Abstract
Objectives:
To compare upper eyelid blepharoplasty patients’ suture techniques with interrupted cutaneous in one eye and running cutaneous in the other in terms of edema, ecchymosis, and scar index.
Methods:
Among patients whose suture techniques with interrupted cutaneous in one eye and running cutaneous in the other, 34 patients in the vicryl group and 46 patients in the polypropylene group were included in the study. The patients’ edema and ecchymosis levels on postoperative days 1, 7, and 30 days and 3 months were selected. The Manchester Scar Scale was used to evaluate the scar index at 30 days and 3 months after surgery. Suture material (either 6-0 polypropylene sutures or 6-0 vicryl sutures) were evaluated independently.
Results:
In vicryl group, there was significantly less ecchymosis and edema first week postoperatively in interrupted sutured eyelid than running sutured eyelid (p=0.001, p=0.011, respectively). In polypropylene group, there was significantly less ecchymosis at the first day and first week postoperatively in interrupted sutured eyelid than running sutured eyelid (p=0.025, p=0.001, respectively). The total scar index scores in both groups at first month and third month were significantly better at the interrupted sutured eyelid than running sutured eyelid (p<0.05, for all).
Conclusion:
In upper eyelid blepharoplasty, an interrupted suture technique yielded the lowest rates of edema, ecchymosis, and scar formation compared with a running suture technique.
Keywords: Interrupted, running, suture, upper eyelid blepharoplasty
Introduction
Aging is an unavoidable phenomenon, and it undeniably brings substantial alterations all over the body. Face and eyes are the most remarkable areas. Their age-related changes such as brow ptosis, dermatochalasis, blepharochalasis, periorbital wrinkles, and fat pads under the eyes will become so prominent that they lead to significant physical and psychological problems (1, 2). Therefore, a surgical procedure by which the eyelid skin, orbicularis oculi muscle, and orbital fat are excised or sculpted to rejuvenate the aesthetic look of the patient called blepharoplasty has become one of the most common procedures employed for facial rejuvenation and beautification (3, 4).
Blepharoplasty can be performed successfully when performed for the correct indications. However, complications such as edema, infection, asymmetry secondary to excessive or insufficient excision of skin, muscle, or fat, and unsightly scarring are infrequent but are highly important for patients’ satisfaction (4, 5). Although scarring is among the most common and unwanted complications associated with blepharoplasty that affect patients’ satisfaction, there is not a consensus on the precise cutting technique or cutting instruments used, the techniques and materials used for the closure of blepharoplasty incisions in the literature (1, 2, 4). Materials commonly used for closure include vicryl, polypropylene, nylon, fast-absorbing gut, and ethyl cyanoacrylate adhesives, and techniques frequently used are subcutaneous continues, interrupted cutaneous, and running cutaneous (3, 4, 6–8). All these materials and techniques can be used safely, but it seems that the selection of technique and material relies largely on the surgeon’s personal preference.
Although blepharoplasty has a high rate of patient satisfaction, there are subtleties in closure techniques that affect outcomes. Previously reported articles evaluated the complications and scar formation of different suture materials and techniques (6–8), but the effect of the interrupted cutaneous and running cutaneous suture techniques on the postoperative edema, ecchymosis, and scar index was not studied before. In light of these findings, we aimed to compare the results of the upper eyelid blepharoplasty patients’ suture techniques with interrupted cutaneous in one eye and running cutaneous in the other in terms of edema, ecchymosis, and scar index.
Methods
This prospective cross-sectional study was carried out in the Department of Ophthalmology at the Adıyaman University Training and Research Hospital. The study protocol was approved by the Adıyaman University clinical research ethics committee (Approval number: 2021-3-4, Approval date: February 11, 2021), and the study was carried out in accordance with the Declaration of Helsinki. Informed written consent was obtained from the participants prior to their admission into the study.
