Abstract
Background
People from lower and middle socioeconomic classes and vulnerable populations are among the worst affected by the COVID-19 pandemic, thus exacerbating disparities and the digital divide.
Objective
To draw a portrait of e-services as a digital approach to support digital health literacy in vulnerable populations amid the COVID-19 infodemic, and identify the barriers and facilitators for their implementation.
Methods
A scoping review was performed to gather published literature with a broad range of study designs and grey literature without exclusions based on country of publication. A search was created in Medline (Ovid) in March 2021 and translated to Medline, PsycINFO, Scopus and CINAHL with Full Text (EBSCOhost). The combined literature search generated 819 manuscripts. To be included, manuscripts had to be written in English, and present information on digital intervention(s) (e.g. social media) used to enable or increase digital health literacy among vulnerable populations during the COVID-19 pandemic (e.g. older adults, Indigenous people living on reserve).
Results
Five articles were included in the study. Various digital health literacy-enabling e-services have been implemented in different vulnerable populations. Identified e-services aimed to increase disease knowledge, digital health literacy and social media usage, help in coping with changes in routines and practices, decrease fear and anxiety, increase digital knowledge and skills, decrease health literacy barriers and increase technology acceptance in specific groups. Many facilitators of digital health literacy-enabling e-services implementation were identified in expectant mothers and their families, older adults and people with low-income. Barriers such as low literacy limited to no knowledge about the viruses, medium of contamination, treatment options played an important role in distracting and believing in misinformation and disinformation. Poor health literacy was the only barrier found, which may hinder the understanding of individual health needs, illness processes and treatments for people with HIV/AIDS.
Conclusions
The literature on the topic is scarce, sparse and immature. We did not find any literature on digital health literacy in Indigenous people, though we targeted this vulnerable population. Although only a few papers were included, two types of health conditions were covered by the literature on digital health literacy-enabling e-services, namely chronic conditions and conditions that are new to the patients. Digital health literacy can help improve prevention and adherence to a healthy lifestyle, improve capacity building and enable users to take the best advantage of the options available, thus strengthening the patient’s involvement in health decisions and empowerment, and finally improving health outcomes. Therefore, there is an urgent need to pursue research on digital health literacy and develop digital platforms to help solve current and future COVID-19-related health needs.
Keywords: Digital health, literacy, vulnerable, COVID-19, misinformation, digital divide
Introduction
The COVID-19 pandemic has imposed various restrictions, such as lockdown and social distancing, affecting the quality of life and inter-individual social interactions. A survey conducted with 256 college students in the United States showed that, on average, student discussed pandemic-related health topics with 4–5 people, which did not vary by health literacy or digital health literacy (DHL) measures. 1 Information and Communication Technologies (ICTs) have always played a pivotal role in enabling communication and information exchange among people and digital health is one of its prominent applications in healthcare as communicating health information matters. 2 The need for natural interpersonal communication has been disrupted by the COVID-19 lockdown; however, technology is playing a major role in maintaining social interaction. Digital health and technologies have provided many online e-services to address the social challenges of the pandemic like communication gaps, information provision and remote work. The pandemic has extensively increased the reliance of the people on digital media platforms and social media (e.g. Quora, Facebook, YouTube, Instagram, Reddit, TikTok). Social media are undoubtedly one of the major means of accessing to information. For example, a study exploring the satisfaction level of the online information related to COVID-19 in more than 4000 persons with and without chronic diseases has revealed that the majority of people with chronic diseases sought online information related to COVID-19 from social media. 3 The level of information satisfaction of the online information related to COVID-19 was significantly lower in people with chronic diseases as compared to people without chronic diseases. 3
E-services focused on health literacy have emerged extremely quickly to cover the population’s need for information about the progress of the pandemic and its implications in terms of health management, such as continuing the management of chronic conditions. Due to the widespread surge in COVID-19 cases around the world, there is an abundance of COVID-19-related information available on various online platforms and social media tools that people commonly used for different information-seeking purposes. For example, people use digital platform to find health information such as COVID statistics and research, protective approaches, preventive measures, treatment guidelines, vaccine deployment and lifestyle recommendations. 4 This sea of online information related to COVID-19 can contain accurate and incorrect information, which has brought in the concept of ‘infodemic’ in this context. 5 An infodemic is defined by the WHO as ‘too much information including false or misleading information in digital and physical environments during a disease outbreak’. 6 Accessibility to the correct information, at the right time, in the right place, and in the right way is crucial in the pandemic; therefore, proper tackling and management of infodemic is imperative. The Internet encompasses various information channels and tools, for example, online search engines, video sharing platforms, social media channels and article indexing and abstracting services used to disseminate information or misinformation. Although these are some of the key information sources that people usually rely on for seeking health-related information, most of these sources are vulnerable to the spread of misleading pandemic-related information. Misinformation can negatively affect and endanger human health and lives.7,8
To deal with complex health information, one needs health literacy to understand, assimilate and use health information and be able to communicate effectively with their care provider. Health literacy is defined as ‘the degree to which individuals can obtain, process, understand and communicate about health-related information needed to make informed health decisions’.9,10 Looking it in the digital context, the DHL, which is also often used interchangeably as eHealth Literacy, is ‘the ability to seek, find, understand and appraise health information from electronic sources and apply the knowledge gained to addressing or solving a health problem’. 11 DHL is of particular interest in the current historical context where the COVID-19 pandemic has forced lockdown, and access to health information through traditional means (e.g. information sheets, pamphlets in medical offices) has become obsolete. As reflected from its name, DHL is more linked with the ability to use digital technologies for online information, interaction and activities related to the online environments, and an individual’s ability to understand and judge the information for appropriate decision making. 12 Higher DHL is associated with better health, positive behaviour and increased health knowledge. 13 A cross-sectional survey 14 conducted with more than 1000 Vietnamese students has explored the association between the importance of online information search and subjective well-being through their ability to find, understand, appraise and use online health-related information during lockdown throughout the first COVID-19 pandemic wave. According to the same survey, 87.2% of students reported sufficient well-being, while almost 13% reported low or very low well-being. 14 Another study 1 explored whether COVID-19- related information access, attitudes, and behaviours were associated with health literacy and DHL among 256 college students in the United States. Half of the cohort (49%) reported adequate health literacy, and 57% found DHL tasks easy overall. 1 Patil et al. 1 showed that DHL did not vary by health literacy level, and both health literacy and DHL were independently associated with overall compliance with basic COVID-19-related preventive practices. The authors also reported that higher DHL, but not HL, was significantly associated with greater willingness to get a COVID-19 vaccine and the belief that acquiring the disease would negatively affect their life. Ease of access to information and the reliability of the retrieved health information remains questionable. A cross-sectional survey 15 conducted with 3621 students in Slovenia showed that, although the level of DHL among students is sufficient, assessing the reliability of information remains problematic among half of the participants to the study. Approximately one third of the students reported having problems in finding information of their interest, and about one third reported having difficulties in selecting the information that is relevant to them. However, literature exploring the associations between DHL skills and health and wellbeing among vulnerable groups seems very limited.
