Abstract
Background:
Detection of ≥50% diameter stenosis left main coronary artery disease (LMD) has prognostic and therapeutic implications. Noninvasive stress imaging or an exercise tolerance test (ETT) are the most common methods to detect obstructive coronary artery disease, though stress test markers of LMD remain ill-defined.
Objectives:
We sought to identify markers of LMD as detected on coronary computed tomography angiography (CCTA), using clinical and stress testing parameters.
Methods:
This was a post hoc analysis of ISCHEMIA, including randomized and nonrandomized participants who had locally determined moderate or severe ischemia on nonimaging ETT, stress nuclear myocardial perfusion imaging, or stress echocardiography followed by CCTA to exclude LMD. Stress tests were read by core laboratories. Prior coronary artery bypass grafting was an exclusion. In a stepped multivariate model, we identified predictors of LMD, first without and then with stress testing parameters.
Results:
Among 5146 participants (mean age 63 years, 74% male), 414 (8%) had LMD. Predictors of LMD were older age (p<0.001), male sex (p<0.01), absence of prior myocardial infarction (p<0.009), transient ischemic dilatation (TID) of the left ventricle on stress echocardiography (p=0.05), magnitude of ST-segment depression on ETT (p=0.004) and peak metabolic equivalents achieved (METs) on ETT (p=0.001). The models were weakly predictive of LMD (C-index 0.643 and 0.684).
Conclusions:
In patients with moderate or severe ischemia, clinical and stress testing parameters were weakly predictive of LMD on CCTA. For most patients with moderate or severe ischemia, anatomic imaging is needed to rule out LMD.
Keywords: Stress testing, coronary CT angiography, stable ischemic heart disease, coronary artery disease
Condensed Abstract
Detection of ≥50% diameter stenosis left main coronary artery disease (LMD) has both prognostic and therapeutic implications. In this post hoc analysis of 5146 ISCHEMIA randomized and non-randomized participants, we assessed clinical and stress testing predictors of LMD on coronary CT angiography. Models for LMD demonstrated suboptimal prediction overall. Thus for most patients with moderate or severe ischemia, exclusion of LMD will require anatomic imaging with either CCTA or coronary angiography.
Introduction
Detection of significant (≥50%) left main disease (LMD) has major prognostic and therapeutic implications.(1) While the detection of obstructive coronary artery disease (CAD) is important, this is especially true of LMD because current guidelines recommend revascularization to improve survival when LMD is present.(2)
The ISCHEMIA trial, which randomized patients with moderate or severe ischemia to guideline-directed medical therapy vs guideline-directed medical therapy plus optimal revascularization, showed no statistical difference between the groups for the primary composite outcome or the secondary outcome of cardiovascular death or myocardial infarction.(3) However, patients with LMD ≥50% on computed coronary tomographic angiography (CCTA) were excluded from randomization. Hence, detection of LMD during the initial evaluation of patients with myocardial ischemia is important as revascularization remains the guideline-recommended management strategy in these patients. Previous studies that evaluated clinical or functional tests (i.e, stress test) criteria for the identification of LMD are sparse and mostly performed in small populations.(4)
The aim of this post hoc analysis of ISCHEMIA(5) was to explore the markers of LMD using clinical and noninvasive functional parameters and to identify whether functional testing modalities can predict LMD on CCTA.
Study Population
In brief, the ISCHEMIA cohort comprised patients with stable ischemic heart disease and moderate or severe ischemia on clinically indicated stress imaging or severe ischemia on exercise tolerance test (ETT) as determined by enrolling sites and read later at centralized trial core laboratories. Patients were eligible if they were clinically stable, including stable angina or silent ischemia. CCTA was performed to confirm the presence of obstructive CAD and to rule out LMD. Major exclusion criteria included estimated glomerular filtration rate (eGFR) less than 30mL/min/ 1.73m2, myocardial infarction (MI) or unstable angina within 2 months of randomization, left ventricular ejection fraction less than 35%, LMD ≥50% on CCTA, New York Heart Association class III to IV heart failure or exacerbation of chronic heart failure within 6 months, or unacceptable angina despite maximally tolerated medical therapy.(5) Enrolled patients that were not confirmed to be eligible for randomization after additional testing and core laboratory review were excluded from the trial. ISCHEMIA was funded by the National Heart, Lung, and Blood Institute. IRB approval was obtained at the Clinical Coordinating Center (NYU Grossman School of Medicine IRB) and at each coordinating center and site. All participants provided informed consent.
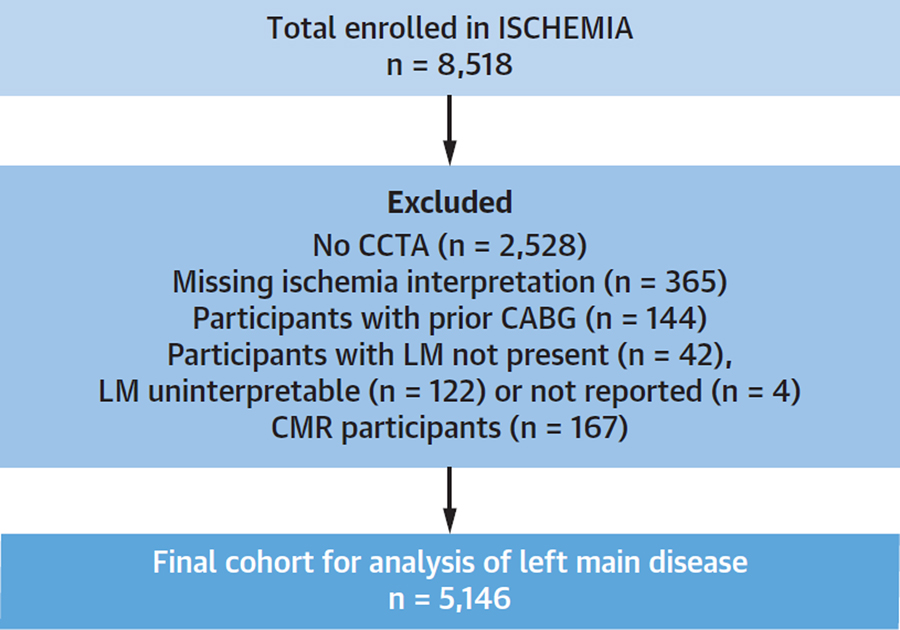
For this analysis, enrolled ISCHEMIA participants with available CCTA interpretation for the presence or absence of LMD and available core laboratory interpretation of ischemia severity were analyzed. Patients with prior coronary artery bypass grafts (CABG) were excluded from this analysis. Patients who had CCTA done before the study were also excluded. Figure 1 depicts how the study population was derived. Stress imaging and ETT eligibility criteria for the ISCHEMIA trial have been previously described.(5) Stress testing details are mentioned in brief below.
Figure 1. Study Flow Diagram.
This analysis included participants enrolled in ISCHEMIA and either excluded from randomization or randomized in the trial. Those without a coronary CT angiogram (CCTA) were excluded, as were participants with missing data for ischemia or left main stenosis. Those with prior coronary artery bypass grafting (CABG) were excluded because the left main is often bypassed. Participants enrolled after stress cardiac magnetic resonance imaging (CMR) were excluded due to inadequate sample size to permit detailed analysis.
Stress testing
Sites were directed to screen and enroll patients with moderate or severe ischemia, as determined locally on a stress test performed for clinical indications, preferably within the prior 3 months. Stress test data (e.g., images and ECG recordings for those undergoing ETT) were transferred electronically to the relevant core laboratory. The core laboratories independently interpreted baseline stress tests for all trial participants. For stress nuclear imaging (single-photon emission computed tomography or positron-emission tomography), mild ischemia was defined as reversible ischemia affecting <10% of the myocardium (summed difference score <7 segments), moderate ischemia was defined as reversible ischemia affecting ≥10% but <14.9% of the myocardium (summed difference score ≥7–9) and severe ischemia was defined as >15% ischemia (summed difference score ≥10). For stress echocardiography, mild ischemia was defined as <3 segments with reversible wall motion abnormalities in a 16 segment left ventricular model, moderate ischemia was defined as 3 segments with severe inducible wall motion abnormalities and severe ischemia as ≥ 4 segments with severe inducible wall motion abnormalities. Exercise testing entry criteria for severe ischemia required all of the following: (1) history of stable or exercise test-induced typical angina; (2) an interpretable resting ECG (e.g., no resting ST segment depression ≥1 mm); (3) at least 2 leads showing new exercise-induced ST segment depression ≥1.5 mm or a single lead ≥2 mm as compared to the baseline tracing occurring at ≤7 METs or peak heart rate <75% of age-predicted maximum confirmed by the ECG core-lab laboratory and (4) anatomic>70% stenosis of a major coronary artery on CCTA. We did not analyze cardiac magnetic resonance (CMR) data in relation to LMD due to the low number of patients enrolled after this stress test modality.
CCTA
CCTA was interpreted centrally by a core laboratory, without regard to stress test findings or clinical information. At least two readers evaluated the presence and severity of LMD, with any disagreements resolved by the core laboratory director.
Statistical Analysis
Presence of LMD was defined as LMD stenosis ≥50%. Continuous variables are presented as medians (Q1, Q3) and differences compared using the Wilcoxon rank-sum test or Student’s t-test, as appropriate. Categorical variables are presented as counts (raw percentages) and differences compared using Pearson’s chi-square test or Fisher’s exact test if cell frequencies were not sufficient. A multivariable logistic regression model was used to assess the association between the following clinical characteristics and LMD: age at enrollment, sex, race/ethnicity, hypertension, diabetes, smoking status, prior MI and eGFR (ml/min). An additional multivariable logistic regression model assessed the association between imaging and stress test variables and disease status, adjusting for the clinical characteristics. Specific imaging and stress test variables included: the number of ischemic segments on SE, number of infarcted segments on SE, summed differences score on nuclear, TID on nuclear, TID on SE, ST depression on ETT, peak exercise METs on ETT, severe or moderate anterior ischemia on nuclear or SE and LAD and LCX ischemia on nuclear or SE. Both models combined data from imaging and ETT patients and the latter model included a sex by modality interaction term. Multiple imputation by chained equations was used to impute missing covariates for the logistic regression models. Imaging and stress test variables were set to a constant value for patients that did not undergo the particular test; the odds ratios for the imaging and stress test indicators are not reported due to lack of interpretability. The model’s ability to distinguish between patients with relatively high versus low likelihood of LMD > 50% was assessed by calculating the C-index and by plotting the distribution of predicted probabilities of LMD > 50% within each modality. Predicted probabilities of LMD >50% from the full model were further analyzed with the goal of identifying non-rare subgroups with a low average probability of LMD >50%. The search for subgroups was performed both in the combined cohort and separately within each modality. In the combined cohort, candidate subgroup factors included all predictor variables with a p-value <0.2 in the full multivariable model plus the core-laboratory determined degree of ischemia (none/mild/moderate/severe). In modality-specific analyses, we used modality-specific predictors in place of the degree of ischemia. Subgroups were identified by calculating the average predicted probability of LMD >50% across patients within each level of each candidate subgroup factor and within groups formed by the cross-classification of 2 or more candidate subgroup factors. Subgroups were reported here if they included at least 350 patients and if the average predicted probability was ≤2.5%. To account for statistical uncertainty in these estimates, we present results along with 95% bootstrap confidence intervals.
RESULTS
A total of 5146 patients were enrolled after stress testing who underwent CCTA, who did not have prior CABG, and had interpretable ischemia testing using a modality other than CMR imaging (Figure 1), of whom 414 (8.0%) had LMD. The median age was 63 years and 74% were males (Table 1). Participants with LMD were older, more likely to be male, of Asian ethnicity, and had a lower prevalence of prior MI and lower median eGFR. There was no meaningful difference between those with or without LMD in the prevalence of diabetes mellitus, systemic hypertension and history of smoking. The proportion of LMD patients undergoing nuclear imaging, stress echocardiography and ETT were 38%, 22% and 40%, respectively (p<0.001 vs. without LM). Those with LMD had a greater degree of inducible ischemia than those without LMD, on all stress test modalities. Transient ischemic dilatation (TID) was observed more often in patients with as compared to those without LMD among those undergoing stress echocardiography but not significantly more often in patients undergoing nuclear imaging. Patients with LMD had a lower exercise capacity on ETT than those without LMD. The proportion of LMD patients with moderate or severe anterior ischemia was higher among patients undergoing stress echocardiography and nuclear imaging. The proportions of patients with ischemia in both the left anterior descending (LAD) and circumflex (LCX) territories were not different in patients with and without LMD by nuclear imaging but were significantly more in LMD group by stress echocardiography. Among patients who underwent nuclear imaging, 45% underwent exercise testing and 55% received pharmacological agents; the proportions in stress echocardiography were 77% and 23%, respectively. Exercise hemodynamics were not routinely available for stress imaging tests.
TABLE 1.
Baseline Clinical Characteristics of the Study Population with and without LMD
| Characteristic | Overall N= 5146 | Left main stenosis ≥ 50% N=414 |
No Left main stenosis ≥ 50% N=4732 |
P-Value |
|---|---|---|---|---|
| Demographics | ||||
| Age at Enrollment | 63.4 (56.6 – 69.7) | 64.6 (59.1 – 70.5) | 63.3 (56.4 – 69.7) | <.001 |
| Male | 3816 (74.2%) | 367 (88.6%) | 3449 (72.9%) | <.001 |
| Race/Ethnicity | 0.008 | |||
| Non-Hispanic White | 2464/4769 (51.7%) | 189/384 (49.2%) | 2275/4385 (51.9%) | |
| Non-Hispanic Asian | 1310/4769 (27.5%) | 130/384 (33.9%) | 1180/4385 (26.9%) | |
| Other | 995/4769 (20.9%) | 65/384 (16.9%) | 930/4385 (21.2%) | |
| Cardiovascular Risk Factors | ||||
| Hypertension | 3472/5120 (67.8%) | 268/412 (65.0%) | 3204/4708 (68.1%) | 0.210 |
| Diabetes | 1888 (36.7%) | 146 (35.3%) | 1742 (36.8%) | 0.531 |
| Cigarette Smoking | 0.693 | |||
| Never Smoked | 2365/5017 (47.1%) | 187/380 (49.2%) | 2178/4637 (47.0%) | |
| Former Smoker | 2021/5017 (40.3%) | 148/380 (38.9%) | 1873/4637 (40.4%) | |
| Current Smoker | 631/5017 (12.6%) | 45/380 (11.8%) | 586/4637 (12.6%) | |
| Cardiovascular Disease History | ||||
| Prior MI | 684/5106 (13.4%) | 36/400 (9.0%) | 648/4706 (13.8%) | 0.007 |
| Baseline Labs | ||||
| eGFR (ml/min) | 86 (73 – 101) | 83 (73 – 99) | 86 (73 – 101) | 0.511 |
| Imaging and Stress Test | ||||
| Modality | <.001 | |||
| Nuclear SPECT/PET | 2286 (44.4%) | 158(38.2%) | 2128 (45.0%) | |
| SE | 1279 (24.9%) | 89 (21.5%) | 1190 (25.0%) | |
| ETT | 1581(30.7%) | 167 (40.3%) | 1414 (29.9%) | |
| Number of ischemic segments on SE | 4 (3 – 5) | 4 (3 – 6) | 4 (3 – 5) | 0.008 |
| Number of infarcted segments on SE | 0 (0 – 0) | 0 (0 – 0) | 0 (0 – 0) | 0.311 |
| Summed difference score on SPECT | 8 (7 – 11) | 9 (7 – 12) | 8 (7 – 11) | <.001 |
| Summed stress score on SPECT | 9 (7 – 14) | 11 (8 – 15) | 9 (7 – 14) | 0.007 |
| TID (Transient ischemic dilation in the LV) on SPECT | 309/2286 (13.5%) | 26/158 (16.5%) | 283/2128 (13.3%) | 0.263 |
| TID (Transient ischemic dilation in the LV) on SE | 349/1279 (27.3%) | 38/89 (42.7%) | 311/1190 (26.1%) | <.001 |
| Maximum ST Depression in Any Lead on ETT, mm | 2.5 (2.0 – 3.1) | 2.7 (2.2 – 3.3) | 2.4 (2.0 – 3.1) | 0.001 |
| Peak METs on ETT | <.001 | |||
| < 7 | 579/1167 (49.6%) | 48/68 (70.6%) | 531/1099 (48.3%) | |
| ≥ 7 | 588/1167 (50.4%) | 20/68 (29.4%) | 568/1099 (51.7%) | |
| Severe or moderate anterior ischemia on SPECT | 683/2285 (29.9%) | 58/158 (36.7%) | 625/2127 (29.4%) | 0.052 |
| Severe or moderate anterior ischemia on SE | 422/1277 (33.0%) | 40/89 (44.9%) | 382/1188 (32.2%) | 0.013 |
| LAD + LCX ischemia on SPECT | 201/2286 (8.8%) | 16/158 (10.1%) | 185/2128 (8.7%) | 0.539 |
| LAD + LCX ischemia on SE | 211/5146 (4.1%) | 22/89 (24.7%) | 189/1190 (15.9%) | 0.03 |
| Coronary Anatomy on CCTA | ||||
| Number of Diseased Vessels with ≥70% stenosis | <.001 | |||
| 0 | 1016/5146 (19.7) | 15/414 (3.6) | 1001/4732 (21.2) | |
| 1 | 1048/5146 (20.4) | 49/414 (11.8) | 999/4732 (21.1) | |
| 2 | 776/5146 (15.1) | 97/414 (23.4) | 679/4732 (14.3) | |
| 3 | 551/5146 (10.7) | 113/414 (27.3) | 438/4732 (9.3) | |
| Non-evaluable | 1755/5146 (34.1) | 140/414 (33.8) | 1615/4732 (34.1) | |
| Multi-vessel Disease with ≥70% stenosis | <.001 | |||
| No | 2511/5146 (48.8) | 86/414 (20.8) | 2425/4732 (51.2) | |
| Yes | 1633/5146 (31.7) | 256/414 (61.8) | 1377/4732 (29.1) | |
| Not evaluable | 1002/5146 (19.5) | 72/414 (17.4) | 930/4732 (19.7) |
Continuous variables are presented as medians (Q1, Q3) and categorical variables are presented as counts (column percentages). The number of diseased vessels was not evaluable if pre-determined key segments were not interpretable for stenosis severity.
