Objectives
The coronavirus disease 2019 (COVID-19) pandemic has led to reported change in electroconvulsive therapy (ECT) services worldwide. However, minimal data have been published demonstrating tangible changes across multiple ECT centers. This article aimed to examine changes in ECT patients and ECT service delivery during the pandemic.
Methods
We retrospectively assessed data collected on ECT patients within the Clinical Alliance and Research in Electroconvulsive Therapy and Related Treatments (CARE) Network during a 3-month period starting at the first COVID-19 restrictions in 2020 and compared data with predicted values based on the corresponding 3-month period in 2019. Mixed-effects repeated-measures analyses examined differences in the predicted and actual number of acute ECT courses started and the total number of acute ECT treatments given in 2020. Sociodemographic, clinical, treatment factors, and ECT service delivery factors were compared for 2020 and 2019.
Results
Four Australian and 1 Singaporean site participated in the study. There were no significant differences between the predicted and actual number of acute ECT courses and total number of acute ECT treatments administered in 2020. During 2020, there were statistically significant increases in the proportion of patients requiring ECT under substitute consent and receiving ECT for urgent reasons compared with 2019.
Conclusions
This multisite empirical study is among the first that supports anecdotal reports of changes in the triaging and delivery of ECT during COVID-19. Results suggest that ECT was prioritized for the most severely ill patients. Further data assessing the impacts of COVID-19 on ECT are needed.
Key Words: COVID-19, coronavirus, electroconvulsive therapy, practice, mental health service
The coronavirus disease 2019 (COVID-19) pandemic has led to significant changes in the delivery and distribution of health services, including mental health services. In response, psychiatric professional bodies published guidelines on the provision and rationalization of ECT during the pandemic1–5 so that patients whose conditions required ECT as a lifesaving or essential treatment to prevent relapse were prioritized. Globally, ECT clinicians have described changes and rationalizations in the triage and delivery of ECT in response to competition for resources required to provide ECT safely and in adherence to infection control protocols.6–14 Such changes in practice are likely to have impacts on the outcomes of ECT patients. For example, the Royal College of Psychiatrists has stated that the reduced accessibility of ECT services due to the COVID-19 pandemic led to patients becoming more unwell, hospitalized, or having longer hospitalization.15 Although there have been anecdotal reports on the effect of the COVID-19 pandemic on ECT practice and service delivery at individual units, to date, there has been minimal empirical data published demonstrating the impact of these changes across different services.
The main objective of our study was to examine whether there were any changes in sociodemographic, clinical, treatment factors, and ECT service delivery during the first 2020 lockdown period across participating sites in the Clinical Alliance and Research in Electroconvulsive Therapy and Related Treatments (CARE) Network. We hypothesized that compared with equivalent pre-COVID periods in the previous years, there would be a reduction in overall number of ECT treatments provided and a decrease in the number of patients undergoing acute ECT. We further expected an increase in the proportion of ECT provided for more severely ill patients (eg, those with substitute consent for ECT and/or those with more urgent indications).
MATERIALS AND METHODS
Study Population
The CARE Network
The CARE Network, which has been described elsewhere,16 is a growing clinical and research consortium composed of multiple psychiatric services that provide ECT and related treatments in sites in Australia and internationally. The network was initially set up in 2015 to collect standardized deidentified sociodemographic, clinical, ECT treatment, and outcome data for the purposes of benchmarking and quality improvement, including developing translational research. Electroconvulsive therapy centers within the CARE Network deliver ECT to inpatients or outpatients in public or private hospitals. Ethics approval for this study was obtained from the Health Research Ethics Committee from the Sydney Local Health District (Protocol No X19-0311 and 2019/ETH12595) and Singapore National Healthcare Group Domain Specific Review Board (DSRB No: 2015/01283), with waiver of consent.
Period for Comparison
For this study, CARE data were extracted and compared between 2 periods. The study period was selected as the 3-month period beginning on the date the strictest government restrictions for control of the COVID-19 pandemic first imposed on free movement for each jurisdiction. For Australian sites, this period was March 23, 2020, to June 23, 2020, and for Singapore the period was April 7, 2020, to July 7, 2020. A 3-month period was chosen primarily to capture the acute and some of the delayed effects of restrictions during the first wave of COVID-19 infections and to obtain comparable samples of data from different participating sites. In Australia and Singapore, the strictest social restrictions imposed during the first wave of the pandemic were gradually eased after 1 to 2 months. The control period was the equivalent 3-month period for each respective jurisdiction in the previous year to compare year-to-year variability. For Australia, the control period was March 23, 2019, to June 23, 2019, and for Singapore, the comparator period was April 7, 2019, to July 7, 2019. The number of ECT treatments provided and ECT courses started in the equivalent 3-month calendar periods in 2017, 2018, and 2019 were also examined.
