evidence that the costs of medical procedures are usually higher than capitation and INA-CBG tariffs.44,45 Poorer households may still face OOP paymentseven if they are insured under the JKN.
Our analysis showed that direct taxes were progressive across the entire five years, but their contribution to the overall progressivity of health financing was relatively small, unlike other LMICs where direct taxes are a major driver of overall progressivity.8,36,37,46 In addition, the dominance tests showed that direct taxes were regressive for the population with lowest ATP. This suggests that the poorest bore a proportionally higher burden of financing health through direct taxes compared with the richer population. In contrast, health financing through indirect taxes was regressive, which is consistent with findings from the majority of FIA studies.8 This is mainly because indirect taxes such as value-added taxes and excise taxes are levied at a uniform rate. The poor would contribute a larger proportion of their income to indirect taxes than the rich if they consume the same amount of goods and services. Indonesia has recently increased cigarette taxes by 12·5% to reduce tobacco consumption and increase tax revenue.47 However, there is evidence that the poor, with higher smoking rates,48 are burdened with higher cigarette taxes than the rich.49 It is possible that indirect taxes, as a source of health financing, will become more regressive following the new cigarette tax policy in Indonesia. To reduce the regressivity of indirect taxes, while at the same time maintaining high cigarette taxes to curb consumption, other measures could be considered such as increasing taxes on luxury goods, as luxury taxes with a concentration index above 0·8 are borne disproportionately by the rich (Table 3).
Another finding of our study is that the progressivity of CHC also contributed to the progressivity of the overall health financing system in 2015 – 2018. CHC was highly progressive in 2015 but progressivity fell in the following years, becoming regressive in 2019. This is likely to be the result of rising CHC payments among poorer households over the years while contributions by the richest 20% of household fell considerably over the same period. It is likely that more people from poorer households started to enter formal employment and contribute to CHC. However, this finding needs to be interpreted with caution - while around 40% of the Indonesian population work in the formal sector,50 less than 4% of households in the SUSENAS surveys report having CHC every year. Thus, calculating the progressivity of CHC might be biased by an underrepresentation of the population who have CHC in the survey.
The major strength of this study is that it's a multi-year FIA, depicting the changes in sources of financing and financial incidence in Indonesia following the implementation of the JKN. Such information is essential to inform Indonesia's future policies to improve financial equity while extending coverage to the whole population through the JKN. Another strength is that we conducted rigorous sensitivity analyses to examine our assumptions and uncertainty in key parameters, especially the Gini indices. In the baseline analysis, Gini indices were calculated based on non-food consumption and were found to be higher than World Bank estimates.51 In the sensitivity analysis, we used total consumption to measure ATP and derived Gini indices closer to the World Bank estimates. Using the more equitable Gini indices resulted in higher Kakwani indices in the sensitivity analysis, but did not change the downward trend in the progressivity of overall health financing in Indonesia. One limitation of this study is that we relied on survey data on household consumption and expenditure, which is subject to recall bias and missing data. Another limitation is that the SUSENAS datasets did not directly provide household income data. To estimate direct tax payments, we adopted an innovative method of mapping household income in the IFLS5 to the SUSENAS datasets. We included only expenditure-income ratios smaller than one from the IFLS5 dataset, since there were wide variations within and across the IFLS surveys for ratios greater than one (Appendix Table A1). Given that it is possible to spend more than what is earned, omitting expenditure-income ratios greater than one might have led to an overestimate of personal income in the analysis. In addition, the IFLS5 was conducted in 2014 and covered only 13 provinces in Indonesia. This may have also biased our predictions of personal income. Comparison of our study findings with other countries needs to take into account these strengths and weaknesses.