DHL can be influenced by age, health status, educational background, digital literacy skills and motivations for seeking information.11,16 COVID-19-related information-seeking behaviour might vary between groups of people. Sense of coherence (SOC) seems hard to reach by the times of a pandemic. Data from three Asian countries (China, the Philippines and Singapore) extracted from a larger-scale cross-sectional survey conducted across 41 countries explored the relationship between DHL, SOC and anxiety among 266 older adults. 17 Leung et al. 17 reported that 43.2% expressed anxiety about the future and concluded that SOC had direct negative effect on anxiety and mediated the relationships between anxiety and DHL and financial satisfaction. According to Leung et al. 17 , actions should be taken to enhance SOC and DHL among older adults, as these capacities may help to manage anxiety during the pandemic. This review paper extends the negative effects of loss of SOC beyond older adults to cover a wider range of vulnerable populations. Vulnerable populations commonly show diversity from different perspectives, such as age, gender, ethnicity, race, and socioeconomic status, and represent the population’s category that usually gets fewer healthcare services than the requirements of their healthcare issues. 18 In the literature, many papers have discussed the concept of vulnerability in healthcare,19–22 and several definitions exist for the vulnerable populations,21,23–28 as it is utilized in different contexts and might change over time. In general, the vulnerable populations are already on the low level of health literacy and have health disparities in a social, economic or environmental context, so it might be difficult for vulnerable populations to cope and rely on complex technologies for information seeking. 12 The information gap among the people who have access to ICTs compared to those who do not have – or have less – access to ICTs brings the digital divide issue. 29 Therefore, vulnerable populations must adopt the current and emerging ICTs to address the digital divide and improve their quality of life. Various online information resources have emerged during the COVID-19 pandemic to close this digital divide by inducing online patient education, a key element of quality virtual patient care. For example, online education tools, including dedicated search engines, online classes and digital education stations, are valuable resources that can help patients with low health literacy find reliable patient education materials. 30
Similarly, virtual education practices, such as video tutorials, one-on-one trainings, and regular group trainings, can provide an opportunity for community healthcare workers to interact, guide and educate different communities; particularly, the underprivileged, disadvantaged and neglected communities that are increasingly vulnerable to multiple health burdens; for example, people who belong to high-risk groups. Examples of high-risk groups are the highly conservative and patriarchal families and persons living with regressive sociocultural norms. 31 On a broader level, governments should take practical steps to provide access to the technology and implement DHL programs in these populations to move forward to the era of an increasingly digital future. 32 There are various studies about DHL, digital divide, and COVID-19 for different population categories in multiple healthcare settings in the literature. This paper aims to draw a portrait of the barriers and facilitators of implementing e-services as a digital approach to support DHL in vulnerable populations amid the COVID-19 pandemic. To the best of our knowledge, this article is one among very scarcely available literature review that explores the DHL and information-seeking behaviour aspects related to the COVID-19 pandemic among vulnerable populations. 30 We define the vulnerable populations in this paper as the group of persons in need of special support adapted to their socioeconomic status, health needs or any context that prevents access to digital health information. As such, we non-exhaustively consider the following profiles as ‘vulnerable’: illiterate, digitally illiterate, older adults, with visual or hearing impairments, with mental or cognitive impairments, living in remote or underserved communities, with limited access to the Internet, Indigenous living on reserve, immigrants, having language barriers and with low socioeconomic status. The specific objectives of this literature review are:
To profile the users of e-services for DHL documented in the literature.
To depict the needs in terms of health-related information among the vulnerable populations.
To portray e-services that were implemented during the pandemic to support or promote DHL among vulnerable individuals.
To explore the effects of DHL on individual behaviours and perceptions about the pandemic.
To draw a portrait of the future of DHL based on the learning from the pandemic.