Outcomes
The primary outcomes collected for this study were the overall number of treatments of acute ECT and the number of acute ECT treatment courses started within the CARE Network in the ascribed periods. Because patients may require more than 1 course of acute ECT during the study period, we considered that using the total number of acute ECT treatment courses would reflect the true demand on ECT services.
Other outcomes examined included sociodemographic data and clinical factors including consent for ECT, involuntary admission status, the main indication for ECT, the main reason for ECT, and past response to ECT. The main reason for ECT was classified into 2 groups, urgent and nonurgent reasons for ECT. We considered urgent reasons for acute ECT were suicide risk, aggression/agitation, and inadequate oral intake. Failure of medication, previous good response to ECT, patient preference, poor tolerability, and risks with medications were grouped as reasons for nonurgent ECT. Finally, treatment variables including the type of ECT, frequency of ECT, and the number of treatments in acute ECT course were examined.
Statistical Analysis
Data analysis was performed using SPSS Statistics 26.17 The total number of acute ECT treatment courses started during the 3-month study period was extracted for each site for each equivalent study period from 2017 to 2020. The total number of acute ECT treatments at each site was extracted, regardless of whether patients had commenced acute ECT before or during the 3-month study periods. Using the same 3-month period from 2017 to 2019, linear slope functions were individually fitted for each site and used to predict both outcomes for the 2020 study period. A mixed-effects repeated-measures model was then used to examine differences between the predicted and actual 2020 values for both primary outcomes. In this model, time (2017, 2018, 2019, 2020 predicted, 2020 actual) was entered as a fixed-effect predictor variable and site as a random-effect term. Post hoc tests examined for differences between the predicted and actual 2020 values.
χ2 and independent sample t tests were used to examine for differences on secondary outcomes between the 2019 and 2020 study periods and included demographic (age and sex), clinical (substitute consent for ECT, involuntary admission status, indication for ECT, urgent reason for ECT, past response to ECT), and ECT treatment characteristics (ECT type and frequency). Statistical significance was set at P < 0.05.
RESULTS
Primary Outcomes
A total of 5 CARE Network sites participated in this study with 1 study site located in Singapore and the remaining sites in Australia. All participating sites were public hospitals, and the majority provided or started acute ECT exclusively in the inpatient setting. Figure 1 shows the number of patients who started acute ECT at each site during the different study periods. Figure 2 shows the number of acute ECT treatments administered during the study periods for each site. For both primary outcomes, there was no significant difference between the predicted and actual 2020 values.
FIGURE 1.
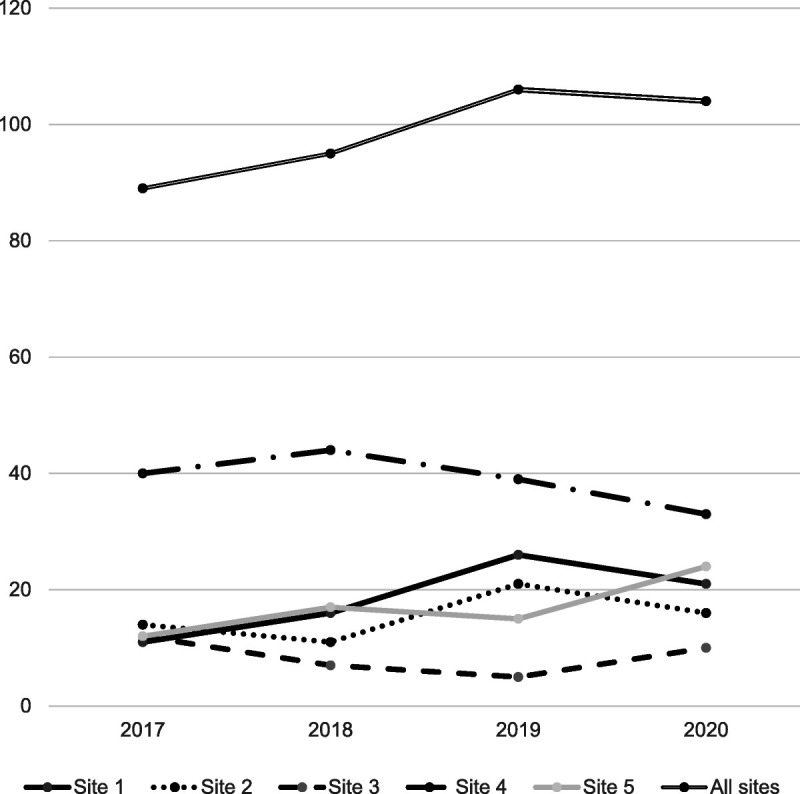
Number of acute ECT courses started during the 3-month study period.