Conclusion and recommendations
Indonesia has made significant progress in implementing its UHC agenda. The declining progressivity of the overall health financing system between 2015 and 2019 however suggests room for improvement towards a fair and equitable health financing system. Based on the results of this study we have a number of recommendations. First, given that direct tax contributions to overall progressivity is limited, efforts must be intensified to increase direct tax revenue collection and to increase the progressive tax rate across income brackets. Second, there is an urgent need to make the system for paying contributions to the SHI more progressive. Raising the salary ceiling when collecting JKN premiums should be considered to allow the burden of SHI to be shifted more towards the rich. Third, the finding that OOP payments fell as a share of total health expenditure and were progressive between 2015 and 2019, gives reason to be optimistic. Nonetheless, OOP payments must be closely monitored as they appear to be becoming less progressive overtime. Also, it is likely that the progressivity of OOP payments is driven by unmet need among the low-income population and a preference for higher cost care amongst the wealthy. Further studies, such as benefit incidence analyses, are warranted to ensure that the poor are not simply forgoing health care. To further reduce OOP payments, the capitation and INA-CBG tariffs need to be reviewed to match real health care costs. Finally, we recommend that future SUSENAS surveys include household income questions to facilitate direct estimates of financing incidence.
Declaration of interests
The authors declare no conflicts of interest.
Acknowledgments
Author contribution
VW, HT, AA, SK, LG, AM, AH, VT conceived and designed the study. VW and HT co-supervised the study. DS, RAF, DN, GC, EA contributed to data curation. QC and NM conducted the data analysis. All authors contributed to the interpretation of the results. QC drafted the manuscript which all authors commented on. All authors critically reviewed and approved the final manuscript.
Data sharing
Post-processing source data and supplementary data are presented within this study. Access to the SUSENAS datasets can be requested from the Central Bureau of Statistics of Indonesia. IFLS-5 Survey data is publicly available at https://www.rand.org/well-being/social-and-behavioral-policy/data/FLS/IFLS/ifls5.html.
Acknowledgements
This study was supported through the Health Systems Research Initiative in the UK, and is jointly funded by the Department of International Development, the Economic and Social Research Council, the Medical Research Council and the Wellcome Trust. The funders of this research were not involved in the study.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100400.
Appendix. Supplementary materials
References
- 1.World Health Organization . World Health Organization; Geneva: 2010. 5.Health Systems Financing. Monitoring the Building Blocks of Health Systems: a Handbook of Indicators and their Measurement Strategies.https://apps.who.int/iris/handle/10665/258734 [Google Scholar]
- 2.World Health Organization . World Health Organization; Geneva: 2010. The World Health Report: Health Systems Financing: the Path to Universal Coverage.https://apps.who.int/iris/handle/10665/44371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O’Donnell O., van Doorslaer E., Wagstaff A., Lindelow M. World Bank; Washington, DC: 2008. Analyzing Health Equity Using Household Survey Data: A Guide to Techniques and Their Implementation.http://hdl.handle.net/10986/6896 [Google Scholar]
- 4.World Bank . World Bank; Washington, DC: 2012. Health Equity and Financial Protection in Ghana. Health Equity and Financial Protection Report.http://hdl.handle.net/10986/27067 [Google Scholar]
- 5.Wagstaff A., Eozenou P., Neelsen S., Smitz M. World Bank; Washington, DC: 2019. The 2019 Update of the Health Equity and Financial Protection Indicators Database : An Overview.http://hdl.handle.net/10986/31869 [DOI] [PubMed] [Google Scholar]
- 6.Ataguba J.E., Asante A.D., Limwattananon S., Wiseman V. How to do (or not to do) … a health financing incidence analysis. Health Policy Plann. 2018;33(3):436–444. doi: 10.1093/heapol/czx188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.OECD. Sources of health care financing 2017. https://www.oecd-ilibrary.org/content/component/health_glance-2017-47-en. Accessed 13 March 2021.
