Abstract
Study Design
A prospective study with a minimum follow-up of 24 months.
Purpose
This study aimed to evaluate the results of minimally invasive anteroposterior surgery for osteoporotic vertebral fractures (OVFs) associated with bony spinal canal compromise in elderly patients.
Overview of Literature
There is a recent increase in the incidence of osteoporosis with OVFs, causing an increasing burden on medical systems.
Methods
The study included 47 patients, of whom 45 completed a minimum of 24-month follow-up. The inclusion criteria were OVF types 3 and 4 according to the osteoporotic fracture classification in patients aged ≥65 years with bony stenosis. The surgical management consisted of anterior corpectomy and decompression using a thoracoscopic or mini-laparotomy approach, together with posterior percutaneous cement-augmented short-segment fixation. Self-reported outcome measures included Visual Analog Scale (VAS) and Oswestry Disability Index (ODI) in the preoperative phase and regular follow-up at a minimum of 24 months. Radiological measures included segmental lordosis, dual-energy X-ray absorptiometry for osteoporosis assessment, and radiological fracture healing.
Results
There were 33 patients with lumbar fracture and 12 patients with thoracic fracture. Thirteen patients had preoperative neurological deficits. The mean age was 77.4±8.3 years. The mean preoperative VAS score was 8.12±1.5, and the mean ODI score was 24.4±8.2. The mean preoperative sagittal Cobb angle was 6.3°±4.2° kyphosis. The mean operative time was 220.3±55.5 minutes, with a mean blood loss of 360.75±200.6 mL. After a mean follow-up of 32.6±6.4 months, the mean VAS significantly improved to 2.3, and the ODI to 12. Only three patients still had a partial neurological deficit. The mean final sagittal Cobb angle was significantly better, with 12.5°±4.3° of lordosis.
Conclusions
Short-segment percutaneous fixation with cement augmentation combined with minimally invasive anterior decompression and corpectomy is a less invasive and safe approach in elderly patients with OVF and canal compromise.
Keywords: Osteoporosis, Fractures, Lumbar, Thoracic, Minimally-invasive, Retroperitoneal, Thoracoscopy, Short-segment, Cement-screws
Introduction
There is a recent increase in the incidence of osteoporosis with osteoporotic vertebral fractures, causing an increasing burden on medical systems [1]. Classification systems were recently developed to assess injury severity and find a suitable treatment algorithm, especially in elderly patients with associated medical comorbidities and increased surgical risk [2–4]. For the lower degrees of fracture, conservative treatment is accepted. However, in higher degrees, especially in the presence of spinal canal stenosis with local kyphosis, surgery is recommended [4–8].
In the presence of spinal canal compromise, additional surgical decompression is necessary. This can be through a posterior or anterior approach. In fractures with an intact posterior column, the posterior approach leads to more destabilization and may lead to extension of the posterior fixation to higher levels to achieve a stable construct. In contrast, the anterior approach leaves the posterior intact elements without injury and allows better reconstruction of the anterior column [5,7,9].
Short-segment posterior fixation of thoracolumbar fractures is biomechanically stable, and many studies proved its efficacy in the case of normal bone quality [10,11]. In osteoporosis, the screw pullout strength is lower, and screw loosening is common. Recently, there is increasing use of bone cement-augmented pedicle screws in the osteoporotic spine. Cement augmentation leads to improved screw purchase and allows it to achieve stable short-segment constructs even in the osteoporotic vertebrae [4,10–12].
In the current study, the surgical treatment of osteoporotic thoracolumbar fractures with spinal canal compromise in elderly patients (≥65 years) through minimally invasive short-segment cement-augmented fixation with anterior decompression and anterior column reconstruction was prospectively evaluated. The clinical and radiological results were assessed for a minimum of 2 years postoperatively.
Materials and Methods
This prospective evaluation of minimally invasive short-segment anteroposterior surgery for thoracolumbar osteoporotic fractures with osseous spinal canal stenosis was initiated in 2014 and extended until 2017, in 4 years. Institutional review board approval was obtained (128-2014). An informed consent was obtained from all participants included in this study before the surgical treatment. For this study, candidates included patients aged ≥65 years with American Society of Anesthesiologists (ASA) score III or less presenting with an osteoporotic thoracolumbar fracture from T5 to L5. Only fractures types 3 or 4—according to the osteoporotic fracture classification [2]—were included when associated with osseous spinal canal stenosis necessitating decompression. The indications of surgery were persistent pain (Visual Analog Scale [VAS] score ≥5) despite conservative therapy in patients without neurological deficits, acute neurological deficits regardless of the pain duration, confirmed spinal canal stenosis in the preoperative magnetic resonance imaging (MRI) and computed tomography (CT), and segmental sagittal profile malalignment.
The exclusion criteria were pathological fractures due to metastasis and spondylodiscitis, fracture–dislocation osteoporotic fracture type 5, and critical general condition not allowing a combined ventrodorsal approach. All included patients had an isolated spine injury and did not have any other associated injuries necessitating surgical intervention. Further exclusion criteria were multi-level fractures, polytrauma and injury to other spine segments, and spontaneous spine fusion, such as diffuse idiopathic skeletal hyperostosis syndrome and ankylosing spondylitis.