Logistic regression analysis (Table 2) indicated that among clinical factors, older age, male sex, Asian race and lack of prior MI were the only significant predictors of LMD. The C index for the clinical logistic model was 0.643. Among imaging and exercise parameters, after adjusting for clinical factors (Table 3), significant predictors of LMD were older age, male sex, lack of prior MI, greater ST depression and lower peak METs on ETT and TID on stress echocardiography. Nuclear imaging parameters were not independently associated with LMD. The C index for this model was only marginally but statistically significantly improved compared with the clinical model, to 0.684 (p<0.001). Sensitivity analysis performed after excluding patients with prior MI showed that TID on stress echocardiography was no longer significant, with no change in C-index.
TABLE 2 -.
RESULTS FROM CLINICAL LOGISTIC MODEL FOR LMD
| Left main stenosis ≥ 50% | |||
|---|---|---|---|
| Variable | OR | 95% CI | P-value |
| Age at Enrolment, years1 | <.001 | ||
| 65 versus 55 | 1.42 | 1.21 – 1.66 | |
| 75 versus 55 | 1.56 | 1.21 – 2.01 | |
| Female Sex | 0.32 | 0.24 – 0.44 | <.001 |
| Race/Ethnicity | 0.028 | ||
| Non-Hispanic White | ref | ||
| Non-Hispanic Asian | 1.34 | 1.04 – 1.73 | |
| Other | 0.90 | 0.67 – 1.2 | |
| Hypertension | 0.93 | 0.74 – 1.18 | 0.560 |
| Diabetes | 0.88 | 0.71 – 1.1 | 0.268 |
| Cigarette Smoking | 0.219 | ||
| Never Smoked | ref | ||
| Former Smoker | 0.81 | 0.64 – 1.03 | |
| Current Smoker | 0.92 | 0.65 – 1.3 | |
| Prior MI | 0.61 | 0.42 – 0.88 | 0.008 |
| eGFR (ml/min)1 | 0.908 | ||
| 60 versus 120 | 1.05 | 0.76 – 1.44 | |
| 90 versus 120 | 0.98 | 0.77 – 1.24 | |
Modeled as a restricted cubic spline
C-index for Left main stenosis ≥ 50%: 0.643
TABLE 3.
RESULTS FROM STRESS TEST MODEL FOR LMD ADJUSTING FOR CLINICAL FACTORS
| Left main stenosis ≥ 50% | |||
|---|---|---|---|
| Clinical Variables | OR | 95% CI | P-value |
| Age at Enrolment, years 1 | <.001 | ||
| 65 versus 55 | 1.40 | 1.19 – 1.65 | |
| 75 versus 55 | 1.56 | 1.21 – 2.01 | |
| Female Sex among nuclear modality | 0.26 | 0.14 – 0.48 | <.001 |
| Race/Ethnicity | 0.489 | ||
| Non-Hispanic White | ref | ||
| Non-Hispanic Asian | 1.01 | 0.74 – 1.37 | |
| Other | 0.84 | 0.62 – 1.14 | |
| Hypertension | 0.95 | 0.75 – 1.2 | 0.681 |
| Diabetes | 0.87 | 0.70 – 1.09 | 0.217 |
| Cigarette Smoking | 0.36 | ||
| Never Smoked | ref | ||
| Former Smoker | 0.84 | 0.66 – 1.07 | |
| Current Smoker | 0.97 | 0.67 – 1.35 | |
| Prior MI | 0.61 | 0.42 – 0.88 | 0.009 |
| eGFR (ml/min)1 | 0.977 | ||
| 60 versus 120 | 1.03 | 0.74 – 1.43 | |
| 90 versus 120 | 1.00 | 0.78 – 1.27 | |
| Stress Test Variables | |||
| Number of ischemic segments on stress echo, per 1 segment increase | 1.10 | 0.96 – 1.25 | 0.158 |
| Number of infarcted segments on stress echo, per 1 segment increase | 1.08 | 0.94 – 1.25 | 0.268 |
| Summed difference score on nuclear ≥ 10 | 1.49 | 0.95 – 2.33 | 0.080 |
| Summed stress score on nuclear | 1.00 | 0.96 – 1.04 | 0.977 |
| TID (Transient ischemic dilation in the LV) on nuclear | 1.01 | 0.63 – 1.62 | 0.965 |
| TID (Transient ischemic dilation in the LV) on stress echo | 1.63 | 1 – 2.66 | 0.049 |
| Maximum ST Depression in Any Lead on ETT, per 1 mm increase | 1.28 | 1.08 – 1.52 | 0.004 |
| Peak exercise METs on ETT 3 | <.001 | ||
| Peak exercise METs up to 5 | 0.82 | 0.58 – 1.17 | |
| Peak exercise METs above 5 | 0.74 | 0.63 – 0.86 | |
| Severe or Moderate Anterior Ischemia on nuclear | 1.32 | 0.91 – 1.92 | 0.141 |
| Severe or Moderate Anterior Ischemia on stress echo | 1.04 | 0.58 – 1.84 | 0.904 |
| LAD + LCX ischemia on nuclear | 1.32 | 0.76 – 2.32 | 0.327 |
| LAD + LCX ischemia on stress echo | 1.24 | 0.69 – 2.22 | 0.475 |
Modeled as a restricted cubic spline.
Note: There is a sex by modality interaction term in model. The odds ratios for modality by sex are not presented in this table due to the modality specific covariates.
The sex by modality interaction p-value in LM>= 50% model is: 0.15
Modeled as a linear spline.
Cindex for Left main stenosis ≥ 50%: 0.684
Joint test for Imaging and Stress Test variables is: <.001
ETT = exercise tolerance testing (non-imaging); METs = metabolic equivalents achieved during stress testing
Analysis was also performed based on ≥70% LMD (n=82 patients). The proportion of enrolled participants with ≥70% LMD was 1.1% with nuclear imaging, 1.3% with stress echocardiography and 2.7% with ETT (p<0.001). Due to the limited number of patients with LMD, only modality-specific variables were included in the models; clinical characteristics were not included as adjustment variables. ETT parameters of ST depression (p=0.02) and lower peak workload (p=0.04) were associated with ≥70% LMD, but neither nuclear nor stress echocardiography data provided incremental information over clinical parameters in ≥70% LMD prediction.
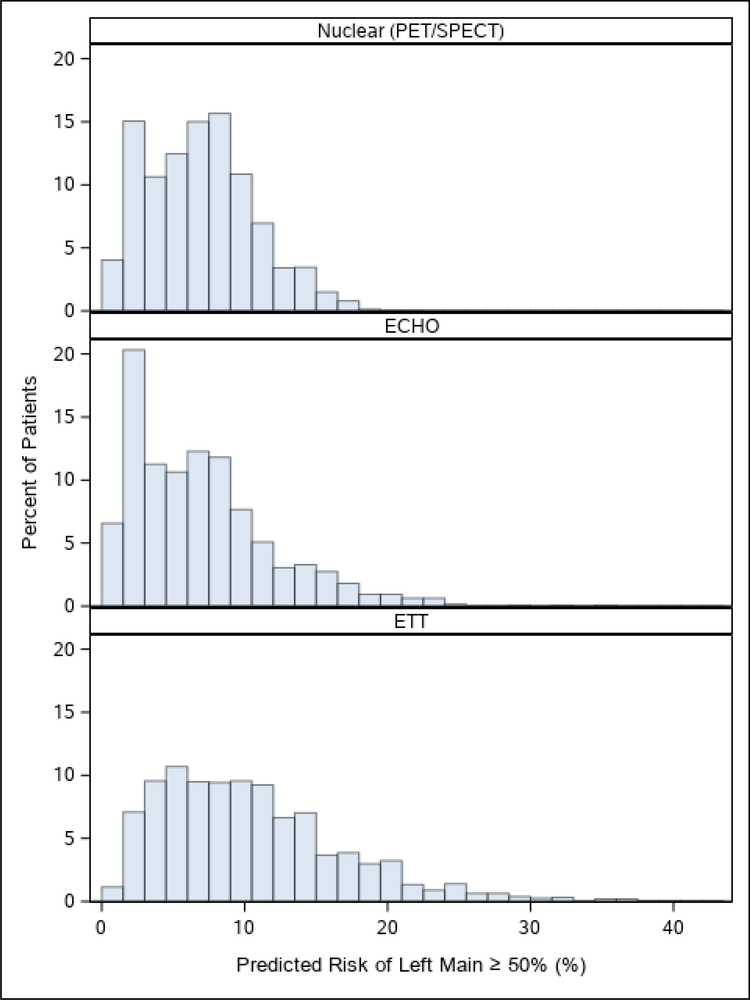
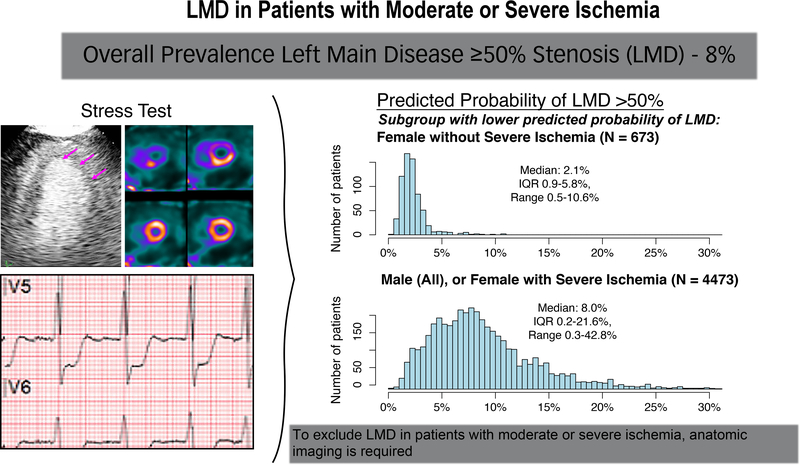
Figure 2 illustrates the distribution of the predicted risk estimates of LMD, ranging from less than 2% through over 30%, by stress test modality. Tables 4 and 5 depict the subgroups defined by combinations of clinical and imaging parameters that were associated with less than 2.5% probability of LMD on average. Table 4 shows the combined effect of nuclear and stress echocardiography on the model, with ischemia categorized as severe, moderate, mild or none. The variables considered were age, sex, prior MI and the degree of ischemia. The simplest combination of clinical features that excluded LMD with more than 97.5% probability on average in an adequately sized subgroup was female sex with mild or moderate ischemia (Central Illustration). Among remaining participants (women with severe ischemia, and men), the prevalence of LMD was 8.9%. Table 5 shows the modality-specific parameters (nuclear, stress echocardiography, ETT) associated with LMD. Clinical variables were the same as in the clinical analysis in Table 4. There were no ETT subgroups of the specified size with ≤2.5% predicted likelihood of LMD.
Figure 2. Distribution of the predicted risk estimates of left main disease (LMD).
The sample was stratified by qualifying stress test modality, whether nuclear, echocardiography (echo) or exercise tolerance testing (ETT). The predicted risk of significant LMD, defined as ≥50% on coronary CT angiography, ranged from less than 2% through over 30%. The proportion of participants with each level of predicted risk is shown.
TABLE 4.
SUBGROUPS WITH AN AVERAGE MODEL-PREDICTED PROBABILITY OF LMD THAT IS ≤ 2.5% (COMBINED COHORT)
| Subgroup definition | N | Mean Predicted Probability (Bootstrapped 95% confidence interval) |
|---|---|---|
| Female; No, Mild or Moderate Ischemia | 673 | 0.023 (0.019–0.024) |
| Female; Mild or Moderate Ischemia | 577 | 0.023 (0.019–0.024) |
| Female; Mild or Moderate Ischemia; Age ≤ 75 | 501 | 0.022 (0.018–0.023) |
| Female; Mild or Moderate Ischemia; Age > 55 | 480 | 0.024 (0.020–0.025) |
| Female; Moderate Ischemia | 444 | 0.024 (0.020–0.025) |
| Female; Moderate Ischemia; Age > 55 | 376 | 0.025 (0020–0.026) |
The following variables were used to define subgroups: Sex, age (categorized as ≤55, ≤65, and ≤75), prior MI and degree of ischemia (none, none/mild, none/mild/moderate). Only subgroups including at least 350 participants were considered.
TABLE 5.
SUBGROUPS WITH AN AVERAGE MODEL-PREDICTED PROBABILITY OF LMD THAT IS ≤ 2.5% DEFINED USING MODALITY SPECIFIC VARIABLES
| Subgroup definition | N | Mean Predicted Probability (Bootstrapped 95% confidence interval) |
|---|---|---|
| Female; Nuclear | 508 | 0.024 (0.018–0.026) |
| Female; Stress Echo | 446 | 0.025 (0.019–0.028) |
| Female; Nuclear; Summed difference score <10 | 389 | 0.021 (0.016–0.023) |
| Female; Stress Echo; Number of ischemic segments ≤5 | 361 | 0.021 (0.016–0.024) |
The following variables were used to define subgroups: Sex, age (categorized as ≤55, ≤65, and ≤75), prior MI, imaging modality (Nuclear, Stress Echo, and ETT). Modality specific variables included: Summed difference score on Nuclear≥ 10; Severe or Moderate Anterior Ischemia on Nuclear; Number of ischemic segments (categorized as ≤3, ≤5) on Stress Echo; TID (Transient ischemic dilation in the LV) on Stress Echo; Maximum ST Depression in Any Lead on ETT (categorized as ≤2, ≤3). Only subgroups including at least 350 participants were considered.
Central Illustration. LMD in Patients with Moderate or Severe Ischemia.
Enrolled participants in ISCHEMIA had moderate or severe ischemia on a stress test (e.g., stress echocardiography, upper left, stress nuclear, upper right of stress test panel, or exercise tolerance testing, bottom left). Those with LMD on coronary computed tomography angiography (CCTA) after enrollment were excluded from randomization.
Top right histogram, distribution of predicted probability of LMD among females without severe ischemia.Half of the patients in this subgroup had predicted probability of LMD >2.1%.
Histogram, bottom right, distribution of predicted probability of LMD among males with any degree of ischemia, or among females with severe ischemia.”
Discussion
This large study assessed commonly used non-invasive stress modalities for the prediction of significant LMD as assessed by CCTA among patients with a relatively high likelihood of LMD, approximately 8%. We demonstrated that stress testing offered only modest incremental value over clinical parameters for prediction of LMD in this cohort of patients with moderate or severe ischemia as determined by sites on clinically indicated stress testing before enrollment in the ISCHEMIA trial. Overall, the predictive value was suboptimal. ISCHEMIA showed that high-risk stable ischemic heart disease patients with significant inducible ischemia on noninvasive testing did not have a statistically lower rate of the composite primary outcome or of cardiovascular death and MI when routine revascularization was added to guideline-directed medical therapy as compared to guideline-directed medical therapy alone.(3) Application of these results to clinical practice, however, may be challenging when LMD status is not known, since patients with LMD were excluded from randomization in the ISCHEMIA trial. Though the results of ISCHEMIA and other strategy trials(6,7) indicate that the majority of patients without LMD can be managed conservatively, it is nonetheless important to exclude LMD. Available studies indicate that patients with LMD benefit from revascularization, though these trials predated effective medical therapy for risk reduction.(8) A pre-trial survey of cardiologists indicated a lack of equipoise regarding revascularization for LMD.(9)
Previous studies have identified stress testing parameters that are associated with higher likelihood of LMD. To our knowledge, this is the first study attempting to identify predictors of LMD among patients with clinically diagnosed moderate or severe ischemia, a group with a relatively high likelihood of LMD. In contrast, the prevalence of LMD in the CONFIRM registry in patients with suspected angina without known CAD was only 0.9%. (10) We found that stress test parameters were not adequate for ruling out LMD. Though TID on stress echocardiography and severe ST depression and low workload on ETT were independent predictors of LMD beyond clinical variables and independent of other imaging markers of LMD disease, their incremental predictive value was modest. The imaging findings are consistent with other, smaller studies(4) and can be explained by the fact that in LMD, hyperemic blood flow is rarely affected to the same degree in the LAD and left circumflex territory. Indeed, distal LMD disease may preferentially reduce blood flow in the LAD as the plaque frequently extends into the LAD vs left circumflex territory.(11) Furthermore, it is recognized that it may be difficult to discriminate LMD from the disease in the LAD and left circumflex coronary arteries without LMD commonly known as left main equivalent.(12) Patients with LMD have a high prevalence of associated multivessel disease. This is highly relevant in the ISCHEMIA trial, in which 66% of patients undergoing CCTA had multivessel CAD.(3)
There are also imaging specific issues that may have affected the discriminatory power of the imaging modalities. Nuclear imaging (particularly SPECT, which was the major nuclear modality in the ISCHEMIA trial) depends on a relative myocardial blood flow difference of at least 2:1 ratio to detect reduced perfusion. Thus, differential reduction in flow in the LAD vs left circumflex territory may not be detected. On the other hand, a similar reduction in perfusion in large areas of the left ventricle (balanced ischemia) may result in normalization of tracer uptake in ischemic segments and thus may underestimate ischemia.(13) Perfusion defect patterns in these studies identified only 19%−29% of patients with LMD.(14) The sensitivity of SPECT compared to stress echocardiography for the detection of LMD tended to be lower for the same reasons as stated above.(4,14). Exercise stress echocardiography has previously been reported to have similar high sensitivity for the detection of LMD compared to dobutamine stress echocardiography.(15) In our study, neither stress echocardiography nor SPECT demonstrated a significant relationship between increasing ischemia severity and LMD.
Transient ischemic dilation as detected by stress echocardiography, but not SPECT, was independently associated with LMD. Transient ischemic dilation was more commonly observed during stress echocardiography than during nuclear imaging in this study, perhaps related to a greater proportion of patients undergoing exercise rather than pharmacological stress with stress echocardiography in contrast with the proportions used for nuclear imaging.(15) It is noteworthy that exercise-induced ST depression and reduced workload by ETT was associated with LMD. Unfortunately, we could not analyze exercise time and hemodynamics in patients undergoing stress imaging in this study, and therefore cannot comment on whether these parameters would have refined risk prediction.