FIGURE 2.
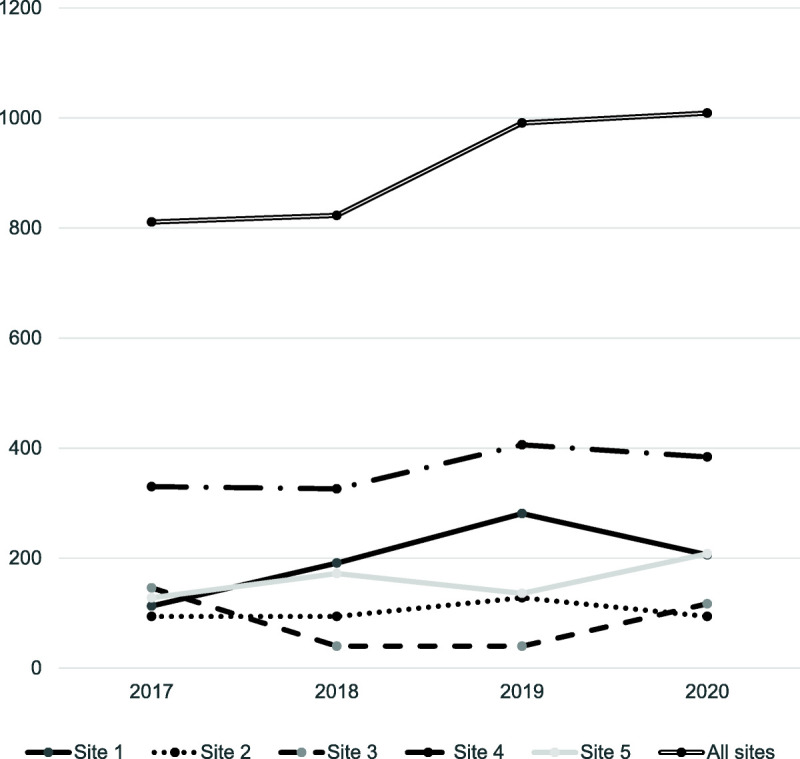
Total number of acute ECT sessions during the 3-month study period.
Secondary Outcomes
In terms of sociodemographic factors, which are available in Table 1, there was no significant difference in the age of ECT patients from 2019 and 2020 with a mean age of 47.9 and 49.3 years, respectively. There was a reduction in proportion of male ECT patients from 2019 (45.6%) to 2020 (33.0%) although this difference did not reach statistical significance (χ2(1) = 3.4, P = 0.06).
TABLE 1.
Sociodemographic Factors of the ECT Patients
| CARE Network Site | Age, Mean (SD) | Male, n (%) | ||
|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | |
| Site 1 | 55.46 (18.0) | 54.1 (17.5) | 7/26 (26.9) | 4/21 (19.0) |
| Site 2 | 46.81 (15.9) | 48.4 (17.8) | 15/21 (71.4) | 5/16 (31.3) |
| Site 3 | 49.61 (15.9) | 42.6 (18.5) | 2/5 (40.0) | 1/10 (10.0) |
| Site 4 | 41.14 (15.3) | 43.1 (16.7) | 20/36 (55.6) | 11/32 (34.4) |
| Site 5 | 57.27 (23.0) | 60.3 (18.8) | 3/15 (20.0) | 13/24 (54.2) |
| CARE Network total | 47.9 (19.2) | 49.3 (17.7) | 47/103 (45.6) | 34/103 (33.0) |
Descriptive statistics for the clinical factors at each site are shown in Tables 2 and 3. The proportion of patients who had substitute consent for ECT significantly increased from 2019 (44.1%) to 2020 (68.7%, χ2(1) = 12.3, P < 0.001). In addition, there was a statistically significant rise in the proportion of ECT patients with involuntary admission status from 2019 (29.1%) to 2020 (59.4%, χ2(1) = 19.0, P < 0.001). There was a statistically significant growth in the proportion of patients receiving ECT for an urgent reason, from 29.7% in 2019 to 40.2% in 2020 (χ2(1) = 6.0, P = 0.049). In contrast, we found that the main indication for ECT did not change significantly (χ2(4) = 5.6, P = 0.24). Compared with 2019, there was a nonsignificant increase in the proportion of patients receiving ECT in 2020 who had a previous partial or good response to ECT from 36.7% to 48.6%.
TABLE 2.