Patients who planned for upper eyelid blepharoplasty and whose suture techniques included interrupted cutaneous in one eye and running cutaneous in the other were selected for the study. Patients with previous blepharoplasties, diseases that may affect wound healing such as diabetes, connective tissue disorders, and patients using anticoagulants or anti-inflammatory drugs were excluded. Patients who have not attended control visits and those with missing data were also excluded from the study.
All blepharoplasty surgeries were performed by the same surgeon (EA) with the same surgery technique. Before the operation, incision lines were marked with a waterproof pencil. All the operations were performed under local anesthesia. After the skin had been disinfected, skin infiltration was performed with lidocaine 2% (Xylocaine; AstraZeneca BV, Zoetermeer, The Netherlands) with 1:100,000 epinephrine. Skin incision and subcutaneous layer were incised with high-frequency radiosurgery. Meticulous hemostasis was performed via monopolar coagulation. During the operation, the septum was then either simply cauterized using unipolar needlepoint cautery or buttonholed to expose the nasal and medial fat pads. If necessary, fat was excised with needlepoint cautery. Hemostasis was obtained. Finally, the wound was closed with a running cutaneous style in one eye and interrupted cutaneous in the other with the same suture material either 6-0 polypropylene sutures or 6-0 vicryl sutures. Randomization was performed to determine on which upper eyelid the suture was interrupted and on which upper eyelid it was running. After the operation, cooling packs were applied to both eyelids. The sutures were removed after 7 days. The preoperative and immediate postoperative image of a patient who has undergone upper eyelid blepharoplasty is shown in Figure 1.
Figure 1.

Preoperative and immediate postoperative image of a patient who has undergone upper eyelid blepharoplasty. The suturing was performed as interrupted in the right upper eyelid and running in the left upper eyelid.
In our clinic, patients underwent extensive perioperative and postoperative evaluation, along with photo documentation, at 1 day, 1 week, 1 month, 3 months, and 6 months, and every 6 months thereafter (9). Each patient was evaluated for edema and ecchymosis independent of postoperative days 1, 7, and 30 and 3 months using a Likert scale (9). The scars were also measured after 1 month and 3 months using the Manchester Scar Scale. The scale includes: (i) color (1: perfect, 2: slight mismatch, 3: obvious mismatch, 4: gross mismatch); (ii) matte versus shiny (1: matte, 2: shiny); (iii) contour (1: flush with the surrounding skin, 2: slightly proud or indented, 3: hypertrophic, 4: keloid); (iv) distortion (1: none, 2: mild, 3: moderate, 4: severe); and (v) texture (1: normal, 2: just palpable, 3: firm, 4: hard) (10). Complications such as wound infections, milia, and dehiscence, lagophthalmos, ptosis, xerophthalmia, and upper eyelid anomalies were also evaluated. All these measurements were reviewed and selected for statistical comparison. In addition, we grouped the patients according to the suture material used (polypropylene or vicryl), and statistical analysis was done independently for each group.
Statistical Analysis
SPSS, version 22 (IBM Corp, Armonk, NY) was used for the analysis. Edema and ecchymosis were analyzed on postoperative days 1, 3, 7, 14, and 30 using the independent t-test. An independent t-test was also used to analyze the results of the Manchester Scar Index. The results were then analyzed using SPSS, version 22 (IBM Corp, Armonk, NY). P<0.05 was considered to indicate statistical significance.
Results
From the patients who had undergone upper eyelid blepharoplasty, 38 patients in the vicryl group and 48 patients in the polypropylene group were eligible for inclusion. Four patients in the vicryl group and 2 patients in the polypropylene group were excluded from the study because of missing data in their medical records. Finally, 34 patients (22 female, 12 male) in the vicryl group and 46 patients (27 female, 19 male) in the polypropylene group were reviewed for statistical comparison. The mean age in the vicryl group and polypropylene group was 56.7±5.7 years (min: 50, max: 69) and 58.8±5.4 years (min: 49, max: 67), respectively.