Given that the presence of LMD is a critical factor in selection for revascularization, particularly after publication of the main ISCHEMIA results, we explored clinical and stress test variables that could be used in combination to rule out LMD. Female sex alone was significantly associated with lower likelihood of LMD in patients with moderate or severe ischemia on either nuclear imaging or stress echocardiography, but female patients undergoing exercise tolerance testing had a slightly higher probability of LMD not meeting our predetermined threshold. Further, there was substantial variability in predicted risk of LMD even within the lower risk female subsets. There was no subgroup of men with low likelihood of LMD meeting our predetermined sample size, regardless of stress testing results. The subgroups with the lowest average risk of LMD were female sex with induced ischemia with <10 score by stress nuclear and female sex with <5 segments by stress echocardiography. Unfortunately, these two subgroups were small, 7.6% and 7%, respectively. Our finding of lower likelihood of LMD in patients with prior MI may be related to anatomic coronary imaging at the time of the prior MI; if LMD was found then, the patient would not be considered eligible for the trial.
Limitations
We analyzed left main stenosis using the 50% threshold, but not all 50–70% left main stenosis may be flow limiting. The population studied was comprised of patients who were enrolled following site-interpreted moderate or severe ischemia by imaging or severe ischemia ETT criteria, and on core laboratory review, 24% of stress imaging tests submitted by sites showed mild or no ischemia, and 23% of ETTs showed less than severe ischemia.(16)These proportions were higher than in the randomized trial cohort.(16) Exercise hemodynamic data were not available in enough patients with stress imaging to permit inclusion into this analysis. We used CCTA to define LMD. It is known that CCTA and invasive coronary angiography may not yield identical results due to inherent differences in the techniques. CCTA may overestimate stenosis severity(12). Calcification may also obscure stenosis assessment by CCTA. Our sites did not use echocardiography to identify flow in the LM coronary artery, though movement artifact can compromise its ability to consistently image the LM(17). In another post-hoc analysis of the ISCHEMIA trial despite high concordance (97.1%), when the 1728 patients in whom CCTA showed no significant left main disease underwent invasive coronary angiography, 2.9% of patients had ≥50% LMD, which may have implications regarding which anatomic testing may be performed for the exclusion of LMD.(12)
Conclusions
In patients with moderate or severe inducible ischemia who underwent CCTA in this analysis, the prevalence of left main stenosis ≥50% was 8%. Transient ischemic dilation by stress echocardiography, and the magnitude of ST depression and low achieved workload by ETT, were associated with LMD independent of clinical factors, but the discriminatory capacity of the model was modest. Women with a lower burden of ischemia by either stress nuclear or stress echocardiography had a very low predicted likelihood of LMD, on average 2.3%. Thus for most patients with moderate or severe ischemia, exclusion of LMD will require anatomic imaging with either CCTA or invasive coronary angiography.
Clinical Implications
It is desirable for clinicians to know whether a patient with stable ischemic heart disease has significant left main stenosis because guidelines recommend revascularization to improve survival in patients with LMD. Among patients with moderate-severe ischemia who were considered for initial conservative therapy, clinical and stress testing parameters were inadequate for ruling out LMD with a high degree of certainty overall. There was high concordance of CCTA and invasive angiography for LMD in ISCHEMIA. Thus for most patients, exclusion of LMD will require anatomic imaging, with CCTA or conventional invasive angiography.
CLINICAL PERSPECTIVES.
Competency in Medical Knowledge:
Among patients with moderate or severe ischemia on stress testing, the likelihood of left main coronary artery disease (LMD) is 8%, but the predictive value of clinical assessment and stress testing is limited, and anatomic imaging is necessary for accurate identification of LMD.
Translational Outlook:
Subgroups of patients with LMD in prior trials comparing revascularization to medical therapy have been small in size and predated effective preventive medical therapy. Future trials may consider inclusion of patients with LMD.
Sources of Funding:
NIH grants U01HL105907, U01HL105462, U01HL105561, U01HL105565
Disclosure Statements:
Dr. Roxy Senior reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Harmony R. Reynolds reports grants from National Heart, Lung, and Blood Institute during the conduct of the study; non-financial support from Abbott Vascular, non-financial support from Siemens, non-financial support from BioTelemetry, outside the submitted work;
Dr. James K. Min reports grants from National Heart, Lung and Blood Institute during the conduct of the study; also receives grants from CLEERLY INC., GE HEALTHCARE ARINETA, outside the submitted work.
Dr. Daniel S. Berman reports grants from National Heart, Lung, and Blood Institute during the conduct of the study; reports grants from GE, CSMC Heartflow, and Bayer; receives software royalties from Cedars-Sinai Medical Center outside the submitted work.
Dr. Michael H. Picard reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Bernard R. Chaitman reports grants from National Heart, Lung, and Blood Institute during the conduct of the study; personal fees from Merck, NovoNordisk, Lilly,Johnson and Johnson, Daiichi Sankyo, Imbria, Xylocor, Sanofi, Tricida, and Xylocor outside the submitted work;
Dr. Leslee J. Shaw reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Courtney B. Page reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Sajeev C. Govindan reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Jose Lopez Sendon reports grants from National Heart, Lung, and Blood Institute during the conduct of the study; grants from Bayer, Merck and Amgen; grants and personal fees from Pfizer, Menarini, Sanofi, Boeringher Infleheim outside the submitted work. Dr. Jesus Peteiro reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Gupreet S. Wander reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Jaroslaw Drozdz reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Jose Marin-Neto reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Joseph B. Selvanayagam reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Jonathan D. Newman reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Christophe Thuaire reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Johann Christopher reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. James J. Jang reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Raymond Y. Kwong reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Sripal Bangalore reports grants from National Heart, Lung, and Blood Institute, during the conduct of the study; grants and personal fees from Abbott Vascular, personal fees from Biotronik, Pfizer, Amgen, and Reata outside the submitted work.
Dr. Gregg W. Stone reports grants and personal fees from National Heart, Lung, and Blood Institute, during the conduct of the study; personal fees from Terumo, personal fees from Amaranth, personal fees from Shockwave, personal fees and other from Valfix, personal fees from TherOx, personal fees from Reva, personal fees from Vascular Dynamics, personal fees from Robocath, personal fees from HeartFlow, personal fees from Gore, personal fees from Ablative Solutions, personal fees from Matrizyme, personal fees from Miracor, personal fees from Neovasc, personal fees from V-wave, personal fees from Abiomed, personal fees from Claret, personal fees from Sirtex, personal fees and other from Ancora, personal fees and other from Qool Therapeutics, other from Cagent, other from Applied Therapeutics, other from Biostar family of funds, other from MedFocus family of funds, personal fees and other from SpectraWave, personal fees from MAIA Pharmaceuticals, personal fees and other from Orchestra Biomed, other from Aria, personal fees from Vectorious, other from Cardiac Success, outside the submitted work;
Dr. Sean M. O’Brien reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. William E. Boden reports grants from National Heart, Lung, and Blood Institute, during the conduct of the study; grants from Abbvie, grants from Amarin, grants from Amgen, personal fees from Amgen, personal fees from Cleveland Clinic Clinical Coordinating Center, personal fees from Janssen, outside the submitted work;
Dr. David J. Maron reports grants from National Heart, Lung, and Blood Institute during the conduct of the study.
Dr. Judith S. Hochman is PI for the ISCHEMIA trial for which, in addition to support by National Heart, Lung, and Blood Institute grant, devices and medications were provided by Abbott Vascular; Medtronic, Inc.; Abbott Laboratories (formerly St. Jude Medical, Inc); Royal Philips NV (formerly Volcano Corporation); Arbor Pharmaceuticals, LLC; AstraZeneca Pharmaceuticals, LP; Merck Sharp & Dohme Corp.; Omron Healthcare, Inc, Sunovion Pharmaceuticals, Inc. Espero BioPharma; and Amgen, Inc; and financial donations from Arbor Pharmaceuticals LLC and AstraZeneca Pharmaceuticals LP.
Disclaimer:
This article refers to work supported by National Heart, Lung, and Blood Institute grant U01HL105907, U01HL105462, U01HL105561, U01HL105565; device donations from Abbott Vascular; Medtronic, Inc.; St. Jude Medical, Inc.; Volcano Corporation; and Omron Healthcare, Inc.; medications provided by Amgen Inc; Arbor Pharmaceuticals, LLC; AstraZeneca Pharmaceuticals, LP; Merck Sharp & Dohme Corp.; and by financial donations from Arbor Pharmaceuticals LLC and AstraZeneca Pharmaceuticals LP. The content of this manuscript is solely the responsibility of the authors and does not necessarily reflect the views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the United States Department of Health and Human Services.
This project was supported in part by Clinical Translational Science Award Nos. 11UL1 TR001445 and UL1 TR002243 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences, the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the Department of Health and Human Services.
Abbreviations
- CAD
coronary artery disease
- CCTA
computed coronary tomographic angiography
- ECG
electrocardiography
- ETT
exercise tolerance test
- ISCHEMIA
International Study of Comparative Health Effectiveness With Medical and Invasive Approaches
- LAD
left anterior descending coronary artery
- LCX
left circumflex coronary artery
- LMD
left main coronary artery disease with ≥50% diameter stenosis SPECT = single photon emission computed tomography
I. ISCHEMIA Committee, CCC, Trial-Related Personnel
Past and Current Committee Members
Leadership Committee
Judith S. Hochman (Chair)
David J. Maron (Co-Chair)
William Boden (Co-Principal Investigator)
Bruce Ferguson (Co-Principal Investigator)
Robert Harrington (Co-Principal Investigator)
Gregg W. Stone (Co-Principal Investigator)
David Williams (Co-Principal Investigator)
Executive Committee
Judith S. Hochman (Chair)
David J. Maron (Co-Chair)
Karen P. Alexander
Sripal Bangalore
Jeffrey Berger
William Boden
Robert Harrington
Daniel Mark
Sean M. O'Brien
Harmony R. Reynolds
Yves Rosenberg
Leslee J. Shaw
John Spertus
Gregg W. Stone
Steering Committee
Judith S. Hochman (Chair)
David J. Maron (Co-Chair)
Members of Executive Committee
Christie Ballantyne*
Daniel Berman
Rafael Beyar*
Balram Bhargava
Chris Buller*
Antonio (Tony) Carvalho**
Bernard R. Chaitman
Rafael Diaz*
Rolf Doerr
Vladimir Dzavik
Bruce Ferguson
Shaun Goodman
Gilbert Gosselin
Rory Hachamovitch*
Christian Hamm*
Claes Held
Malte Helm*
Kurt Huber*
Lixin Jiang
Matyas Keltai
Shun Kohsaka
Irene Lang*
Renato Lopes
Jose Lopez-Sendon
Aldo Maggioni
John Mancini
C. Noel Bairey Merz
James Min
Eric Peterson*
Michael H. Picard
Witold Ruzyllo
Joseph Selvanayagam
Roxy Senior
Tali Sharir
Gabriel Steg
Hanna Szwed
Frans Van de Werf*
William Weintraub
Harvey White
David Williams
Optimal Medical Therapy Committee
William Boden (Co-Chair)
David J. Maron (Co-Chair)
Christie Ballantyne
Sripal Bangalore
Karen Calfas **
Bernard R. Chaitman
Mary Ann Champagne
Michael Davidson
Jerome Fleg
Peter A. McCullough
Jonathan Newman
Peter Stone
Optimal Revascularization Therapy Planning Committee
Gregg W. Stone (Chair)
Subcommittee: CABG
Bruce Ferguson (Co-Chair)
Philippe Menasche (Co-Chair)
Sripal Bangalore
Michael Davidson**
Stephen Fremes
Robert Guyton
Michael Mack
Fred Mohr
Anupama Rao
Joe Sabik
Oz Shapira
David Taggart
James Tatoulis
Subcommittee: PCI
David Williams (Co-Chair)
Sripal Bangalore
Jim Blankenship
Sorin Brener
Chris Buller
Antonio Colombo
Bernard de Bruyne
Philippe Généreux
Robert Harrington
Dean Kereiakes
Thierry Lefevre
Jeffrey Moses
Clinical Events
Endpoint Definition Panel
Bernard R. Chaitman (Chair)
Karen P. Alexander
Judith S. Hochman
Ken Mahaffey
David J. Maron
Gregg W. Stone
Harvey White
Clinical Event Review Committee
Bernard R. Chaitman (Chair)
Salvador Cruz-Flores
Nicholas Danchin
Eli Feen
Mario J. Garcia
Paul Hauptman
Abhay A. Laddu
Eugene Passamani
Ileana L. Pina
Maarten Simoons
Hicham Skali
Kristian Thygesen
David Waters
CEC Administrative Group
Karen P. Alexander
Patricia Endsley*
Gerard Esposito
Jeffrey Kanters
John Pownall
Dimitrios Stournaras
ISCHEMIA Imaging Committee
Leslee J. Shaw (Chair)
Daniel Berman
Matthias Friedrich
Rory Hachamovitch
Raymond Kwong
John Mancini
James Min
Dana Oliver
Michael H. Picard
Harmony R. Reynolds
Biostatistics Planning Committee
Frank Harrell (Chair)
Jeffrey Blume
Kerry Lee
Sean M. O'Brien
BioRepository Committee
Jeffrey Berger (Chair)
Claes Held
Iftikhar Kullo
Bruce McManus
Kristin Newby
EQOL Committee
Daniel Mark (Co-Chair)
John Spertus (Co-Chair)
David Cohen
William Weintraub
Recruitment for Women & Minorities
C. Noel Bairey Merz (Chair)
Raffaele Bugiardini
Jelena Celutkiene
Jorge Escobedo
Angela Hoye
Radmila Lyubarova
Deirdre Mattina
