Abstract
Study Design:
Retrospective analysis of inpatient and outpatient medical insurance claims data from a database containing over 100 million individuals.
Objective:
To quantify the healthcare resource utilization (HCRU) of non-surgical treatments in the first 2 years after a chronic, refractory low back pain (CRLBP) diagnosis.
Summary of Background Data:
Patients with persistent low back pain (LBP) despite conventional medical management and who are not candidates for spine surgery are considered to have chronic, refractory low back pain (CRLBP) and incur substantial healthcare costs over time. Few data exist on the HCRU of this specific population.
Methods:
The IBM MarketScan Research databases from 2009 to 2016 were retrospectively analyzed to identify US adults with a diagnosis of non-specific LBP and without cancer, spine surgery, failed back surgery syndrome, or recent pregnancy. We required >30 days of utilization of pain medications or non-pharmacologic therapies within both the 3–12- and 12–24-month periods post-diagnosis. Annual total healthcare costs, costs subdivided by insurance type, and use of non-surgical therapies were determined for 2 years after diagnosis of LBP.
Results:
55,945 patients with CRLBP were identified. Median total cost was $6,590 (Q1 $2,710, Q3 $13,922) in the first year, almost doubling the baseline cost; costs were highest for patients with Medicare Supplemental insurance, reaching $10,156 (Q1 $5,481, Q3 $18,570). 33,664 (60.2%) patients engaged physical therapy, 28,016 (50.1%) engaged chiropractors, and 14,488 (25.9%) had steroid injections. 36,729 (65.7%) patients used prescription pain medications, most commonly opioids (N=31,628, 56.5%) and muscle relaxants (N=21,267, 38.0%).
Conclusion:
This study is one of the first to investigate the HCRU of a large, longitudinal US cohort of patients with CRLBP. These patients experience substantial healthcare costs. Contrary to LBP management guidelines, most patients used opioids, and several non-pharmacologic therapies were used by only a few patients.
Introduction
Low back pain (LBP) is the leading cause of disability worldwide.[1] In the United States (US), the total economic burden of LBP has been estimated as high as $624.8 billion.[2] Chronic LBP (cLBP), defined as ≥3 months in duration, accounts for most of this cost.[3] Treatment approaches for cLBP often include combinations of medications, non-pharmacologic interventions, and spine surgery when necessary.[4]
Chronic LBP can be broadly classified into specific and non-specific pathologies. Specific pathologies, such as vertebral compression fractures and herniated discs, are often indications for spine surgery.[5] However, all but 10% of patients with cLBP have non-specific LBP,[6] and while up to 42% of patients with cLBP recover within 12 months,[7] the pain persists despite conservative medical management for some patients. These patients are considered to have chronic, refractory low back pain (CRLBP). Recent data suggest that within the first year of their LBP diagnosis, the vast majority of these patients do not undergo surgery, but total direct healthcare costs reach $1.8 billion.[8]
Although the healthcare resource utilization (HCRU) among patients with cLBP has been investigated,[9–11] to our knowledge few data exist for the CRLBP subpopulation. The healthcare resource utilization (HCRU) of patients with CRLBP includes a variety of costs, including multiple outpatient visits, emergency department visits, and medications.[9] This study aims to characterize a longitudinal cohort of US patients with CRLBP and investigate their initial HCRU and use of non-surgical therapies. Such data will aid patients, healthcare providers, payers and policy makers in the management of CRLBP.
Materials and Methods
Data source
The IBM MarketScan Research databases, which contain data from the Commercial Claims and Encounters (patients <65 years old), Medicare Supplemental and Coordination of Benefits (patients ≥65 years old), and Medicaid databases, were retrospectively analyzed to assess the HCRU associated with CRLBP. Data from 2009–2016 were used.
Cohort selection
The index date was defined as the first outpatient or inpatient service with a diagnosis of LBP (i.e., non-cervical, non-thoracic). Patients 18 years or older with an index date between January 1, 2010 and December 31, 2014 were selected. Diagnoses of interest were identified by International Classification of Diseases, Ninth Revision (ICD-9) codes. Codes for common non-specific LBP diagnoses[12, 13] were included: spondylosis not otherwise specified (NOS; 721.90), lumbar/lumbosacral disc degeneration (722.52), disc degeneration NOS (722.6), lumbar spinal stenosis without claudication (724.02), lumbago (724.2), lumbosacral spondylosis (756.11), lumbosacral spondylosis without myelopathy (721.3), and backache (724.5). Patients with diagnoses of cancer (identified by the HCUP[14] Clinical Classifications Software [CCS] categories 11–45) at any point during the study period or pregnancy (identified by CCS categories 180–186, 196) in the year prior to index diagnosis were excluded because patients with cancer or pregnancy may represent a different patient population. Patients with <1 year of data pre-diagnosis or <2 years of data post-diagnosis, without continuous enrollment, and without complete outpatient pharmacy data during the study period were also excluded.
To characterize LBP refractory to non-surgical management, individuals with a diagnosis of post-laminectomy syndrome (i.e., failed back surgery syndrome, FBSS) or who underwent spine surgery or spinal cord stimulation (SCS) during the study period were excluded. Procedures for non-pharmacologic therapy, spine surgery, and SCS were identified by Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes. Codes for spine surgery and SCS were compiled from previous studies[15, 16] and a comprehensive search of coding databases (see Table, Supplemental Digital Content 1, which includes these procedure codes).
Conventional therapy included pain medications and non-pharmacologic treatments in accordance with previous literature[17, 18] (see Table, Supplemental Digital Content 2, which lists these procedure codes). For LBP to qualify as refractory to conventional therapy, patients must have used at least 1 pain medication for >30 days or non-pharmacologic treatment within both the 3–12-month and 12–24-month periods after index diagnosis. Requisite utilization of conventional therapy for the 3–12 months after diagnosis distinguished cLBP from an episode of acute LBP that recurred in the second year.[4, 19] The requirement that patients continue to use these therapies in the 12–24 months after diagnosis represented the subset of patients without resolution of cLBP within 12 months.[7]
Demographics and patient characteristics
Age, sex, year of index diagnosis, employment status, insurance type, and geographic region of residence were collected from insurance claims data at time of diagnosis. Elixhauser Comorbidity Index[20] scores were derived from claims data at baseline (1-year pre-diagnosis period).