Methods
Study design
Literature corresponding to the topic of DHL in relation to the COVID-19 pandemic is expected to be emerging and disparate; therefore, we performed a scoping review to gather published literature with a broad range of study designs and grey literature without exclusions based on country of publication.33,34 The ‘Indigenous’ concept was primarily focused on North American and Taiwanese terms (Appendix 1). We performed the scoping review following the recommendation of Arksey and O’Malley 33 and Levac et al. 34
Search strategy
A health sciences librarian (CM) developed and tested the search strategy in consultation with the research team. The librarian used a combination of controlled vocabulary and keywords to create the DHL search concept. As there is no Medical Subject Heading (MeSH) term for DHL, the librarian used different keywords to capture the concept entirely. Keywords included: ‘patient education’, ‘digital divide’, ‘e-health literacy’, ‘m-health literacy’ and ‘digital health literacy’. The librarian utilized the Canadian Agency for Drugs and Technologies in Health (CADTH) Covid-19 search filter developed and peer-reviewed by CADTH Information Specialists. 35 During the search development, we included a search concept for Indigenous peoples, comprising of North American, Australian, New Zealand and Austronesian (including Taiwanese) Indigenous peoples. However, adding this concept resulted in zero results and was ultimately removed. The extraction took place in the following databases in March 2021: Medline, PsycINFO, Scopus and CINAHL with Full Text (EBSCOhost). The original search was created in Medline (Ovid) and translated to the other databases. The Medline (Ovid) search strategy is available in Appendix 2. All other search strategies are available upon request. To locate grey literature, we focused on preprint servers. With the rapidly evolving research on COVID-19, preprint servers have become essential tools to find and disseminate coronavirus information. We searched the DHL keywords previously mentioned on preprint servers, including MedRxiv, SocArXiv (OSF Preprints), Research Square and SSRN (The Lancet). All records were exported into EndNote (version x9; Clarivate Analytics, Philadelphia, PA, USA), and duplicates were removed. 36 All records were screened in Rayyan – a free online tool used for initial screening of articles to support systematic or narrative, or scoping review processes. 37 Full-text manuscripts of the included papers were retrieved, and the data extraction was processed in a customized Excel table.
Inclusion and exclusion criteria
To be included, manuscripts had to be written in English, and present information on digital intervention(s) used to enable or increase DHL among vulnerable populations during the COVID-19 pandemic. The manuscripts included an e-service focused on health literacy content (e.g. Internet, mobile application, web-based platforms and social media) related to the COVID-19 pandemic. The manuscripts specifically focused on vulnerable populations (e.g. older adults, Indigenous people living on reserve and people with low socioeconomic status). Two independent reviewers performed the search and study selection by reviewing the titles and abstracts relevant to the research question and inclusion criteria. A manuscript had to be judged relevant by both reviewers to be included. If consensus could not be reached, a third reviewer was consulted. The disagreement for the inclusion or exclusion of articles was resolved through discussions. Only empirical manuscripts of various formats were screened, namely, journal articles, abstracts, MSc and PhD theses and project reports. Literature reviews, methodological papers and study protocols were excluded.
Data analysis and extraction
A data extraction form was developed by MAC and independently piloted on three articles by two reviewers (M.P. and S.S.A.). All selected manuscripts were read by the authors and publication details were extracted accordingly, as follows:
Article details: first author name, publication year, article’s title, country of publication and study type.
DHL-enabling e-service: technology supporting DHL, description/modality of use, maturity level (under testing/already implemented), target users (vulnerable populations), and population characteristics.
Issues expressed by e-services users.
Focus on COVID-19 matters.
Knowledge about COVID-19.
Individual-level outcomes: Use of e-service, ability to process information, engagement in own health, ability to engage with digital services, feel safe and control, motivated to engage with digital services and other.
System-level outcomes: access to digital services that work, digital services that suit individual needs, incentives (e.g. discount) and other.
Expected long-term shift to digital health services.
Conclusions.
Recommendations for future research.
The extracted information related to DHL-enabling e-services was not consistent across the included studies; therefore, we performed a qualitative synthesis 38 to classify the information according to the emerging themes; for example, the needs for DHL-enabling e-services along with the barriers and facilitators for their implementation. Thematic analysis was chosen as a flexible methodological approach that can be tailored to the needs of the current review to cluster and concise the set of data retrieved in the included articles, and provide a rich and detailed portrait of the literature.39,40
Results
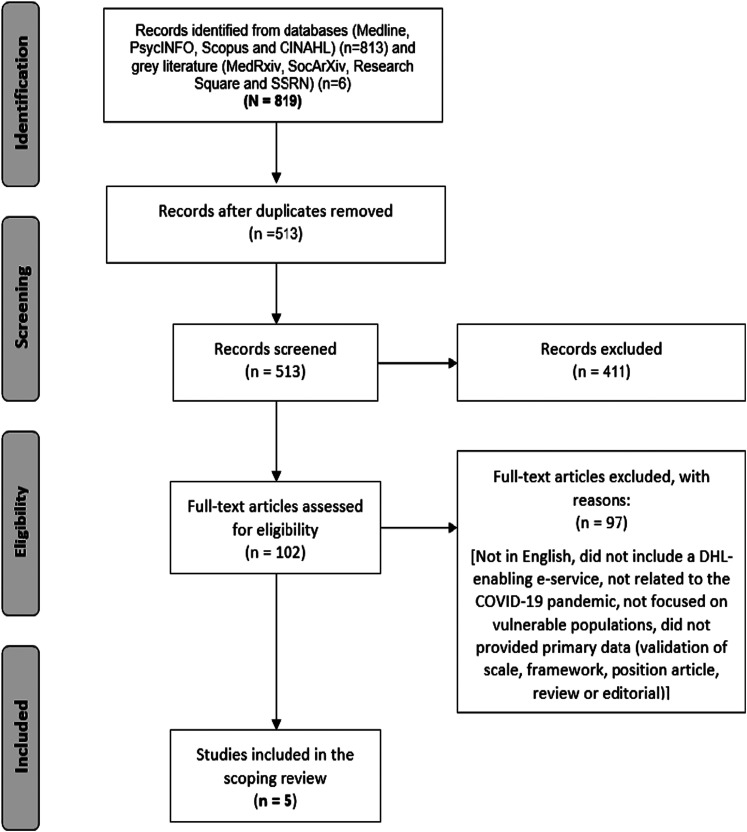
The initial search yielded 819 documents, of which 306 were duplicates, leaving 513 manuscripts that were screened for relevance. Of these, 411 were excluded, resulting in 102 manuscripts being considered for a full-text review. From these, 97 were excluded because they were not written in English, or did not include a DHL-enabling e-service, not related to the COVID-19 pandemic, not focused on vulnerable populations, or did not provide primary data (validation of scale, framework, position articles, reviews or editorials). Five articles were included in the scoping review. The complete article selection process is described in Figure 1.