Jesus Peteiro
Harmony R. Reynolds
Paola Smanio
Publications
David J. Maron (Chair)
Karen P. Alexander
Sripal Bangalore
Jeffrey Berger
William Boden
Robert Harrington
Judith S. Hochman
Sean M. O'Brien
Harmony R. Reynolds
Yves Rosenberg
Gregg W. Stone
Publication Subcommittees
Economics
Daniel Mark (Chair)
John Spertus
QOL
John Spertus (Chair)
Daniel Mark
Stress Testing
Leslee J. Shaw (Chair)
Dan Berman
Bernard R. Chaitman
Jerome Fleg
Raymond Kwong
Michael H. Picard
Harmony R. Reynolds
Roxy Senior
CCTA
James Min (Chair)
Jonathan Leipsic
John Mancini
Angiography/Optimal Revascularization Therapy
Gregg W. Stone (Chair)
Ziad Ali (Co-chair)
Sripal Bangalore
T. Bruce Ferguson
David Williams
(Philippe Genereux, former Chair, Angiography Subcommittee)*
Optimal Medical Therapy
William Boden (Co-Chair)
David J. Maron (Co-Chair)
Jerome Fleg
Jonathan Newman
Biorepository
Jeffrey Berger (Chair)
Sripal Bangalore
Claes Held
Judith S. Hochman
David J. Maron
Kristin Newby
Jonathan D. Newman
CEC
Bernard R. Chaitman (Chair)
Karen P. Alexander
CKD
Sripal Bangalore (Chair)
Karen P. Alexander
Jerome Fleg
Judith S. Hochman
David J. Maron
Roy Mathew
Sean M. O'Brien
Harmony R. Reynolds
Mandeep Sidhu
CIAO
Harmony R. Reynolds (Chair)
DSMB Members
Lawrence Friedman (Chair)
Jeffrey Anderson
Jessica Berg *
David DeMets
C. Michael Gibson
Gervasio Lamas
Nicole Deming
Jonathan Himmelfarb
Pamela Ouyang
Pamela Woodard
Independent Statistical Analysis Center for DSMB Reporting
Frank Harrell
Samuel Nwosu
NHLBI Program Staff
Project Office
Yves Rosenberg (Project Officer)
Jerome Fleg
Ruth Kirby
Statisticians
Neal Jeffries
ISCHEMIA Clinical Coordinating Center (CCC)
Study Leadership
Judith S. Hochman (Study Chair, Director of CCC)
David J. Maron (Study Co-Chair, Co-Director of CCC, US Country Leader)
CCC Faculty
Sripal Bangalore (Optimal Revascularization Therapy CCC Director, Regional Leader)
Jeffrey Berger (Director of the Biorepository, Regional Leader)
William Boden (US-VA Regional Leader)
Jonathan Newman (Optimal Medical Therapy CCC Director, Regional Leader)
Harmony R. Reynolds (Associate Director of CCC, CCC Imaging Lead, Regional Leader)
Mandeep Sidhu (US-VA Regional Co-Leader)
Program Directors
Jean E. Denaro**
Stephanie Mavromichalis
Project Managers
Kevin Chan
Gia Cobb*
Aira Contreras
Diana Cukali*
Stephanie Ferket*
Andre Gabriel*
Antonietta Hansen*
Arline Roberts
Clinical Research Associates
Michelle Chang
Sharder Islam*
Graceanne Wayser*
Solomon Yakubov*
Michelle Yee
Clinical Trial Assistants
Caroline Callison
Isabelle Hogan
Albertina Qelaj*
Charlotte Pirro*
Kerrie Van Loo
Brianna Wisniewski*
Grants and Finance Administration
Margaret Gilsenan (Grants Manager)
Bevin Lang
Samaa Mohamed
Publications Team
Jihyun Lyo (Publications Manager)
Nadia Gakou
Data Analyst
Vincent Setang*
Mark Xavier*
Statistical and Data Coordinating Center (SDCC)
Sean M. O’Brien (Principal Investigator)
Karen P. Alexander (Co-Principal Investigator)
Akshay Bagai*
Samuel Broderick
Michelle Crowder
Derek Cyr
Patricia Endsley
Jyotsna Garg
Xiangqiong Gu
Robert Harrington*
Lisa Hatch
Anne Heath*
Zhen Huang
Jeffrey Kanters
Kerry Lee*
Jeff Leimberger
Jill Marcus
Courtney Page
Wanda Parker*
Wayne Pennachi
John Pownall
Frank Rockhold
Susanna Stevens
Allegra Stone
Dimitrios Stourna
Omar Thompson
Sheri Ussery
Jennifer White*
Mary (Kaye) Williams
Weibing Xing
Songlin Zhu
Economics and Quality of Life Coordinating Center (EQOL CC)
Duke Clinical Research Institute, Durham, NC
Daniel B. Mark (Principal Investigator)
Kevin Anstrom
Khaula Baloch
Janet Blount
Patricia Cowper
Linda Davidson-Ray
Laura Drew
Tina Harding
J David Knight
Diane Minshall Liu
Betsy O’Neal
Thomas Redick
Saint Luke’s Mid America Heart Institute, Kansas City, MO
John Spertus (Principal Investigator)
Philip Jones
Karen Nugent
Grace Jingyan Wang
ISCHEMIA Imaging Coordinating Center (ICC)
Leslee J. Shaw (Principal Investigator)
Lawrence Phillips
Abhinav Goyal
Holly Hetrick
Dana Oliver
Nuclear Core Lab
Daniel Berman (Director)
Sean W. Hayes (Co-Director)
John D. Friedman
R. James Gerlach
Mark Hyun
Romalisa Miranda-Peats
Piotr Slomka
Louise Thomson
CMR Core Lab
Raymond Y. Kwong (Director)
Matthias Friedrich (Director)*
Francois Pierre Mongeon (Co-Director)
Steven Michael
Echo Core Lab
Michael H. Picard (Director)
Judy Hung
Marielle Scherrer-Crosbie
Xin Zeng
ECG/ETT CoreLab
Bernard R. Chaitman (Director)
Jane Eckstein
Bandula Guruge
Mary Streif
Angiographic Core Lab
Ziad Ali (Director)
Philippe Genereux (Director)*
Maria A. Alfonso
Maria P. Corral
Javier J. Garcia
Jennifer Horst
Ivana Jankovic
Maayan Konigstein
Mitchel B. Lustre*
Yolayfi Peralta
Raquel Sanchez
CCTA Core Lab
James Min (Director)
Reza Arsanjani
Matthew Budoff
Kimberly Elmore
Millie Gomez
Cameron Hague
Niree Hindoyan
Jonathan Leipsic
GB John Mancini
Rine Nakanishi
M. Barbara Srichai-Parsia
Eunice Yeoh
Tricia Youn
Academic Research Organizations (AROs)
Associazione Nazionale Medici Cardiologi Ospedalieri (ANMCO) -Italy & Switzerland
Aldo P. Maggioni (Country Leader)
Francesca Bianchini
Martina Ceseri
Andrea Lorimer
Marco Magnoni
Francesco Orso
Laura Sarti
Martinia Tricoli*
Brazilian Clinical Research Institute (BCRI) - Brazil
Antonio Carvalho (Country Leader)**
Renato Lopes (Country Leader)
Lilian Mazza Barbosa
Tauane Bello Duarte
Tamara Colaiácovo Soares
Julia de Aveiro Morata
Pedro Carvalho
Natalia de Carvalho Maffei
Flávia Egydio*
Anelise Kawakami*
Janaina Oliveira*
Elissa Restelli Piloto*
Jaqueline Pozzibon*
Canadian Heart Research Centre (CHRC) - Canada
Shaun Goodman (Country Leader)
Diane Camara
Neamat Mowafy
Caroline Spindler
China Oxford Centre for International Health Research - China
Lixin Jiang (Country Leader)
Hao Dai
Fang Feng
Jia Li
Li Li*
Jiamin Liu
Qiulan Xie
Haibo Zhang
Jianxin Zhang
Lihua Zhang
Liping Zhang
Ning Zhang
Hui Zhong
Estudios Clínicos Latino America (ECLA) - Argentina
Rafael Diaz*
Claudia Escobar
Maria Eugenia Martin*
Andrea Pascual*
Foundation for Biomedical Research of La Paz University Hospital (FIBHULP) - Spain
José Lopez-Sendon (Country Leader)
Paloma Moraga
Victoria Hernandez
Almudena Castro
Maria Posada*
Sara Fernandez
José Luis Narro Villanueva
Rafael Selgas
French Alliance for Cardiovascular Trials (FACT) - France
Gabriel Steg (Country Leader)
Helene Abergel
Jean Michel Juliard
Green Lane Coordinating Centre Ltd. (GLCC) -Malaysia, New Zealand, Singapore, Taiwan, Thailand
Harvey White (Country Leader)
Caroline Alsweiler
KU Leuven Research & Development - Belgium*
Frans Van de Werf (Country Leader)
Kathleen Claes
Kaatje Goetschalckx
Ann Luyten
Valerie Robesyn
South Australian Health and Medical Research Institute Ltd (SAHMRI) - Australia
Joseph B. Selvanayagam (Country Leader)
Deirdre Murphy
Contract Research Organizations (CROs) for ISCHEMIA Trial
FOCUS Clinical Research Center d.o.o. Belgrade - Serbia
Nevena Garcevic
Jelena Stojkovic
iProcess Global Research Inc. - India
Asker Ahmed
Richa Bhatt
Nitika Chadha*
Vijay Kumar*
Sadath Lubna*
Pushpa Naik
Shruti Pandey*
Karthik Ramasamy*
Mohammed Saleem
Pratiksha Sharma
Hemalata Siddaram*
II. Site Personnel
| Country (No.Randomizations) | Investigator(s) | Study Coordinator(s) | City & State (if applicable) | Institution (No. Randomizations) |
|---|---|---|---|---|
|
*United States (853) Country Leader David J. Maron, MD Regional Leader for VA Sites William E. Boden, MD |
||||
| Kreton Mavromatis, MD | John Doan, MD | Decatur, GA | Atlanta VA Medical | |
| Jason Linefsky, MD | Raven Lee, CCRP Risha Patel So Yang Cho |
Center (139) | ||
| Todd D. Miller, MD | Susan Milbrandt Dawn Shelstad |
Rochester, MN | Mayo Clinic (50) | |
| Preeti Kamath, BDS, | V.A. North Texas | |||
| Subhash Banerjee, MD | MHA, CCRP Ishita Tejani, BDS, MS, MSPH |
Dallas, TX | Health Care System (35) | |
| Harmony R. Reynolds, MD | Stanley E. Cobos, BA | |||
| Jonathan D. Newman, MD, MPH Sripal Bangalore, MD, MHA |
Kirsten J. Quiles, MS Raven R. Dwyer, MPH |
NYU Langone | ||
| Robert M. Donnino, MD Lawrence M. Phillips, MD Muhamed Saric, MD, PhD |
Dalisa Espinosa, MBS | New York, NY | Medical Center-Bellevue Hospital (26) | |
| Khaled Abdul-Nour, MD | Allison Schley, BS Heather Golden |
Detroit, MI | Henry Ford Health System (21) | |
| Peter H. Stone, MD | Hermine Osseni, MS Charlene Wiyarand Peter Douglass, BA Hayley Pomeroy, BA Alexandra Craft, BA Bethany Harvey, BA |
Boston, MA | Brigham & Women’s Hospital, Harvard Medical School (21) | |
| James J. Jang, MD Gennie Yee, MD |
Olivia Anaya Phoebe Goold, RN Steven Giovannone |
San Jose, CA | Kaiser Permanente San Jose (18) Cardiology |
|
| Steven Weitz, MD | Lori Pritchard, RN | Schenectady, | NY | |
| Associates of Schenectady P.C. (17) | ||||
| Suzanne Arnold, MD | Rosann Gans, RN | |||
| James Henry O’Keefe, Jr, MD (PI from 2012–2016) | Paul Kennedy, RN | Kansas City, MO | Saint Luke’s Hospital (17) | |
| Shobana Ganesan, PhD | ||||
| Michael D. Shapiro, DO | David Schlichting, LPN Aynun Naher |
Portland, OR | Oregon Health & Science University (17) | |
| Mohammad El-Hajjar, MD Mandeep S. Sidhu, MD, MBA |
||||
| Steven A. Fein, MD | Wendy L. Stewart, MS | |||
| Mikhail T. Torosoff, MD, PhD | Kristin M. Salmi, BS | Albany, NY | Albany Medical Center Hospital (16) | |
| Radmila Lyubarova, MD | ||||
| Sulagna Mookherjee, MD | ||||
| Krzysztof Drzymalski, MD | ||||
| Edward O. McFalls, MD, PhD | ||||
| Santiago A. Garcia, MD | ||||
| Stefan C. Bertog, MD | Debra K. Johnson, RN | Minneapolis, MN | Minneapolis VAMC (15) | |
| Rizwan A. Siddiqui, MD | Rebekah R. Herrmann, RN | |||
| Areef Ishani, MD | ||||
| Ronnell A. Hansen, MD | ||||
| Michel Georges Khouri, MD | Kristine Arges Melissa LeFevre Jennifer Tomfohr |
Durham, NC | Duke University Medical Center (15) | |
| Kimberly Ann Byrne | Louis Stokes | |||
| Jonathan L. Goldberg, MS, MD | Taissa Zappernick | Cleveland, OH | Cleveland Veterans Affairs Medical Center (14) | |
| Richard Goldweit, MD | Sallie Canada Meghana Kakade Patricia Mieses Stanley E. Cobos, BA Raven R. Dwyer, MPH |
Englewood, NJ | Englewood Hospital and Medical Center (13) | |
| Ronny A. Cohen, MD | Dalisa Espinosa, MBS | |||
| Brooks Mirrer, MD | Kirsten J. Quiles, MS | Brooklyn, NY | NYU-HHC Woodhull Hospital (12) | |
| Victor Navarro, MD | Magdalena Rantinella, BS Jessica Rodriguez, BS |
|||
| Olivia Mancilla, BS | ||||
| David E. Winchester, MD, MS | Susan Stinson, RN | Gainesville, FL | Malcom Randall VAMC (11) | |
| Marvin Kronenberg, MD | Terry Weyand | |||
| Philip Rogal, MD Christopher McFarren, MD |
Sherron C. Crook | Nashville, TN | Vanderbilt University Medical Center (11) | |
| John F. Heitner, MD | Jean Ho Saadat Khan Mahmoud Mohamed Mary R. Soltau, RN Delsa K. Rose, RN |
Brooklyn, NY | New York - Presbyterian/Brookly n Methodist Hospital (10) | |
| Ira M. Dauber, MD | Rebecca J. Wimmer, RN Kathy E. Siegel, RN Susan Derbyshire |
Littleton, CO | South Denver Cardiology Associates, P.C. (10) | |
| Charles Cannan, MD | Michelle Dixon Gerald Leonard Ciarra Heard, LVN |
Portland, OR | Providence Heart and Vascular Institute (10) | |
| Sriram Sudarshan, MD | Viviana Gabriel, LVN Sukie Desire |
Wichita Falls, TX | Wichita Falls Heart Clinic (9) | |
| Puja K. Mehta, MD Michael McDaniel, MD |
Fauzia Rashid, PhD | |||
| Stamatios Lerakis, MD | Senait Asier | |||
| Atlanta, GA | Emory University (9) | |||
| Arshed Quyyumi, MD | Keyur Patel | |||
| Nanette K. Wenger, MD | ||||
| Chester M. Hedgepeth, MD, PhD | Jennifer Gillis, APRN | |||
| Heather Hurlburt, MD | Megan Manocchia, RN | Warwick, RI | Kent Hospital (9) | |
| Alan Rosen, MD | Susan Moore, RN Elizabeth Congdon Gail Brandt |
|||
| Zakir Sahul, MD | Nora Marchelletta Kristina Wippler |
Ypsilanti, MI | Michigan Heart, PC (9) | |
| David Booth, MD | Yvonne Taul, RN | |||
| Steve Leung, MD | Jennifer Isaacs, MS | |||
| Ahmed Abdel-Latif, MD, PhD | Viktoria Bulkley, RN | Lexington, KY | University of Kentucky (8) | |
| Hassan Reda, MD | Caroline Rodgers | |||
| Khaled Ziada, MD | ||||
| Sampoornima | Kimberly E. Halverson, RHIT | La Crosse, WI | Gundersen Lutheran | |
| Setty, MD | Christine Roraff, RN Jonean Thorsen, RN |
Medical Center (8) | ||
| Rajat S. Barua, MD, PhD | Amarachi Ojajuni Oni Olurinde Kamalakar Surineni |
Kansas City, MO | Kansas City VA Medical Center (8) | |
| Fadi Hage, MD Christiano Caldeira, MD James E. Davies, MD Massoud Leesar, MD Jaekyeong Heo, MD Amy Iskandrian, MD Firas Al Solaiman, MD Satinder Singh, MD |
Badhma Valaiyapathi, MD | Birmingham, AL | UAB Vascular Biology and Hypertension Program (8) | |
| Khaled Dajani, MD | Carol M. Kartje, BSN | Maywood, IL | Loyola University Medical Center (8) | |
| Mohammad El-Hajjar, MD Paul Der Mesropian, MD Joseph Sacco, MD |
Michele Rawlins, NP | Samuel Stratton VA | ||
| Brian McCandless, MD Marisa Orgera, MD |
Jennifer Thomson, MA | Albany, NY | Medical Center of Albany NY (7) | |
| Mandeep S. Sidhu, MD, MBA (2012–2016) | ||||
| Mary Colleen Rogge, RN | ||||
| Imran Arif, MD | Julie Bunke, BA | |||
| Hanan Kerr, MD | Kendra Unterbrink, PA Jacqueline Fannon, RN Cynthia Burman, NP |
Cincinnati, OH | Cincinnati VA Medical Center (7) | |
| Jorge F. Trejo (Gutierrez), MD Gerald Fletcher, MD |
||||
| Gary E. Lane, MD Lynn M. Neeson, DNP Pragnesh P. Parikh, MD Peter M. Pollak, MD |
Marcia F. Dubin, CCRP | Jacksonville, FL | Mayo Clinic Florida (7) | |
| Brian P. Shapiro, MD Kevin Landolfo, MD |
||||
| Anthony Gemignani, MD | Sarah Beaudry, RN | White River | VAMC-White River | |
| Daniel O’Rourke, MD | Junction, VT | Junction (7) | ||
| Judith L. Meadows, MD | Stephanie A. Tirado, RN | West Haven, CT | VA Connecticut | |
| Janet Halliday Pamela Julian Stephanie, M. Lane, |
Healthcare System (7) | |||
| Winchester | ||||
| Jason T. Call, MD | RN, BSN, CCRN Jennifer L. Stanford, RN, MSN |
Winchester, VA | Cardiology and Vascular Medicine, PC (7) | |
| Joseph Hannan, MD | Saint Vincent | |||
| Robert Bojar, MD Deepti Kumar, MD John Mukai, MD |
Patricia Arsenault, RN Pamela Sigel, RN |
Worcester, MA | Hospital at Worcester Medical Center (7) | |
| Edward T. Martin, MS, MD | Miriam Brooks | Tulsa, OK | Oklahoma Heart Institute (7) | |
| Gabriel Vorobiof, MD | Ladda Douangvila | Los Angeles, CA | Ronald Reagan | |
| Rubine Gevorgyan Fatima Ranjbaran, RN |
UCLA Medical Center (7) | |||