Provider visits and admissions
Outpatient and emergency department visits and inpatient admissions billed with an eligible LBP diagnosis were quantified for 2 years post-diagnosis.
Utilization of prescription medications and non-pharmacologic therapies
Utilization of prescribed pain medications was represented by the proportion of patients who filled valid prescriptions (i.e., non-negative metric quantity or days of supply) for analgesics (MarketScan therapeutic classes 62, 203), anticonvulsants (classes 64, 68), muscle relaxants (classes 29, 30, 31, 214), non-steroidal anti-inflammatory drugs (NSAIDs; classes 58, 59), and opioids (propoxyphene, codeine, hydrocodone, tramadol, pentazocine, morphine, oxycodone, hydromorphone, meperidine, oxymorphone, levorphanol, methadone, fentanyl, buprenorphine, butorphanol, opium, tapentadol). The utilization of each non-pharmacologic therapy was determined by calculating the number of services per patient and the proportion of patients with procedure codes for each of the following treatments billed with an eligible LBP diagnosis: epidural or facet steroid injection, trigger point injection, botulinum toxin injection, physical therapy, psychological therapy, chiropractic therapy, massage therapy, occupational therapy, radiofrequency ablation, acupuncture, biofeedback. Utilization of these non-surgical therapies was determined for 2 years post-diagnosis.
Cost analysis
Selection of patients included in the cost analysis is outlined in Figure 1. The primary outcome was total cost, which comprised the total amount paid to providers. Service costs represented all costs excluding outpatient medications. Back-pain related costs comprised claims associated with any of the eligible LBP diagnoses. Medication costs did not include inpatient medications, as available data were from outpatient pharmacy claims. A secondary analysis subdivided patients by insurance type (commercial, Medicaid, Medicare Supplemental). Costs were calculated at baseline (1-year pre-index period) and for 2 years post-diagnosis; medication costs were calculated for patients who had valid prescriptions for the medications. All costs were adjusted for cost inflation with the reference year of 2018 using the Consumer Price Index provided by the US Department of Labor Bureau of Labor Statistics.[21]
Figure 1. Flow diagram of selection of study cohort.
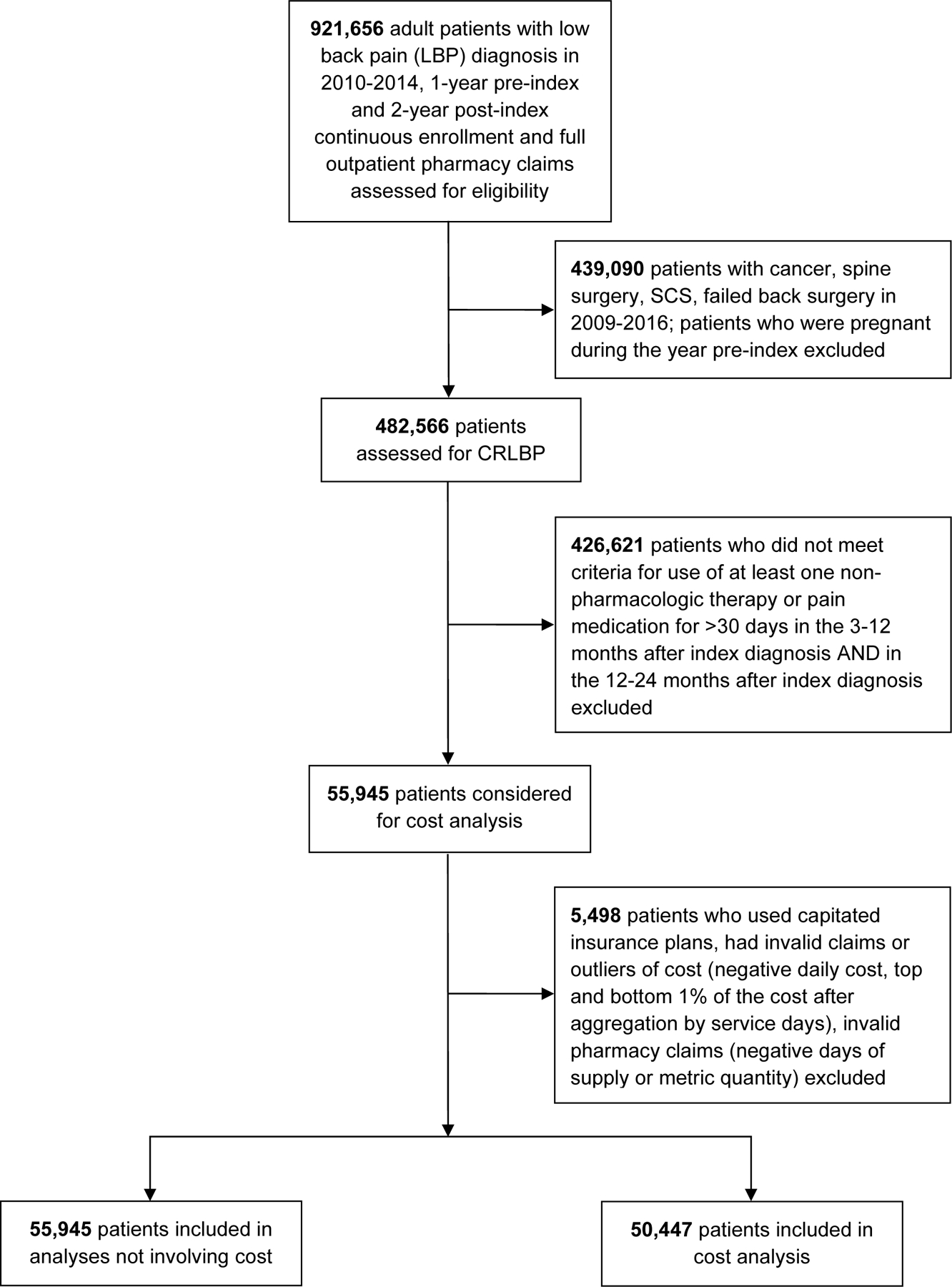
CRLBP: Chronic, refractory low back pain; SCS: Spinal cord stimulation.
Statistical analysis
Data were summarized with descriptive statistics. Analyses were performed using SAS software version 9.4 (SAS Institute Inc., Cary, NC). The ggplot2 package in R 3.5.3 (R Core Team, Vienna, Austria) was used to graphically illustrate data.