1. Preoperative workup
All patients underwent radiological examinations before surgical treatment, including plain radiography, CT, and MRI of the spine’s affected region. Extension lateral-view radiography was performed in patients without neurological deficits to assess the kyphotic deformity’s flexibility in the fracture site. Anterior-posterior and lateral-view radiography was performed in addition to a whole spine standing radiography.
Segmental lordosis or kyphosis was measured in the preoperative images. Measurement of the local kyphotic angle was from the upper surface of the adjacent distal intact vertebra to the upper surface of the adjacent proximal intact vertebra (Fig. 1). An independent radiologist evaluated the segmental lordosis or kyphosis in the preoperative and follow-up radiography. Dual-energy X-ray absorptiometry (DEXA) was additionally performed to determine the presence of osteoporosis or osteopenia. Neurological examination was performed in every case by an independent neurologist. Each patient was assigned a score according to the ASA to evaluate the expected risk during the surgical procedure. Patients were clinically evaluated with the VAS to quantify pain intensity and the low back disability questionnaire “Oswestry Disability Index” (ODI).
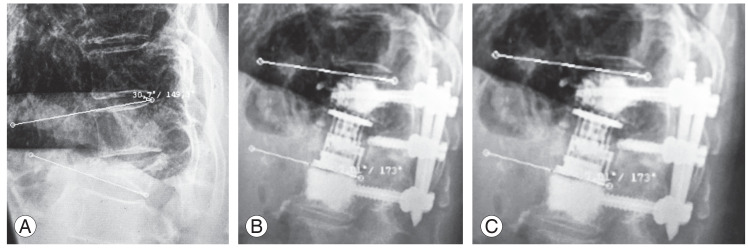
Fig. 1.
Measurement of segmental kyphosis or lordosis. From the upper surface of the distal adjacent intact vertebra to the proximal adjacent vertebra’s upper surface. Preoperative radiograph (30° kyphosis) (A), immediate postoperative radiograph (7° lordosis) (B), and final follow-up radiograph (7° lordosis) (C).
2. Operative technique
1) Anterior approach
In the thoracic spine, a biportal video-assisted thoracoscopic surgery (VATS) in the prone position was performed for corpectomy, decompression of the spinal canal, and vertebral body replacement using an expandable titanium implant (Fig. 2). Biportal VATS was performed in all thoracic and upper lumbar regions to L1, one portal was used for the camera, and the other working portal was a mini-thoracotomy of 2.5 cm, which was planned according to the fracture level and position of the great vessels. Usually, a left-sided approach was used from T10 to L1, and a right-sided approach for levels above T10. An expandable titanium implant was used as a vertebral body replacement; the implant was filled with the collected bone during corpectomy.
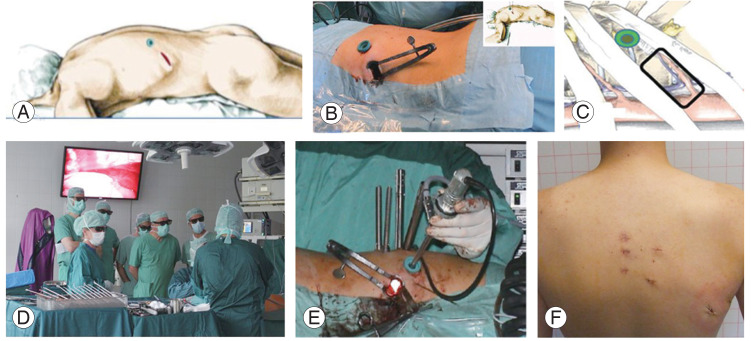
Fig. 2.
Video-assisted thoracoscopic surgery, planning of the incisions (A), two-portal approach for light (small) and instruments (larger) (B), a schematic image for the anatomical landmarks (C), arrangement of the operating room with monitoring of the patient and position of the surgical team (D), intraoperative image of the approach (E), and follow-up clinical image showing the scares of the thoracoscope and percutaneous screws (F).
In the lumbar spine, left-sided mini-laparotomy was performed, and a retroperitoneal approach was used to access the targeted level, decompress the spinal canal, and replace the fractured vertebral body using an expandable titanium implant again. The mini-laparotomy was performed in the supine position for L4 and L5. The L2 and L3 were operated in the lateral decubitus position.
2) Posterior approach
In the prone position, percutaneous bisegmental cannulated screw fixation was performed under the guidance of two perpendicular C-arms. Two short pedicle screws were inserted in the pedicles of the fractured vertebra. The screws in the proximal and distal vertebrae were augmented using high viscosity bone cement. The amount of injected cement depended on the fracture level. In the thoracic area, a maximum amount of 6 mL (3 mL in each screw) was used, and in the lumbar area, a maximum amount of 8 mL was used (4 mL in each screw). In the case of cement leakage, the injection was stopped immediately regardless of the amount of injected bone cement. These values were adopted based on previously published work [13].