Comparison of edema: In the vicryl group, only edema in the first week was better at interrupted sutured eyelid (p=0.011). In the polypropylene group, there were no significant changes between both eyelids in terms of edema (p>0.05, for all).
Comparison of ecchymosis: In the vicryl group, the level of ecchymosis in the interrupted sutured eyelid was significantly less than running sutured eyelid in the first week (p=0.001). In the polypropylene group, there was significantly less ecchymosis at the first day and first week postoperatively in interrupted sutured eyelid than running sutured eyelid (p=0.025, p=0.001, respectively). The edema and ecchymosis levels of both groups are shown in Figure 2.
Figure 2.
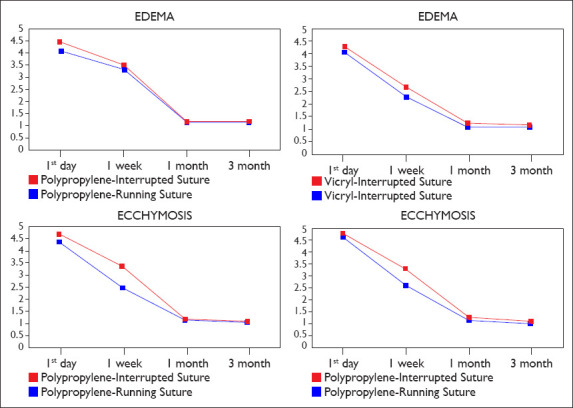
Postoperative alterations in edema and ecchymosis between interrupted and running suture techniques in both suture materials.
The comparison of scar indexes between eyes in both groups is summarized in Table 1. The total scores in both groups at first month and third month were significantly better at the interrupted sutured eyelid than running sutured eyelid (p<0.05, for all). The complications of both groups are shown in Table 2.
Table 1.
Postoperative results of Manchester Scar Index in ınterrupted and running suture techniques in both vicryl and polypropylene groups
| Groups | Vicryl group | Polypropylene group | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Time | 1st month | 3rd month | 1st month | 3rd month | ||||||||
|
|
|
|
|
|
||||||||
| Scar index score | Interrupted suture | Running suture | Interrupted suture | Running suture | Interrupted suture | Running suture | Interrupted suture | Running suture | p1 | p2 | p3 | p4 |
| Color | 1.80±0.6 | 2.20±0.4 | 1.05±0.2 | 1.30±0.4 | 1.65±0.6 | 2.05±0.3 | 1.05±0.2 | 1.35±0.4 | 0.045 | 0.038 | 0.025 | 0.017 |
| Matte vs Shiny | 1.15±0.3 | 1.45±0.5 | 1.10±0.1 | 1.20±0.4 | 1.10±0.3 | 1.30±0.4 | 1.00±0.1 | 1.15±0.3 | 0.039 | 0.036 | 0.120 | 0.075 |
| Contour | 1.60±0.5 | 2.15±0.4 | 1.10±0.3 | 1.30±0.4 | 1.40±0.5 | 2.10±0.4 | 1.10±0.3 | 1.20±0.4 | 0.003 | 0.120 | 0.001 | 0.389 |
| Distortion | 1.50±0.5 | 1.90±0.6 | 1.05±0.2 | 1.30±0.4 | 1.30±0.4 | 1.7±0.5 | 1.05±0.2 | 1.20±0.4 | 0.036 | 0.038 | 0.008 | 0.159 |
| Texture | 1.25±0.5 | 1.85±0.7 | 1.05±0.2 | 1.10±0.3 | 1.40±0.5 | 1.5±0.5 | 1.10±0.3 | 1.20±0.3 | 0.006 | 0.560 | 0.414 | 0.960 |
| Total score | 8.05±1.0 | 8.90±1.2 | 5.25±0.9 | 6.20±1.1 | 7.25±1.4 | 8.35±1.8 | 5.30±0.7 | 6.00±0.9 | 0.045 | 0.007 | 0.009 | 0.011 |
Bold values indicate p<0.05. p1: independent t-test, comparison of 1st month single and running suture in vicryl group; p2: independent t-test, comparison of 3rd month single and running suture in vicryl group; p3: independent t-test, comparison of 1st month single and running suture in polypropylene group; p4: independent t-test, comparison of 3rd month single and running suture in polypropylene group.