Results
An initial cohort of 921,656 adult patients with an eligible LBP diagnosis with an index date during 2010–2014, continuous enrollment, and full outpatient pharmacy claims during the study period was identified. Excluding patients with a cancer, spine surgery, SCS, or FBSS between 2009–2016 or pregnancy in the year prior to diagnosis yielded a cohort of 482,566 patients. A final cohort of 55,945 patients was identified after applying criteria for utilization of therapies. 50,447 patients were included in the cost analysis (Figure 1).
Demographics and patient characteristics
Demographic information for the entire cohort is summarized in Table 1. The median age was 51.0 years (IQR 41.0–59.0). Patients were mostly female (58.9%), employed (55.7%), and enrolled in commercial insurance (71.9%). While several patients had comorbidities, median baseline Elixhauser Comorbidity Index was 0.0 (Q1 0.0, Q3 0.0), indicating a relatively healthy study cohort.
Table 1.
Demographics and characteristics of entire cohort.
| Demographic Characteristic | Baseline Value (at Diagnosis) |
|---|---|
| No. of patients included in cohort | 55,945 |
| Age at diagnosis | |
| Mean (SD) | 50.5 (14.2) |
| Median (Q1, Q3) | 51.0 (41, 59) |
| Sex, No. (%) | |
| Female | 32,943 (58.9) |
| Year of diagnosis, No. (%) | |
| 2010 | 3,213 (5.7) |
| 2011 | 6,871 (12.3) |
| 2012 | 4,565 (8.2) |
| 2013 | 1,903 (3.4) |
| 2014 | 39,393 (70.4) |
| Employment status,a No. (%) | |
| Full time/part time | 31,138 (55.7) |
| Retired | 10,778 (19.3) |
| Dependent/other | 6,465 (11.6) |
| Long-term disability | 106 (0.2) |
| Medicaid | 7,458 (13.3) |
| Insurance type, No. (%) | |
| Commercial | 40,208 (71.9) |
| Medicaid | 7,458 (13.3) |
| Medicare | 8,279 (14.8) |
| Elixhauser Comorbidity Indexb | |
| Mean (SD) | 0.7 (3.9) |
| Median (Q1, Q3) | 0.0 (0.0, 0.0) |
| Range | −16.0–47.0 |
| Elixhauser comorbidities,c No. (%) | |
| HIV/AIDS | 118 (0.2) |
| Alcohol abuse | 920 (1.6) |
| Anemia deficiency | 4,047 (7.2) |
| Rheumatoid arthritis | 3,221 (5.8) |
| Blood loss anemia | 237 (0.4) |
| Congestive heart failure | 1,262 (2.3) |
| Chronic pulmonary disease | 8,344 (14.9) |
| Coagulopathy | 524 (0.9) |
| Depression | 6,673 (11.9) |
| Diabetes without chronic complications | 8,241 (14.7) |
| Diabetes with chronic complications | 2,371 (4.2) |
| Drug abuse | 1,712 (3.1) |
| Fluid and electrolyte disorders | 3,267 (5.8) |
| Hypertension | 20,607 (36.8) |
| Hypothyroidism | 6,218 (11.1) |
| Liver disease | 1,329 (2.4) |
| Lymphoma | 2,663 (4.8) |
| Metastatic cancer | 5,506 (9.8) |
| Other neurological disorders | 463 (0.8) |
| Obesity | 2,380 (4.3) |
| Paralysis | 5,405 (9.7) |
| Peripheral vascular disease | 543 (1.0) |
| Psychoses | 1,195 (2.1) |
| Pulmonary circulation disorder | 37 (0.1) |
| Renal failure | 2,221 (4.0) |
| Solid tumor without metastasis | 776 (1.4) |
| Peptic ulcer disease | 37 (0.1) |
| Valvular disease | 2,221 (4.0) |
| Weight loss | 776 (1.4) |
Full time/part time includes Active full time, Active part time; Retiree includes Early retiree, Medicare eligible retiree, Retiree (status unknown); Other includes COBRA continuee, Surviving spouse/Dependent, Other/Unknown.
Elixhauser Comorbidity Index was calculated at 1 year pre-diagnosis using van Walraven et al composite (VW) score without cardiac arrhythmia.
The proportion of patients with each Elixhauser comorbidity was calculated at 1 year pre-index diagnosis.
Q1: First quartile; Q3: Third quartile; SD: Standard deviation.
Back pain-related provider visits
We included 27,997 (50.0%) patients with at least 4 outpatient visits (excluding the index visit) in the first year, and 38,340 (68.5%) in the second year. Few patients (N=2,768, 4.9%) had an emergency department visit in the first year, and 3,752 (6.7%) in second year. Only 0.1% of patients (33 in the first year, 52 in the second year) had at least 1 back pain-related inpatient admission.
Cost analysis
Costs at baseline and for the first and second years post-diagnosis are summarized in Table 2. Median total cost in the first year almost doubled the baseline cost to $6,590 (Q1 $2,710, Q3 $13,922) and decreased slightly in the second year. Outpatient services accounted for the majority of total costs. Fewer than 2% of patients had back pain-related inpatient claims.
Table 2.
Costs for entire cohort.