Figure 1.
PRISMA flow diagram for article selection process. 41
Study characteristics
In the selected five manuscripts, four articles were published in 2020 and one report in 2021. Manuscripts were published in five different countries: USA (n = 1), UK (n = 1), China (n = 1), Italy (n = 1) and Turkey (n = 1). Regarding the publication channel, all the manuscripts were peer-reviewed journal articles involving survey data (n = 4) and one report (n = 1).
Vulnerable populations targeted by the DHL approaches
Three vulnerability categories were identified in this scoping review. The vulnerability was either health-related (diabetes, 42 cancer, 43 expectant mothers and new families 44 ), related to aging 45 and/or socioeconomic (low-income persons 46 ). None of the included manuscripts reported on Indigenous people.
Needs for DHL-enabling e-services
The thematic analysis focused on clustering the needs for DHL-enabling e-services into categories. The included papers reported on the following needs for e-services to support DHL:
- To cope with changes in routines and practices.
- Restrictions placed on hospital visitors during birth and postpartum. 44
- To overcome fear and anxiety.
- Fear about cancer care disruption by COVID-19. 43
- Many clients voiced fear and concerns of potential exposure to the virus while in the hospital and had questions about the hospital’s safety measures. 44
- Some clients had tested positive for COVID-19 and were anxious about separation from their babies and possible exposure and transmission to their newborns. 44
- To increase digital knowledge and skills.
- More male patients stated that their knowledge about the COVID-19 was inadequate compared to female patients. 43
- To decrease health literacy barriers and increase technology acceptance among specific groups (e.g. older adults).
- Problems with cognition, decreased physical abilities, hearing or visual impairments and lack of motivation could impede the acceptance of technology among older adults. 45
DHL approaches
Table 1 shows the retrieved e-services used to support and promote DHL and describes their characteristics, modality of use and the vulnerable populations that each e-services targets (Table 1).
Table 1.
DHL addressing the needs of vulnerable populations during the COVID-19 pandemic.
| e-service supporting DHL | Country | Description /modality of use | Target users | Population characteristics | Study type | Reference |
|---|---|---|---|---|---|---|
| E-class childbirth education program and a free online hospital information session virtual tour, ‘Ready, Set, Baby’. | USA | The program uses WEBEX for prerecorded classes and Zoom for the support groups and more interactive sessions (90min to 2 h) + EMAIL checked daily 5/7 + FACEBOOK + HOTLINE to convey a breastfeeding support system. The virtual sessions are offered at a 40% to 50% discount from the in-person class fees to increase access to more families. | Expectant and new families | The number of session participants Increased from 2459 to 2616 in the transition to virtual learning ( + 6.4) | Report | 44 |
| MyDesmond, an online program to support people with diabetes with their self-management. It is accessible on the NHS. Apps Library and incorporates content from the NICE endorsed face-to-face DESMOND program. | UK | The theory-based digital program adopts evidence-based strategies to optimize learning and engagement while allowing people with diabetes to progress through the educational content at their own pace. Other features of MyDesmond include discussion forums, booster sessions, goal setting features, monitoring steps, ‘Ask the Expert,’ step challenges, health trackers and a buddy system to tailor self-management strategies and promote behaviour change | People with diabetes. Of those who responded
(n = 803), the majority had been
diagnosed with type 2 diabetes in the last year (55%), 28% had been living with type 2 diabetes for 1 -5 years, and 17% for more than 10 years |
Of those who responded (n = 803), the majority had been diagnosed with type 2 diabetes in the last year (55%), 28% had been living with type 2 diabetes for 1-5 years, and 17% for more than 10 years. Experience of MyDesmond also varied with 21% having used the program for <1 month, 51% for 1-6 months and 28% for >6 months. | Online survey | 42 |
| TV and social media | Turkey | Common TV and social media use | Cancer patients | 195 patients [20–82 year] (Median 59), 57% females. More than a third of patients were 65 + . 74.6% under palliative treatment for the advanced-stage disease. 23.8% breast cancer patients. There were differences in the sources of knowledge among patients, and a significant portion of patients had false knowledge about COVID-19. | Survey | 43 |
| Social media as public preventive behaviour in China during the COVID-19 pandemic. the most frequently used media types were public social media and aggregated social media and professional social media, and official social media | China | Online | General population with low-income | Low-income users were about 34.7% (n = 802)
in this paper. Respondents were also equipped with high levels of disease knowledge and eHealth literacy. |
National web-based cross-sectional survey | 46 |
| mHealth, telecare and telehealth/behaviour monitoring solutions | Italy | Enable constant and effective communication between older adults and professionals. On the one hand, the older adults increase their autonomy and awareness in managing their health and, on the other, physicians can quickly intervene in case of emergency. | Elderly | Elderly | Workshop Proceedings | 45 |
Facilitators and barriers to DHL-enabling e-services implementation
Table 2 summarizes the barriers and facilitators of the different DHL approaches as retrieved in the included literature. This study is informed by the e-health literacy framework (eHLF) by Norgaard et al., 47 who describe the eHLF as a conceptual model that ‘offers a framework for evaluating an individual’s or a population’s capacity to understand, use and benefit from e-services to promote and maintain their health’. 47 Therefore, barriers and facilitators were categorized to match the seven components of the eHLF. 47 The information presented in Table 2 reflects data from three articles.42,44,46
Table 2.