3. Postoperative workup
An ambulation and rehabilitation program was started on the first postoperative day. No orthosis was used postoperatively. Plain radiography was performed on the first day and the day before discharge (5–10 days according to the patient’s general condition and neurological status). The postoperative segmental kyphosis or lordosis angles were measured and recorded. The VAS score was recorded daily during the hospital stay to regulate the analgesic dose, and the ODI score was evaluated before discharge. Subsequently, regular follow-up visits were scheduled after 3, 6, 12 months and then yearly. In these visits, radiography and clinical examinations were performed, including VAS and ODI. The sagittal profile was analyzed in lateral radiography and recorded.
Furthermore, bone healing and presence of any implant-related complications were recorded. The minimum follow-up duration for the included patients in this study was 2 years. Bone healing was assessed using digital radiographic analysis of the regular postoperative follow-up. Healing was confirmed according to four radiological and clinical criteria: bridging bone anteriorly or through the implant (Fig. 3), absence of screw loosening or lucency between implant endplate and adjacent vertebrae, absence of deterioration of segmental kyphotic angle (<5°), and, clinically, absence of instability symptoms.
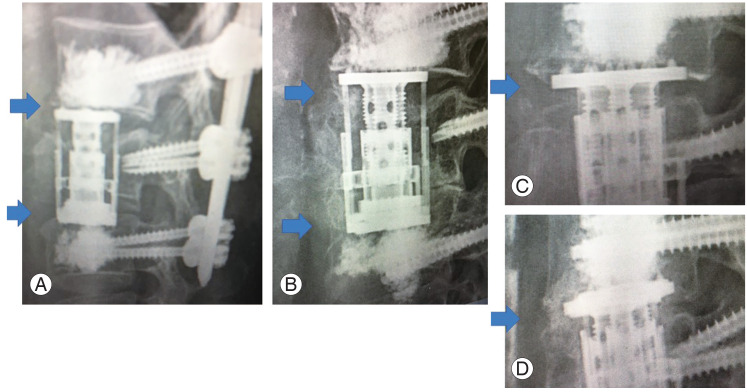
Fig. 3.
Assessment of healing and fusion. The arrows show the interface between the implant and adjacent vertebral endplate. Postoperative radiograph without bridging bone (A), follow-up radiograph after 18 months showing bridging bone through the whole anterior aspect of the implant (B), magnified image at the endplate showing postoperative position without fusion (C), and after 24 months with bridging fusion (D).
4. Data analysis
The collected data were analyzed using the IBM SPSS ver. 19.0 (IBM Corp., Armonk, NY, USA). Time until fracture healing, changes in the sagittal profile during healing, reoperations, and clinical parameters according to the ODI and VAS scores were calculated and compared in the study’s different phases. Demographic data were assessed using mean, range, and standard deviation. The changes in the sagittal profile, VAS score, and ODI score were assessed using Student t-test, and the significance was set at a p-value of 0.05.
Results
1. Demographic data
The surgical procedure was performed in 47 consecutive patients in the study period. Two patients died in the first year postoperatively due to non-related medical causes and did not complete the 2-year follow-up. They were consequently excluded from the final results. The remaining 45 patients consisted of 25 women (55.5%) and 20 men (44.5%). The mean age at surgery was 77.4±8.3 years. Thirty-three patients had lumbar fracture, and 12 had thoracic fracture. In 13 patients (28.9%), a preoperative neurological deficit was documented. Partial cauda equina lesion was observed in eight patients, and radiculopathy in five patients. The injury mechanism was a low grade in 30 patients, and a medium-high grade in ten. In the remaining five patients, the fracture occurred spontaneously without associated trauma. During the study period, another 37 patients were managed in our department due to osteoporotic fractures with spinal canal stenosis but had one or more exclusion criteria and hence were not analyzed in this study (Figs. 4, 5).