| Alec Moorman, MD | Bryn Smith, BS Carly Ohmart |
Seattle, WA | University of Washington Medical Center (7) | |
| Scott Kinlay, MBBS, PhD Robert J. Hamburger, MD Thomas P. Rocco, MD |
Samantha Ly, MA | |||
| Deepak L. Bhatt, MD, MPH Kevin Croce, MD, PhD |
Margot C. Quinn, BA Sara Temiyasathit, PhD |
West Roxbury, MA | VA Boston Healthcare System (6) | |
| Jacquelyn A Quin, MD | Jacquelyn Do, MPH | |||
| Jati Anumpa, MD Marco Zenati, MD, MSc David P Faxon, MD |
Desiree Tobin, MPH | |||
| Glenn Rayos, MD | Jennifer Langdon Marcia Werner Bayer |
Daytona Beach, FL | Daytona Heart Group (6) | |
| Ashraf Seedhom, MD Lance Sullenberger, MD |
Amanda O’Malley Erin Orvis |
Albany, NY | Capital Cardiology Associates (6) | |
| Mandy Murphy, RN | Bethesda, MD | |||
| Gregory | Ann Greenberg, RN | NIH Heart Center at | ||
| Kumkumian, MD Steven P. Sedlis, MD |
Margaret Iraola, RN | Suburban Hospital (6) | ||
| Leandro C.Maranan, | VA New York Harbor | |||
| Robert M. Donnino, MD Jeffrey Lorin, MD |
CCRC | New York, NY | Health Care System (6) | |
| Jacqueline E. Tamis-Holland, MD Robert Kornberg, MD |
Ammy Malinay, RN | Ridgewood, NJ | Mount Sinai Saint Luke’s Hospital (6) | |
| Robert Leber, MD Souheil Saba, MD Michael W. Lee, MD |
||||
| Delano R. Small, MD Wassim Nona, MD Patrick B. Alexander, MD |
Candice P. Edillo, RN | Southfield, MI | Providence - Providence Park Hospital (6) | |
| Iram Rehman, MD | ||||
| Ann Ostrander, RN | ||||
| Umesh Badami, MD | Stephanie Wasmiller, RN | Saginaw, MI | Covenant Medical Center, Inc. (5) | |
| Kevin Marzo, MD | Wendy Drewes, RN Dipti Patel, RN |
Mineola, NY | NYU Winthrop (5) | |
| Inga H. Robbins, MD | ||||
| Howard A. Levite, MD | Jackie M White, RN, BSN CCRC | Pomona, NJ | AtlantiCare Regional Medical Center (5) | |
| Sanjay Shetty, MD Mayuri Patel, MD |
Alison Hallam | |||
| Glenn S. Hamroff, MD | Benjamin J Spooner, RPA-C | Cortlandt | NYP Medical Medical Group Hudson Valley | |
| Linda M Hollenweger, LPN,CCRC | Manor, NY | Cardiology (5) | ||
| Raymond W. Little, MD Brandi D. Zimbelman, FNP-C Charles Y. Lui, MD |
Holly Little Tiffany Little |
Houston, TX | Houston Heart & Vascular Associates (5) | |
| Brigham R. Smith, MD Daniel P. Vezina, MD, MSC |
||||
| Lillian L. Khor, MBBCh, MSc Josephine D. Abraham, MD, MPH David A. Bull, MD Stephen H. |
McKellar, MD, MSc | Nona A Eskelson, RN Salt Lake City, |
||
| Salt Lake City VA Medical Center (4) | ||||
| David Booth, MD John Kotter, MD |
Yvonne Taul, RN Caroline Rodgers, RN |
|||
| Ahmed Abdel-Latif, MD, PhD | Jennifer Isaacs, MS | Lexington, KY | Lexington VA Medical Center (4) | |
| Viktoria Bulkley | ||||
| Bob Hu, MD | Renee Kaneshiro | Palo Alto, CA | Palo Alto Medical Foundation Research Institute (4) | |
| Arthur J. Labovitz, MD Michael Berlowitz, MD |
Bonnie J. Kirby, RN, MSN | |||
| Philip Rogal, MD | Nhi N. Tran, MS | University of South Florida (4) |
||
| Christopher McFarren, MD Fadi Matar, MD |
Catherine Jahrsdorfer, RN, BSN | Tampa, FL | ||
| Christiano Caldeira, MD David J. Maron, MD |
||||
| Fatima Rodriguez, MD, MPH | Reem Yunis, PhD | |||
| Ingela Schnittger, MD William F. Fearon, MD |
Jhina Patro | Stanford, CA | Stanford University School of Medicine (4) | |
| Prakash | UCSF - Fresno | |||
| Deedwania, MD Kiran Reddy, MD |
Antonia Vega | Fresno, CA | Community Regional Medical Center (4) | |
| Hugo Bloise-Adames | ||||
| Joseph Sweeny, MD | Santa Jimenez Nicole Saint Vrestil Reyna Bhandari |
New York, NY | Icahn School of Medicine at Mount Sinai (4) | |
| Christopher Spizzieri, MD | Danielle Schade Roxanne Yost |
Camp Hill, PA | Holy Spirit Hospital Cardiovascular Institute (4) | |
| Claudia P Hochberg, MD | Paula Beardsley | Boston, MA | Boston Medical Center (4) | |
| Denise Fine Jana Tancredi, RN, MA/MSN, CCRN | ||||
| William D. Salerno, MD | Patricia Arakelian Susan Mathus |
Saddle Brook, NJ | Hackensack University Medical Center (4) | |
| Deborah O’Neill Joy Burkhardt, CCRP |
||||
| Ray Wyman, MD | Suellen Hosino, RN, BSN, CCRP | Torrance, CA | Torrance Memorial Medical Center (4) | |
| Oksana A. Lubyanaya, BA se D. Salas, BS |
Santa Ana, CA | |||
| Coastal Heart Medical Group (4) | ||||
| Amer Zarka, MD Anil V. Shah, MD |
Maria Aguirre Manu Dhawan |
|||
| Diana Parra Tri Tran |
||||
| Catherine Weick, BSRT(R)(VI) Katie Fowler-Lehman, BSN |
||||
| Thomas Haldis, DO | Natalie Spitzer, BSN Casey Riedberger Catherine Weick |
Fargo, ND | Sanford Health (4) | |
| Stanley E. Cobos, BA Raven R. Dwyer, MPH |
NYU New York | |||
| Jeffrey A. Kohn, MD | Dalisa Espinosa, MBS Kirsten J. Quiles, MS Carrie Drum, RN |
New York, NY | Medical Associates (4) | |
| Saket Girotra, MD | Kimberly Miller-Cox, RN Amy Ollinger, RN Elizabeth Capasso-Gulve |
Iowa City, IA | University of Iowa Hospitals and Clinics (4) | |
| Omar Almousalli, MD | Alaine Melanie Loehr Marlowe Mosley |
Fairview Heights, IL |
Advanced Heart Care Group (4) | |
| Mayil S. Krishnam, MD | Shirin Heydari, MS | |||
| Jeffrey C. Milliken, MD | Andrea M. Lundeen, MA | |||
| Pranav M. Patel, MD | Edgar Karanjah, MD | |||
| Arnold H. Seto, MD Kevin T. Harley, MD |
Wanda C. Marfori, MD Eduardo Hernandez-Rangel, MD |
Orange, CA | University of California Irvine Medical Center (3) | |
| Michael A. Gibson, MD Byron J. Allen, MD |
Pam Singh | |||
| Rita Coram, MD | Anne Marie Webb, BSN | Louisville, KY | University of Louisville (3) | |
| Ellie Fridell, BS Heidi Wilson, BS |
||||
| Sabu Thomas, MD, MSc | Angela Kim, BS | |||
| Ronald G Schwartz, MD, MS Wei Chen, MD, MS |
Patrick Wilmot, BS | Rochester, NY | University of Rochester (3) | |
| Mahfouz El Shahawy, MD | Ramona Stevens | Sarasota, FL | Cardiovascular Center of Sarasota (3) | |
| James Stafford, MD | Loriane Black | Baltimore, MD | University of Maryland Medical Center (3) | |
| Amber B. Hull, RN Olivia J. Lim, RN Helen C. Tucker |
||||
| William B. Abernethy, MD | Natasha C. Putnam, RN Linda L. Hall Tia Cauthren Trish Tucker |
Asheville, NC | Asheville Cardiology Associates (3) | |
| Andrew Zurick, MD | Hollie Horton Jan Orga |
Nashville, TN | Saint Thomas Hospital (3) | |
| Thomas M. Meyer, MD Ronald G. Morford, MD |
Joyce R. White, MSN NP-C Cynthia Baumann, RN |
Lynchburg, VA | Stroobants Cardiovascular Center (3) | |
| Bruce Rutkin, MD | Vidya Seeratan | Manhasset, NY | Northwell Health - Manhasset (3) | |
| Sabahat Bokhari, MD | Magnolia Jimenez | New York, NY | Columbia University Medical Center (3) | |
| Seth I. Sokol, MD Jay Meisner, MD |
Cidney Schultz, RN Jeanne Russo, RN |
Bronx, NY | Jacobi Medical Center (3) | |
| Ihab Hamzeh, MD Arunima Misra, MD |
Zohra Huda, RN, BSN, CCRP | |||
| Matthew Wall Jr., MD Veronica Lenges De Rosen, MD Mahboob Alam, MD |
Araceli Boan | Houston, TX | Baylor College of Medicine (3) | |
| Michael C. Turner, MD Thomas J. Mulhearn, MD |
Christine R Hinton | Lake Charles, | Cardiovascular Specialists of Southwest Louisiana (3) | |
| Beth A. Archer, BSN, RN Julia S. Dionne, BA |
LA | |||
| Arnold P. Good, MD | Cheryl A. Allardyce, BSN, RN Lindsey N. Sikora, BSN, RN Jennifer H. Czerniak, RN |
Columbus, OH | Ohio Health Grant Medical Center (3) | |
| Jennifer A. Mull, MSN, RN Elizabeth Ferguson Frances Laube |
||||
| Gail A Shammas, BSN, RN | Midwest | |||
| Nicolas W. Shammas, MD, MS | Lori Christensen Holly Park | Davenport, IA | Cardiovascular Research Foundation (3) | |
| Robert Chilton, MD | Joan Hecht | San Antonio, TX | Audie Murphy V.A. (2) | |
| Patricia K. Nguyen, MD | Davis Vo, BS James Hirsch |
Palo Alto, CA | VA Palo Alto Healthcare System (2) | |
| Matthew Jezior, MD | Jody Bindeman Sara Salkind Dalisa Espinosa, MBS Lori-Ann Desimone, BSN |
Palo Alto, CA Bethesda, MD | VA Palo Alto Healthcare System (2) Walter Reed National Military Medical Center (2) |
|
| Paul C. Gordon, MD Thomas Crain, MD |
Lina Felix-Stern Jassira Gomes Catherine Gordon, BSN |
Providence, RI | Miriam Hospital (2) | |
| Robert Stenberg, MD | Aimee Mann | Johnstown, PA | Conemaugh Valley Memorial Hospital (2) | |
| Ronald P. Pedalino, MD | Theresa McCreary Stanley E. Cobos, BA Raven R. Dwyer, MPH Dalisa Espinosa, MBS Kirsten J. Quiles, MS Stanley E. Cobos, BA |
Brooklyn, NY | NYU-HHC Kings County Hospital Center (2) New York University - Langone |
|
| Joseph Wiesel, MD | Raven R. Dwyer, MPH Dalisa Espinosa, MBS Kirsten J. Quiles, MS Candace Gopaul, BS |
Flushing, NY | Cardiovascular Associates (2) | |
| George J. Juang, MD | Karen Hultberg Tauqir Huk Afshan Hussain Yesenia Zambrano, BS |
Brooklyn, NY | Coney Island Hospital (2) | |
| Mohammed Al-Amoodi, MD | Sarah Medina Rodriguez Trudie Milner Abbey Mulder, RN |
Yuma, AZ | Yuma Regional Medical Center (2) | |
| David Wohns, MD | Stacie Van Oosterhout, MEd |
Grand Rapids, MI | Spectrum Health (2) | |
| Ellis W. Lader, MD | Martha Meyer, RN, MSN Nancy L. Clapp, RN, BA, CCRC |
Kingston, NY | Mid Valley Cardiology (1) | |
| Michael Mumma, MD | Heather Barrentine Jenne M. Jose, PA | Sarasota, FL | Sarasota Memorial Hospital (1) | |
| Lekshmi Dharmarajan, MD | Stanley E. Cobos, BA Raven R. Dwyer, MPH Dalisa Espinosa, MBS Kirsten J. Quiles, MS |
Jenne Manchery | Bronx, NY | |
| NYU-HHC Lincoln Medical and Mental Health Center (1) | ||||
| Joseph F.X. McGarvey Jr, MD Thomas R. Downes, MD (till Dec. 2016) |
Vera McKinney, RN Linda Schwarz, RN Scott M. Kaczkowski |
Doylestown, PA | Doylestown Health Cardiology (1) | |
| Gary J. Luckasen, MD (from Dec. 2016) | Adam J. Jaskowiak Joel Klitch | Loveland, CO | Medical Center of the Rockies (1) | |
| Joel Klitch | ||||
| Benjamin Cheong, MD Srinivasa Potluri, MD |
Debra Dees Precilia Vasquez |
Houston, TX Plano, TX |
Baylor St. Luke’s Medical Center (1) Baylor Research Institute at Legacy Heart Center (1) ** |
|
| Ronald A. Mastouri, MD | ||||
| Jeffery A. Breall, MD, PhD George E. Revtyak, MD Jonathan W. Bazeley, MD |
Elise L. Hannemann, RN,CCRC Judy Mae Foltz, RN,CCRC |
Indianapolis, IN | Indiana University/Krannert Institute of Cardiology (1) | |
| Emily DeRosa | ||||
| Dayuan Li, MD | Beth Jorgenson Joyce Riestenberg-Smith |
St. Paul, MN | HealthEast Saint Joseph’s Hospital (1) | |
| Kenneth Giedd, MD | New York, NY | Beth Israel Medical Center (1) | ||
| Wayne Old, MD Francis Burt, MD |
Rebecca Bariciano | Chesapeake, VA Bethlehem, PA |
Cardiovascular Associates, Ltd. (1) Saint Luke’s Hospital and Health Network (1) |
|
| Kozhaya Sokhon, MD | Jessica Waldron | Sugar land, TX | Medicus Alliance | |
| Michelle Mayon | Clinical Research Org., Inc. (1) | |||
| Deepika Gopal, MD | Plano, TX | The Heart Hospital Baylor (1) | ||
| Uma S. Valeti, MD | Gretchen Ann Peichel, RN Brandy Starks |
Minneapolis, MN | University of Minnesota (1) | |
| Jon Kobashigawa, MD | Rajesh Gopalan Nair, MD, DNB, DM | Lucilla Garcia Maria Thottam | ||
| India (941) Country Leader |
||||
| Balram Bhargava, DM | Anjali Anand, MSc | |||
| Sajeev Chakanalil Govindan, MD, DNB, DM, PhD |
Janitha Raj, B.Tech Reshma Ravindran, MSc |
|||
| Beverly Hills, Cedars Sinai Medical CA Center (1) | ||||
| Calicut Government Medical College (208) | ||||
| Rajalekshmi VS, MSc, MScCRRA | ||||
| Cholenahally Nanjappa Manjunath, MD, DM Nagaraja Moorthy, MD, DM |
Nandita Nataraj, BE(Biotech) PGDICRCDM Soundarya Nayak, BE(Biotech) PGDICRCDM |
|||
| Satvic Cholenahally Manjunath, MD,DM | Mahevamma Mylarappa, GNM (General Nursing) | Bangalore | Sri Jayadeva Institute of Cardiovascular Sciences and Research (149) | |
| Suryaprakash Narayanappa, MBBS Neeraj Pandit, MD, DM |
Sheromani Bajaj | |||
| Ranjit Kumar Nath, MD, DM | Vandana Yadav, Msc,PGDACR Girish Mishra, Msc, PGDACR |
New Delhi | Dr Ram Manohar Lohia Hospital (101) | |
| S.K. Dwivedi, DM V.S. Narain, DM |
Roma Tewari, PG Meenakshi Mishra, PG |
King George’s | ||
| Sharad Chandra, DM | Shivali Patel Suman Singh, PG |
Lucknow | Medical University, Department of Cardiology (100) | |
| Gurpreet S. Wander, DM Rohit Tandon MD |
||||
| Sarju Ralhan, M.Ch (CTVS) | Baljeet Kaur, MSc (Biotechnology) | Ludhiana | Hero DMC Heart Institute, Dayanand Medical College and | |
| Naved Aslam, DM | Sonika Gupta, MBA, B. Pharmacy | Hospital (83) | ||
| Abhishek Goyal, DM Balram Bhargava, DM G.Karthikeyan, DM |
||||
| S.Ramakrishnan, DM | ||||
| Sandeep Seth, DM | ||||
| Rakesh Yadav, DM Sandeep Singh, DM |
||||
| Ambuj Roy, DM Neeraj Parakh, DM |
Chandini Suvarna, BDS | New Delhi | All India Institute Of Medical Sciences (67) | |
| Sunil Kumar Verma, DM Rajiv Narang, DM Sundeep Mishra, DM Nitish Naik, DM Gautam Sharma, DM |
||||
| Shiv Kumar Choudhary, M.Ch Chetan Patel, DNB Gurpreet Gulati, MD |
||||
| Sanjeev Sharma, MD V K Bahl, DM |
||||
| Anoop Mathew, MD | Binoy | MOSC Medical | ||
| Eapen Punnoose, MD | Mannekkattukudy Kurian | Kolenchery | College Hospital (39) | |
| Milind Avdhoot Gadkari, MD | Sheetal Rupesh Karwa, BHMS | |||
| Siddharth Gadage, MD DNB Tapan Umesh Pillay, BHMS MSc |
Suvarna Kolhe, MSc | Pune | KEM Hospital Pune (35) | |
| Santhosh Satheesh, MBBS, MD, DM | R. J. Vindhya, B.Sc. (Bio-Technology), MSc(Bio-Informatics) |
Pondicherry | Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER) (31) |
|
| Peeyush Jain, MD Ashok Seth, MD |
||||
| Zile Singh Meharwal, MD | ||||
| Atul Mathur, MD Upendra Kaul, MD |
Atul Verma, MD Mona Bhatia, MD Ankush Sachdeva, MD Thounaojam Indira Devi, RN Nungshi Jungla, RN |
New Delhi | Fortis Escort Heart Institute (31) | |
| Johann Christopher, MD, DNB | K. Manjula Rani, MSc. | |||
| Rajeev Menon, MD, DNB | M. Sowjanya Reddy, BSc | Hyderabad | Gurunanak CARE Hospital (27) | |
| Nirmal Kumar, MD, DNB | K. Preethi, BSc | |||
| Abraham Oomman, MD,DM,DNB | Rinu R sidh, MSc(Clinical Research) | |||
| Robert Mao, MD, DM | Ramakrishnan T., B.Tech(Biotechnology) | Chennai | Apollo Research and Innovation (23) | |
| Hilda Solomon, PhD | Rajesh Francis, MSc(Clinical Research) | |||
| Sudhir Naik, MD, DM | ||||
| Sajeeda Parveen Khan, MBBS, (Dip.Card) | Vamshi Priya P., MSc | Hyderabad | Apollo Research & Innovations (13) | |
| Johann Christopher, MD Nirmal Kumar, MD |
Kotiboinna Preethi | Hyderabad | CARE Nampally (11) | |
| Purvez Grant, MD | Shweta Hande, BHMS, PGDCR Poonam Sonawane, B.ScMicrobiology, ACCR |
Pune | Ruby Hall Clinic,Grant Medical Foundation (10) | |
| Ranjan Kachru, MD | Abhishek Dubey Kavita Rawat |
New Delhi | Fortis Healthcare Fl.t Lt. Rajan Dhall Hospital (4) | |