- 8.Asante A., Price J., Hayen A., Jan S., Wiseman V. Equity in health care financing in low- and middle-income countries: a systematic review of evidence from studies using benefit and financing incidence analyses. PLOS ONE. 2016;11(4) doi: 10.1371/journal.pone.0152866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Molla A.A., Chi C. Who pays for healthcare in Bangladesh? An analysis of progressivity in health systems financing. Int J Equity Health. 2017;16(1):167. doi: 10.1186/s12939-017-0654-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwesiga B., Ataguba J.E., Abewe C., Kizza P., Zikusooka C.M. Who pays for and who benefits from health care services in Uganda? BMC Health Serv Res. 2015;15(1):44. doi: 10.1186/s12913-015-0683-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asante A.D., Irava W., Limwattananon S., et al. Financing for universal health coverage in small island states: evidence from the Fiji Islands. BMJ Glob Health. 2017;2(2) doi: 10.1136/bmjgh-2016-000200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Onwujekwe O., Hanson K., Ichoku H., Uzochukwu B. Financing incidence analysis of household out-of-pocket spending for healthcare: getting more health for money in Nigeria? Int J Health Plann Manag. 2014;29(2):e174–e185. doi: 10.1002/hpm.2166. [DOI] [PubMed] [Google Scholar]
- 13.The World Bank. Life expectancy at birth, total (years) - Indonesia 2018. https://data.worldbank.org/indicator/SP.DYN.LE00.IN?locations=ID. Accessed 18 March 2021
- 14.Mboi N., Murty Surbakti I., Trihandini I., et al. On the road to universal health care in Indonesia, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2018;392(10147):581–591. doi: 10.1016/S0140-6736(18)30595-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Suparmi, Kusumawardani N., Nambiar D., Trihono, Hosseinpoor A.R. Subnational regional inequality in the public health development index in Indonesia. Glob Health Action. 2018;11(sup1) doi: 10.1080/16549716.2018.1500133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hodge A., Firth S., Marthias T., Jimenez-Soto E. Location matters: trends in inequalities in child mortality in Indonesia. Evidence from repeated cross-sectional surveys. PloS one. 2014;9(7) doi: 10.1371/journal.pone.0103597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization . World Health Organization; Indonesia Geneva: 2017. State of Health Inequality.https://apps.who.int/iris/handle/10665/259685 [Available from: [Google Scholar]
- 18.Ministry of Health of the Republic of Indonesia . Ministry of Health of the Republic of Indonesia; Jakarta: 2015. Strategic Planning Ministry of Health 2015-2019 Decree of the Minister of Health of the Republic of Indonesia Number hk.02.02/menkes/52/2015.https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/indonesia/restra_2015_translated_1.pdf [Google Scholar]
- 19.Badan Penyelenggara Jaminan Sosial Kesehatan [Social Security Agency for Health]. Ringkasan Eksekutif Laporan Pengelolaan Program dan Laporan Keuangan BPJS Kesehatan tahun 2019 (Auditan) [Executive Summary of Program Management Reports and BPJS Health Financial Reports 2019 (Audited)] Jakarta: BPJS Kesehatan; 2020. https://bpjs-kesehatan.go.id/bpjs/arsip/detail/1514. Accessed 12 January 2021.
- 20.Kementerian Keuangan [Ministry of Finance] Ministry of Finance; 2020. Buku II Nota Keuangan beserta Anggaran Pendapatan dan Belanja Negara Tahun Anggaran 2020 [Book II Financial Notes and the State Budget for Fiscal Year 2020] Jakarta.https://www.kemenkeu.go.id/media/14041/nota-keuangan-beserta-apbn-ta-2020.pdf [Google Scholar]
- 21.Kementerian Keuangan [Ministry of Finance] Ministry of Finance; 2021. Buku II Nota Keuangan beserta Anggaran Pendapatan dan Belanja Negara Tahun Anggaran 2021 [Book II Financial Notes and the State Budget for Fiscal Year 2021] Jakarta.https://www.kemenkeu.go.id/media/16834/buku-ii-nota-keuangan-beserta-apbn-ta-2021.pdf [Google Scholar]
- 22.Kementerian Kesehatan [Ministry of Health]. National Health Accounts Indonesia 2019 (unpublished). 2021.
- 23.O'Donnell O., van Doorslaer E., Rannan-Eliya R.P., et al. Who pays for health care in Asia? J Health Econ. 2008;27(2):460–475. doi: 10.1016/j.jhealeco.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 24.Badan Pusat Statistik [Central Bureau of Statistics]. Survei Sosial Ekonomi Nasional (SUSENAS) - Modul Sosial Budaya dan Pendidikan (Tahunan), 2015 [Socio-Cultural and Educational Module (Annual), 2015]. 2015. https://sirusa.bps.go.id/sirusa/index.php/dasar/pdf?kd=1581&th=2015. Accessed 13 January 2021.
