Abstract
In this paper, a serological assay for the detection of antibodies to Capillaria hepatica, a zoonotic parasite, is described. In the past, the only way of detecting Capillaria hepatica was to perform a liver biopsy. The indirect immunofluorescence (IIF) assay, based on liver sections of naturally infected mice and human serum samples, is suitable for detecting early stages of human infections and for screening purposes. No cross-reactivity with other parasitic infections was detected. We have applied the IIF assay to serum samples of 60 employees of the Zoological Garden of Vienna, Schönbrunn, Austria, and found one positive and one questionable sample.
Capillaria hepatica (Bancroft, 1893) (2) is a zoonotic liver nematode of mammals of worldwide distribution. The parasite frequently causes hepatic infections in rodents and lagomorphs. In humans, infections are rarely found. To our knowledge, only 37 reports of human infections have been published so far; however, human infections may lead to severe disease and death; approximately half of the cases have been diagnosed by liver biopsy, and half of them have been diagnosed at autopsy (Table 1). The life cycle of this parasite, which reveals a marked affinity for the liver (32), is a direct one. Following ingestion of embryonated eggs, larvae hatch in the cecum and reach the liver via the portal vein system. They mature in the parenchyma of the liver and mate, leading to the production of eggs an average of 28 days after mating. Sexually mature males are found in the livers of mice, 15 (18) to 18 (34) days postinfection (p.i.), and sexually mature females are found 15 (18) to 20 (34) days p.i. The life spans of adult organisms are short. References in the literature range from 18 (23) to 60 (34) days p.i. in mice. Eggs deposited in the liver parenchyma remain there and develop only to the eight-cell stage. Further cleavage does not take place until they are released from the liver tissue. Eggs reach the environment only through the decay of an infected carcass or when they are excreted in the feces either of carnivores or of scavengers feeding on infected mammals. Eggs embryonate and become infective in the soil, under optimal conditions, such as exposure to air with a high relative humidity and temperatures of 25 to 30°C, within 5 to 8 weeks. Embryonated eggs remain viable for 25 months at room temperature. The life cycle is completed when a new host ingests the parasite (34).
TABLE 1.
Cases of human C. hepatica infestation reported in the literature
| Reference | Age | Sexa (no. of patients) | Region | Therapy | Outcome |
|---|---|---|---|---|---|
| 19 | 20 years | M | India | None | Died |
| 20 | 17 months | F | Louisiana | None | Died |
| 21 | 7 years | F | Maryland | Chloroquine | Died after 2 years |
| 30 | 60 years | M | Turkey | None | Incidental detection |
| 11 | 15 months | F | Hawaii | Diethylcarbamazine | Died after 4 months |
| 9 | 15 months | F | South Africa | Antibiotics, cortisone, antimony | Survived (15 years) |
| 33 | 2 years | F | Louisiana | None | Died, but incidental detection |
| 5 | 20 months | M | Illinois | Dithiazanine iodide | Survived (10 months) |
| 15 | 5 years | F | South Africa | None | Incidental detection |
| 26 | 22 months | F | Mexico | Unknown | Unknown |
| 25 | 25 years | F | Brazil | None | Incidental detection |
| 6 | 11 months | M | Ivory Coast | Antibiotics, cortisone | Died, but incidental detection |
| 8 | 3 years | F | Italy | Some anthelmintic drugs | Unknown |
| 10 | Unknown | F | Canada | Unknown | Died |
| 28 | 17 months | F | South Africa | Diethylcarbamazine, antimony | Survived (1 year) |
| 29b | 19–83 years | F (5), M (4) | Czechoslovakia | None | Incidental detection |
| 31 | 2 years | M | Mexico | Thiabendazole, cortisone | Survived (1 month) |
| 24 | 39 years | M | Brazil | Pyrantel | Survived (8 years) |
| 1 | 27 years | F | Nigeria | None | Unknown |
| 3 | 1 year | F | Switzerland | Thiabendazole | Survived |
| 17 | 2 years | F | Yugoslavia | Levamisole | Survived |
| 22 | 18 months | F | Germany | Ivermectine, thiabendazole, cortisone | Survived |
| 27 | 26 years | M | Japan | None | Survived |
| 7 | 14 months | F | Korea | Thiabendazole | Survived |
| 16 | 32 years | F | Japan | Surgery | Survived |
| 4 | 19 months | M | Mexico | Unknown | Unknown |
| 13 | 54 years | F | Mexico | None | Incidental detection |
| 14 | 6 years | M | India | Antimonials | Survived |
| 35 | 60 years | F | Greece | Some anthelmintic drugs | Survived |
M, male; F, female.