| Baseliney | First Year | Second Year | |
|---|---|---|---|
| No. of patients included in cohort | 50,447 | 50,447 | 50,447 |
| Total cost, $ | |||
| N (%) | 50,447 (100.0) | 50,447 (100.0) | 50,447 (100.0) |
| Mean (SD) | 7,272 (9,694) | 10,796 (12,500) | 10,069 (11,590) |
| Median (Q1, Q3) | 3,732 (1,292, 9,072) | 6,590 (2,710, 1,3922) | 5,948 (2,297, 13,252) |
| Range | (0–65,148) | (0–122,742) | (0–65,162) |
| Total service cost, $ | |||
| N (%) | 50,447 (100.0) | 50,447 (100.0) | 50,447 (100.0) |
| Mean (SD) | 5,153 (8,051) | 8,276 (10,619) | 7,434 (9,615) |
| Median (Q1, Q3) | 2,192 (772, 5,757) | 4,655 (1,904, 10,139) | 3,929 (1,536, 9,079) |
| Range | 0–64,413 | 0–117,674 | 0–64,298 |
| Outpatient service cost, $ | |||
| N (%) | 50,447 (100.0) | 50,447 (100.0) | 50,447 (100.0) |
| Mean (SD) | 4,323 (6,160) | 7,214 (8,473) | 6,361 (7,632) |
| Median (Q1, Q3) | 2,140 (767, 5,270) | 4,505 (1,887, 9,270) | 3,800 (1,522, 8,154) |
| Range | 0–63,333 | 0–117,674 | 0–64,060 |
| Back pain-related outpatient service cost, $ | |||
| N (%) | 0 (0.0) | 50,447 (100.0) | 50,447 (100.0) |
| Mean (SD) | - | 2,586 (3,872) | 1,638 (3,017) |
| Median (Q1, Q3) | - | 1,328 (520, 3,144) | 678 (234, 1,787) |
| Range | - | 0–79,625 | 0–55,036 |
| Pain medication cost,a $ | |||
| N (%) | 28,117 (56.7) | 33,588 (66.6) | 32,205 (63.8) |
| Mean (SD) | 431 (1,646) | 533 (1,737) | 595 (1,818) |
| Median (Q1, Q3) | 42 (9, 226) | 81 (12, 375) | 82 (10, 415) |
| Range | 0–52,610 | 0–60,950 | 0–52,758 |
| Opioid cost,a $ | |||
| N (%) | 24,108 (48.6) | 29,403 (58.3) | 27,979 (55.5) |
| Mean (SD) | 352 (1,608) | 427 (1,647) | 491 (1,707) |
| Median (Q1, Q3) | 26 (7, 137) | 46 (9, 245) | 49 (8, 291) |
| Range | 0–52,518 | 0–60,577 | 0–52,479 |
Baseline costs were calculated for the year prior to diagnosis. Back pain-related costs represented costs incurred after an eligible low back pain diagnosis and therefore were not available at baseline. Medication costs were calculated for patients with valid prescriptions for pain medications.
Q1: First quartile; Q3: Third quartile; SD: Standard deviation.
For the 33,588 (66.6%) patients with claims for pain medications and the 29,403 (58.3%) patients with claims for opioids in the first year post-diagnosis, median costs were $81 (Q1 $12, Q3 $375) and $46 (Q1 $9, Q3 $245), respectively. These costs approximately doubled the baseline costs and were similar in the second year.
Costs subdivided by insurance type
Most patients (N=36,710, 72.8%) had commercial insurance, while 6,714 (13.3%) had Medicaid, and 7,023 (13.9%) had Medicare Supplemental insurance at diagnosis. Costs were consistently highest for Medicare Supplemental insurance and lowest for Medicaid. First-year median (Q1, Q3) total cost was $10,156 ($5,481, $18,570) for patients with Medicare Supplemental insurance, $6,377 ($2,818, $13,339) for patients with commercial insurance, and $3,243 ($0, $11,188) for patients with Medicaid (Figure 2).
Figure 2. Total costs subdivided by insurance type.
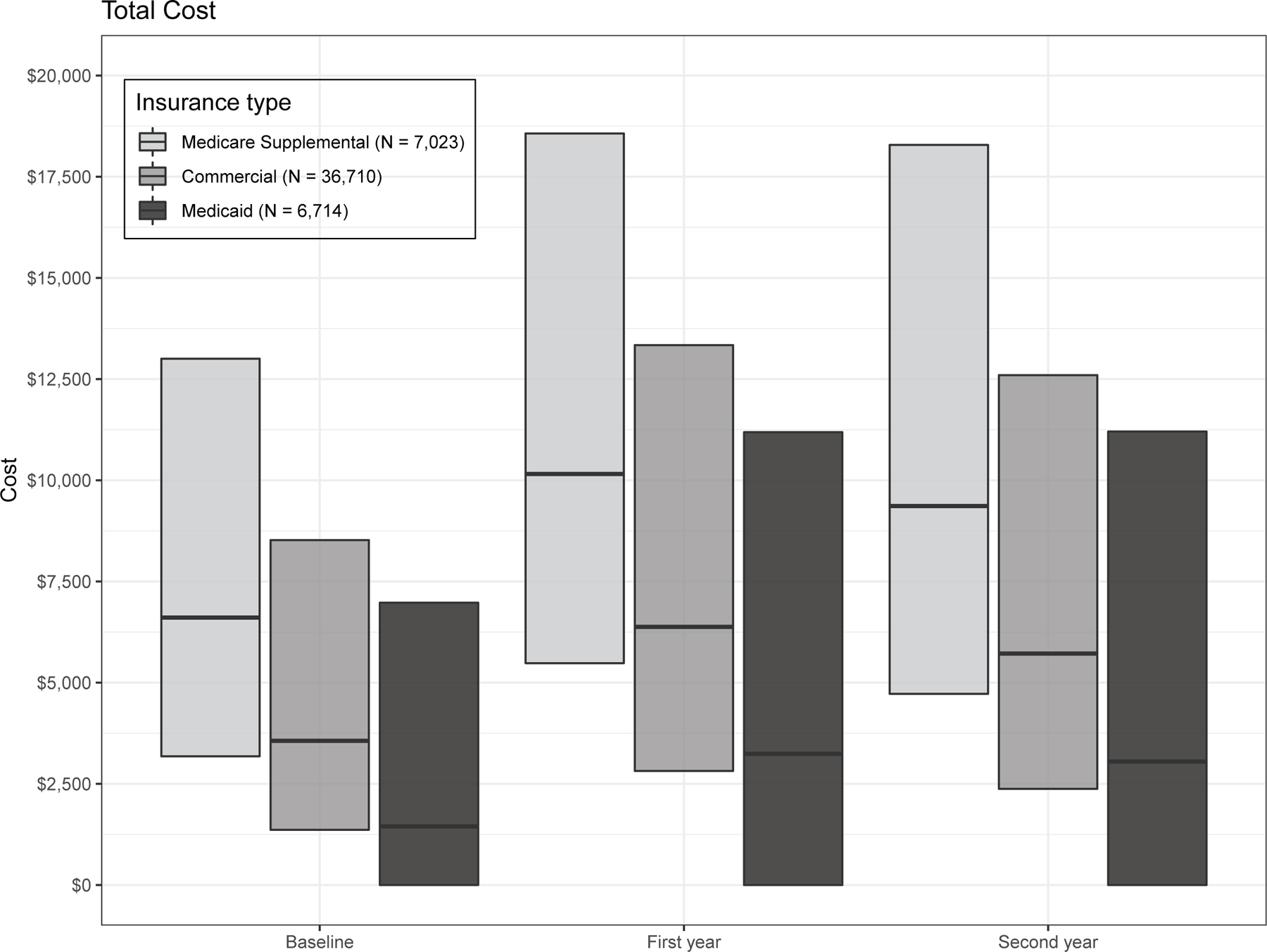
Costs were calculated at baseline (1 year pre-index diagnosis) and for the first and second years post-index diagnosis. Median (black horizontal line), Q1 (first quartile; lower portion of bar), and Q3 (third quartile; upper portion of bar) are depicted. Minimum and maximum values are not depicted due to large range ($0-$122,742). Note: Patients with commercial insurance are <65 years old, and patients with Medicare Supplemental are ≥65 years old.