Table 2.
Postoperative complications in interrupted and running suture techniques in both vicryl and polypropylene groupsa
| Running suture | Interrupted suture | |
|---|---|---|
| Vicryl group (n=34) | 5 patients had milia (15%) | 2 patients had milia (6%) |
| 2 patients had wound dehiscence (6%) | 3 patients had wound dehiscence (9%) | |
| Polypropylene | 6 patients had milia (13%) | 4 patients had milia (9%) |
| group (n=46) | 4 patients had wound dehiscence (9%) | 4 patients had wound dehiscence (9%) |
| 2 patients had an infection (6%) |
aAs one eye of each patient is running sutured and the other eye is interrupted sutured, it has the same value as the number of people in both groups.
Discussion
Upper eyelid blepharoplasty is among the most common surgeries around the world. Different surgery techniques, cutting techniques or cutting instruments, wound closure materials and wound closure techniques are being used mostly in compliance with surgeons’ preferences. In this prospective study, we evaluated the postoperative results of patients whose suture techniques are interrupted cutaneous in one eye and running cutaneous in the other in terms of edema, ecchymosis, and scar index. The comparison of suture techniques showed us that the suture techniques that were used had an impact on postoperative edema, ecchymosis, and scar.
Upper eyelid blepharoplasty is mostly performed for aesthetic purposes. That is why it cannot stand any problems such as scar formation or other postoperative complications (3). The goal of blepharoplasty is an excellent result with minimal complications and discomfort. The desire to achieve perfect results has led many surgeons to try different methods. Scaccia et al. (8) compared the results of subcuticular closure with a 5-0 polypropylene suture in one eye with those of closure with a running 6-0 fast-absorbing catgut approximation in the other eye in upper eyelid blepharoplasty. They concluded that running 6-0 fast-absorbing catgut suture may offer some surgeons slightly better results than a subcuticular permanent suture for closure of the upper eyelid blepharoplasty incision (8). In addition, they identified no significant differences in postoperative discomfort levels (8). Pool et al. (6) investigated whether an internal intradermal suture technique affects the occurrence of suture abscess formation and focal inflammation in upper eyelid blepharoplasty. They found a statistically significant reduction in the incidence of medial wound inflammation and suture abscess formation if the suture is started in the medial side of an upper eyelid blepharoplasty wound (6).
Incisions can be closed with different nonabsorbable and absorbable suture materials, as well as different techniques such as simple, running, running locking, and subcuticular closure. Previously, a combination of different suture materials and techniques was evaluated. Joshi et al. (4) evaluated a running subcuticular Prolene suture, a running-locking cutaneous 5-0 Prolene suture, a running cutaneous 6-0 plain gut suture, and two interrupted 6-0 Prolene sutures (for the ends of the incision) along with a running 6-0 fast-absorbing gut suture and compared the complication rates. They observed significant differences between suture materials and techniques with respect to milia formation, erythema, and scarring. They concluded that closure with two interrupted 6-0 Prolene sutures and a running 6-0 fast-absorbing gut resulted in the lowest rates of complications and revisions, postoperatively. Alternatively, wounds can be approximated with tissue adhesives. Kouba et al. (7) assessed upper eyelid blepharoplasty scars in patients who closured with 6-0 polypropylene sutures, 6-0 fast-absorbing gut sutures, or ethyl cyanoacrylate tissue adhesive. They reported that adhesive appears to provide greater cosmesis than absorbable suture material over short- and intermediate-term follow-up. However, they did not demonstrate any advantage of tissue adhesive over polypropylene sutures. Tissue adhesives are good options, but their availability at every clinic may not be possible.