Nine cases.
It has to be noted that the ingestion of nonembryonated eggs does not lead to hepatic capillariasis. In such cases, ova just pass through the gastrointestinal tract of the host following ingestion of uncooked or poorly cooked livers of infected animals and are excreted in the feces. In such spurious infections there are no definite clinical signs (12, 19, 21). Reports of spurious infections must be kept well apart from reports of genuine infections. In the former, eggs of C. hepatica are found in stool, in the latter, they are not. Genuine infections cause severe hepatic disease in humans and animals. Persistent fever, hepatomegaly, and leucocytosis with eosinophilia are reported to be the symptom triad of hepatic capillariasis. Anemia, pulmonary symptoms, splenomegaly, enlargement of the kidneys, and wasting may also occur. Unsanitary practices, poor hygienic conditions, and the presence of dense rodent populations are predisposing factors for genuine human infections. Children or adults with the habit of eating soil (geophagia, pica) (9, 11, 12, 27), as well as children with soil-to-hand-to-mouth contact, are especially at risk.
For differential diagnosis, infections with Toxocara canis or Toxocara cati (the dog and cat roundworms, respectively; symptom, larva migrans visceralis), Fasciola hepatica, and Echinococcus granulosus or Echinococcus multilocularis must also be considered.
All together, only 37 cases of hepatic capillariasis in humans have been reported between 1924 and 1996 worldwide, with 15 of them having been in Europe. However, human infections with C. hepatica probably occur more frequently, showing a milder or even subclinical course (as was demonstrated by different authors who incidentally detected the infection) (Table 1). Until now, the only way of diagnosing C. hepatica infections was taking and examining liver biopsy samples.
We report in this paper a serological assay which requires only a serum sample of the patient. The assay is easy to perform and can be used for detecting early stages of human infections as well as for screening purposes.
Six-micrometer cryocut sections were prepared from livers of naturally infected mice, which showed a massive infestation with nonembryonated C. hepatica eggs. The mice originated from the natural population of house mice (Mus musculus) in the Zoological Garden of Vienna, Schönbrunn, Austria. During 1996 and 1997, mice were trapped and examined for the presence of C. hepatica in their livers, both macroscopically by looking for the characteristic yellowish-white lesions and by the tissue press technique. The presence of the parasite was confirmed by recovery of the typical bipolar plugged eggs in the liver preparations. Hepatic lesions consisted of minimal to severe replacement of liver tissue by C. hepatica eggs. Nonembryonated eggs from infected livers were recovered by peptic digestion, and their morphological characteristics were examined microscopically. Eggs showed the characteristic features described by Calle (5). They were oval and showed a double-layer shell with radial striations in the outer shell. The average size of the nonembryonated eggs (n = 100) was 55.8 by 30 μm (ranges, 49.2 to 61.5 μm [length] and 24.6 to 41.0 μm [width]). Several (42.7%) of the 166 examined livers proved positive. In the infected livers, no larval stages or adult parasites were found except in one case. In this case, a live nematode was slightly connected to the surface of the liver of a mouse. The nematode was identified as C. hepatica on the basis of its morphological characteristics (34).
Because of the high rate of infestation of house mice with C. hepatica in the Zoological Garden of Vienna, Schönbrunn, Austria, and the resulting high probability of a severe contamination of the environment, there was a potential risk for the employees of the zoo. Therefore, we initiated a serological survey, using the assay described below. Sixty employees agreed to participate in the study.