Facilitators and barriers to DHL-enabling e-services .
| Outcomes as per the eHLF 47 | Facilitators | Reference | Barriers | Reference | |
|---|---|---|---|---|---|
| Systemic level | Digital services that suit individual needs | - | Inclusion of the updated guidelines and evidence-based practice during COVID-19. - Adding content to meet the emotional needs and challenges families were facing | 44 | |
| Official social media may be challenged by different competitive sources (maybe sources of misinformation) | 46 | ||||
| Access to digital services that work | Effectiveness in getting patients questions answered | 44,46 | - | ||
| Individual level | Motivated to engage with digital services | - | - | ||
| Feel safe and in control | Connection to a healthcare professional is key | 44 | - | ||
| Ability to actively engage with digital services | Ability to connect despite the lockdown | 44 | Patient-provider cannot replicate in-person sessions | 44 | |
| Engaging interactively | 42 | - | |||
| Engagement in own health | Helping patients understand their condition: helpful educational material, for example., helping patient improving their diet, becoming more active, better managing stress | 42 | - | ||
| Increasing preventive behaviours | 46 | - | |||
| Ability to process information | Ease of use: Content sufficiently detailed, providing clear and concise information, program that is easy and enjoyable to use | 42 | - |
Effects of DHL on individual behaviours and perceptions about the pandemic
The effects of DH-enabling e-services on the behaviours and perception about the pandemic underwent a thematic analysis that helped in characterizing the barriers and facilitators of implementing DHL-enabling e-services.
Facilitators of DHL-enabling interventions implementation during the COVID-19 pandemic
Virtual perinatal education is an alternative format for providing evidence-based guidance and support after suspension of all in-person classes and support groups due to the COVID-19 pandemic. 44
Connection to a live educator can help ease anxiety and address concerned families’ emotional needs. 44
Connecting to a live educator provides a forum for questions and discussion and enhances the educational program’s success. 44
COVID-19 has ushered in a new era for delivering patient education by combining in-person and digital education approaches that can increase access to education, reduce disparities, and improve quality of care. 42
Medical expert systems, provided with solid AI technologies, can promote healthy ageing by providing aid to older adults to maintain their functional ability and improve their wellbeing. 45
There is a definite need for action, both in the short and long terms, to minimize the adverse effects of the digital divide caused by this pandemic as well as to act to close the divide in the long term, and the shift to focus on digital tools can have a successful role in it. 46
Barriers to DHL-enabling interventions implementation during the COVID-19 pandemic
Poor health literacy created barriers in understanding individual health, illness, and treatments for people with HIV/AIDS. 46
Expected long-term transformation in DHL-enabling e-services
The thematic analysis helped identify and classify the previsions and expectations regarding long-term transformation in DHL-enabling e-services. The analysis of the included articles allows us to draw the following generalized recommendations and previsions:
Social media as a practical preventative approach – social media is helpful to disseminate pandemic news and disease knowledge, which can help the public to adopt necessary preventive measures for disease control collectively. On the other hand, the predictive ability of disease knowledge and DHL literacy provided an endorsement that improving one’s level of health literacy is essential during a pandemic in the long term. 46
Permanent virtual patient education – Virtual perinatal education could reasonably become the permanent way of providing support for the near future. The increase in the volume of participants suggests that the delivery of information via a virtual modality may be preferable with this generation of expectant families. 44
Digital equipment for the patients who do not have access to them – Some ways for health care organizations to meet the need in marginalized groups might be to have electronic tablets accessible in provider practices preloaded with educational content that the client could view during an office visit. Another option is to provide or increase telephonic information and support lines for expectant mothers and new parents. 44
Virtual education for non-English patients – Providing virtual education to non-English speaking clients and gathering and examining survey data to stay abreast of evolving patients’ needs. 44
Discussion
This study aimed to portray the e-services implemented as a digital approach to support DHL in vulnerable populations amid the COVID-19 infodemic and identify the barriers and facilitators for their implementation. The literature on the topic is scarce, sparse and immature. We classified the needs in terms of health-related information among the vulnerable populations. We have identified three types of needs: informational, transformational and adaptive:
Informational need – was characterized as a need to increase public awareness of health literacy in different disease conditions. 46 Health-related information appears to be widely available; however, it is not necessarily accessible by everyone, in particular, to some vulnerable populations. Health information is one of the very first bases for someone to understand, assimilate and use health practices,9,10 such as preventative approaches (e.g. hand washing, face masking, social distancing) or to contribute to health management, such as understanding the institution-related organizational procedures and the clinical processes as explained by the health professionals. Once accessed, the information has to be satisfactory for the user regardless of their vulnerability level. Satisfaction level seems proportionate to the level of complexity of each case and health condition (e.g. chronic diseases vs an acute disease). 3 Transformational needs – included increasing digital knowledge and skills required to use any DHL enabling e-service, 43 decreasing health literacy barriers and increasing technology acceptance among specific groups. 45 Transformational needs appear to be related to digital literacy as enabled by DHL-enabling e-services, namely the ability of someone to use digital means (the Internet, social media and mobile apps) to search, understand and use health information relevant to a specific health condition. 46
Adaptive needs – were reflected in the new ways of delivering healthcare amid the pandemic, including important adjustments supported by digital means. For instance, remote interventions targeting expectant mothers and their families successfully adapted to the restrictions placed on hospital visitors during birth and postpartum 44 and have helped expectant families cope with the changes in the related routines and practices. 44 E-services were also needed to support self-management in people with type-2 diabetes during the COVID-19 pandemic 42 and to help patients overcome COVID-19-related fear and anxiety, such as the fear of care disruption amongst chronic patients (e.g. cancer care). 43 Fear and anxiety were reported in expectant mothers about hospital safety measures, potential exposure to the virus while in hospital, 44 and, if they tested positive, would transmit the virus to their newborns 44 or be separated from their babies. E-services implemented during the pandemic to support and promote DHL among vulnerable individuals include a virtual childbirth education program together with a free online hospital information session virtual tour offered to expectant mothers, 44 an online program to support self-management in people with diabetes, 42 a virtual behaviour monitoring for elderly, 45 as well as the use of TV and social media to explore knowledge and concerns in cancer patients 43 and to promote preventive behaviour during the COVID-19 pandemic. 46