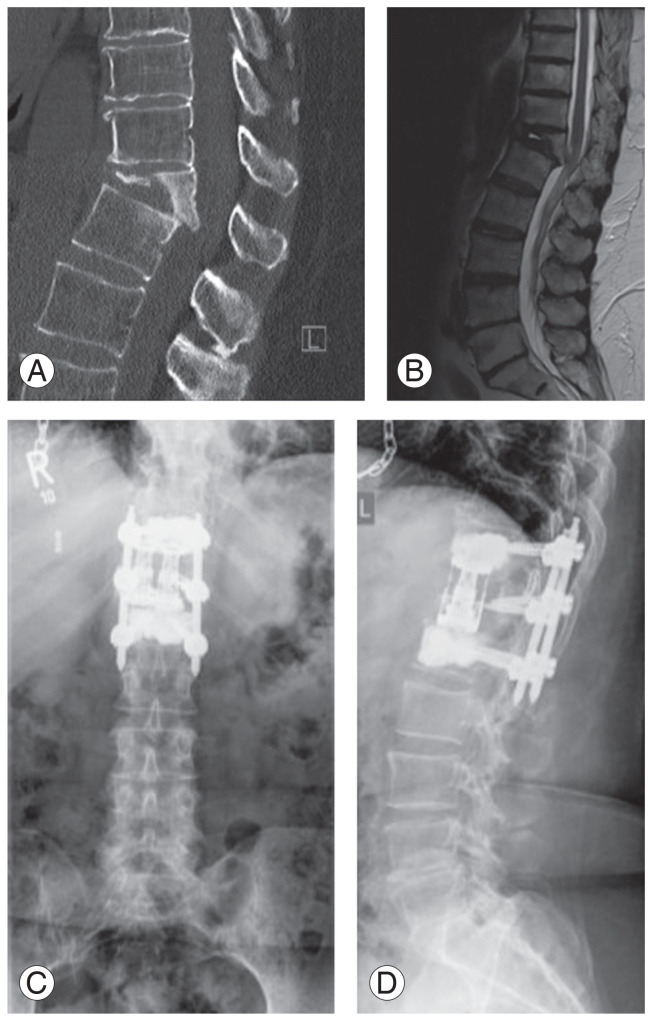
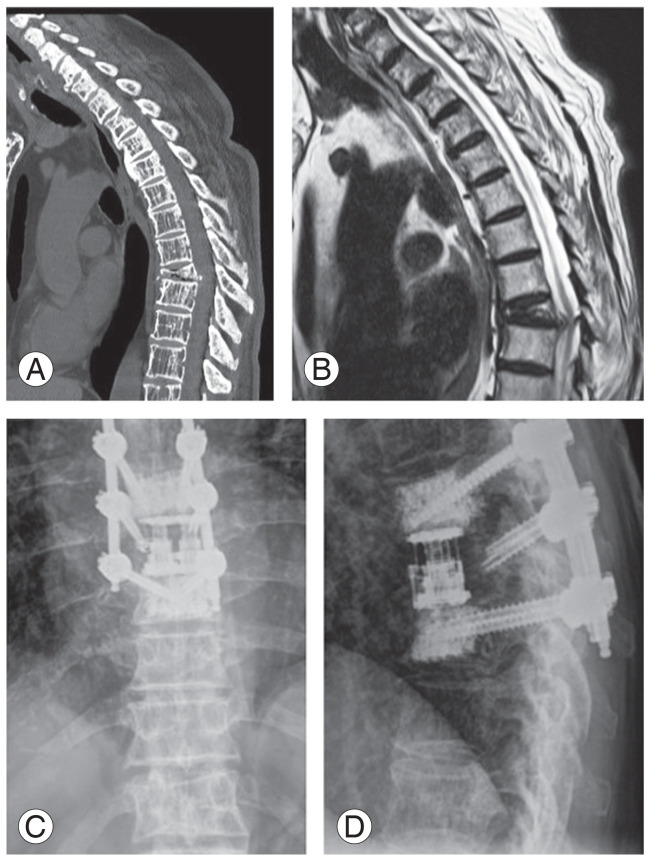
Fig. 4.
Computed tomography (A) and magnetic resonance imaging (B) of a 69-year-old woman showing an osteoporotic fracture T12 with canal compromise and segmental kyphosis. Anterior thoracoscopic corpectomy with decompression of the spinal canal and vertebral body replacement together with posterior short-segment fixation and cement augmentation was performed. Postoperative radiograph shows good correction of the kyphosis (C) with good maintenance of the correction after 3 years of follow-up (D).
Fig. 5.
A 71-year-old woman presenting with incomplete paraplegia due to osteoporotic fracture T8 with canal stenosis. Computed tomography shows the bony stenosis and osteoporosis (A). Magnetic resonance imaging shows the absolute spinal canal stenosis (B). Postoperative anteroposterior and lateral radiographs (C) after anterior thoracoscopic corpectomy and decompression and posterior short-segment cement-augmented fixation. (D) Complete postoperative recovery of the paraplegia was achieved with a stable construct over a 28-month follow-up.
2. Preoperative data
Preoperatively, the mean VAS score was 8.12±1.5, and the mean ODI score was 24.4±8.2. In preoperative lateral radiography, the mean segmental Cobb angle was 6.3°±4.2° kyphosis (range, 5° lordosis to 25° kyphosis). The mean DEXA t-score was −2.1±0.8 (range, −1.7 to −2.8). In all patients, spinal canal bone stenosis was confirmed by both CT and MRI. According to the osteoporotic fracture classification, 12 patients (26.6%) had type 3, and 33 patients (73.4%) had type 4. Surgery was performed after admission by a mean of 2.5±1.7 days (range, 0 to 4 days) (Table 1).
Table 1.
Epidemiological and demographic data of the studied patients
| Characteristic | Value |
|---|---|
| No. of patients | 45 |
| Age (yr) | 77.4±8.3 (range, 65 to 84) |
| Gender | |
| Female | 25 |
| Male | 20 |
| Fracture level | |
| Lumbar | 33 |
| Thoracic | 12 |
| Approach | |
| VATS | 18 (12 thoracic and 8 L1) |
| Mini-lumbotomy (L2 to L5) | 27 |
| T-score (DEXA scan) | −2.1±0.8 (range, −1.7 to −2.8) |
| Operation time (min) | 220.3±55.5 |
| Blood loss (mL) | 360.75±200.6 |
| Neurological status | |
| Preoperative | 13 |
| End of follow-up | 3 |
| Bladder paralysis | 1 |
| Foot drop (L5 radiculopathy) | 1 |
| ASIA C at the level Th8 | 1 |
| Follow-up period (mo) | 32.6±6.4 |
| Complications | 2 (4.4) |
| Pneumonia | 1 |
| Contra-lateral pleural effusion | 1 |
| Reoperations | 2a) |
Values are presented as number, mean±SD (range), mean±SD, or number (%), unless otherwise stated.