The common approaches used for closing the upper eyelid blepharoplasty incision are running and interrupted cutaneous suture techniques with either an absorbable or nonabsorbable material. The postoperative results of running and interrupted suture techniques in the same patient who had gone through upper eyelid blepharoplasty could give us a better comparison for eliminating different skin texture differences. Our study design is the first to evaluate postoperative edema, ecchymosis, and scar index.
The postoperative edema comparison gave different results among suture materials. While postoperative edema in the first week was better at the interrupted sutured eyelid in the vicryl group, there were no significant changes between both eyelids in the polypropylene group. These results demonstrated that edema levels are similar in both suture techniques. The comparison of ecchymosis levels in the interrupted sutured eyelid was significantly less than running sutured eyelid in the first week at the vicryl group. There was significantly less ecchymosis at first day and first week postoperatively in interrupted sutured eyelid than running sutured eyelid in polypropylene group. When we evaluate the results of both groups, it is observed that although the interrupted suture technique causes less ecchymosis in the early period, there is no difference in the long term. In patients who may be disturbed by early ecchymosis, the interrupted suture technique can be considered as an option. However, to prevent these problems in the early postoperative period, it is always more important to talk to the patient and state that this situation can be seen.
Postoperative scar formation is the most unwanted complication of cosmetic surgeries such as blepharoplasty. When we evaluate the scar index in the vicryl group, all indexes were better in an interrupted sutured group than the running suture group at the postoperative first month, yet differences in the texture and contour were diminished at the postoperative third month. In the polypropylene group, while color, contour, and distortion indexes were better at the interrupted sutured eyelid at the postoperative first month, only differences at color remained at the same level at the postoperative third month. The comparisons of total scores of scar index in both groups were significantly better at interrupted sutured eyelid at postoperative first and third months. The better results in the interrupted sutured eyelid could be results of better tissue approximation of the interrupted suture technique. As we know, running suture technique could result in tissue–tissue overlapping and pronouncing which affect tissue healing. That is why the interrupted suture technique could be superior on the scar formation after upper eyelid blepharoplasty.
Milia and wound dehiscence were the most common minor complications associated with blepharoplasty in our study. In the vicryl group, while 5 patients had milia, 2 patients had wound dehiscence in running sutured eyelid, 2 patients had milia, and 3 patients had wound dehiscence in interrupted sutured eyelid. In the polypropylene group, while 6 patients had milia and 4 patients had wound dehiscence, 2 patients had an infection in running sutured eyelid, 4 patients had milia, and 4 patients had wound dehiscence in interrupted sutured eyelid. As seen, milia formation is seen more common in running suture technique. Wound dehiscence rates were similar in both suture techniques. Scaccia et al. (8) reported a higher rate of milia formation (7.5%) after using the running subcuticular polypropylene. Joshi et al. (4) found nearly equal rates of milia formation with subcuticular polypropylene (2.5%) and with 6-0 running-fast absorbing gut, 5-0 simple interrupted Prolene (2%). Similarly, Scaccia et al. (8) observed no significant difference in milia formation after using a permanent subcuticular and an absorbable skin suture. Joshi et al. (4) observed higher rates of milia (6.7%) with a running 6-0 plain suture and a running cutaneous locked Prolene (17%) when compared with either a subcuticular closure or a running closure with fast-absorbing gut suture. Milia are believed to result from the entrapment of epithelial cells along suture line tracts. Tissue–tissue overlapping and pronouncing that resulted in entrapment of epithelial cells along suture line tracts is prominent with the running suture technique. That could be an explanation for higher rates of milia formation of running suture technique.
Our study has several limitations. The small sample size may affect the validity of our results. These points may be evaluated in future prospective studies with longer follow-up periods. On the other hand, we preliminarily evaluated the suture techniques that do not suture materials. Therefore, we did not compare the results of suture materials. However, the comparison of suture materials on different patients may not be as effective as the comparison in the same patient. These ideas could be a subject for future studies with a prospective design.