| Ajit Kumar VK, MD, DM | ||||
| Sanjay Ganapathi, MD, DM | ||||
| Jayakumar K, MS, M.Ch | Vineeth CP | Sree Chitra Tirunal Institute for Medical Sciences and Technology (3) | ||
| Harikrishnan Sivadasanpillai, MD, DM | Manas Chacko, RN | Trivandrum | ||
| Bijulal Sasidharan, MD, DM Kapilamoorthy TR, MD |
Suresh Babu | |||
| Johann Christopher, MD | Sowjanya Reddy | |||
| Praneeth Polamuri, MD | Manjula Rani | Hyderabad | CARE Hospital (3) | |
| Priyadarshani | Batra Hospital and | |||
| Upendra Kaul, MD | Arambam Bebek Singh | New Delhi | Medical Research Centre (BHMRC) (3) | |
| United Kingdom (539) Country Leaders |
||||
| Roxy Senior, MBBS, MD, DM Keith AA Fox, MBChB (past) Country Coordinators |
||||
| Grace M. Young, MSc, BSc (Hons) | ||||
| Kathryn Carruthers (past) | ||||
| Roxy Senior, MBBS, MD, DM Ahmed Elghamaz, MB BCh Sothinathan Gurunathan, MBChB |
Harrow | Northwick Park Hospital Harrow/ Royal Brompton Hospital London (202) | ||
| Nikolaos Karogiannis, MBBS | Grace M. Young, MSc, BSc (Hons) | |||
| Benoy N Shah, MD, MBBS, BSc (Hons) Richard HJ Trimlett, MBBS, CCST |
Christopher Kinsey Raisa Kavalakkat, MSc, BSc, RN |
|||
| Michael B Rubens, LRCP, MRCS, MBBS, DMRD | Jo Evans, RN | |||
| Edward D Nicol, MD, BMedSci, MBBS, DTM&H Tarun K Mittal, MD |
Ikraam Hassan, RN | |||
| Reinette Hampson, BSc (Hons), BA (Hons) | ||||
| Sarah Williams, RN | ||||
| Reto Andreas Gamma, MBBS | Kim Holland, RN Karen Swan, RN |
Chelmsford | Broomfield Hospital (39) | |
| Mark A de Belder, MD | Bev Atkinson, RN | Middlesbrough | The James Cook University Hospital, Middlesbrough (37) | |
| Jeet Thambyrajah, MD | ||||
| Thuraia Nageh, BSc(Hons) MBBS MD MRCP John R Davies, MBBS, PhD |
Swapna Kunhunny, MRes Clin Res, BSc (N), RN | Westcliffe on Sea | Southend University Hospital (34) | |
| Steven J. Lindsay, MD | Craig Atkinson, RN | |||
| John Kurian, MD Haqeel Jamil, MD |
Carita Krannila, RN Manitha Vinod, RN |
Bradford | Bradford Royal Infirmary (20) | |
| Osama Raheem, MD | ||||
| Angela Hoye, MD | Lisa Chaytor | |||
| Leanne Cox Julie Morrow Kay Rowe |
Cottingham | The University of Hull/Castle Hill Hospital (19) | ||
| Patrick Donnelly, MD | Stephanie Kelly, RN | |||
| Bernardas Valecka, MD | Susan Regan, RN | Belfast | South Eastern Health and Social Care (17) | |
| Dawn Turnbull Catherine Fleming |
||||
| Anoop Chauhan, MD | Arijit Ghosh Karen Gratrix |
Blackpool | Blackpool Teaching Hospitals (16) | |
| Stephen Preston | ||||
| Craig Barr, MD | Anne Cartwright | Dudley | Russells Hall Hospital (15) | |
| Khaled Alfakih, MBBS, MD Jonathan Byrne, PhD Ian Webb, PhD, MA |
Abigail Knighton, BSc., PG Dip. Katherine Martin, RGN, Dip. N, MSc |
London | King’s College NHS Foundation Hospital (14) | |
| Peter Henriksen, PhD, MB ChB, BSc(Hons) | Laura Flint, RGN James Harrison, BSc(Hons), PG dip |
Edinburgh | Royal Infirmary of Edinburgh (13) | |
| Peter OKane, MD | Nicki Lakeman | Bourneouth | Royal Bournemouth Hospital (13) | |
| Ramesh de Silva, MB ChB, MD | Anja Ljubez | Bedford | Bedford Hospital NHS Trust (11) | |
| Dwayne S. G. Conway, MD | Judith Wright Donna Exley |
Wakefield | Pinderfields Hospital (11) | |
| Alexander A Sirker, MB BChir, PhD | Mervyn Andiapen, RN Amy J. Richards, BSc |
London | University College London Hospitals NHS Foundation Trust BartsHealth NHS Trust (11) |
|
| Stephen P Hoole, MD | Lisa Wong, MSc | Cambridge | Papworth Hospital (10) | |
| Fraser N. Witherow, MD | Melanie J. Munro, RGN | Dorchester | Dorset County Hospital (8) | |
| Nicola Johnston, MB, Bch BAO, MRCP, MD | Michelle McEvoy, RN | |||
| Mark Harbinson, MB, Bch BAO, MRCP, MD Simon Walsh, MB, Bch BAO, MD |
Caroline Brown, RN | Belfast | Belfast Trust (7) | |
| Hanna Douglas, MB, Bch BAO, MRCP, MD | ||||
| Thabitha Charles | Central Manchester | |||
| Matthew Luckie, MD | Laurel Kolakaluri Hannah Phillips Louise Morby, RN |
Manchester | University Hospital (7) | |
| Jolanta Sobolewska, MD | Karen Hallett, RN Carolyn Corbett, RN Lynne Winstanley |
Oldham | The Pennine Acute Hospitals NHS Trust (6) | |
| Paramjit Jeetley, MD | Royal Free London | |||
| Niket Patel, MD Tushar Kotecha, MBChB, Mpharm Christopher Travill, MBBS, MD Iqbal Karimullah, |
MBBS | Angelique Smit, RN London Susan Gent, SRN |
||
| RGN Nafisa Hussain, BSc | Luton | NHS Foundation T rust (6) | ||
| Luton and Dunstable University Hospital NHS FT (5) | ||||
| Mahmud Al-Bustami, MBBS | ||||
| Denise Braganza, MD | Fiona Haines | Peterborough | Peterborough City Hospital (5) | |
| Robert Henderson, MD | Joanne Taaffe Jane Burton |
|||
| Kate Pointon, MBBS | Maria Colton | Nottingham | Nottingham University Hospitals (4) | |
| Surendra Naik, PhD Thomas Mathew, MBBS, MD, DM |
Rachel King | |||
| Ammani Brown, MSc BA RN Andrew Docherty, RN |
||||
| Colin Berry, BSc MB ChB, PhD Damien Collison, MB ChB Giles Roditi, MB ChB |
Lisa McCloy, RN Kate Robb, RN Craig Paterson, PhD |
Clydebank | University of Glasgow (4) | |
| Wenda Crawford, RN Joanne Kelly, RN |
||||
| Lorraine McGregor, RN | ||||
| Andrew J Moriarty, BSc MB PhD | Anne Mackin, RN, BSc | Craigavon | Cardiovascular Research Unit, Craigavon Area Hospital (2) | |
| Jason D. Glover, MBBS Jiwan Pradhan, MBBS |
Janet P Knight, RN | Basingstoke | Hampshire Hospitals NHS Foundation Trust (2) | |
| Ghada Mikhail, MD | Imperial College | |||
| Darrel P. Francis, MD, MA | Tuhina Bose | London | IHealthcare NHS Trust (1) | |
|
*Canada (447) Country Leaders Vladimir Dzavik, MD |
||||
| Shaun G. Goodman, MD, MSc Gilbert Gosselin, MD |
Anna Proietti, RN Myriam Brousseau, RN |
|||
| Gilbert Gosselin, MD | Magalie Corfias, RN Patricia Blaise Luc Harvey |
Montreal, QC | Montreal Heart Institute (90) | |
| Ariel Diaz, MD Philippe Rheault, MD |
Trois-Rivieres, QC | Centre Hospitalier de Regional Trois-Rivieres (71) |
||
| Miguel Barrero, MD Carl-Éric Gagné, MD | Patricia Alarie | |||
| Yanek Pépin-Dubois, MD | Linda Arcand | |||
| Ricardo Costa, MD | Isabelle Roy | |||
| Ying Tung Sia, MD | Estelle Montpetit | |||
| Catherine Lemay, MD | ||||
| Alejandro Gisbert, MD | ||||
| Pierre Gervais, MD | ||||
| Alain Rheault, MD | ||||
| Katia Drouin, RN | ||||
| Denis Carl Phaneuf, MD | Christine Bergeron, RN | Terrebonne, QC | CISSSL - Hopital Pierre-Le Gardeur (42) | |
| Gilbert Gosselin, MD | Christine Shelley | |||
| Christine Masson Sandy Carr, RN | ||||
| Pallav Garg, MBBS, MSc | Catherine Bone, RN | London, ON | London Health Sciences Centre (35) | |
| Benjamin J.W. Chow, MD | Ermina Moga | |||
| Renee C. Hessian, MD | Janetta Kourzenkova | Ottawa, ON | University of Ottawa Heart Institute (29) | |
| Rob S. Beanlands, MD | Olga Walter | |||
| Richard F. Davies, MD | ||||
| Kevin R. Bainey, MD, MSc | Norma Hogg, RN Suzanne Welsh, RN | Edmonton, AB | University of Alberta (28) | |
| Asim N. Cheema, MD, PhD | ||||
| Akshay Bagai, MD, MHS | ||||
| Ron Wald, MDCM, MPH | ||||
| Shaun G. Goodman, MD, MSc | Khrystyna Kushniriuk, HBSc, MD | Toronto, ON | St. Michael’s Hospital (27) | |
| John Joseph Graham, MRCP, MB ChB, BSc | Mohammed Hussain | |||
| Mark Peterson, MD, FRCSC, PhD | Olugbenga Bello | |||
| Chi-Ming Chow, MD, CM, MSc | ||||
| Beth Abramson, MD, MSc | ||||
| Asim Nazir Cheema, MD | Ishba Syed, MBBS | Mississauga, ON | Dixie Medical Group (24) | |
| Mohammad Tariq Vakani, MD | Mohammed Hussain, BSc(H) | |||
| Khrystyna Kushniriuk, MBBS | ||||
| Judy Otis, CRC | ||||
| James Cha, MD | Rebecca Otis, CRC Michelle M Seib, RN | Oshawa, ON | Dr. James Cha (21) | |
| Andrew G Howarth, MD, PhD | Sandra M Rivest, RN | Calgary, AB | University of Calgary (15) | |
| Rosa Sandonato, BSCN | ||||
| Graham Wong, MD | Jackie Chow Andrew Starovoytov Naomi Uchida Ngaire Meadows |
Vancouver, BC | Vancouver General Hospital (15) | |
| Amar Uxa, MD | Nadia Asif Suzana Tavares |
Toronto, ON | University Health Network (14) | |
| Paul Galiwango, MD | Bev Bozek, RN, CCRC | |||
| Saleem Kassam, MD | Maria Shier | Scarborough, ON | Scarborough Cardiology Research (9) | |
| Ashok Mukherjee, MD | Lori-Ann Larmand | |||
| A. Joseph Ricci, MD | Amir Janmohamed | |||
| Andy Lam, MD | Brenda Hart Jane Marucci Sharon Tai Sonya Brons, RN Chris Beck, RN |
East Grimsby, ON | West Lincoln Memorial Hospital (8) | |
| Shamir Mehta, MD | Glenda Wong, RN Krystal Etherington |
Hamilton, ON | Hamilton General Hospital (7) | |
| Thippeekaa Arumairajah Maria Aprile |
||||
| Jacob Udell, MD | Sara Karlsson Susan Webber |
Toronto, ON | Women’s College Hospital (7) | |
| Philippe Généreux, MD | Chantale Mercure | Montréal, QC | Centre Intégré Universitaire de Santé et de Services Sociaux du Montréal (2) | |
| Adnan Hameed, MD | Nancy Aedy | St. Catharines, ON | Saint Catharines General Hospital (2) | |
| Fran Farquharson | Northwest GTA | |||
| Ledjalem Daba, MD | Anam Siddiqui | Vaughan, ON | Cardiovascular and Heart Rhythm Program (1) | |
| Brazil (399) | ||||
| Country Leaders | ||||
| Antonio Carlos Carvalho, MD, PhD | ||||
| Renato D. Lopes, MD, PhD | ||||
| Whady A. Hueb, MD | ||||
| Paulo Cury Rezende, MD | Myrthes Emy Takiuti, RN | Sao Paulo | Heart Institute (InCor) University of São Paulo (127) | |
| Expedito Eustáquio Ribeiro Silva, MD | ||||
| Alexandre Ciappina Hueb, MD Paola Emanuela Poggio Smanio, MD, PhD |
Leonardo Pizzol Caetano, PhD | São Paulo | Instituto Dante Pazzanese de Cardiologia (98) | |
| Alexandre Schaan de Quadros, MD | ||||
| Renato Abdala Karam Kalil, MD | Aline Peixoto Deiro | |||
| José Luiz da Costa Vieira, MD | Alice Manica Muller | |||
| Gabriel Grossmann, MD | Maria Antonieta Pereira de Moraes Bruna Maria Ascoli | Porto Alegre | Instituto de Cardiologia de Porto Alegre (41) | |
| Pedro Píccaro de Oliveira, MD | ||||
| Leonardo Bridi, MD | Sílvia Zottis Poletti | |||
| Simone Savaris, MD | ||||
| João V Vitola, MD, PhD | ||||
| Rodrigo J Cerci, MD, Msc | Sandra S. Zier, BSc | Curitiba | Quanta Diagnostico & Terapia (33) | |
| Fabio R Farias, MD, Msc | Vilmar Veiga Jr, BSc | |||
| Miguel M Fernandes, MD, PhD | ||||
| José Antonio Marin-Neto, MD, PhD | ||||
| André Schmidt, MD, PhD | Hospital das Clinicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (31) | |||
| Moysés de Oliveira Lima Filho, MD, PhD | Diego Franca da Cunha | Ribeirao Preto | ||
| Ricardo Mendes Oliveira, MD | ||||
| João Reynaldo Abbud Chierice, MD | ||||
| Carísi A. Polanczyk, MD | Guilherme G Rucatti, PsyD | Hospital de Clínicas de Porto Alegre (12) | ||
| Mariana V. Furtado, MD | Fernanda Igansi, BSc | Porto Alegre | ||
| Luis F. Smidt, MD | Mauren P Haeffner, BSc | |||
| Antonio Carlos Carvalho, MD | Viviane Almeida | Sao Paulo | Unifesp - Hospital Sao Paulo (9) | |
| Gustavo Pucci, MD | Gabriela Sanchez de Souza | |||
| Flavio Lyra, MD Alvaro Rabelo Alves Junior, MD |
Mayana Almeida Viviane dos Santos |
Salvador | Fundacao Bahiana de Cardilogia (9) | |
| Marianna D. A. Dracoulakis, MD, PhD | ||||
| Rodolfo G. S. D Lima, MD | Natalia S Oliveira, RN | Salvador | Hospital da Bahia (8) | |
| Estevao Figueiredo, MD | Bruna Edilena Paulino Azevedo Marco Bizzaro Santos |
Belo Horizonte | Hospital Lifecenter (8) | |
| Paulo Ricardo Caramori, MD | Amanda Germann Vitor Gomes Rosa Homem Ellen Magedanz |
Porto Alegre | Hospital Sao Lucas da Pontificia Universidade Catolica do Rio Grande do Sol (7) | |
| Rogerio Tumelero, MD | Rosane Laimer Alexandre Tognon |
Fundo | Hospital Sao Vicente de Paulo (5) | |
| Frederico Dall’Orto, MD | Pocos de Caldas | Hospital Maternidade e Pronto Socorro Santa Lucia (4) | ||
| Claudio T. Mesquita, MD | ||||
| Alexandre S. Colafranseschi, MD | ||||
| Amarino C. Oliveira Jr., MD | Roberta P Santos, RN | Botafogo | Hospital Pró-Cardiaco (3) | |
| Luiz A. Carvalho, MD | ||||
| Isabella C. Palazzo, MD | ||||
| Andre S. Sousa, MD | ||||
| Expedito Eustáquio Ribeiro da Silva, MD, PhD | ||||
| Pedro Gabriel Melo de Barros e Silva, MD, PhD | Mariana Yumi Okada, RN | |||
| Luciana de Pádua Silva Baptista, MD, PhD | Ana Paula Batista, RN | Sao Paulo | Hospital TotalCor (2) | |
| Marcelo Jamus Rodrigues, MD | Aline Nogueira Rabaça, BS | |||
| Marcos Valério Coimbra de Resende, MD, PhD | ||||
| Jose Francisco Saraiva, MD | Larissa Miranda Trama | Sao Paulo | Hospital Celso Pierro (1) | |
| Talita Silva Camila Thais de Souza Ormundo Carla Vicente |
||||
| Costantino Costantini, MD, PhD | Caroline Pinheiro Daniele Komar |
Curitiba | Hospital Cardiologico Costantini (1) | |
| Poland (333) | ||||
| Country Leaders | ||||
| Witold Ruzyllo, MD, PhD | ||||
| Hanna Szwed, MD, PhD | ||||
| Country Coordinator | ||||
| Radoslaw Pracon, MD, PhD | ||||
| Marcin Demkow, MD, PhD | ||||
| Radoslaw Pracon, MD, PhD | ||||
| Cezary Kepka, MD PhD | Coronary and Structural Heart Diseases Department, Institute of Cardiology (127) | |||
| Anna Teresinska, MD PhD | Olga Walesiak | Warsaw | ||
| Karolina Kryczka, MD PhD | Katarzyna Malinowska | |||
| Jan Henzel, MD PhD | ||||
| Mateusz Solecki, MD PhD | ||||
| Edyta Kaczmarska, MD PhD | ||||
| Jakub Maksym, MD | ||||
| Karolina Wojtera, MD | ||||
| Tomasz Mazurek, MD, PhD | Anna Fojt, MD | Warszawa | Medical University of Warsaw (48) | |
| Ewa Szczerba, MD | ||||
| Szymon Jonik, MD | ||||
| Jaroslaw Drozdz, PhD | ||||
| Bartosz Czarniak, MD | ||||
| Malgorzata Frach (formerly Stasiak), MD | Lodz | Cardiology Clinic, Medical University in Lodz (43) | ||
| Konrad Szymczyk, MD | ||||
| Iwona Niedzwiecka, MD | ||||
| Sebastian Sobczak, MD | ||||
| Tomasz Ciurus, MD | ||||
| Piotr Jakubowski, MD | ||||
| Magdalena Misztal-Teodorczyk, MD | ||||
| Dawid Teodorczyk, MD | Marta Swiderek, MA | |||
| Aleksandra Fratczak, MD | Ewelina Wojtala, MA | |||
| Marcin Szkopiak, MD | ||||
| Patrycja Lebioda, MD | ||||
| Michal Wlodarczyk, MD | ||||
| Anna Plachcinska, MD | ||||
| Jacek Kusmierek, MD | ||||
| Magdalena Miller, MD | ||||
| Halina Marciniak, MD | ||||
| Karolina Wojtczak-Soska, MD | ||||
| Katarzyna Łuczak, MD | ||||
| Tomasz Tarchalski, MD | ||||
| Anna Cichocka-Radwan, MD | ||||
| Hanna Szwed, MD, PhD | Jaroslaw Karwowski, MD | Warsaw | National Institute of Cardiology, Warsaw (35) | |
| Grazyna Anna Szulczyk, MD | ||||
| Adam Witkowski, MD, PhD | ||||
| Krzysztof Kukuła, MD, PhD | Warsaw | Department of Interventional Cardiology & Angiology, Institute of Cardiology (20) | ||
| Małgorzta Celińska-Spodar, MD | ||||
| Joanna Zalewska, MD | ||||
