Abstract
Faecalibacterium prausnitzii is prevalent in the human gut and is a potential candidate for next-generation probiotics (NGPs) or biotherapeutics. However, the biodiversity and physiological characteristics of Faecalibacterium prausnitzii remain unclear. This study isolated 26 novel F. prausnitzii strains from human feces using a combination of negative screening and prime-specific PCR amplification (NSPA). Based on a 16S rRNA gene analysis, F. prausnitzii strains can be classified into two main phylogroups (phylogroups I and II), which were further clustered into five subgroups (I-A, II-B, II-C, II-D, and II-E). The ultrastructure, colony morphology, growth performance, and short-chain fatty acids (SCFAs)-producing ability were found to be variable among these F. prausnitzii isolates. The optimal pH for the isolates growth ranged between 6.0 and 7.0, while most isolates were inhibited by 0.1% of bile salts. Antimicrobial resistance profiles showed that all F. prausnitzii isolates were susceptible to vancomycin, whereas >80% were kanamycin and gentamicin resistant. Additionally, all strains can utilize maltose, cellulose, and fructose but not xylose, sorbose, and 2′-FL. Overall, our work provides new insights into the biodiversity and physiological characteristics of F. prausnitzii, as well as the choices of strains suitable for NGPs.
Keywords: F. prausnitzii, isolation, antimicrobial resistance, carbohydrate utilization, phylogenetic analysis
1. Introduction
The human gastrointestinal tract harbors a large number of microbes that facilitate digestion and nutrient absorption, affect host metabolism, and shape immunity [1]. Although the gastrointestinal tract contains 500–1000 bacterial genera, only a few are predominant (Bacteroides, Clostridium, Bifidobacterium, and Faecalibacterium) [2]. The genus Faecalibacterium, currently reclassified into the family Oscillospiraceae within the order Eubacteriales, consists of three validated species: F. longum, F. butyricigenerans, and F. prausnitzii [3,4]. F. prausnitzii is one of the predominant bacteria in the human gut, accounting for approximately 5% of the total fecal microbiota in healthy adults [5]. The relative abundance of F. prausnitzii in humans reveals that this species could play a crucial role in the gut microbiota, thereby impacting the physiological health of the host [6].
Recent studies have reported a correlation between low F. prausnitzii abundance and the risk of inflammatory bowel disease (IBD) [7,8]. In patients with Crohn’s disease (CD), a low relative population of F. prausnitzii represents a risk of recurrence within 6 months following treatment [9]. Likewise, in ulcerative colitis (UC) patients, there is an evident association between the F. prausnitzii population level and the maintenance of clinical remission [10]. Interestingly, supplementation of F. prausnitzii strains in vivo demonstrated anti-inflammatory effects in both the UC and CD models [11,12,13]. Moreover, F. prausnitzii also has a beneficial effect on improving hepatic steatosis and diabetes mellitus [14,15]. Therefore, the ingestion of F. prausnitzii might be a potential strategy for the treatment of human IBS and metabolic diseases. However, the health-promoting effect of F. prausnitzii is mostly limited to the type strain A2-165 (DSMZ 17677). Thus, there is a need to isolate more strains of F. prausnitzii for further functional characterization.
Although metagenomic studies have shown that F. prausnitzii is a predominant commensal species present in the human gut microbiome, it is difficult to isolate and culture, even under anaerobic conditions [16]. F. prausnitzii is an extremely oxygen-sensitive (ESO) bacterium that survives for <2 min when exposed to air [17]. As a consequence, few F. prausnitzii strains have been successfully isolated, resulting in the constant updating of the phylogenetic relationship among F. prausnitzii strains. Furthermore, a large number of studies concerning F. prausnitzii are performed based on metagenomic data, with scant data available on the isolation and functionality of this strain [18,19]. Therefore, the gap between microbiological and metagenomic data needs to be narrowed to better understand the beneficial effects of this species, as well as to reveal its phylogenetic profile.
The present study aimed to isolate novel F. prausnitzii strains from healthy donors and further characterize the biodiversity and physiological characteristics of these strains. Metabolic and physiological tests were performed to better understand the biological properties of the isolated strains, especially in the gastrointestinal tract. Moreover, phylogenetic analysis involving the newly isolated F. prausnitzii strains and sequences from the literature was performed to further classify their phylogroups.
2. Materials and Methods
2.1. Bacterial Strains and Growth Conditions
The reference strain A2-165 (DSM17677, Braunschweig, Germany) and newly isolated F. prausnitzii strains were grown in a modified M2GSC medium [20] at 37 °C in an anaerobic workstation (Electrotek 400TG workstation, Eletrotek, West Yorkshire, UK). The M2GSC medium consisted of (per 1000 mL): 5 g yeast extract, 4 g NaHCO3, 5 g glucose, 2 g fructose, 2 g cellobiose, 10 g casitone, 1.0 g cysteine, 0.45 g K2HPO4, 0.45 g KH2PO4, 0.9 g NaCl, 0.9 g (NH4)2SO4, 0.09 g MgSO4, 0.09 g CaCl2, 1 mg resazurin, and either 200 mL (for isolation) or 10 mL (for culture) of clarified rumen fluid.
2.2. Sample Collection and Isolation of F. prausnitzii Strains
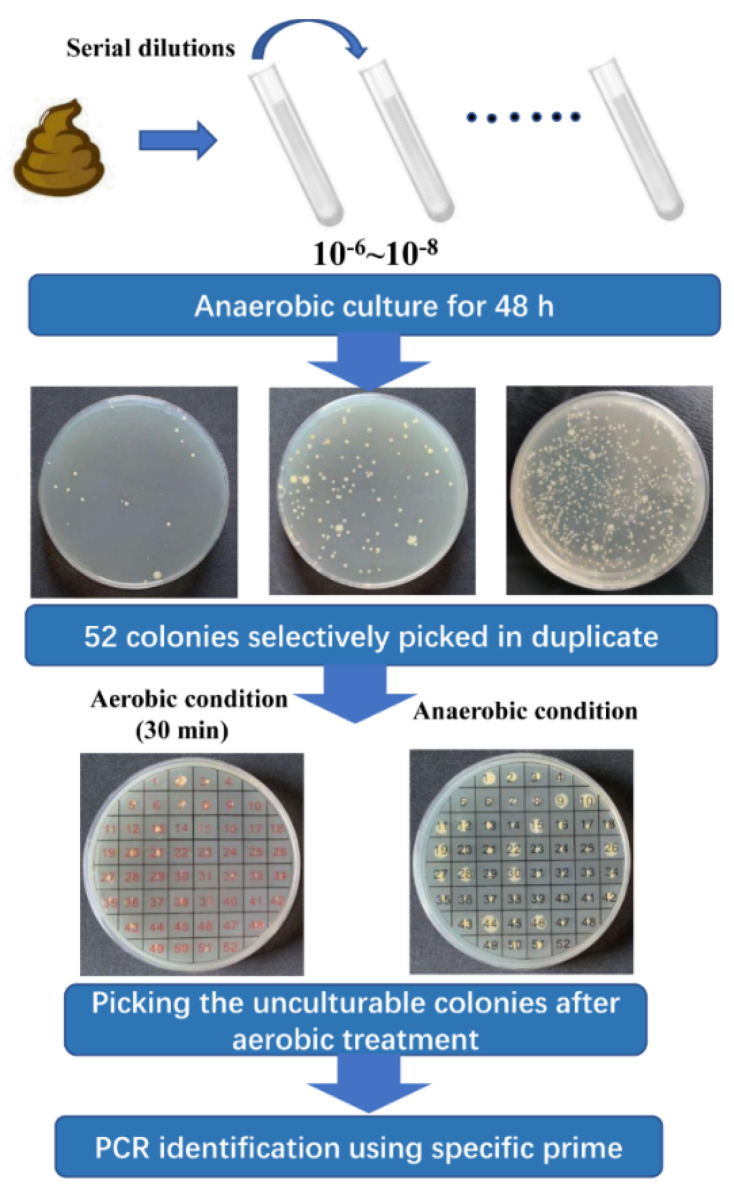
Nine healthy volunteers were recruited (Table 1) to provide fresh fecal samples, which were promptly transferred into the anaerobic workstation (N2:CO2:H2 = 8:1:1) within half an hour. All volunteers signed their informed consent and an agreement of confidentiality. The entire procedure for the isolation of F. prausnitzii strains was performed in the anaerobic workstation. The NSPA method for isolation of F. prausnitzii was carried out by referring to a previous study with some modifications [18]. In short, fecal samples were homogenized and serially diluted with phosphate-buffered saline (PBS) (0.1 M, pH 7.2). Dilutions 10−6, 10−7, and 10−8 were plated on M2GSC agar in triplicate. After 48 h of incubation, 52 varied colonies from each sample were selected and inoculated on M2GSC agar plates in duplicate and further arranged into two groups. One group was used as inoculum, while the other was treated as the negative control and exposed to the ambient air for 30 min. After 48 h of incubation, negative screening was performed to select the extremely oxygen-sensitive (EOS) strains. These EOS strains were further identified using the specific prime for F. prausnitzii (FPR-2F: 5′-GGAGGAAGAAGGTCTTCGG-3′; Fprau-645R: 5′-AATTCCGCCTACCTCTGCACT-3′) [5]. Finally, the isolated F. prausnitzii strains were stocked at -80 ℃ with 30% of glycerol. A flowchart illustrating the isolation of F. prausnitzii strains is shown in Figure 1.