Health conditions could be considered the first reason of concern about someone in the context of a pandemic. Although only a few papers were included, we can see two types of health conditions, namely chronic conditions and conditions that are new to the patient. Chronic conditions are overwhelming conditions as scheduled follow-up appointments are needed, sometimes with different health care professionals. People living with chronic conditions would be more concerned about managing their condition amid unprecedented times, such as the COVID-19 pandemic. For example, in ref. 43 cancer patients had a significant degree of fear of disruption of cancer care due to the COVID-19 restriction, in addition to the population-wide fear of contracting the COVID-19 virus. Another example is the lower level of information satisfaction of the online information related to COVID-19 in people with chronic diseases as compared to people with an acute disease. 3
Interestingly, a significant number of cancer patients had the wrong information about protection necessities and discontent about the adequacy of information. 43 The role of DHL-enabling e-services in the context of chronic disease is of the highest necessity, as mismanaging the condition would directly worsen patient outcomes. Older people are at double risk during the pandemic from contracting the virus per se and the loneliness and boredom induced by the social distancing restrictions. A recent study noted that loneliness among Dutch older people increased during the COVID-19 pandemic and was influenced by personal losses, pandemic-related worries, and reduced trust in societal organizations. 48 Digital media can help people stay socially connected and positively affect health and quality of life. However, subsequent to challenges, such as overcoming deficiencies in digital skills, decreasing health literacy barriers and increasing technology acceptance, 32 once online, older people are susceptible to pandemic-related misinformation that negatively affect their health. DHL-enabling-e-services are therefore essential to overcome these challenges to support older people in improving digital literacy, online safety and adaptive behaviours toward the pandemic-related restrictions. Patients faced with a new condition, such as expecting childbirth, always live with a certain amount of anxiety related to uncertainty about their health and how the healthcare system manages their healthcare needs. In Pasadino et al. 44 , a virtual perinatal education program has been reported as a successful way of enabling DHL about pregnancy, labour, delivery and postpartum among expectant mothers and as an alternative format for providing evidence-based guidance and support when in-person sessions are not possible. Connection to a live educator has been reported as a facilitator to easing anxiety and addressing the emotional needs of families. Surprisingly, there is no literature on DHL manuscripts reported on Indigenous people despite the vulnerability of this population that could be exacerbated by the pandemic. Choukou et al. 49 have reported various advantages of using digital technology for Indigenous populations, particularly the Indigenous older adults, and barriers to implementing such technologies in Indigenous communities. Implementing DHL-enabling e-services in Indigenous communities seems an urgent matter, and it is recommended according to the literature 49 to keep Indigenous patient’s acceptance and culture at the forefront and to provide appropriate e-services by digital-health-trained healthcare professionals.
Under the pandemic lockdown, we have seen ICT become more readily available as a convenient and effective way of providing primary health guidelines and care; 50 however, the vulnerable population will be deprived of such opportunities due to a lack of access to digital information. The governments, health organizations, health-care providers and academia should not overestimate patient’s health literacy, 51 and should increase awareness about DHL-enabling e-services as a mean of promoting health literacy and create best practice guidelines targeting vulnerable groups to take advantage of ICT tools. COVID-19 pandemic has shown the transition of traditional care to telemedicine and home care. 45 DHL plays a pivotal role in teaching the elderly how to use ICT tools, thus allowing them to maintain their privacy, independence, and at the same time, be confident while they are under quarantine or home care. Wildenbos et al. 52 identified four significant barriers to technology acceptance by the elderly; 52 namely, cognitive impairments (memory loss and dementia), physical abilities, may be bound to hearing or visual impairments and motivation, which could be represented by the lack of perceived usefulness or ease of use of the new technologies. DHL can be useful to mitigate these mentioned concerns and facilitate elderly to accept and use digital solutions whether during the pandemic or beyond. This scoping review also aimed to draw a portrait of the future of DHL based on the learning from the COVID-19 pandemic. The illiterate in this Internet era will not be those who cannot read and write (e.g. a pamphlet distributed in a hospital, a public website, YouTube), but those who cannot distinguish between trustworthy and misleading information available online. 53 Citizens’ DHL is an essential element for successful eHealth deployment. However, although they might be digitally literate, vulnerable citizens often do not have the necessary skills to understand and appraise online health information and apply their knowledge to make health decisions. DHL can indeed help improve prevention and adherence to a healthy lifestyle, improve capacity building and take the best advantage of the available options, thus strengthening the patient’s involvement in health decisions and empowerment, and finally improving health outcomes.
Limitations
This scoping review has focused on the studies that reported on empirical research involving data collection. Literature reviews, editorials, theses and magazines were also excluded from this review. Therefore, these exclusion criteria could have limited the amount of DHL-enabling e-services included in the review. The general scope of the current review may not have highlighted all the DHL-enabling e-services that could be available, such as on social media and the Internet in general, without being studied. Findings encourage the implementation of DHL-enabling e-services and their use in digital health research reports. Due to the limited number of results and heterogeneity of the included articles, the included articles were not critically appraised to identify the strengths and weaknesses of the research and assess the usefulness and validity of research findings. As a quality assessment check approach, critical appraisal of manuscripts will be necessary for future reviews to help provide solid guidance to developers of DHL-enabling e-services based on the most substantial published work.