Cryocut sections of mice livers heavily infested with nonembryonated C. hepatica eggs were fixed for 10 min on glass slides with precooled acetone. Subsequently, the human serum samples to be examined were added to the sections in dilutions of 1 in 40, 1 in 80, and 1 in 160 (in phosphate-buffered saline [PBS]) and incubated for 45 min at 37°C. Following a triplicate washing procedure in PBS, a fluorescein isothiocyanate-conjugated antihuman immunoglobulin G antiserum (Sigma, St. Louis, Mo.) was added to the sections at a dilution of 1 in 80. After another 45-min incubation period at 37°C, the sections were again washed three times with PBS, covered with buffered glycerol (glycerol-PBS, 9:1), and examined in a microscope under UV light. A serum sample taken from a convalescent 1-year-old child from Switzerland who had suffered from severe hepatic capillariasis (3) served as positive control serum, and serum samples from three healthy colleagues at the University of Veterinary Medicine, Vienna, Austria, were used as negative controls. Because hepatic capillariasis is a rare infection in humans, it was not possible to obtain sera from other patients. However, to further evaluate the sensitivity of the assay, we tested serum samples of four mice with verified C. hepatica infection and three negative control mice.
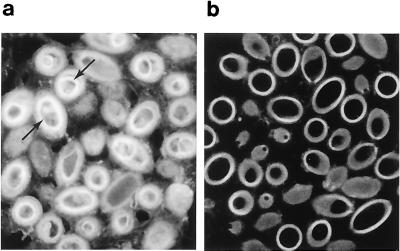
One employee of the zoo showed antibodies to C. hepatica, with a titer of 1 in 40 (Fig. 1a), and another one was questionably positive at the 1 in 40 dilution; the other samples proved negative (one of the negative serum samples is shown in Fig. 1b). In addition to the bright fluorescence, which is seen all over the sections of the parasite eggs when antibodies to C. hepatica are present in the serum, we especially draw the reader's attention to the fluorescing inner structures of the eggs, which seem to be highly specific. During the evaluation of the assay, about 10% of the serum samples showed a low-level nonspecific fluorescence (which was seen only in serum dilutions of <1 in 20). When we used the recommended serum dilutions of 1 in 40 and higher, however, we could clearly discriminate between sera with antibodies to C. hepatica and negative sera. The serum of the convalescent Swiss child with diagnosed hepatic capillariasis repeatedly showed a titer of 1 in 320 in the indirect immunofluorescence (IIF) assay. All four examined serum samples of mice with C. hepatica infection proved positive, with titers of 1 in 80 to 1 in 640; although mouse sera were tested on mouse tissue, there was surprisingly little background staining. The three clinically negative mice were also negative by the IIF assay.
FIG. 1.
IIF assay of sections of C. hepatica eggs to detect antibodies to C. hepatica in human serum samples. (a) Serum with antibodies to C. hepatica. Arrows indicate the highly specific fluorescence of inner structures. (b) Negative serum. Microphotograph magnification, ×100.
The blood parameters of the two individuals seropositive and questionably positive for C. hepatica were normal, and they showed no increase in the activities of the liver-dependent enzymes. Two months later, blood was again taken from them and analyzed by the above-described assay. For the man who initially showed an antibody titer of 1 in 40, the same titer was determined 2 months later, while the other individual with the borderline titer of 1 in 40 tested negative. The two employees will also be monitored in the future, but a transient or subclinical infection with C. hepatica seems to be possible in these cases.
To further assess the specificity of the assay, serum samples of patients with documented infections of E. granulosus, E. multilocularis, F. hepatica, Schistosoma mansoni, T. canis, Trichuris trichiura, and Trichinella spiralis were tested for cross-reactivity with C. hepatica. All sera proved negative for antibodies to C. hepatica at dilutions of 1 in 20 and 1 in 40. Furthermore, to check the other possibility of cross-reaction, the sera of the two employees who were positive and questionably positive for C. hepatica were tested for the presence of antibodies to E. granulosus (enzyme-linked immunosorbent assay [ELISA] and Western blotting), E. multilocularis (ELISA and Western blotting), F. hepatica (ELISA), S. mansoni (ELISA), T. canis (ELISA and Western blotting), Trichuris trichiura (ELISA), and Trichinella spiralis (ELISA). No antibodies to any of the above-named parasites were found in the sera.
In summing up the advantages and limitations of the IIF assay described in this paper, we report that this assay offers for the first time the possibility of a large-scale screening of persons at risk for C. hepatica infections; it will be possible to detect infections at an early stage, thus increasing the chances for a successful treatment significantly. Furthermore, only a small amount of serum is required from the patient to carry out this assay. It is possible to perform this test in every histology lab, and the results are ready after 2 h. In our opinion, the only limitation of this assay is some nonspecific fluorescence of unknown origin at lower serum dilutions.