Table 1.
Information about fecal samples and newly identified F. prausnitzii strains.
| Subject | Sex | Age (Years) | Isolation Source | %EOS | Identified F. prausnitzii Strains | Accession Number |
|---|---|---|---|---|---|---|
| A | M | 28 | Human feces | 42.3 | FJNHS1Y51 | OL587609 |
| B | M | 25 | Human feces | 53.5 | FJNJZ1Y10 | OL587617 |
| FJNJZ1Y25 | OL587618 | |||||
| FJNJZ1Y27 | OL587619 | |||||
| FJNJZ1Y40 | OL587620 | |||||
| C | F | 56 | Human feces | 34.6 | FJNPY1Y39 | OL587608 |
| D | F | 25 | Human feces | 38.5 | FJNQL1Y13 | OL587633 |
| FJNQL1Y33 | OL587621 | |||||
| E | M | 28 | Human feces | 57.7 | FJNLA1Y02 | OL587622 |
| FJNLA1Y08 | OL587623 | |||||
| FJNLA1Y11 | OL587624 | |||||
| FJNLA1Y27 | OL587625 | |||||
| FJNLA1Y29 | OL587626 | |||||
| FJNLA1Y38 | OL587627 | |||||
| FJNLB1Y08 | OL587628 | |||||
| FJNLB1Y11 | OL587629 | |||||
| FJNLB1Y16 | OL587630 | |||||
| FJNLB1Y25 | OL587631 | |||||
| FJNLB1Y49 | OL587632 | |||||
| F | F | 28 | Human feces | 38.5 | FJNSM1Y10 | OL587615 |
| FJNSM1Y12 | OL587616 | |||||
| G | M | 32 | Human feces | 40.4 | FJNHW1Y09 | OL587610 |
| FJNHW1Y29 | OL587611 | |||||
| H | F | 30 | Human feces | 36.5 | FJNXY1Y35 | OL587612 |
| I | M | 36 | Human feces | 51.9 | FJNZF1Y21 | OL587613 |
| FJNZF1Y25 | OL587614 |
Note: F, female; M, male.
Figure 1.
Combination of negative screening and prime-specific PCR amplification (NSPA) for isolation of F. prausnitzii strains from healthy human feces.
2.3. Polygenetic Analysis
The colony PCR amplification of 16S rRNA from F. prausnitzii isolates was performed using primers 27F (5′-AGAGTTTG ATCCTGGCAG-3′) and 1492R (5′-GGCTACCTTGTTAC GACTT-3′) according to the method described by Packeiser et al. [21]. After, the 16S rRNA amplification was sequenced in Genewiz Co., Ltd. (Suzhou, China). To perform a phylogenetic analysis of the isolated strains, the 16S rRNA gene sequences for 26 F. prausnitzii strains were compared with those from the NCBI nucleotide database (http://www.ncbi.nlm.nih.gov, accessed on 18 October 2021). Multiple sequence alignments and a phylogenetic analysis were carried out using MEGA version 7.0 software. The phylogenetic tree based on the 16S rRNA was constructed using the maximum likelihood (ML) approach. The nucleotide sequences of the 16S rRNA reported in this paper have been deposited in the GenBank database under accession numbers OL587608—OL587633 (Table 1).
2.4. Scanning Electron Microscopy (SEM)
Cultures of the F. prausnitzii isolates were washed with PBS (0.1M, pH 7.2) and fixed with 2.5% glutaraldehyde overnight at 4 ℃. Then, the fixed specimens were dehydrated, dried, mounted, and observed using a scanning electron microscope (Hitachi SU-8010, Hitachi Ltd., Tokyo, Japan).
2.5. Growth Performance
To determine the growth curve of the F. prausnitzii isolates, the inoculum of each isolate was inoculated in 100 mL of M2GSC broth and cultured anaerobically at 37 °C for 36 h. During the culture procedure, the optical density (OD) of the culture broth was determined at λ = 600 nm using a microplate reader (Multiskan Go, Thermo Scientific, Waltham, MA, USA). Colony-forming units (CFU) for the F. prausnitzii isolates were determined using the Miles and Misra Method [22].
2.6. Resistance to pH and Bile Salts
The F. prausnitzii strains were inoculated in the M2GSC broth with adjusted pH levels of 3.0, 4.0, 5.0, 6.0, 7.0, 8.0, 9.0, and 10.0. The OD of the cultures was measured at λ = 600 nm using a microplate reader (Multiskan Go, Thermo Scientific, USA). Additionally, the bacterial growth in the M2GSC broth supplemented with 0.1%, 0.25%, and 0.5% (w/v) bile salts (consisting mainly of sodium glycocholate and taurocholate; Oxoid LP0055, Basingstoke, UK) was also evaluated.
2.7. SCFAs Analysis
The F. prausnitzii isolates and the reference strain A2-165 were incubated in the M2GSC broth at 37 °C for 36 h under aerobic condition. The concentrations of acetate, propionate, butyrate, and isobutyrate in the M2GSC broth before inoculation and in the F. prausnitzii supernatants were determined using GC–MS as previously described [23]. Each measurement for analysis was done in triplicate.
2.8. Determination of Antibiotics Resistance
The minimum inhibitory concentrations (MICs) of twelve antibiotics (ampicillin, vancomycin, trimethoprim, ciprofloxacin, kanamycin, gentamicin, streptomycin, neomycin, tetracycline, erythromycin, clindamycin, and chloramphenicol) were determined using the broth microdilution methods according to ISO 10932 (IDF 223:2010) [24]. Bifidobacterium longum ATCC 15707 was used as a quality control strain. Given the weak growth in the reference medium and EOS property of the F. prausnitzii isolates, the determining method based on ISO 10932 was performed with some modifications. In short, 100 uL of serial two-fold dilutions of antibiotics were added to each well of the 96 plates, followed by the addition of 100 uL diluted suspensions of the F. prausnitzii strains (dilution in M2GSC broth with a final concentration of approximately 3 × 105). Plates were incubated in the anaerobic workstation at 37 ℃ for 36 h. MICs were recorded as the lowest concentration of an antibiotic at which visible growth was inhibited. Epidemiological cut-off (ECOFF) values were retrieved from the European Food Safety Authority (ESFA) [25].
2.9. Determination of Carbohydrate Utilization
In order to investigate the capabilities of carbohydrate utilization, 26 F. prausnitzii isolates were tested for growth on 19 different carbohydrates (glucose, maltose, fructose, arabinose, cellulose, raffinose, rhamnose, ribose, sucrose, xyloses, mannose, mannitol, galactose, lactose, trehalose, sorbose, soluble starch, inulin, and 2′-FL). The isolated strains were cultured in a modified M2GSC broth that was supplemented with a given carbohydrate (final concentration 0.5%, w/v), and the OD at 600 nm was recorded after 36 h of incubation. M2GSC broth without the addition of a carbohydrate substrate served as the negative control, while the cultures of F. prausnitzii strains in normal M2GSC broth were set as the positive control. The OD ratio of cultures with a given carbohydrate substrate to the positive control was used to distinguish no growth (<25% positive), moderate growth (25–75% positive), and good growth (>75% positive). All tests were done in triplicate.