SD, standard deviation; VATS, video-assisted thoracoscopic surgery; DEXA, Dual-energy X-ray absorptiometry; ASIA, American Spinal Injury Association.
Adjacent segment fractures treated by vertebroplasty (Fig. 1).
3. Intraoperative profile
Anterior corpectomy was performed thoracoscopically in the prone position for the thoracic and upper lumbar regions to L1 (18 patients), lateral decubitus position for L2 and L3 (19 patients), and supine position for L4 and L5 (eight patients). In all patients, posterior percutaneous fixation and cement augmentation of the screws were performed in the prone position in the same setting. The mean operative time was 220±80 minutes. The mean blood loss was 360±350 mL. There were no intraoperative complications.
4. Postoperative data
The mean postoperative hospital stay was 10±4 days. In the direct postoperative radiography, the segmental Cobb angle improved to a mean of 13.5°±6.3° of lordosis, and this change was statistically significant (t=2.3 and p=0.02). The mean postoperative VAS score on discharge significantly improved to 5.4±2.1 (t=2.4 and p=0.01). Five patients showed complete neurological recovery during the hospital stay. In-hospital complications developed in two patients (4.4%). One patient had mild postoperative pneumonia and was treated with antibiotics and stayed for 3 days in the intermediate care unit. Another patient developed contralateral pleural effusion postoperatively and was managed by drainage with a chest tube for 3 days.
5. Final follow-up
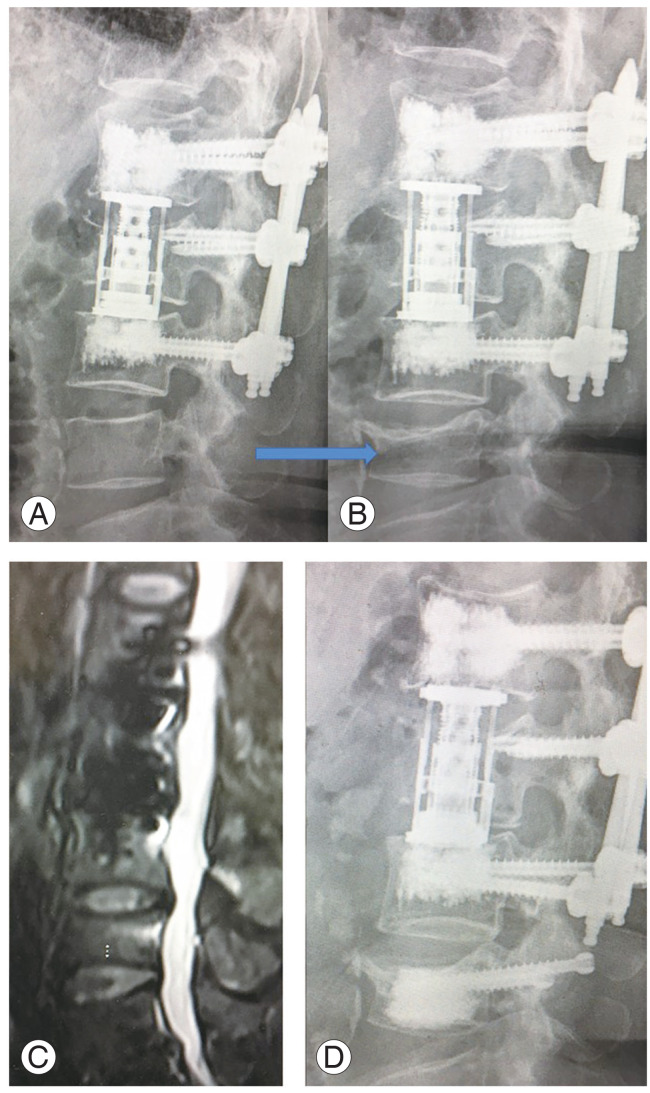
After a mean follow-up of 32.6±8.4 months, there was a significant improvement in the mean VAS score to 2.3±2 (t=3.2 and p=0.02). The mean ODI score improved to 12.6±6.5 (t=3.4 and p=0.03). At the end of the follow-up, only three patients still had partial neurological deficit. One of them still had urinary bladder paralysis and was managed using a self-catheter. The second patient had a foot drop due to the L5 root’s motor paralysis on the right side. The last patient had American Spinal Injury Association (ASIA) C spinal cord paralysis at the level of T8, which was improved from preoperative ASIA B paralysis. The segmental sagittal Cobb angle was significantly improved at a mean of 12.5°±4.3° lordosis (p=0.001). The mean loss of segmental lordosis correction in the follow-up period was 2.5°±2.3°, and this was not statistically significant (t=3.2 and p=0.52). No postoperative infection was recorded in any of the patients. There were no revisions due to mechanical complications. Two patients presented after a mean of 3 months with adjacent vertebra fracture and were treated with vertebroplasty (Fig. 6).