Acknowledgments
We thank Hans-Peter Marti, Schweizer Tropeninstitut, Basel, Switzerland, for providing the positive control serum and the two anonymous reviewers of the manuscript for their constructive criticism.
REFERENCES
- 1.Attah E B, Nagarajan S, Obineche E N, Gera S C. Hepatic capillariasis. Am J Clin Pathol. 1983;79:127–130. doi: 10.1093/ajcp/79.1.127. [DOI] [PubMed] [Google Scholar]
- 2.Bancroft T L. On the whip-worm of the rat's liver. J Proc R Soc N S W. 1893;27:86–90. [Google Scholar]
- 3.Berger T, Degrémont A, Gebbers J O, Tönz O. Hepatic capillariasis in a 1-year-old child. Eur J Pediatr. 1990;149:333–336. doi: 10.1007/BF02171560. [DOI] [PubMed] [Google Scholar]
- 4.Bustamente-Sarabia J, Suswillo R, Contreras-Moreno E. Capillaria hepatica in a 19-month old boy, third case in Mexico. Bol Med Hosp Infant Mex. 1996;53:395–400. [Google Scholar]
- 5.Calle S. Parasitism by Capillaria hepatica. Pediatrics. 1961;27:648–655. [PubMed] [Google Scholar]
- 6.Camain R, Dor X, Ranavo F. Infestation hépatique àCapillaria hepatica chez un enfant de 11 mois. Ann Pediatr (Paris) 1965;12:559–562. [PubMed] [Google Scholar]
- 7.Choe G, Lee H S, Seo J K, Chai J Y, Lee S H, Eom K S, Chi J G. Hepatic capillariasis: first case report in the Republic of Korea. Am J Trop Med Hyg. 1993;48:610–625. doi: 10.4269/ajtmh.1993.48.610. [DOI] [PubMed] [Google Scholar]
- 8.Cislaghi F, Radice C. Infection by Capillaria hepatica. First case report in Italy. Helv Paediatr Acta. 1970;25:647–654. [PubMed] [Google Scholar]
- 9.Cochrane J C, Sagorin L, Wilcocks M G. Capillaria hepatica infection in man. A syndrome of extreme eosinophilia, hepatomegaly and hyperglobulinaemia. S Afr Med J. 1957;31:751–755. [PubMed] [Google Scholar]
- 10.Eaton R D P. Current problems in parasitology in Canadian native peoples. Proceedings of the Second International Symposium on Circumpolar Health, Oulu, Finland. Acta Socio Med Scand Suppl. 1972;6:249–253. [PubMed] [Google Scholar]
- 11.Ewing G M, Tilden I L. Capillaria hepatica. Report of fourth case of true human infestation. J Pediatr. 1956;48:341–348. doi: 10.1016/s0022-3476(56)80261-8. [DOI] [PubMed] [Google Scholar]
- 12.Foster A O, Johnson C M. An explanation for the occurrence of Capillaria hepatica ova in human feces suggested by the finding of three new hosts used as food. Trans R Soc Trop Med Hyg. 1939;32:639–644. [Google Scholar]
- 13.Gonzalez-Barranco D, Pelaez D, Jaramillo-Rodriguez Y, Rodriguez-Martinez H A. Third case of human hepatic capillariasis in Mexico. Rev Investig Clin. 1996;48:301–305. [PubMed] [Google Scholar]
- 14.Govil H, Desai M. Capillaria hepatica parasitism. Indian J Pediatr. 1996;63:698–700. doi: 10.1007/BF02730826. [DOI] [PubMed] [Google Scholar]
- 15.Kallichurum S, Elsdon-Dew R. Capillaria in man. A case report. S Afr Med J. 1961;35:860–861. [PubMed] [Google Scholar]
- 16.Kohatsu H, Zaha O, Shimada K, Chibana T, Yara I, Shimada A, Hasegawa H, Sato Y. A space-occupying lesion in the liver due to Capillaria infection. Am J Trop Med Hyg. 1995;52:414–418. doi: 10.4269/ajtmh.1995.52.414. [DOI] [PubMed] [Google Scholar]
- 17.Kokai G K, Misic S, Perisic V N, Grujovska S. Capillaria hepatica infestation in a 2-year old girl. Histopathology. 1990;17:275–277. doi: 10.1111/j.1365-2559.1990.tb00723.x. [DOI] [PubMed] [Google Scholar]