2.10. Statistical Analysis
R (version 3.5) was used for data analysis and visualization. Results are presented as mean ± SEM. The phylogenetic tree was reconstructed using an online platform (https://www.evolgenius.info/evolview, accessed on 10 November 2021).
3. Results
3.1. Isolation and Identification of F. prausnitzii Strains
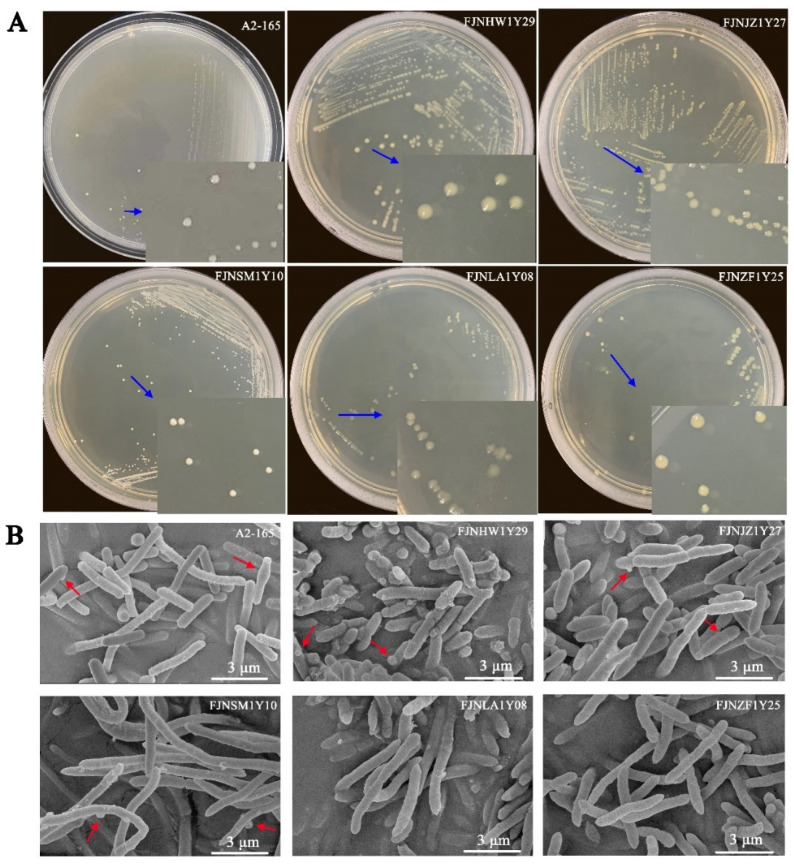
Based on the NSPA method, we identified 34.6–57.7% EOS strains in the fecal bacteria of healthy donors (Table 1). These EOS isolates were further identified by F. prausnitzii-specific primers. Consequently, 26 F. prausnitzii isolates were characterized among the selected 468 colonies (5.56%). In the M2GSC agar plate, colonies were circular or irregular, opaque to transparent, and 2–4 mm in diameter (Figure 2A).
Figure 2.
Colony and scanning electron microscopy images of F. prausnitzii strains: (A) the colony images of F. prausnitzii isolates and (B) the scanning electron microscopy images of F. prausnitzii isolates. The blue arrows show that colonies of F. prausnitzii isolates were 2–4 mm in diameter, circular, and opaque to transparent. The red arrows indicate the special ultrastructure of “swelling”. Scale bars indicate 3 μm.
SEM analyses revealed that the F. prausnitzii isolates were long bacillus (2~10 μm) with rounded ends (Figure 2B). Moreover, most F. prausnitzii isolates had a similar morphotype with cell wall “swellings”, which had already been described in the analysis of the reference strain A2-165. However, not all F. prausnitzii isolates held the phenotype of “swellings”, such as the FJNLA1Y08 and FJNZF1Y25 strains, indicating that there may be a morphological diversity within the F. prausnitzii species.
3.2. Phylogenetic Diversity of Faecalibacterium prausnitzii Strains
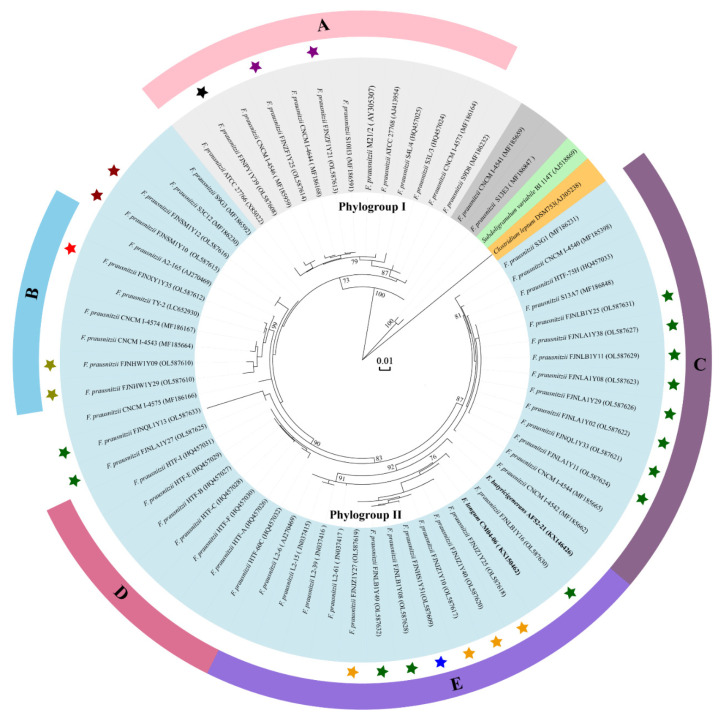
A phylogenetic tree illustrating the relationships of the 16S rRNA sequences from the F. prausnitzii strains is shown in Figure 3. Overall, the F. prausnitzii strains can be divided into two phylogroups, named phylogroup I and phylogroup II, which clearly split into five subgroups (I-A, II-B, II-C, II-D, and II-E). However, the CNCM I-4541 and S13E3 strains do not fit in any phylogroup. The S13E3 strain shares 92.88% and 93.41% 16s rRNA sequence similarities with type strains A2-165 and ATCC 27768, respectively, indicating it may not be an F. prausnitzii strain. Moreover, the FJNLB1Y16 strain showed a close relationship with F. longum CM04-06. Interestingly, several strains (FJNLB1Y25, FJNLB1Y11, FJNLB1Y16, FJNLB1Y08, and FJNLB1Y49) with distinctly different genotypes were isolated from the same donor.
Figure 3.
Phylogenetic tree of F. prausnitzii strains based on 16S rRNA gene sequences. The rooted tree was constructed with the MEGA7 software package using the maximum likelihood method. Clostridium leptum DSM 753 was used as an out-group. Bootstrap values higher than 70% are shown at the branching points. Background colors indicate different categories (light grey, phylogroup I; light blue, phylogroup II; grey, unclustered branches; light green, other genera from oscillospiraceae family; orange, out-group). The F. prausnitzii strains isolated in the present study were marked with stars (isolates derived from the same donor were presented with the same color). Colors and letters (A, B, C, D, and E) represent the tree subgroups formed by our isolated strains. The bold characters indicate type strains of two newly identified species (F. longum and F. butyricigemerams) of genus Faecalibacterium.