| Grzegorz Gajos, MD, PhD | Krakow | Department of Coronary Disease, John Paul II Hospital, Jagiellonian University Medical College (16) | ||
| Krzysztof Bury, MD, PhD | ||||
| Piotr Pruszczyk, MD, PhD | Andrzej Łabyk, MD | Warszawa | Department of Internal Medicine and Cardiology, Infant Jesus Teaching Hospital, Medical University of Warsaw (15) | |
| Marek Roik, MD, PhD | Agnieszka Szramowska, MD | |||
| Olga Zdończyk, MD | ||||
| Krystyna Łoboz-Grudzień, MD, PhD | ||||
| Leszek Sokalski, MD, PhD | Joanna Jaroch, MD, PhD | Wrocław | T.Marciniak Hospital (11) | |
| Barbara Brzezińska, MD, PhD | ||||
| Maciej Lesiak, Professor, MD | Szpital Kliniczny | |||
| Magdalena Łanocha, MD | Poznan | Przemienienia Pańskiego (10) | ||
| Krzysztof W. Reczuch, MD | Adam Kolodziej, MD | Wroclaw | Military Hospital / Medical University (4) | |
| Zbigniew Kalarus, MD | Medical University of Silesia, School of Medicine with the Division of Dentistry, Department of Cardiology, Congenital Heart Diseases and Electrotherapy, Silesian Center for Heart Diseases (3) | |||
| Andrzej Swiatkowski, MD | ||||
| Mariola Szulik, MD | ||||
| Zabrze | ||||
| Wlodzimierz J. Musial, MD | Marta Marcinkiewicz-Siemion, MD | Bialystok | University Hospital in Bialystok (1) | |
| Russia (303) | ||||
| Country Coordinator | ||||
| Olga Bockeria, MD, PhD | ||||
| Leo Bockeria, MD, PhD | Olga Bockeria, MD, PhD | National Medical Research Center for Cardiovascuar Surgery (113) | ||
| Karen Petrosyan, MD, PhD | Zalina Kudzoeva, MD | Moscow | ||
| Tatiana Trifonova, MD | Nodira Aripova, MD | |||
| Alexander M. Chernyavskiy, MD, PhD | Ivan A. Naryshkin, MD | E.Meshalkin National Medical Research Center of the Ministry of Health of the Russian Federation (101) | ||
| Evgeniy I. Kretov, MD | Alena Kuleshova, MD | Novosibirsk | ||
| Igor O. Grazhdankin, MD | Dastan Malaev, MD | |||
| Leonid L. Bershtein, MD, PhD | ||||
| Sergey A. Sayganov, MD, PhD | Irina Subbotina | Saint Petersburg | North-Western State Medical University (50) | |
| Anastasia M. Kuzmina-Krutetskaya, MD | Victoria Gumerova | |||
| Elizaveta V. Zbyshevskaya, MD, PhD | ||||
| Nana O. Katamadze, MD, PhD | ||||
| Elena A. Demchenko, MD, PhD | ||||
| Pavel S. Kozlov, MD | Olga B. Nikolaeva, MD | Saint Petersburg | Federal Almazov North-West Medical Research Centre (39) | |
| Vikentiy Y. Kozulin, MD | ||||
| Ekaterina I. Lubinskaya, MD | ||||
| *Spain (286) | ||||
| Country Leader | ||||
| Jose Luis Lopez-Sendon, MD, PhD | ||||
| Country Coordinator | ||||
| Almudena Castro, MD | ||||
| Jose Lopez-Sendon, MD, PhD | ||||
| Almudena Castro, MD | ||||
| Elena Refoyo Salicio, MD | Virginia Fernández-Figares, Pharm | Madrid | Hospital La Paz. IdiPaz (118) | |
| Gabriela Guzman, MD | ||||
| Gabriel Galeote, MD | ||||
| Silvia Valbuena, MD | ||||
| Jesús Peteiro, MD, PhD | Complejo Hospitalario Universitario A Coruña (CHUAC) Sergas, Department of Cardiology. INIBIC | |||
| María Dolores Martínez-Ruíz, MD | ||||
| Ruth Pérez-Fernández, MD | Moisés Blanco-Calvo, PhD | |||
| José J Cuenca-Castillo, MD | Encarnación Alonso-Álvarez, BSc | A Coruna | A Coruña. CIBER-CV. Universidad de A Coruña, Spain (112) | |
| Xacobe Flores-Ríos, MD | Paula García-González, BSc | |||
| Óscar Prada-Delgado, MD | ||||
| Gonzalo BargeCaballero, MD | ||||
| Jose Ramon Gonzalez Juanatey, MD, PhD | ||||
| Miguel Souto Bayarri, MD, PhD | Hospital Clinico Universitario de Santiago (17) | |||
| Virginia Pubull Nuñez, MD | Jose Seijas Amigo, Pharm | Santiago de Compostela | ||
| Raymundo Ocaranza Sanchez, MD, PhD | ||||
| Belen Cid Alvarez, MD | ||||
| Carlos Peña Gil, MD, PhD | ||||
| Amparo Martinez Monzonis, MD | ||||
| Alessandro Sionis, MD | ||||
| Montserrat Vila Perales, MD | ||||
| Josep Maria Padró, MD | ||||
| Antonio Serra Peñaranda, MD | ||||
| Joan García Picart, MD | Ana Fernández Martínez, RN | Barcelona | Hospital de la Santa Creu i Sant Pau (11) | |
| Antonino Ginel Iglesias, MD | ||||
| Xavier Garcia-Moll Marimon, MD | ||||
| Guillem Pons Lladó, MD | ||||
| Francesc Carreras Costa, MD | ||||
| Vicente Miro, MD | ||||
| Jose L Diez, MD | Begoña Igual, MD | Valencia | Hospital Universitario y Politecnico La Fe (10) | |
| Pilar Calvillo, MD | ||||
| F. Marin Ortuño, MD, PhD | ||||
| M. Valdés Chávarri, MD, PhD | M. Quintana Giner, MD | HUVA, Hospital Clínico Universitario Virgen De La Arrixaca (8) | ||
| A. Tello Montolliu, MD, PhD | A.I. Romero Aniorte, MD | Murcia | ||
| E. Pinar Bermudez, MD, PhD | JM. Rivera Caravaca, MD | |||
| G. De La Morena, MD, PhD | ||||
| Olga Cañavate | ||||
| Montserrat Gracida Blancas, MD | Sonia Guerrero Silvia Riera Jose Enrique Castillo |
Barcelona | Hospital De Bellvitge (4) | |
| Jose Enrique Castillo Luena, MD | Luena Maria Lasala |
Zaragoza | Hospital Universitario Miguel Servet (4) | |
| Francisco Fernandez-Aviles, MD | Maria Lorenzo Olga Sobrino Alexandra Vazquez |
Madrid | Hospital General Universitario Gregorio Maranon (2) | |
| China (246) | ||||
| Country Leader | ||||
| Lixin Jiang, MD, PhD | ||||
| Haojian Dong | ||||
| Jiyan Chen, MD | Peiyu He Chunli Xia |
Guangzhou | Guangdong General Hospital (102) | |
| Junqing Yang Qi Zhong |
||||
| Yongjian Wu, MD, PhD | Yanmeng Tian, MD Dongze Li |
Beijing | Chinese Academy of Medical Sciences, Fuwai Hospital (17) | |
| Yitong Ma, MD | Xiaomei Li | Urumqi | First Affiliated Hospital of Xinjiang Medical University (15) | |
| Yining Yang, MD | Xiang Ma Zixiang Yu Qian Zhao Chunguang Li |
|||
| Zheng Ji, MD | Lei Zhang Yu Zhao Bolin Zhu |
Tangshan | Tangshan Gongren Hospital (15) | |
| Mulei Chen | Beijing | Beijing Chao-yang Hospital, Capital Medical University (12) | ||
| Xinchun Yang, MD | Hongjie Chi Yang Wang Jing Zhang |
|||
| Wenhua Lin, MD | Rui Jing Jingjing Liu Qiang Zhou, MD Chang Xu, MD |
Tianjing | TEDA International Cardiovascular Hospital (12) | |
| Hesong Zeng, MD | Zhuxi Li, MD Junhua Li, MD Luyang Xiong, MD Dan Gao |
Wuhan | Tongji Medical College (11) | |
| Xin Fu, MD | Dengke Jiang Ran Leng Xutong Wang Qianqian Yuan Lili Zhang Ziliang Bai Jianhua Li Jie Qi |
Zhengzhou | The First Affiliated Hospital of Zhengzhou University (11) | |
| Bin Yang, MD | Fei Wang Haitao Wang Bin Yang Zhou Yue Zhulin Zhang Yumei Dong |
Taiyuan | Shanxi Cardiovascular Hospital (10) | |
| Songtao Wang, MD | Jiajia Mao Bin Zhang |
Qingdao | Qingdao Fuwai Hospital (8) | |
| Gong Cheng, MD | Xiuhong Li Xiaowei Yao Nier Zhong Ning Zhou |
Xian | Shanxi Provincial People’s Hospital (6) | |
| Yulan Zhao, MD | Yaping Huang, MS Panpan Zhou, MS |
Zhengzhou | The Second Affiliated Hospital of Zhengzhou University (6) | |
| Xuehua Fang, MD | Wei Su | Beijing | Liangxiang Hospital, Beijing Fangshan District (6) | |
| Qiutang Zeng, MD | Yu Kunwu Yudong Peng Xin Su |
Wuhan | Wuhan Union Hospital, Tongji Medical College, Huazhong Science and Tech University (3) | |
| Xi Su, MD | Chen Wang Yunhai Zhao |
Wuhan | Wuhan Asia Heart Hospital (3) | |
| Qingxian Li, MD | Yaming Geng Yanfu Wang Jing-yao Fan, MD Si-ting Feng, MD,PhD |
Jining | Affiliated Hospital of Jining Medical University (3) | |
| Shao-ping Nie, MD, PhD | Xiao Wang, MD,PhD Yan Yan, MD,PhD Hui-min Zhang, MD,PhD |
Beijing | Beijing Anzhen Hospital (2) | |
| Qin Yu, MD | Lingping Chi Fang Liu |
Dalian | Affiliated Zhongshan Hospital of Dalian University (2) | |
| Jian’an Wang, MD | Han Chen Jun Jiang Huajun Li Jian’an Wang Yechen Han, MM Lihong Xu, RN |
Hangzhou | The Second Affiliated Hospital Zhejiang University School of Medicine (1) | |
| Shuyang Zhang, MD, PhD | Zhenyu Liu | Beijing | Peking Union Medical College Hospital (1) | |
| Zhenyu Liu, MD | Gang Chen Rongrong Hu |
|||
| *Italy (139) | ||||
| Country Leader | ||||
| Aldo P. Maggioni, MD | ||||
| Gian Piero Perna, MD Marco Marini, MD |
Francesca Pietrucci, PhD | Ancona | Cardiology and CCU - Ospedali Riuniti Ancona (54) | |
| Gabriele Gabrielli, MD Stefano Provasoli, MD Edoardo Verna, MD |
Anna Di Donato | Varese | Ospedale di Circolo e Fondazione Macchi (23) | |
| Lorenzo Monti, MD Barbara Nardi, MD |
Rozzano | Humanitas Research Hospital, Rozzano (MI) (17) | ||
| Antonio Di Chiara, MD | Francesca Pezzetta, MD | Tolmezzo | Azienda Servizi Sanitaria n.3 Alto Friuli-Collinare-Medio Friuli (9) | |
| Andrea Mortara, MD Marcello Galvani, MD |
Valentina Casali, MD | Monza | Policlinico di Monza, Monza MB (8) Ospedale “G.B. Morgagni – L. Pierantoni” Forli (AUSL della Romagna) (8) | |
| Filippo Ottani, MD | Chiara Attanasio | Forli | ||
| Gianpiero Leone, MD | ||||
| Marco Sicuro, MD | Francesco Pisano, MD Cristina Bare, BSc |
Aosta | Ospedale Regionale Umberto Parini (5) | |
| Paolo Calabro, MD | AORN Dei Colli “V. Monaldi” UOC Cardiologia Università della Campania “L.Vanvitelli” (4) | |||
| Tiziana Formisano, MD | Fabio Fimiani | Napoli | ||
| Giuseppe Tarantini, MD | Alberto Barioli, MD | |||
| Umberto Cucchini, MD Anto Luigi Andres, MD |
Federica Ramani | Padua | University of Padua-Cardiology Clinic (3) | |
| Emanuela Racca, MD | Fabrizio Rolfo, MD Cecilia Goletto |
Cuneo | Azienda Ospedaliera S. Croce e Carle (3) | |
| Carlo Briguori, MD | Francesca De Micco | Naples | Clinica Mediterranea (2) | |
| Roberto Amati, MD | Stefano Di Marco, MD | UO Cardiologia Ospedale SS Cosma e Damiano (2) | ||
| William Vergoni, MD | Martina Tricoli | Pescia | ||
| Aldo Russo, MD Raffaele Fanelli, MD |
Massimo Villella, MD | San Giovanni Rotondo | IRCCS “Casa Sollievo della Sofferenza” (1) | |
| *Singapore (61) | ||||
| Country Leader | ||||
| Harvey D. White, DSc | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Kian-Keong Poh, MD Ping Chai, MD |
||||
| Joshua P. Loh, MD Edgar L. Tay, MD |
||||
| Kristine Teoh, MD Lynette L. Teo, MD |
Sik-Yin V Tan, BSc Winnie C Sia, BSc |
Singapore | National University Heart Center Singapore (33) | |
| Ching-Ching Ong, MD Raymond C. Wong, MD Poay-Huan Loh, MD Theodoras Kofidis, MD David Foo, MBBS |
Audrey W Leong, BSc | |||
| Jason Loh Kwok Kong, MD Ching Min Er, MD |
Li Hai Yan, RN | Singapore | Tan Tock Seng Hospital (22) | |
| Fahim Haider Jafary, MD | ||||
| Terrance Chua, MD | Nasrul Ismail Min Tun Kyaw Deborah Yip |
Singapore | National Heart Centre Singapore (6) | |
| Germany (54) | ||||
| Country Leader | ||||
| Rolf Doerr, MD | ||||
| Rolf Doerr, MD | ||||
| Juergen Stumpf, MD | Dorit Grahl | |||
| Klaus Matschke, MD, PhD | Franziska Guenther | Dresden | Praxisklinik Herz und Gefaesse (29) | |
| Gregor Simonis, MD, PhD Clemens T. Kadalie, MD |
Kerstin Bonin | |||
| Udo Sechtem, MD Peter Ong, MD |
Ina Wenzelburger Susanne Gruensfelder, RN |
Stuttgart | Robert-Bosch-Krankenhaus (22) | |
| P. Christian Schulze, MD, PhD | Jena | University Hospital Jena (2) | ||
| Bjoern Goebel, MD | ||||
| Karsten Lenk, MD | ||||
| Georg Nickenig, MD | Jan-Malte Sinning, MD Marcel Weber, MD Nikos Werner, MD |
Bonn | Universitatsklinikum Bonn (1) | |
| Austria (50) | ||||
| Country Leaders | ||||
| Irene Marthe Lang, MD Kurt Huber, MD |
||||
| Herwig Schuchlenz, MD Stefan Weikl, MD |
Gudrun Steinmaurer | Graz | LKH Graz West Austria (35) | |
| Irene Marthe Lang, MD | Max-Paul Winter, MD | Vienna | Medical University of Vienna, Department of Cardiology (8) | |
| Kurt Huber, MD | Tijana, Andric, MD Maximilian, Tscharre, MD |
|||
| Gabriele, Jakl-Kotauschek, MD | Claudia, Wegmayr, MSc Bernhard, Jäger, MD Florian, Egger, MD |
Vienna | Wilhelminen Hospital Vienna (7) | |
| Hungary (49) | ||||
| Country Leader | ||||
| Matyas Keltai, MD, PhD, DSc | ||||
| Judit Sebo, MD | ||||
| Andras Vertes, MD | Zoltan Davidovits, MD | Budapest | Eszszk- Szent Istvan Hospital (20) | |
| Albert Varga, MD, PhD | Laszlone Matics Gergely Ágoston, MD | Szeged | University of Szeged (12) | |
| Geza Fontos, MD | Gabor Dekany, MD | Budapest | George Gottsegen National Institute of Cardiology (9) | |
| Bela Merkely, MD, PhD, DSc | Andrea Bartykowszki, MD Pal Maurovich-Horvat, MD, PhD, MPH |
Budapest | Heart and Vascular Center, Semmelweis University (8) | |
| Serbia (47) | Gabor Kerecsen, MD | Agnes Jakal | Budapest | Military Hospital, Budapest (1) |
| Sasa Hinic, MD, | BSc | |||
| Jelena Djokic, MD | Belgrade | |||
| Marija Zdravkovic, MD, PhD Vladan Mudrenovic, MD Bogdan Crnokrak, MD |
University Hospital Center Bezanijska Kosa (13) | |||
| Branko D. Beleslin, MD, PhD Nikola N. Boskovic, MD Marija T. Petrovic, MD |
Ana D. Djordjevic-Dikic, MD, PhD Vojislav L. Giga, MD, PhD |
Belgrade | Faculty of Medicine, University of Belgrade; Cardiology Clinic, Clinical Center of Serbia (10) | |
| Milan R. Dobric, MD | Jelena J. Stepanovic, MD, PhD | |||
| Zeljko Z. Markovic, MD, PhD Ana S. Mladenovic, MD, PhD |
||||
| Lazar Velicki, MD | Institute of Cardiovascular Diseases Vojvodina, Sremska Kamenica, Serbia and Faculty of Medicine, University of Novi Sad (9) | |||
| Nada Cemerlic-Adjic, MD | Ljiljana Pupic | Sremska Kamenica | ||
| Goran Davidović, MD, PhD Rada Vučić, MD |
Stefan M. Simović, MD | Kragujevac | Clinical Center Kragujevac (7) | |
| Milica Nikola Dekleva, MD PhD | Miroslav Stevo Martinovic, MD Gordana Stevanovic |
Belgrade | University Clinical Hospital Zvezdara (6) | |
| Goran Stankovic, MD | Milan Dobric | Belgrade | Clinical Center of Serbia (1) | |
| Svetlana Apostolovic, MD | Sonja Salinger Martinovic Dragana Stanojevic |
Nis | Clinic for Cardiovascular Diseases, Clinical Center Nis (1) | |
| Mexico (46) | Jorge Escobedo, MD Rubén Baleón-Espinosa, MD Arturo S Campos-Santaolalla, MD Elihú Durán-Cortés, MD |
|||
| José M Flores-Palacios, MD Andrés García-Rincón, MD Moisés Jiménez-Santos, MD |
Joaquín | V Peñafiel, MD | ||
| Ramon de Jesús- Pérez, RN | Benito Juarez Instituto Mexicano del | Seguro Social (35) | ||
| José A Ortega-Ramírez, MD Aquiles Valdespino-Estrada, MD |
||||
| Erick Alexánderson Rosas, MD | María Fernanda Canales Brassetti, MD Diego Adrián Vences Anaya, MD María Pérez García Isabel Estela Carvajal Juarez, MD Magdalena Madero Rovalo, MC Erick Donato Morales Rodríguez, MD |
Mexico City | Instituto Nacional de Cardiología “Ignacio Chávez” (11) | |
| Australia (45) | ||||
| Country Leaders | ||||
| Joseph B. Selvanayagam, MBBS (Hons), DPhil | ||||
| Jamie Rankin, MBBS (past) | ||||
| Country Coordinator | ||||
| Deirdre Murphy | ||||
| Joseph B. Selvanayagam, MBBS (Hons), DPhil Majo X. Joseph, MBBS |