Pain medication costs (N=33,588) and opioid costs (N=29,403) were fairly similar between the insurance types and between the first and second years post-diagnosis. First-year median (Q1, Q3) pain medication costs were $99 ($24, $346) for patients with Medicare Supplemental insurance, $78 ($14, $359) for patients with commercial insurance, and $75 ($0, $452) for patients with Medicaid. Median (Q1, Q3) first-year costs for opioids were $59 ($16, $243) for patients with Medicare Supplemental, $45 ($10, $231) for patients with commercial insurance, and $36 ($0, $289) for patients with Medicaid.
Utilization of prescription pain medications
Utilization of prescription medications for the entire 2 years post-diagnosis is summarized in Figure 3. Overall, most patients (N=36,729, 65.8%) had valid prescription(s) for pain medications. Opioids were the most frequently used (N=31,628, 56.7%), followed by muscle relaxants (N=21,267, 38.1%).
Figure 3. Proportions of patients using prescription pain medications.
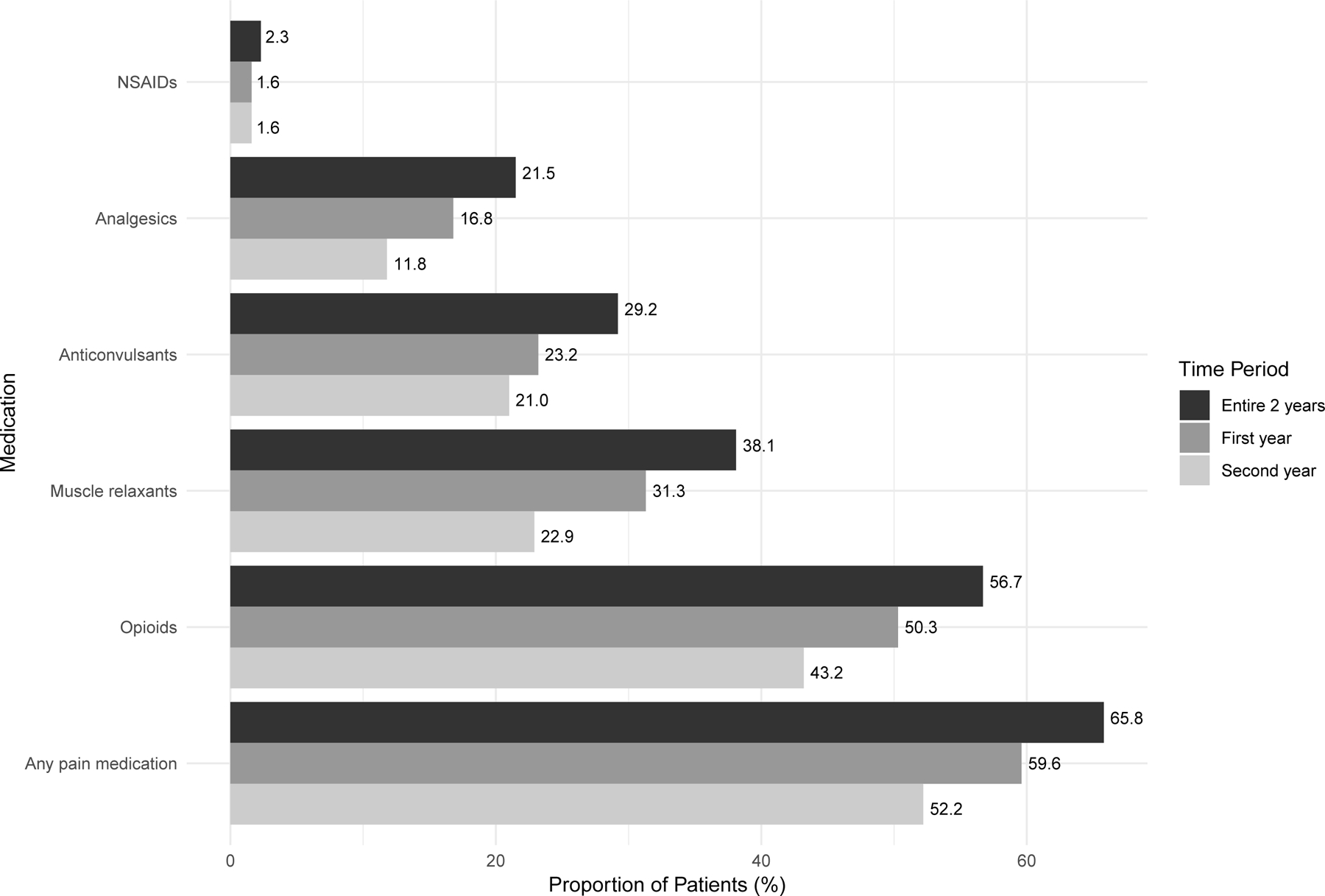
Proportions represent patients with non-negative metric quantity or days of supply of each pain medication. NSAIDs: Non-steroidal anti-inflammatory drugs.
Utilization of non-pharmacologic therapy
Most patients (N=48,648, 87.0%) used non-pharmacologic therapy during the 2 years post-diagnosis (Figure 4). Patients most commonly used physical therapy (N=33,664, 60.2%) chiropractic therapy (N=28,016, 50.1%), and steroid injection (N=14,488, 25.9%).
Figure 4.