3.3. Growth Performance of F. prausnitzii Isolates
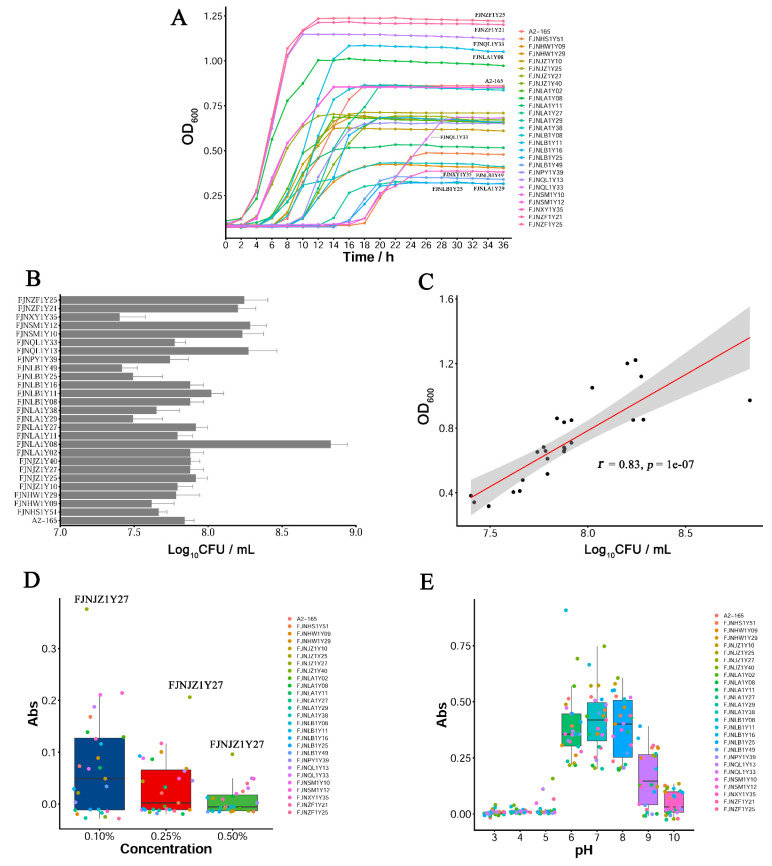
To investigate the growth performance of the F. prausnitzii isolates, the growth curve, CFU counts, and resistance to pH and bile salts were evaluated. As shown in Figure 4A, the F. prausnitzii strains displayed different growth rates in M2GSC broth. The FJNQL1Y13, FJNLA1Y08, FJNZF1Y21, and FJNZF1Y25 strains proliferated rapidly after inoculation, reaching the stationary phase 10 h later. In contrast, the FJNLA1Y29, FJNLB1Y25, FJNLB1Y49, and FJNXY1Y35 strains exhibited a relatively flat growth curve, and their optical densities during the stationary phase were between 0.3 and 0.4, which were lower than other strains. Most strains (20/27 strains) reached the stationary phase 10 to 20 h after inoculation, except for the FJNQL1Y33 and FJNXY1Y35 strains.
Figure 4.
The growth performance of F. prausnitzii strains. (A) The growth curves of F. prausnitzii isolates; (B) the determination of colony-forming units (CFU) for F. prausnitzii strains; (C) the correlation of optical density with log10 CFU/mL; (D) the effect of bile salts on bacterial growth; (E) the effect of pH on bacterial growth.
To measure the number of viable F. prausnitzii strains in M2GSC broth, CFU counts were measured. As presented in Figure 4B, the number of viable F. prausnitzii strains was calculated between 2.5 × 107 ~ 6.8 × 108 CFU/mL in the stationary phase. There was a positive correlation between log10 CFU /mL and OD600nm (Figure 4C, r = 0.83). Moreover, bile salts inhibited the growth of numerous isolates, and only a few isolates can grow in the presence of 0.1% and 0.25% (w/v) bile salts (Figure 4D). Surprisingly, the FJNJZ1Y27 isolate showed weak growth in the presence of 0.5% bile salt. The optimal pH for the growth of the F. prausnitzii strains was 6.0–7.0, and no growth occurred below a pH of 4.0–5.0 or above 8.0–9.0 (Figure 4E).
3.4. SCFAs Analysis
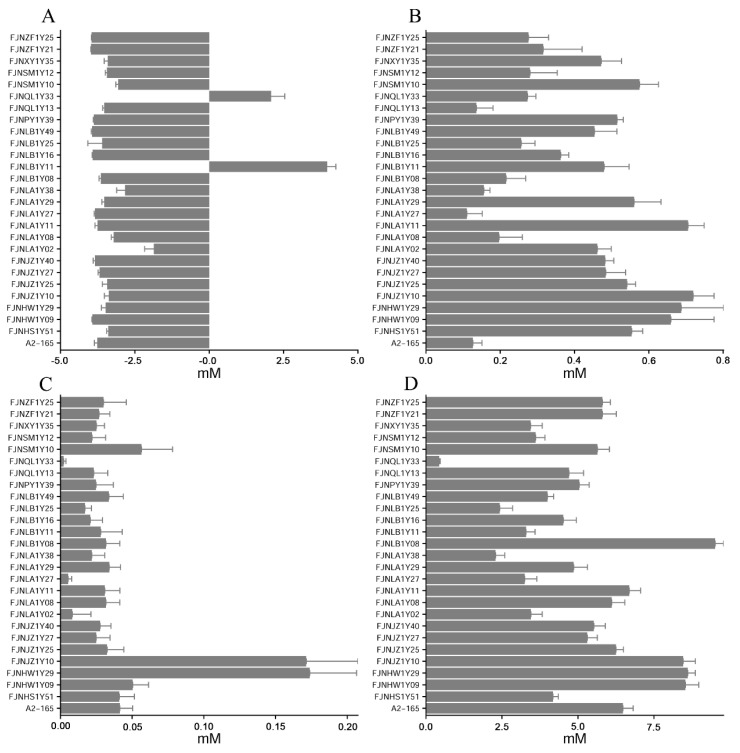
The supernatant concentrations of the acetate, propionate, isobutyrate, and butyrate are shown in Figure 5. An evident reduction in acetate concentration was observed in the F. prausnitzii strains, except for the FJNQL1Y33 and FJNLB1Y11 isolates (Figure 5A). The low content of propionate (~0.8 mM, Figure 5B) and iso-butyrate (~0.2 Mm, Figure 5C) was observed in the fermented media of the F. prausnitzii isolates. The F. prausnitzii isolates produced butyrate ranging from 2.5 to 10 mM (Figure 5D). Moreover, the FJNLB1Y08, FJNJZ1Y10, FJNHW1Y09, and FJNHW1Y29 isolates exhibited higher butyrate-producing capability than the reference strain A2-165.
Figure 5.
SCFAs production of F. prausnitzii strains in the cultural media. (A) Acetic acid concentration; (B) propionic acid concentration; (C) iso-butyric acid concentration; (D) butyric acid concentration.
3.5. Resistance to Antibiotics
The MICs of different antibiotics for the F. prausnitzii strains are presented in Table 2. Vancomycin was the only antibiotic that all of the F. prausnitzii strains were susceptible to (MICs < 2 μg/mL). Besides, the F. prausnitzii strains tended to be susceptible to ampicillin, streptomycin, tetracycline, clindamycin, and chloramphenicol, with only <25% of resistant isolates. In contrast, most of the F. prausnitzii isolates were resistant to kanamycin (85.2%, 23/27 strains) and gentamicin (81.5%, 22/27 strains). For erythromycin, the resistance level and the susceptibility level were comparable, with 40.7% and 59.3% of resistant isolates, respectively. Finally, regarding ciprofloxacin, trimethoprim, and neomycin, results were varied for different isolates, with MICs ranging from 0.25 to 64 μg/mL.
Table 2.
Antimicrobial resistance profile of the F. prausnitzii strains isolated from healthy human feces.
| Antibiotic | Distribution of Isolates | Percentage of Resistant Isolates (%) | MIC50 | MIC90 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ~0.03 | ~0.25 | 0.5 | 1 | 2 | 4 | 8 | 16 | 32 | 64 | 128 | 256 | 512 | 1024~ | ||||
| Trimethoprim | - | 1 | - | 2 | - | - | - | 1 | 3 | 20 | - | - | - | - | ND | 64 | 64 |
| Ciprofloxacin | - | 1 | 2 | 1 | 4 | 13 | 4 | 2 | - | - | - | - | - | - | ND | 4 | 8 |
| Ampicillin | - | 2 | 12 | 7 | 2 | 3 | - | 1 | - | - | - | - | - | - | 22.2 | 0.5 | 4 |
| Vancomycin | - | 16 | 7 | 2 | 2 | - | - | - | -- | - | - | - | - | 0 | 0.25 | 1 | |
| Kanamycin | - | - | - | - | - | - | 1 | 3 | 9 | 5 | 2 | - | 3 | 4 | 85.2 | 64 | 1024 |
| Gentamicin | - | - | - | - | 1 | 4 | 2 | 10 | 4 | 1 | 1 | 4 | - | - | 81.5 | 16 | 256 |
| Streptomycin | - | - | 2 | 1 | 4 | 7 | 11 | 1 | - | - | 1 | - | - | - | 7.4 | 4 | 8 |
| Tetracycline | - | 18 | 4 | 1 | - | 1 | - | - | 3 | - | - | - | - | - | 14.8 | 0.25 | 4 |
| Clindamycin | 10 | 5 | 3 | 1 | 1 | 5 | 2 | - | - | - | - | - | 7.4 | 0.25 | 4 | ||
| Erythromycin | - | 5 | 3 | 8 | 3 | - | 8 | - | - | - | - | - | - | - | 40.7 | 1 | 8 |
| Chloramphenicol | - | 5 | 5 | 4 | 6 | 1 | 3 | 3 | - | - | - | - | - | - | 22.2 | 1 | 8 |
| Neomycin | - | - | - | - | - | 3 | 11 | 9 | 1 | - | 3 | - | - | ND | 8 | 32 | |
Distribution of the minimal inhibitory concentrations (MICs) for the 26 F. prausnitzii isolates and the reference strain A2-165 (DSM 17677) among the variable antimicrobial concentration (0.03–1024 μg/mL). Vertical bars represent the breakpoint between sensitivity and resistance. The resistance breakpoints are based on Gram+ bacterium from EFSA. The MICs of each F. prausnitzii strain are present in Table S1. MIC50, the MIC value at which at least 50% isolates were inhibited; MIC90, the MIC value at which at least 90% isolates were inhibited; ND, not defined.