Fig. 6.
Adjacent vertebral osteoporotic fracture occurred after 3 months (arrow). Immediate postoperative radiograph (A), radiographs after 3 months showing adjacent vertebral fracture caudally (B), magnetic resonance imaging showing vertebral body edema due to fracture (C), and radiography showing cement augmentation of the adjacent vertebra (D).
Healing was achieved in 42 patients (four criteria of healing mentioned in the Methods section) after a mean of 9.3±3.6 months. The remaining three patients (6.6%) did not achieve all criteria of healing: two patients’ screw loosening was observed after 10 and 14 months, and in the third patient, worsening of the sagittal profile was up to 10°. All three patients had mild symptoms (VAS score ≤3) and were managed conservatively.
Discussion
1. Surgical versus conservative treatment
Osteoporotic thoracolumbar fractures are becoming more common with aging of the population. Most of these fractures are conservatively treated [8]. However, the combination of spinal instability with vertebral collapse and retropulsion of bony fragments in the spinal canal is an indication for surgery among most investigators [5–8,10]. McLain [11] reported that operative treatment offers several advantages in such cases: First, immediate orthosis-free spinal stability is provided to prevent prolonged recumbency. Second, surgical treatment more reliably restores sagittal alignment. Finally, surgical decompression more reliably restores neurologic function and decreases rehabilitation time [11]. A similar recommendation was published by Muratore et al. [4], who performed a systematic review to analyze the predictive factors for conservative treatment failure in OVFs. One of these factors was neurological impairment with a retropulsed bone fragment in the spinal canal. The data obtained in the current study supports these facts. Our patients started ambulation and rehabilitation on the first postoperative day without the need for an orthosis. The mean sagittal Cobb angle significantly improved postoperatively by 18.5°. Again, most patients presenting with neurological deficits significantly improved postoperatively. These three aspects highlight the beneficial effects of surgery in this specific group of patients.
2. Anterior column support
Once the decision for surgery is made, it is important to find the best suitable technique to achieve the surgical goals and avoid future problems in this fragile group of patients with this specific type of injury. Nakashima et al. [8] compared the surgical results of anteroposterior combined surgery and posterior fixation with vertebroplasty for treating osteoporotic delayed vertebral collapse. They concluded that the addition of anterior cage support provides more stable spinal fixation and reduces implant failure. Similarly, Wei et al. [14] evaluated the relative benefits of posterior fixation combined with vertebroplasty or vertebral column resection (VCR) for osteoporotic vertebral compression fractures with intravertebral cleft complicated by neurological deficits. Again, they concluded that the anterior column support through the posterior VCR significantly achieved more long-term pain relief, vertebral height maintenance, and deformity correction. The surgical technique applied in this study is in line with the publications favoring anterior column support, as no mechanical complications needing revision were recorded. The advantage of the technique applied in our series is its minimally invasive nature and its complete preservation of the posterior column integrity, which cannot be achieved during VCR. This led Wei et al. [14] to compensate for this deficiency by extending the posterior instrumentation over several levels, which was unnecessary for our work, in which all patients underwent only bisegmental fixation.
3. Decompression
Another advantage of the anterior approach is the direct removal of the retropulsed bone fragments from the anterior approach, thus addressing the pathology from the site of pathology. This concept avoids the removal of intact posterior structures just for approach purposes. Studies on this concept in osteoporotic fractures are limited. Theologis et al. [15] applied the same concept but for traumatic burst fractures. They performed anterior corpectomy combined with a short-segment posterior fixation for single-level traumatic lumbar burst fractures. Similarly, Walker et al. defined two indications for the anterior approach in traumatic fractures, namely, neural compromise and need for anterior column support [16]. These two indications were also included in all patients.
The alternative to this concept is performing decompression through posterior laminotomy or laminectomy, as reported by Piccone et al. [17]. They performed decompression and stabilization using the posterior surgical approach alone in thoracolumbar burst fractures with stenosis and reported good results. However, all patients were aged <40 years. It is possible to extend the instrumentation at this young age, as later partial implant removal is possible when necessary. In our opinion, addressing anterior stenosis through a posterior approach weakens the intact posterior column in a patient with unstable anterior column. In osteoporosis, the associated longer segment instrumentation would unnecessarily transfer possible mechanical problems into the intact vertebrae.
Moreover, a second later surgery for implant removal or shortening exposes these fragile elderly patients to an avoidable second surgery. In the current series, no second surgery related to screw placement was needed in any of the patients. Only two patients presented later by adjacent vertebral osteoporotic fracture, which was successfully augmented.
4. Posterior short-segment instrumentation
Waqar et al. [18] compared short- versus long-segment fixation in the treatment of thoracolumbar fractures in a series of 28 patients. They identified a trend toward better clinical and radiological outcomes in the long-segment group than in the short-segment group.