Sau Lee, PhD Prince Thomas, RN Melissa D Chaplin, RN |
Adelaide | Flinders Medical Centre (30) | |
| Suku T. Thambar, MBBS | Stephanie C Boer, B Biotechnology (Honours) | New Lambton Heights | John Hunter Hospital (8) | |
| John F. Beltrame, MD | Jeanette K. Stansborough, RN Marilyn Black, RN Michelle M. Bonner, B. Nursing |
Woodville | The Queen Elizabeth Hospital (5) | |
| Graham S. Hillis, PhD | Kim F. Ireland, RN Clare Venn-Edmonds, RN |
South Perth | Royal Perth Hospital (2) | |
| France (42) | ||||
| Country Leader | ||||
| Philippe-Gabriel Steg, MD | ||||
| Country Coordinators | ||||
| Helene Abergel | ||||
| Jean-Michel Juliard | ||||
| Christophe Thuaire, MD Téodora Dutoiu, MD |
Corine Thobois, RN Emilie Tachot, RN Christophe Laure, RN Christel Vassaliere, RN |
Chartres | C.H. Louis Pasteur (21) | |
| Philippe Gabriel Steg, MD Jean-Michel Juliard, MD |
Helene Abergel, MSc Axelle Fuentes, MSc |
Paris | Bichat Hospital (9) | |
| Michel S. Slama, MD | Ludivine Eliahou, MD Olivier Dubourg, MD |
Clamart Cedex | Antoine-Beclere Hospital (5) | |
| Rami El Mahmoud, MD | Pierre Michaud, MD | Boulogne | Ambroise Pare Hospital (2) | |
| Eric Nicollet, MD | Sarah Hadjih | Corbeil-Essonnes Cedex | Centre Hospitalier Sud Francilien (2) | |
| Pascal Goube, MD | Patricia Brito | |||
| Gilles Barone-Rochette, MD | Gilles Barone-Rochette | Grenoble | Grenoble University Hospital (2) | |
| Alain Furber, MD Loïc Bière, MD |
Charles Cornet, MD, PhD Jeremy Rautureau, MD, PhD |
Angers Cedex 9 | Centre Hospitalier Universitaire d’Angers (1) | |
| Lithuania (39) | Agne Juceviciene, MD | |||
| Irma Kalibataite-Rutkauskiene, MD Laura Keinaite |
||||
| Aleksandras Laucevicius, MD Jelena Celutkiene, MD |
Monika Laukyte Gelmina Mikolaitiene Akvile Smigelskaite, MD Ilona Tamasauskiene, MD Agne Urboniene, MD |
Vilnius | Vilnius University Hospital Santariskes Clinic (39) | |
| *Netherlands (37) | ||||
| Elvin Kedhi MD, PhD | ||||
| Jorik Timmer, MD Rik Hermanides, MD |
Ilse Bouwhuis | Eliza Kaplan, MD Robert K. Riezebos, |
||
| Lia Nijmeijer | Zwolle Isala Klinieken (25) | |||
| MD, PhD Pouneh Samadi, MD |
Jeannette, J. M. Schoep, RN | Cardio Research Amsterdam | Hartcentrum OLVG (11) | |
| Elise van Dongen, MD Sander R. Niehe, MD Harry Suryapranata, MD |
Elisabeth, M. Janzen, RN | |||
| Stijn van Vugt, MD, PhD | Sandra Ahoud | Nijmegen | Radboudumc (1) | |
| Portugal (33) | ||||
| Ruben Ramos, MD | ||||
| Duarte Cacela, MD | ||||
| Ana Santana, MD | ||||
| Antonio Fiarresga, MD | ||||
| Lidia Sousa, MD | ||||
| Hugo Marques, MD | ||||
| Lino Patricio, MD | Mafalda Selas | |||
| Luis Bernanrdes, MD | Filipa Silva | Lisbon | Hospital de Santa Marta (25) | |
| Pedro Rio, MD | Cláudia Freixo | |||
| Ramiro Carvalho, MD | ||||
| Rui Ferreira, MD | ||||
| Tiago Silva, MD | ||||
| Ines Rodrigues, MD | ||||
| Pedro Modas, MD | ||||
| Guilherme Portugal, MD | ||||
| Jose Fragata, MD | ||||
| Fausto J. Pinto, PhD | Inês Zimbarra Cabrita, PhD | |||
| Miguel Nobre Menezes, MD | Andreia Rocha, MSc | |||
| Guilhermina Cantinho Lopes, MD | Francisca Patuleia Figueiras, PhD | Santa Maria University Hospital, Cardiology Department, CHLN (6) | ||
| Ana Gomes Almeida, PhD | Andreia Coelho, BSc | Lisbon | ||
| Pedro Canas Silva, MD | Marta Capinha | |||
| Angelo Nobre, MD | Maria Inês Caetano | |||
| Ana Rita Francisco, MD | Susana Silva | |||
| Nuno Ferreira, MD | ||||
| Ricardo L. Lopes, MD | Vila Nova de Gaia | Centro Hospitalar de Vila Nova de Gaia/Espinho, EPE (2) | ||
| Argentina (29) | ||||
| Country Leader | ||||
| Rafael Diaz, MD (past) | ||||
| Luis Guzman, MD | Veronica Tinnirello | Cordoba | Instituto Medico DAMIC (11) | |
| Julio César Figal, MD | ||||
| Oscar Méndiz, MD Claudia Cortés, MD |
Matías Nicolás Mungo | Ciudad Autonoma de Buenos Aires | Fundación Favaloro (10) | |
| Roberto René Favaloro, MD | ||||
| Carlos Alvarez, MD | Marina Garcia | Bahia Blanca | Hospital Italiano Regional del Sur Bahia Blanca (3) | |
| Javier Courtis, MD Gabriela Zeballos, MD |
Valeria Godoy | Cordoba | Clinica Romagosa and Clinica De La Familia (2) | |
| Lilia Schiavi, MD | Maria Victoria Actis | Cordoba | Clinica Del Prado (2) | |
| Mariano Rubio, MD | Graciela Scaro, MD | Cordoba | Clínica Privada Vélez Sarsfield (1) | |
| *New Zealand (28) | ||||
| Country Leader | ||||
| Harvey D. White, DSc | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Gerard Patrick Devlin, MD | Liz Low, RN | |||
| Raewyn Fisher, MD | Jayne Scales, RN | Hamilton | Waikato Hospital (22) | |
| Kirsty Abercrombie, RN | ||||
| Ralph Alan Huston Stewart, MB,ChB, MD | Leah Howell, RN | Auckland City Hospital (6) | ||
| Harvey D. White, DSc Jocelyne Benatar, MD |
Cathrine Patten, RN | Auckland | ||
| *Macedonia (28) | ||||
| Sasko Kedev, MD, PhD Irena Peovska Mitevska, MD, PhD |
Skopje | University Clinic of Cardiology (28) | ||
| Elizabeta Srbinovska Kostovska, MD, PhD | ||||
| Hristo Pejkov, MD, PhD | ||||
| *Sweden (23) | ||||
| Country Leader | ||||
| Claes Held, MD, PhD | ||||
| Claes Held, MD, PhD Kai Eggers, MD, PHhD Gunnar Frostfelt, MD, PhD Nina Johnston, MD, PhD Maciej Olsowka, MD Axel Åkerblom, MD, PhD Inga Soveri, MD, PhD |
Christina Björklund, RN Maria Andreasson, RN Marie Essermark, RN |
Uppsala | Uppsala University (18) | |
| Johannes Aspberg, MD | Liselotte Persson | Stockholm | Karolinska Institutet at Danderyd Hospital (5) | |
| Israel (15) | ||||
| Country Leaders | ||||
| Rafael Beyar, MD, MD, DSc, MPH | ||||
| Tali Sharir, MD | ||||
| Country Coordinator | ||||
| Eugenia Nikolsky, MD | ||||
| Tali Sharir, MD Dan Elian, MD |
Or Harel, MA | Tel-Aviv | Assuta Medical Centers (9) | |
| Arthur Kerner, MD Samia Massalha, MD |
Margalit Bentzvi Ludmila Helmer |
Haifa | Rambam Medical Center (6) | |
| Japan (14) | ||||
| Country Leader | ||||
| Shun Kohsaka, MD | ||||
| Keiichi Fukuda, MD, PhD | Ikuko Ueda, PhD | Shinjuku-ku | Keio University (7) | |
| Shun Kohsaka, MD | Jun Fujita, MD | |||
| Satoshi Yasuda, MD, PhD Kanae Hirase, RN |
Akemi Furukawa, RN Toshiyuki Nagai, MD, PhD Fumiyuki Otsuka, MD, PhD |
Suita-shi | National Cerebral and Cardiovascular Center (4) | |
| Shigeyuki Nishimura, MD | Shintaro Nakano | Hidaka | Saitama Medical University (3) | |
| *Belgium (7) | ||||
| Country Leader | ||||
| Frans Van de Werf, MD, PhD | ||||
| Country Coordinator | ||||
| Kaatje Goetschalckx, MD | ||||
| Kaatje Goetschalckx, MD Frans Van de Werf, PhD, MD Kathleen Claes, PhD, MD |
Valerie Robesyn | Leuven | University Hospital Leuven (7) | |
| *Taiwan (7) | ||||
| Country Leader | ||||
| Harvey D. White, DSc | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Chung-Lieh Hung, MD | ||||
| Chun-Ho Yun, MD | ||||
| Charles Jia-Yin Hou, MD | ||||
| Jen-Yuan Kuo, MD | ||||
| Hung-I Yeh, MD, PhD | ||||
| Ta-Chuan Hung, MD | ||||
| Jiun-Yi Li, MD, PhD | Yi-Hsuan Yang | Taipei City | Mackay Memorial Hospital (7) | |
| Chen-Yen Chien, MD, PhD | ||||
| Cheng-Ting Tsai, MD | ||||
| Chun-Chieh Liu, MD | ||||
| Fa-Chang Yu, MD | ||||
| Yueh-Hung Lin, MD | ||||
| Wei-Ren Lan, MD | ||||
| Chih-Hsuan Yen, MD | ||||
| Jui-Peng Tsai, MD | ||||
| Kuo-Tzu Sung, MD | ||||
| *South Africa (7) | ||||
| Mpiko Ntsekhe, MD | ||||
| Shaheen Pandie, MD | Constance Philander (Nee Talliard), ND Noloyiso Mtana, RN | Cape Town | Groote Schuur Hospital / University of Cape Town (7) | |
| Charle A Viljoen, MD | ||||
| Marianne De Andrade, MD | ||||
| *Switzerland (7) | ||||
| Country Leader | ||||
| Aldo P. Maggioni, MD | ||||
| Tiziano Moccetti, MD | Adriana Anesini, RN | Cardiocentro (7) | ||
| M.Grazia Rossi, MD | Simona Maspoli, RN | Lugano | ||
| Manuela Mombelli, RN | ||||
| Egypt (6) | ||||
| Magdy Abdelhamid, MD | ||||
| Ahmed Adel, MD | ||||
| Ahmed Kamal, MsC | ||||
| Hossam Mahrous, MD | Ahmed Talaat, MD | Cairo | Cairo University (6) | |
| Sameh El Kaffas, MD | ||||
| Hussien El Fishawy, MD | ||||
| Romania (5) | ||||
| Calin Pop, MD, PhD | Emergency County Hospital Baia Mare (4) | |||
| Matei Claudia, MD, PhD | Bucharest | |||
| Bogdan A. Popescu, MD, PhD | ||||
| Carmen Ginghina, MD, PhD | Monica Rosca, MD, PhD | Bucharest | Emergency Institute of Cardiovascular Diseases “Prof. Dr. C. C. Iliescu” (1) | |
| Dan Deleanu, MD, PhD | Carmen C. Beladan, MD, PhD | |||
| Vlad A. Iliescu, MD, PhD | ||||
| *Saudi Arabia (5) | ||||
| Mouaz H. Al-Mallah, MD MSc | Sarah Zahrani, RN | Central Province | King AbdulAziz Cardiac Center (5) | |
| Ahmed Aljzeeri, MD | ||||
| Hani Najm, MD | ||||
| Ali Alghamdi, MD | ||||
| *Peru (4) | ||||
| Walter Enrique Mogrovejo Ramos, MD | Marco Antonio Monsalve Davila, RN | Mirafloes | Instituto Neuro Cardiovascular De Las Americas (4) | |
| Thailand (3) | ||||
| Country Leader | ||||
| Harvey D. White, DSc | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Srun Kuanprasert, MD | ||||
| Arintaya Prommintikul, MD | ||||
| Weerachai Nawarawong, MD | Supatchara Khwakhong, RN | |||
| Surin Woragidpoonpol, MD | Anong Chaiyasri, RN | |||
| Thitipong Tepsuwan, MD | Warangkana Mekara, RN | Chiang Mai | Maharaj Nakorn Chiang Mai Hospital (2) | |
| Noppon Taksaudom, MD | Supap Kulthawong, RN | |||
| Chataroon Rimsukcharoenchai, MD | Anong Amaritakomol, RN | |||
| Juntima Euathrongchit, MD | ||||
| Yutthaphan Wannasopha, MD | ||||
| Sukit Yamwong, MD | ||||
| Piyamitr Sritara, MD | ||||
| Suthara Aramcharoen, MD | Pachara Panpunuan, RN | Bangkok | Ramathibodi Hospital (1) | |
| Krissada Meemuk, MD | ||||
| *Malaysia (2) | ||||
| Country Leader | ||||
| Harvey D. White, DSc | ||||
| Country Coordinator | ||||
| Caroline Alsweiler | ||||
| Ahmad Khairuddin, MD | Noor Syamira Mokhtar, RN | Kuala Lumpur | Institut Jantung Negara (2) | |
| Hafidz Abd Hadi, MD | Nor Asiah Basri, RN | |||
| Shaiful Azmi Yahaya, MD | Irni Yusnida, RN | |||
| Humayrah Hashim | ||||
Countries participated in Economics Quality of Life (EQoL) Questionnaires
This site received one participant in transfer that was randomized at another site
Footnotes
past members / past organizations
deceased
ClinicalTrials.gov Identifier: NCT01471522;
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Task Force M, Montalescot G, Sechtem U et al. 2013 ESC guidelines on the management of stable coronary artery disease: the Task Force on the management of stable coronary artery disease of the European Society of Cardiology. Eur Heart J 2013;34:2949–3003. [DOI] [PubMed] [Google Scholar]
- 2.Fihn SD, Gardin JM, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation 2012;126:e354–471. [DOI] [PubMed] [Google Scholar]
- 3.Maron DJ, Hochman JS, Reynolds HR et al. Initial Invasive or Conservative Strategy for Stable Coronary Disease. The New England journal of medicine 2020;382:1395–1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mahajan N, Polavaram L, Vankayala H et al. Diagnostic accuracy of myocardial perfusion imaging and stress echocardiography for the diagnosis of left main and triple vessel coronary artery disease: a comparative meta-analysis. Heart 2010;96:956–66. [DOI] [PubMed] [Google Scholar]
- 5.Group ITR, Maron DJ, Hochman JS et al. International Study of Comparative Health Effectiveness with Medical and Invasive Approaches (ISCHEMIA) trial: Rationale and design. Am Heart J 2018;201:124–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boden WE, O’Rourke RA, Teo KK et al. Optimal medical therapy with or without PCI for stable coronary disease. The New England journal of medicine 2007;356:1503–16. [DOI] [PubMed] [Google Scholar]
- 7.Group BDS, Frye RL, August P et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. The New England journal of medicine 2009;360:2503–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yusuf S, Zucker D, Peduzzi P, Fisher LD, Takaro T, Kennedy JW, Davis K, Killip T, Passamani E, Norris R, et al. Effect of coronary artery bypass graft surgery on survival: overview of 10-year results from randomised trials by the Coronary Artery Bypass Graft Surgery Trialists Collaboration. Lancet. 1994. Aug 27;344(8922):563–70. [DOI] [PubMed] [Google Scholar]
- 9.Maron DJ, Stone GW, Berman DS et al.Is cardiac catheterization necessary before initial management of patients with stable ischemic heart disease? Results from a web-based survey of cardiologists. Am Heart J 2011;162:1034–1043. [DOI] [PubMed] [Google Scholar]
- 10.Xie JX, Eshtehardi P, Varghese T et al. Prognostic Significance of Nonobstructive Left Main Coronary Artery Disease in Women Versus Men: Long-Term Outcomes From the CONFIRM (Coronary CT Angiography Evaluation For Clinical Outcomes: An International Multicenter) Registry. Circulation Cardiovascular imaging 2017;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Oviedo C, Maehara A, Mintz GS et al. Intravascular ultrasound classification of plaque distribution in left main coronary artery bifurcations: where is the plaque really located? Circulation Cardiovascular interventions 2010;3:105–12. [DOI] [PubMed] [Google Scholar]
- 12.Mancini GBJ, Leipsic J, Budoff MJ et al. Coronary CT Angiography Followed by Invasive Angiography in Patients With Moderate or Severe Ischemia-Insights From the ISCHEMIA Trial. JACC: Cardiovascular Imaging 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berman DS, Kang X, Slomka PJ et al. Underestimation of extent of ischemia by gated SPECT myocardial perfusion imaging in patients with left main coronary artery disease. J Nucl Cardiol 2007;14:521–8. [DOI] [PubMed] [Google Scholar]
- 14.Sareen N, Ananthasubramaniam K. Left main coronary artery disease: A review of the spectrum of noninvasive diagnostic modalities. J Nucl Cardiol 2016;23:1411–1429. [DOI] [PubMed] [Google Scholar]
- 15.Attenhofer CH, Pellikka PA, Oh JK, Roger VL, Sohn DW, Seward JB. Comparison of ischemic response during exercise and dobutamine echocardiography in patients with left main coronary artery disease. Journal of the American College of Cardiology 1996;27:1171–7. [DOI] [PubMed] [Google Scholar]
- 16.Hochman JS Reynolds HR,Bangalore S et al. Baseline Characteristics and Risk Profiles of Participants in the ISCHEMIA Randomized Clinical Trial. JAMA Cardiol 2019;4(3):273–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rink LD, Feigenbaum H, Godley RW et al. Echocardiographic detection of left main coronary artery obstruction. Circulation 1982;65:719–24. [DOI] [PubMed] [Google Scholar]