3.6. Carbohydrate Utilization
To assess the profile of carbohydrate utilization for the F. prausnitzii strains, in vitro growth assays were performed involving 19 carbohydrates as sole carbon sources. As shown in Table 3, all strains displayed good growth in glucose, maltose, cellulose, and fructose. Apart from FJNPY1Y39 and FJNQL1Y33, the remaining strains were able to ferment (limited) inulin. Moreover, just two strains, FJNLA1Y27 and FJNLA1Y29, were capable of (limited) growth with arabinose as the sole carbon source; similarly, only FJNLB1Y25 was able to utilize raffinose and ribose, and just two strains, FJNZF1Y21 and FJNZF1Y25, were able to weakly grow when mannitol was utilized as the sole carbon source. None of the 27 strains were able to metabolize xylose, sorbose, and 2′-FL. The fermentation capabilities for the remaining seven carbohydrates (rhamnose, sucrose, mannose, galactose, lactose, trehalose, and soluble starch) were shown to be variable among the 27 strains (Table 3).
Table 3.
Carbohydrate utilization of Faecalibacterium prausnitzii strains.
| Strains | Glu | Mal | Fru | Ara | Cel | Raf | Rha | Rib | Suc | Xyl | Man | Mai | Gal | Lac | Tre | Sor | SS | In | 2F |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A2-165 | + | + | + | - | + | - | - | - | - | - | - | - | + | + | - | - | + | + | - |
| FJNHS1Y51 | + | + | + | - | + | - | - | - | - | - | w | - | w | w | w | - | - | + | - |
| FJNJZ1Y10 | + | + | + | - | + | - | w | - | w | - | + | - | + | w | - | - | - | + | - |
| FJNJZ1Y25 | + | + | w | - | + | - | w | - | w | - | + | - | + | + | - | - | - | + | - |
| FJNJZ1Y27 | + | + | + | - | + | - | w | - | w | - | w | - | + | w | + | - | - | w | - |
| FJNJZ1Y40 | + | w | + | - | + | - | w | - | + | - | w | - | w | w | w | - | + | w | - |
| FJNPY1Y39 | + | - | + | - | - | - | w | - | - | - | - | - | - | - | - | - | - | - | - |
| FJNQL1Y13 | + | - | + | - | - | - | - | - | w | - | - | - | - | - | - | - | - | w | - |
| FJNQL1Y33 | + | w | w | - | w | - | - | - | + | - | - | - | - | - | - | - | - | - | - |
| FJNLA1Y02 | + | w | + | - | + | - | - | - | w | - | w | - | w | w | - | - | - | + | - |
| FJNLA1Y08 | + | - | + | - | - | - | - | - | - | - | w | - | - | - | - | - | - | + | - |
| FJNLA1Y11 | + | - | + | - | - | - | - | - | - | - | w | - | - | - | - | - | - | + | - |
| FJNLA1Y27 | + | + | + | w | + | - | - | - | + | - | + | - | - | - | + | - | - | + | - |
| FJNLA1Y29 | + | + | + | + | + | - | - | - | + | - | + | - | + | + | + | - | - | + | - |
| FJNLA1Y38 | + | + | + | - | + | - | - | - | w | - | w | - | w | w | + | - | - | + | - |
| FJNLB1Y08 | + | + | + | - | + | - | - | - | - | - | w | - | + | - | - | - | - | w | - |
| FJNLB1Y11 | + | w | + | - | + | - | - | - | - | - | w | - | w | w | - | - | - | w | - |
| FJNLB1Y16 | + | + | + | - | w | - | - | - | + | - | + | - | + | + | - | - | - | + | - |
| FJNLB1Y25 | + | + | w | - | + | + | + | + | + | - | w | - | + | + | + | - | w | + | - |
| FJNLB1Y49 | + | + | + | - | + | - | - | - | - | - | w | - | + | + | w | - | w | w | - |
| FJNSM1Y10 | + | + | + | - | + | - | w | - | - | - | w | - | w | w | - | - | - | w | - |
| FJNSM1Y12 | + | + | + | - | + | - | + | - | w | - | + | - | + | w | - | - | - | + | - |
| FJNHW1Y09 | + | + | w | - | + | - | - | - | w | - | + | - | w | w | + | - | - | + | - |
| FJNHW1Y29 | + | + | w | - | w | - | - | - | w | - | w | - | w | w | w | - | w | + | - |
| FJNXY1Y35 | + | + | + | - | + | - | - | - | - | - | w | - | + | - | - | - | - | w | - |
| FJNZF1Y21 | + | + | w | - | w | - | + | - | w | - | w | w | w | w | + | - | w | w | - |
| FJNZF1Y25 | + | + | w | - | w | - | + | - | w | - | w | w | w | w | + | - | w | + | - |
The F. prausnitzii strains were cultured in a modified M2GSC broth that was supplemented with a given carbohydrate (final concentration 0.5%, w/v), and the OD at 600 nm was recorded after 36 h of incubation. The cultures of the F. prausnitzii strains in normal M2GSC broth were set as the positive control. Note: +, >75% positive (good growth); -, 0–25% positive (no growth); w, 25–75% positive (moderate growth). Glu, glucose; Mal, maltose; Fru, fructose; Ara, arabinose; Cel, cellulose; Raf, raffinose; Rha, rhamnose; Rib, ribose; Suc, sucrose; Xyl, xylose; Man, mannose; Mai, mannitol; Gal, galactose; Lac, lactose; Tre, trehalose; Sor, sorbose; SS, soluble starch; In, inulin; 2F, 2′-FL.
4. Discussion
F. prausnitzii is one of the predominant species of commensal bacteria present in the human gut [26]. Recently, it has aroused extensive attention due to its significant association with various human diseases [27,28,29]. However, the biodiversity and health-promoting effects of F. prausnitzii remain unclear, which could be attributed to the small number of strains isolated thus far. The NSPA method for the isolation of F. prausnitzii was performed based on its EOS property and prime-specific PCR amplification. Compared with the method reported by Foditsch et al. [30], two main procedures, including negative screening and prime-specific PCR amplification, were added to eliminate the non-EOS bacteria, as well as to save the cost of identification. Moreover, the NSPA method increased approximately eight-fold (52 colonies vs. 6 colonies per stool sample) the screening throughput compared to the method described by Martin et al. [18], thereby raising the isolated probability of F. prausnitzii per stool sample (26 isolates/9 stool samples vs. 17 isolates/13 stool samples). Here, we identified 26 F. prausnitzii isolates based on the NSPA method. Biodiversity and physiological characterizations, including the ultrastructural features, growth performance, SCFAs metabolism, phylogenetic diversity, resistance to antibiotics, and carbohydrate utilization, were further determined.