Clinical Characteristics of ECT Patients
| CARE Network Site | Substitute Consent for ECT, n (%)* | Involuntary Admission Status, n (%)* | ||
|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | |
| Site 1 | 6/26 (23.1) | 9/21 (42.9) | 8/26 (30.7) | 14/21 (66.7) |
| Site 2 | 6/21 (28.6) | 9/13 (69.2) | 6/21 (28.6) | 11/15 (73.3) |
| Site 3 | 1/5 (20.0) | 9/10 (90.0) | 1/5 (20.0) | 9/10 (90.0) |
| Site 4 | 26/35 (74.3) | 26/31 (83.9) | 11/36 (30.6) | 15/32 (46.9) |
| Site 5 | 6/15 (40.0) | 15/24 (62.5) | 4/15 (26.7) | 11/23 (47.8) |
| CARE Network total | 45/102 (44.1) | 68/99 (68.7)† | 30/103 (29.1) | 60/101 (59.4)† |
*Inconsistencies in numbers across variables within the same site due to missing data.
†P < 0.05.
TABLE 3.
Clinical Characteristics of the ECT Patients
| CARE Network Site | Main Indication for ECT, n (%)* | Urgent Reason for ECT, n (%)* | Past Partial/Good Response to ECT, n (%)* | |||
|---|---|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | 2019 | 2020 | |
| Site 1 | Mania: 3/22 (13.6) | Mania: 1/16 (6.3) | 7/22 (31.8) | 11/21 (52.4) | 5/18 (27.8) | 4/12 (33.3) |
| Depression: 17/22 (77.4) | Depression: 9/16 (56.2) | |||||
| SCZ/SAD: 1/22 (4.5) | SCZ/SAD: 3/16 (18.7) | |||||
| Catatonia: 1/22 (4.5) | Catatonia: 1/16 (6.3) | |||||
| Other: 0 | Other: 2/16 (12.5) | |||||
| Site 2 | Mania: 4/20 (20.0) | Mania: 2/11 (18.2) | 6/17 (35.3) | 6/11 (54.5) | 1/9 (11.1) | 4/5 (80.0) |
| Depression: 14/20 (70.0) | Depression: 5/11 (45.4) | |||||
| SCZ/SAD: 1/20 (5.0) | SCZ/SAD: 3/11 (27.3) | |||||
| Catatonia: 0 | Catatonia: 1/11 (9.1) | |||||
| Other: 1/20 (5.0) | Other: 0 | |||||
| Site 3 | Mania: 1/5 (20.0) | Mania: 0 | 3/5 (60.0) | 1/10 (10.0) | 2/5 (40.0) | 4/5 (80.0) |
| Depression: 3/5 (60.0) | Depression: 6/7 (85.7) | |||||
| SCZ/SAD: 1/5 (20.0) | SCZ/SAD: 1/7 (14.3) | |||||
| Catatonia: 0 | Catatonia: 0 | |||||
| Other: 0 | Other: 0 | |||||
| Site 4 | Mania: 4/32 (12.5) | Mania: 5/31 (16.1) | 5/32 (15.6) | 8/31 (25.8) | 13/32 (40.6) | 12/31 (38.7) |
| Depression: 5/32 (15.6) | Depression: 7/31 (22.6) | |||||
| SCZ/SAD: 18/32 (56.3) | SCZ/SAD: 15/31 (48.3) | |||||
| Catatonia: 5/32 (15.6) | Catatonia: 2/31 (6.5) | |||||
| Other: 0 | Other: 2/31 (6.5) | |||||
| Site 5 | Mania: 2/15 (13.3) | Mania: 4/23 (17.4) | 6/15 (40.0) | 13/24 (54.2) | 8/15 (53.3) | 12/21 (57.1) |
| Depression: 9/15 (60.0) | Depression: 10/23 (43.4) | |||||
| SCZ/SAD: 1/15 (6.7) | SCZ/SAD: 8/23 (34.9) | |||||
| Catatonia: 3/15 (20.0) | Catatonia: 1/23 (4.3) | |||||
| Other: 0 | Other: 0 | |||||
| CARE Network total | Mania: 14/94 (14.9) | Mania: 12/88 (13.6) | 27/91 (29.7) | 39/97 (40.2)† | 29/79 (36.7) | 36/74 (48.6) |
| Depression: 48/94 (51.0) | Depression: 37/88 (42.1) | |||||
| SCZ/SAD: 22/94 (23.4) | SCZ/SAD: 30/88 (34.1) | |||||
| Catatonia: 9/94 (9.6) | Catatonia: 5/88 (5.7) | |||||
| Other: 1/94 (1.1) | Other: 4/88 (4.5) | |||||
Urgent reasons for acute ECT: suicide risk, aggression/agitation, and inadequate oral intake; nonurgent reasons for ECT: failure of medication, previous good response to ECT, patient preference, and poor tolerability/risks with medications.