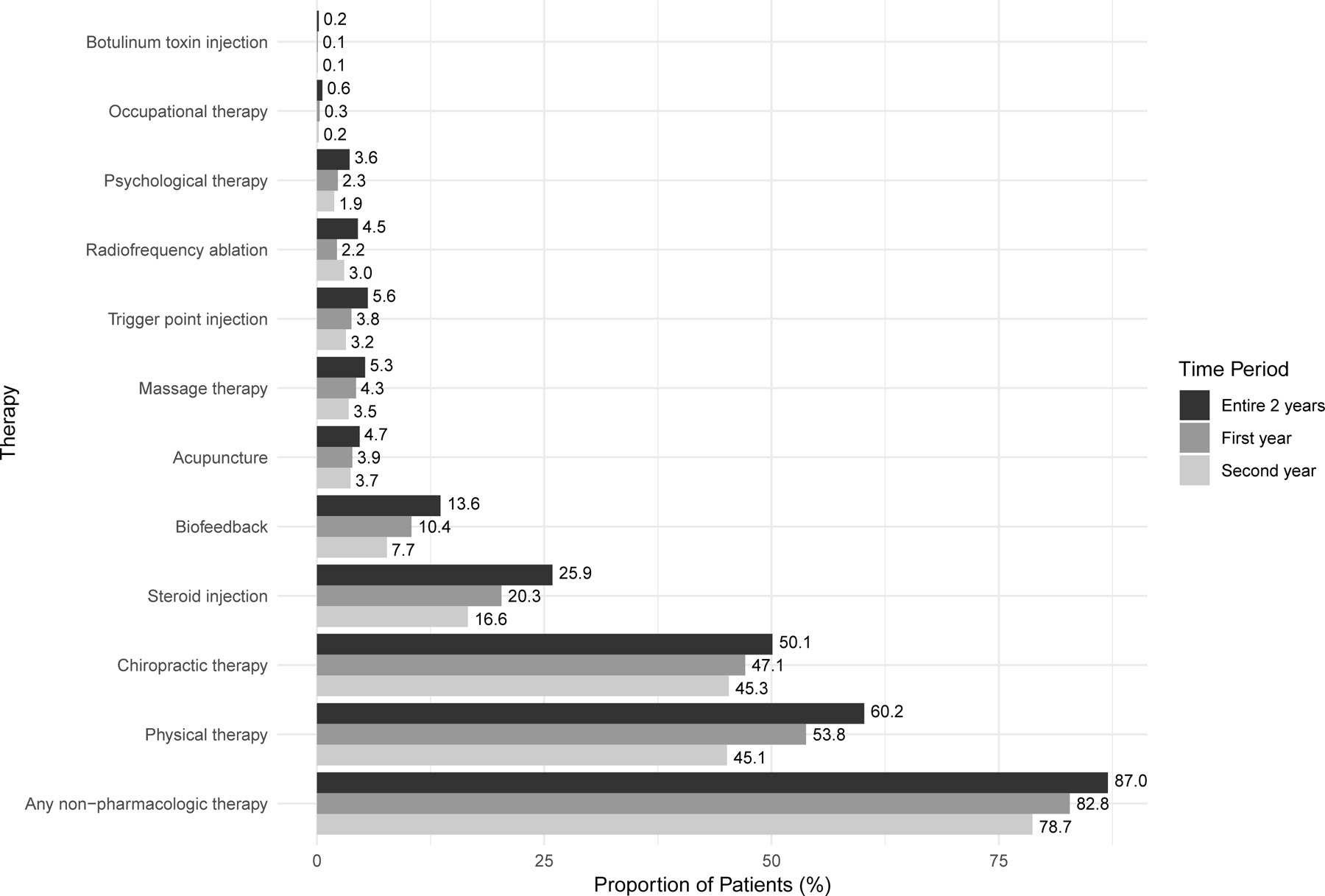
Proportions of patients using non-pharmacologic therapies.
Discussion
This study is one of the first to retrospectively analyze medical insurance claims data to investigate the HCRU of a large, longitudinal cohort of patients with CRLBP, which was defined as cLBP that was refractory to 2 years of medications and/or non-pharmacologic therapies and for which spine surgery was not performed. We found that patients experienced substantial post-diagnosis increases in healthcare costs associated with multiple outpatient visits per year and use of non-surgical therapies.
Changes in healthcare costs after low back pain diagnosis
Costs for the first year after diagnosis approximately doubled baseline costs and remained high in the second year. Interestingly, we observed relatively high median baseline costs. While these may include treatment for comorbid conditions, our cohort had a relative lack of comorbidities. Therefore, these costs may be associated with conditions not captured by the Elixhauser Comorbidity Index or our inclusion criteria or with multiple provider visits, costly (and often inappropriate)[8] diagnostics, and therapies for other LBP diagnoses before the final index diagnosis was determined. Ultimately, the dramatic increase in cost may be accounted for by the tendency of providers to try increasingly more invasive and expensive therapies as the LBP becomes refractory. To better characterize the HCRU of this population, future research should compare the HCRU among patients whose LBP resolves and investigate the change in healthcare costs over several years among patients with CRLBP, particularly among those who eventually undergo surgery.[22]
While total costs were high, median pain medication costs were unexpectedly low. One explanation is that using pharmacy data to quantify medication utilization does not capture use of over-the-counter medications. For example, prescription NSAIDs, which are ubiquitous and recommended as first-line therapy for cLBP,[4] were used by 2.3% of patients in this study, compared to an estimated 26.2% in a previous retrospective analysis of claims data.[9] Further, the presence of relatively substantial pain medication costs at baseline reflects the presence of other pain diagnoses and/or errors in identifying the index visit. Finally, our pain medication prescription duration requirements did not distinguish episodic use from consistent use. Therefore, patients may have had relatively low overall medication use over time.
Effects of insurance coverage on healthcare resource utilization
One cannot overstate the impact of insurance coverage on healthcare costs. Patients with Medicaid consistently incurred the lowest costs, and patients with Medicare Supplemental insurance experienced much higher costs than other patients. This discrepancy may be partly explained by previously observed increased spending for patients >65 years old relative to patients <65 years old[23] but warrants further research. Nevertheless, the influence of insurance coverage on HCRU should be considered in decisions regarding treatment of CRLBP.