To date, there are three species identified in the genus Faecalibacterium [3]; however, phylogenetic diversity within this genus is continuously being updated with the increase in identification of new F. prausnitzii isolates [5,18,31,32]. Overall, the F. prausnitzii strains can be divided into two main phylogroups (Figure 3, phylogroups I and II) based on the analysis of 16S rRNA gene sequences, as previously described [5,18,31]; however, the assignment for certain strains was different from those reported in previous studies. The CNCM I-4575, SG93, and S3C12 strains were previously arranged into phylogroups I [18], but these three strains were clustered into phylogroup II in the present study. This discrepancy could be attributed to the alteration of the evolutional distance with the addition of the newly isolated F. prausnitzii. For consistency with previously used taxonomy [18,31,32], the newly observed subgroups were named as I-A, II-B, II-C, II-D, and II-E (subgroups II-D and II-E were newly defined based on the genetic distance). It should be noted, however, that subgroup II-C, containing the strains CNCM I-4540, CNCM I-4542, and CNCM I-4544, appears to have a common ancestor with phylogroup I, based on the whole genome analysis [5]; this is probably caused by inconsistent similarities of the 16S rRNA gene sequences among the F. prausnitzii strains with that of the whole genomes. For instance, Fitzgerald et al. described that the CNCM I-4540 strain has a higher ANI (average nucleotide identity) with ATCC 27768 (85.2%, type strain of phylogroup I) than that with A2-165 (83.6%, type strain of phylogroup II) [5], but the result is contrary in the 16S rRNA gene sequence similarities (97.5% vs. 98.1%-). Interestingly, several strains (FJNLB1Y25, FJNLB1Y11, FJNLB1Y16, FJNLB1Y08, and FJNLB1Y49) with distinct subgroups were isolated from the same donor, indicating that population diversity could be present in a single human gut microbiome. Surprisingly, Filippis et al. identified 22 different species-level genome bins through analysis of the metagenome-assembled genomes, with 12 globally spread in the human gut [19]. Furthermore, some strains, such as FJNQL1Y13, FJNLA1Y27, and S9D8, cannot be arranged into any subgroups, suggesting that the phylogenetic relationship between F. prausnitzii remains unknown. These results suggested that the 16S rRNA of F. prausnitzii exhibits a high level of diversity, indicative of a potential for separation into new species-level taxa, which should be further verified by whole-genome sequence analysis and biochemical characterization.
When examining the physiological properties of the F. prausnitzii isolates, it is clear that cell morphotypes, as well as the growth performance, were varied. For instance, most F. prausnitzii isolates displayed similar ultrastructure with cell wall “swellings”, but these morphotypes were not observed in the FJNLA1Y08 and FJNZF1Y25 isolates, indicating that the F. prausnitzii isolates may have morphological variation (Figure 2B). Furthermore, under anaerobic condition, most F. prausnitzii isolates grew fast in the M2GSC broth, reaching the stationary phase 10 to 20 h after inoculation. In contrast, the FJNQL1Y33 and FJNXY1Y35 isolates reached the stationary phase 28 h after inoculation (Figure 4A). Additionally, the number of viable F. prausnitzii strains in the stationary phase had a large span, ranging from 2.5 × 107~6.8 × 108 CFU/mL (Figure 4B). These phenotypic differences provide new information about the cultural and physiological characteristics of F. prausnitzii.
To imitate the adverse conditions encountered by F. prausnitzii in vivo, growth at a low pH or in the presence of bile salts was determined. The appropriate pH for the growth of F. prausnitzii ranged from 6.0 to 7.0, which was consistent with the results of a previous study [30]. The median fasting gastric pH presented in adults is approximately 1.5, which increases and peaks at approximately pH 6.5 after a standard meal, then decreases continuously returning to the fasting state value over the subsequent two hours [33]. In addition, the pH in the intestine varied between 5.0 and 8.0 [34]. Thus, a low pH of the stomach is considered a barrier to the ingestion of probiotics. The results of the present study suggested that F. prausnitzii could be ingested after food consumption to escape a low gastric pH, which is detrimental to bacterial cells (Figure 4F). Moreover, the F. prausnitzii isolates were found to be vulnerable to bile salts in vitro (Figure 4E). Previous studies have demonstrated that hepatic and gastrointestinal disorders arise along with increased luminal concentrations of bile salts, explaining the low counts of F. prausnitzii displayed among individuals suffering from such disorders [35,36].
SCFAs have various positive effects on gut health, such as shaping the gut environment, influencing the physiology of the colon, or being used as energy sources by the intestinal microbiota [37,38]. Moreover, SCFAs play a crucial role in energy homeostasis, insulin sensitivity, and glucose and lipid metabolism [39]. As a dominant member of the gut microbiota, the ability of F. prausnitzii to produce SCFAs requires investigation to evaluate the potential as a health-promoting commensal bacterium. SCFAs metabolic measurements for our F. prausnitzii isolates indicated that F. prausnitzii is an acetate consumer and butyrate producer, as previously described [18,32]. Moreover, F. prausnitzii can also produce minor amounts of propionate and isobutyrate (Figure 5). Importantly, the FJNLB1Y08, FJNJZ1Y10, FJNHW1Y09, and FJNHW1Y29 isolates produced higher levels of butyrate than the reference strain A2-165, showing much more potential for future probiotic candidates.
The EFSA emphasizes the need for determining whether a candidate probiotic has no acquired or transferable resistance factor before declaring it safe for human and animal consumption and obtaining qualified presumption of safety (QSP) status [40]. Furthermore, the World Health Organization and the Food and Agriculture Organization recommend that probiotics used for food consumption should be evaluated for the safety of antibiotic resistance in commercial applications [41]. However, the antimicrobial resistance profiles of the F. prausnitzii strains were not well characterized due to the limited number of strains isolated. Here, we tested their antimicrobial susceptibilities based on the EFSA guidance. Our findings suggested that the F. prausnitzii strains exhibited high-level sensitivity to vancomycin, ampicillin, clindamycin, and chloramphenicol, as well as resistance to kanamycin, as previously described [18,32]. Surprisingly, data obtained in the present study revealed that most F. prausnitzii isolates were gentamicin resistant (MICs ranging from 2 to 256 μg/mL) and streptomycin sensitive (MICs ranging from 0.5 to 16 μg/mL), which was contrary to the results reported in the previous study [18]. This inconsistency may be attributed to the intraspecies genomic diversity of F. prausnitzii strains, resulting in phenotypic changes. According to the findings of this and previous investigations, the genomics of F. prausnitzii strains might contain kanamycin-resistant genes, as well as the gentamicin- and streptomycin-resistant genes. Given the successful transfer of antibiotic-resistant genes from a commensal to a pathogenic bacterium [42], evaluating whether there is no transferable antibiotic resistance gene is crucial for F. prausnitzii strains to be granted QSP status.
The capacity to utilize carbohydrates is critical for commensal bacteria adapting to the dynamic and multiple intestinal microbiota circumstances. We thus determined the capacities of F. prausnitzii isolates to metabolize diverse carbohydrates. Our findings showed that all F. prausnitzii isolates were able to ferment a common set of sugars, including maltose, cellulose, and fructose. In contrast, all isolates were not able to utilize 2′-FL, one of the most abundant HMOs present in the human breast milk and a significant early-life stable conization factor for gut microbes [43]. The inability to metabolize 2′-FL might metabolically explain the reason why the amount of F. prausnitzii-specific RNA in infant stools is under the detection threshold [10], indicating that F. prausnitzii hardly resides in the infant gut. Additionally, almost all strains were able to utilize inulin, a dietary fiber beneficial for human health. Inulin was approved as a functional food ingredient to improve the nutritional value of food products manufactured by the Food and Drug Administration in 2018 [44]. Given its favorable impact on commensal bacteria, inulin has been used as a prebiotic for Bifidobacterium proliferation [45,46]. Consequently, inulin might be considered as a dietary supplement to increase the population of F. prausnitzii in the human gut.
This study still has some limitations that need to be mentioned. For example, the phylogenetic relationship among the F. prausnitzii strains was not verified by the whole genome sequence analysis. Compared with the 16S rRNA gene sequence, core genomes have higher resolution for the phylogenetic analysis of intraspecies bacteria [47]. Moreover, determining the genotype–phenotype association is also our future direction.
In summary, this study isolated 26 novel F. prausnitzii strains from human feces based on the NSPA method and further investigated the biodiversity and physiological characteristics of these strains. Differences in the ultrastructural feature, growth performance, SCFAs metabolism, antibiotic resistance, and carbohydrate utilization capabilities indicated a high intraspecies diversity among F. prausnitzii strains. Furthermore, the phenotypic characterization in combination with the phylogenetic analysis proposed a potential for F. prausnitzii separating into new species-level taxa. This work substantially increased the number of F. prausnitzii strains derived in the human gut and provided new insights into the biodiversity and physiological characteristics of F. prausnitzii.