To save segments of vertebral motion, Wahba et al. [19] suggested cross-links to short-segment constructs to obtain more stability. They analyzed the biomechanical results in a human cadaveric unstable thoracolumbar burst fracture model and found that cross-links to short-segment posterior fixation improved stiffness and decreased motion in axial rotation [19]. However, this idea was not applicable in our study, as the posterior instrumentation was conducted in a minimally invasive percutaneous technique, which does not allow insertion of cross-links.
Another way to save mobile segments is to add pedicle fixation at the fracture level. Mahar et al. [10] underwent a cadaveric biomechanical study in six human spines and additionally reviewed the clinical results in 12 patients with an unstable thoracolumbar fracture to evaluate this technique. They found that short-segment fixation with additional screws at the fracture level offers improved stability. Dobran et al. [20] compared the use of long-segment fixation versus short-segment fixation with the fracture level inclusion in a series of 60 patients with unstable thoracolumbar fracture. They concluded that inclusion of fracture level in a short-segment fixation results in kyphosis correction and maintenance of the sagittal alignment similar to long-segment instrumentation, which allowed them to save two or more segments of vertebral motion. The same conclusion was obtained by Ahsan et al. [21], which again compared the two constructs retrospectively in 88 patients with unstable thoracolumbar fractures. To obtain the benefit of this fact, we added short pedicle screws also inserted percutaneously at the fracture level in all patients. With the anterior column support, this type of short-segment fixation offered a stable construct until the end of the follow-up.
5. Cement augmentation of the screws
Most previously mentioned studies dealt with traumatic thoracolumbar fractures at a young age. The reduced bone quality in the elderly patients included in our study was not a barrier to apply the principle of short-segment instrumentation. However, this would not have been possible without the addition of bone cement in the adjacent vertebrae. This was applied through the cannulated and fenestrated pedicle screws and achieved two main functions: First, augmentation of the screws improved the purchase in the osteoporotic vertebral bone. Second, the application of bone cement with good distribution, especially near the endplates, prevented cage subsidence, allowing minimal loss of segmental lordosis correction over the follow-up period by a mean of 2.5°±2°. These results coincide with those obtained by Singh et al. [22] in their systematic review on cement-augmented pedicle screws in osteoporosis of the spine. They concluded at the end of their analysis that cement-augmented screws have better immediate stability through improved anchorage, improving the radiological parameters by achieving minimal correction loss at the end of follow-up.
6. Limitation of the study
This study has some limitations: absence of a control group managed using another surgical technique and relatively few patients (n=45). The results were compared with the published literature using conventional methods of decompression and open posterior fixation. The study period was designed to be 4 years, and we continued to perform this procedure; the results of a larger patient cohort will be evaluated in the future.
Conclusions
Percutaneous short-segment cement-augmented instrumentation combined with minimally invasive anterior decompression and vertebral body replacement is a less invasive, effective, and safe approach in elderly patients with osteoporotic spinal fracture and canal compromise. The combination of anterior column support, cement augmentation, and short pedicle screws at the fracture level achieved good restoration of the sagittal alignment and allowed its maintenance until the end of follow-up, with the advantage of saving mobile segments.
Footnotes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Mohamed Alhashash: study idea, study design, operative management of the patients, data collection, literature review, writing the manuscript, and editing the manuscript. Mootaz Shousha: operative management of the patients, statistical analysis, revision of the manuscript, and critical reviewing of the manuscript.
References
- 1.Hadji P, Klein S, Gothe H, et al. The epidemiology of osteoporosis--Bone Evaluation Study (BEST): an analysis of routine health insurance data. Dtsch Arztebl Int. 2013;110:52–7. doi: 10.3238/arztebl.2013.0052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schnake KJ, Blattert TR, Hahn P, et al. Classification of osteoporotic thoracolumbar spine fractures: recommendations of the spine section of the German Society for Orthopaedics and Trauma (DGOU) Global Spine J. 2018;8(2 Suppl):46S–49S. doi: 10.1177/2192568217717972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schnake KJ, Bula P, Spiegl UJ, et al. Thoracolumbar spinal fractures in the elderly: classification and treatment. Unfallchirurg. 2017;120:1071–85. doi: 10.1007/s00113-017-0435-x. [DOI] [PubMed] [Google Scholar]