Insurance coverage also impacts treatment decisions. First, we only investigated usage of therapies associated with insurance claims. The out-of-pocket costs for other therapies may be prohibitive for some patients, further limiting treatment options. Second, as reflected in this study by their widespread use and low cost, opioids are often classified on low formulary tiers with non-opioid alternatives, with minimal difference in cost sharing.[24] Past and present cLBP treatment guidelines recommend psychotherapy in conjunction with multidisciplinary rehabilitation and exercise, reserving opioids for severe, refractory pain, and only for a short time.[25, 26] We found that the most-used non-pharmacologic therapies were physical therapy and chiropractic services, which are among the therapies most commonly covered by commercial, Medicaid, and Medicare Advantage plans.[27] In contrast, our study captured very few patients using massage therapy, acupuncture and psychological therapy, which currently are not covered by most payers,[27] and the low utilization we observed likely reflects a lack of insurance coverage during the study period as well. These discrepancies highlight a lag between published recommendations and efficacy data and insurance coverage for some therapies.[24, 27]
Limitations
As with all large database studies, interpretations of this study are limited by the administrative nature of the data. Use of the IBM MarketScan databases relies on accurate coding of diagnoses and procedures, but this process is subject to errors. Because we had incomplete inpatient pharmacy data, we could only report outpatient medication cost and usage. However, this limitation is mitigated by the low proportion of inpatient claims (6.7%), of which a small fraction was associated with a diagnosis of LBP, and the even lower proportion of patients (0.1%) with inpatient admissions. Data not associated with an insurance claim, such as medications or services not billed to or covered by insurance, results of diagnostics, or patient-reported pain scores or costs, are not available in the dataset. Therefore, the costs reported here likely underestimate the true total cost. Finally, the duration of pain medication prescriptions does not necessarily reflect the actual medication utilization or degree of pain and suffering patients experienced; the latter is likely underestimated by our requirement of a prescription duration of >30 days.
Of note, a diagnosis of CRLBP relies on provider expertise. This posed a challenge to characterizing a cohort that is representative of an already heterogeneous target population. Our demographic results were consistent with literature demonstrating that patients with LBP are more likely to be female and aged 40–69.[28] However, one primary difference between our cohort and the target population is accounted for by our exclusion of patients with spine surgery or FBSS, which served as a proxy for expert opinion not to pursue surgery. In practice, some patients with non-specific cLBP eventually undergo fusion or disc replacement.[22] Patients with persistent or recurrent pain after surgery are considered to have FBSS.[29] As repeat surgery is rarely recommended,[30] these patients may progress to CRLBP. Ultimately, our cohort may be more heterogeneous and therefore representative of the target population than suggested by our inclusion and exclusion criteria, as we did not explicitly exclude many specific LBP diagnoses, and patients may have had spine surgery outside of the study period.
Conclusions
In the face of changing recommendations regarding the management of LBP, including greater emphasis on non-surgical, non-pharmacologic therapy,[4] and legislation surrounding opioid prescribing practices,[31] there is a growing need for progressive policy changes focused on non-opiate solutions and for private and public insurance payers to provide coverage for non-opioid analgesics prior to initiating opioids. For CRLBP, comprehensive care should include exercise, physical therapy, behavioral therapy, and complementary and alternative medicine approaches[25, 32, 33]—all covered by payers. By creating policies empowering patients to adopt non-opioid treatments, we can begin to change the culture of pain management and make an impact on LBP-related HCRU and opioid-related morbidity and mortality in the US.
Supplementary Material
Table, Supplemental Digital Content 1. Procedure codes for spine surgery and spinal cord stimulation. docx
Table, Supplemental Digital Content 2. Procedure codes for non-pharmacologic therapies classified as conventional medical management. Docx
Key Points.
The healthcare resource utilization among patients with chronic low back pain has been investigated, but few data exist for the specific population of patients who have not undergone spine surgery.
Patients with chronic, refractory low back pain experience substantial increases in healthcare costs in the first year after diagnosis.
Contrary to low back pain management guidelines, opioids were used more commonly than many non-pharmacologic therapies, even in the first year after low back pain diagnosis.
Insurance claims for several recommended non-pharmacologic therapies, which are often not covered by insurance companies, were identified for few patients.
Comprehensive care should emphasize non-opioid treatment approaches and should be covered by insurance payers.
Acknowledgements:
Dr. Lad acknowledges funding support for this research from Nevro Corp. Dr. Lad is a consultant for Abbott, Boston Scientific, Higgs Boson Health, Medtronic, Minnetronix, Nevro, and Presidio Medical. Dr. Lee and Ms. Yang acknowledge funding support by the National Center For Advancing Translational Sciences of the National Institutes of Health under Award Number UL1TR002553. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. All other authors report no conflicts of interest or funding support.
Institutional Review Board:
This study was submitted to the Duke University Health System Institutional Review Board under protocol number Pro00053624 and determined exempt.