Acknowledgments
We thank Qingqing Ma, Zhen Jin, and Xinyi Wang for their technical assistance.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/microorganisms10020297/s1, Table S1: Minimum inhibitory concentrations (MIC) (μg/mL) of tested antibiotics for each F. prausnitzii isolates and reference strain A2-165.
Author Contributions
Conceptualization, W.C., H.Z., W.L. and J.Z.; methodology, W.H. and W.L.; software, W.H., Z.L. and W.G.; validation, W.H., W.L. and Z.F.; formal analysis, W.H. and W.G.; investigation, W.H., Z.L. and W.G.; resources, W.H., Z.F. and J.Z.; data curation, W.H. and W.G.; writing-original draft preparation, W.H.; writing-review and editing, H.Z., W.C., J.Z. and W.L.; visualization, W.H. and Z.L.; supervision, H.Z., J.Z. and W.L.; project administration, W.H., J.Z. and W.L.; funding acquisition, W.C., J.Z., H.Z. and W.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 31820103010) and the Collaborative Innovation Center of Food Safety and Quality Control in Jiangsu Province.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Jiangnan University (Wuxi, China).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The accession numbers for all 16S rRNA gene sequences used in this study are presented in Table 1.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chang P.V., Hao L., Offermanns S., Medzhitov R. The microbial metabolite butyrate regulates intestinal macrophage function via histone deacetylase inhibition. Proc. Natl. Acad. Sci. USA. 2014;111:2247–2252. doi: 10.1073/pnas.1322269111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harusato A., Chassaing B. Insights on the impact of diet—Mediated microbiota alterations on immunity and diseases. Am. J. Transplant. 2018;18:550–555. doi: 10.1111/ajt.14477. [DOI] [PubMed] [Google Scholar]
- 3.Zou Y., Lin X., Xue W., Tuo L., Chen M.-S., Chen X.-H., Sun C.-h., Li F., Liu S.-W., Dai Y., et al. Characterization and description of Faecalibacterium butyricigenerans sp. nov. and F. longum sp. nov., isolated from human faeces. Sci. Rep. 2021;11:11340. doi: 10.1038/s41598-021-90786-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schoch C.L., Ciufo S., Domrachev M., Hotton C.L., Kannan S., Khovanskaya R., Leipe D., McVeigh R., O’Neill K., Robbertse B., et al. NCBI Taxonomy: A comprehensive update on curation, resources and tools. Database. 2020;2020:baaa062. doi: 10.1093/database/baaa062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fitzgerald C.B., Shkoporov A.N., Sutton T.D.S., Chaplin A.V., Velayudhan V., Ross R.P., Hill C. Comparative analysis of Faecalibacterium prausnitzii genomes shows a high level of genome plasticity and warrants separation into new species-level taxa. BMC Genom. 2018;19:1–20. doi: 10.1186/s12864-018-5313-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lopez-Siles M., Duncan S.H., Garcia-Gil L.J., Martinez-Medina M. Faecalibacterium prausnitzii: From microbiology to diagnostics and prognostics. ISME J. 2017;11:841–852. doi: 10.1038/ismej.2016.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Machiels K., Joossens M., Sabino J., De Preter V., Arijs I., Eeckhaut V., Ballet V., Claes K., Van Immerseel F., Verbeke K. A decrease of the butyrate-producing species Roseburia hominis and Faecalibacterium prausnitzii defines dysbiosis in patients with ulcerative colitis. Gut. 2014;63:1275–1283. doi: 10.1136/gutjnl-2013-304833. [DOI] [PubMed] [Google Scholar]
- 8.Cao Y., Shen J., Ran Z.H. Association between Faecalibacterium prausnitzii reduction and inflammatory bowel disease: A meta-analysis and systematic review of the literature. Gastroent. Res. Pract. 2014;2014:872725. doi: 10.1155/2014/872725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sokol H., Pigneur B., Watterlot L., Lakhdari O., Bermudez-Humaran L.G., Gratadoux J.J., Blugeon S., Bridonneau C., Furet J.P., Corthier G., et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl. Acad. Sci. USA. 2008;105:16731–16736. doi: 10.1073/pnas.0804812105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miquel S., Martin R., Bridonneau C., Robert V., Sokol H., Bermudez-Humaran L.G., Thomas M., Langella P. Ecology and metabolism of the beneficial intestinal commensal bacterium Faecalibacterium prausnitzii. Gut Microbes. 2014;5:146–151. doi: 10.4161/gmic.27651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rossi O., Khan M.T., Schwarzer M., Hudcovic T., Srutkova D., Duncan S.H., Stolte E.H., Kozakova H., Flint H.J., Samsom J.N., et al. Faecalibacterium prausnitzii strain HTF-F and its extracellular polymeric matrix attenuate clinical parameters in DSS-Induced colitis. PLoS ONE. 2015;10:e0123013. doi: 10.1371/journal.pone.0123013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miquel S., Martin R., Lashermes A., Gillet M., Meleine M., Gelot A., Eschalier A., Ardid D., Bermudez-Humaran L.G., Sokol H., et al. Anti-nociceptive effect of Faecalibacterium prausnitzii in non-inflammatory IBS-like models. Sci. Rep. 2016;6:19399. doi: 10.1038/srep19399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kawade Y., Sakai M., Okamori M., Morita M., Mizushima K., Ueda T., Takagi T., Naito Y., Itoh Y., Shimada T. Administration of live, but not inactivated, Faecalibacterium prausnitzii has a preventive effect on dextran sodium sulfate-induced colitis in mice. Mol. Med. Rep. 2019;20:25–32. doi: 10.3892/mmr.2019.10234. [DOI] [PubMed] [Google Scholar]
- 14.Ganesan K., Chung S.K., Vanamala J., Xu B. Causal relationship between diet-Induced gut microbiota changes and diabetes: A novel strategy to transplant Faecalibacterium prausnitzii in preventing diabetes. Int. J. Mol. Sci. 2018;19:3720. doi: 10.3390/ijms19123720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Munukka E., Rintala A., Toivonen R., Nylund M., Yang B., Takanen A., Hanninen A., Vuopio J., Huovinen P., Jalkanen S., et al. Faecalibacterium prausnitzii treatment improves hepatic health and reduces adipose tissue inflammation in high-fat fed mice. ISME J. 2017;11:1667–1679. doi: 10.1038/ismej.2017.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miquel S., Martin R., Rossi O., Bermudez-Humaran L.G., Chatel J.M., Sokol H., Thomas M., Wells J.M., Langella P. Faecalibacterium prausnitzii and human intestinal health. Curr. Opin. Microbiol. 2013;16:255–261. doi: 10.1016/j.mib.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Duncan S.H., Hold G.L., Harmsen H.J.M., Stewart C.S., Flint H.J. Growth requirements and fermentation products of Fusobacterium prausnitzii, and a proposal to reclassify it as Faecalibacterium prausnitzii gen. nov., comb. nov. Int. J. Syst. Evol. Microbiol. 2002;52:2141–2146. doi: 10.1099/00207713-52-6-2141. [DOI] [PubMed] [Google Scholar]
- 18.Martin R., Miquel S., Benevides L., Bridonneau C., Robert V., Hudault S., Chain F., Berteau O., Azevedo V., Chatel J.M., et al. Functional characterization of novel Faecalibacterium prausnitzii strains isolated from healthy volunteers: A step forward in the use of F. prausnitzii as a next-generation probiotic. Front. Microbiol. 2017;8:1226. doi: 10.3389/fmicb.2017.01226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Filippis F., Pasolli E., Ercolini D. Newly explored Faecalibacterium diversity Is connected to age, lifestyle, geography, and disease. Curr. Biol. 2020;30:4932–4943. doi: 10.1016/j.cub.2020.09.063. [DOI] [PubMed] [Google Scholar]