- 25.Strauss J., Witoelar F., Sikoki B. RAND Corporation; 2016. The Fifth Wave of the Indonesia Family Life Survey: Overview and Field Report: Volume 1.https://www.rand.org/pubs/working_papers/WR1143z1.html [Google Scholar]
- 26.Kementerian Keuangan DJPMoF, Directorate General of Taxation],. PPh (Pajak Penghasilan) [Income tax] Jakarta: Ministry of Finance; 2013. https://www.kemenkeu.go.id/sites/default/files/buku%20pph%20upload.pdf. Accessed 13 January 2021.
- 27.Republik Indonesia. Undang-Undang Republic Indonesia Nomor 42 Tahun 2009 Tentang Perubahan Ketiga Atas Undang-Undang Nomor 8 Tahun 1983 Tentang Pajak Pertambahan Nilai Barang Dan Jasa Dan Pajak Penjualan Atas Barang Mewah[Law Number 42 of 2009 Republic of Indonesia Third Amendment to Law Number 8 Year 1983 concerning Value Added Tax on Goods and Services and Sales Tax on Luxury Goods] Jakarta 2009. https://pajak.go.id/id/undang-undang-nomor-42-tahun-2009. Accessed 13 January 2021.
- 28.Kementerian Keuangan [Ministry of Finance]. Peraturan Menteri Keuangan Republik Indonesia Nomor 17 /Pmk. 010/2018 Tentang Perubahan Kedua Atas Peraturan Menteri Keuangan Nomor 6/Pmk.0l0/2017 Tentang Penetapan Sistem Klasifikasi Barang DanPembebanan Tarif Bea Masuk Atas Barang Impor [Second Amendment to Regulation of the Minister of Finance Number 6 /PMK.010 / 2017 concerning Stipulation of Goods Classification System and Imposing Import Duty Tariff on Imported Goods] Jakarta: Ministry of Finance; 2018. https://jdih.kemenkeu.go.id/fullText/2018/17∼PMK.010∼2018Per.pdf. Accessed 13 January 2021.
- 29.Kementerian Keuangan [Ministry of Finance]. Peraturan Menteri Keuangan Nomor 6/PMK.010/2017 tentang Penetapan Sistem Klasifikasi Barang dan Pembebanan Tarif Bea Masuk atas Barang Impor [Minister of Finance Regulation Number 6 /PMK.010 / 2017 concerning Stipulation of Goods Classification System and Imposing Import Duty Tariff on Imported Goods] Jakarta: Ministry of Finance; 2017. https://jdih.kemenkeu.go.id/in/page/dokumen-peraturan/e34b1791-06b7-44a3-a1cb-4636f16d5b02. Accessed 13 January 2021.
- 30.Badan Penyelenggara Jaminan Sosial Kesehatan [Social Security Agency for Health]. Iuran 2021. https://bpjs-kesehatan.go.id/bpjs/pages/detail/2014/13. Accessed 16 March 2021.
- 31.Kakwani N.C. Measurement of tax progressivity: an international comparison. Econ J. 1977;87(345):71–80. [Google Scholar]
- 32.Mills A., Ataguba J.E., Akazili J., et al. Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet. 2012;380(9837):126–133. doi: 10.1016/S0140-6736(12)60357-2. [DOI] [PubMed] [Google Scholar]
- 33.Badan Penyelenggara Jaminan Sosial Kesehatan [Social Security Agency for Health]. Laporan pengelolaan program Dan Laporan Keuangan Jaminan Sosial Kesehatan Tahun 2017 [program management report and health social security financial report 2017] 2018. https://bpjs-kesehatan.go.id/bpjs/arsip/detail/1071. [Accessed 12 Jan 2021].
- 34.Badan Penyelenggara Jaminan Sosial Kesehatan [Social Security Agency for Health]. Laporan Pengelolaan Program dan Laporan Keuangan Tahun 2018 - Bagian 2 [Program Management Report and Financial Report 2018 - Part 2] 2019. https://bpjs-kesehatan.go.id/bpjs/arsip/detail/1329. Accessed 12 January 2021.
- 35.Deaton A, Zaidi S. Guidelines for constructing consumption aggregates for welfare analysis. LSMS Working Paper No. 135. Washington DC: World Bank; 2002.