Conclusions
This review revealed that several factors could either facilitate or hinder the implementation of DHL-enabling e-services for vulnerable populations. Literature was scarce, which prevented us from drawing robust conclusions. However, we pointed out an absence of implementation of DHL-enabling e-services in Indigenous communities. We also identified the need for researchers to fill in the knowledge gap regarding the contribution to developing not only effective DHL-enabling e-services but also strategies to support and promote DHL. Strategies should focus on increasing digital skills, health literacy to combat misinformation and awareness of DHL-enabling e-services and their benefits in terms of prevention, adherence to health and wellness guidelines and active involvement of the patient in health decisions.
Supplementary Material
Acknowledgements
MAC and SAS have initiated the study and built the search strategy with CM, DSR, MP, MU and SAS. The authors run the screening, data extraction and materials preparation. MAC has initiated a first draft of the manuscript. All the authors contributed to the final version of the manuscript. The article processing charges for this article are supported by the University of Manitoba, College of Rehabilitation Sciences.
Footnotes
Conflict of interest: The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical Approval: Not applicable, because this article does not contain any studies with human or animal subjects.
Funding: The authors disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This work was supported by the Gerry McDole Professorship in Improved Healthcare Delivery to Rural, Remote and Underserved Populations of Manitoba 2020-2023 Grant.
Peer review: Dr. Mitja Vrdelja, National Institute of Public Health of the Republic of Slovenia.
ORCID iDs: Mohamed-Amine Choukou https://orcid.org/0000-0001-9477-2412
Diana C. Sanchez-Ramirez https://orcid.org/0000-0003-1637-4309
Shabbir Syed-Abdul https://orcid.org/0000-0002-0412-767X
Supplemental material: Supplementary material for this article is available online.
References
- 1.Patil U, et al. Health literacy, digital health literacy, and COVID-19 pandemic attitudes and behaviors in U.S. College students: implications for interventions. Int J Environ Res Public Health 2021; 3301: 1–14. doi: 10.3390/ijerph18063301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Syed Abdul S, et al. The pandemic, infodemic, and people's resilience in India: viewpoint. JMIR Public Health Surveill 2021; 7: e31645: 1–7. doi: 10.2196/31645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kor PPK, et al. Are people with chronic diseases satisfied with the online health information related to COVID-19 during the pandemic? J Nurs Scholarsh 2021; 53: 75–86. [DOI] [PubMed] [Google Scholar]
- 4.Dadaczynski K, et al. Digital health literacy and web-based information-seeking behaviors of university students in Germany during the COVID-19 pandemic: cross-sectional survey study. J Med Internet Res 2021; 23: e24097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cinelli M, et al. The COVID-19 social media infodemic. Sci Rep 2020; 10: 16598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.WHO. Infodemic, https://www.who.int/health-topics/infodemic#tab = tab_1 (2020).
- 7.Islam MS, et al. COVID-19-Related infodemic and its impact on public health: a global social media analysis. Am J Trop Med Hyg 2020; 103: 1621–1629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhattacharya C, et al. The nature, cause and consequence of COVID-19 panic among social media users in India. Soc Netw Anal Min 2021; 11: 53–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Berkman ND, Davis TC, McCormack L. Health literacy: what is it? J Health Commun 2010; 15: 9–19. [DOI] [PubMed] [Google Scholar]
- 10.Patil U, et al. Health literacy, digital health literacy, and COVID-19 pandemic attitudes and behaviors in U.S. College students: implications for interventions. Int J Environ Res Public Health 2021; 18: 3301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.First Meeting of the WHO GCM/NCD Working Group on Health Literacy for NCDs Digital Health Literacy for NCDs (Geneva, 27-28 February, 2017).
- 12.Harris K, Jacobs G, Reeder J. Health systems and adult basic education: a critical partnership in supporting digital health literacy. Health Lit Res Pract 2019; 3: S33–s36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van der Vaart R, Drossaert C. Development of the digital health literacy instrument: measuring a broad Spectrum of health 1.0 and health 2.0 skills. J Med Internet Res 2017; 19: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nguyen LHT, et al. Digital health literacy about COVID-19 as a factor mediating the association between the importance of online information search and subjective well-being Among university students in Vietnam. Frontiers Digit Health 2021; 3. Article 739476. doi: 10.3389/fdgth.2021.739476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vrdelja M, Vrbovšek S, Klopčič Vet al. et al. Facing the growing COVID-19 infodemic: digital health literacy and information-seeking behaviour of university students in Slovenia. Int J Environ Res Public Health 2021; 18: 8507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Norman CD, Skinner HA. Ehealth literacy: essential skills for consumer health in a networked world. J Med Internet Res 2006; 8: e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leung AYM, et al. Sense of coherence mediates the relationship between digital health literacy and anxiety about the future in aging population during the COVID-19 pandemic: a path analysis. Aging Ment Health 2021: 1–10. doi: 10.1080/13607863.2020.1870206 [DOI] [PubMed] [Google Scholar]
- 18.Chang BL, et al. Bridging the digital divide: reaching vulnerable populations. J Am Med Inform Assoc 2004; 11: 448–457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clark B, Preto N. Exploring the concept of vulnerability in health care. CMAJ 2018; 190: E308–E309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bracken-Roche D, Bell E, Macdonald MEet al. et al. The concept of ‘vulnerability’ in research ethics: an in-depth analysis of policies and guidelines. Health Res Policy Syst 2017; 15: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aday LA. Health status of vulnerable populations. Annu Rev Public Health 1994; 15: 487–509. [DOI] [PubMed] [Google Scholar]
- 22.de Groot N, Bonsel GJ, Birnie Eet al. et al. Towards a universal concept of vulnerability: broadening the evidence from the elderly to perinatal health using a Delphi approach. PLoS One 2019; 14: e0212633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Association WM. Declaration of Helsinki. Ethical principles for medical research involving human subjects. Jahrbuch für Wissenschaft und Ethik 2009; 14: 233–238. [Google Scholar]
- 24.Greenall M, Kunii O, Thomson Ket al. et al. Reaching vulnerable populations: lessons from the global fund to fight AIDS, Tuberculosis and malaria. Bull World Health Organ 2017; 95: 159–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tangcharoensathien V, Mills A, Palu T. Accelerating health equity: the key role of universal health coverage in the sustainable development goals. BMC Med 2015; 13: 01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vulnerable populations: who are they? Am J Manag Care 2006; 12: S348–S352. [PubMed] [Google Scholar]
- 27.Claeson M, Folger P. in International Encyclopedia of Public Health (ed Harald Kristian Heggenhougen) 197-204 (Academic Press, 2008).