*Inconsistencies in numbers across variables within the same site due to missing data.
†P < 0.05.
SAD indicates schizoaffective disorder; SCZ, schizophrenia.
Table 4 summarizes the descriptive statistics for ECT treatment characteristics and indicates most sites administered acute ECT 3 times per week in both 2019 and 2020. One exception was site 2, which had mostly given index ECT twice a week in 2019, although it increased the frequency of ECT in 2020. Furthermore, although the proportion of patients receiving ultrabrief ECT decreased from 2019 to 2020 and there was an increase in use of bifrontal placements, the overall difference in the type of ECT was not significant (χ2(4) = 7.6, P = 0.11).
TABLE 4.
Electroconvulsive Therapy Treatment Characteristics
| CARE Network Site | Type of ECT, n (%) | Acute ECT 3×/wk, n (%)* | ||
|---|---|---|---|---|
| 2019 | 2020 | 2019 | 2020 | |
| Site 1 | Bifrontal: 9/25 (36.0) | Bifrontal: 21/21 (100) | 25/25 (100) | 21/21 (100) |
| Bitemporal: 0 | Bitemporal: 0 | |||
| Right unilateral: 1/25 (4.0) | Right unilateral: 0 | |||
| Ultrabrief: 15/25 (60.0) | Ultrabrief: 0 | |||
| Site 2 | Bifrontal: 13/20 (65.0) | Bifrontal: 8/12 (66.7) | 3/20 (15.0) | 5/10 (50.0) |
| Bitemporal: 0 | Bitemporal: 1/12 (8.3) | |||
| Right unilateral: 4/20 (20.0) | Right unilateral: 2/12 (16.7) | |||
| Ultrabrief: 3/20 (15.0) | Ultrabrief: 1/12 (8.3) | |||
| Site 3 | Bifrontal: 1/5 (20.0) | Bifrontal: 1/10 (10.0) | 4/5 (80.0) | 9/10 (90.0) |
| Bitemporal: 0 | Bitemporal: 2/10 (20.0) | |||
| Right unilateral: 0 | Right unilateral: 0 | |||
| Ultrabrief: 1/5 (20.0) | Ultrabrief: 2/10 (20.0) | |||
| Other: 3/5 (60.0) | Other: 5/10 (50.0) | |||
| Site 4 | Bifrontal: 16/32 (50.0) | Bifrontal: 14/31 (45.2) | 32/32 (100) | 29/30 (96.7) |
| Bitemporal: 8/32 (25.0) | Bitemporal: 3/31 (9.7) | |||
| Right unilateral: 0 | Right unilateral: 3/31 (9.7) | |||
| Ultrabrief: 8/32 (25.0) | Ultrabrief: 11/31 (35.5) | |||
| Site 5 | Bifrontal: 5/15 (33.3) | Bifrontal: 13/24 (54.2) | 15/15 (100) | 22/23 (95.7) |
| Bitemporal: 0 | Bitemporal: 0 | |||
| Right unilateral: 6/15 (40.0) | Right unilateral: 9/24 (37.5) | |||
| Ultrabrief: 4/15 (26.7) | Ultrabrief: 2/24 (8.3) | |||
| CARE Network total | Bifrontal: 44/97 (45.4) | Bifrontal: 57/98 (58.2) | 79/97 (81.4) | 86/94 (91.5) |
| Bitemporal: 8/97 (8.2) | Bitemporal: 6/98 (6.1) | |||
| Right unilateral: 11/97 (11.3) | Right unilateral: 14/98 (14.3) | |||
| Ultrabrief: 31/97 (32.0) | Ultrabrief: 16/98 (16.3) | |||
| Other: 3/97 (3.1) | Other: 5/98 (5.1) | |||
Acute ECT is defined as patients given ECT 2 or 3 times per week.
*Inconsistencies in numbers across variables within the same site due to missing data.
DISCUSSION
To the best of our knowledge, this is one of the first multisite studies to present empirical data observing changes in demographic, clinical, and service data on ECT patients due to the first wave of COVID-19 restrictions. This study corroborates some prior speculation that changes have occurred in ECT patients and service provision as a result of the COVID-19 pandemic. Electroconvulsive therapy clinicians have expressed fears that access to ECT during the COVID-19 pandemic can potentially become even more inequitable8 despite ECT being vital to a population group that is among the most unwell and disadvantaged.18 It can be conjectured that the advice to limit the availability of maintenance ECT has similarities to elective surgery being deferred, where the lack of access to timely treatment could prolong disability, morbidity, and poor quality of life.19,20 However, increasing mental health distress and morbidity in the population during the pandemic21–24 may increase the need for ECT in the future.