- 20.Barcenilla A., Pryde S.E., Martin J.C., Duncan S.H., Stewart C.S., Henderson C., Flint H.J. Phylogenetic relationships of butyrate-producing bacteria from the human gut. Appl. Environ. Microbiol. 2000;66:1654–1661. doi: 10.1128/AEM.66.4.1654-1661.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Packeiser H., Lim C., Balagurunathan B., Wu J., Zhao H. An extremely simple and effective colony PCR procedure for bacteria, yeasts, and microalgae. Appl. Biochem. Biotechnol. 2013;169:695–700. doi: 10.1007/s12010-012-0043-8. [DOI] [PubMed] [Google Scholar]
- 22.Hedges A.J. Estimating the precision of serial dilutions and viable bacterial counts. Int. J. Food Microbiol. 2002;76:207–214. doi: 10.1016/S0168-1605(02)00022-3. [DOI] [PubMed] [Google Scholar]
- 23.Mao B., Li D., Ai C., Zhao J., Zhang H., Chen W. Lactulose differently modulates the composition of luminal and mucosal microbiota in C57BL/6J mice. J. Agric. Food Chem. 2016;64:6240–6247. doi: 10.1021/acs.jafc.6b02305. [DOI] [PubMed] [Google Scholar]
- 24.International Organization for Standardization (ISO) Milk and Milk Products: Determination of the Minimal Inhibitory Concentration (MIC) of Antibiotics Applicable to Bibidobacteria and Non-Enterococcal Lactic Acid Bacteria (LAB) ISO; Geneva, Switzerland: 2010. [(accessed on 20 July 2020)]. ISO 10932:2010 (IDF 223:2010) Available online: https://www.iso.org/standard/46434.html. [Google Scholar]
- 25.Additives E.P.o., Feed P.o.S.u.i.A., Rychen G., Aquilina G., Azimonti G., Bampidis V., Bastos M.d.L., Bories G., Chesson A., Cocconcelli P.S., et al. Guidance on the characterisation of microorganisms used as feed additives or as production organisms. EFSA J. 2018;16:e05206. doi: 10.2903/j.efsa.2018.5206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hornef M.W., Pabst O. Real friends: Faecalibacterium prausnitzii supports mucosal immune homeostasis. Gut. 2016;65:365–367. doi: 10.1136/gutjnl-2015-310027. [DOI] [PubMed] [Google Scholar]
- 27.He X., Zhao S., Li Y., Chen T. Faecalibacterium prausnitzii: A next-generation probiotic in gut disease improvement. Can. J. Infect. Dis. Med. 2021;2021:6666114. doi: 10.1155/2021/6666114. [DOI] [Google Scholar]
- 28.Quevrain E., Maubert M.A., Michon C., Chain F., Marquant R., Tailhades J., Miquel S., Carlier L., Bermudez-Humaran L.G., Pigneur B., et al. Identification of an anti-inflammatory protein from Faecalibacterium prausnitzii, a commensal bacterium deficient in Crohn’s disease. Gut. 2016;65:415–425. doi: 10.1136/gutjnl-2014-307649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tian Y., Wang K.M., Ji G.Z. Faecalibacterium prausnitzii prevents tumorigenesis in a model of colitis-associated colorectal cancer. Gastroenterology. 2017;152:S354–S355. doi: 10.1016/S0016-5085(17)31445-2. [DOI] [Google Scholar]
- 30.Foditsch C., Santos T.M., Teixeira A.G., Pereira R.V., Dias J.M., Gaeta N., Bicalho R.C. Isolation and characterization of Faecalibacterium prausnitzii from calves and piglets. PLoS ONE. 2014;9:e116465. doi: 10.1371/journal.pone.0116465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lopez-Siles M., Khan T.M., Duncan S.H., Harmsen H.J.M., Garcia-Gil L.J., Flint H.J. Cultured representatives of two major phylogroups of human colonic Faecalibacterium prausnitzii can utilize pectin, uronic acids, and host-derived substrates for growth. Appl. Environ. Microbiol. 2012;78:420–428. doi: 10.1128/AEM.06858-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Benevides L., Burman S., Martin R., Robert V., Thomas M., Miquel S., Chain F., Sokol H., Bermudez-Humaran L.G., Morrison M., et al. New insights into the diversity of the genus Faecalibacterium. Front. Microbiol. 2017;8:1790. doi: 10.3389/fmicb.2017.01790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith J.L. The role of gastric acid in preventing foodborne disease and how bacteria overcome acid conditions. J. Food Prot. 2003;66:1292–1303. doi: 10.4315/0362-028X-66.7.1292. [DOI] [PubMed] [Google Scholar]
- 34.Koziolek M., Grimm M., Becker D., Iordanov V., Zou H., Shimizu J., Wanke C., Garbacz G., Weitschies W. Investigation of pH and temperature profiles in the GI tract of fasted human subjects using the Intellicap®system. J. Pharm. Sci. 2015;104:2855–2863. doi: 10.1002/jps.24274. [DOI] [PubMed] [Google Scholar]
- 35.Jia W., Xie G., Jia W. Bile acid-microbiota crosstalk in gastrointestinal inflammation and carcinogenesis. Nat. Rev. Gastroenterol. Hepatol. 2018;15:111–128. doi: 10.1038/nrgastro.2017.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jiao N., Baker S.S., Chapa-Rodriguez A., Liu W., Nugent C.A., Tsompana M., Mastrandrea L., Buck M.J., Baker R.D., Genco R.J. Suppressed hepatic bile acid signalling despite elevated production of primary and secondary bile acids in NAFLD. Gut. 2018;67:1881–1891. doi: 10.1136/gutjnl-2017-314307. [DOI] [PubMed] [Google Scholar]
- 37.den Besten G., van Eunen K., Groen A.K., Venema K., Reijngoud D.J., Bakker B.M. The role of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J. Lipid Res. 2013;54:2325–2340. doi: 10.1194/jlr.R036012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Louis P., Flint H.J. Formation of propionate and butyrate by the human colonic microbiota. Environ. Microbiol. 2017;19:29–41. doi: 10.1111/1462-2920.13589. [DOI] [PubMed] [Google Scholar]
- 39.Canfora E.E., Jocken J.W., Blaak E.E. Short-chain fatty acids in control of body weight and insulin sensitivity. Nat. Rev. Endocrinol. 2015;11:577–591. doi: 10.1038/nrendo.2015.128. [DOI] [PubMed] [Google Scholar]
- 40.Hazards E.P.o.B. Scientific Opinion on the maintenance of the list of QPS biological agents intentionally added to food and feed (2013 update) EFSA J. 2013;11:3449. [Google Scholar]
- 41.Hill C., Guarner F., Reid G., Gibson G.R., Merenstein D.J., Pot B., Morelli L., Canani R.B., Flint H.J., Salminen S., et al. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat. Rev. Gastro. Hepat. 2014;11:506–514. doi: 10.1038/nrgastro.2014.66. [DOI] [PubMed] [Google Scholar]
- 42.Schjørring S., Krogfelt K.A. Assessment of bacterial antibiotic resistance transfer in the gut. Int. J. Microbiol. 2011;2011:312956. doi: 10.1155/2011/312956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matsuki T., Yahagi K., Mori H., Matsumoto H., Hara T., Tajima S., Ogawa E., Kodama H., Yamamoto K., Yamada T. A key genetic factor for fucosyllactose utilization affects infant gut microbiota development. Nat. Commun. 2016;7:11939. doi: 10.1038/ncomms11939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Food & Drug Administration Guidance for Industry: The Declaration of Certain Isolated or Synthetic Non-Digestible Carbohydrates as Dietary Fiber on Nutrition and Supplement Facts Labels. [(accessed on 11 August 2021)];2018 Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/guidance-industry-declaration-certain-isolated-or-synthetic-non-digestible-carbohydrates-dietary.
- 45.Gupta N., Jangid A.K., Pooja D., Kulhari H. Inulin: A novel and stretchy polysaccharide tool for biomedical and nutritional applications. Int.J. Biol. Macromol. 2019;132:852–863. doi: 10.1016/j.ijbiomac.2019.03.188. [DOI] [PubMed] [Google Scholar]
- 46.Vandeputte D., Falony G., Vieira-Silva S., Wang J., Sailer M., Theis S., Verbeke K., Raes J. Prebiotic inulin-type fructans induce specific changes in the human gut microbiota. Gut. 2017;66:1968–1974. doi: 10.1136/gutjnl-2016-313271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chung M., Munro J.B., Tettelin H., Hotopp J.C.D., Dorrestein P.C. Using core genome alignments to assign bacterial species. mSystems. 2018;3:e00236-18. doi: 10.1128/mSystems.00236-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The accession numbers for all 16S rRNA gene sequences used in this study are presented in Table 1.