- 36.Munge K., Briggs AH. The progressivity of health-care financing in Kenya. Health Policy Plan. 2014;29(7):912–920. doi: 10.1093/heapol/czt073. [DOI] [PubMed] [Google Scholar]
- 37.Mtei G., Makawia S., Ally M., Kuwawenaruwa A., Meheus F., Borghi J. Who pays and who benefits from health care? An assessment of equity in health care financing and benefit distribution in Tanzania. Health Policy Plann. 2012;27(suppl_1):i23–i34. doi: 10.1093/heapol/czs018. [DOI] [PubMed] [Google Scholar]
- 38.StataCorp . StataCorp LLC; College Station, TX: 2017. Stata Statistical Software: Release 15. [Google Scholar]
- 39.Bayati M., Mehrolhassani M.H., Yazdi-Feyzabadi V. A paradoxical situation in regressivity or progressivity of out of pocket payment for health care: which one is a matter of the health policy maker's decision to intervention? Cost Effect Resour Alloc. 2019;17(1):28. doi: 10.1186/s12962-019-0197-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.El Omari S., Karasneh M. Social health insurance in the Philippines: do the poor really benefit? J Econ Financ. 2021;45(1):171–187. [Google Scholar]
- 41.van Hees S.G.M., O'Fallon T., Hofker M., et al. Leaving no one behind? Social inclusion of health insurance in low- and middle-income countries: a systematic review. Int J Equity Health. 2019;18(1):134. doi: 10.1186/s12939-019-1040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kusuma Y.S., Pal M., Babu B.V. Health insurance: awareness, utilization, and its determinants among the Urban Poor in Delhi, India. J Epidemiol Glob Health. 2018;8(1-2):69–76. doi: 10.2991/j.jegh.2018.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kotoh A.M. Van der Geest S. Why are the poor less covered in Ghana's national health insurance? A critical analysis of policy and practice. Int J Equity Health. 2016;15(1):34. doi: 10.1186/s12939-016-0320-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ekawati F.M., Claramita M. Indonesian general practitioners’ experience of practicing in primary care under the implementation of universal health coverage scheme (JKN) J Prim Care Community Health. 2021;12 doi: 10.1177/21501327211023707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Satibi S., Andayani T.M., Endarti D., Suwantara I.P.T., Agustini N.P.D. Comparison of real cost versus the indonesian case base groups (INA-CBGs) tariff rates among patients of high- incidence cancers under the national health insurance scheme. Asian Pac J Cancer Prev. 2019;20(1):117–122. doi: 10.31557/APJCP.2019.20.1.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yu C.P., Whynes D.K., Sach T.H. Equity in health care financing: the case of Malaysia. Int J Equity Health. 2008;7(1):15. doi: 10.1186/1475-9276-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kementerian Keuangan [Ministry of Finance]. Pemerintah Tetapkan Kebijakan Tarif Cukai Hasil Tembakau Tahun 2021 [The Government Sets the Tobacco Excise Tariff Policy in 2021] Jakarta: Ministry of Finance; 2020. https://www.kemenkeu.go.id/media/16913/sp-96_pemerintah-tetapkan-kebijakan-tarif-cukai-hasil-tembakau-tahun-2021.pdf. Accessed 13 January 2021.
- 48.Sreeramareddy C.T., Harper S., Ernstsen L. Educational and wealth inequalities in tobacco use among men and women in 54 low-income and middle-income countries. Tob Control. 2018;27(1):26–34. doi: 10.1136/tobaccocontrol-2016-053266. [DOI] [PubMed] [Google Scholar]
- 49.Martin G.R. Department of Economics Working Papers 2019_01. Universidad Torcuato Di Tella; 2019. Increasing Cigarette Taxes is Unfair to the Poor? Evidence from Argentina.https://ideas.repec.org/p/udt/wpecon/2019_01.html [Google Scholar]
- 50.Pratomo DS, Manning C. Structural change and formal sector employment growth in Indonesia: the Australian National University, Arndt-Corden Department of Economics; 2020. https://ideas.repec.org/p/pas/papers/2020-15.html. Accessed 20 June 2021.
- 51.World Bank. Gini index (World Bank estimate) - Indonesia 2021. https://data.worldbank.org/indicator/SI.POV.GINI?locations=ID. Accessed 05 February 2021.
- 52.Kakwani N., Wagstaff A., van Doorslaer E. Socioeconomic inequalities in health: measurement, computation, and statistical inference. J Econom. 1997;77(1):87–103. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.