Although pandemics can increase the mental health morbidity in the affected population and despite the concerns of professional bodies worldwide about the decreased resources allocated to ECT, we found no significant changes in the total number of acute ECT treatments or in the number of acute ECT courses started across the CARE Network. Although there was a trend at a group level of increasing number of acute ECT treatments and courses started across the last 4 years, there was variability across sites. Between 2019 and 2020, sites 3 and 5 experienced increases, yet decreases were observed in sites 1, 2, and 4. The variability between sites is reflective of true numbers because no cases were removed from the primary analyses because of missing data. This was despite the potential for poorer ECT data collection during the COVID-19 pandemic due to speculation that there would be an increase in demand on mental health clinical resources, which would come at the expense of research.
We hypothesized that greater illness severity, due to the increased mental health morbidity as a result of the COVID-19 pandemic, would be associated with a rise in urgent indications for ECT and increase use of ECT techniques that favors efficacy and faster treatment response. In addition, there were anecdotal reports from 2 sites that their local mental health service experienced reductions in resources for home visits and community-based management, which could contribute to an increase in patients with severe illness who needed ECT. Secondary analyses indeed revealed statistically significant increases in patients with an involuntary admission status, who had substitute consent for ECT, and who had ECT for urgent reasons. This accords with prior discussions that severity of illness is a consideration in allocating ECT resources during the pandemic.14 Furthermore, real-world experience has shown that ECT is highly effective in those lacking capacity to provide consent for ECT, with data showing greater symptom and functional improvement than in those with capacity for consent.25
We also expected and found a nonsignificant reduction in use of ultrabrief ECT and increase in use of brief pulse ECT for bifrontal and unilateral ECT, but not for bitemporal ECT. Furthermore, despite global descriptions of reduced ECT accessibility, including the frequency of ECT, in our sample, there was no major difference in the frequency of acute ECT provided per week. Only 1 site, where twice-a-week ECT formed the majority of acute ECT treatments in 2019, saw an increase in the frequency of ECT in 2020 possibly to complete a course of acute ECT faster. These results taken in context with the decrease in the number of ECT treatments and courses started at site 2 in 2020 show that there were fewer patients receiving ECT but that these patients completed a course of ECT more quickly. Clinicians at site 2 have stated that the rationale of moving from 2 to 3 times per week of ECT in 2020 was to induce quicker recovery because of the uncertainty of accessibility to ECT resources. In addition, clinicians at site 2 indicated that there was a reduction in ECT service capacity and that the increase in ECT frequency was accommodated through the reduction of number of ECT patients. We also speculated that the nonsignificant increase in ECT patients who had a history of good response to ECT in the 2020 study period could be explained by their being prioritized because of declines in ECT resources.
The combination of findings that there was no significant change in ECT service delivery and an upsurge in the proportion of patients requiring urgent ECT may mean that there was a ceiling in ECT resources and that these were diverted to patients with more severe illness. Our results did not demonstrate a decline in the total number of ECT treatments provided, but health service utilization is complicated and influenced by multiple factors, not just by patient illness factors. For example, there may be a change in health behaviors such as delays in seeking treatment for clinical symptoms of mental illness due to the fear of contracting COVID-19 from healthcare settings. In addition, government policies and intervention could differ at each jurisdiction with direct effects (eg, health services diverting ECT services to one specific center) or indirect effects (eg, by affecting the demand in the local labor market and hence levels of unemployment and subsequent effects on mental health).
Strengths and Limitations
This study's main strength is that it is one of the first multisite studies to collect empirical data on the effects of COVID-19 on ECT, using a common data collection framework across sites. The data from this study provide a preliminary observation of the acute impact of COVID-19 on ECT services and examined year-to-year variability by using a corresponding 3-month period in previous year(s) for analysis.
One limitation of this study is the short duration of the study period. This, in turn, may have failed to capture the full extent of effects from COVID-19 restrictions and the delay to relapse in illness once maintenance ECT is reduced or ceased. There may also be a delay in onset of mental health morbidity from the height of psychosocial stress from socioeconomic issues, such as unemployment and reduction of social security payments.