Conclusion
In this study, we present a large series of patients who have undergone blepharoplasty of the upper eyelid. We have observed significant differences between suture techniques with respect to edema, ecchymosis, and scar formation. It seems that an interrupted suture technique yielded the lowest rates of edema, ecchymosis, and scar formation. Although we do not expect surgeons to change the suturing techniques according to our research, we may say that the results of an interrupted suture are better in such special surgeries.
Footnotes
Disclosures
Ethics Committee Approval: The study protocol was approved by the Adıyaman University clinical research ethics committee (Approval number: 2021-3-4, Approval date: February 11, 2021), and the study was carried out in accordance with the Declaration of Helsinki.
Peer-review: Externally peer-reviewed.
Conflict of Interest: None declared.
Authorship Contributions: Involved in design and conduct of the study (EA); preparation and review of the study (HK); data collection (GAA); and statistical analysis (HK).
References
- 1.Balzani A, Chilgar RM, Nicoli M, Sapountzis S, Lazzeri D, Cervelli V, et al. Novel approach with fractional ultrapulse CO2 laser for the treatment of upper eyelid dermatochalasis and periorbital rejuvenation. Lasers Med Sci. 2013;28:1483–7. doi: 10.1007/s10103-012-1255-4. [DOI] [PubMed] [Google Scholar]
- 2.Fallahi HR, Keyhan SO, Niamtu J, Alikazemi M, Habibagahi R. Comparison of clinical outcomes of CO2 laser-assisted blepharoplasty using two different methods. J Oral Maxillofac Surg. 2020;78:1006–12. doi: 10.1016/j.joms.2020.01.015. [DOI] [PubMed] [Google Scholar]
- 3.Bhattacharjee K, Misra DK, Deori N. Updates on upper eyelid blepharoplasty. Indian J Ophthalmol. 2017;65:551–8. doi: 10.4103/ijo.IJO_540_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joshi AS, Janjanin S, Tanna N, Geist C, Lindsey WH. Does suture material and technique really matter?Lessons learned from 800 consecutive blepharoplasties. Laryngoscope. 2007;117:981–4. doi: 10.1097/MLG.0b013e31804f54bd. [DOI] [PubMed] [Google Scholar]
- 5.Morax S, Touitou V. Complications of blepharoplasty. Orbit. 2006;25:303–18. doi: 10.1080/01676830600985841. [DOI] [PubMed] [Google Scholar]
- 6.Pool SM, Krabbe-Timmerman IS, Cromheecke M, van der Lei B. Improved upper blepharoplasty outcome using an internal intradermal suture technique:a prospective randomized study. Dermatol Surg. 2015;41:246–9. doi: 10.1097/DSS.0000000000000245. [DOI] [PubMed] [Google Scholar]
- 7.Kouba DJ, Tierney E, Mahmoud BH, Woo D. Optimizing closure materials for upper lid blepharoplasty:a randomized, controlled trial. Dermatol Surg. 2011;37:19–30. doi: 10.1111/j.1524-4725.2010.01834.x. [DOI] [PubMed] [Google Scholar]
- 8.Scaccia FJ, Hoffman JA, Stepnick DW. Upper eyelid blepharoplasty. A technical comparative analysis. Arch Otolaryngol Head Neck Surg. 1994;120:827–30. doi: 10.1001/archotol.1994.01880320029007. [DOI] [PubMed] [Google Scholar]
- 9.Douven I. A Bayesian perspective on Likert scales and central tendency. Psychon Bull Rev. 2018;25:1203–11. doi: 10.3758/s13423-017-1344-2. [DOI] [PubMed] [Google Scholar]
- 10.Mahalingam S, Alatsatianos A, Pitkin L, D'Souza A. Does the technique of skin closure affect the cosmesis of cervical thyroidectomy and parathyroidectomy scars?A review of literature. Facial Plast Surg. 2018;34:524–8. doi: 10.1055/s-0038-1660844. [DOI] [PubMed] [Google Scholar]