References
- 1.Hoy D, March L, Brooks P, et al. The Global Burden of Low Back Pain: Estimates from the Global Burden of Disease 2010 Study. Ann Rheum Dis. 2014;73(6):968–74. [DOI] [PubMed] [Google Scholar]
- 2.Dagenais S, Caro J, Haldeman S. A Systematic Review of Low Back Pain Cost of Illness Studies in the United States and Internationally. Spine J. 2008;8(1):8–20. [DOI] [PubMed] [Google Scholar]
- 3.Deyo RA, Dworkin SF, Amtmann D, et al. Report of the NIH Task Force on Research Standards for Chronic Low Back Pain. Spine (Phila Pa 1976). 2014;39(14):1128–43. [DOI] [PubMed] [Google Scholar]
- 4.Maher C, Underwood M, Buchbinder R. Non-Specific Low Back Pain. Lancet. 2017;389(10070):736–47. [DOI] [PubMed] [Google Scholar]
- 5.Lemmon R, Roseen EJ. Chronic Low Back Pain. Integrative Medicine: Elsevier; 2018. p. 662–75.e3. [Google Scholar]
- 6.Koes BW, Van Tulder M, Thomas S. Diagnosis and Treatment of Low Back Pain. BMJ. 2006;332(7555):1430–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Costa LdCM, Maher CG, McAuley JH, et al. Prognosis for Patients with Chronic Low Back Pain: Inception Cohort Study. BMJ 2009;339:b3829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim LH, Vail D, Azad TD, et al. Expenditures and Health Care Utilization Among Adults With Newly Diagnosed Low Back and Lower Extremity Pain. JAMA Netw Open. 2019;2(5):e193676–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gore M, Sadosky A, Stacey BR, Tai K-S, Leslie D. The Burden of Chronic Low Back Pain: Clinical Comorbidities, Treatment Patterns, and Health Care Costs in Usual Care Settings. Spine (Phila Pa 1976). 2012;37(11):E668–E77. [DOI] [PubMed] [Google Scholar]
- 10.Stewart WF, Yan X, Boscarino JA, et al. Patterns of Health Care Utilization for Low Back Pain. J Pain Res. 2015;8:523–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elsamadicy AA, Farber SH, Yang S, et al. Impact of Insurance Provider on Overall Costs in Failed Back Surgery Syndrome: A Cost Study of 122,827 Patients. Neuromodulation. 2017;20(4):354–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Deyo RA, Hallvik SE, Hildebran C, et al. Use of Prescription Opioids Before and After an Operation for Chronic Pain (Lumbar Fusion Surgery). Pain. 2018;159(6):1147–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cherkin DC, Deyo RA, Volinn E, Loeser JD. Use of the International Classification of Diseases (icd-9-Cm) to Identify Hospitalizations for Mechanical Low Back Problems in Administrative Databases. Spine (Phila Pa 1976). 1992;17(7):817–25. [DOI] [PubMed] [Google Scholar]
- 14.Agency for Healthcare Research and Quality. Healthcare Cost and Utilization Project (HCUP) Tools and Software. Healthcare Cost and Utilization Project (HCUP). 2019. [PubMed] [Google Scholar]
- 15.Veeravagu A, Cole TS, Azad TD, Ratliff JK. Improved Capture of Adverse Events After Spinal Surgery Procedures with a Longitudinal Administrative Database. J Neurosurg Spine. 2015;23(3):374–82. [DOI] [PubMed] [Google Scholar]
- 16.Idowu OA, Boyajian HH, Ramos E, Shi LL, Lee MJ. Trend of Spine Surgeries in the Outpatient Hospital Setting Versus Ambulatory Surgical Center. Spine (Phila Pa 1976). 2017;42(24):E1429–E36. [DOI] [PubMed] [Google Scholar]
- 17.Ackerman S, Knight T, Schneider K, Holt T, Cummings J, Polly D. Comparison of the Costs of Nonoperative Care to Minimally Invasive Surgery for Sacroiliac Joint Disruption and Degenerative Sacroiliitis in a United States Commercial Payer Population: Potential Economic Implications of a New Minimally Invasive Technology. Clinicoecon Outcomes Res. 2014:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun E, Moshfegh J, Rishel CA, Cook CE, Goode AP, George SZ. Association of Early Physical Therapy with Long-Term Opioid Use Among Opioid-Naive Patients with Musculoskeletal Pain. JAMA Netw Open. 2018;1(8):e185909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stanton TR, Henschke N, Maher CG, Refshauge KM, Latimer J, McAuley JH. After an Episode of Acute Low Back Pain, Recurrence is Unpredictable and Not as Common as Previously Thought. Spine (Phila Pa 1976). 2008;33(26):2923–8. [DOI] [PubMed] [Google Scholar]
- 20.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity Measures for Use with Administrative Data. Med Care. 1998:8–27. [DOI] [PubMed] [Google Scholar]
- 21.Bureau of Labor Statistics USDoL. Consumer Price Index (CPI) Databases. Consumer Price Index. 2018. [Google Scholar]
- 22.Phillips FM, Slosar PJ, Youssef JA, Andersson G, Papatheofanis F. Lumbar Spine Fusion for Chronic Low Back Pain Due to Degenerative Disc Disease: A Systematic Review. Spine (Phila Pa 1976). 2013;38(7):E409–E22. [DOI] [PubMed] [Google Scholar]
- 23.Lassman D, Hartman M, Washington B, Andrews K, Catlin A. US Health Spending Trends by Age and Gender: Selected Years 2002–10. Health Aff (Millwood). 2014;33(5):815–22 [DOI] [PubMed] [Google Scholar]
- 24.Lin DH, Jones CM, Compton WM, et al. Prescription Drug Coverage for Treatment of Low Back Pain Among US Medicaid, Medicare Advantage, and Commercial Insurers. JAMA Netw Open. 2018;1(2):e180235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oliveira CB, Maher CG, Pinto RZ, et al. Clinical Practice Guidelines for the Management of Non-Specific Low Back Pain in Primary Care: An Updated Overview. Eur Spine J. 2018;27(11):2791–803. [DOI] [PubMed] [Google Scholar]
- 26.Chou R, Qaseem A, Snow V, et al. Diagnosis and Treatment of Low Back Pain: A Joint Clinical Practice Guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–91. [DOI] [PubMed] [Google Scholar]
- 27.Heyward J, Jones CM, Compton WM, et al. Coverage of Nonpharmacologic Treatments for Low Back Pain Among US Public and Private Insurers. JAMA Netw Open. 2018;1(6):e183044–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoy D, Bain C, Williams G, et al. A Systematic Review of the Global Prevalence of Low Back Pain. Arthritis Rheum. 2012;64(6):2028–37. [DOI] [PubMed] [Google Scholar]
- 29.Chan C-w, Peng P. Failed Back Surgery Syndrome. Pain Med. 2011;12(4):577–606. [DOI] [PubMed] [Google Scholar]
- 30.Sebaaly A, Lahoud M-J, Rizkallah M, Kreichati G, Kharrat K. Etiology, Evaluation, and Treatment of Failed Back Surgery Syndrome. Asian Spine J. 2018;12(3):574–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory Provider Review and Pain Clinic Laws Reduce the Amounts of Opioids Prescribed and Overdose Death Rates. Health Aff (Millwood). 2016;35(10):1876–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bernstein IA, Malik Q, Carville S, Ward S. Low Back Pain and Sciatica: Summary of NICE Guidance. BMJ. 2017:i6748. [DOI] [PubMed] [Google Scholar]
- 33.Qaseem A, Wilt TJ, McLean RM, Forciea MA, for the Clinical Guidelines Committee of the American College of P. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Ann Intern Med. 2017;166(7):514. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table, Supplemental Digital Content 1. Procedure codes for spine surgery and spinal cord stimulation. docx
Table, Supplemental Digital Content 2. Procedure codes for non-pharmacologic therapies classified as conventional medical management. Docx