The study was also limited by the lack of data on treatment outcomes, whether ECT was provided on an inpatient or outpatient ECT basis, maximum capacity of ECT at each site, and maintenance ECT. This study did not have data on the number and types of referrals for ECT, which would allow comparison of referred patients who did not receive ECT with patients who did receive ECT. However, some of the secondary outcomes directly and indirectly reflected the anecdotal descriptions from participating sites of the types of patients who were prioritized for ECT. All sites described placing more emphasis on providing acute ECT for urgent reasons. To facilitate rapid discharge from mental health units, some sites selected bilateral treatments to facilitate faster recovery or finished acute ECT courses more rapidly. Other sites anecdotally reported that nonurgent reasons for ECT including treatment for outpatients, maintenance treatments, and depression not requiring an urgent response were deprioritized.
It would be ideal to include treatment outcomes and draw from a larger data set, ideally with comparable data from preceding years to examine changes compared with periods before the COVID-19 pandemic. Given that professional guidelines recommended deprioritizing patients for which relapse in their illness would not lead to significant risk during COVID-19 restrictions, we would have expected a decrease in maintenance ECT patients and maintenance ECT treatments.
Lastly, except for 1 site in Singapore, all of the CARE Network sites included in the analysis were located in Australia, hence reflecting aspects of the Australian context that may not be generalizable internationally because of the different level of social restrictions. Compared with the global context, the duration of the strictest social restrictions of up to 2 months in Australia and Singapore during the first wave of COVID-19 lockdown was relatively short. Even within Australia, there was variability in the level of social restrictions imposed between states and within local areas. As participating sites in this study were all public mental health services, the results may not generalize to private hospital and private clinic settings. We also acknowledge that health systems in Australia and Singapore during the first wave of COVID-19 never reached critical capacity experienced in other countries that were more severely impacted by COVID-19, particularly in those countries with recurrent waves of infections and associated social restrictions. However, this study is a catalyst to encourage global data collection on ECT, so comparisons can be made between health systems, which experienced different levels of stress on hospital capacity.
Implications
Modern ECT practice has not previously been affected by a pandemic with such serious and pervasive effects, with anecdotal reports of decreased provision of ECT due to difficulties accessing personal protective equipment, staffing, time for cleaning, and availability of treatment facilities. Therefore, there was a need to clarify the present situation with quantitative data. This study is among the first to demonstrate the impact of the pandemic on ECT practice and patients even in its early stages.
The Royal Australian and New Zealand College of Psychiatrists specifically issued guidelines on ECT provision during COVID-19, and we have demonstrated changes in ECT practice and ECT patients after that publication. Given the comparable advice from multiple professional bodies globally on the delivery of ECT during COVID-19 and widespread social restrictions, we would expect changes in ECT provision in countries and areas with similarities in ECT practice to Australia such as New Zealand, United Kingdom, Europe, and the United States.26
There is a need for further research through collaboration and collection of empirical data to monitor the effects of the COVID-19 pandemic on the mental health of the population and the changes on mental health policies and resourcing. Pandemics and other natural and man-made disasters remain ongoing threats that can develop quickly, and mental health services require data to help them respond to crises in a timely manner. The availability of high-quality data could allow clinicians, clinical ethicists, health services, professional bodies, and public health policy makers, to develop, refine, and advocate for safe, ethical, and equitable ECT service delivery during the pandemic and in the future.
Footnotes
E.K. declares honoraria from the Lundbeck Institute outside the submitted work. C.K.L. reports equipment support from Mecta for research. D.M.M. and V.D. were supported by a National Health and Medical Research grant awarded to C.L. (Grant No. 1195651). The other authors declare no conflict of interest.
Contributor Information
Brandon Le, Email: ble@kirby.unsw.edu.au.
Colleen K. Loo, Email: colleen.loo@unsw.edu.au.
Vanessa Dong, Email: v.dong@unsw.edu.au.
Phern-Chern Tor, Email: phern_chern_tor@imh.com.sg.
Don Davidson, Email: Don.Davidson@sa.gov.au.
Titus Mohan, Email: Titus.Mohan@sa.gov.au.
Susan Waite, Email: Sue.Waite@sa.gov.au.
Grace Branjerdporn, Email: Grace.Branjerdporn@health.qld.gov.au.
Shanthi Sarma, Email: Shanthi.Sarma@health.qld.gov.au.
Salam Hussain, Email: Salam.Hussain@health.wa.gov.au.
Donel M. Martin, Email: donel.martin@unsw.edu.au.
REFERENCES
- 1.American Psychiatric Association . COVID-19 pandemic guidance document: electroconvulsive therapy as an essential procedure. Available at: https://www.psychiatry.org/File%20Library/Psychiatrists/APA-Guidance-ECT-COVID-19.pdf. Accessed October 25, 2020.
- 2.Royal Australian and New Zealand College of Psychiatrists . Information about the provision of ECT treatment during the COVID-19 pandemic. 2020. Available at: https://www.ranzcp.org/files/resources/college_statements/practice_guidelines/ranzcp-information-ect-and-covid-19_may-2020.aspx. Published April 2020. Accessed June 27, 2020.