- 28.Jennings B, Arras JD, Barrett DHet al. et al. Emergency ethics. Oxford, United Kingdom; Oxford University Press, 2016. ISBN-13: 9780190270742. doi: 10.1093/med/9780190270742.001.0001 [DOI] [Google Scholar]
- 29.Soomro KA, Kale U, Curtis Ret al. et al. Digital divide among higher education faculty. Int J Educ Technol Higher Educ 2020; 17: 21. [Google Scholar]
- 30.Giuliani M, Papadakos T, Papadakos J. Propelling a New Era of patient education into practice-cancer care post-COVID-19. Int J Radiat Oncol Biol Phys 2020; 108: 404–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jafree SR, Bukhari N, Muzamill Aet al. et al. Digital health literacy intervention to support maternal, child and family health in primary healthcare settings of Pakistan during the age of coronavirus: study protocol for a randomised controlled trial. BMJ Open 2021; 11: e045163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martins Van Jaarsveld G. The effects of COVID-19 Among the elderly population: a case for closing the digital divide. Front Psychiatry 2020; 11: 577427–577427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8: 19–32. [Google Scholar]
- 34.Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010; 5: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.CADTH. COVID-19 Search Strings. Accessed March 9, 2021. https://covid.cadth.ca/literature-searching-tools/cadth-covid-19-search-strings/.
- 36.Bramer WM, Giustini D, de Jonge GBet al. et al. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc 2016; 104: 240–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ouzzani M, Hammady H, Fedorowicz Zet al. et al. Rayyan—a web and mobile app for systematic reviews. Syst Rev 2016; 5: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nowell LS, Norris JM, White DEet al. et al. Thematic analysis. Int J Qual Methods 2017; 16: 1–13. doi: 10.1177/1609406917733847 [DOI] [Google Scholar]
- 39.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 40.King N. Using templates in the thematic analysis of text. In: Essential guide to qualitative methods in organizational research. California, United States: Sage Publication Ltd, 2004, pp.256–270. doi: 10.4135/9781446280119.n21 [DOI] [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff Jet al. et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J 2009; 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Quinn LM, et al. Use of MyDesmond digital education programme to support self-management in people with type 2 diabetes during the COVID-19 pandemic. Diabetic Med 2021; 38: e14469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guven DC, et al. Perspectives, knowledge, and fears of cancer patients about COVID-19. Front Oncol 2020; 10: 1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pasadino F, DeMarco K, Lampert E. Connecting with families through virtual perinatal education during the COVID-19 pandemic. MCN. Am J Maternal Child Nurs 2020; 45: 364–370. [DOI] [PubMed] [Google Scholar]
- 45.Saibene A, et al. Addressing digital divide and elderly acceptance of medical expert systems for healthy ageing. Vol. 2804 (CEUR-WS, 2020).
- 46.Li X, Liu QU. Social Media Use, eHealth literacy, disease knowledge, and preventive behaviors in the COVID-19 pandemic: cross-sectional study on Chinese netizens. J Med Internet Res 2020; 22: e19684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Norgaard O, et al. The e-health literacy framework: a conceptual framework for characterizing e-health users and their interaction with ehealth systems. Knowl Manage E-Learn 2015; 7: 522. [Google Scholar]
- 48.van Tilburg TG, Steinmetz S, Stolte Eet al. et al. Loneliness and mental health during the COVID-19 pandemic: a study among Dutch older adults. J Gerontol, Series B 2020; 76: e249–e255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Choukou MA, Maddahi A, Polyvyana Aet al. et al. Digital health technology for indigenous older adults: a scoping review. Int J Med Inform 2021; 148: 104408. [DOI] [PubMed] [Google Scholar]
- 50.Sixsmith A. COVID-19 and AgeTech. Qual Ageing Older Adults 2020; 21: 247–252. [Google Scholar]
- 51.Voigt-Barbarowicz M, Brütt AL. The agreement between patients’ and healthcare professionals’ assessment of patients’ health literacy – a systematic review. Int J Environ Res Public Health 2020; 17: 2372. doi: 10.3390/ijerph17072372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wildenbos GA, Peute L, Jaspers M. Aging barriers influencing mobile health usability for older adults: a literature based framework (MOLD-US). Int J Med Inform 2018; 114: 66–75. [DOI] [PubMed] [Google Scholar]
- 53.Syed-Abdul S, et al. Misleading health-related information promoted through video-based social media: anorexia on YouTube. J Med Internet Res 2013; 15: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.