- 4.Muratore M, Ferrera A, Masse A, Bistolfi A. Osteoporotic vertebral fractures: predictive factors for conservative treatment failure: a systematic review. Eur Spine J. 2018;27:2565–76. doi: 10.1007/s00586-017-5340-z. [DOI] [PubMed] [Google Scholar]
- 5.Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J. 2006;6:479–87. doi: 10.1016/j.spinee.2006.04.013. [DOI] [PubMed] [Google Scholar]
- 6.Patil S, Rawall S, Singh D, et al. Surgical patterns in osteoporotic vertebral compression fractures. Eur Spine J. 2013;22:883–91. doi: 10.1007/s00586-012-2508-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sudo H, Ito M, Kaneda K, et al. Anterior decompression and strut graft versus posterior decompression and pedicle screw fixation with vertebroplasty for osteoporotic thoracolumbar vertebral collapse with neurologic deficits. Spine J. 2013;13:1726–32. doi: 10.1016/j.spinee.2013.05.041. [DOI] [PubMed] [Google Scholar]
- 8.Nakashima H, Imagama S, Yukawa Y, et al. Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. Spine (Phila Pa 1976) 2015;40:E120–6. doi: 10.1097/BRS.0000000000000661. [DOI] [PubMed] [Google Scholar]
- 9.Alpantaki K, Dohm M, Korovessis P, Hadjipavlou AG. Surgical options for osteoporotic vertebral compression fractures complicated with spinal deformity and neurologic deficit. Injury. 2018;49:261–71. doi: 10.1016/j.injury.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Mahar A, Kim C, Wedemeyer M, et al. Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine (Phila Pa 1976) 2007;32:1503–7. doi: 10.1097/BRS.0b013e318067dd24. [DOI] [PubMed] [Google Scholar]
- 11.McLain RF. The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine (Phila Pa 1976) 2006;31(11 Suppl):S70–9. doi: 10.1097/01.brs.0000218221.47230.dd. [DOI] [PubMed] [Google Scholar]
- 12.Girardo M, Rava A, Fusini F, Gargiulo G, Coniglio A, Cinnella P. Different pedicle osteosynthesis for thoracolumbar vertebral fractures in elderly patients. Eur Spine J. 2018;27(Suppl 2):198–205. doi: 10.1007/s00586-018-5624-y. [DOI] [PubMed] [Google Scholar]
- 13.Alhashash M, Shousha M, Barakat AS, Boehm H. Effects of polymethylmethacrylate cement viscosity and bone porosity on cement leakage and new vertebral fractures after percutaneous vertebroplasty: a prospective study. Global Spine J. 2019;9:754–60. doi: 10.1177/2192568219830327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wei H, Dong C, Zhu Y. Posterior fixation combined with vertebroplasty or vertebral column resection for the treatment of osteoporotic vertebral compression fractures with intravertebral cleft complicated by neurological deficits. Biomed Res Int. 2019;2019:4126818. doi: 10.1155/2019/4126818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Theologis AA, Tabaraee E, Toogood P, et al. Anterior corpectomy via the mini-open, extreme lateral, transpsoas approach combined with short-segment posterior fixation for single-level traumatic lumbar burst fractures: analysis of health-related quality of life outcomes and patient satisfaction. J Neurosurg Spine. 2016;24:60–8. doi: 10.3171/2015.4.SPINE14944. [DOI] [PubMed] [Google Scholar]
- 16.Walker CT, Xu DS, Godzik J, Turner JD, Uribe JS, Smith WD. Minimally invasive surgery for thoracolumbar spinal trauma. Ann Transl Med. 2018;6:102. doi: 10.21037/atm.2018.02.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Piccone L, Cipolloni V, Nasto LA, et al. Thoracolumbar burst fractures associated with incomplete neurological deficit in patients under the age of 40: is the posterior approach enough?: surgical treatment and results in a case series of 10 patients with a minimum follow-up of 2 years. Injury. 2020;51:312–6. doi: 10.1016/j.injury.2019.12.031. [DOI] [PubMed] [Google Scholar]
- 18.Waqar M, Van-Popta D, Barone DG, Bhojak M, Pillay R, Sarsam Z. Short versus long-segment posterior fixation in the treatment of thoracolumbar junction fractures: a comparison of outcomes. Br J Neurosurg. 2017;31:54–7. doi: 10.1080/02688697.2016.1206185. [DOI] [PubMed] [Google Scholar]
- 19.Wahba GM, Bhatia N, Bui CN, Lee KH, Lee TQ. Biomechanical evaluation of short-segment posterior instrumentation with and without crosslinks in a human cadaveric unstable thoracolumbar burst fracture model. Spine (Phila Pa 1976) 2010;35:278–85. doi: 10.1097/BRS.0b013e3181bda4e6. [DOI] [PubMed] [Google Scholar]
- 20.Dobran M, Nasi D, Brunozzi D, et al. Treatment of unstable thoracolumbar junction fractures: short-segment pedicle fixation with inclusion of the fracture level versus long-segment instrumentation. Acta Neurochir (Wien) 2016;158:1883–9. doi: 10.1007/s00701-016-2907-0. [DOI] [PubMed] [Google Scholar]
- 21.Ahsan MK, Mamun AA, Zahangiri Z, et al. Short-segment versus long-segment stabilization for unstable thoracolumbar junction burst fractures. Mymensingh Med J. 2017;26:762–74. [PubMed] [Google Scholar]
- 22.Singh V, Mahajan R, Das K, Chhabra HS, Rustagi T. Surgical trend analysis for use of cement augmented pedicle screws in osteoporosis of spine: a systematic review (2000–2017) Global Spine J. 2019;9:783–95. doi: 10.1177/2192568218801570. [DOI] [PMC free article] [PubMed] [Google Scholar]