- 3.Royal College of Psychiatrists . Continuing to provide ECT during the COVID-19 pandemic. 2020. Available at: https://www.rcpsych.ac.uk/docs/default-source/about-us/covid-19/ect-covid-19-briefing-may-20-submitted.pdf?sfvrsn=dd39d278_2. Accessed July 11, 2020.
- 4.Department of Psychiatry National Institute of Mental Health & Neurosciences . Mental Health in the Times of COVID-19 Pandemic: Guidance for General Medical and Specialised Mental Health Care Settings. Bengaluru, India: National Institute of Mental Health & Neurosciences; 2020. [Google Scholar]
- 5.International Society for ECT and Neurostimulation . Position statement on ECT as an essential procedure during COVID-19. Available at: https://www.isen-ect.org/covid-19-essential-procedure. 2020. Accessed January 5, 2021.
- 6.Boland X, Dratcu L. ECT and COVID-19 in acute inpatient psychiatry: more than clinical issues alone. J ECT. 2020;36:223–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bryson EO, Aloysi AS. A strategy for management of ECT patients during the COVID-19 pandemic. J ECT. 2020;36:149–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demas ML. Electroconvulsive therapy and triaging during reduced access & the COVID-19 pandemic: a personal perspective. J ECT. 2020;36:226–228. [DOI] [PubMed] [Google Scholar]
- 9.Espinoza RT, Kellner CH, McCall WV. Electroconvulsive therapy during COVID-19: an essential medical procedure—maintaining service viability and accessibility. J ECT. 2020;36:78–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tor PC Phu AHH Koh DSH, et al. Electroconvulsive therapy in a time of coronavirus disease. J ECT. 2020;36:80–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramakrishnan VS Kim YK Yung W, et al. ECT in the time of the COVID-19 pandemic. Australas Psychiatry. 2020;28:527–529. [DOI] [PubMed] [Google Scholar]
- 12.Bellini H Cretaz E Rigonatti LF, et al. Electroconvulsive therapy practice during the COVID-19 pandemic. Clinics. 2020;75:e2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Warren N, Siskind D, Lie D. Electroconvulsive therapy during severe acute respiratory syndrome coronavirus 2 pandemic. Aust N Z J Psychiatry. 2020;54:1224–1224. [DOI] [PubMed] [Google Scholar]
- 14.Tor P-C, Tan J, Loo C. Model for ethical triaging of electroconvulsive therapy patients during the COVID-19 pandemic. BJPsych Bulletin. 2020;45:175–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Royal College of Psychiatrists . Two Thirds of Patients Can't Get Life-saving ECT Treatment for Mental Illness During the Pandemic. London, United Kingdom: Royal College of Psychiatrists; 2020. [Google Scholar]
- 16.Martin DM Gálvez V Lauf S, et al. The Clinical Alliance and Research in Electroconvulsive Therapy Network: an australian initiative for improving service delivery of electroconvulsive therapy. J ECT. 2018;34:7–13. [DOI] [PubMed] [Google Scholar]
- 17.IBM Corp . IBM SPSS Statistics for Windows. 26.0 ed. Armonk, NY: IBM Corp; 2019. [Google Scholar]
- 18.Weiss A Hussain S Ng B, et al. Royal Australian and New Zealand College of Psychiatrists professional practice guidelines for the administration of electroconvulsive therapy. Aust N Z J Psychiatry. 2019;53:609–623. [DOI] [PubMed] [Google Scholar]
- 19.COVIDSurg Collaborative . Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020;107:1440–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Royal Australasian College of Surgeons . Surgery Triage: Responding to the COVID-19 Pandemic: A Rapid Review Commissioned by RACS. 5 May 2020. Australia: Melbourne; 2020. [Google Scholar]
- 21.Huang Y, Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian J Psychiatry. 2020;51:102052. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 22.Pierce M Hope H Ford T, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7:883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.O'Connor RC Wetherall K Cleare S, et al. Mental health and wellbeing during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. 2020;1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salari N Hosseinian-Far A Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020;16:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tor P-C Tan FJS Martin D, et al. Outcomes in patients with and without capacity in electroconvulsive therapy. J Affect Dis. 2020;266:151–157. [DOI] [PubMed] [Google Scholar]
- 26.Leiknes KA, Schweder LJ-v, Høie B. Contemporary use and practice of electroconvulsive therapy worldwide. Brain Behav. 2012;2:283–344. [DOI] [PMC free article] [PubMed] [Google Scholar]