- 18.Luttermoser G W. An experimental study of Capillaria hepatica in the rat and the mouse. Am J Hyg. 1938;27:321–340. [Google Scholar]
- 19.McArthur W P. A case of infestation of human liver with Hepaticola hepatica (Bancroft, 1893) Hall, 1916; with sections from the liver. Proc R Soc Med. 1924;17:83–84. doi: 10.1177/003591572401702222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McQuown A L. Capillaria hepatica: report of genuine and spurious cases. Am J Trop Med. 1950;30:761–767. doi: 10.4269/ajtmh.1950.s1-30.761. [DOI] [PubMed] [Google Scholar]
- 21.Otto G F, Berthrong M, Appleby R E, Rawlins J C, Wilbur O. Eosinophilia and hepatomegaly due to Capillaria hepatica infection. Bull John Hopkins Hosp. 1954;94:319–336. [PubMed] [Google Scholar]
- 22.Pannenbecker J, Miller T C, Müller J, Jeschke R. Schwerer Leberbefall durch Capillaria hepatica. Monatsschr Kinderheilkd. 1990;138:767–771. [PubMed] [Google Scholar]
- 23.Pavlov A V. Trichocephalidae and Capillariidae of animals and man and the diseases caused by them, 404–411. In: Skrjabin K I, editor. Principles of nematodology. Vol. 6. Moscow, Russia: Izdatelstvo Akademii Nauk SSSR; 1970. [Google Scholar]
- 24.Pereira V G, Mattosinho Franca L C. Successful treatment of Capillaria hepatica infection in an acutely ill adult. Am J Trop Med Hyg. 1983;32:1272–1274. doi: 10.4269/ajtmh.1983.32.1272. [DOI] [PubMed] [Google Scholar]
- 25.Piazza R, Correa M A, Fleury R N. Sobre um caso de infestacao humana por Capillaria hepatica. Rev Inst Med Trop Sao Paulo. 1963;5:37–41. [PubMed] [Google Scholar]
- 26.Romero G, Mendiola y Biagi F. Eosinofilia elevada con manifestationes viscerales. Primer caso de infeccion por Capillaria hepatica en Mexico. Bol Med Hosp Infant Mex. 1962;19:473. [PubMed] [Google Scholar]
- 27.Sekikawa H, Hasegawa H, Otsuru M, Igarashi T, Kaneko H, Wada K, Sato O, Wakakuwa R, Tajima K, Homma K. First human case of Capillaria hepatica infection in Japan. Jpn J Parasitol. 1991;40:528–532. [Google Scholar]
- 28.Silvermann N H, Katz J S, Levin S E. Capillaria hepatica infestation in a child. S Afr Med J. 1973;47:219–221. [PubMed] [Google Scholar]
- 29.Slais J. The finding and identification of solitary Capillaria hepatica (Bancroft, 1893) in man from Europe. Folia Parasitol (Prague) 1973;20:149–161. [PubMed] [Google Scholar]
- 30.Turhan B, Unat E K, Ynermar M, Sumer C. Insan karacigerinde: Capillaria hepatica (Bancroft, 1893) Travassos 1915. Microbiol Dergisi. 1954;7:149–159. [Google Scholar]
- 31.Vargas-Carreto G, Lopez-Martinez H, Victoria-Victoria R, Hernandez-Munoz G. Capillaria hepatica. Report of the 2nd case found in the Mexican Republic. Bol Med Hosp Infant Mex. 1979;36:909–917. [PubMed] [Google Scholar]
- 32.Vogel H. Über die Organotropie von Hepaticola hepatica. Z Parasitenkd. 1930;2:502–505. [Google Scholar]
- 33.Ward B L, Dent J H. Capillaria hepatica infection in a child. Bull Tulane Univ Med Fac. 1959;19:27–33. [PubMed] [Google Scholar]
- 34.Wright K A. Observations on the life cycle of Capillaria hepatica (Bancroft, 1893) with a description of the adult. Can J Zool. 1961;38:167–182. [Google Scholar]
- 35.Yfanti G, Andreadis E, Spiliadou C, Diamantopoulos E J. A woman with fever and a jejunal stricture. Lancet. 1996;347:802. doi: 10.1016/s0140-6736(96)90872-7. [DOI] [PubMed] [Google Scholar]